
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Virtual Real., 05 January 2022
Sec. Virtual Reality in Medicine
Volume 2 - 2021 | https://doi.org/10.3389/frvir.2021.722558
This article is part of the Research TopicThe Use of Virtual-Reality Interventions in Reducing AnxietyView all 8 articles
Diaphragmatic breathing and progressive muscle relaxation (PMR) are an effective way for relaxation training and anxiety control, but their use is not common to the general public. Today, as the need for non-face-to-face contact increases, virtual reality (VR)-based self-training is gaining attention in public health. This study aimed to evaluate the feasibility of the newly developed VR-based relaxation training program. Both diaphragmatic breathing and PMR can be trained without an assistant using this VR application in three steps: 1) learning in a virtual clinic, 2) review in a comfortable virtual environment, and 3) practice in outdoor virtual environments. Self-training is recommended on a 3-weeks schedule with a total of 4–6 trials per day for 4 days a week. Thirty-one healthy volunteers were divided into the VR (n = 15) and worksheet (n = 16) groups, and participated in self-training under similar conditions as much as possible. Multiple evaluations were performed before, during, and after self-training. The change rates of all psychological and psychophysiological measures before and after self-training did not significantly differ between the two groups. The levels of tension after breathing practices showed no group difference, whereas those after PMR practices were significantly lower in the VR group than in the worksheet group. In the VR group, trials of outdoor practices tended to induce a decrease of the tension level, particularly after outdoor breathing trials. The VR group gave a practicable score of 70 points or more, average 43.5, and average 180.3 for usability, cybersickness, and presence of this program, respectively. These results suggest that the VR-based relaxation self-training program can be used by healthy people as a means of relaxation. In the use of this program, diaphragmatic breathing may be used more easily, but the benefit of using VR is higher in PMR. These findings provide justification for a randomized controlled study of whether this program can be used for stress relief in the general population and, furthermore, treatment of patients with anxiety disorders.
Anxiety disorders are very common worldwide, with the global current prevalence of 7.3% (Baxter et al., 2013). Excessive anxiety causes not only mental health problems, but also various problems such as functional impairment (McKnight et al., 2016), poor quality of life (Prisnie et al., 2018), and negative effects on physical health (Fields et al., 2012; Kidwell et al., 2015). Therefore, proper control of anxiety in daily life is very important in preventing deterioration in physical and mental health and maintaining a healthy life. It has been reported through a meta-analysis study that various types of relaxation training are generally effective in alleviating anxiety (Manzoni et al., 2008).
One example of relaxation training is diaphragmatic breathing, which is a breathing technique that increases breathing volume by contracting the diaphragm muscles to provide more air to the body. Breathing therapy for anxiety disorders using this technique has been used as a component of cognitive behavioral therapy (CBT) (Barlow et al., 1989; Norton and Price, 2007) or the sole component (Hibbert and Chan, 1989; Han et al., 1996). Diaphragmatic breathing effectively reduces anxiety in patients with a variety of diseases in clinical settings (Jiménez-Rodríguez et al., 2019; Grinberg et al., 2020) and in care recipients in community settings (Chen et al., 2017). In terms of the physiological mechanism, diaphragmatic breathing increases the partial pressure of carbon dioxide to normal levels by counteracting hyperventilation in panic patients (Kim et al., 2012), and has a relaxing effect on the autonomic nervous system by strengthening parasympathetic activity (Subbalakshmi et al., 2014). These effects may be due to secondary responses to respiration control, but additional mechanisms may be involved. For instance, diaphragmatic breathing can improve sustained attention and decrease negative affect and cortisol responses to stress (Ma et al., 2017).
Another example is progressive muscle relaxation (PMR), which involves sequentially alternating tension and relaxation in all of the body’s large muscle groups. This therapy has been used as a good means of controlling anxiety in patients with anxiety disorders (Conrad and Roth, 2007). The use of PMR also improves quality of life by reducing anxiety in medically or surgically ill patients (Cheung et al., 2003; Zhao et al., 2012). In particular, cancer patients undergoing chemotherapy can benefit from PMR to reduce their anxiety (Molassiotis et al., 2002; Charalambous et al., 2015; Pelekasis et al., 2017). There is a report that PMR reduces anxiety and improves the sleep quality even in patients with COVID-19 (Özlü et al., 2021). The physiological mechanism of PMR is uncertain due to the lack of related studies. However, since PMR does not depend on breathing control, a physiological mechanism different from diaphragmatic breathing can be expected to act, and there have been reports of such. For instance, while both diaphragmatic breathing and PMR provide good improvement in psychological relaxation level, physiological relaxation as measured by electrodermal activity was provided by PMR, but not by diaphragmatic breathing (Toussaint et al., 2021).
According to recent technological innovations, CBT or therapeutic training is developing into a more effective therapy through the application of virtual reality (VR). This technology has been most commonly applied to the management of anxiety disorders in the field of psychiatry (Carl et al., 2019), and has also provided a useful means for the treatment of other mental disorders such as schizophrenia (Park et al., 2011), depression (Migoya-Borja et al., 2020), eating disorder (Marco et al., 2013), and various addictive disorders (Segawa et al., 2019). The reason VR was particularly useful in managing anxiety was that it was advantageous for exposure to objects or situations of fear through the ability to reproduce various daily life environments repeatedly by grade. Accordingly, VR exposure therapy has been employed in treating various types of anxiety, including acrophobia (Emmelkamp et al., 2001), arachnophobia (Boucharda et al., 2006), agoraphobia (Cárdenas et al., 2006; Malbos et al., 2013), fear of flying (Tortella-Feliu et al., 2011), social anxiety disorder (Anderson et al., 2013; Kampmann et al., 2016), and posttraumatic stress disorder (Kothgassner et al., 2019).
For individuals with anxiety, diaphragmatic breathing and PMR are a kind of coping training that needs to be learned rather than exposure. In fact, VR has been a useful tool for providing efficient education and learning methods. Real-world training has a number of limitations, such as time consuming for setting up the site and traveling to the site, the high cost of hiring a trainer, and the gap between the training content and the actual training site, whereas VR-based training can reduce the cost of training while increasing the number of training scenarios and allow trainees to experience a virtual place related to the training content while learning in the comfort of their personal site (Xie et al., 2021). In terms of the cost and site, home training videos and websites are also useful for self-training or rehabilitation (Moore et al., 2009; Lai et al., 2016; Palazzo et al., 2016), but the advantages of VR technology, such as being able to access simulated human bodies in a safe, ethical, and repetitive way, producing objective measures of performance, and allowing real-time feedback to trainees cannot be utilized in these ways. Therefore, VR has been used to facilitate learning and evaluation and improve training in numerous medical areas, including medical education (Scalese et al., 2008), surgical training (Alaker et al., 2016; Sheik-Ali et al., 2019), and education of endoscopic techniques (Khan et al., 2019).
Meanwhile, the recent increase in the availability of mobile VR equipment provides a favorable environment for personalized learning. Accordingly, we have introduced the application of the self-training method using mobile VR to the treatment of several phobias (Hong et al., 2017; Kim et al., 2017). With the pressing need for an option of relaxation training that is easily accessible to individuals with anxiety, we have developed a mobile-based VR program that would allow them to train alone. Furthermore, with COVID-19 outbreak worldwide in 2020 and the increasing need for non-face-to-face contact, VR-based self-managements are gaining attention in the medical field, especially in psychiatry. Recently, a self-management relaxation tool using mobile VR was introduced, which used a method of gaining stability by navigating peaceful 3-D natural environments (Veling et al., 2021). Unlike this navigation method, we developed a VR self-training program that allows individuals to learn diaphragmatic breathing and PMR in a virtual training room and to execute the learned contents in outdoor environments that cause anxiety.
