- 1VCA Japan Dolphin Animal Hospital Urawamisono, Saitama, Japan
- 2Department of Veterinary Teaching Hospital, Faculty of Agriculture, Tokyo University of Agriculture and Technology, Tokyo, Japan
- 3Department of Animal Medicine (Internal Medicine), Faculty of Veterinary Medicine, Suez Canal University, Ismailia, Egypt
- 4Department of Small Animal Medical Center, Obihiro University of Agriculture and Veterinary Medicine, Obihiro, Japan
- 5Ashiya Limone Animal Hospital, Ashiya, Japan
- 6Department of Clinical Engineering, National Hospital Organization Osaka National Hospital, Osaka, Japan
- 7VCA Japan Shiraishi Animal Hospital, Saitama, Japan
- 8Department of Small Animal Clinical Sciences, College of Veterinary Medicine University of Florida, Gainesville, FL, United States
Background: Myxomatous mitral valve disease (MMVD) is the most common acquired heart disease in dogs. Mitral valvuloplasty (MVP) addresses regurgitation, but the pre- and postoperative changes in myocardial function remain uncertain.
Objectives: This study evaluated myocardial motion before and after MVP using two-dimensional speckle-tracking echocardiography (2D-STE).
Animals: Eight client-owned dogs undergoing MVP for MMVD.
Methods: Myocardial deformation was assessed by 2D-STE before surgery and at 1- and 3-months post-surgery. Measurements included left ventricular global longitudinal strain (GLS), global circumferential strain (GCS), global radial strain (GRS), cardiac twist, and right ventricular free wall GLS (RVFW-GLS).
Results: Postoperative decreases were observed in left ventricular internal dimensions, left atrial size, and early diastolic myocardial velocity, with an increase in peak late diastolic velocity. LV-GLS decreased at 1 month (−14.4%) and 3 months (−16.3%) compared to preoperative values (−24.4%) (p = 0.0078, p = 0.015). GCS decreased at 1 month (−12.9%) and 3 months (−14.8%) compared to preoperative values (−21.7%) (p = 0.0078). GRS decreased at 1 month (27.7%) and 3 months (32.0%) compared to preoperative values (67.7%) (p = 0.0078). No significant changes were observed in RVFW-GLS. Peak systolic twist increased at 3 months (9.1° vs. 4.9°, p = 0.039). Peak systolic apical rotation showed an upward trend at 3 months (p = 0.109). Left ventricular twist was mildly affected by LVIDd, LVIDDN, and sphericity index (R2 = 0.187, p = 0.034; R2 = 0.33, p = 0.0029; R2 = 0.22, p = 0.019).
Conclusions and clinical importance: Postoperative myocardial motion approached reference values, indicating significant improvement, particularly in left ventricular twisting motion. These findings highlight the positive impact of surgery on cardiac function in dogs with MMVD.
1 Introduction
Myxomatous mitral valve degeneration (MMVD) stands as a primary factor necessitating valve repair or replacement as it leads to mitral regurgitation, cardiac enlargement, systolic dysfunction, and eventual heart failure (1). Recent insights have underscored the potential of mitral valvuloplasty (MVP) to facilitate full recuperation, MVP emerges as a promising therapeutic avenue for MMVD, fostering reverse remodeling and restoring the dilated dimensions of the left atrium and left ventricle to their physiological state (2, 3).
Left ventricular fractional shortening (FS) is commonly used to assess left ventricular systolic function in veterinary medicine. Preoperative FS often increases due to improved preload. However, post-surgery, FS tends to normalize, although some cases show persistently low FS values despite the absence of heart failure signs (4), indicating that conventional echocardiography alone may not provide a precise assessment of postoperative cardiac function.
Two-dimensional speckle-tracking echocardiography (2D-STE) is an advanced imaging technique that allows for comprehensive evaluation of myocardial function through deformation imaging. It provides valuable insights into both global and regional myocardial function, as well as the ability to quantify cardiac rotation and synchronicity parameters not accessible with conventional echocardiography (5).
Resolution of regurgitation and congestion before and after mitral valve surgery has been observed (4). However, it’s unclear if this mitigated dysfunction translates into postoperative improvement or simply slows progression. Precise evaluation of surgery’s impact on cardiac function is crucial to substantiate its efficacy.
Speckle-tracking strain analysis has demonstrated precise reflection of LV myocardial function with angle-independent assessment (6). Regarding Global longitudinal strain (GLS), earlier studies have indicated a decrease in GLS in both ventricles post-surgery (7). However, in veterinary medicine, preoperative left ventricular GLS was reported to remain unchanged depending on the disease stage (8), and alterations in GLS following surgery have not yet been documented. Global circumferential strain (GCS) and Global radial strain (GRS) have been reported to increase with enlargement of the left ventricular chamber (8). However, the postoperative course of these parameters remains unclear. The subepicardial and subendocardial fibers are warped around the LV into left- and right-handed helix causing clockwise and counterclockwise rotation of the base and the apex. The left ventricular rotational deformation includes systolic twist and diastolic untwist, resembling the wringing and unwringing of a towel, can be evaluated by 2D-STE. Twist has been noted to deteriorate in severe MMVD (9), where the LV twist variables were decreased with increasing systolic LV internal diameter (10), suggesting that twisting and untwisting may improve following MVP. The postoperative changes of twist in dogs undergoing MVP remains unexplored.
This study aims to clarify improvements in GLS and twist of both ventricles after MVP in MMVD cases. GLS is a sensitive indicator of longitudinal myocardial fiber function, and twist reflects the torsional mechanics of the heart, both of which are critical for effective cardiac output. Monitoring these parameters post-surgery provides valuable insights into the heart’s recovery and reverse remodeling process, which may not be fully captured by conventional echocardiography alone. Understanding these changes can help optimize post-surgical management and further refine surgical techniques. By analyzing GLS and twist changes post-surgery, it seeks to address limitations in evaluating postoperative cardiac function solely through conventional echocardiography, emphasizing 2D-STE.
2 Materials and methods
2.1 Animals
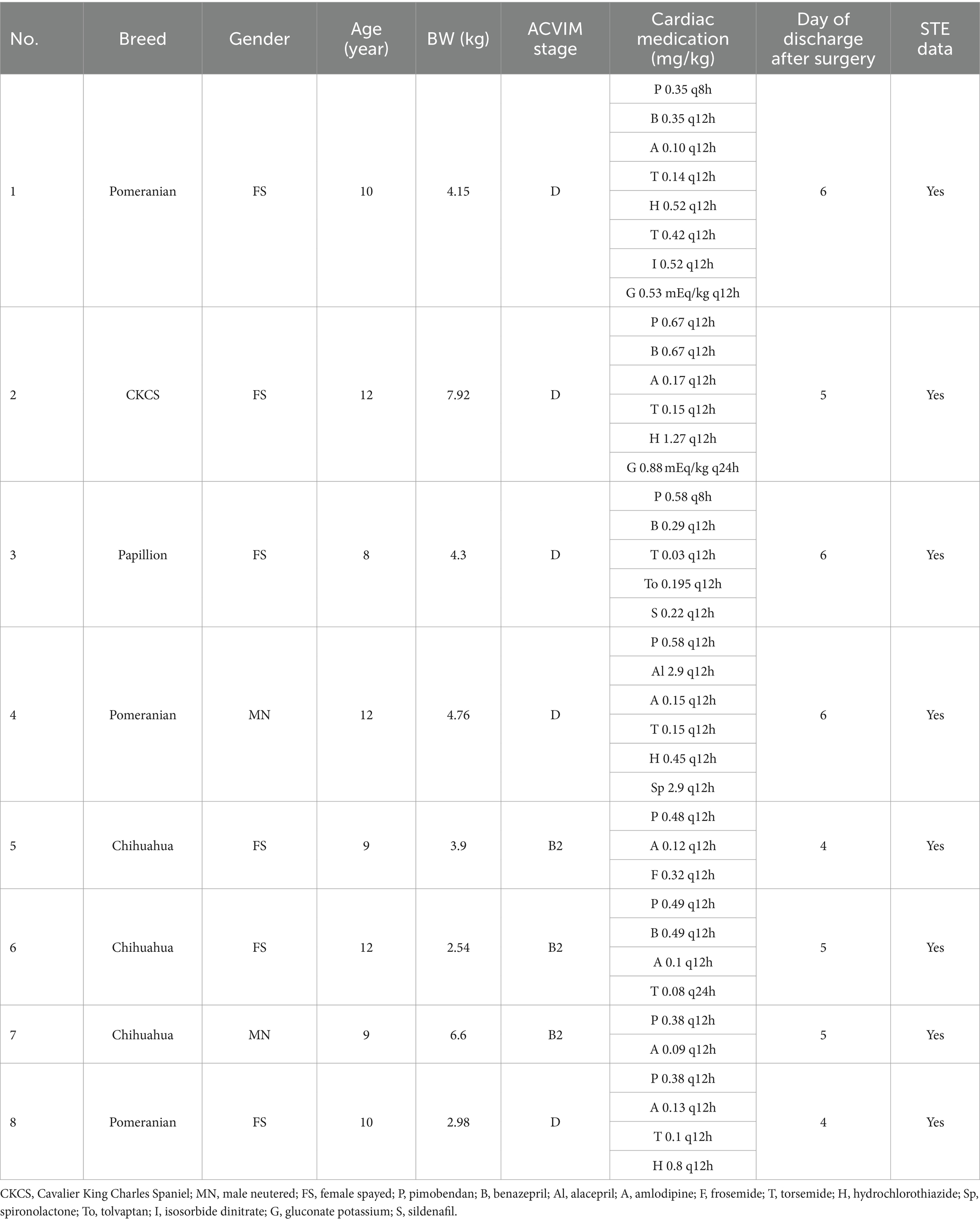
Table 1 describes the signalments of the patients included in the study. Eight client-owned dogs undergoing mitral valvuloplasty (MVP) exclusively for MMVD between January 2022 and April 2023 at Dolphin Animal Hospital Urawamisono were recruited for this study. Prior to enrollment, informed consent was obtained from the respective dog owners. Diagnosis of MMVD was established through conventional cardiac echocardiography, and dogs were categorized according to the guidelines set by the American College of Veterinary Internal Medicine (ACVIM). Among the eight dogs, three were classified as Stage B2, and five as Stage D. Each dog received treatment tailored to their specific stage. Some Stage B2 cases were already receiving diuretic medication prior to MVP. Baseline measurements were recorded within 1 month before the scheduled surgery date. Post-MVP, the dogs underwent a two-week course of pimobendan (Pimobeheart, Kyoritsu Seiyaku Corporation, Tokyo, Japan), Potassium Clavulanate Amoxicillin Hydrate (Augmentin, GlaxoSmithKline K.K., Tokyo, Japan), Orbifloxacin (Victas®, Bussan Animal Health Co., Ltd., Osaka, Japan), and rivaroxaban (Rivaroxaban, Bayer Yakuhin, Ltd., Osaka, Japan) administration. Following this period, all cases ceased the use of inotropic agents and antibiotics, while rivaroxaban continued for 3 months postoperatively. In one instance, amlodipine besilate (Norvasc Tablets, Viatris Pharmaceutical Co., Ltd., Tokyo, Japan) administration resumed 2 weeks after surgery, while in another case, benazepril hydrochloride (FORTECOL®, Elanco Japan Co., Ltd., Tokyo, Japan) and amlodipine were maintained due to chronic kidney disease.
