
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Virtual Real. , 21 May 2021
Sec. Virtual Reality and Human Behaviour
Volume 2 - 2021 | https://doi.org/10.3389/frvir.2021.657638
Background: Body image (BI) disturbances have been identified in both clinical and non-clinical populations. Virtual reality (VR) has recently been used as a tool for modulating BI disturbances through the use of eliciting a full body illusion (FBI). This meta-analysis is the first to collate evidence on the effectiveness of an FBI to reduce BI disturbances in both clinical and non-clinical populations.
Methods: We performed a literature search in MEDLINE (PubMed), EMBASE, PsychINFO, and Web of Science with the keywords and synonyms for “virtual reality” and “body image” to identify published studies until September 2020. We included studies that (1) created an FBI with a modified body shape or size and (2) reported BI disturbance outcomes both before and directly after the FBI. FBI was defined as a head-mounted display (HMD)-based simulation of embodying a virtual body from an egocentric perspective in an immersive 3D computer-generated environment.
Results: Of the 398 identified unique studies, 13 were included after reading full-texts. Four of these studies were eligible for a meta-analysis on BI distortion inducing a small virtual body FBI in healthy females. Significant post-intervention results were found for estimations of shoulder width, hip width, and abdomen width, with the largest reductions in size being the estimation of shoulder circumference (SMD = −1.3; 95% CI: −2.2 to −0.4; p = 0.004) and hip circumference (SMD = −1.0; 95% CI: −1.6 to −0.4; p = 0.004). Mixed results were found in non-aggregated studies from large virtual body FBIs in terms of both estimated body size and BI dissatisfaction and in small virtual body FBI in terms of BI dissatisfaction.
Conclusions: The findings presented in this paper suggest that the participants' BIs were able to conform to both an increased as well as a reduced virtual body size. However, because of the paucity of research in this field, the extent of the clinical utility of FBIs still remains unclear. In light of these limitations, we provide implications for future research about the clinical utility of FBIs for modulating BI-related outcomes.
Eating disorders (EDs) are the third leading cause of chronic illness in female adolescents (Mathews et al., 2011), and anorexia nervosa (AN) has the highest mortality rate of all mental disorders (Arcelus et al., 2011), with a lifetime prevalence of 3.3–18.6% and 0.1–3.6% among women, respectively (Galmiche et al., 2019). An important characteristic of EDs is a persistent body image (BI) disturbance. Current treatment approaches for AN are limited with regard to their effectiveness (Murray et al., 2019), as one-third of the patients with AN relapse (Berends et al., 2018). While standard multidisciplinary treatment programs, including cognitive behavioral therapy (CBT), mainly focus on normalizing weight and eating behavior (Attia and Walsh, 2009), BI disturbances have been identified to be among the most difficult ED features to change within pre-existing therapies (Rorty et al., 1993).
Body image can be defined as “the picture of our own body which we form in our mind” (Schilder, 1935). A BI disturbance entails having negative perceptions, cognitions, and emotions concerning one's own body. Counterintuitively, BI disturbances are often understated in ED treatment (Dakanalis et al., 2016; Phillipou et al., 2018), resulting in its frequent persistence even after recovery (Bachner-Melman et al., 2006). Clinical efforts that focus on targeting BI disturbance could play a key role in improving overall treatment efficacy, not only because BI disturbance is a core symptom of ED (American Psychiatric Association, 2013), but also in response to the mounting evidence indicating that it is a risk factor for the development, maintenance, and relapse of AN (Glashouwer et al., 2019). Moreover, the subsistence of BI disturbance symptoms can also be seen in other disorders such as body dysmorphic disorder (BDD) (American Psychiatric Association, 2013) and obesity (Sarwer et al., 1998; Gavin et al., 2010), as well as in non-clinical populations (Bellisle et al., 1995). Therefore, in order to further enhance the clinical insight into these complex disorders, it is crucial to focus on developing diagnostic and therapeutic interventions that target BI disturbance.
The constituents of BI disturbance research are BI distortion and BI dissatisfaction. BI distortion is defined as the inability to accurately perceive one's own body size or shape (Cash and Deagle, 1997). For example, an overestimated body size is a common perception of patients with ED (Mölbert et al., 2017). Regarding individuals with obesity, inaccurate perceptions of body size could be the result of either an overestimation (Garner et al., 1976; Collins et al., 1987; Gardner et al., 1987; Docteur et al., 2010; Scarpina et al., 2014; Thaler et al., 2018) or an underestimation (Bell et al., 1986; Valtolina, 1998). BI dissatisfaction entails the inability to like, accept, or value one's own body (Cash and Deagle, 1997). BI interventions often include mirror exposure, video exposure, and virtual reality (VR) (Ziser et al., 2018).
Virtual reality is a technology that allows users to explore computer-generated virtual environments (VE) that are entirely digital. The compositional building blocks of these VEs can consist of both 3D computer-aided design (CAD) models or from live or pre-recorded video streams capturing real-world environments. One of the different means for presenting the virtual content is by displaying it through apparatuses called head-mounted displays (HMD), which are non-transparent glasses that rest over the eyes of the user. VR has been successfully implemented across a diversity of different psychiatric disorders as an effective tool to aid in both treatment (Dellazizzo et al., 2020) and diagnostics (Van Bennekom et al., 2017). In BI disturbance, VR has mainly been used to create specific environmental settings that provoked BI-related symptoms (Riva, 1997). These tailored environmental settings are then often combined with traditional CBT, which is referred to as Experiential Cognitive Therapy (ECT) (Riva et al., 1998).
Another approach to assess and treat BI disturbance is to expose patients to modified virtual bodies. HMD-based VR is especially well-suited for this, due to the natural ergonomics of being able to display a 3D model of a body, i.e., an avatar, from an egocentric point of view. The result of this interaction can subsequently elicit the feeling of embodiment, which is the sensation of having a body, over the virtual body. The sensation of embodiment over a virtual body is referred to as a bodily illusion and VR has the unique ability to create graded bodily illusions that can be of individual body parts, such as a hand (Yuan and Steed, 2010), or even the whole body (Slater et al., 2010; Peck et al., 2013; Maister et al., 2015), with the latter being termed as a full body illusion (FBI). An FBI can also occur via body swapping with other real bodies (Oliveira et al., 2016). This method has been proposed as it is able to embody seemingly repulsive, i.e., large, virtual bodies in patients with AN (Koskina et al., 2013; Ziser et al., 2018). A similar approach of embodying both repulsive and desirable bodies (Corno et al., 2018; Mölbert et al., 2018; Neyret et al., 2020; Provenzano et al., 2020) could be applied to improve the accuracy of BI disturbance assessment methods. When patients select their ideal or perceived BI and experience it from an egocentric perspective, it would be reasonable to hypothesize that the results would more closely resemble their own experience compared to more traditional methods used for BI disturbance assessment such as paper-based questionnaires (Reed et al., 1991; Cash et al., 2002; Gardner et al., 2009).
While the clinical significance of FBIs in BI disturbance research can be postulated theoretically, its ability to modify any BI disturbance outcomes has not yet been studied in the context of a systematic review or meta-analysis. While previous reviews have addressed the use of VR in ED (Ferrer-García and Gutiérrez-Maldonado, 2012; Wiederhold et al., 2016; de Carvalho et al., 2017; Clus et al., 2018), the focus was only centered around ECT and other environment-modifying VR interventions. Therefore, it is still unclear to what extent FBIs can effectively trigger BI disturbance symptoms and what influence it will have on BI disturbance outcomes.
The first research question of this study is: Do full body illusions affect body image distortion?