Our VR program is the mobile-based self-learning application that offers relaxation training without human support. This study aimed to summarize the implementation method of this VR self-training program and to preliminarily evaluate its feasibility in healthy adults before applying it to individuals with high level of anxiety. For this aim, we compared psychological and psychophysiological changes before and after self-training and satisfaction with use between the groups using this VR program versus a worksheet for learning diaphragmatic breathing and PMR. We expected that the VR group may feel more uncomfortable in use due to frequent mechanical operations, but more easily learn the training contents than the worksheet group. Based on these expectations and the benefits of VR, we hypothesized that the usability would be scored as more inconvenient in the VR group than in the worksheet group, but the levels of tension would be lower after breathing and PMR practices.
Participants were recruited through open Internet advertisement among healthy volunteers who were aged between 19 and 60 years. They were verified for normal intellectual level by a clinical psychologist (HK) using Korean Wechsler Adult Intelligence Scale-IV (K-WAIS-IV) short form (Choe et al., 2014), had no significant psychiatric illness, had no history of brain damage or any neurological disorders, had no serious physical illness, and were not pregnant. Thirty-one participants who met these inclusion criteria were randomly assigned to the VR group (n = 15) and worksheet group (n = 16) using a program containing a random number generator and stratified randomization of sex and age. The worksheet was a 10-page document of a text and illustrations produced by the research team, explaining how to perform diaphragmatic breathing and PMR. All participants signed an informed consent form, and this study was approved by the institutional review board of Gangnam Severance Hospital.
This section presents the design of our Virtual Relaxation Training System (VRTS), is outlined in Figure 1. In the main menu shown after the login process, two icons are presented to the user to enter the diaphragmatic breathing module or PMR module. Each module consists of three steps, including 1) learning in a virtual clinic, 2) review in a comfortable virtual environment, and 3) practice in outdoor virtual environments. The comfortable environments in the second step are the beach and studio, and the outdoor environments in the third step are the elevator, theater, subway, taxis, and airplane, which are well known places that provoke claustrophobia or panic symptoms. These environments were created with a 3D VR animation or a video filmed a real scene using a 360-degree 3D camera (Insta360 Pro, Insta360 Inc., Irvine, CA).
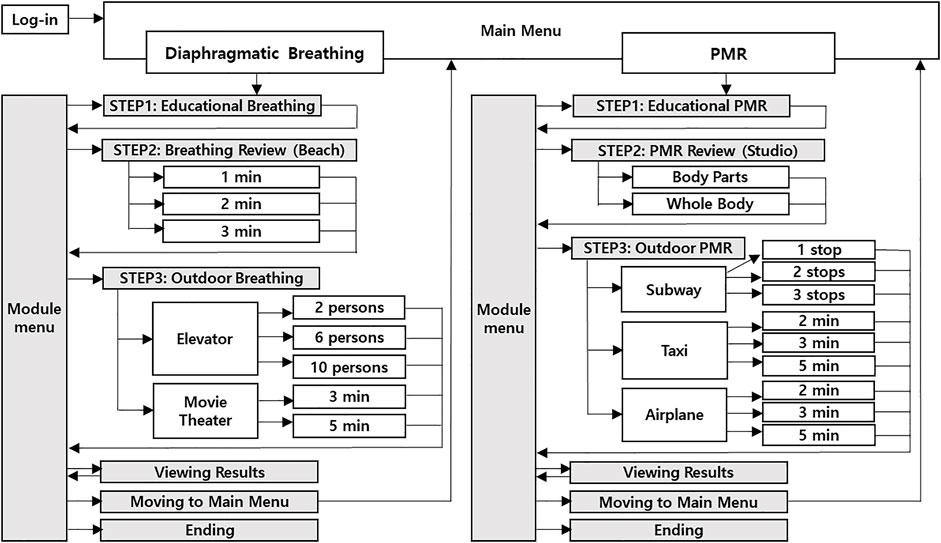
FIGURE 1. Configuration diagram of the Virtual Relaxation Training System for diaphragmatic breathing and progressive muscle relaxation (PMR).
The virtual environments are displayed via the head-mounted display (HMD), which consists of a Samsung Galaxy S9 latched onto Samsung Gear VR allowing a 360° view with 96° field-of-view. The users can execute the VRTS by themselves based on to the built-in instructions presented as text on the screen or by voice via the audio system, and can proceed to the next step by clicking the icons with a spear-shaped cursor on the screen using the controller, an accessory of Samsung Gear VR. The user is informed that the training can be stopped by taking off the HMD, when it is no longer possible to continue experiencing the virtual environment due to cybersickness or intensifying anxiety.
By selecting the diaphragmatic breathing icon from the main menu, the user enters the virtual clinic, in which he/she sits face to face with a therapist, listens to explanations, and follows the movements. The scene in the virtual clinic was created by filming the therapist explaining the diaphragmatic breathing method step by step using a 360-degree 3D camera. While the therapist explains, a circle-shaped help video of the assistant’s breathing scene and abbreviated text tips are presented to the right of the therapist (Figure 2A). The main content of the training consists of inhaling for 2 s to make the stomach bulge, with one hand on the stomach and the other on the chest, and slowly exhaling for the next 4 s. When listening and following explanations are finished, the scene automatically goes to the diaphragmatic breathing module menu. For users who do not need to hear the explanation repeatedly, a skip icon is provided in the upper left corner of the screen, and the user can move to the diaphragmatic breathing module menu at any time by clicking this icon. Six icons for re-entering the step 1, entering the step 2, entering the step 3, viewing results, moving to main menu, and ending are presented in the diaphragmatic breathing module menu.
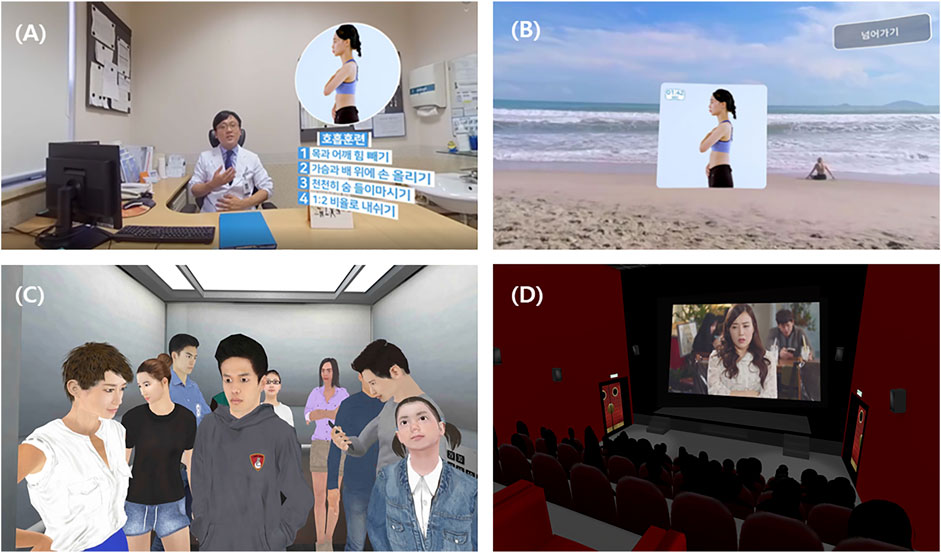
FIGURE 2. A training course of diaphragmatic breathing. Three steps included education breathing in a virtual clinic (A), review in a comfortable virtual environment (B), and practice in outdoor virtual environments: elevator (C) and movie theater (D).