In two out of eight cases, medications impacting hemodynamics were introduced 2 weeks post-surgery (in case 3: amlodipine and benazepril, in case 4: amlodipine). Nonetheless, the administration of pimobendan and diuretics, pivotal in managing MMVD, was ceased in all cases 2 weeks following MVP.
2.2 Mitral valvuloplasty
Mitral valvuloplasty was conducted following established procedures as previously described (2, 11). In summary, an incision was made in the left fifth intercostal chest, and the pericardial tent was deployed. A cannula containing myocardial protection fluid was then inserted into the aorta. Cardiac arrest was induced using myocardial protection after aortic blockade with an extracorporeal circulatory system. Subsequently, access to the mitral valve apparatus was gained through a left atrial incision. Reconstruction of the mitral annulus was performed, followed by closure of the left atrium. Upon completion, the cannula was removed, and the patient was gradually weaned from extracorporeal circulation following the release of cardiac arrest.
2.3 Echocardiography
2.3.1 Conventional echocardiography
Echocardiographic assessments were conducted utilizing a Hitachi Arietta 60 or Hitachi Arietta 750 ultrasound system, both manufactured by Hitachi Aloka Medical in Tokyo, Japan, equipped with a 2–9 MHz probe. Standard conventional echocardiography was performed from both right and left sides (12), encompassing ordinary long-axis and short-axis views for each dog at baseline (preoperative) and two time points postoperative (at 1 and 3 months).
The following conventional echocardiographic indices were measured: left ventricular internal dimension in diastole (LVIDd), LVIDd normalized to body weight, using an allometric approach (LVIDDN), fractional shortening, peak mitral E wave velocity, peak mitral A wave velocity, the E-to-A ratio, and mitral regurgitation (MR) velocity. Additionally, the ratio of the left atrial dimension to the aortic annulus dimension (LA/Ao) was measured at the basal level using two-dimensional echocardiography. Tissue Doppler imaging was utilized to measure myocardial velocity during early diastole (E′) at the lateral annulus and septal annulus, as well as the tricuspidal velocity during systole (S′) at the lateral annulus. LV sphericity index (LVSI) was calculated as the ratio of the long axis to the short axis of the left ventricle (13).
2.3.2 Two-dimensional speckle tracking echocardiography
Left ventricular (LV) twist was assessed utilizing basal- and apical-level images from the right parasternal short-axis view. Left ventricular global longitudinal strain (LV-GLS) was derived from the apical four-chamber section. Global circumferential strain (GCS) and global radial strain (GRS) were obtained at the papillary muscle level images from the right parasternal short-axis view (14). Analysis of right ventricular (RV) free wall global longitudinal strain (RVFW-GLS) was conducted using RV-focused view. Digital cine-loops capturing three consecutive heart cycles, with a frame rate ranging from 72 to 86 frames per second, were acquired from all dogs and stored as DICOM files for subsequent processing on echo machine. Data from three dogs (Nos. 6, 7, 8 on Table 1), where accurate evaluation of RVFW-GLS was hindered due to issues with the acquired images, were excluded from analysis.
2.4 Statistical analysis
The data were presented as median and interquartile range. Statistical analyses were conducted using commercial statistical software (Prism 10.0v; GraphPad Software Inc., San Diego, CA, United States). Preoperative and postoperative 1-month, as well as preoperative and postoperative 3-month data obtained from conventional echocardiographic examination and 2D-STE analysis, were assessed using the Wilcoxon signed-rank test, respectively. A p-value less than 0.05 was considered to indicate statistical significance for the Gaussian approximation of nonparametric data. Nonparametric data are presented as median and range. Additionally, the relationship between the data obtained from conventional echocardiographic examination and 2D-STE analysis or between 2D-STE analysis was evaluated using simple linear regression analysis. A significance level of p < 0.05 was considered statistically significant.
3 Results
3.1 Echocardiographic measurement
3.1.1 Conventional echocardiography
The results of the conventional echocardiographic examination are presented in Table 2. Heart rate (HR), LVIDd, LVIDDN, LA/Ao, FS, E′ sep, E′ lat exhibited significant decreases at both 1 month and 3 months post-surgery compared to preoperative values, while mitral A velocity significantly increased at 3 months post-surgery. Additionally, LVSI significantly increased at both 1 month and 3 months after MVP. Furthermore, E/E′ sep significantly decreased at 1 month after surgery compared to preoperative values. Body weight (BW) showed a significant decrease at 1 months after surgery compared to preoperative values (Figure 1).
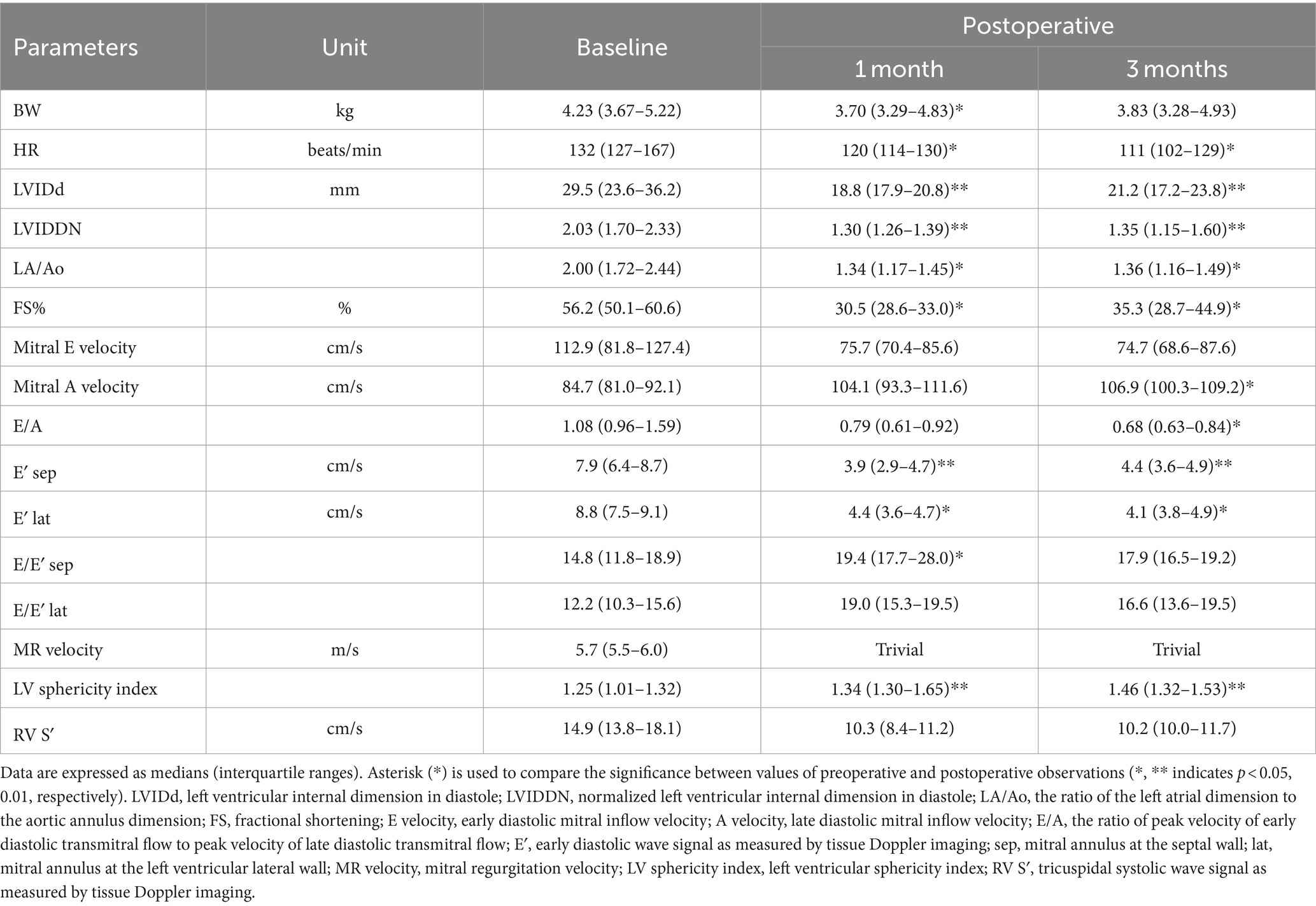
Table 2. Conventional echocardiography results for 8 dogs preoperatively, 1 month, and 3 months postoperatively.
