- 1Department of Neurosurgery, Hôpitaux Universitaires de Genève (HUG), Geneva, Switzerland
- 2Faculty of Medicine, Université de Genève (UNIGE), Geneva, Switzerland
- 3Laboratory of Cognitive Neuroscience, Center for Neuroprosthetics & Brain Mind Institute, Ecole Polytechnique Fédérale de Lausanne (EPFL), Geneva, Switzerland
Background: Virtual Reality (VR) technologies have numerous beneficial applications for patients during hospitalization (through complete immersion in a virtual, distant place allowing to “escape” from the context of hospitalization). Their positive effects in pain and anxiety management, neurorehabilitation and psychotherapy have been demonstrated. Here, we evaluated the effects of VR on the quality of hospitalization and postoperative pain after neurosurgery.
Methods: Patients hospitalized in our department between 2019 and 2020 were prospectively enrolled and divided into a group that received a personal, 30-minutes-long, VR session using an Oculus Go ™ VR headset (VR group) or not (non-VR group). Surgeries were classified in simple or complex spinal and simple or complex cranial. Patient‘s overall satisfaction was considered as primary outcome, with secondary outcomes encompassing duration of hospitalization, pain reduction and patients’ opinion regarding VR.
Results: 161 patients were enrolled (77 in the VR group and 84 in the non-VR group). There was no statistical difference between the two groups regarding satisfaction. The VR group presented with a significantly longer duration of hospitalization and higher maximal pain. Interestingly, pain reduction during hospitalization was significantly higher in the VR group, particularly in simple surgeries and spine surgeries. A vast majority of the VR group patients appreciated their VR experience (89.2%) and advocated for its systematic use (83.8%).
Conclusion: VR can improve pain reduction during hospitalization after neurosurgery, particularly for simple spine surgeries. Furthermore, patients experiencing VR appear to appreciate it and advocate for its systematic use in neurosurgery. Further research is warranted to identify patients for whom addition of VR during hospitalization might bring the most benefit.
Introduction
Hospitalized patients frequently experience physical, emotional, and social distress that is further exacerbated by a radical change in living environment, loss of customary rights and privileges, and a high prevalence of pain (Henderson, 1976). Nearly half of hospitalized patients experience pain, of which a quarter is considered “unbearable” (Helfand and Freeman, 2009). Thus, hospital clinicians should not only consider the physical impact of illness, but also its psychosocial aspect. However, the dynamic nature of hospital medicine, coupled with limited time to spend with individual patients, poses challenges to offering such holistic approach.
When faced with upcoming surgeries, patients often claim a psychological fear of surgical failure, of anesthesia, or, more generally, of the ‘‘unknown’’ (Pritchard, 2009). A widely accepted cause of surgical anxiety is the recently increasing demands for efficiency in hospital operations, leading to less time spent by healthcare professionals to reassure patients about their well-being. Patients also invoke personal reasons for surgery-related anxiety, including sociodemographic or psychological variables as well as past surgical experiences (Karanci and Dirik, 2003). Patients under surgical distress can experience adverse effects on their mental and physiological states, and slowed postoperative recovery (Kiecolt-Glaser et al., 1998). Even patients reporting low levels of anxiety are susceptible to physiological changes, including increased respiratory rate, heart rate, blood pressure, vasoconstriction, and gastric stasis (Bailey, 2010). Intense forms of surgical distress can activate the sympathetic nervous system and downregulate immune functions (Moon and Cho, 2001). By addressing this issue, hospitals might improve surgical outcomes, patient recovery and patient psychological and physical well-being.
Efforts are currently centered on preoperative anxiety. Medical interventions, such as midazolam, and therapeutic attempts, such as music in waiting rooms, have shown mixed results (Ni et al., 2012). Treatment of pain in the acute care setting is often focused on pharmacological management, which can yield inconsistent and suboptimal pain control (Turk et al., 2011). However, extensive data reveal that adjunctive nonpharmacological techniques, such as cognitive behavioral therapy and relaxation techniques, can modify cognitions and behaviors that influence the perception of pain (Okifuji and Ackerlind, 2007).
Neurosurgery is a surgical specialty that is particularly distressing for patients because of its consequences in terms of potential postoperative complications that can be particularly disabling (Fugate, 2015). In this field, postoperative care, especially pain, is difficult to manage (Vadivelu et al., 2016) and the use of opiates is frequent. In the current context of opiate crisis (Volkow and Blanco, 2020) it is therefore essential to have effective alternative treatments for the management of analgesia.
Virtual reality (VR) technology provides an immersive, multisensory and three-dimensional (3D) environment that enables users to have modified experiences of reality by creating a sense of “presence” (Malloy and Milling, 2010; Li et al., 2011). To date, VR has been used in numerous clinical settings to help treat anxiety disorders, to control pain, to support physical rehabilitation and to distract patients during wound care (Malloy and Milling, 2010; Morris et al., 2010). For example, VR coupled with medication is effective in decreasing pain during bandage changes for severe burns (Hoffman et al., 2000a; Hoffman et al., 2000b; Hoffman et al., 2008; Carrougher et al., 2009). Similarly, VR reduces pain and provides positive distraction during routine procedures such as intravenous line placements (Gold et al., 2006) and dental procedures (Hoffman et al., 2001; Furman et al., 2009; Sato et al., 2010). Other studies reveal that VR helps in managing chronic pain conditions such as complex regional pain syndrome (Sato et al., 2010; Solcà et al., 2018) and chronic neck pain (Sarig-Bahat et al., 2010). By stimulating the visual and auditory senses (Pozeg et al., 2017), VR acts as a distraction to limit the user’s processing of nociceptive stimuli (Li et al., 2011).