When this step for reviewing the learned techniques in a comfortable virtual environment is selected in the diaphragmatic breathing module menu, the user is placed on a quiet beach filmed with a 360-degree 3D camera, and three icons are presented on the screen to select a training length of 1, 2, or 3 min. The user is allowed to stay on the beach for the suggested length of time by selecting one of them, and can relieve tension by breathing according to the therapist’s voice guidance while watching a help video of the assistant’s motion played in the center of the screen (Figure 2B). After the given time has elapsed, the scene automatically goes to the diaphragmatic breathing module menu. The user can finish this step at any time by clicking a skip icon provided in the upper right corner.
When this step for trying diaphragmatic breathing in outdoor virtual environments that simulate busy real life is selected in the diaphragmatic breathing module menu, icons are presented that allow the user to select one of three conditions inside the elevator and two conditions in a movie theater so that the user can experience tension-producing conditions on different difficulty levels and select any condition according to his or her needs. When one of the elevator conditions is selected, the user starts with the scene standing in front of the elevator door, stays inside the elevator where 2, 6, or 10 people ride together, and ends with the scene where the door opens when arriving at the destination. This virtual environment was created with animated graphics (Figure 2C). When one of the movie theater conditions is selected, the user sits in an auditorium in a dark theater and enjoys a movie for 3 or 5 min, and the scene ends automatically after a given time. This scene was produced in a way that an actual movie film was played in the screen of a virtual theater environment created with animated graphics (Figure 2D). In these environments, the user can practice diaphragmatic breathing according to the therapist’s voice guidance while watching a help video of the assistant’s motion played in the upper right corner of the screen. When the scene is over, it returns to the diaphragmatic breathing module menu, and the user can finish this step at any time by clicking a skip icon provided in the upper left corner.
By selecting the PMR icon from the main menu, the user enters the virtual clinic, which was created by filming the therapist explaining the PMR techniques step by step. All conditions such as the method of creating a virtual environment, the appearance of the therapist and assistant, the method of explaining, and the methods of ending and skipping are the same as the diaphragmatic breathing module (Figure 3A). The main content of the training is to forcefully contract the muscles for 10 s and then slowly relax them for 20 s in the order of the arms, legs, chest and abdomen, shoulders, neck, and whole body. When the scene is finished, it automatically goes to the PMR module menu, in which six icons for re-entering the step 1, entering the step 2, entering the step 3, viewing results, moving to main menu, and ending are presented.
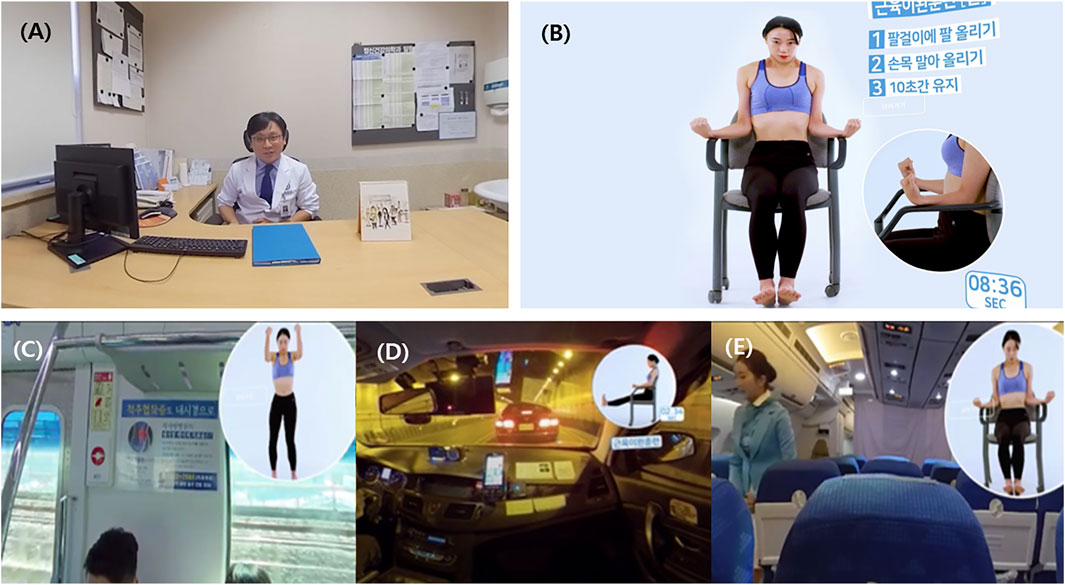
FIGURE 3. A training course of progressive muscle relaxation. Three steps included education in a virtual clinic (A), movement review in a studio (B), and movement practice in outdoor virtual environments: subway (C), taxi (D), and airplane (E).
When this step for reviewing the learned techniques in a comfortable virtual environment is selected in the PMR menu, the user is placed on a studio with an empty background filmed with a 360-degree 3D camera, and two icons are presented on the screen to select movement review for each body part or whole-body movement review. The user is allowed to stay in the studio and review PMR while listening to the therapist’s voice guidance and seeing a demonstration of the movement of the assistant sitting in a chair and abbreviated text tips (Figure 3B). In movement review for each body part, the assistant demonstrates the whole-body movement in the middle, and a circle-shaped help video located on the right side of the assistant shows a close-up of a specific body part in the order of arms, legs, chest and abdomen, shoulders, and neck. In whole-body movement review, the assistant repeatedly shows the whole-body movement in the middle without the help video. When all of the given demonstrations have been presented, the scene automatically goes to the PMR module menu. The user can finish this step at any time by clicking a skip icon provided in the upper left corner.
When this step for trying PMR in outdoor virtual environments that simulate busy real life is selected in the PMR module menu, icons are presented that allow the user to select one of the subway, taxi, and airplane situations. In each situation, a variety of conditions are presented so that the user can experience the tension at different difficulty levels, and the user can select any condition according to his or her needs. If selecting the subway, the user is placed on a subway platform waiting for the train, and icons for riding one, two, or three stops are presented. When one of the icons is clicked, the user is moved to the inside of a subway running on a ground section. If selecting the taxi, the user stands next to a taxi stopped on the street, and icons are provided to ride for 2, 3, or 5 min. When clicking one of the icons, the user is moved to the inside of a taxi trapped in a tunnel in a traffic jam. If selecting the airplane, the user is located at a check-in at an airport with a large number of people, and icons are provided to flight for 2, 3, or 5 min. When clicking one of the icons, the user is moved to the inside of an airplane flying in the sky. All of these virtual environments were filmed with a 360-degree 3D camera. In these conditions, the user can practice PMR according to the therapist’s voice guidance while watching a help video of the assistant’s motion presented in the upper right corner of the screen (Figure 3C). When the scene is over, it returns to the PMR module menu, and the user can finish this step at any time by clicking a skip icon provided in the upper left corner.
The system is designed so that the user must respond to self-evaluations given within the virtual world at each training trial. The purpose of these self-evaluations is not only to assess whether the training actually helps by comparing scores, but also to monitor whether the training itself is on time. The in-app self-evaluations in diaphragmatic breathing include three questions for the level of tension after training (How tense are you now?), comfort during training (How comfortable was your inhalation and exhalation during breathing?), and concentration during training (How much could you focus on breathing?). Those in PMR are two questions for the level of tension after training (How tense are you now?) and comfort during training (How well did you relax in 20 s of muscle relaxation). These questions are asked at the end of the step-2 breathing or PMR review trials. In the step-3 outdoor breathing or PMR trials, only the level of tension is assessed before and after the trials. All of these questions are answered on a 11-point Likert scale from 0 (not at all) to 10 (very much). The answers are instantly stored with login information in a certain folder on the smartphone. By clicking the icon of viewing results in the diaphragmatic breathing or PMR module menu, the user can listen to advice on coping with anxiety while seeing the results of self-evaluations placed on a graded bar.