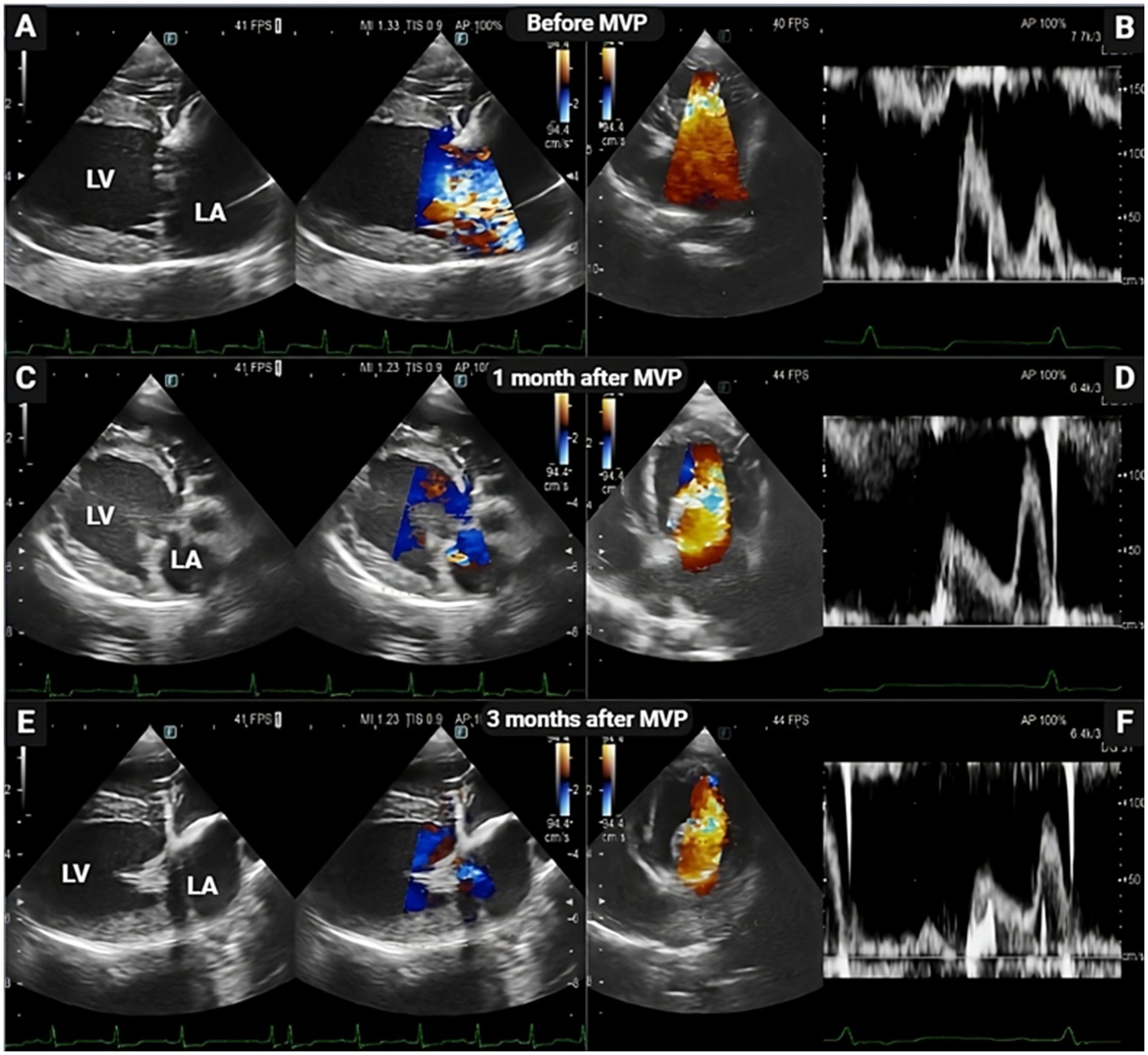
Figure 1. Representative echocardiogram images before, 1 month, and 3 months after mitral valvuloplasty (MVP) in dog patients. Two-dimensional echocardiography at the long-axis LV inflow view demonstrating the thickening of the mitral valve, enlarged left ventricle and left atrium chambers with mitral valve regurgitation (A) and elevated mitral inflow velocity (B) before MVP. Following mitral MVP, there was significant restoration in cardiac functional parameters, characterized by reduced left ventricular and atrium lumen size (C,E) and reduced early mitral inflow velocities (D,F). LA, left atrium; LV, left ventricle.
3.1.2 Two-dimensional speckle tracking echocardiography
Figure 2 depict the longitudinal strains of the left and right ventricles utilizing 2D-STE, while Figure 3 showcases the global circumferential strain (GCS) and global radial strain (GRS) before, at 1 month, and at 3 months post MVP using two-dimensional speckle tracking echocardiography. Similarly, Figure 4 illustrates the LV twist at various time points before and after MVP.
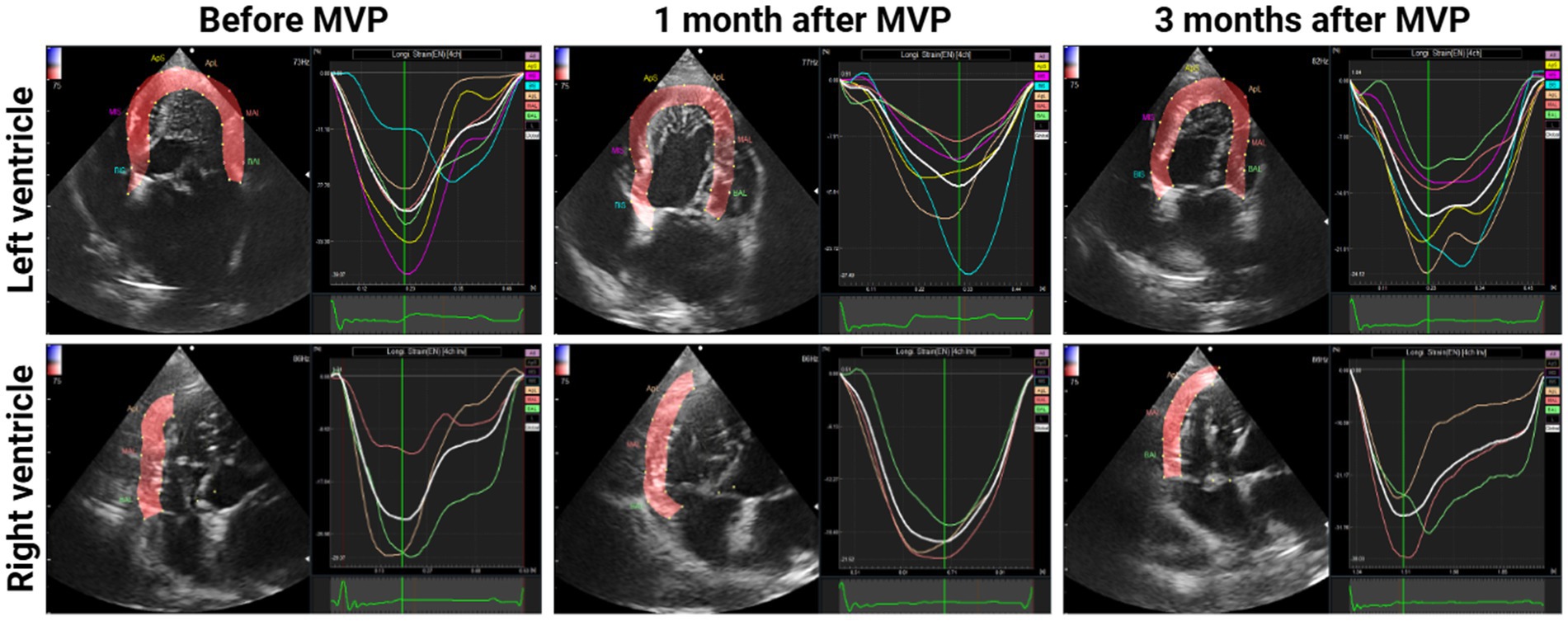
Figure 2. Longitudinal strains of the left and right ventricles before, at 1 month, and at 3 months After MVP using two-dimensional speckle tracking echocardiography. A central line demonstrated the downward peak strain was captured.