We hypothesize that the participants' BI conforms to the dimensions of the virtual body since people tend to adopt the characteristics of their avatars, which is referred to as the Proteus effect (Yee and Bailenson, 2007). Following this reasoning, participants will perceive themselves as smaller directly after embodying a small virtual body and larger after directly embodying a large one.
The second research question of this study is: Do full body illusions affect body image dissatisfaction?
Because in populations of individuals with AN and obesity, BI dissatisfaction stems from feeling overweight and the wish to be thinner, we expect that embodying a small virtual body will reduce BI dissatisfaction, and embodying a large one will increase it. Since this weight-related BI dissatisfaction is also present in non-clinical populations (Bellisle et al., 1995), we expect the same effect in healthy populations.
We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines for the reporting of meta-analyses (Moher et al., 2009).
Two authors (CT & AG) performed a literature search in MEDLINE (PubMed), EMBASE, PsychINFO, and Web of Science to identify published studies until September 2020 with the search terms “virtual reality” AND “body image” and their synonyms (see Table 1). We chose to use the more overarching search term “virtual reality,” since not all studies containing FBIs mention this term explicitly in the title or abstract. The search terms and syntax were checked by a clinical librarian.
The Rayyan QCRI (Ouzzani et al., 2016) application was used to search for duplicates and to start the inclusion process by screening titles and abstracts for eligibility. Additional articles were searched with citation and similarity tracking. After an independent screening of the titles and abstracts by two authors (CT & AG), the following inclusion criteria were applied to full texts. We included studies that (1) created an FBI with a modified body shape or size and (2) reported BI disturbance outcomes both before and directly after the FBI. FBI was defined as an HMD-based simulation of embodying a virtual body from an egocentric perspective in an immersive 3D computer-generated environment. There were no restrictions on study designs as long as the studies reported the relevant pre- and post-FBI data. Studies were eligible for the meta-analysis if they contained means with SDs of BI outcomes before and directly after the FBI. We checked to see if different studies used shared data sets.
In case of missing data, the authors were contacted by mail. To prevent comparing apples and oranges, the studies were only aggregated in a meta-analysis if a minimum of three had similar FBIs, populations, and outcome measures. When heterogeneity is reduced this way, a meta-analysis is the most valid synthesis technique, even for a low amount of studies (Valentine et al., 2010). Reviews and conference abstracts were excluded.
The primary outcome measure for BI disturbance was the pre-post change in body size estimation. For BI dissatisfaction, we looked at questionnaires [BISS (Cash et al., 2002), PASTAS (Reed et al., 1991), and BIAS-O (Gardner et al., 2009)] or visual analog scales (VAS). Secondary outcome measures included embodiment scores and potential adverse effects of HMD use, such as motion sickness. Moreover, we collected the following data: authors, year of publication, sample size, study design, control conditions, population characteristics (pathology, age, gender, BMI), VR equipment, and the dimensions of the virtual body.
Methodological quality was determined by two authors (CT & AG) using the Quality Assessment Tool for Quantitative Studies (Effective Public Healthcare Panacea Project, 1998). This tool is used for assessing any quantitative study design and was judged a suitable tool for systematic reviews of effectiveness (Deeks et al., 2003).
The Comprehensive Meta-Analysis (Borenstein et al., 2013) software was used by two authors (CT & AG) to calculate weighted standardized mean differences (SMDs) between pre-test and post-test scores, resulting in a forest plot. These pre-post SMDs correspond with Cohen's drm (for repeated measures), which is specifically used in designs with one sample. Since these differ from the classical Cohen's d (Lakens, 2013), we are not directly applying the standard benchmarks of Cohen [small (d = 0.2), medium (d = 0.5), and large (d = 0.8)] (Cohen, 1988) but rather using them cautiously in order to give a general indication. A random effects analysis was used because we assumed to encounter a significant degree of heterogeneity among studies.
Since outcome measures pre- and post-test are not independent of each other, we searched the articles for pre-post correlations (r). In case these were not reported, but raw data were available, we used the data to calculate the correlations. If raw data were also unobtainable, we used estimations based on the available correlations of studies with similar interventions (i.e., FBI in a small body), populations (i.e., healthy female subjects), and outcome measures (i.e., body part estimation tasks). The used pre-post correlations ranged from r = 0.73 to r = 0.92.
Due to the limited number of included studies, we were unable to perform additional sensitivity analyses or construct a funnel plot for the assessment of publication bias.
As depicted in the PRISMA flowchart (Figure 1), the literature search yielded 398 unique studies; 51 remained after screening titles and abstracts and 13 remained after reading full-texts. Four of these studies were eligible for a meta-analysis on BI distortion because they are homogenous in interventions (FBI in a small virtual body), outcome measures (body size estimation tasks of hips, abdomen, and shoulders), and populations (healthy female university students, having a within-study mean age of 21–29, n = 85) (Keizer et al., 2016; Serino et al., 2016a, 2018; Scarpina et al., 2019). Other studies were not aggregated due to differences in interventions (different body sizes in the FBI), outcome measures (reported in medians, using different questionnaires), or populations [different age groups, gender, or body mass indices (BMI)].
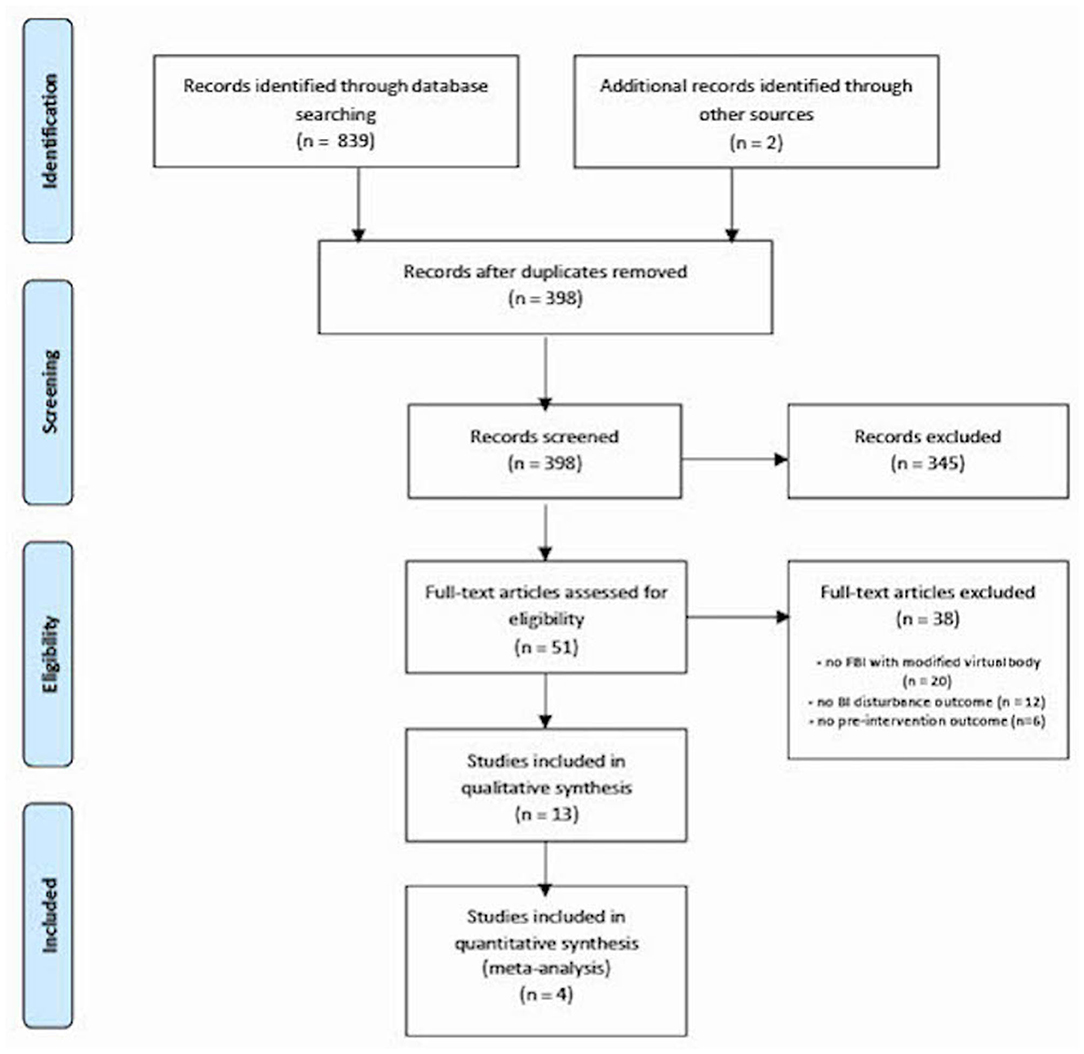
Figure 1. Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flowchart of study selection.