Despite evidence of the benefit of VR in clinical care, its integration into the routine of hospitalization is far from easy, and several questions remain open concerning the possibilities, the challenges and the benefits for providing such care to patients of a neurosurgery unit.
This study thus aimed at evaluating the practical implications for offering VR as a freely available entertainment system during patients stays after neurosurgery (e.g. training of staff, catalogue of content, maintenance of hardware) and at evaluating its effect on quality of hospitalization. Importantly, in order to establish a profile of the target population, we also attempted to evaluate its potential for pain reduction and to identify which patients’ category might benefit the most from VR. Finally, we also asked whether patients appreciated the use of VR and whether they would recommend it in the future.
Material and Methods
Patients’ Selection and Groups Formation
Patients hospitalized in the department of Neurosurgery of the HUG (University hospital of Geneva) between January 2019 and December 2020 were prospectively recruited in the following way. Procedural instructions were given to the patients during their hospitalization. Consent to participate and basic demographic information were collected. A clinical professional recorded relevant vital sign. Reason for hospitalization was also recorded (emergency or not). When applicable, surgeries were classified in four groups: simple spine (lumbar discectomy, canal stenosis decompression, ACDF…); complex spine (TLIF, ALIF, PLIF…); simple cranial (cranioplasty, Shunt, Subdural hemorrhage…) and complex cranial (brain tumor, aneurismal clipping…). Once all preliminary data were collected, patients were randomly assigned to either the control group (non-VR group) or the VR group. A nurse or a resident (always from our neurosurgical department) installed the head mounted display on the patient’s head to display a VR simulation. Of note, there was no difference in the care of the patients (being medication, frequency and duration of interactions with physicians and nurses…) between the VR and non-VR groups except for the presence/absence of VR.
Inclusion Criteria
Adult patients (over 18 years of age) undergoing elective or urgent neurosurgical procedures (i.e., any surgical procedure at the brain or spinal levels) and capable of giving informed consent were enrolled.
Exclusion Criteria
Patients under 18 years of age (minors) or lacking the capacity to consent to the study, patients under the influence of drugs, under acute alcoholism or known to be dependent of such substances, patients with major visual impairment (strabismus, amblyopia) and patients with known untreated recurrent panic attacks or epilepsy were excluded from this study.
Analgesic Treatment of the Subjects
Enrolled patients all followed a same postoperative standard protocol. For the first 48 h (minimum duration), patients received oral morphine treatment (posology was adjusted to the patients’ weight). In some rare cases, a fentanyl pump was used to deliver medication. Morphine was then switched for paracetamol, NSAID and tramadol treatment.
Equipment and Procedure
A set of four Oculus Go ™ VR headset (1280 × 1440 per eye, 72 Hz refresh rate, 101° FOV) was purchased and stored in a closed cabinet easily accessible to the caregivers (nurses and doctors). When stored, the devices were disinfected, dried, covered and plugged for charging, ready for the next use.
The medical personnel were trained to the use of the VR headset and followed the following procedure when using the device. Firstly, both caregiver and patient cleaned their hands with an hydroalcoholic gel. Secondly, the patient’s head was covered with a hygiene cap. Thirdly, the headset was cleaned with an ethanol solution. Fourthly, the caregiver selected the VR scenario (according to the patient’s wishes) and launched the program (using the Oculus Go controller). Finally, the patient was helped to wear the headset and to adjust it to be comfortable (see Figures 1A,B).

FIGURE 1. Illustration of patients’ recruitment and VR session. (A) A patient receives explanation regarding the study protocol before giving consent for participation. (B) A patient of the VR group receives explanation on the VR devise use before a VR session. (C) Representative example of one of the five cyber-therapeutic environments: first screen of the “Forest of Serenity.”
VR Exposure
The VR exposures were freely chosen by the patient from a catalogue prepared in advance: the patient could decide based on a short description and a graphical representation. A set of five cyber-therapeutic environments (developed by the Virtual Reality Medical Center in San Diego, CA) was available: Cliff, Dream Castle, Forest of Serenity, Icy Cool World, and Drive, Walk, Bike (see Figure 1C). The patient was allowed to explore the VE during one session of up to 30 min while sitting in their bed. Throughout the simulation, all patients were conscious, had normal vision, free movement of limbs and did not have airway cannulation or hemodynamic disorders.