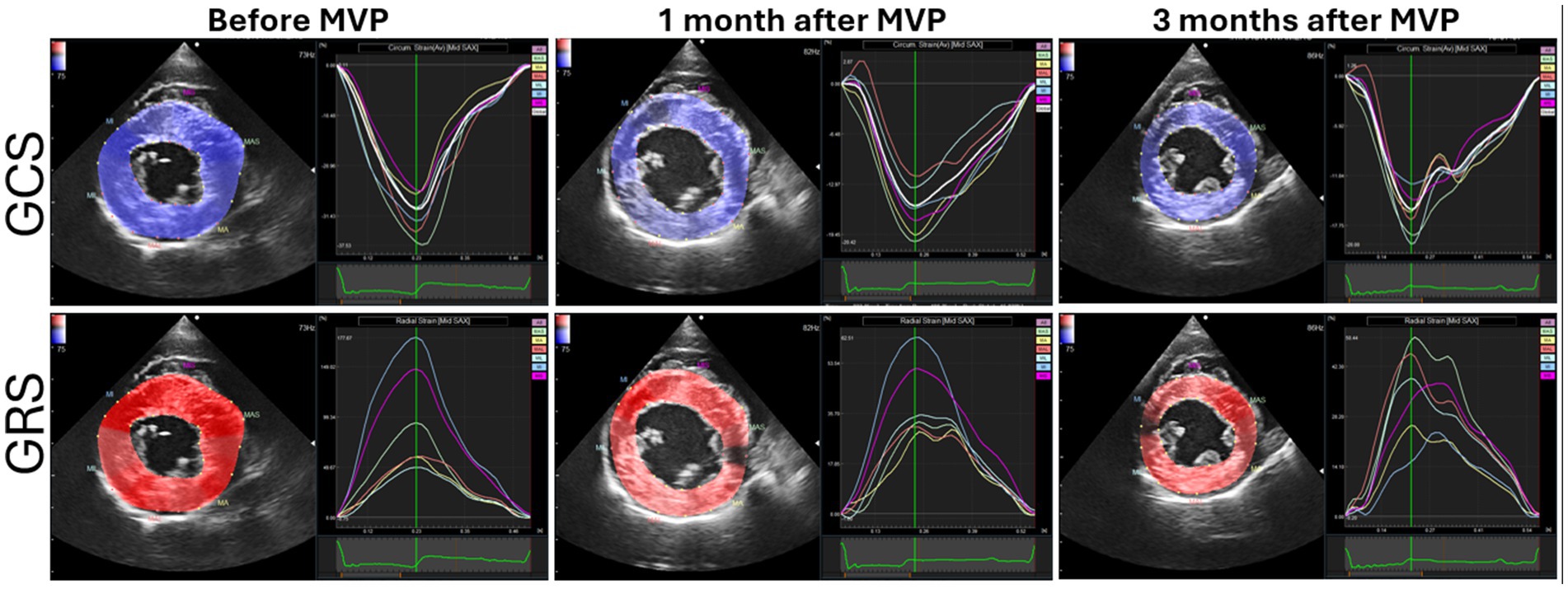
Figure 3. Global circumferential strain (GCS) and global radial strain (GRS) before, at 1 month, and at 3 months after mitral valvuloplasty (MVP) using 2D-STE.
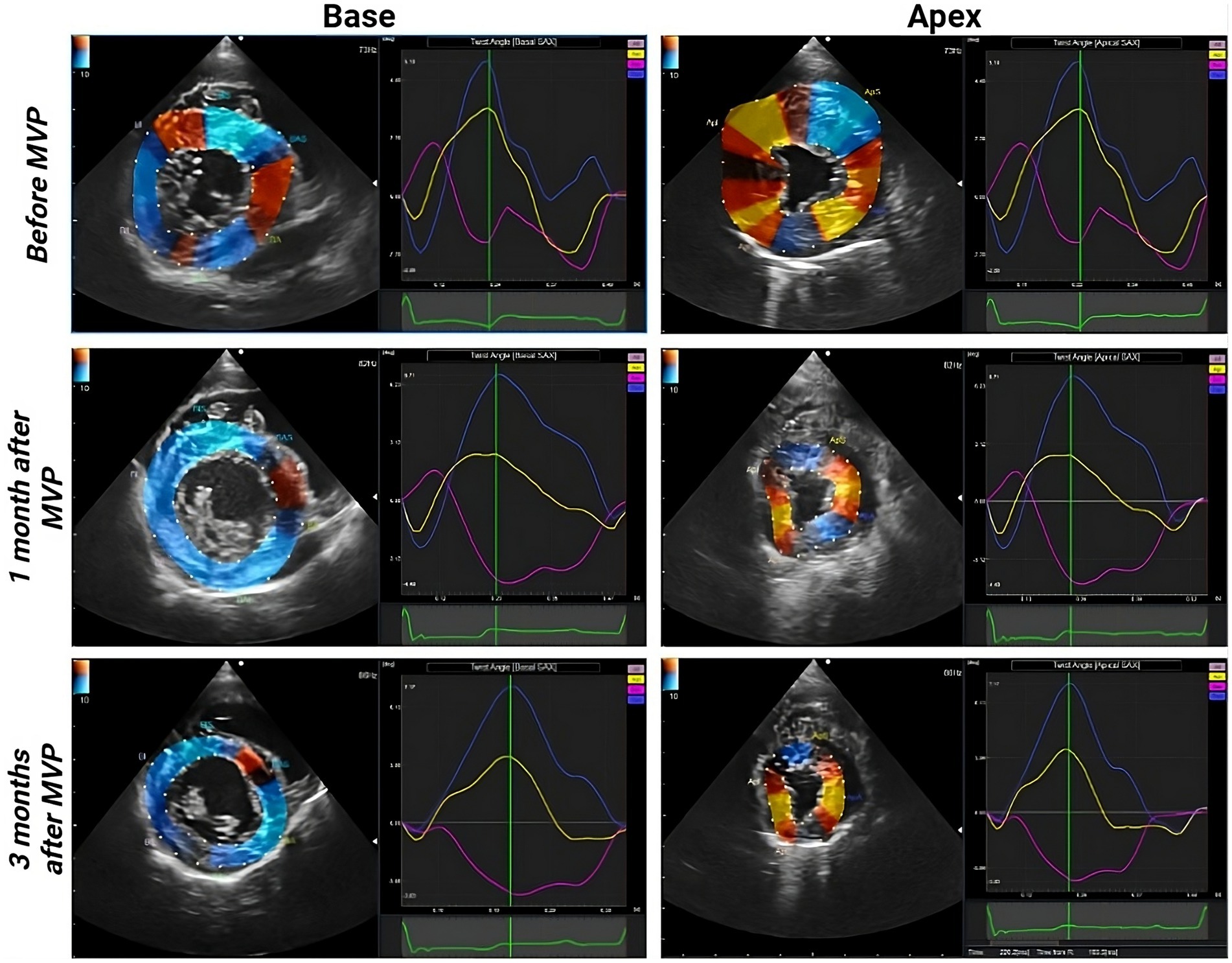
Figure 4. Left ventricular (LV) twist before, at 1 month, and at 3 months after MVP. Blue curve: LV twist, yellow curve: apex rotation, pink curve: base rotation.
LV-GLS, GCS, and GRS exhibited a significant decrease at both 1 month (p = 0.0078, 0.0078, 0.0078, respectively) and 3 months (p = 0.0156, 0.0078, 0.0078, respectively) post-surgery compared to preoperative values. Notably, no significant changes were observed in RVFW-GLS at any time point compared to the preoperative values. The results of the offline workstation analysis for all eight cases are presented in Table 3. Reference values were obtained from past reports (8, 9, 15, 16). In the 3-month postoperative group, peak systolic twist demonstrated a significant increase compared to the preoperative group (p = 0.039) (Figure 5). Peak systolic apical rotation increased at 3 months postoperatively compared to the preoperative values, although statistical significance was not reached (p = 0.1094).