Table 2 summarizes the main characteristics and results of the included studies. The 13 included studies were all written in English and published in peer-reviewed journals. They were either case studies/reports (n = 3) (Serino et al., 2016b, 2019; Porras-Garcia et al., 2020) or cohort studies (n = 10) (Normand et al., 2011; Preston and Ehrsson, 2014, 2018; Keizer et al., 2016; Serino et al., 2016a, 2017, 2018; Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019; Scarpina et al., 2019). FBIs were created for small virtual bodies (n = 10) (Preston and Ehrsson, 2014, 2018; Keizer et al., 2016; Serino et al., 2016a,b, 2017, 2018, 2019; Scarpina et al., 2019; Porras-Garcia et al., 2020) and large virtual bodies (n = 5) (Normand et al., 2011; Preston and Ehrsson, 2014, 2018; Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019). Clinical populations were only studied in small virtual bodies for female patients with AN (n = 4) (Keizer et al., 2016; Serino et al., 2017, 2019; Porras-Garcia et al., 2020) and obesity (n = 2) (Serino et al., 2016b; Scarpina et al., 2019). Studies of healthy participants were predominantly restricted to female samples (n = 8) (Preston and Ehrsson, 2014, 2018; Keizer et al., 2016; Serino et al., 2016a, 2018; Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019; Scarpina et al., 2019); however, other studies also included male samples (n = 3) (Preston and Ehrsson, 2014, 2018; Porras Garcia et al., 2019), or investigated male participants exclusively (n = 1) (Normand et al., 2011). The majority of the studies measured some type of BI distortion outcome (n = 11) (Normand et al., 2011; Preston and Ehrsson, 2014; Keizer et al., 2016; Serino et al., 2016a,b, 2017, 2018, 2019; Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019; Scarpina et al., 2019). BI dissatisfaction was also determined (n = 5) (Preston and Ehrsson, 2014, 2018; Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019; Porras-Garcia et al., 2020), especially in large virtual bodies (n = 4) (Preston and Ehrsson, 2014, 2018; Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019). All the studies used synchronous visuotactile stimulation as a means to induce the FBI. The participants were simultaneously stroked with a physical instrument while concurrently receiving visual input of being stroked. To assess the influence of embodiment on the effect of the FBI, cohort studies used asynchronous visuotactile stimulation as a control condition (n = 9) (Normand et al., 2011; Preston and Ehrsson, 2014, 2018; Keizer et al., 2016; Serino et al., 2016a, 2017, 2018; Porras Garcia et al., 2019; Scarpina et al., 2019), mainly as a within-subjects design (n = 8) (Normand et al., 2011; Preston and Ehrsson, 2014, 2018; Keizer et al., 2016; Serino et al., 2016a, 2017; Ferrer-Garcia et al., 2018; Scarpina et al., 2019). The studies were conducted between 2011 and 2020. The number of included participants in the ten cohort studies varied between 21 and 59, with a median of 39.
Besides examining whether FBI could affect BI disturbance outcomes, study objectives of the reviewed publications included comparing clinical populations with healthy controls (n = 2) (Keizer et al., 2016; Scarpina et al., 2019) and examining the influence of gender (n = 2) (Preston and Ehrsson, 2014, 2018) and age (n = 1) (Serino et al., 2018).
Table 3 gives an overview of the risk of bias of the included studies that were assessed with the Quality Assessment Tool for Quantitative Studies (Effective Public Healthcare Panacea Project, 1998). Overall, the quality of the cohort studies was either weak (n = 8) (Normand et al., 2011; Keizer et al., 2016; Serino et al., 2016a, 2017, 2018; Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019; Scarpina et al., 2019) or moderate (n = 2) (Preston and Ehrsson, 2014, 2018). The reason why no study had a strong overall quality was that none of the participants were randomly selected from a list of the target population, nor was another systematic selection process reported. Avoiding selection bias may be a low priority, especially in the recruitment of healthy participants. Furthermore, in the only cohort study with a follow-up (Keizer et al., 2016), <60% of participants completed the study, which resulted in a weak rating. Although this study was one of the four studies included for the meta-analysis, the follow-up results were not included in it and therefore did not contribute to bias. Other reasons for poor methodological quality were the absence of information about group characteristics (n = 2) (Ferrer-Garcia et al., 2018; Porras Garcia et al., 2019) or a description of the test validity and reliability (n = 6) (Normand et al., 2011; Keizer et al., 2016; Serino et al., 2016a, 2017, 2018; Scarpina et al., 2019).
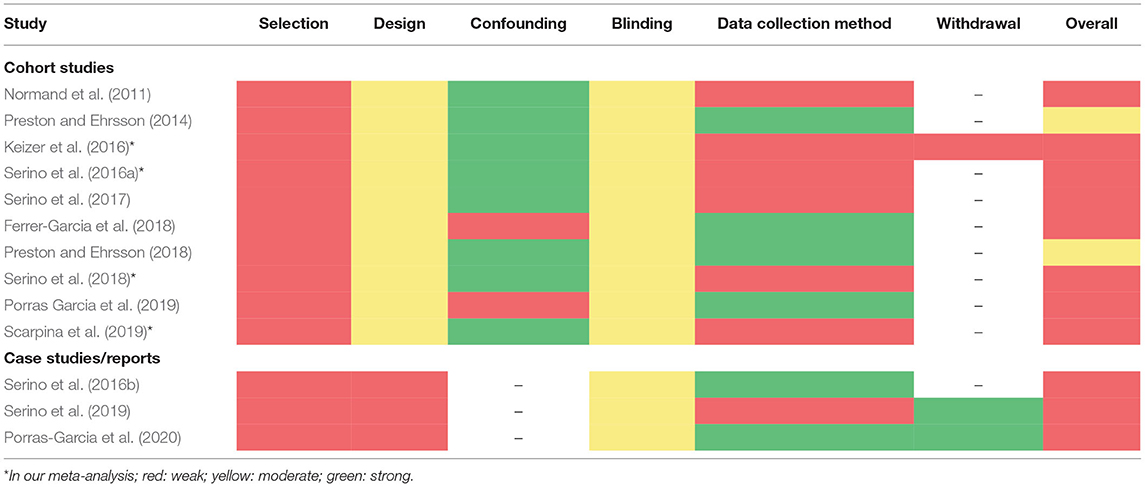
Table 3. Methodological quality of the included studies, assessed with the quality assessment tool for quantitative studies (Effective Public Healthcare Panacea Project, 1998).