Self-training using the VRTS can be implemented through the recommended schedule of training for 3 weeks, which is detailed in Supplementary Table 1. In the entire training period, a total of 4–6 trials per day for 4 days a week (Mon, Tue, Thu, and Fri) are divided into morning and afternoon sessions. A total of 22 trials of the first week consist of sequential and repetitive training of diaphragmatic breathing from step 1 to step 3, and all morning or afternoon sessions always include breathing review. A total of 23 trials of the second week consist of sequential and repetitive training of PMR step 1 and step 2 and re-exercise for diaphragmatic breathing, and all morning or afternoon sessions always include PMR review body parts and breathing review. A total of 23 trials of the third week consist of sequential and repetitive training of PMR step 2 and step 3 and re-exercise for diaphragmatic breathing, and all morning or afternoon sessions always include breathing review. Additional training is allowed at any step every Saturday, but this is not mandatory and is executed at the user’s own discretion.
The self-training schedule in the worksheet group (Supplementary Table 2) was configured to be as close as possible to that in the VR group. In the 3-weeks training period, a total of 2–4 trials per day for 4 days a week (Mon, Tue, Thu, and Fri) were divided into morning and afternoon sessions. Participants in this group replaced Step 1: Learning in a virtual clinic and Step 2: Review in a comfortable virtual environment in the VRTS with reading education materials and breathing practice on their own, respectively. However, Step 3: Practice in outdoor virtual environments could not be performed on them due to the impossibility of implementation. A total of 10 trials of the first week consisted of reading an educational material for diaphragmatic breathing and breathing practices of various times, and all sessions always included breathing practice. A total of 16 trials of the second week consisted of reading an educational material for PMR, PMR body parts, and re-exercise for diaphragmatic breathing, and all sessions always included breathing practice. A total of 16 trials of the third week consisted of PMR body parts, PMR whole body, and re-exercise for diaphragmatic breathing, and all sessions always included breathing practice. While the self-training schedule consisted of 68 trials (total of 241 min) in the VR group, it included a small number of 42 trials in the worksheet group, and thus the training time per trial was lengthened to make a total of 224 min to approximate the total time of the VR group. Additional training was allowed at any step every Saturday, but this was not mandatory. Self-evaluations in the worksheet group were conducted immediately after all breathing and PMR practices using a questionnaire printed with the same questions and response forms as in the VRTS’s in-app measurements.
At the first laboratory visit prior to self-training, participants provided demographic and clinical information. The level of anxiety and depression was evaluated using the Hospital Anxiety and Depression Scale (HADS), scored by 14-item 4-point Likert measurements (Zigmond and Snaith, 1983). The level of subjectively felt stress was assessed using the Perceived Stress Scale (PSS), scored by 10-item 5-point Likert measurements (Cohen et al., 1983). The objective level of stress was evaluated by various parameters of heart rate variability (HRV), which was measured using SA-3000P (Medicore Co., Ltd, Seoul, Korea). These parameters included standard deviation of normal to normal RR intervals (SDNN) and root mean square of successive differences (RMSSD) in the time domain and average of normalized low frequency component (nLF), average of normalized high frequency component (nHF), and the ratio between average of low frequency and high frequency (LF/HF) in the frequency domain. All participants in both groups revisit the laboratory after 3-weeks self-training, and received the same evaluation as at the first visit and completed the System Usability Scale (SUS), which assesses the usability of a tool using 10-item 5-point Likert measurements (Brooke, 1996) and has a criterion for determining that the score calculated by the formula is within the acceptable range as the top 50% if it is 70 or more (Brooke, 2013). Additionally, the VR group provided responses to two more questionnaires, the modified version of the Presence Questionnaire (PQ) (Witmer and Singer, 1998) scoring from 94 to 226 points for the presence of being in the virtual environment and the Simulator Sickness Questionnaire (SSQ) (Kennedy et al., 1993) scoring from 0 to 235.6 points for sicknesses felt while experiencing a VR program.
The demographic variables, psychological and psychophysiological measures before self-training, change rates of psychological and psychophysiological measures before and after self-training, and self-evaluations during self-training were compared between the VR and worksheet groups using the Mann-Whitney test. Changes in psychological and physiological measures before and after self-training in each group and the self-evaluated levels of tension before and after trials of outdoor practice during self-training in the VR group were analyzed using the Wilcoxon signed rank test. In addition, in order to evaluate whether self-training was being performed on schedule, we calculated the self-evaluation execution rate, that refers to the percentage of the number of actual evaluations out of a total of 29 times after breathing review, 18 times after PMR review, 14 times before and after outdoor breathing trials, or 14 times before and after outdoor PMR trials in the VR group and 15 times after breathing practice or 15 times after PMR practice in the worksheet group. These rates were compared within and between the groups using the Wilcoxon signed rank test or Mann-Whitney test.
Of 15 participants in the VR group, four were considered dropouts because they did not use the VR program properly and had no stored data. One out of 16 participants in the worksheet group was dropped out. Thus, the data of 11 participants in the VR group (six males and five females; 24.3 ± 2.1 years old) and 15 participants in the worksheet group (seven males and eight females; 23.0 ± 2.3 years old) were used for the analysis. There was no significant difference in intelligence quotient, education level, and the levels of anxiety, depression, and perceived stress before self-training between the two groups (see Supplementary Table 3).
As shown in Table 1, the VR group showed no significant changes in the levels of anxiety, depression, and perceived stress and all parameters of HRV before and after self-training. The worksheet group also showed no changes in those levels except the PSS, which was significantly decreased after self-training (z = −2.50, p = 0.013). The change rates of all the scores did not significantly differ between the two groups.
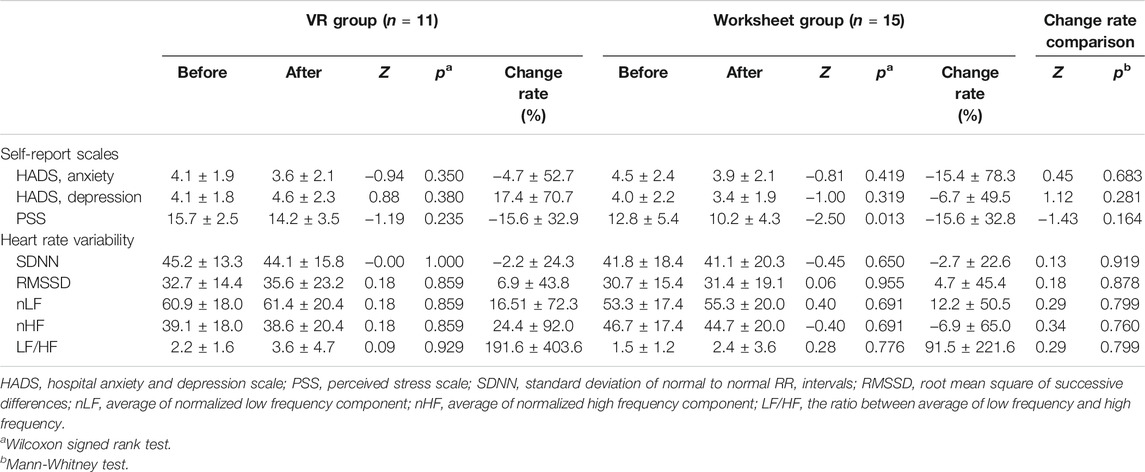
TABLE 1. Changes in psychological and physiological measures (mean ± standard deviation) before and after self-training.
In the results of self-evaluations during self-training (Table 2), the levels of tension after breathing practices showed no group difference, whereas the levels of tension after PMR practices were significantly lower in the VR group than in the worksheet group (z = −2.93, p = 0.003). The levels of comfortable performance during breathing and PMR and the levels of concentration during breathing did not significantly differ between the two groups.
