
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Vet. Sci., 27 February 2025
Sec. Veterinary Surgery
Volume 12 - 2025 | https://doi.org/10.3389/fvets.2025.1528345
This article is part of the Research TopicThe Integration of Clinical Veterinary Anatomy and Diagnostic ImagingView all 14 articles
 Nicole Diana Wolf1*
Nicole Diana Wolf1* Lukas Kleiner2
Lukas Kleiner2 Christina Precht3
Christina Precht3 Julien Guevar4
Julien Guevar4 Mathieu de Preux5
Mathieu de Preux5 Franck Forterre1
Franck Forterre1 Pia Duever1
Pia Duever1Introduction: The delicate anatomy of the feline sacrum presents challenges for surgeons to perform a safe and accurate surgery without risking to damage vital neurovascular structures. In this context computer-assisted surgery represents an attractive minimally invasive surgical solution to increase the accuracy and safety of the intervention. This cadaveric study evaluates the feasibility and safety of a minimally invasive approach by a novice surgeon using computer navigation compared to traditional fluoroscopy as well as a new method for patient reference array positioning.
Material and methods: Eleven cats' cadavers were used to simulate sacroiliac joint luxation whereas one had to be excluded due to a sacral fracture. Sides were randomly assigned to two groups: (1) minimally invasive computer-assisted drilling group (MICA group); (2) fluoroscopy-controlled group (FC group). All surgeries were performed by a first-year ECVS resident. After positioning of the reference array, cone beam computer tomography scans were conducted for planning of the temporary and final fixation of the sacroiliac luxation. Final fixation was achieved through a minimally invasive approach via computer-assisted drilling of the iliac wing and the sacral body for the placement of a positional screw (2.4 mm). The other side was operated on via an open dorsal, fluoroscopy-controlled approach. Comparison between the two groups for surgical time, accuracy of screw placement, radiologic safety and the learning curve was recorded. Statistical analysis consisted of Fisher's exact test to compare the assigned radiological safety grades and the Wilcoxon signed-rank test for total surgery time and accuracy.
Results: Mean total time for MICA and FC groups were 44 min and 45 s and 19 min and 54 s, respectively. The mean total time for the first five cases was 53 min and 30 s in the MICA group and 20 min and 15 s in the FC group and improved to a mean total time of 36 min and 15 s in the MICA group and to 18 min and 40 s in the FC group in the second five cadavers. Accuracy aberration of surgery in the MICA group improved from a mean deviation on the target point, the end of the drill tract, from 4.2 mm in the first five to 0.9 mm in the second five cats. This criterion was only applicable in the MICA group. Evaluation for radiologic safety was assessed with three radiologic categories (I-III) and four subcategories (a-d). Additionally, the surgery was classified into radiographically safe implant placement (yes/no). The first five cats of the MICA as well as the FC group received a lower safety grade compared to the second five cats. The novel method for placement of the patient reference array was categorized as grade I without violating any vital structures in all 10 cats.
Discussion: The computer-assisted surgery for minimal invasive surgical fixation of sacroiliac luxation seems to be a safe procedure with a steep learning curve. Compared to previous study using the same technical set-up, the safety of the computer-assisted surgical procedure was improved by changing the smooth to the negative threaded pin to have better bone purchase for sufficient anchoring in the spinous process alone and therefore minimizing the risk for violation of the spinal canal.
Sacroiliac luxation is a common injury in cats, especially after high velocity trauma like road traffic accident or high-rise trauma. Sacroiliac luxation occurred in 59.2% of cats with pelvic injuries and accounted for 27% of all pelvic fractures. Sacroiliac separation was the second most common injury after pelvic floor fractures (1, 2). Treatment options are either conservative or surgical. If displacement is minimal or the luxation is unilateral with no concurrent pelvic fractures it might be treated conservatively with analgesics, cage rest and monitoring of urination and defecation (3). Surgical stabilization of sacroiliac luxation is indicated if there are signs of severe pain, inability to ambulate, neurologic deficits attributable to the luxation, severe instability or displacement (>50%) of one or both hemipelvises, pelvic outlet obstruction and/or concurrent orthopedic injuries (1, 4, 5).
The method of choice for surgical fixation is a cortical screw in lag fashion, or alternatively in a positional fashion (1, 2). Furthermore, a single transiliosacral pin in cats or a transiliosacral rod in dogs as well as transiliosacral toggle sutures, transileac pin/bolt/screw and tension band technique are described for successful stabilization (6–10). The fixation can be achieved through an open, dorsal or ventral, or closed, minimally invasive, approach with or without the help of fluoroscopy (3, 4, 11–16).
Since the sacral body of cats is very small, penetrating vital structures like the spinal canal dorsally, the intervertebral disc cranially and important nervous and vascular structures ventrally while placing the lag screw into the sacral body is a feared complication. Therefore, accurate positioning is essential, best at the first attempt (17, 18).
The correct position of the screw can be secured either through fluoroscopic control or as shown by the study of Kleiner et al. with computer-assisted surgery using an optical tracking system, the StealthStation (12, 16, 19, 20). However, this study showed, that placement of the patient tracker pin could increase the risk of complications by penetrating the spinal canal to achieve enough stability of the patient tracker. Open reduction techniques are invasive and correct screw placement can be challenging.
Previous studies showed that closed reduction and stabilization provided more accurate and consistent screw placement along safe corridors and optimal sacral purchase with minimal tissue dissection (12, 16, 20–24). Further documented benefits in human surgery are reduced blood loss, shorter surgical and hospitalization times, improved pain scores, faster weight bearing, lower complication rates and lower costs (25–32).
To the authors knowledge there is no study demonstrating the feasibility and safetiness of a minimal invasive approach for the fixation of the sacroiliac joint by computer-assisted drilling with any surgical navigation system. The hypothesis of this study is that minimal invasive computer-assisted surgery is more accurate than fluoroscopy-controlled drilling for the repair of sacroiliac joint luxation and that the procedure might be conducted by an unexperienced surgeon.
The study considered cadavers of 11 skeletally mature cats with an intact pelvic region that died or were euthanized for reasons unrelated to this study. Exclusion criteria were all pelvic or sacral pathologies like pelvic fractures, sacroiliac luxation, lumbosacral (sub) luxation and sacral fractures. Therefore, all cadavers underwent examination with a cone beam computed tomography (CBCT) scan beforehand. One cat had to be excluded due to an accidentally induced sacral fracture while manually luxating the sacroiliac joint during preparation which resulted in 10 cats included in the study.