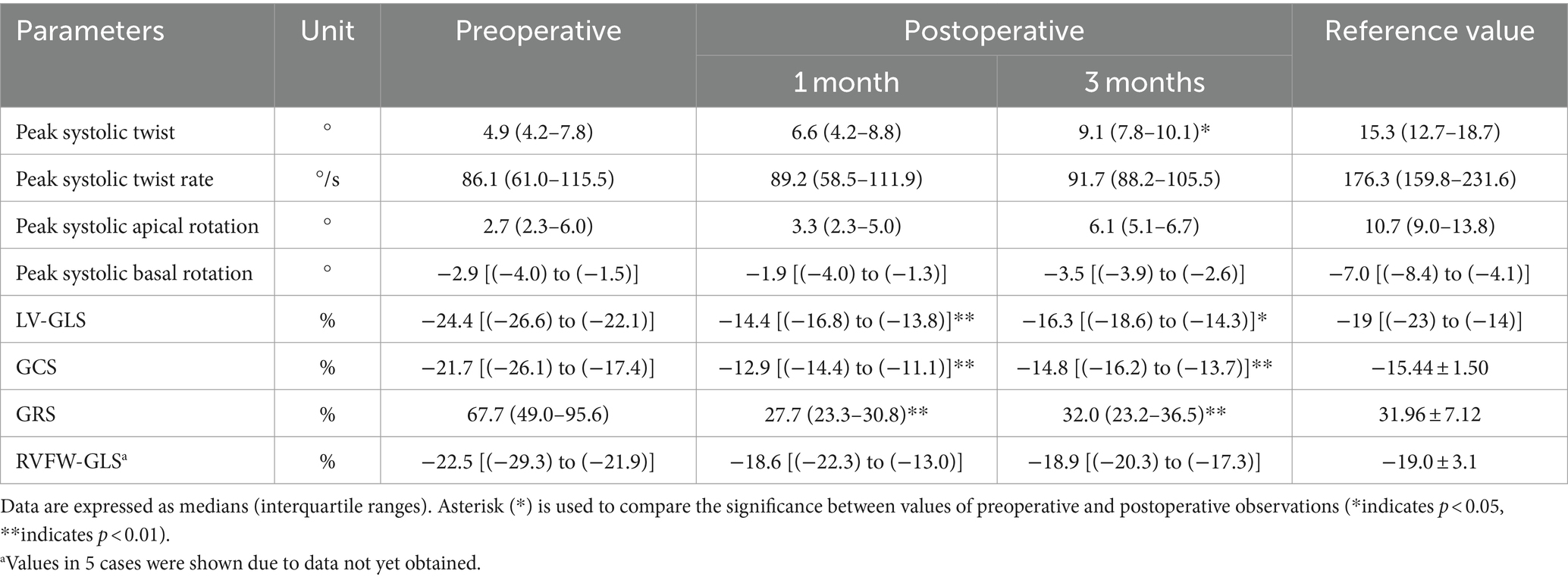
Table 3. Two-dimensional speckle-tracking echocardiography results for 8 dogs preoperatively and at 1 month and 3 months postoperatively.
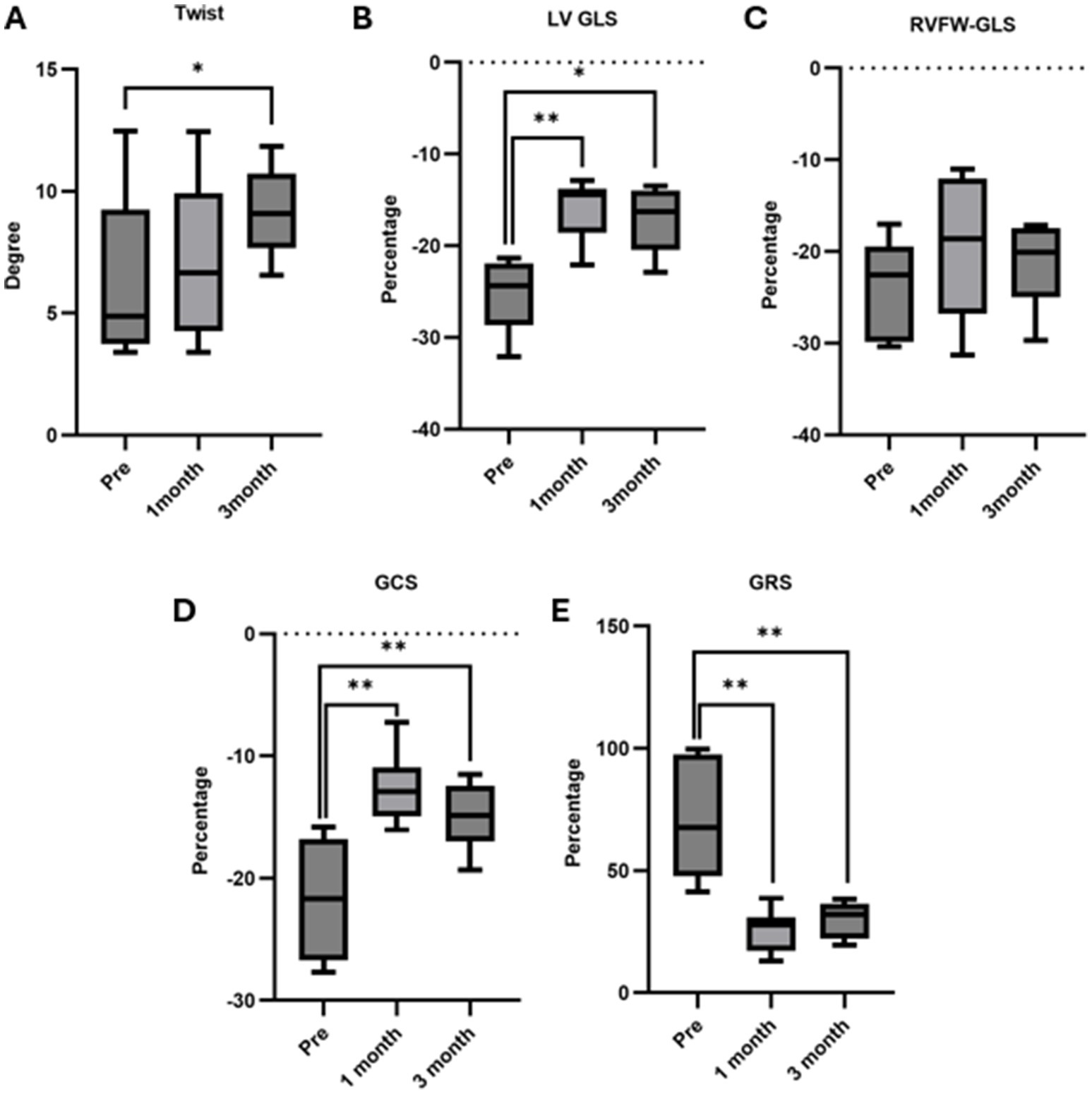
Figure 5. Twist, LV GLS, RVFW GLS Analysis via 2D-STE. (A) Twist: no significant changes were noted between preoperative and 1-month postoperative assessments, but a notable increase was observed at 3 months postoperatively compared to preoperative (p = 0.039). (B) LV-GLS: there was a significant decrease at 1 month (p = 0.0078) and 3 months (p = 0.0156) post-surgery compared to preoperative. (C) RVFW-GLS: no significant changes were observed at 1 month and 3 months post-surgery compared to preoperative. (D) GCS: there was a significant decrease at 1 month (p = 0.0078) and 3 months (p = 0.0078) post-surgery compared to preoperative. (E) GRS: there was a significant decrease at 1 month (p = 0.0078) and 3 months (p = 0.0078) post-surgery compared to preoperative. Data are presented as medians with interquartile ranges. An asterisk (*) indicates significance in the comparison between preoperative and postoperative values (*indicates p < 0.05, **indicates p < 0.01).
The analysis results for cases classified as MMVD Stage D are summarized in Table 4. When comparing preoperative and postoperative 1-month data, no significant differences were observed in any of the measured 2D-STE parameters. Similarly, when comparing preoperative and three-month postoperative values in Stage D, a trend change was noted in peak systolic twist (p = 0.0625), peak systolic apical rotation (p = 0.0625), LV-GLS (p = 0.1250), GCS (p = 0.0625), GRS (p = 0.0625), and RVFW-GLS (p = 0.2500) (Figure 6).