The results of self-evaluations for the levels of tension before and after trials of outdoor practice during 3-weeks self-training in the VR group are presented in Table 3. In outdoor breathing, the levels of tension tended to decrease in all trials. Significant decreases after individual trials were found only in the trials of elevator 10 persons, 1 min and theater, 3 min, and the decrease of the mean tension level throughout the trials was significant (z = −3.81, p < 0.001). In outdoor PMR, the levels of tension also tended to decrease in all trials. Although no significant decrease was found in individual trials, the decrease of the mean tension level was significant (z = −3.61, p < 0.001). In the worksheet group, there were no data comparable to these values in the VR group because outdoor practice was not carried out due to the impossibility of implementation.

TABLE 3. Results of self-evaluations for tension before and after trials of outdoor practice during 3-weeks self-training in the virtual reality group.
Table 4 shows the self-evaluation execution rates as the outcome of whether individual participants performed self-training as scheduled. The VR group scored 11 to 29 times out of a total of 29 self-evaluations after breathing review and 5 to 18 times out of a total of 18 self-evaluations after PMR review, showing an average execution rate of 77.4% after breathing review and 73.7% after PMR review and no significant difference between these two execution rates. These rates were relatively low compared to the average 89.2% execution rate for a total of 15 self-evaluations after breathing practice and average 86.2% for a total of 15 self-evaluations after PMR practice in the worksheet group, but both rates did not significantly differ between the two groups. Meanwhile, in the VR group, the average self-evaluation execution rates before and after a total of seven outdoor breathing trials was 83.1%, which was higher than the average of 70.1% before and after a total of seven outdoor PMR trials, but the difference was not statistically significant.
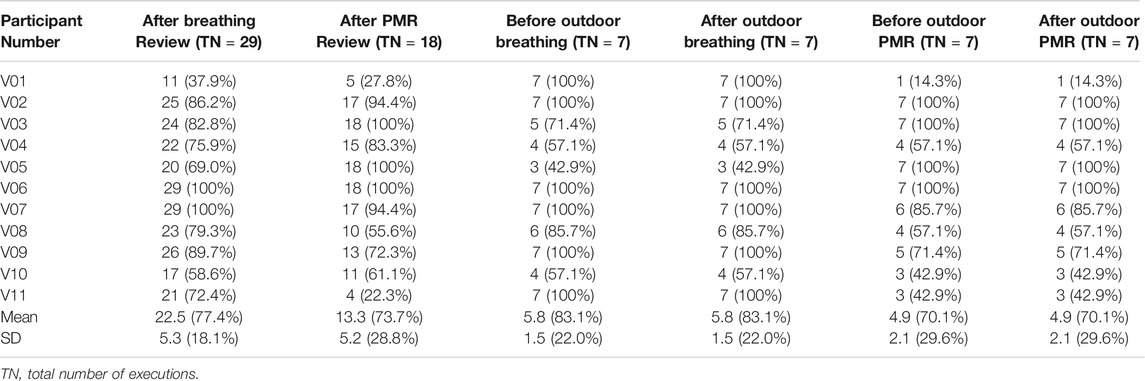
TABLE 4. The number and execution rate of self-evaluations in the participants of the virtual reality group.
The SUS scores after self-training were above 70 in both groups. They were lower in the VR group (70.9 ± 13.5) than in the worksheet group (78.7 ± 9.3), but the difference was not statistically significant. In addition, after self-training, the VR group reported 43.5 ± 32.4 in the total SSQ score and 180.3 ± 12.8 in the PQ score.
This study evaluated the feasibility of self-training using the VRTS in healthy adults. It may have been burdensome to the participants in the VR group that they had to use a device that was not familiar with how to operate, and that they had to follow a tight training schedule that required them to perform a total of four to six trials per day for 4 days a week during 3 weeks. Although the total number of participants was small, four out of 15 (26.7%) in the VR group were dropped out, and it is likely that this burden was attributable to the high dropout rate. This burden may also be the reason why the SUS scores and self-evaluation execution rates evaluated by the VR group who completed self-training were lower than those of the worksheet group, though the differences were not statistically significant. These are consistent with our expectation that the VR group would feel more uncomfortable in use due to frequent mechanical operations. However, since the SUS score was within the acceptable range with an average of 70 or more (Brooke, 2013), the usability of the VRTS deserves a decent level despite this burden.
In both the VR group and worksheet group, all psychological and psychophysiological measures tended to decrease after self-training, but none of these decreases were statistically significant and the change rates showed no significant difference between the two groups. These insignificant results seem to be due to the fact that the measures before self-training were low within the normal range because the participants of this experiment were healthy adults. Considering that relaxation therapy including diaphragmatic breathing and PMR can be an effective treatment for patients with anxiety disorders (Hibbert and Chan, 1989; Han et al., 1996; Conrad and Roth, 2007), it is possible that meaningful results were derived if it was targeted to psychiatric patients with high anxiety scores.
During self-training, the tension-relieving effect of diaphragmatic breathing and PMR was measured by self-evaluation at each trial. Because all the participants in this study were healthy volunteers, the tension level before self-training was very low, and thus the likelihood of a decrease after self-training was low due to the bottom effect. Nonetheless, there was no significant difference in the tension scores after breathing trials between the two groups, but those after PMR trials were significantly lower in the VR group than in the worksheet group. These results suggest that grasping the execution method with only a worksheet may be relatively easy in breathing practice, but not in PMR practice. In other words, VR program users can easily grasp the execution method by performing the practice while watching the actual movement and listening to the explanation, and the advantage is maximized in PMR rather than diaphragmatic breathing. This advantage in PMR confirms our prediction that the VR group would more easily learn the training contents than the worksheet group despite the inconvenience of mechanical operations. It should be noted that VR contents have strengths in reputable practice, especially in unfamiliar practice (Moline, 1997).
Training in outdoor environments was impossible in the worksheet group and could only be performed in the VR group. This training is a kind of experiential learning that implies learning through direct experiences. VR technologies allowing direct interaction with virtual environments enhance vividness, interactivity, presence, and experientiality, and thus makes experiential learning possible (Kwon, 2019). In this training, trials of breathing practice generally resulted in a decrease in the tension scores, but those of PMR practice did not, suggesting that diaphragmatic breathing is easier to perform in outdoor than PMR. The fact that the self-evaluation execution rate during practice in outdoor virtual environments was higher at 83.1% in breathing practice than 70.1% in PMR practice, though the difference was insignificant, may also reflect the relative ease of diaphragmatic breathing in outdoor. It has been reported that breathing training is superior to PMR in controlling repetitive negative thoughts that can cause tension (Feldman et al., 2010). Therefore, if users learn the method using the VRTS, there is a possibility that when tension relief is needed in everyday life similar to that implemented in the system, only diaphragmatic breathing, which can be applied easily without PMR, is likely to be effective. It should be noted, however, that while diaphragmatic breathing is more effective in increasing relaxation state, PMR is more effective in inducing physical relaxation and disengagement (Matsumoto and Smith, 2001). Accordingly, we believe that individuals with high body tension or low disengagement can be particularly helped with PMR learned through repetitive VR self-training.
In this study, immersion and safety of the VRTS were evaluated by the degree of presence and cybersickness, respectively. In fact, according to a recent review (Weech et al., 2019), these two appear to be closely related. Presence was measured with the mean PQ score of 180.3, suggesting that the participants experienced the VRTS with high immersion. This is an encouraging result in that increased feelings of presence in VR simulations can allow increased effectiveness of VR training (Piccione et al., 2019). Cybersickness was assessed with the mean SSQ total score of 43.5, indicating that it is tolerable to a degree similar to or higher than the scores in previous reports (Wibirama and Hamamoto, 2014; Gálvez-García et al., 2015). The closed-type HMD used in the VRTS is favorable to immersion, but results in increasing cybersickness (Moss and Muth, 2011). Given that cybersickness often leads to high dropout rates (Cobb et al., 1999), the possibility that four participants in the VR group were dropped out due to such cybersickness cannot be excluded. Therefore, while our VR program is deemed to be safe, caution for severe cybersickness needs to be warned to the users.