Data Sampling
At the end of their hospitalization, patients were provided with a written questionnaire, the Visual Analogical Scale or VAS, to evaluate their satisfaction (ranked from 1 to 10, with one being no satisfaction at all and 10 being complete satisfaction) regarding their entire stay in our department which was considered as the first outcome. Secondary outcomes were also evaluated such as the total duration of the hospitalization (in days) and the patients’ subjective evaluation of their pain (patients were provided with a written questionnaire to evaluate this outcome, ranked from 0 to 10, with 0 being no pain at all and 10 being described as “the worst pain they could ever imagine”) just after surgery and at the time of release from the hospital (written as PainMax and Painmin, respectively). The difference between the two values (ΔPain) was calculated using the following formula: ΔPain = PainMax–Painmin, and used as a marker of pain improvement during hospitalization. Finally, patients’ opinion regarding VR was assessed by asking two more questions to a subgroup of patients in the VR group (“Did you appreciate VR?,” “Do you think that VR should be systematically used during hospitalization in neurosurgery?”).
Statistical Analysis
GraphPad Prism version 9 was used for statistical analysis. Descriptive statistics were expressed as average ± standard deviations (±SD) in the tables. Both groups (VR VS non-VR) were compared using unpaired t-test for continuous values and Chi-square test in the case of categorical values.
Study Design and Ethical Approval
Data were collected in a prospective way. An informed consent was obtained from all patients included in the study. The study was undertaken in accordance with the ethical standards as defined in the Declaration of Helsinki and was approved by our local Ethical commission.
Role of the Funding Source
The funding source did not take part in any way during study design, in the analysis and interpretation of data, in the writing of the report or in the decision to submit the paper for publication. The corresponding author (PV) had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Patients and Public Involvement
Patients were not involved in any part of the research except for obtaining informed consent, completing VR session in the VR group and filling of the questionnaire.
Results
Groups
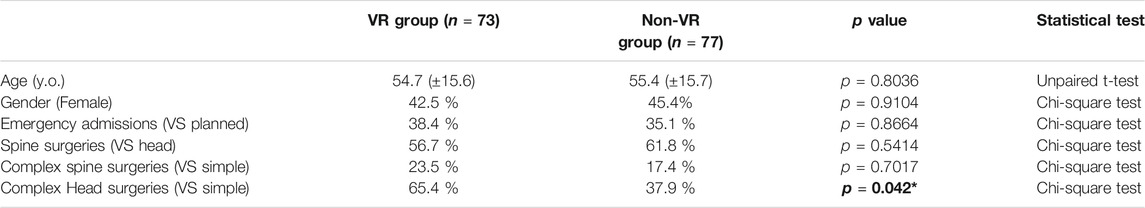
161 patients, 70 women (43%) and 91 men (54%) with a mean age of 55.1 (±15.6) years old, hospitalized in our institution were prospectively recruited between January 2019 and December 2020. 34.2% of these patients (n = 55) were hospitalized in emergency. Of note, patients hospitalized in emergency did not show any significant difference compared to “non-emergency” patients regarding the duration of stay (p = 0.3161) and maximal pain (p = 0.8006). The patients were randomly divided into a VR group (n = 77) and a control or non-VR group (n = 84). 11 patients, four in the VR group and 7 in the non-VR group, later decided to exit the study and were therefore removed from any data sampling and analysis. The patients remaining in the two groups (n = 150) were not statistically different for age, gender or the reason of their admission (emergency VS planned admission) (see Table 1).
Regarding the type of surgery, the VR group presented with a significantly higher proportion of patients with complex head surgeries (p = 0.042). There was no other statistical difference between the two groups regarding the proportion of the other types of surgeries (see Table 1). Of note, patients undergoing complex head surgeries showed significantly longer duration of hospitalization compared to patients that underwent simple spine surgery (p = 0.0176, η (Helfand and Freeman, 2009) = 0.09521) and patients undergoing complex spine surgery reported higher levels of pain immediately after surgery (p = 0.0094, η (Helfand and Freeman, 2009) = 0.2179) (See Supplementary Figure S1).
VR Patients Reported Higher Improvement in Pain During Hospitalization
We analyzed patients’ answers to the questionnaire (satisfaction and VAS) given at the end of the hospitalization for both groups (VR and non-VR). There was no difference regarding the main outcome between the two groups with a relatively high level of satisfaction in general (see Table 2). Of note, patients in the VR group presented with significantly higher pain at the beginning of the hospitalization (PainMax) (p = 0.0199, η (Helfand and Freeman, 2009) = 0.03633) and remained for a significantly longer duration in our institution compared to the non-VR group (p = 0.0319, η (Helfand and Freeman, 2009) = 0.03072) (see Table 2). There was however no statistically significant difference regarding the patients’ evaluation of their pain at the end of the hospitalization (Painmin) between the two groups. Interestingly, the difference between PainMax and Painmin (ΔPain), corresponding to the improvement in pain during the hospitalization, was significantly higher in the VR group compared to the non-VR group (p = 0.011, η (Helfand and Freeman, 2009) = 0.06961), suggesting a higher improvement regarding pain (see Table 2 and Figure 2). These results suggest that VR might improve pain recovery following neurosurgical interventions, particularly in patients presenting higher levels of pain and remaining for a longer duration in hospital.