Evaluation of all three case reports/studies resulted in weak overall study quality ratings, which is an inevitable consequence of their design type.
Figure 2 shows the effect sizes of FBI with a small virtual body in the studies investigating healthy females (k = 4, n = 85) for body size estimations of the width and circumference of shoulders, abdomen, and hips. Directly after the FBI in a small virtual body, subjects tended to estimate their body parts as smaller than before the illusion. This effect appears to be stronger for the shoulders and hips than for the abdomen and stronger for circumference than for the width. Shoulder circumference (SMD = −1.3; 95% CI: −2.2 to −0.4; p = 0.004) and hip circumference (SMD = −1.0; 95% CI: −1.6 to −0.4; p = 0.004) tended to result in the largest reduction in size estimates. Smaller effects were found for estimations of shoulder width (SMD = −0.4; 95% CI: −0.6 to −0.2; p = 0.000), hip width (SMD = −0.3; 95% CI: −0.4 to −0.1; p = 0.010), and both the abdomen circumference (SMD = −0.6; 95% CI: −1.5 to +0.1; p = 0.134) and width (SMD = −0.3; 95% CI: −0.7 to +0.03; p = 0.076).
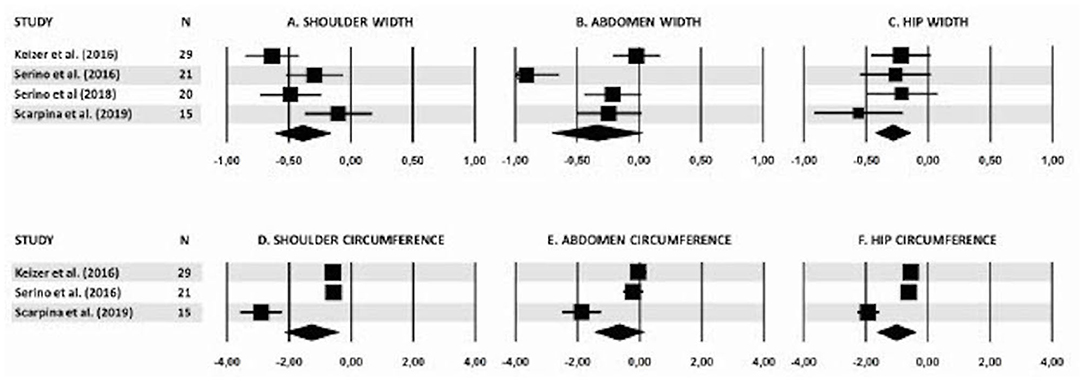
Figure 2. Forest plots of the effect sizes (and 95% CIs) of the FBI in a small virtual body-on-body size estimation in healthy female subgroups.
Concerning the results that were not aggregated, two studies investigated the effect of small virtual body FBI in patients with AN (Keizer et al., 2016; Serino et al., 2017). One study (Keizer et al., 2016) found a decrease in five of the six body size estimates (p's < 0.05), while the other (Serino et al., 2017) found this decrease only in the circumference of hips (z = −3.024; p = 0.002) and abdomen (z = −2.352; p = 0.019). In the only study with a group of patients with obesity (Scarpina et al., 2019), the estimation of hip circumference was reduced for both controls with obesity as well as for healthy controls [t(28) = 2.6; p = 0.014]. Interestingly, the individuals with obesity reported subjective embodiment scores that were comparable to those of the healthy participants [F(1, 28) = 0.25; p = 0.62) while owning a virtual body that was significantly smaller than their own.
While the three case reports/studies were integrated into multidisciplinary treatment, they all found positive effects (Serino et al., 2016b, 2019; Porras-Garcia et al., 2020).
All studies examining BI distortion after the embodiment of large virtual bodies (k = 4) used healthy individuals. We did not aggregate these studies because the outcome measures relate to different body parts (hips, abdomen, whole body), their populations contained different genders, and one study (Preston and Ehrsson, 2014) only reported a median. Two studies (Normand et al., 2011; Porras Garcia et al., 2019) found an increased estimated body size after the FBI (all p's < 0.05), while one (Preston and Ehrsson, 2014) found no significant effect (z = −0.72, p = 0.473). Another study (Ferrer-Garcia et al., 2018) found no effect when the outcomes were compared to baseline, but an increased estimated body size compared to an FBI in a real-size virtual body [F(1, 38) = 5.636; p = 0.023].
The studies about BI dissatisfaction were not aggregated because they used different questionnaires, their populations contained different genders, and one study (Preston and Ehrsson, 2014) only reported a median. The results of embodiment in large virtual bodies followed a similar pattern for BI dissatisfaction (k = 4), as two studies (Preston and Ehrsson, 2018; Porras Garcia et al., 2019) found a decrease in satisfaction (all p's < 0.05). Furthermore, there is one study (Preston and Ehrsson, 2014) that found no significant effect on satisfaction (z = −1.09, p = 0.275) and another (Ferrer-Garcia et al., 2018) that only found an effect when compared to an FBI in a real-size virtual body [F(1, 38) = 12.527; p = 0.001].
Concerning BI dissatisfaction after embodying a small virtual body (k = 2), one study (Preston and Ehrsson, 2014) found an increase in satisfaction (all p's < 0.05), while the other (Preston and Ehrsson, 2018) did not (all p's ≥ 0.263).
As a post-hoc procedure, we evaluated the effect of the control condition. Even after undergoing the perceptual alienation of asynchronous touch, most populations still experienced embodiment and changes in BI disturbance outcomes, though usually to a lesser extent compared to after synchronous visuotactile stimulation.
Adverse effects of VR or FBI were not reported in any of the studies.
In the reported meta-analysis, we showed that FBIs in a small virtual body are able to effectively reduce body size estimates in healthy female university students, especially the estimates of the circumference of the hips (SMD = −1.0) and shoulders (SMD = −1.3). In two out of four studies that examined the effect of FBIs in a large virtual body, body size estimates increased. These findings suggest that the participants' BIs were able to conform to the dimensions of the virtual body in both directions. Furthermore, BI dissatisfaction was reduced after an FBI in a small virtual body and, as mentioned earlier, increased in two out of four studies that tested an FBI in a large virtual body. Collectively, these data suggest that both components of BI disturbance can be modified directly after inducing an FBI.
While FBIs seem like a promising means for modulating BI disturbance, the limited amount of available data precludes us from drawing strong conclusions due to small-study effects (Sterne et al., 2000), such as publication bias (Gilbody et al., 2000). Heterogeneity further complicates the interpretation of these results because the studies used different populations (AN, obesity, and non-clinical), interventions (FBIs with several different body dimensions), and outcome measures (different questionnaires and visual tasks). Moreover, in general, the overall study quality was poor; all of the included studies appeared to be susceptible to selection bias because they mainly relied on self-referred participants, which could distort outcomes (Haynes and Robinson, 2019). Another caveat to consider is that body-part size estimation, which is the most frequently used assessment method for BI distortion, has not been tested for validity or reliability yet. Widths of hips, abdomens, and shoulders were usually estimated by participants placing adhesive markers on a wall, while circumferences were estimated with a string on the floor (Keizer et al., 2016; Serino et al., 2016a, 2017, 2018; Scarpina et al., 2019). More sophisticated and controlled methods currently exist, such as Body Image Assessment Software (Ferrer-García and Gutiérrez-Maldonado, 2008) and VR-based methods that allow participants to adjust their body size in virtuality settings (Corno et al., 2018; Mölbert et al., 2018; Neyret et al., 2020; Provenzano et al., 2020). Incorporating these evolved assessment methods might help improve the accuracy and reliability of these measurements.