There are several limitations in this study. First, at this stage, only the results of the self-evaluations that the VR user answered after the training trials can be checked with feedback. However, considering that the pulse rate changes rapidly depending on the level of tension (Knight and Rickard, 2001), we can build a system to feedback changes in the pulse rate using photoplethysmograph (PPG) before and after the training trials. Since the accuracy and reliability of the PPG signals are highly influenced by motion artifacts (Lee et al., 2020) and there is inevitably a lot of body movement during diaphragmatic breathing and PMR, a sensor of the earlobe clip type can be used to minimize motion artifacts. The level of tension can be monitored using electroencephalogram (EEG) in that changes in the amplitude of alpha and theta waves are associated with the severity of anxiety (Dadashi et al., 2015). The EEG sensor can be inserted into the HMD’s forehead contact pad to detect the signals from the frontal lobe while minimizing motion artifacts. Since a work is underway to incorporate these biosignal-measuring devices into the VRTS, the results of using them may be presented in the future in our subsequent studies. Another important limitation of this study is that the number of samples that participated to test the feasibility of the VRTS was too small. In addition, as the participants were limited to young adults who are relatively familiar with the use of electronic devices, it may be difficult to generalize the results to the entire adult population.
This study evaluated the feasibility of the VRTS, including diaphragmatic breathing and PMR, and consisting of learning in a virtual clinic, review in a comfortable virtual environment, and practice in outdoor virtual environments. The change rates of all psychological and psychophysiological measures before and after self-training for 3 weeks did not significantly differ between the VR and worksheet groups. The levels of tension did not differ after breathing practices between the two groups, but were significantly lower after PMR practices in the VR group than in the worksheet group. In the VR group, trials of outdoor practices tended to decrease the tension level, particularly after outdoor breathing trials. The VR group gave an acceptable level of usability, cybersickness, and presence. Therefore, our VRTS deserves to be used by healthy individuals to relieve tension. In particular, diaphragmatic breathing may be used more easily, but the benefit of using VR is higher in PMR. These results provide justification for a randomized controlled study of whether this system can be used for stress relief in the general population and, furthermore, treatment of patients with anxiety disorders.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Gangnam Severance Hospital Institutional Review Board. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
JO, MP, SJ, and J-JK contributed to conception and design of the study. JO coordinated the project. HK performed the user evaluation. BK was responsible for data acquisition and analysis. HJ performed the statistical analyses and wrote the manuscript draft. J-JK supervised the work and corrected the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by 2018 VR/AR/MR flagship project of the National IT Industry Promotion Agency (NIPA) and by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (No. NRF-2021M3E5D9025019).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2021.722558/full#supplementary-material
Alaker, M., Wynn, G. R., and Arulampalam, T. (2016). Virtual Reality Training in Laparoscopic Surgery: A Systematic Review & Meta-Analysis. Int. J. Surg. 29, 85–94. doi:10.1016/j.ijsu.2016.03.034
Anderson, P. L., Price, M., Edwards, S. M., Obasaju, M. A., Schmertz, S. K., Zimand, E., et al. (2013). Virtual Reality Exposure Therapy for Social Anxiety Disorder: a Randomized Controlled Trial. J. Consulting Clin. Psychol. 81 (5), 751–760. doi:10.1037/a0033559
Barlow, D. H., Craske, M. G., Cerny, J. A., and Klosko, J. S. (1989). Behavioral Treatment of Panic Disorder. Behav. Ther. 20 (2), 261–282. doi:10.1016/s0005-7894(89)80073-5
Baxter, A. J., Scott, K. M., Vos, T., and Whiteford, H. A. (2013). Global Prevalence of Anxiety Disorders: a Systematic Review and Meta-Regression. Psychol. Med. 43 (5), 897–910. doi:10.1017/S003329171200147X
Bouchard, S., Côté, S., St-Jacques, J., Robillard, G., and Renaud, P. (2006). Effectiveness of Virtual Reality Exposure in the Treatment of Arachnophobia Using 3D Games. Thc 14 (1), 19–27. doi:10.3233/thc-2006-14103
Brooke, J. (1996). “SUS: A ‘Quick and Dirty’ Usability Scale,” in Usability Evaluation in Industry; Jordan Patrick, W., Thomas, B., Weerdmeester, B.A., McClelland, I.L., Eds.; London, UK: Taylor & Francis, 189–194.
Cárdenas, G., Muñoz, S., González, M., and Uribarren, G. (2006). Virtual Reality Applications to Agoraphobia: a Protocol. CyberPsychology Behav. 9 (2), 248–250. doi:10.1089/cpb.2006.9.248
Carl, E., Stein, A. T., Levihn-Coon, A., Pogue, J. R., Rothbaum, B., Emmelkamp, P., et al. (2019). Virtual Reality Exposure Therapy for Anxiety and Related Disorders: A Meta-Analysis of Randomized Controlled Trials. J. Anxiety Disord. 61, 27–36. doi:10.1016/j.janxdis.2018.08.003
Charalambous, A., Giannakopoulou, M., Bozas, E., and Paikousis, L. (2015). A Randomized Controlled Trial for the Effectiveness of Progressive Muscle Relaxation and Guided Imagery as Anxiety Reducing Interventions in Breast and Prostate Cancer Patients Undergoing Chemotherapy. Evidence-Based Complement. Altern. Med. 2015, 1–10. doi:10.1155/2015/270876
Chen, Y.-F., Huang, X.-Y., Chien, C.-H., and Cheng, J.-F. (2017). The Effectiveness of Diaphragmatic Breathing Relaxation Training for Reducing Anxiety. Perspect. Psychiatr. Care 53 (4), 329–336. doi:10.1111/ppc.12184
Cheung, Y. L., Molassiotis, A., and Chang, A. M. (2003). The Effect of Progressive Muscle Relaxation Training on Anxiety and Quality of Life after Stoma Surgery in Colorectal Cancer Patients. Psycho-Oncology 12 (3), 254–266. doi:10.1002/pon.638
Choe, A., Hwang, S., Kim, J., Park, K., Chey, J., and Hong, S. (2014). Validity of the K-WAIS-IV Short Forms. Kor. J. Clin. Psychol. 33 (2), 413–428.
Cobb, S. V. G., Nichols, S., Ramsey, A., and Wilson, J. R. (1999). Virtual Reality-Induced Symptoms and Effects (VRISE). Presence: Teleoperators. Virtual Environ. 8 (2), 169–186. doi:10.1162/105474699566152
Cohen, S., Kamarck, T., and Mermelstein, R. (1983). A Global Measure of Perceived Stress. J. Health Soc. Behav. 24 (4), 385–396. doi:10.2307/2136404
Conrad, A., and Roth, W. T. (2007). Muscle Relaxation Therapy for Anxiety Disorders: it Works but How? J. Anxiety Disord. 21 (3), 243–264. doi:10.1016/j.janxdis.2006.08.001
Dadashi, M., Birashk, B., Taremian, F., Asgarnejad, A. A., and Momtazi, S. (2015). Effects of Increase in Amplitude of Occipital Alpha & Theta Brain Waves on Global Functioning Level of Patients with GAD. Basic Clin. Neurosci. 6 (1), 14–20.