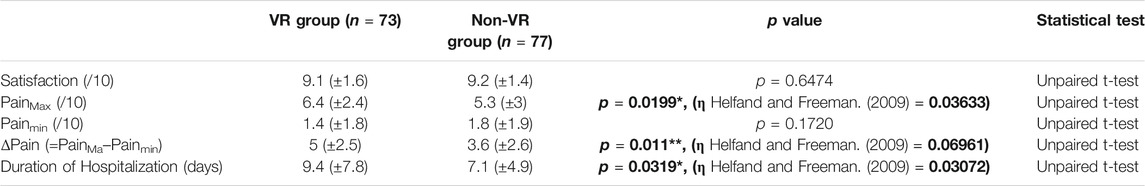
TABLE 2. Comparison of main and secondary outcomes (Average ± SD), *p < 0.05, **p <0.01, eta squared [η (Helfand and Freeman, 2009)] coefficients are written when significance was reached.
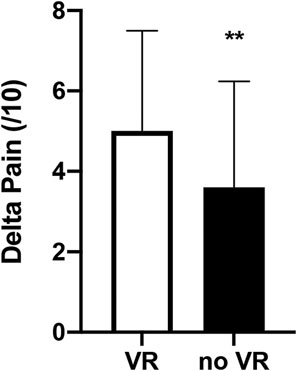
FIGURE 2. VR group shows a significantly higher pain improvement. Comparison of ΔPain (= PainMax–Painmin) between the VR and the non-VR groups (evaluated by the Visual Analogical Scale). Unpaired t-test; error bars, SD; **p < 0.01.
VR-Induced Improvement in Pain is More Pronounced for Spine and Simple Surgeries
We then further analyzed the improvement in pain by separating both groups between surgery types (simple VS complex or head VS spine). When comparing ΔPain by separating spine and head surgeries, we observed that ΔPain was significantly higher in the VR group compared to the non-VR group only for spine surgeries (p = 0.0076, η (Helfand and Freeman, 2009) = 0.08171), A similar tendency was observed for head surgeries, albeit not significant (see Table 3).
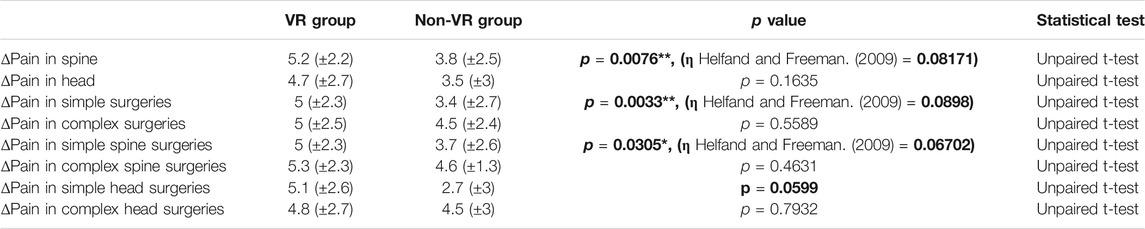
TABLE 3. ΔPain in VR VS non-VR subgroups (Average ± SD); *p < 0.05, **p <0.01, eta squared (η (Helfand and Freeman, 2009)) coefficients are written when significance was reached.
Regarding the comparison between VR and non-VR patients when separating patients in simple and complex surgeries, we observed a significant improvement in pain for the VR group only in simple surgeries (p = 0.0033, η (Helfand and Freeman, 2009) = 0.0898) (see Table 3). When dividing the simple surgeries between spine and head, we observed that the VR group showed higher ΔPain in both cases, with the difference being significant for simple spine surgeries (p = 0.0305, η (Helfand and Freeman, 2009) = 0.06702) and almost significant for simple head surgeries (p = 0.0599, η (Helfand and Freeman, 2009) = 0.007649) (see Table 3). These results suggest that VR-linked improvement in pain is more pronounced in spine and simple neurosurgical surgeries.
Patients Experiencing VR Advocate for Its Systematic Use in Neurosurgery
We finally analyzed the opinion of a randomly selected subgroup of patients that benefitted from VR (n = 37). These patients were asked 2 supplementary questions regarding VR: 1—Did you appreciate VR?; 2—Do you think that VR should be systematically used during hospitalization in neurosurgery? Interestingly, a vast majority (89.2%) of these patients appreciated their VR experience. Furthermore, a majority (83.8%) also advocated for a systematic use of VR during hospitalization in neurosurgery. These results suggest that neurosurgical patients not only appreciate but also support a systematic use of VR technology as an adjuvant therapy in neurosurgery.
Discussion
With this study, we first confirmed that integrating VR into the clinical routine of a neurosurgery unit today requires a minimal investment and a simple training of the medical team. A simple procedure for a hygienic and safe use of VR headsets could rapidly be implemented and has proven to be efficient and quick to setup, allowing us to involve more than 70 patients without a considerable workload, advocating for a more frequent use of VR.
We then further examined the level of satisfaction of patients who benefited of virtual reality after a neurosurgical intervention. There was no difference regarding the improvement of the quality of the hospital stay when patients benefitting from VR were compared to patients the control, non-VR group. However, the study suggests that VR might improve pain recovery after neurosurgical interventions, especially for patients who benefited of simple spine surgeries and remaining for longer period of times in neurosurgical departments. Furthermore, neurosurgical patients not only appreciated but also supported a systematic use of this technology as an adjuvant therapy in neurosurgery.
No Difference Regarding the Improvement of the Evaluation of the Quality of the Hospital Stay
There was no difference between VR and non-VR group regarding the satisfaction of patients on their hospital stay. This lack of difference might stem from the fact that patients in the non-VR group already reported with a really high level of satisfaction (higher than 9 on a scale of 10) regarding the quality of their hospitalization. Thus, further improvement in satisfaction due to VR could only be minimal and would not be significant.