After considering the limitations and pitfalls of these studies, it is still reasonable to suggest that these FBIs were able to elicit a form of change in cognition, emotion, or perception. These changes could imply that these individuals were sufficiently virtually embodied, corroborating the results from the subjective embodiment questionnaires. Interestingly, the FBI still succeeded when participants with obesity were put in a small virtual body (Serino et al., 2016b; Scarpina et al., 2019). However, in the control condition for embodiment, i.e., asynchronous visuotactile stimulation, participants often still experienced modified body size estimates, and some even reported experiencing embodiment, though to a lesser extent compared to after synchronous touch. Therefore, researchers may consider other control conditions, such as being in a virtual environment without owning a virtual body of any kind, which makes an FBI impossible.
Other interesting results are the reduced body size estimates in patients with AN after the embodiment of a small virtual body (Keizer et al., 2016; Serino et al., 2019). Since patients with AN are already thin, embodying a small virtual body would not be a markedly different experience from their everyday life. However, the researchers reported that despite being slimmer than the avatar, many patients with AN spontaneously mentioned “Oh! I'm so skinny now!” (Keizer et al., 2016). One possible neuroscientific framework for being able to explain these results is the Allocentric Lock Theory (ALT) (Riva, 2011, 2012; Riva et al., 2014; Malighetti et al., 2016; Lander et al., 2020). According to the ALT, patients with ED keep clinging to their distorted body image because they are unable to adequately update their “remembered” body (allocentric representation) with perceptual information from their “experienced” body (egocentric representation). As a result, they are “locked” in an unfavorable BI that they constructed long ago. In theory, the ability to swap their body with another body in VR could allow the individual to experience a novel egocentric representation that they have been illusioned to believe as their own. This could allow for a unique opportunity to better understand conflict resolution between the perceived virtual self and the actual self. However, more research is necessary to support the ALT.
This systematic review and the meta-analysis have several limitations. In the absence of sufficient control conditions, we calculated SMDs using pre-post differences; however, the validity of using this method has been called into question (Cuijpers et al., 2017). Although we agree that an effect size based on control conditions would be preferable, we argue that pre-post-SMDs could still be used in this instance. The most important reason to avoid pre-post SMDs is that the time between the pre- and post-test could significantly distort this value. For example, natural processes such as spontaneous recovery could cause an overestimation of the effect size. Here, however, the time between pre- and post-tests is almost equal to the duration of the FBI, which is less than half an hour. Because we do not expect non-FBI-related influences to intervene in this short time period, we assume that the pre-post differences can be attributed to the FBI.
Besides, because we analyzed all six body size estimations separately, we have to consider the problem of multiple testing: the chance of finding at least one significant effect increase with every additional simultaneous test. Since five out of six outcome measures resulted in statistically significant effects, we assume that multiple testing is not a prominent problem in this study.
Finally, this study is limited by the inability to assess publication bias. Due to an insufficient number of studies, we did not create a funnel plot. Moreover, we did not search for study protocols or other gray literature that might give an indication of all unpublished articles about this topic. Additionally, as previously stated above, we were only able to descriptively summarize the results of the BI dissatisfaction data. The lack of a standardized approach to measure both perceptual and affective components in a singular design is problematic for being able to more clearly determine the clinical utility of this method.
Despite the limited amount of available evidence, the implications of this meta-analysis cautiously support the attempts to further incorporate FBIs within clinical settings as a therapeutic and/or diagnostic tool for BI disturbance. One of the potential benefits of FBIs is that it allows patients to gain experiential knowledge of what it is like to have a different body with different physical dimensions. Experiential knowledge has the ability to enhance clinical insight from the perspectives of both the clinicians and the patients (De Vos et al., 2016). Moreover, the ability to acquire experiential knowledge within clinical settings may expand the potential of patients with a rigid thinking pattern who would otherwise drop out because of a lack of emotional engagement (Riva, 2003). Because VR is a flexible technology, clinicians can readily tailor any of the settings of the exposure based on which treatment phase the patient is in. In this regard, VR may have multiple advantages over mirror exposure. Namely, VR enables clinicians to have a limitless degree of precision over creating and scaling augmentations at any point in time, allowing for highly customized exposures on an individual-to-individual basis. This high degree of control may help ameliorate complications that are present in the early phases of treatment, specifically, creating a more graded level of exposure to anxiety-inducing stimuli. It is not possible to have this degree of control over the augmentations and exposure parameters in mirror therapy, which could cause significant distress (Windheim et al., 2011; Walker et al., 2012; Veale et al., 2016), leading to setbacks in treatment (Griffen et al., 2018).
During clinical assessment, VR technology can be supplemented with other tools that can help better objectively quantify BI-related outcomes during symptom provocation. Examples include being able to measure gazing patterns (Porras-Garcia et al., 2020) as well as using ambulatory apparatuses to measure sympathetic/parasympathetic activity (Van Bennekom et al., 2017). These data may be used in conjunction with subjective methods such as questionnaires, monitoring disease severity more accurately. Assessment is even possible without the live presence of a clinician, permitting the ability to remotely monitor the diseases of patients in their home settings through quantitative and/or qualitative measurements. This additional availability of disease monitoring could be used by both patients and clinicians to detect relapse tendencies, and subsequently, restart treatment. Other clinical tools that can be used to improve FBI interventions include the use of invasive brain stimulation devices. The methodological benefits of using invasive measures will allow researchers to implement closed-loop neuromodulation in tandem with VR visual feedback in singular paradigms to study both perceptual (i.e., modulate body size) and affective (i.e., psychiatric) components of these symptoms. Previous research has demonstrated that deep brain stimulation (DBS) of the nucleus accumbens (NAcc) in treatment-refractory patients with AN improved both BMI and psychiatric symptoms (Liu et al., 2020). By inducing different levels of FBIs that have varying levels of realness, i.e., perceived body size, researchers can further decode the neurophysiological markers of the reward system activity, which, in turn, can lead to nuanced approaches for trying to modulate that activity. Additional methodological benefits from a technological point of view include the use of non-invasive brain stimulation devices. Previous research utilized a combination of transcranial magnetic stimulation (TMS) and VR to show that temporally synced TMS pulses and visual feedback were able to induce illusory embodiment over a rubber hand, demonstrating the potential to substitute the use of external tactile stimulation for neurostimulation (Bassolino et al., 2018).
The data analyzed in this study is subject to the following licenses/restrictions: Three publicly available datasets were analyzed in this study. This data can be found at: https://doi.org/10.1371/journal.pone.0163921, https://doi.org/10.1089/cyber.2015.0229, https://doi.org/10.1089/cyber.2017.0674. One of the datasets that supports the findings of this study is not publicly available (Scarpina et al., 2019). Requests to access these datasets should be directed to Federica Scarpina, ZmVkZXJpY2Euc2NhcnBpbmFAdW5pdG8uaXQ=.