The cat cadavers were donated to our institution by the owners who gave consent to use them for research purposes.
All images (Fluoroscopic and CBCT) were generated remotely without exposing personnel to radiation.
The first side was operated with the new computer-assisted technique through a minimal invasive approach (minimal invasive computer-assisted surgery, MICA). The second side of each cat was operated using an open dorsal, fluoroscopy controlled, approach (fluoroscopy-controlled surgery, FC). As a result, a total of 20 surgeries were carried out. The sides with which to start with (right or left sacroiliac joint) were randomized.
All joints of all cats were luxated manually with a Freer periosteal elevator through a ventral abdominal approach as described by Borer et al. (3, 11) and Montavon et al. (39).
For comparable stability during the surgeries, the first sacroiliac joint was luxated and surgically stabilized with the positional screw before the second side was luxated and fixated. Using a ventral abdominal approach, the pelvic symphysis was separated by an oscillating saw to imitate additional pelvic fractures (Colibri II; DePuy Synthes, West Chester, PA). Following this, only one side was luxated during each surgery.
Images for the minimally invasive computer-assisted surgical repair of sacroiliac luxation were acquired with a mobile cone beam computed tomography unit (CBCT; O-Arm; Medtronic, Louisville, Colorado), which was coupled to a surgical navigation system equipped with an optical tracking system, the StealthStation S8 (Medtronic). Specific instrumentation for the navigated procedure included a patient reference array, a navigated pointer (Passive Planar Marker, Medtronic) and an instrument tracker (SureTrak II clamps and tracker, Medtronic) mounted on a battery-powered surgical drill (Colibri II, DePuy Synthes, West Chester, PA) (Figure 1). Every instrument and tracker that had to be detected by the localizer camera of the optical tracking system was mounted with infrared reflecting spheres, also called fiducials. Furthermore, a radiolucent carbon fiber table (Opera Swing; General Medicale Merate SPA, Seriate, Italy) was used.
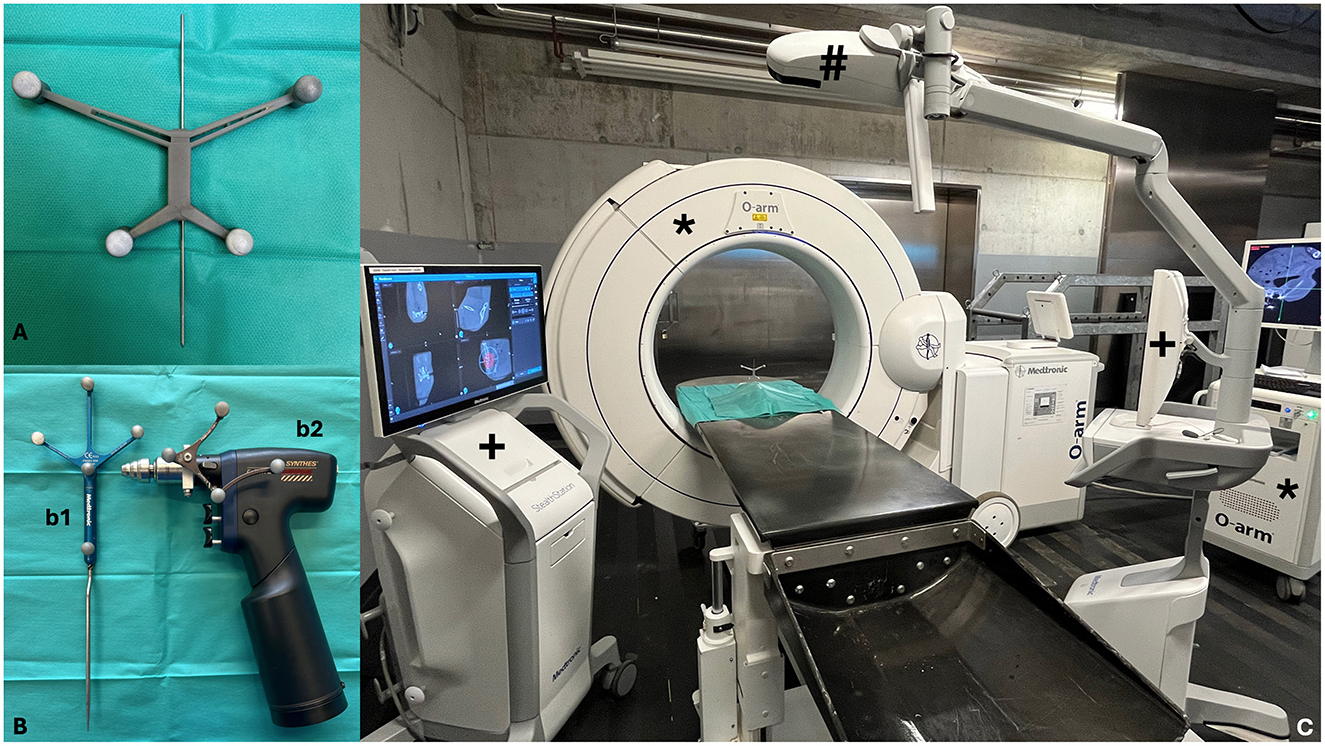
Figure 1. (A) 3D printed patient reference array with its reflecting spheres and pre-positioned 1.4 mm negative threaded pin. (B) Specific instrumentation for the navigated procedure: (b1) Navigated Pointer (Passive Planar Marker); (b2) Instrument tracker on a battery-powered drill (SureTrakII clamps and tracker on Colibri II). (C) Set-up for the computer-navigated drilling: O-arm with screen (*), Stealth Station S8 with its two screens (+), infrared camera for optical tracking (#).
A lighter, custom-made copy of the original patient reference array was 3D printed to avoid excessive lever arm on the small feline sacral bone. The patient reference array was a modification of the version used by Papacella-Beugger et al. (33), printed out of Formlabs Tough 1500 and weighted 9 g. The array was equipped with six holes through the middle segment to press fit a 1.4 mm negative threaded stainless-steel pin for the fixation into the sacral spinous process.