It is important to note that the average age in our patients’ cohort was 55.1 (±15.6) years old. VR is a new technology which can be very disturbing for many people, particularly for those not experienced with new technology. Individual differences such as demographic variables (such as age), computer experience, cognitive abilities and personality factors have long been acknowledged as important in computing research (Zmud, 1979). Such individual differences were reported as significant factors in both technology acceptance and user behavior (Chua et al., 1999; Arning and Ziefle, 2006). Of note, “age” might also play an important role as an independent factor in the explanation of the variability in system acceptance and performance. Regarding performance when using such devices as VR, previous studies consistently showed that older users usually encounter greater difficulties in handling a computer device or in the acquisition of computer skills (Ziefle, 2012). Actually, despite the fact that the average patient is not familiar with new technology, VR was well accepted and not considered negatively. Such difficulties in the use of VR might lead to a reduced capability to fully immerse oneself in it, resulting in turn in a decreased effect of VR on the patients and thus, further explaining the absence of difference between the two groups.
VR Patients Reported Higher Improvement in Pain During Hospitalization
In the current study, we observed that reduction in pain during the hospitalization was significantly higher in the VR group compared to the non-VR group (p = 0.011), suggesting a higher improvement regarding pain. These results suggest that VR exposure played a role in improving pain recovery after neurosurgical interventions.
Distraction is one of the suggested mechanisms that explain the effects of VR on pain and has received considerable attention as an effective means of managing pain during both acute and invasive medical procedures. This study thus extends this knowledge by reporting VR-induced improvement in the post-operative care. While traditional medical and distraction techniques remain useful, recent technological advances in the field of VR have paved the way to substantially more engaging modes of pain management. By definition, distraction is “the engagement of cognitive and attentional resources that are necessary for pain processing” (Chen et al., 2017). It is believed that the distractor (the VR program) diminishes the perception of pain by acting on the signaling pathways that lead to pain (Gold et al., 2007; Citrome, 2014). This suggests that VR may change the activity of the body’s complex pain modulation system by acting at the cognitive level, decreasing the level of attention paid to the pain, causing the individual to no longer perceive a stimulus as painful.
Of note, patients of the VR group spent significantly more time in our department compared to patients in the non-VR group. This is explained, at least in part, by the fact that patients in the VR group underwent significantly more complex head surgeries, a subgroup of surgeries that showed the longest inpatient stay compared to others. It is important to note that this longer duration of hospitalization might also impact the pain reduction, with patients remaining longer receiving more medication against pain, and we cannot rule out that the VR group showed better pain improvement independently of VR. There is however another potential explanation to this fact as a longer duration of hospitalization might also offer the possibility, for the patients, to familiarize themselves better with the VR technology, allowing for a stronger immersion with an increased number of VR sessions. These observations suggest that patients with longer duration of hospitalization might benefit more from VR than others and that the effects of VR on patients’ pain reduction might only appear after several days of VR experience. This would suggest the existence of a “VR training” period for patients and would advocate for an early use of VR during hospitalization to allow patients to benefit from VR. This could be addressed in future studies by gathering regular pain reports and analyzing its evolution with the VR intervention as well as comparing the correlation of the level of immersion and pain reduction reported by patients with the number of VR sessions. Moreover, the introduction of a training period for the use of VR before hospitalization might improve patients’ immersion in advance, allowing for a quicker improvement after the surgery.
VR-Induced Improvement in Pain Is More Pronounced in Spine and Simple Surgeries
In this study, we report for the first time a difference in the effect of VR on postoperative pain. However, our results suggest that this difference is only present in simple (such as discal herniation or trepanation) but not complex surgeries (such as spine fixation or complex vascular surgeries). This difference might be explained in the state in which patients are after surgeries. Indeed, for the “distractive” effect or VR to take place, patients need to have sufficient cognitive abilities and patients having underwent head surgery might show neuropsychological impairments (transitory or not) that might result in a temporary incapability to “phase” with VR. The extreme pain also experienced by patients after complex surgeries, particularly in spine, might also explain some resistance to the effect of VR. These points, together with the fact that a longer hospitalization duration might improve the “immersion readiness” of the patients, need to be addressed in further research to 1) better identify patients susceptible to benefit from VR and 2) further develop VR programs and immersive capability to also reach patients that previously were resistant to it.
When further subdividing the simple surgeries between spine and head, we observed that the VR group showed higher Pain reduction in both cases, with the difference being significant for simple spine surgeries (p = 0.0305) and almost significant for simple head surgeries (p = 0.0599) (see Table 3). These results suggest that VR-linked improvement in pain is more pronounced in simple spine surgeries (albeit the results regarding simple head surgeries were also almost significant).
Until today, studies on VR in spine failed to show any beneficial effect on parameters such as pain compared to other adjuvant therapies for spinal surgery (Ahern et al., 2020). Just as our study did not show any significant change in patients’ satisfaction with overall management. What is important to note is that, even if the effect is not significantly better with VR, there is equal effect of VR compared to other therapies (such as manual therapy spinal mobilization and spinal surgery), compared to other active therapies (exercise, physical therapy (Coulter et al., 2018) and dry needling of the low back), compared to acupuncture and sham needling (Hu et al., 2018)). Furthermore, our study allowed us for the first time to identify a potential subgroup of patients for who VR might be particularly indicated and further research should aim to identify patients’ subgroups more suited for VR as VR, just like any other medical intervention, should be selected at the right moment and for the right patient.