Emmelkamp, P. M. G., Bruynzeel, M., Drost, L., and van der Mast, C. A. (2001). Virtual Reality Treatment in Acrophobia: a Comparison with Exposure In Vivo. CyberPsychology Behav. 4 (3), 335–339. doi:10.1089/109493101300210222
Feldman, G., Greeson, J., and Senville, J. (2010). Differential Effects of Mindful Breathing, Progressive Muscle Relaxation, and loving-kindness Meditation on Decentering and Negative Reactions to Repetitive Thoughts. Behav. Res. Ther. 48 (10), 1002–1011. doi:10.1016/j.brat.2010.06.006
Fields, J. A., Nichols, L. O., Martindale-Adams, J., Zuber, J., and Graney, M. (2012). Anxiety, Social Support, and Physical Health in a Sample of Spouses of OEF/OIF Service Members. Mil. Med. 177 (12), 1492–1497. doi:10.7205/milmed-d-12-00036
Gálvez-García, G., Hay, M., and Gabaude, C. (2015). Alleviating Simulator Sickness with Galvanic Cutaneous Stimulation. Hum. Factors 57 (4), 649–657. doi:10.1177/0018720814554948
Grinberg, A. S., Sellinger, J. J., Sprenkle, P. C., Bandin, A. J., Nawaf, C. B., Syed, J. S., et al. (2020). Effect of Diaphragmatic Breathing on Procedural Anxiety during Transrectal Prostate Biopsy. Urology 137, 26–32. doi:10.1016/j.urology.2019.12.024
Han, J. N., Stegen, K., De Valck, C., Clément, J., and Van de Woestijne, K. P. (1996). Influence of Breathing Therapy on Complaints, Anxiety and Breathing Pattern in Patients with Hyperventilation Syndrome and Anxiety Disorders. J. Psychosomatic Res. 41 (5), 481–493. doi:10.1016/s0022-3999(96)00220-6
Hibbert, G. A., and Chan, M. (1989). Respiratory Control: Its Contribution to the Treatment of Panic Attacks. Br. J. Psychiatry 154 (2), 232–236. doi:10.1192/bjp.154.2.232
Hong, Y.-J., Kim, H. E., Jung, Y. H., Kyeong, S., and Kim, J.-J. (2017). Usefulness of the mobile Virtual Reality Self-Training for Overcoming a Fear of Heights. Cyberpsychology, Behav. Soc. Networking 20 (12), 753–761. doi:10.1089/cyber.2017.0085
Jiménez-Rodríguez, D., Conesa-Garcerán, M., and Belmonte-García, T. (2019). Evaluación del efecto de la terapia de relajación en pacientes con hipertensión arterial. Enfermería Clínica 29 (3), 178–185. doi:10.1016/j.enfcli.2018.07.005
Kampmann, I. L., Emmelkamp, P. M. G., Hartanto, D., Brinkman, W.-P., Zijlstra, B. J. H., and Morina, N. (2016). Exposure to Virtual Social Interactions in the Treatment of Social Anxiety Disorder: A Randomized Controlled Trial. Behav. Res. Ther. 77, 147–156. doi:10.1016/j.brat.2015.12.016
Kennedy, R. S., Lane, N. E., Berbaum, K. S., and Lilienthal, M. G. (1993). Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int. J. Aviation Psychol. 3 (3), 203–220. doi:10.1207/s15327108ijap0303_3
Khan, R., Plahouras, J., Johnston, B. C., Scaffidi, M. A., Grover, S. C., and Walsh, C. M. (2019). Virtual Reality Simulation Training in Endoscopy: a Cochrane Review and Meta-Analysis. Endoscopy 51 (7), 653–664. doi:10.1055/a-0894-4400
Kidwell, K. M., Nelson, T. D., and Van Dyk, T. (2015). Parenting Stress and Child Physical Health Among a Low-Income Sample: The Moderating Role of Child Anxiety. J. Health Psychol. 20 (11), 1377–1387. doi:10.1177/1359105313512352
Kim, H. E., Hong, Y.-J., Kim, M.-K., Jung, Y. H., Kyeong, S., and Kim, J.-J. (2017). Effectiveness of Self-Training Using the mobile-based Virtual Reality Program in Patients with Social Anxiety Disorder. Comput. Hum. Behav. 73, 614–619. doi:10.1016/j.chb.2017.04.017
Kim, S., Wollburg, E., and Roth, W. T. (2012). Opposing Breathing Therapies for Panic Disorder: Randomized Controlled Trial Of Lowering vs Raising End-Tidal P(CO(2). J. Clin. Psychiatry 73 (7), 931–939. doi:10.4088/JCP.11m07068
Knight, W. E. J., and Rickard, N. S. (2001). Relaxing Music Prevents Stress-Induced Increases in Subjective Anxiety, Systolic Blood Pressure, and Heart Rate in Healthy Males and Females. J. Music Ther. 38 (4), 254–272. doi:10.1093/jmt/38.4.254
Kothgassner, O. D., Goreis, A., Kafka, J. X., Van Eickels, R. L., Plener, P. L., and Felnhofer, A. (2019). Virtual Reality Exposure Therapy for Posttraumatic Stress Disorder (PTSD): a Meta-Analysis. Eur. J. Psychotraumatology 10 (1), 1654782. doi:10.1080/20008198.2019.1654782
Kwon, C. (2019). Verification of the Possibility and Effectiveness of Experiential Learning Using HMD-Based Immersive VR Technologies. Virtual Reality 23 (1), 101–118. doi:10.1007/s10055-018-0364-1
Lai, B., Rimmer, J., Barstow, B., Jovanov, E., and Bickel, C. S. (2016). Teleexercise for Persons with Spinal Cord Injury: A Mixed-Methods Feasibility Case Series. JMIR Rehabil. Assist. Technol. 3 (2), e8. doi:10.2196/rehab.5524
Lee, J., Kim, M., Park, H. K., and Kim, I. Y. (2020). Motion artifact reduction in wearable photoplethysmography based on multi-channel sensors with multiple wavelengths. Sensors 20 (5), 1493–370. doi:10.3390/s20051493
Ma, X., Yue, Z.-Q., Gong, Z.-Q., Zhang, H., Duan, N.-Y., Shi, Y.-T., et al. (2017). The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Front. Psychol. 8, 874. doi:10.3389/fpsyg.2017.00874
Malbos, E., Rapee, R. M., and Kavakli, M. (2013). A Controlled Study of Agoraphobia and the Independent Effect of Virtual Reality Exposure Therapy. Aust. N. Z. J. Psychiatry 47 (2), 160–168. doi:10.1177/0004867412453626
Manzoni, G. M., Pagnini, F., Castelnuovo, G., and Molinari, E. (2008). Relaxation Training for Anxiety: a Ten-Years Systematic Review with Meta-Analysis. BMC Psychiatry 8 (1), 41. doi:10.1186/1471-244X-8-41
Marco, J. H., Perpiñá, C., and Botella, C. (2013). Effectiveness of Cognitive Behavioral Therapy Supported by Virtual Reality in the Treatment of Body Image in Eating Disorders: One Year Follow-Up. Psychiatry Res. 209 (3), 619–625. doi:10.1016/j.psychres.2013.02.023
Matsumoto, M., and Smith, J. C. (2001). Progressive Muscle Relaxation, Breathing Exercises, and ABC Relaxation Theory. J. Clin. Psychol. 57, 1551–1557. doi:10.1002/jclp.1117
McKnight, P. E., Monfort, S. S., Kashdan, T. B., Blalock, D. V., and Calton, J. M. (2016). Anxiety Symptoms and Functional Impairment: A Systematic Review of the Correlation between the Two Measures. Clin. Psychol. Rev. 45, 115–130. doi:10.1016/j.cpr.2015.10.005
Migoya-Borja, M., Delgado-Gómez, D., Carmona-Camacho, R., Porras-Segovia, A., López-Moriñigo, J.-D., Sánchez-Alonso, M., et al. (2020). Feasibility of a Virtual Reality-Based Psychoeducational Tool (VRight) for Depressive Patients. Cyberpsychology, Behav. Soc. Networking 23 (4), 246–252. doi:10.1089/cyber.2019.0497
Molassiotis, A., Yung, H. P., Yam, B. M., Chan, F. Y., and Mok, T. (2002). The Effectiveness of Progressive Muscle Relaxation Training in Managing Chemotherapy-Induced Nausea and Vomiting in Chinese Breast Cancer Patients: a Randomised Controlled Trial. Support. Care Cancer 10 (3), 237–246. doi:10.1007/s00520-001-0329-9
Moline, J. (1997). Virtual Reality for Health Care: a Survey. Stud. Health Technol. Inform. 44, 3–34.