Further surgical instruments included a Backhaus clamp and a kern bone holding forceps, a 1-0 Kirschner (K)-wire, tap sleeves of the according size, 1.1 and 1.8 mm drill bit, a 2.4 mm self-tapping cortical screw, a screwdriver and a pin cutter.
All surgeries were performed by a first year European College of Veterinary Surgery (ECVS) resident without significant experience in orthopedic surgical procedures. For both procedures (i.e., the computer-assisted and the fluoroscopic guided drilling) the cats were placed in lateral recumbency on the carbon fiber table whereas the correct positioning with superimposition of the transverse processus of the seventh lumbar vertebra was evaluated through fluoroscopy.
One latero-lateral fluoroscopic projection was performed to confirm the correct positioning of the sacroiliac region of the cadaveric specimen in the isocenter of the gantry of the O-arm. A navigated 3D CBCT-scan (high resolution scan of 192 images during one tube rotation with an exposure of 120 kV and 20 mA and a voxel size of 0.4 × 0.4 × 0.8 mm3) was then acquired. During the scan acquisition, the camera of the StealthStation S8 had to detect simultaneously the tracker of the O-arm gantry and the patient reference array. The acquired CBCT data set was automatically transferred to the navigation system.
Preoperative surgical planning of the drill corridor was performed using the planning function of the Stealth Station S8. The entry point was set on the lateral aspect of the ilial wing whereas the target point marked the end of the drill hole at 50% of the depth in the sacral body. The planning of the drill corridor was done on the axial and coronal view and verified with probe's eye view.
The O-arm was then moved away from the surgical area to provide unrestricted access to the surgical site. To start the navigated surgical procedure, patient registration (32) was performed by touching the divot of the patient reference array with the tip of the navigated pointer. Instrument calibration was performed by following consecutive steps instructed by the StealthStation S8 for the identification of the plane, tip and long axis of the instrument. Calibration was repeated whenever a drill bit of different length was used, in order to display the correct length on the screen of the navigation system. For intraoperative, real-time orientation, the “navigation” mode was selected, and the trajectory 1 and 2 as well as the guidance function were displayed on the screen (Figure 2).

Figure 2. Screen view during computer-assisted drilling in trajectory 1 and 2 as well as guidance view. The dark blue cylinder represents the drill bit following the planned drill corridor (light blue line).
The location of the spinous process of the first and second sacral vertebra was determined by percutaneous palpation. Decision to use S1 or S2 was made individually depending on the size of S1 or S2 on each cadaver, whereas the larger spinous process was selected for patient reference array placement.
A stab incision to the cortex of the spinous process was performed using a #11 scalpel blade. A negative threaded 1.4 mm pin with the pre-positioned reference array and its fiducials was drilled at a 45-degree angle from ipsilateral through the spinous process and, in contrast to the study of Kleiner et al., not anchored into the roof of the sacrum (19). The reference array was moved away from the surgical site by bending the anchoring pin to prevent spatial interference with the navigated instruments and ensure continuous detection by the localizer camera throughout the procedure.
The first CBCT scan was conducted to plan the location in the caudal part of sacrum for the temporary fixation pin to hold the reduction in place. Reduction of the sacroiliac luxation was achieved with the help of a Backhaus clamp in the ischial tuberosity to facilitate movement of the bone while manually pushing the wing of the ilium in its desired place. Assessment of reduction was estimated with the symmetrical palpation of the iliac wings in its cranial and dorsal plane.
The navigated pointer was used to determine the location of the entry point according to the predefined plan on the StealthStation 8. A stab incision was then performed with a #11 scalpel blade onto the near cortex of the ilium in the correct location as seen on the screen for temporary fixation pin placement. A 1.1 mm tap sleeve was placed and the location and direction of the pin placement was verified again with the help of the navigated pointer and the 1-0 K-wire was drilled through the tap sleeve in the desired direction to temporarily keep the ilium to the sacrum.
Another CBCT scan was made to assess the reduction and create the plan for the computer-assisted drilling of a hole through the ilium and sacrum for correct screw placement in the center of the sacral body, as described by Burger et al. (17). If the reduction was not accurate, the previously described procedure had to be repeated.
After planning and calibration of the instruments, the hole in the ilium and sacrum was drilled under surgical navigation guidance. Stability of the patient reference array and thus accuracy of the navigation system was verified before each drilling by touching the entry point of the patient reference array pin with the navigated pointer and by simultaneously assessing the virtual images displayed on the screen of the navigation system.
The first three cats were directly drilled with a 1.8 mm drill bit of 100 mm in length. As slippage of the drill bit on the iliac wing as well as bending of the drill was evident, the following seven cats were predrilled with a smaller 1.1 mm drill bit of 37 mm in length and the use of a 2.0 mm tap sleeve to protect the soft tissues. The first hole was enlarged with a 1.8 mm drill bit. A 2.4 mm self-tapping positional cortical screw of appropriate length was placed.
The conducted drill holes aimed to reach only 50% of the width of the sacral body to not interfere with the subsequent contralateral procedure.
A conventional open dorsal approach to the sacroiliac joint was chosen. To allow good visualization of the sacral wing the iliac wing was retracted caudoventrally by an assistant. A surgical power drill (Colibri II) was used to place a 0.8 mm K-wire in the sacral wing to facilitate the correct screw placement through the sacral body according to Burger et al. (17) via fluoroscopic control. The K-wire placement was targeted at the center of the first sacral body. Fluoroscopic control was performed after every new pin positioning. Once the correct positioning of the pin was achieved, the pin was removed and the hole within the sacral body was sequentially overdrilled with a 1.1 mm and a 1.8 mm drill bit. Reduction of the luxation was carried out under visualization and held in place by the assistant until the equivalent hole in the wing of the ilium was drilled with a 1.8 mm drill bit and the 2.4 mm self-tapping positional cortical screw of appropriate length was placed.
For all procedures “total time” was noted and split into “time on patient” and “time off patient”. “Total time” started with the placement of the patient reference array (MICA group) or the manipulation of the previously luxated sacroiliac joint (FC group). It ended in both groups after the placement of the 2.4 mm positional screw. “Time on patient” was defined as time needed for the surgical procedures which includes surgical approach, placement of the reference array, reduction and temporary fixation of the luxation, the drilling process itself and placement of the screw. “Time off patient” was defined as time needed for the imaging procedures in both groups (CBCT scans and fluoroscopy) and the planning of temporary fixation and the drill hole in the MICA group.