Another thing is the fact that VR is becoming more widely available. This is likely due to recent emergence of low-cost VR technologies (Cipresso et al., 2018). A VR system poses a one-time cost to the clinic, and then it may be used repeatedly.
Patients Experiencing VR Advocate for Its Systematic Use in Post-operative Care
A crucial point for the use of VR is the capacity for patients to interact with it. Indeed, patients need to immerse themselves in VR for its effect to take place. Such paradigm entails the necessity for patients to be able to “appreciate” and “adhere” to the VR-created environment. Indeed, without any will from the patient to immerse themselves in VR, any possibility of VR being effective (being in the reduction of the patients’ pain or in the increase of their satisfaction) will be void. In this aspect, our study brings hope to the field as a vast majority (89.2%) of the subgroup of patients in the VR group, when asked, reported that they appreciated their VR experience. Furthermore, a majority of them (83.8%) also advocated for a systematic use of VR during hospitalization in neurosurgery. These results thus advocate for a more systematic use of VR in the clinical care as they demonstrate that integrating VR technology into neurosurgical care is relatively easily feasible, with both patients and hospital personal (i.e. nurses and physicians) being ready for the use of such new technology. Moreover, VR implementation is of particular interest as it presents with the potential for patients to experience further stimulation during their hospital stay without the need for an increased presence of hospital personal in the current context of limited availability of this personal due to time constraints. As it is, VR should not replace human interaction with the patients but it shows great potential as an adjuvant, empowering therapy.
This observation should encourage clinicians to further push for a more systematic use of VR in everyday neurosurgical practice as well as further research in this field to better adapt it to the very specific field of neurosurgery.
Limitations
This study presents with some limitations, already partly mentioned. Firstly, the two groups (VR and non-VR) were not homogeneous regarding the type of surgeries, with the VR group having more complex head surgeries. As such patients tended to remain for a longer period in hospital, the increased duration of hospitalization observed in the VR group might be, in part, due to this difference. Further randomized studies are required to remove this bias as it might also influence the overall satisfaction rate of the patients as-well-as the improvement in their pain. Also, only 37 patients in the VR group were asked about their opinion concerning VR and this might create a certain bias of selection. This warrants further research regarding the subjective experience of patients regarding new technologies such as VR.
Finally, it would also be important to extend the collect of background information on our sample, such as education level or past experiences with new technologies, and especially VR. Such variables might indeed influence the capability of the patient to interact with VR and, with it, their ability to immerse themselves in the virtual environment.
Conclusion
In this study, we show that VR improves pain reduction after neurosurgery. Furthermore, we show for the first time that this effect of VR on pain reduction depends on the surgery, with patients having undergone simple spine surgeries reporting the best outcome. Finally, we also show that patients that experienced VR advocate for its systematic use, confirming the fact that VR does have a place in the neurosurgical patients’ care. Our study underlines the potential for the growing clinical use of VR and underscores the need for more research in this area, especially in the identification of both the patients and surgeries that might benefit the most from it as well as in the identification of the correct period for the use of VR during hospitalization.
Data Availability Statement
Data are available from corresponding author upon reasonable request.
Ethics Statement
The study was undertaken in accordance with the ethical standards as defined in the Declaration of Helsinki and was approved by our local Ethical commission (2021-01443).
Author Contributions
Conception and design: PV, NB, and PB Acquisition of samples and data: PV, PC, NB, and CD Analysis and interpretation of data: PV, PC, BH, and PB Statistical analysis: PV and PC Drafting the article: PV, PC, BH, and PB Critically revising the article: BH, OB, KS, and PB Study supervision: OB, KS, and PB.
Funding
This research was funded by funds of the neurosurgical department of University Hospitals of Geneva dedicated to research.
Conflict of Interest
OB is member of the board and shareholder at Mindmaze SA and co-founder and shareholder at Metaphysiks Engineering SA.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2021.736122/full#supplementary-material
Abbreviations
ICU, intensive care unit; VE, virtual environment; VR, virtual reality
References
Ahern, M. M., Dean, L. V., Stoddard, C. C., Agrawal, A., Kim, K., Cook, C. E., et al. (2020). The Effectiveness of Virtual Reality in Patients with Spinal Pain: A Systematic Review and Meta‐Analysis. Pain Pract. 20 (6), 656–675. doi:10.1111/papr.12885
Arning, K., and Ziefle, M. (2006). What Older Users Expect from mobile Devices: an Empirical Survey. Linz, Austria: Proceedings.