CT was responsible for conceptualizing and designing the work, data acquisition, data analysis, interpreting the data, and drafting the work. AG was responsible for data acquisition, data analysis, interpreting the data, and drafting the work. PK was responsible for interpreting the data and critically reviewing the work. FS was responsible for data analysis and critically reviewing the work. DD was responsible for critically reviewing the work and the final approval of the published version. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: APA. doi: 10.1176/appi.books.9780890425596
Arcelus, J., Mitchell, A. J., Wales, J., and Nielsen, S. (2011). Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch. Gen. Psychiatry 68, 724–731. doi: 10.1001/archgenpsychiatry.2011.74
Attia, E., and Walsh, B. T. (2009). Behavioral management for anorexia nervosa. N. Engl. J. Med. 360, 500–506. doi: 10.1056/NEJMct0805569
Bachner-Melman, R., Zohar, A. H., and Ebstein, R. P. (2006). An examination of cognitive versus behavioral components of recovery from anorexia nervosa. J. Nerv. Ment. Dis. 194, 697–703. doi: 10.1097/01.nmd.0000235795.51683.99
Bassolino, M., Franza, M., Bello Ruiz, J., Pinardi, M., Schmidlin, T., Stephan, M.A., et al. (2018). Non-invasive brain stimulation of motor cortex induces embodiment when integrated with virtual reality feedback. Eur. J. Neurosci. 47, 790–799. doi: 10.1111/ejn.13871
Bell, C., Kirkpatrick, S. W., and Rinn, R. C. (1986). Body image of anorexic, obese, and normal females. J. Clin. Psychol. 42, 431–439. doi: 10.1002/1097-4679(198605)42:3<431::AID-JCLP2270420305>3.0.CO;2-I
Bellisle, F., Monneuse, M. O., Steptoe, A., and Wardle, J. (1995). Weight concerns and eating patterns: a survey of university students in Europe. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 19, 723–730.
Berends, T., Boonstra, N., and van Elburg, A. (2018). Relapse in anorexia nervosa: a systematic review and meta-analysis. Curr. Opin. Psychiatry 31, 445–455. doi: 10.1097/YCO.0000000000000453
Borenstein, M., Hedges, L., Higgins, J., and Rothstein, H. (2013). Comprehensive Meta-Analysis Version 3.
Cash, T. F., and Deagle, E. A III. (1997). The nature and extent of body-image disturbances in anorexia nervosa and bulimia nervosa: a meta-analysis. Int. J. Eat. Disord. 22, 107–125. doi: 10.1002/(SICI)1098-108X(199709)22:2<107::AID-EAT1>3.0.CO;2-J
Cash, T. F., Fleming, E. C., Alindogan, J., Steadman, L., and Whitehead, A. (2002). Beyond body image as a trait: the development and validation of the body image states scale. Eat. Disord. 10, 103–113. doi: 10.1080/10640260290081678
Clus, D., Larsen, M. E., Lemey, C., and Berrouiguet, S. (2018). The use of virtual reality in patients with eating disorders: systematic review. J. Med. Internet Res. 20:e157. doi: 10.2196/jmir.7898
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Earlbaum Associates.
Collins, J. K., Beumont, P. J. V., Touyz, S. W., Krass, J., Thompson, P., and Philips, T. (1987). Variability in body shape perception in anorexic, bulimic, obese, and control subjects. Int. J. Eat. Disord. 6, 633–638. doi: 10.1002/1098-108X(198709)6:5<633::AID-EAT2260060506>3.0.CO;2-U
Corno, G., Serino, S., Cipresso, P., Baños, R. M., and Riva, G. (2018). Assessing the relationship between attitudinal and perceptual component of body image disturbance using virtual reality. Cyberpsychol. Behav. Soc. Netw. 21, 679–686. doi: 10.1089/cyber.2018.0340
Cuijpers, P., Weitz, E., Cristea, I. A., and Twisk, J. (2017). Pre-post effect sizes should be avoided in meta-analyses. Epidemiol. Psychiatr. Sci. 26, 364–368. doi: 10.1017/S2045796016000809
Dakanalis, A., Gaudio, S., Serino, S., Clerici, M., Carra, G., and Riva, G. (2016). Body-image distortion in anorexia nervosa. Nat. Rev. Dis. Primers 2:16026. doi: 10.1038/nrdp.2016.26
de Carvalho, M. R., Dias, T. R. S., Duchesne, M., Nardi, A. E., and Appolinario, J. C. (2017). Virtual reality as a promising strategy in the assessment and treatment of bulimia nervosa and binge eating disorder: a systematic review. Behav. Sci. 7:43. doi: 10.3390/bs7030043
De Vos, J. A., Netten, C., and Noordenbos, G. (2016). Recovered eating disorder therapists using their experiential knowledge in therapy: a qualitative examination of the therapists' and the patients view. Eat. Disord. J. Treat. Prev. 24, 207–223. doi: 10.1080/10640266.2015.1090869
Deeks, J.J., Dinnes, J., D'Amico, R., Sowden, A.J., Sakarovitch, C., Song, F., et al. (2003). Evaluating non-randomised intervention studies. Health Technol. Assess. 7, iii–x, 1–173. doi: 10.3310/hta7270
Dellazizzo, L., Potvin, S., Luigi, M., and Dumais, A. (2020). Evidence on virtual reality-based therapies for psychiatric disorders: meta-review of meta-analyses. J. Med. Internet Res. 22:e20889. doi: 10.2196/20889
Docteur, A., Urdapilleta, I., Defrance, C., and Raison, J. (2010). Body perception and satisfaction in obese, severely obese, and normal weight female patients. Obesity 18, 1464–1465. doi: 10.1038/oby.2009.418
Effective Public Healthcare Panacea Project (1998). Quality Assessment Tool for Quantitative Studies. Hamilton, ON: Effective Public Healthcare Panacea Project.
Ferrer-García, M., and Gutiérrez-Maldonado, J. (2008). Body image assessment software: psychometric data. Behav. Res. Methods 40, 394–407. doi: 10.3758/BRM.40.2.394
Ferrer-García, M., and Gutiérrez-Maldonado, J. (2012). The use of virtual reality in the study, assessment, and treatment of body image in eating disorders and nonclinical samples: a review of the literature. Body Image 9, 1–11. doi: 10.1016/j.bodyim.2011.10.001
Ferrer-Garcia, M., Porras-Garcia, B., Moreno, M., Bertomeu, P., and Maldonado, J. G. (2018). Embodiment in different size virtual bodies produces changes in women's body image distortion and dissatisfaction. Annu. Rev. CyberTherapy Telemed. 16, 111–117.