The additional control CBCT scans taken only for radiologic evaluation were not included in any of the time measurements.
The accuracy of the drilling was evaluated for the MICA group where the initial plan and the actual drill hole could be compared via CBCT images (Figure 3). Entry and target points for the conducted drill hole were defined on postoperative CBCT images using Stealth Navigation software (Medtronic). To compare the initial plan and the actual drill hole, pre- and postoperative CBCT images had to be manually merged to achieve superimposition of the images so that 3D coordinates could be extracted. To calculate the deviation in millimeters between the initial plan and the actual drill hole, the coordinates of the entry and target points were described by the Euclidean distance formula
to calculate the deviation in millimeters to compare the initial plan and the actual drill hole (33, 34).
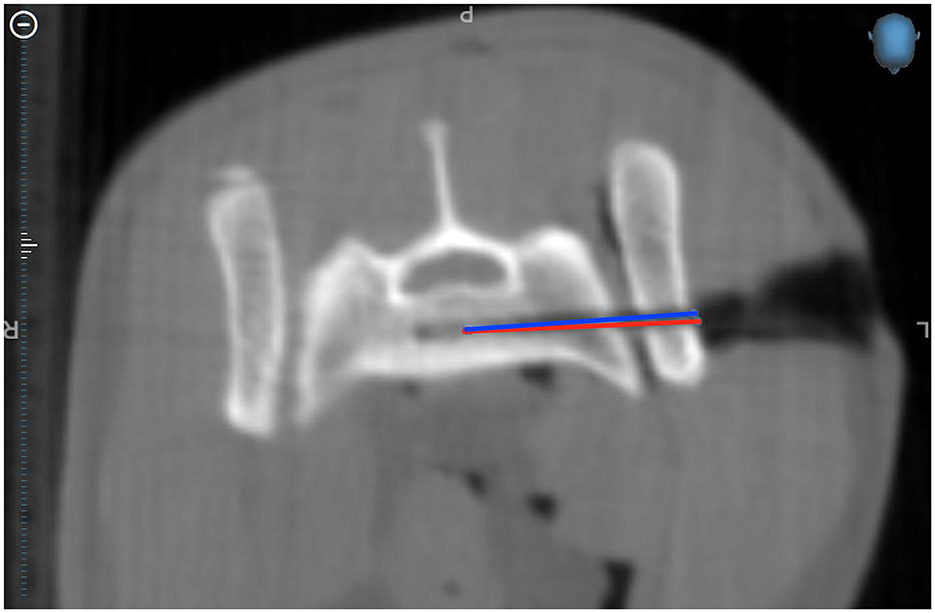
Figure 3. Merged CBCT images where you can see the planned drill corridor (red) and the actual drill corridor (blue) in Cat 10.
To ensure an optimal radiologic evaluation, five additional CBCT scans were conducted after drilling the hole in the sacral body. These included: one scan after completing the computer-assisted drill hole, one scan with the screw placed on the first side, one scan following the fluoroscopy guided freehand drill hole with the first screw still in place, one scan with the first and second screw in place, and the final scan without any implants, showing only the two drill holes.
The postoperative CBCT images were evaluated by a Diplomate of the European College of Veterinary Diagnostic Imaging (DECVDI), C.P. The primary focus was the course of the drill hole in the 20 surgical procedures and the positioning of the patient reference array in the 10 cats in the MICA-group. Radiologic safety was assessed using three categories (I–III) and four directional subcategories (a–d) (Table 1). Additionally, surgeries were classified based on radiographic safety of implant placement (yes/no). Category I represented a drill hole entirely within the vertebral body, category II was assigned if the screw was in contact or eroding the sacral cortex, and category III indicated a violation of the cortex. Categories I and II were considered radiographically safe, whereas category III was classified as radiographically unsafe. The subcategory described the direction of deviation: a = dorsally, b = ventrally, c = cranially, d = caudally. As the drill holes only penetrated 50% of the sacral body to avoid contralateral interference, radiologic evaluation extended to 60% of bone purchase, as recommended for fixation of sacroiliac luxation.
The safety of the patient reference array was categorized into grade I, IIIa, or IIIb. Grade I was assigned if the patient reference array was located within the dorsal spinous process of S1 or S2. Grade III indicated sacral cortex penetration, with IIIa specifying intrusion into the vertebral canal and IIIb indicating direction toward the soft tissues ventral to the sacrum.
The learning curve was analyzed by comparing the first five to the last five surgeries. Wilcoxon signed-rank test was used to compare the two groups concerning the total surgery time. More insight was gained by dividing the total time between the time spent on the cadaver and the time spent planning the surgery. The same method was used to compare the deviation from the target for the screw entry and target sites. Fisher's exact test was performed to compare the frequency of the assigned radiological safety grades. The analysis was performed using the statistical software R (version 4.3.1) in Rstudio (Posit Software, version 2023.09.1.494).
The cadavers of 10 mature domestic shorthair cats were included in the study, seven males and three females with a median weight of 3.88 kg (range 2.1–6.3 kg).
Comparison of the first five procedures to the second five showed an improvement in total time, accuracy and safety, especially in the MICA group.
Inadequate reduction of the sacroiliac luxation was detected on preprocedural CBCT scan and had to be corrected in two cases (Cat 1 and Cat 3). Reduction was adequate in the remaining 8 cats.
The MICA group showed a significantly slower “total time” (p = 0.002) with a mean of 44 min 45 s ± 11 min 53 s compared to the mean “total time” of 19 min 54 s ± 6 min 58 s in the FC group.
For the MICA group the mean “time on patient” was 23 min 50 s ± 8 min 55 s and the “time off patient” was 20 min 40 s ± 5 min 43 s. For the FC group, both, time on-and off-patient were shorter, with the “time on patient” being 14 min 40 s ± 4 min 42 s and “time off patient” of 4 min 40 s ± 3 min 40 s.
In the MICA group, although not statistically significant (p = 0.056), the mean “total time” decreased from 53 min 30 s ± 8 min 20 s to 36 min 15 s ± 8 min 40 s in the first vs. the second five procedures. A less pronounced improvement was seen in the FC group from the first five cases with a mean “total time” of 20 min 30 s ± 3 min 45 s to 18 min 50 s ± 9 min 20 s in the second five procedures, this was also not statistically significant (p = 0.31).