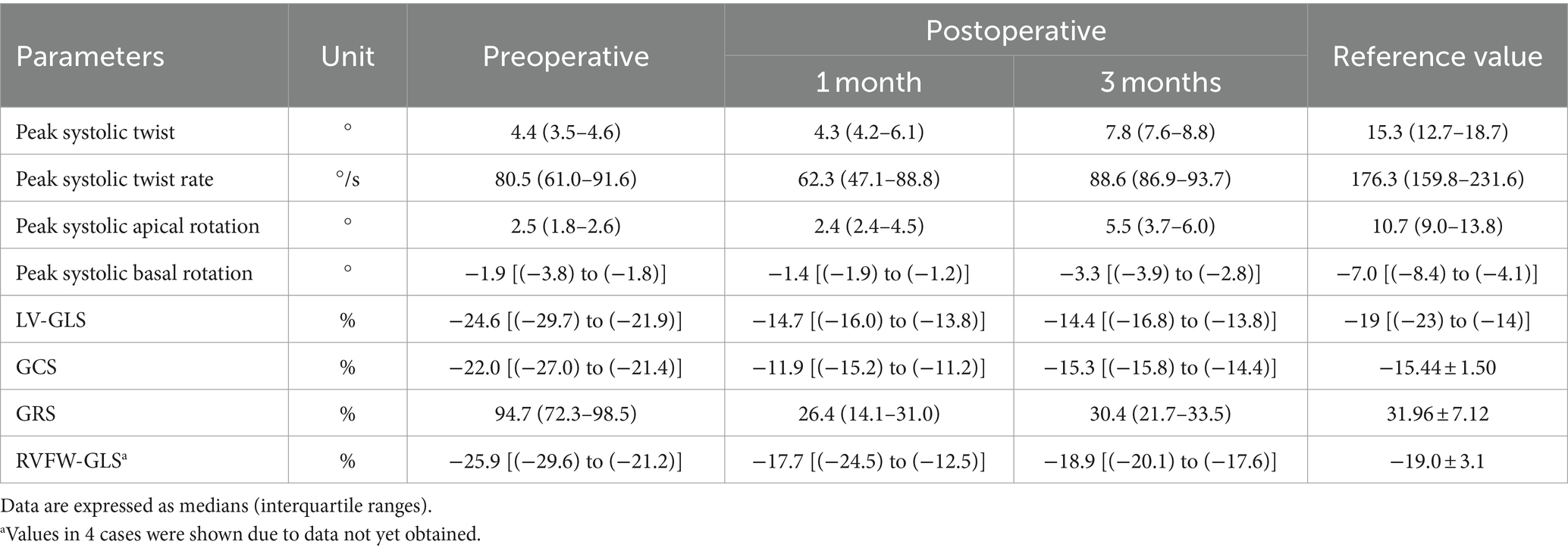
Table 4. Two-dimensional speckle-tracking echocardiography results for 5 dogs (Stage D) preoperatively, 1 month, and 3 months postoperatively.
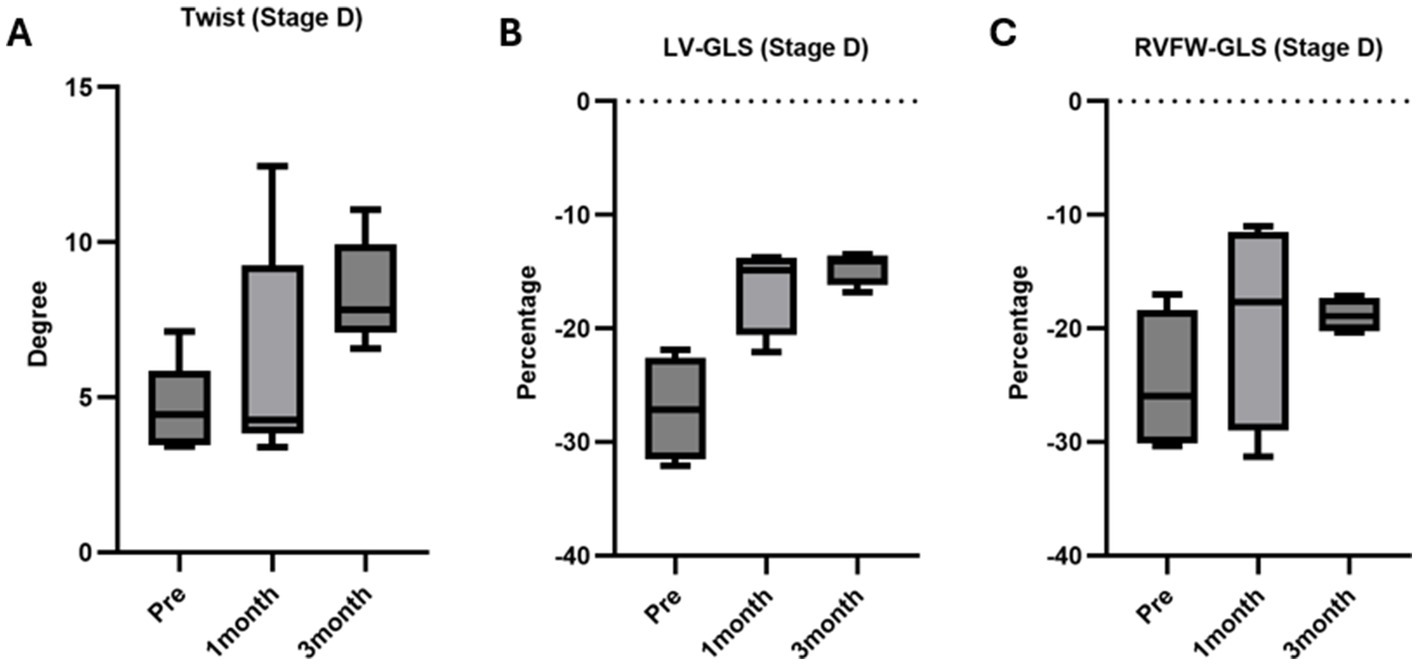
Figure 6. Twist, LV GLS, RVFW GLS analysis via 2D-STE in ACVIM Stage D cases. (A) Twist: no significant differences were noted at 1 month (p = 0.3125) and 3 months (p = 0.0625) post-surgery compared to preoperative values. (B) LV GLS: no significant differences were observed at 1 month (p = 0.1250) and 3 months (p = 0.1250) post-surgery compared to preoperative values. (C) RVFW GLS: no significant differences were observed at 1 month (p = 0.3750) and 3 months (p = 0.2500) post-surgery compared to preoperative values.
3.2 Effect of conventional echocardiographic parameters on twist
The coefficient of determination (R2) obtained from linear regression analysis between indices of contractility (FS), congestion (E velocity), diastolic function (E/e′), left ventricular sphericity index (LVSI), LVIDd, LVIDDN, and twist was illustrated in Figure 7. FS, E velocity, and E/e′ lateral did not exhibit a significant effect on twist. In contrast, LVIDd and LVSI showed a mild significant impact on twist (p = 0.0343, and 0.0190, respectively).

Figure 7. Linear regression analysis between indices of contractility (FS), congestion (E velocity), diastolic function (E/e′), left ventricular sphericity index (LVSI), left ventricular internal diameter in diastole (LVIDd), left ventricular internal diameter in diastole normalized (LVIDDN), and twist, FS, E velocity, and E/e′ lateral did not exhibit a significant regression with twist. In contrast, LVIDd, LVIDDN, and LVSI showed a significant impact on twist.
The collective data showed mild significant effect of LVIDDN on twist (R2 = 0.3380, p = 0.00229). However, the effect of LVIDDN on twist was stronger when considering only the preoperative data (R2 = 0.809, p = 0.0023). Preoperatively, the degree of cardiac twisting was positively affected by the MR velocity (R2 = 0.605, p = 0.023) (Figure 8).