Galmiche, M., Déchelotte, P., Lambert, G., and Tavolacci, M. P. (2019). Prevalence of eating disorders over the 2000-2018 period: a systematic literature review. Am. J. Clin. Nutr. 109, 1402–1413. doi: 10.1093/ajcn/nqy342
Gardner, R. M., Jappe, L. M., and Gardner, L. (2009). Development and validation of a new figural drawing scale for body-image assessment: the BIAS-BD. J. Clin. Psychol. 65, 113–122. doi: 10.1002/jclp.20526
Gardner, R. M., Martinez, R., and Sandoval, Y. (1987). Obesity and body image: an evaluation of sensory and non-sensory components. Psychol. Med. 17, 927–932. doi: 10.1017/S0033291700000738
Garner, D. M., Garfinkel, P. E., Stancer, H. C., and Moldofsky, H. (1976). Body image disturbances in anorexia nervosa and obesity. Psychosom. Med. 38, 327–336. doi: 10.1097/00006842-197609000-00005
Gavin, A. R., Simon, G. E., and Ludman, E. J. (2010). The association between obesity, depression, and educational attainment in women: the mediating role of body image dissatisfaction. J. Psychosom. Res. 69, 573–581. doi: 10.1016/j.jpsychores.2010.05.001
Gilbody, S. M., Song, F., Eastwood, A. J., and Sutton, A. (2000). The causes, consequences and detection of publication bias in psychiatry. Acta Psychiatr. Scand. 102, 241–249. doi: 10.1034/j.1600-0447.2000.102004241.x
Glashouwer, K. A., van der Veer, R. M. L., Adipatria, F., de Jong, P. J., and Vocks, S. (2019). The role of body image disturbance in the onset, maintenance, and relapse of anorexia nervosa: a systematic review. Clin. Psychol. Rev. 74:101771. doi: 10.1016/j.cpr.2019.101771
Griffen, T. C., Naumann, E., and Hildebrandt, T. (2018). Mirror exposure therapy for body image disturbances and eating disorders: a review. Clin. Psychol. Rev. 65, 163–174. doi: 10.1016/j.cpr.2018.08.006
Haynes, A., and Robinson, E. (2019). Who are we testing? Self-selection bias in laboratory-based eating behaviour studies. Appetite 141:104330. doi: 10.1016/j.appet.2019.104330
Keizer, A., Van Elburg, A., Helms, R., and Dijkerman, H. C. (2016). A virtual reality full body illusion improves body image disturbance in anorexia nervosa. PLoS ONE 11:e0163921. doi: 10.1371/journal.pone.0163921
Koskina, A., Campbell, I. C., and Schmidt, U. (2013). Exposure therapy in eating disorders revisited. Neurosci. Biobehav. Rev. 37, 193–208. doi: 10.1016/j.neubiorev.2012.11.010
Lakens, D. (2013). Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front. Psychol. 4:863. doi: 10.3389/fpsyg.2013.00863
Lander, R., Heled, E., and Gur, E. (2020). Executive functioning and spatial processing in anorexia nervosa: an experimental study and its significance for the allocentric lock theory. Eat. Weight Disord. 25, 1039–1047. doi: 10.1007/s40519-019-00728-2
Liu, W., Zhan, S., Li, D., Lin, Z., Zhang, C., Wang, T., et al. (2020). Deep brain stimulation of the nucleus accumbens for treatment-refractory anorexia nervosa: a long-term follow-up study. Brain Stimulat. 13, 643–649. doi: 10.1016/j.brs.2020.02.004
Maister, L., Slater, M., Sanchez-Vives, M. V., and Tsakiris, M. (2015). Changing bodies changes minds: owning another body affects social cognition. Trends Cogn. Sci. 19, 6–12. doi: 10.1016/j.tics.2014.11.001
Malighetti, C., Serino, S., Riva, G., and Cipolletta, S. (2016). Inside and outside the self. Virtual reality and repertory grids in the spatial analysis of anorexic patients' meanings. Annu. Rev. Cyber Ther. Telemed. 14, 78–83.
Mathews, R. R. S., Hall, W. D., Vos, T., Patton, G. C., and Degenhardt, L. (2011). What are the major drivers of prevalent disability burden in young Australians? Med. J. Aust. 194, 232–235. doi: 10.5694/j.1326-5377.2011.tb02951.x
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and Group, T. P. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Med. 6:e1000097. doi: 10.1371/journal.pmed.1000097
Mölbert, S.C, Klein, L., Thaler, A., Mohler, B.J., Brozzo, C., Martus, P., et al. (2017). Depictive and metric body size estimation in anorexia nervosa and bulimia nervosa: a systematic review and meta-analysis. Clin. Psychol. Rev. 57, 21–31. doi: 10.1016/j.cpr.2017.08.005
Mölbert, S.C., Thaler, A., Mohler, B.J., Streuber, S., Romero, J., Black, M.J., et al. (2018). Assessing body image in anorexia nervosa using biometric self-avatars in virtual reality: attitudinal components rather than visual body size estimation are distorted. Psychol. Med. 48, 642–653. doi: 10.1017/S0033291717002008
Murray, S. B., Quintana, D. S., Loeb, K. L., Griffiths, S., and Le Grange, D. (2019). Treatment outcomes for anorexia nervosa: a systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 49, 535–544. doi: 10.1017/S0033291718002088
Neyret, S., Bellido Rivas, A. I., Navarro, X., and Slater, M. (2020). Which body would you like to have? The impact of embodied perspective on body perception and body evaluation in immersive virtual reality. Front. Robot. AI 7:31. doi: 10.3389/frobt.2020.00031
Normand, J. M., Giannopoulos, E., Spanlang, B., and Slater, M. (2011). Multisensory stimulation can induce an illusion of larger belly size in immersive virtual reality. PLoS ONE 6:e16128. doi: 10.1371/journal.pone.0016128
Oliveira, E. C., Bertrand, P., Lesur, M. R., Palomo, P., Demarzo, M. M., Cebolla, A., et al. (2016). “Virtual body swap: a new feasible tool to be explored in health and education,” in 2016 XVIII Symposium on Virtual and Augmented Reality (SVR), (Gramado), 81–89. doi: 10.1109/SVR.2016.23
Ouzzani, M., Hammady, H., Fedorowicz, Z., and Elmagarmid, A. (2016). Rayyan - a web and mobile app for systematic reviews. Syst. Rev. 5:210. doi: 10.1186/s13643-016-0384-4
Peck, T. C., Seinfeld, S., Aglioti, S. M., and Slater, M. (2013). Putting yourself in the skin of a black avatar reduces implicit racial bias. Conscious. Cogn. 22, 779–787. doi: 10.1016/j.concog.2013.04.016
Phillipou, A., Castle, D. J., and Rossell, S. L. (2018). Anorexia nervosa: eating disorder or body image disorder? Aust. N. Z. J. Psychiatry 52, 13–14. doi: 10.1177/0004867417722640
Porras Garcia, B., Ferrer Garcia, M., Olszewska, A., Yilmaz, L., González Ibañez, C., Gracia Blanes, M., et al. (2019). Is this my own body? Changing the perceptual and affective body image experience among college students using a new virtual reality embodiment-based technique. J. Clin. Med. 8:925. doi: 10.3390/jcm8070925
Porras-Garcia, B., Serrano-Troncoso, E., Carulla-Roig, M., Soto-Usera, P., Ferrer-Garcia, M., Figueras-Puigderrajols, N., et al. (2020). Virtual reality body exposure therapy for anorexia nervosa. A case report with follow-up results. Front. Psychol. 11:956. doi: 10.3389/fpsyg.2020.00956
Preston, C., and Ehrsson, H. (2014). H. Illusory changes in body size modulate body satisfaction in a way that is related to non-clinical eating disorder psychopathology. PLoS ONE 9:e85773. doi: 10.1371/journal.pone.0085773
Preston, C., and Ehrsson, H. H. (2018). Implicit and explicit changes in body satisfaction evoked by body size illusions: implications for eating disorder vulnerability in women. PLoS ONE 13:e0199426. doi: 10.1371/journal.pone.0199426