When comparing “time on patient” between the first five and the second five procedures, neither the MICA group (p = 0.222) nor the FC group (p = 0.69) resulted in a statistically significant difference. The “time on patient” decreased in the MICA group from 28 min 20 s ± 10 min 30 s to 19 min 36 s ± 6 min 10 s whereas the FC group showed a minimal improvement in “time on patient” from 15 min 15 s ± 4 min to 14 min 16 s ± 5 min 43 s.
The reduction from the mean “time off-patient” of 24 min 55 s ± 3 min 40 s in the first five procedures to a mean “time off-patient” of 16 min 30 s ± 3 min 35 s in the second five procedures in the MICA group was statistically significant (p = 0.032). This comparison in the FC group did not show a significant improvement (p = 0.222) with a mean “time off-patient” of 5 min 10 s ± 7 min 42 s in the first five compared to the “time off-patient” of 4 min 34 s ± 4 min 40 s in the second five cases.
This criterion was only measurable in the MICA group.
The 10 cases in the MICA group showed a mean deviation of 2 mm at the entry point and a mean deviation of 2.5 mm at the target point. Although not statistically significant (p = 0.063), there was an improvement in the accuracy aberration when comparing the first five to the second five procedures.
The mean deviation on the entry point decreased from 2.4 to 1.6 mm and on the target point from 4.2 to 0.9 mm in the first five compared to the second five procedures.
In all cats, the safety grade for placement of the patient reference array was categorized as I, with a trajectory running correctly within the dorsal spinous process of S1 or S2.
Inferior safety grade for the screw placement was assigned to the first three cadavers of both groups with a IIIb in the MICA and IIb in the FC group compared to grade I in the remaining seven cadavers.
The safety grade in the MICA group was worse in the first five trials compared to the last five ones. Three cadavers (3/10) were categorized a IIIb, whereas the trajectory was violating the ventral cortex of the sacrum or was even ventrally outside of the sacrum and therefore rated as radiographically unsafe implant placement. The following seven cadavers (7/10) were classified in category I and fulfilled the criterion for radiographically safe implant placement (Figures 4A, B).

Figure 4. Final CBCT scans for radiologic evaluation without implants. (A) Drill corridor graded as IIIb where it ended ventrally outside of the sacrum and was categorized as radiographically unsafe (Cat 2, MICA procedure). (B) Drill corridor graded as I where it runs within the vertebrae and was categorized as radiographically safe (Cat 9, MICA procedure on the left side of the image and FC procedure on the right side of the image).
In the FC group the first and third cat were categorized as IIb with the trajectory being in contact or eroding the ventral cortex of the sacrum (2/10). All the other were evaluated as category I (8/10), which means the procedures on all 10 cadavers achieved radiographically safe implant placement.
The radiologic grading wasn't statistically significant when performing the Fisher's exact test due to a small sample size (count range 2–7 for the different grades).
Computer-assisted surgery for minimally invasive surgical fixation of feline sacroiliac luxation seems to be a safe procedure with a steep learning curve for a novice surgeon. Several cadaver surgeries were needed to get comfortable with the handling of the technical instruments and the navigation software. In our experimental set-up, the reduction and surgical fixation of sacroiliac luxation via an open dorsal, fluoroscopy-controlled approach also resulted in safe implant placement in most of the cadaveric specimens. Although the minimally invasive procedure was associated with a significantly longer surgical time, it avoids the creation of a large surgical approach and improves intraoperative control of implant placement.
Compared to the study of Kleiner et al. (19) the safety of the computer-assisted surgery was improved by changing the smooth to the negative threaded pin to have better bone purchase for sufficient anchoring in the spinous process alone and therefore minimizing the risk of violation of the spinal canal.
The technical equipment used from Medtronic is very user-friendly. The only downside was the recognition of the custom-made 3D printed patient reference array by the Stealth Station Navigation system in some trials. In one case (Cat 6) it took 15 min and several adjustments in position of the infrared camera for the Stealth Station to recognize the patient reference array and to conduct a computer navigated scan. In other trials, one of the four reflecting spheres had to be removed for the infrared camera to recognize the patient reference array. These challenges did prolong the “time off patient” but did not interfere with the accuracy. As previously described, the patient reference array was a modification to the version used by Papacella-Beugger et al. (33) Our patient reference array was out of Formlabs Tough 1500 and weighted 9 g whereas the one from Papacella-Beugger is out of polyactide with a weight of 12 g compared to the original patient reference array by Medtronic with 59 g. Modification included the fixation with a press fit negative-threaded pin going through the patient reference array compared to a pre-printed fixation method with variable adapters by Papacella-Beugger. Challenges in recognition of the custom-made patient reference array by the Stealth Station Navigation system were not described in their study and we assume it to be due to a slight deviation in the geometry of the arms of the patient reference array resulting from 3D printing.
The positioning of the patient reference array is a critical point in computer-assisted surgery. An accurate correlation between the CBCT images and therefore the plan and the anatomical structures in the surgical field are only given, if the patient reference array is securely anchored to the target bone throughout the whole procedure, in an angle-stable manner. If any alteration of the spatial relationship between the array and the target bone occurs, the CBCT scans must be redone and a new plan according to the new reference has to be made. In the study of Kleiner et al. the reference array was fixated with a smooth pin which was drilled through the spinous process of S1 or S2 and anchored in the roof of the sacrum (19). As in some of the first cases the pin penetrated the spinal canal, the fixation of the reference array was changed for our study. We used a negative threaded pin to improve stability and eliminating the need for a second anchoring point into the roof of the sacrum due to better bone purchase of the threaded version. As a result, positioning in the spinous process was sufficiently stable and the safety of the procedure was increased. None of the pins in the present study violated any important structures. Furthermore, by placing the patient reference array in the same bony structure as the target bone (Spinous process of S1 or S2 for surgeries on the sacral body), a potential error in surgical accuracy aberration was minimized. As described in other studies (35, 36), applying pressure on the bone during surgical manipulation can alter its imaged position if the patient reference array is fixed to a different structure than the target structure. If the patient reference array is fixed to the same structure where the surgery takes places, movement of it correlates with the image due to a similar movement of the reference array. Nevertheless, movement and manipulation of the imaged position should be minimized.