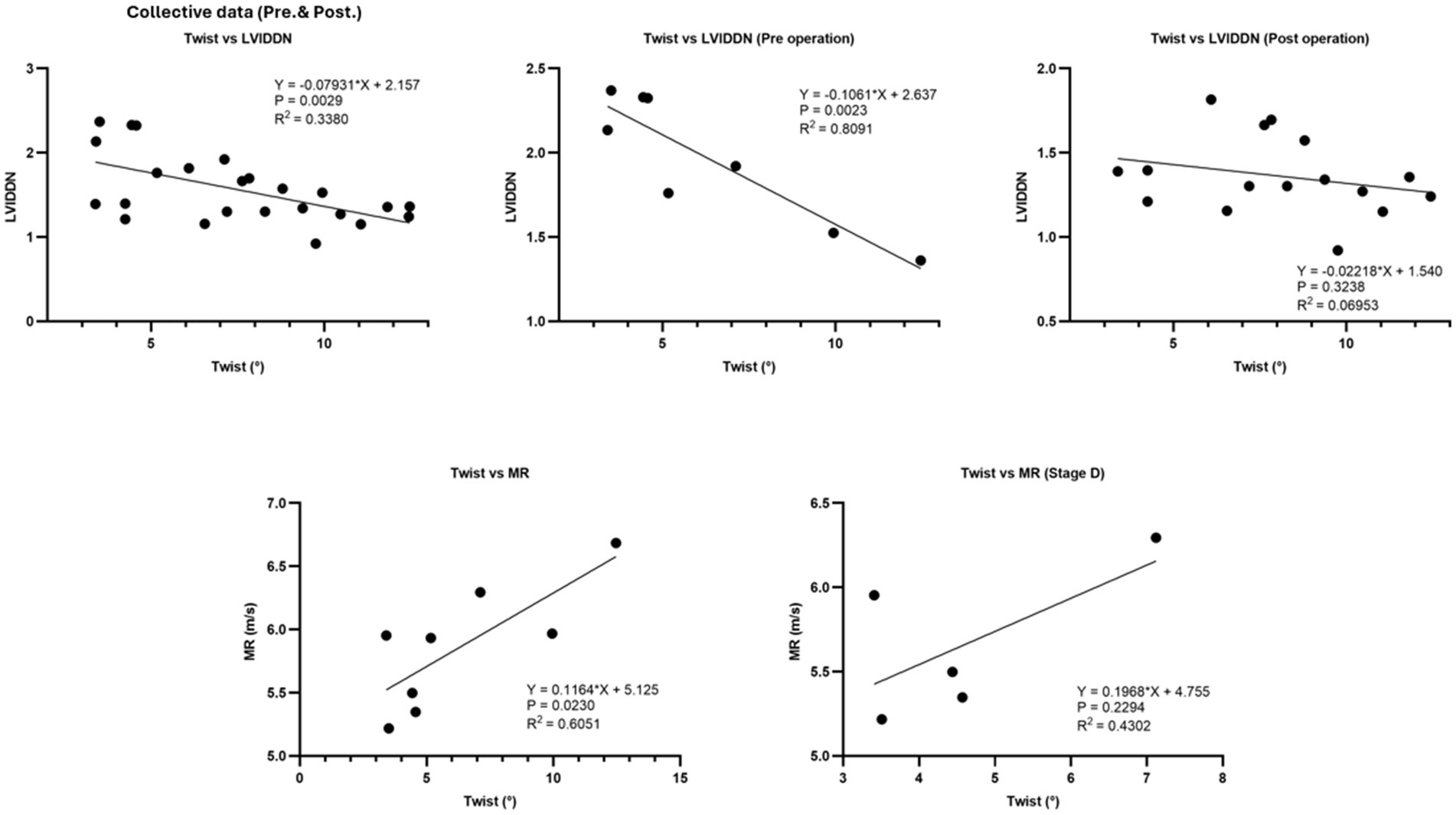
Figure 8. The collective data demonstrated a mild significant effect of LVIDDN on twist. However, the effect of LVIDDN on twist was notably stronger when considering only the preoperative data. Additionally, the degree of cardiac twisting was positively influenced by the regurgitation velocity preoperatively.
3.3 Effect of GCS and GRS on conventional echocardiographic parameters
The coefficient of determination (R2) obtained from linear regression analysis between global circumferential strain (GCS) or global radial strain (GRS) and twist, LVIDd, and LVIDDN was illustrated in Figure 9 twist was not affected by GCS and GRS. However, GRS was significantly and moderately affected by LVIDd (R2 = 0.629, p = 0.0001) and LVIDDN (R2 = 0.637, p = 0.0001). Furthermore, there was negative effect of LVIDd (R2 = 0.409, p = 0.0008) and LVIDDN (R2 = 0.479, p = 0.0002) on circumferential strain.
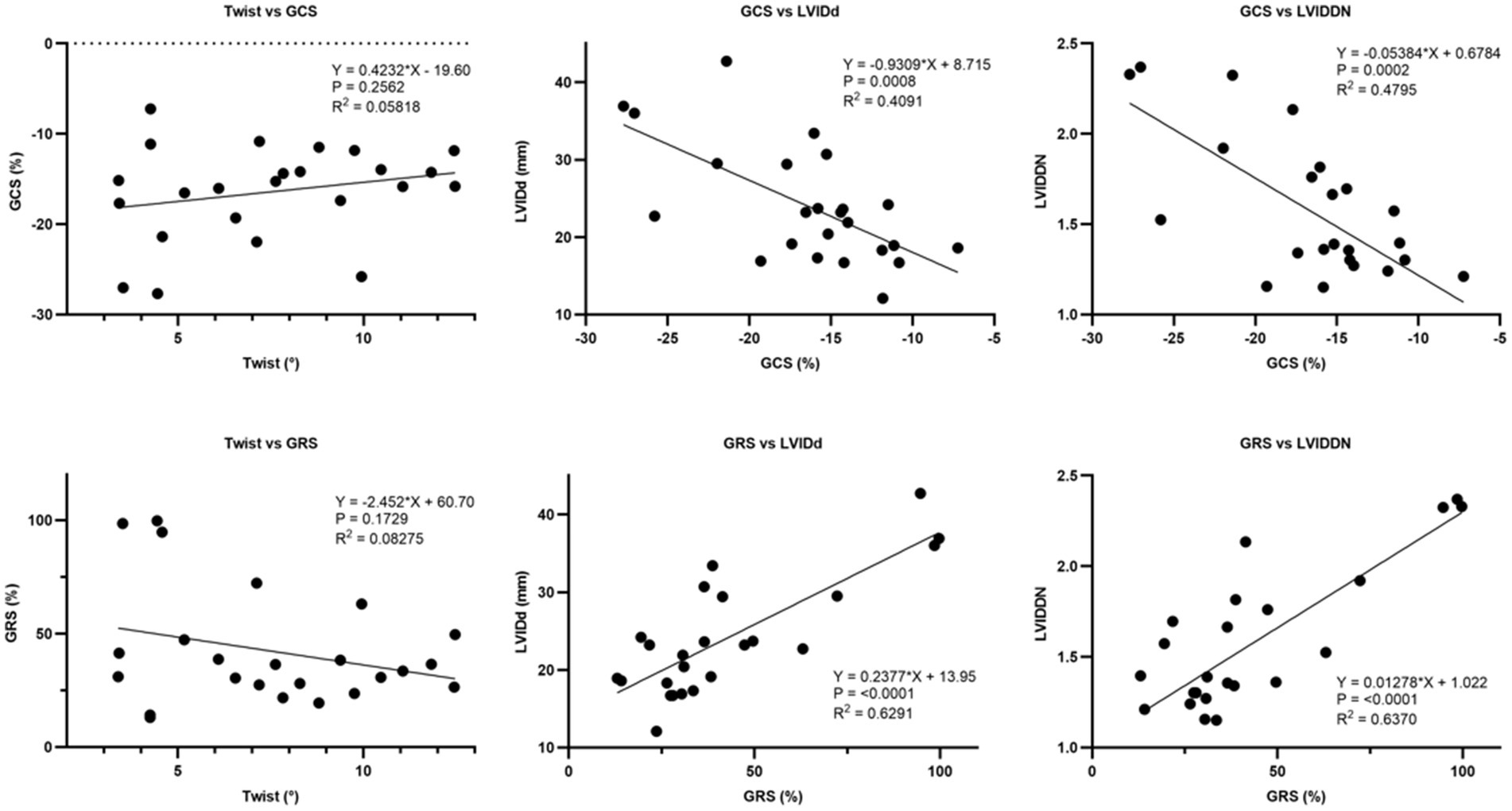
Figure 9. Linear regression analysis between global circumferential strain (GCS) and global radial strain (GRS) and twist, LVIDd, and LVIDDN. There was a significant effect of GCS on LVIDd and LVIDDN. Similarly, GRS exhibited a significant effect on LVIDd and LVIDDN. However, there was no significant effect of GCS or GRS on twist.
3.4 Effect of 2D-STE parameters obtained from LV on RVFW-GLS
The coefficient of determination (R2) obtained from linear regression analysis between twist, LV-GLS, GCS, GRS, and twist was illustrated in Figure 10. RVFW-GLS was not affected by twist, GCS, and GRS. The collective data showed a mild significant effect of LV-GLS on RV-GLS (R2 = 0.3829, p = 0.0139).