Moore, J., Fiddler, H., Seymour, J., Grant, A., Jolley, C., Johnson, L., et al. (2009). Effect of a home Exercise Video Programme in Patients with Chronic Obstructive Pulmonary Disease. J. Rehabil. Med. 41 (3), 195–200. doi:10.2340/16501977-0308
Moss, J. D., and Muth, E. R. (2011). Characteristics of Head-Mounted Displays and Their Effects on Simulator Sickness. Hum. Factors 53 (3), 308–319. doi:10.1177/0018720811405196
Norton, P. J., and Price, E. C. (2007). A Meta-Analytic Review of Adult Cognitive-Behavioral Treatment Outcome across the Anxiety Disorders. J. Nerv. Ment. Dis. 195 (6), 521–531. doi:10.1097/01.nmd.0000253843.70149.9a
Özlü, İ., Öztürk, Z., Karaman Özlü, Z., Tekin, E., and Gür, A. (2021). The Effects of Progressive Muscle Relaxation Exercises on the Anxiety and Sleep Quality of Patients with COVID‐19: A Randomized Controlled Study. Perspect. Psychiatr. Care 57 (4), 1791–1797. doi:10.1111/ppc.12750
Palazzo, C., Klinger, E., Dorner, V., Kadri, A., Thierry, O., Boumenir, Y., et al. (2016). Barriers to home-based Exercise Program Adherence with Chronic Low Back Pain: Patient Expectations Regarding New Technologies. Ann. Phys. Rehabil. Med. 59 (2), 107–113. doi:10.1016/j.rehab.2016.01.009
Park, K. M., Ku, J., Choi, S. H., Jang, H. J., Park, J. Y., Kim, S. I., et al. (2011). A virtual reality application in role-plays of social skills training for schizophrenia: a randomized, controlled trial. Psychiatry Res. 189 (2), 166–172. doi:10.1016/j.psychres.2011.04.003
Pelekasis, P., Matsouka, I., and Koumarianou, A. (2017). Progressive Muscle Relaxation as a Supportive Intervention for Cancer Patients Undergoing Chemotherapy: A Systematic Review. Pall Supp Care 15 (4), 465–473. doi:10.1017/S1478951516000870
Piccione, J., Collett, J., and De Foe, A. (2019). Virtual Skills Training: the Role of Presence and agency. Heliyon 5 (11), e02583. doi:10.1016/j.heliyon.2019.e02583
Prisnie, J. C., Sajobi, T. T., Wang, M., Patten, S. B., Fiest, K. M., Bulloch, A. G. M., et al. (2018). Effects of Depression and Anxiety on Quality of Life in Five Common Neurological Disorders. Gen. Hosp. Psychiatry 52, 58–63. doi:10.1016/j.genhosppsych.2018.03.009
Scalese, R. J., Obeso, V. T., and Issenberg, S. B. (2008). Simulation Technology for Skills Training and Competency Assessment in Medical Education. J. Gen. Intern. Med. 23 (Suppl. 11), 46–49. doi:10.1007/s11606-007-0283-4
Segawa, T., Baudry, T., Bourla, A., Blanc, J.-V., Peretti, C.-S., Mouchabac, S., et al. (2019). Virtual Reality (VR) in Assessment and Treatment of Addictive Disorders: A Systematic Review. Front. Neurosci. 13, 1409. doi:10.3389/fnins.2019.01409
Sheik-Ali, S., Edgcombe, H., and Paton, C. (2019). Next-generation Virtual and Augmented Reality in Surgical Education: A Narrative Review. Surg. Technol. Int. 35, 27–35.
Subbalakshmi, N. K., Adhikari, P., and Shanmugavel Jeganathan, P. (2014). Comparative Study on Cardiac Autonomic Modulation during Deep Breathing Test and Diaphragmatic Breathing in Type 2 Diabetes and Healthy Subjects. J. Diabetes Invest. 5 (4), 456–463. doi:10.1111/jdi.12163
Tortella-Feliu, M., Botella, C., Llabrés, J., Bretón-López, J. M., del Amo, A. R., Baños, R. M., et al. (2011). Virtual Reality versus Computer-Aided Exposure Treatments for Fear of Flying. Behav. Modif. 35 (1), 3–30. doi:10.1177/0145445510390801
Toussaint, L., Nguyen, Q. A., Roettger, C., Dixon, K., Offenbächer, M., Kohls, N., et al. (2021). Effectiveness of Progressive Muscle Relaxation, Deep Breathing, and Guided Imagery in Promoting Psychological and Physiological States of Relaxation. Evidence-Based Complement. Altern. Med. 2021, 1–8. doi:10.1155/2021/5924040
Veling, W., Lestestuiver, B., Jongma, M., Hoenders, H. J. R., and van Driel, C. (2021). Virtual Reality Relaxation for Patients with a Psychiatric Disorder: Crossover Randomized Controlled Trial. J. Med. Internet Res. 23 (1), e17233. doi:10.2196/17233
Weech, S., Kenny, S., and Barnett-Cowan, M. (2019). Presence and Cybersickness in Virtual Reality Are Negatively Related: A Review. Front. Psychol. 10, 158. doi:10.3389/fpsyg.2019.00158
Wibirama, S., and Hamamoto, K. (2014). Investigation of Visually Induced Motion Sickness in Dynamic 3D Contents Based on Subjective Judgment, Heart Rate Variability, and Depth Gaze Behavior. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2014, 4803–4806. doi:10.1109/EMBC.2014.6944698
Witmer, B. G., and Singer, M. J. (1998). Measuring Presence in Virtual Environments: A Presence Questionnaire. Presence 7 (3), 225–240. doi:10.1162/105474698565686
Xie, B., Liu, H., Alghofaili, R., Zhang, Y., Jiang, Y., Lobo, F. D., et al. (2021). A Review on Virtual Reality Skill Training Applications. Front. Virtual Real. 2, 645153. doi:10.3389/frvir.2021.645153
Zhao, L., Wu, H., Zhou, X., Wang, Q., Zhu, W., and Chen, J. (2012). Effects of Progressive Muscular Relaxation Training on Anxiety, Depression and Quality of Life of Endometriosis Patients under Gonadotrophin-Releasing Hormone Agonist Therapy. Eur. J. Obstet. Gynecol. Reprod. Biol. 162 (2), 211–215. doi:10.1016/j.ejogrb.2012.02.029
Keywords: virtual reality, relaxation, self-training, diaphragmatic breathing, progressive muscle relaxation
Citation: Jeong HS, Oh J, Paik M, Kim H, Jang S, Kim BS and Kim J-J (2022) Development and Feasibility Assessment of Virtual Reality-Based Relaxation Self-Training Program. Front. Virtual Real. 2:722558. doi: 10.3389/frvir.2021.722558
Received: 09 June 2021; Accepted: 09 December 2021;
Published: 05 January 2022.
Edited by:
Nadja Heym, Nottingham Trent University, United KingdomReviewed by:
Abdulaziz M. Alshaer, Umm Al-Qura University, Saudi ArabiaCopyright © 2022 Jeong, Oh, Paik, Kim, Jang, Kim and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jae-Jin Kim, amFlamtpbUB5b25zZWkuYWMua3I=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.