As demonstrated in previous studies, a minimally invasive approach for the repair of sacroiliac joint luxation led to more accurate screw placement and less soft tissue damage and therefore a reduction of patient morbidity might be anticipated (12, 16, 20, 23, 24). The control for screw placement was usually done by fluoroscopy. The safety of screw placement in sacroiliac luxation with the help of computer navigation was proven in a study by Kleiner et al. (19), which lead to a combination of a minimally invasive approach with the guidance of computer navigation. The basics of the minimal invasive computer-assisted surgical procedure are similar to the minimal invasive approach described by Tomlinson et al. (12). The advantage of this new technique is the control of reduction via CBCT before fixation and the precise planning of the drill corridor through the ilium and sacral body while sparing the soft tissue. However, for cases with a longer duration from trauma to surgical repair, the surgeon should be prepared to convert to an open approach if a closed approach is not amenable for adequate reduction screw placement.
Due to the CBCT scans, planning process and set up of the technical equipment of the surgical navigation, the total time is doubled in the MICA group compared to the FC group, but with training a clear reduction in time is anticipated as seen when comparing the first five to the second five trials. Thus, training and practice are essential to optimize time when using computer navigation. Similar results were seen in the study of Kleiner et al. (19) with a mean duration of 23 min and 37 s for the computer navigated group and 9 min and 47 s in the FC group with improvement of time in both groups with training. However, a team approach should be considered when applying this technique in clinical cases to optimize the workflow of the navigated procedure in order to shorten the overall surgery time and minimize the associated complications (37).
The observed surgical accuracy aberration from the planned to the actual drilled corridor of 2 mm at the entry point and 2.5 mm at the target point were similar to the results with an open approach computer-assisted surgery shown by Kleiner et al. with a deviation of 2 mm at the entry point and 1.6 mm at the target point in the same anatomical location (19). Comparable results were achieved using the same CBCT-based computer-assisted drilling procedure in other anatomical locations (33, 34). Papacella-Beugger had a median entry point deviation of 1.8 mm (range: 0.3–3.7 mm) and median exit point deviation of 1.6 mm (range: 0.6–5 mm) in lumbar plate fixation (33). In the study by Guevar et al. for minimally invasive stabilization in the thoracolumbar spine the overall mean deviations for the entry points were 2.2 mm for the experienced surgeon and 3.7 mm for the novice surgeon. For the exit points, deviations were 3.0 and 5.0 mm, respectively. Significant difference was found in accuracy between the experienced and novice surgeon for the deviations overall (34). An accuracy aberration of 2 and 2.5 mm in entry and target point matches the accuracy expectations when applying an optical tracking system (like the Stealth Station) for a computer-assisted orthopedic surgical procedure (38). Overall, a deviation in the close range of 2 mm meets the high standards in precision required when working on a bony structure as small as a feline sacrum. Comparison of drill hole accuracy between an experienced surgeon vs. a lesser experienced surgeon in this anatomical location was performed by Kleiner et al. and did not show a significant difference (19). Therefore, this study was carried out by novice first year ECVS resident surgeon only.
The first three cadavers with the highest deviation on entry as well as target point and the poorest radiology safety grade (IIIb in MICA Group/IIb in FC Group) were drilled with a 1.8 mm drill bit. As slippage of the drill bit on the iliac wing was evident, the following 7 cats where predrilled with a smaller 1.1 mm drill bit and showed less deviation from the initial plan and scored a better radiological safety grade. The 1.1 mm drill bit was shorter than the 1.8 mm drill bit (35 vs. 100 mm). It was found that longer drill bits tend to bend more easily and therefore the actual position of the drill tip does not match with the fiducials on the handpiece and the drilling is not accurate to the planned procedure on the screen. Similar observations with bending of the drill were made in equine computer-assisted surgeries, whereas recommendation to use a shorter drill bit was expressed (35). Nevertheless, the lack of surgical experience in drilling uneven, slippery surface on the iliac wing as well as first using a longer drill bit is hypothesized to have influenced the results more than the lack of experience with the navigation system as demonstrated by improvement of accuracy with the transition to a shorter drill bit and more training.
To facilitate radiologic evaluation, account for possible artifacts due to the metal implants and avoid interference between the bilateral drill holes, additional CBCT scans were performed after the surgical procedures with the implants in place and after removal. In a clinical setting, only one CBCT scan would typically be required for temporary fixation without computer navigation, or two scans if computer navigation is used, as opposed to the seven CBCT scans performed in this study. Since time measurement was paused for the additional CBCT scans, total time could only be reduced by omitting the scan for the temporary fixation pin planning. Since there are no critical structures located directly ventral to the vertebra, a previous study by Shales et al. (18, 21) did not consider screws penetrating the ventral cortex as mispositioned. Nevertheless, we did categorize our first three cadavers as a radiographically unsafe implant placement because there was not enough bone purchase before violating the ventral cortex and stability of the fixation could not be ensured as well as neurologic deficits could not be excluded in this ex vivo study. We did consider Category I and II as radiographically safe implant placement where the cortex was not violated, and a good surgical outcome would be expected. Due to possible neurological deficits and screw loosening and therefore unsatisfactory surgical outcome, category III was classified as radiographically unsafe implant placement. Depending on the direction of deviation (a = dorsally, b = ventrally, c = cranially, d = caudally) in category III a revision would be needed or even a fatal outcome could be anticipated.
One of the main limitations of the study is its cadaveric nature with artificially induced unilateral sacroiliac luxation which does not provide an accurate imitation of a clinical case as muscle trauma and additional pelvic fractures are not identical. The feasibility has to be tested for the closed reduction of the sacroiliac luxation in an in vivo study where muscle contracture is present or if a bilateral luxation, and therefore change in known landmarks, complicates the surgery. Furthermore, both sides of each cat were used for this study, this could cause a bias in anatomical landmarks when doing the second procedure. Cautious extrapolation of the results of this experimental study to clinical cases is warranted, and the potential for screw loosening and neurological deficits should be assessed in an in vivo study, particularly in cats that were categorized in group IIIb where the trajectory violated the ventral cortex.