Bailey, L. (2010). Strategies for Decreasing Patient Anxiety in the Perioperative Setting. AORN J. 92 (4), 445–460. doi:10.1016/j.aorn.2010.04.017
Carrougher, G. J., Hoffman, H. G., Nakamura, D., Lezotte, D., Soltani, M., Leahy, L., et al. (2009). The Effect of Virtual Reality on Pain and Range of Motion in Adults with Burn Injuries. J. Burn Care Res. 30 (5), 785–791. doi:10.1097/bcr.0b013e3181b485d3
Chen, K. B., Sesto, M. E., Ponto, K., Leonard, J., Mason, A., Vanderheiden, G., et al. (2017). Use of Virtual Reality Feedback for Patients with Chronic Neck Pain and Kinesiophobia. IEEE Trans. Neural Syst. Rehabil. Eng. 25 (8), 1240–1248. doi:10.1109/tnsre.2016.2621886
Chua, S. L., Chen, D.-T., and Wong, A. F. L. (1999). Computer Anxiety and its Correlates: a Meta-Analysis. Comput. Hum. Behav. 15, 609–623. doi:10.1016/s0747-5632(99)00039-4
Cipresso, P., Giglioli, I. A. C., Raya, M. A., and Riva, G. (2018). The Past, Present, and Future of Virtual and Augmented Reality Research: A Network and Cluster Analysis of the Literature. Front. Psychol. 9, 2086. doi:10.3389/fpsyg.2018.02086
Citrome, L. (2014). Ride ‘em Cowboy! the Therapeutics of Virtual Reality Technology and Simulation. Int. J. Clin. Pract. 68 (8), 931. doi:10.1111/ijcp.12496
Coulter, I. D., Crawford, C., Hurwitz, E. L., Vernon, H., Khorsan, R., Suttorp Booth, M., et al. (2018). Manipulation and Mobilization for Treating Chronic Low Back Pain: a Systematic Review and Meta-Analysis. Spine J. 18 (5), 866–879. doi:10.1016/j.spinee.2018.01.013
Fugate, J. E. (2015). Complications of Neurosurgery. Contioum: Lifelong Learn. Neurol. 21 (5 Neurocritical Care), 1425–1444. doi:10.1212/con.0000000000000227
Furman, E., Jasinevicius, T. R., Bissada, N. F., Victoroff, K. Z., Skillicorn, R., and Buchner, M. (2009). Virtual Reality Distraction for Pain Control during Periodontal Scaling and Root Planing Procedures. J. Am. Dental Assoc. 140 (12), 1508–1516. doi:10.14219/jada.archive.2009.0102
Gold, J. I., Belmont, K. A., and Thomas, D. A. (2007). The Neurobiology of Virtual Reality Pain Attenuation. CyberPsychology Behav. 10 (4), 536–544. doi:10.1089/cpb.2007.9993
Gold, J. I., Kim, S. H., Kant, A. J., Joseph, M. H., and Rizzo, A. S. (2006). Effectiveness of Virtual Reality for Pediatric Pain Distraction during IV Placement. CyberPsychology Behav. 9 (2), 207–212. doi:10.1089/cpb.2006.9.207
Helfand, M., and Freeman, M. (2009). Assessment and Management of Acute Pain in Adult Medical Inpatients: a Systematic Review. Pain Med. 10 (7), 1183–1199. doi:10.1111/j.1526-4637.2009.00718.x
Henderson, A. R. (1976). Reference Corner. J. Clin. Ultrasound 4 (5), 378–383. doi:10.1002/jcu.1870040518
Hoffman, H. G., Doctor, J. N., Patterson, D. R., Carrougher, G. J., and Furness, T. A. (2000). Virtual Reality as an Adjunctive Pain Control during Burn Wound Care in Adolescent Patients. Pain 85 (1-2), 305–309. doi:10.1016/s0304-3959(99)00275-4
Hoffman, H. G., Patterson, D. R., Carrougher, G. J., and Sharar, S. R. (2001). Effectiveness of Virtual Reality-Based Pain Control with Multiple Treatments. The Clin. J. Pain 17 (3), 229–235. doi:10.1097/00002508-200109000-00007
Hoffman, H. G., Patterson, D. R., and Carrougher, G. J. (2000). Use of Virtual Reality for Adjunctive Treatment of Adult Burn Pain during Physical Therapy: a Controlled Study. Clin. J. Pain 16 (3), 244–250. doi:10.1097/00002508-200009000-00010
Hoffman, H. G., Patterson, D. R., Seibel, E., Soltani, M., Jewett-Leahy, L., and Sharar, S. R. (2008). Virtual Reality Pain Control during Burn Wound Debridement in the Hydrotank. Clin. J. Pain 24 (4), 299–304. doi:10.1097/ajp.0b013e318164d2cc
Hu, H.-T., Gao, H., Ma, R.-J., Zhao, X.-F., Tian, H.-F., and Li, L. (2018). Is Dry Needling Effective for Low Back Pain? Medicine (Baltimore) 97 (26), e11225. doi:10.1097/md.0000000000011225
Karanci, A. N., and Dirik, G. (2003). Predictors of Pre- and Postoperative Anxiety in Emergency Surgery Patients. J. Psychosomatic Res. 55 (4), 363–369. doi:10.1016/s0022-3999(02)00631-1