Provenzano, L., Porciello, G., Ciccarone, S., Lenggenhager, B., Tieri, G., Marucci, M., et al. (2020). Characterizing body image distortion and bodily self-plasticity in anorexia nervosa via visuo-tactile stimulation in virtual reality. J. Clin. Med. 9:98. doi: 10.3390/jcm9010098
Reed, D. L., Thompson, J. K., Brannick, M. T., and Sacco, W. P. (1991). Development and validation of the physical appearance state and trait anxiety scale (PASTAS). J. Anxiety Disord. 5, 323–332. doi: 10.1016/0887-6185(91)90032-O
Riva, G. (1997). The virtual environment for body-image modification (VEBIM): development and preliminary evaluation. Pres. Teleoper. Virt. Environ. 6, 106–117. doi: 10.1162/pres.1997.6.1.106
Riva, G. (2003). Virtual environments in clinical psychology. Psychotherapy 40, 68–76. doi: 10.1037/0033-3204.40.1-2.68
Riva, G. (2011). The key to unlocking the virtual body: virtual reality in the treatment of obesity and eating disorders. J. Diabetes Sci. Technol. 5, 283–292. doi: 10.1177/193229681100500213
Riva, G. (2012). Neuroscience and eating disorders: the allocentric lock hypothesis. Med. Hypotheses 78, 254–257. doi: 10.1016/j.mehy.2011.10.039
Riva, G., Bacchetta, M., Baruffi, M., Rinaldi, S., and Molinari, E. (1998). Experiential cognitive therapy in anorexia nervosa. Eat. Weight Disord. 3, 141–150. doi: 10.1007/BF03340002
Riva, G., Gaudio, S., and Dakanalis, A. (2014). I'm in a virtual body: a locked allocentric memory may impair the experience of the body in both obesity and anorexia nervosa. Eat. Weight Disord. 19, 133–134. doi: 10.1007/s40519-013-0066-3
Rorty, M., Yager, J., and Rossotto, E. (1993). Why and how do women recover from bulimia nervosa? The subjective appraisals of forty women recovered for a year or more. Int. J. Eat. Disord. 14, 249–260. doi: 10.1002/1098-108X(199311)14:3<249::AID-EAT2260140303>3.0.CO;2-O
Sarwer, D. B., Wadden, T. A., and Foster, G. D. (1998). Assessment of body image dissatisfaction in obese women: specificity, severity, and clinical significance. J. Consult. Clin. Psychol. 66, 651–654. doi: 10.1037/0022-006X.66.4.651
Scarpina, F., Castelnuovo, G., and Molinari, E. (2014). Tactile mental body parts representation in obesity. Psychiatry Res. 220, 960–969. doi: 10.1016/j.psychres.2014.08.020
Scarpina, F., Serino, S., Keizer, A., Chirico, A., Scacchi, M., Castelnuovo, G., et al. (2019). The effect of a virtual-reality full-body illusion on body representation in obesity. J. Clin. Med. 8:1330. doi: 10.3390/jcm8091330
Schilder, P. (1935). The Image and Appearance of the Human Body: Studies in the Constructive Energies of the Psyche. ed K. Paul (Trench: Trubner & Company Limited).
Serino, S., Chirico, A., Pedroli, E., Polli, N., Cacciatore, C., and Riva, G. (2017). Two-phases innovative treatment for anorexia nervosa: the potential of virtual reality body-swap. Annu. Rev. Cyber Ther. Telemed. 15, 111–115.
Serino, S., Pedroli, E., Keizer, A., Triberti, S., Dakanalis, A., Pallavicini, F., et al. (2016a). Virtual reality body swapping: a tool for modifying the allocentric memory of the body. Cyberpsychol. Behav. Soc. Netw. 19, 127–133. doi: 10.1089/cyber.2015.0229
Serino, S., Polli, N., and Riva, G. (2019). From avatars to body swapping: the use of virtual reality for assessing and treating body-size distortion in individuals with anorexia. J. Clin. Psychol. 75, 313–322. doi: 10.1002/jclp.22724
Serino, S., Scarpina, F., Dakanalis, A., Keizer, A., Pedroli, E., Castelnuovo, G., et al. (2018). The role of age on multisensory bodily experience: an experimental study with a virtual reality full-body illusion. Cyberpsychol. Behav. Soc. Netw. 21, 304–310. doi: 10.1089/cyber.2017.0674
Serino, S., Scarpina, F., Keizer, A., Pedroli, E., Dakanalis, A., Castelnuovo, G., et al. (2016b). A novel technique for improving bodily experience in a non-operable super-super obesity case. Front. Psychol. 7:837. doi: 10.3389/fpsyg.2016.00837
Slater, M., Spanlang, B., Sanchez-Vives, M.V., and Blanke, O. (2010). First person experience of body transfer in virtual reality. PLoS ONE 5:e10564. doi: 10.1371/journal.pone.0010564
Sterne, J. A., Gavaghan, D., and Egger, M. (2000). Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J. Clin. Epidemiol. 53, 1119–1129. doi: 10.1016/S0895-4356(00)00242-0
Thaler, A., Geuss, M. N., Mölbert, S. C., Giel, K. E., Streuber, S., Romero, J., et al. (2018). Body size estimation of self and others in females varying in BMI. PLoS ONE 13:e0192152. doi: 10.1371/journal.pone.0192152
Valentine, J. C., Pigott, T. D., and Rothstein, H. R. (2010). How many studies do you Need?: a primer on statistical power for meta-analysis. J. Educ. Behav. Stat. 35, 215–247. doi: 10.3102/1076998609346961
Valtolina, G. G. (1998). Body-size estimation by obese subjects. Percept. Mot. Skills 86, 1363–1374. doi: 10.2466/pms.1998.86.3c.1363
Van Bennekom, M. J., de Koning, P. P., and Denys, D. (2017). Virtual reality objectifies the diagnosis of psychiatric disorders: a literature review. Front. Psychiatry 8:163. doi: 10.3389/fpsyt.2017.00163
Veale, D., Miles, S., Valiallah, N., Butt, S., Anson, M., Eshkevari, E., et al. (2016). The effect of self-focused attention and mood on appearance dissatisfaction after mirror-gazing: an experimental study. J. Behav. Ther. Exp. Psychiatry 52, 38–44. doi: 10.1016/j.jbtep.2016.03.002
Walker, D. C., Murray, A. D., Lavender, J. M., and Anderson, D. A. (2012). The direct effects of manipulating body checking in men. Body Image 9, 462–468. doi: 10.1016/j.bodyim.2012.06.001
Wiederhold, B. K., Riva, G., and Gutiérrez-Maldonado, J. (2016). Virtual reality in the assessment and treatment of weight-related disorders. Cyberpsychol. Behav. Soc. Netw. 19, 67–73. doi: 10.1089/cyber.2016.0012
Windheim, K., Veale, D., and Anson, M. (2011). Mirror gazing in body dysmorphic disorder and healthy controls: effects of duration of gazing. Behav. Res. Ther. 49, 555–564. doi: 10.1016/j.brat.2011.05.003
Yee, N., and Bailenson, J. (2007). The proteus effect: the effect of transformed self-representation on behavior. Hum. Commun. Res. 33, 271–290. doi: 10.1111/j.1468-2958.2007.00299.x
Yuan, Y., and Steed, A. (2010). “Is the rubber hand illusion induced by immersive virtual reality?,” in 2010 IEEE Virtual Reality Conference (VR), (Boston, MA), 95–102. doi: 10.1109/VR.2010.5444807
Keywords: virtual reality, full body illusion, meta-analysis, mental healthcare, body image disturbance
Citation: Turbyne C, Goedhart A, de Koning P, Schirmbeck F and Denys D (2021) Systematic Review and Meta-Analysis of Virtual Reality in Mental Healthcare: Effects of Full Body Illusions on Body Image Disturbance. Front. Virtual Real. 2:657638. doi: 10.3389/frvir.2021.657638
Received: 23 January 2021; Accepted: 22 March 2021;
Published: 21 May 2021.
Edited by:
Frank Steinicke, University of Hamburg, GermanyReviewed by:
Catherine Preston, University of York, United KingdomCopyright © 2021 Turbyne, Goedhart, de Koning, Schirmbeck and Denys. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Collin Turbyne, Yy5hLnR1cmJ5bmVAYW1zdGVyZGFtdW1jLm5s
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.