Different surgical approaches (minimally invasive vs. open approach) were used for the two different groups and therefore limited an exact comparison concerning time and visualization of anatomical structures. As all surgeries were performed by a first-year surgery resident without major orthopedic experience, some initial problems were evident, like slippage of the drill bit on the bony surface. On the other hand, a steep learning curve was observed. Results could differ if a more experienced surgeon had performed the surgeries.
To allow direct comparison of the plan and the actual drillhole the pre- and postoperative CT images were manually merged using Stealth Station software and could therefore lead to an error in accuracy.
The effect of increased exposure to radiation of patients treated by MICA in comparison to those of the FC group should also be taken in consideration but was not estimated in the present study. This has yet to be tested.
Computer-assisted surgery for minimally invasive sacroiliac luxation in cats can be considered as a safe alternative procedure with a high accuracy for correct screw positioning. The time needed for surgery is increased compared to fluoroscopy controlled freehand surgery but a steep learning curve positively affecting accuracy and duration of the procedure was observed, leading to the assumption that with more experience the observed results might be further improved and further emphasize the advantages of not performing a large open approach, especially regarding intra- and postoperative morbidity.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethical approval was not required for the study involving animals in accordance with the local legislation and institutional requirements because the study only included cadavers of client owned cats who gave consent to use them for research purposes. No alive animals were included in the study.
NW: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. LK: Conceptualization, Data curation, Formal analysis, Methodology, Writing – review & editing. CP: Data curation, Formal analysis, Resources, Writing – review & editing. JG: Writing – review & editing, Resources, Validation. MP: Writing – review & editing, Conceptualization, Software. FF: Conceptualization, Supervision, Writing – review & editing. PD: Conceptualization, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Open access funding by University of Bern.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Gen AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bookbinder PF, Flanders JA. Characteristics of pelvic fracture in the cat. Vet Comp Orthop Traumatol. (1992) 5:122–7.
2. Moens NMM, DeCamp CE. Fractures of the pelvis (Ch. 56). In:Tobias KM, Johnston SA, editors. Small Animal Veterinary Surgery sl. St Louis, MO: Elsevier (2018).
3. Borer LR, Voss K, Montavon PM. Ventral abdominal approach for screw fixation of sacroiliac luxation in clinically affected cats. Am J Vet Res. (2008) 69:549–56. doi: 10.2460/ajvr.69.4.549
4. Tomlinson JL. Fractures of the pelvis. In:Douglas S, , editor. Textbook of Small Animal Surgery. 3rd ed. Philadelphia, PA: WB Saunders Co. (2003). p. 1989–2001.
5. Brinker WO, Piermattei DL, Flo GL. Sacroiliac Fracture-Luxation. Philadelphia, PA: WB Saunders Co. (1997). p. 398–403.
6. Parslow A, Simpson DJ. Bilateral sacroiliac luxation fixation using a single transiliosacral pin: surgical technique and clinical outcomes in eight cats. J Small Anim Pract. (2017) 58:330–6. doi: 10.1111/jsap.12659
7. Leasure CS, Lewis DD, Sereda CW, Mattern KM, Jehn CT, Wheeler JL. Limited open reduction and stabilization of sacroiliac fracture-luxations using fluoroscopically assisted placement of a trans-iliosacral rod in five dogs. Vet Surg. (2007) 36:633–43. doi: 10.1111/j.1532-950X.2007.00315.x
8. Froiedefond B, Moinard M, Caron A. Outcomes for 15 cats with bilateral sacroiliac luxation treated with transiliosacral toggle suture repair. Vet Surg. (2023) 52:983–93. doi: 10.1111/vsu.14008
9. Yap FW, Dunn AL, Farell M, Calvo I. Trans-iliac pin/bolt/screw internal fixation for sacroiliac luxation or separation in cats: six cases. J Feline Med Surg. (2014) 16:354–62. doi: 10.1177/1098612X13503650
10. Raffan PJ, Joly CL, Timm PG, Miles JE. A tension band technique for stabilisation of sacroiliac separations in cats. J Small Anim Pract. (2002) 43:255–60. doi: 10.1111/j.1748-5827.2002.tb00068.x
11. Borer LR, Voss K, Montavon PM. Ventral abdominal approach for screw fixation of sacroiliac luxation in cadavers of cats and dogs. Am J Vet Res. (2008) 69:542–8. doi: 10.2460/ajvr.69.4.542
12. Tomlinson JL. Minimally invasive repair of sacroiliac luxation in small animals. Vet Clin North Am Small Anim Pract. (2012) 42:1069–77. doi: 10.1016/j.cvsm.2012.06.005
13. Jourdain M, Fernandes D, Védrine B, Gauthier O. Fluoroscopically-assisted closed reduction and percutaneous fixation of sacroiliac luxations in cats using 2.4mm headless cannulated compression screws: description, evalutation and clinical outcome. Vet Surg. (2024) 53:603–12. doi: 10.1111/vsu.14070
14. Permattei DL, Johnson KA. Approacht to the ventral aspect of the sacrum. In:Permattei DL, Johnson KA, editors. Permattei's Atlas of Surgical Aproaches to the Bones and Joints of the Dog and Cat. s.l. St Louis, MO: WB Saunders Co. (2014). p. 320–1.
15. Alexander JE, Archibald J, Cawley AJ. Approach to the wing of the ilium and dorsal aspect of the sacrum. In:Johnson KA, , editor. Permattei's Atlas of Surgical Approaches to the Bones and Joints of the Dog and Cat. s.l. St Louis, MO: WB Saunders Co. (2014). p. 312–5.