Kiecolt-Glaser, J. K., Page, G. G., Marucha, P. T., MacCallum, R. C., and Glaser, R. (1998). Psychological Influences on Surgical Recovery: Perspectives from Psychoneuroimmunology. Am. Psychol. 53 (11), 1209–1218. doi:10.1037/0003-066x.53.11.1209
Li, A., Montaño, Z., Chen, V. J., and Gold, J. I. (2011). Virtual Reality and Pain Management: Current Trends and Future Directions. Pain Manage. 1 (2), 147–157. doi:10.2217/pmt.10.15
Malloy, K. M., and Milling, L. S. (2010). The Effectiveness of Virtual Reality Distraction for Pain Reduction: a Systematic Review. Clin. Psychol. Rev. 30 (8), 1011–1018. doi:10.1016/j.cpr.2010.07.001
Moon, J.-S., and Cho, K.-S. (2001). The Effects of Handholding on Anxiety in Cataract Surgery Patients under Local Anaesthesia. J. Adv. Nurs. 35 (3), 407–415. doi:10.1046/j.1365-2648.2001.01855.x
Morris, L. D., Louw, Q. A., and Crous, L. C. (2010). Feasibility and Potential Effect of a Low-Cost Virtual Reality System on Reducing Pain and Anxiety in Adult Burn Injury Patients during Physiotherapy in a Developing Country. Burns 36 (5), 659–664. doi:10.1016/j.burns.2009.09.005
Ni, C. H., Tsai, W. H., Lee, L. M., Kao, C. C., and Chen, Y. C. (2012). Minimising Preoperative Anxiety with Music for Day Surgery Patients - a Randomised Clinical Trial. J. Clin. Nurs. 21 (5-6), 620–625. doi:10.1111/j.1365-2702.2010.03466.x
Okifuji, A., and Ackerlind, S. (2007). Behavioral Medicine Approaches to Pain. Med. Clin. North America 91 (1), 45–55. doi:10.1016/j.mcna.2006.10.008
Pozeg, P., Palluel, E., Ronchi, R., Solcà, M., Al-Khodairy, A.-W., Jordan, X., et al. (2017). Virtual Reality Improves Embodiment and Neuropathic Pain Caused by Spinal Cord Injury. Neurology 89 (18), 1894–1903. doi:10.1212/wnl.0000000000004585
Pritchard, M. J. (2009). Identifying and Assessing Anxiety in Pre-operative Patients. Nurs. Stand. 23 (51), 35–40. doi:10.7748/ns2009.08.23.51.35.c7222
Sarig-Bahat, H., Weiss, P. L., and Laufer, Y. (2010). Neck Pain Assessment in a Virtual Environment. Spine 35 (4), E105–E112. doi:10.1097/brs.0b013e3181b79358
Sato, K., Fukumori, S., Matsusaki, T., Maruo, T., Ishikawa, S., Nishie, H., et al. (2010). Nonimmersive Virtual Reality Mirror Visual Feedback Therapy and its Application for the Treatment of Complex Regional Pain Syndrome: an Open-Label Pilot Study. Pain Med. 11 (4), 622–629. doi:10.1111/j.1526-4637.2010.00819.x
Solcà, M., Ronchi, R., Bello-Ruiz, J., Schmidlin, T., Herbelin, B., Luthi, F., et al. (2018). Heartbeat-enhanced Immersive Virtual Reality to Treat Complex Regional Pain Syndrome. Neurology 91 (5), e479–e489. doi:10.1212/wnl.0000000000005905
Turk, D. C., Wilson, H. D., and Cahana, A. (2011). Treatment of Chronic Non-cancer Pain. The Lancet 377 (9784), 2226–2235. doi:10.1016/s0140-6736(11)60402-9
Vadivelu, N., Kai, A., Tran, D., Kodumudi, G., Legler, A., and Ayrian, E. (2016). Options for Perioperative Pain Management in Neurosurgery. J. Pain. Res. 9, 37–47. doi:10.2147/jpr.s85782
Volkow, N. D., and Blanco, C. (2020). The Changing Opioid Crisis: Development, Challenges and Opportunities. Mol. Psychiatry 26, 218. doi:10.1038/s41380-020-0661-4
Ziefle, K. Aa. M. (2012). Ask and You Will Receive: Training Novice Adults to Use a PDA in an Active Learning Environment. Hershey, PA: Information Science Reference.
Keywords: virtual reality, satisfaction, pain improvement, patients’ selection, neurosurgery
Citation: Vayssiere P, Constanthin PE, Baticam NS, Herbelin B, Degremont C, Blanke O, Schaller K and Bijlenga P (2021) Use of Virtual Reality to Improve the Quality of the Hospital Stay for Patients in Neurosurgery. Front. Virtual Real. 2:736122. doi: 10.3389/frvir.2021.736122
Received: 04 July 2021; Accepted: 30 August 2021;
Published: 06 October 2021.
Edited by:
Thomas C. Sauter, Insel Gruppe AG, SwitzerlandCopyright © 2021 Vayssiere, Constanthin, Baticam, Herbelin, Degremont, Blanke, Schaller and Bijlenga. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pia Vayssiere, cGlhLnZheXNzaWVyZUBoY3VnZS5jaA==
†These authors share first authorship
 Pia Vayssiere1,2*†
Pia Vayssiere1,2*† Paul E. Constanthin
Paul E. Constanthin Bruno Herbelin
Bruno Herbelin Olaf Blanke
Olaf Blanke Karl Schaller
Karl Schaller Philippe Bijlenga
Philippe Bijlenga