16. Tomlinson JL, Cook JL, Payne JT, Anderson CC, Johnson JC. Closed reduction and lag screw fixation of sacroiliac luxations and fractures. Vet Surg. (1999) 28:188–93. doi: 10.1053/jvet.1999.0188
17. Burger M, Forterre F, Brunnberg L. Surgical anatomy of the feline sacroiliac joint for lag screw fixation of sacroiliac fracture-luxation. Vet Compar Orthop Traumatol. (2004) 17:146–51. doi: 10.1055/s-0038-1632803
18. Shales CJ, White L, Langley-Hobbs SJ. Sacroiliac luxation in the cat: defining a safe corridor in the dorsoventral plane for screw insertion in lag fashion. Vet Surg. (2009) 38:343–8. doi: 10.1111/j.1532-950X.2009.00509.x
19. Kleiner L, Wolf ND, Precht Ch, Haenssgen K, Forterre F, Duever P. Feline saroiliac luxation: comparison of fluoroscopy-controlled freehand vs. computer-navigated drilling in the sacrum—a cadaveric study. Front Vet Sci. (2024) 11:1510253. doi: 10.3389/fvets.2024.1510253
20. Tonks CA, Tomlinson JL, Cook JL. Evaluation of closed reduction and screw fixation in lag fashion of sacroiliac fracture-luxations. Vet Surg. (2008) 37:603–7. doi: 10.1111/j.1532-950X.2008.00414.x
21. Shales CJ, Moores A, Kulendra E, White C, Toscano M, Langley-Hobbs S. Stabilization of sacroiliac luxation in 40 cats using screws inserted in lag fashion. Vet Surg. (2010) 39:696–700. doi: 10.1111/j.1532-950X.2010.00699.x
22. DeChamp CE, Braden TD. Sacroiliac fractures-separation in the dog: a study of 92 cases. Vet Surg. (1985) 14:127–30. doi: 10.1111/j.1532-950X.1985.tb00841.x
23. Déjardin LM, Marturello DM, Guiot LP, Guillou RP, DeCamp CE. Comparison of open reduction versus minimally invasive surgical approaches on screw position in canine sacroiliac lag-screw fixation. Vet Compar Orthop Traumatol. (2016) 29:290–7. doi: 10.3415/VCOT-16-02-0030
24. Rollins A, Balfour R, Szabo D, Chesvick CM. Evaluation of fluoroscopic-guided closed reduction versus open reduction of sacroiliac fracture-luxations stabilized with a lag screw. Vet Compar Orthop Traumatol. (2019) 32:467–74. doi: 10.1055/s-0039-1693471
25. Sciulli RL, Daffner RH, Altman DT, Altman GT, Sewecke JJ. CT-guided iliosacral screw placement: technique and clinical experience. Am J Roentgenol. (2007) 188:W181–92. doi: 10.2214/AJR.05.0479
26. Smith AG, Capobianco R, Cher D, Rudolf L, Sachs D, Gundanna M, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res. (2013) 7:1–14. doi: 10.1186/1750-1164-7-14
27. Ledonio CG, Polly DW, Swiontkowski MF. Minimally invasive versus open sacroiliac joint fusion. Are they similarly safe and effective? Clin Orthop Relat Res. (2014) 472:1831–8. doi: 10.1007/s11999-014-3499-8
28. Heiney J, Capobianco R, Cher D. A systematic review of minimally invasive sacroiliac joint fusion utilizing a lateral transarticular technique. Int J Spine Surg. (2015) 9:40. doi: 10.14444/2040
29. Pieske O, Landersdorfer C, Trumm C, Greiner A, Wallmichtrath J, Gottschalk O, et al. CT-guided sacroiliac percutaneous screw placement in unstable posterior pelvic ring injuries: accuracy of screw position, injury reduction and complications in 71 patients with 136 screws. Injury. (2015) 46:333–9. doi: 10.1016/j.injury.2014.11.009
30. Tonetti J, Carrat L, Lavalleé St, Pittet L, Merloz Ph, Chirossel JP. Percutaneous iliosacral screw placement using image guided techniques. Clin Orthop Relat Res. (1998) 354:103–10. doi: 10.1097/00003086-199809000-00013
31. Wang H, Wang F, Leong APY, Xu L, Chen X, Wang Q. Precision insertion of percutaneous sacroiliac screws using a novel augmented reality-based navigation system: a pilot study. Int Orthop. (2016) 40:1941–7. doi: 10.1007/s00264-015-3028-8
32. Cher DJ, Frasco MA, Arnold RJG, Polly DW. Cost-effectiveness of minimally invasive sarcroiliac joint fusion. ClinicoEcon Outcom Res. (2016) 8:1–14. doi: 10.2147/CEOR.S94266
33. Papacella-Beugger A, Forterre F, Samer E, Guevar J, Müller A, Planchamp B, et al. Spinal neuronavigation for lumbar plate fixation in miniature breed dogs. Vet Compar Orthop Traumatol. (2024) 37:279–85. doi: 10.1055/s-0044-1787707
34. Guevar J, Samer ES, Precht C, Rathmann JMK, Forterre F. Accuracy and safety of neuronavigation for minimally invasive stabilization in the thoracolumbar spine using polyaxial screws-rod: a canine cadaveric proof of concept. Vet Compar Orthop Traumatol. (2022) 35:370–80. doi: 10.1055/s-0042-1750056
35. de Preux M, Vidono B, Koch Ch. Influence of a purpose-built frame on the accuracy of computer-assisted orthopedic surgery of equine extremities. Vet Surg. (2020) 49:1367–77. doi: 10.1111/vsu.13484
36. Kim TT, Johnson JP, Pashman R, Drazin D. Minimally invasive spinal surgery with intraoperative image-guided navigation. Biomed Res Int. (2016) 2016:16235. doi: 10.1155/2016/5716235
37. Windhagen H, Thorey F, Ostermeier S, Emmerich J, Wirth CJ, Stukenborg-Colsman C. Das Navigatorkonzept—Prozessoptimierung in der navigierten Knieendprothetik. Orthopäde. (2005) 34:1125–26. doi: 10.1007/s00132-005-0853-2
38. Medtronic. StealthStation S8 Cranial Optical Kurzhandbuch. Louisville, CO: Medtronic Navigation. (2019).
Keywords: minimally invasive, computer-assisted orthopedic surgery (CAOS), sacroiliac luxation, feline, Stealth Station S8, cadaveric study
Citation: Wolf ND, Kleiner L, Precht C, Guevar J, de Preux M, Forterre F and Duever P (2025) Minimally invasive computer-assisted repair of feline sacroiliac luxation—a cadaveric study. Front. Vet. Sci. 12:1528345. doi: 10.3389/fvets.2025.1528345
Received: 14 November 2024; Accepted: 10 February 2025;
Published: 27 February 2025.
Edited by:
Ozan Gündemir, Istanbul University Cerrahpasa, TürkiyeReviewed by:
Caner Bakici, Ankara University, TürkiyeCopyright © 2025 Wolf, Kleiner, Precht, Guevar, de Preux, Forterre and Duever. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicole Diana Wolf, bmljb2xlLndvbGZAdW5pYmUuY2g=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.