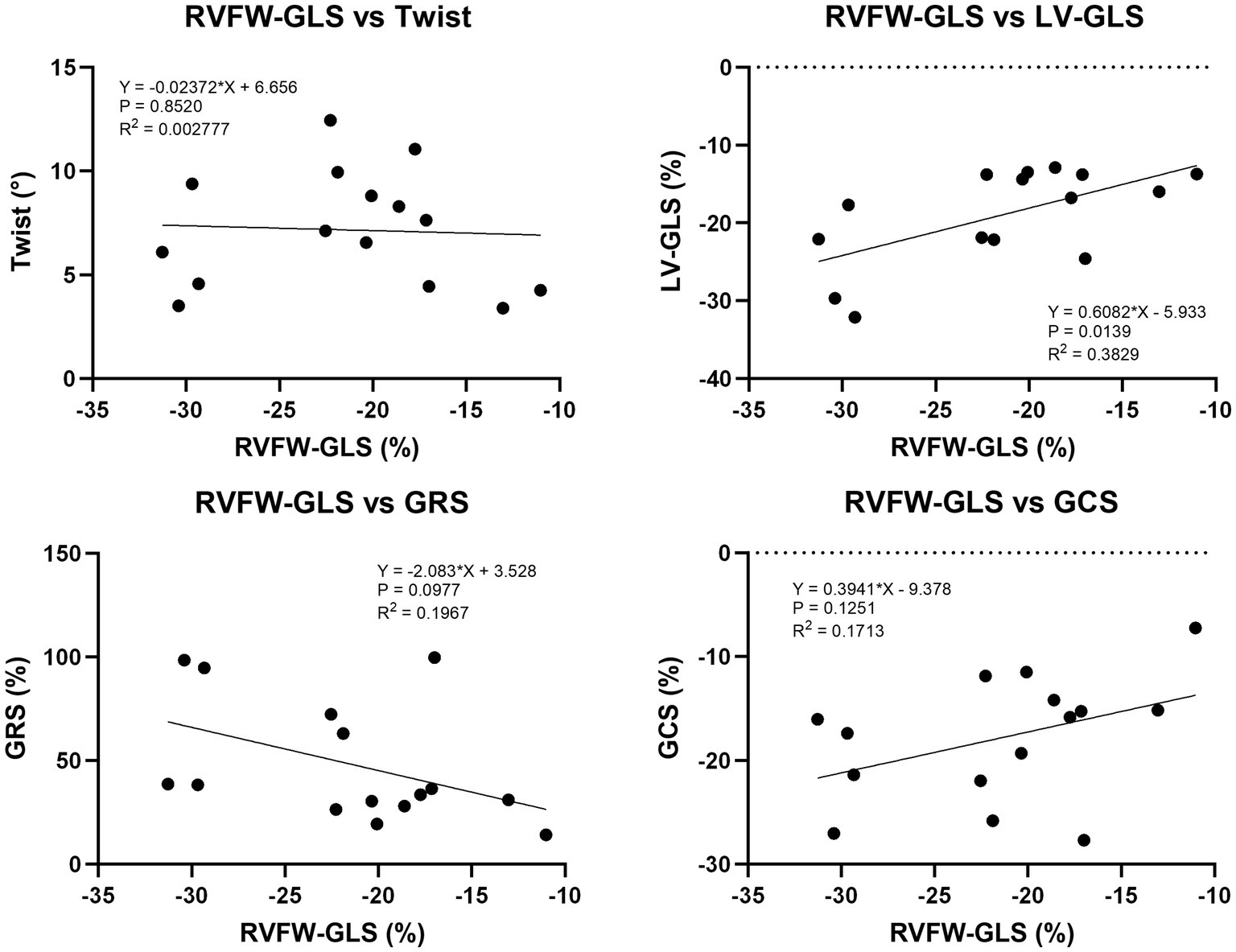
Figure 10. Linear regression analysis between 2D-STE parameters obtained from LV and RVFW-GLS. LV-GLS had a mild significant effect on RVFW-GLS. On the other hand, there was no significant effect of RVFW-GLS on twist, GCS and GRS.
4 Discussion
Through the implementation of MVP, although twist did not reach the standard value, it showed an improvement trend, and GCS and GRS improved to near the standard value. Furthermore, at 3 months after surgery, it was suggested that there was an increase in left ventricular load and subsequent reverse remodeling without the need for inotropic or diuretic drugs. These results underscore MVP’s potential as an independent intervention for managing cardiac conditions, offering promising long-term benefits over medical therapy.
In dogs classified as Class III according to the International Small Animal Cardiac Health Council (ISACHC) classification, previous studies have reported a significant decrease in twist compared to normal dogs and those classified as Class II (9). In our study, preoperative twist in severe cases classified as ACVIM Stage D was notably low. Although not statistically significant in severe cases of ACVIM Stage D, twist exhibited an increasing trend, suggesting that MVP may still offer promise as an effective treatment for severe cases. In contrast, reports in humans with advanced mitral regurgitation indicate less favorable postoperative outcomes linked to a decline in myocardial contractility (17). In our study, all cases showed favorable postoperative progress, possibly attributed to the infrequent occurrence in dogs of conditions where myocardial contractility decreases, as observed in humans with heart failure with reduced ejection fraction (HFrEF) (18). Additionally, the absence of significant improvement in twist at 1 month postoperatively likely indicates that early postoperative myocardial damage or stress, potentially caused by surgical intervention or cardiopulmonary bypass, had not yet fully resolved. Over time, however, as the myocardium healed and recovered from the surgical trauma, twist values began to improve, as seen at the 3-month postoperative check-up. This gradual recovery process is consistent with past findings that it takes time for the heart muscle to recover after heart surgery (19).
Furthermore, reports from human medicine indicate a deterioration in postoperative left ventricular global longitudinal strain (LV-GLS) in patients with isolated primary mitral regurgitation (20), this trend was also observed in our study, as LV-GLS fell below the reference value after surgery. However, it is noteworthy that none of the cases in our study experienced worsened conditions postoperatively due to inadequate cardiac output, suggesting the maintenance of cardiac output through mechanisms beyond longitudinal myocardial motion. This resilience may be attributed to the composition of myocardial fibers in normal canine myocardium, where the ratio of longitudinally oriented fibers to circumferentially arranged fibers is approximately 1:10 (21). Studies have indicated an increase in circumferential strain in dogs classified as Class II in the ISACHC classification compared to normal dogs and those classified as Class I (8). Therefore, movements of myocardial fibers in the circumferential direction, including torsional motion, may play a pivotal role in sustaining effective cardiac output.
Moreover, the presence of cases exhibiting low fractional shortening (FS) but high twist suggests that twist encompasses movements in the short-axis direction as well. Therefore, accurate evaluation of left ventricular function through twist analysis may provide a more comprehensive assessment of the need for postoperative cardiac medication.
In previous studies, right ventricular global longitudinal strain (GLS) has been reported to deteriorate after MVP (20, 22). However, in our study, although there was a decrease in right ventricular GLS post-surgery, these values did not indicate deterioration. This is because, in dogs with MMVD, tricuspid annular plane systolic excursion (TAPSE), which is an indicator of right ventricular contractility, shows a significant positive correlation with the size of the left atrium and left ventricle (23), and TAPSE/Ao, which is expressed as the ratio of TAPSE to aortic diameter, shows a positive correlation with LA/Ao (24), so it has been reported that right ventricular contraction is affected by the left heart system. In other words, it suggests that the excessive contraction of the right ventricle, attributed to the hypercontractile state induced by left ventricular load secondary to MMVD spreading through the interventricular septum, normalized following surgery due to the improvement in left ventricular load. This is consistent with reports that MVP reduces longitudinal contraction in the right ventricle (25, 26). Furthermore, reports in humans indicate a significant decrease in TAPSE and maximum systolic velocity of the tricuspid annulus (PSV) post-surgery, while there was no significant change in right ventricular ejection fraction (27). These findings suggest that vertical motion of the heart in the right ventricle may also be important. Additionally, the weak correlation observed between left ventricular GLS and right ventricular free wall GLS (RVFW-GLS) in our study underscores the influence of interventricular interaction mediated by the interventricular septum. These dynamics may involve short-axis contractions and bellows-like movements in the right ventricle (28), aspects not evaluated in our study.
Increased GCS and GRS in response to progressive left heart load due to MMVD have been documented (8). In this study, preoperative GCS and GRS were observed to be elevated, influenced by LVIDd and LVIDDN, suggesting an association with left ventricular volume overload. This phenomenon may reflect a compensatory mechanism of the myocardium to counter volume overload. Interestingly, postoperative GCS and GRS improved to levels comparable to those reported in healthy dogs (15), indicating that MVP effectively alleviates the burden on the left ventricular system without causing significant myocardial damage, despite the cardiac arrest induced by surgery. Furthermore, twist was not influenced by GCS and GRS, highlighting its distinct role as a mechanism of cardiac output in the left ventricle, separate from circumferential and short-axis myocardial motion. Our data indicates that LV twist is significantly influenced not only LVIDDN and LVIDd, but also by LVSI. Previous studies have reported that twist is influenced by cardiac morphology (29), and our findings suggest that effective reverse remodeling of the left ventricular system following MVP can enhance left ventricular twisting motion, potentially contributing to motion restoration. Additionally, it has been reported that LVSI decreases with the progression of MMVD (30), suggesting that postoperative improvement in preload may alleviate excessively increased wall stresses as the left ventricular morphology returns to normal.
Previous reports in human medicine have shown variability in postoperative twist changes, with some groups experiencing increased left ventricular end-diastolic volume (LVEDV) and others showing a decrease (31). Similarly, it is conceivable that the degree of recovery in dogs may vary by stage as well. This suggests that postoperative outcomes may differ depending on the extent of preoperative myocardial impairment. In our study, some Stage B2 patients did not exhibit significant changes in twist between the preoperative and postoperative periods, suggesting that patients at lower stages may experience a milder decline in left heart function. However, the maintenance or recovery of twist in all patients despite discontinuation of inotropic drugs compared to preoperative levels suggests that MVP may be an effective treatment across all stages.
5 Limitations
One of the limitations of this study is that there were no healthy individuals or Stage B2 cases before or after treatment with pimobendan to use as a control group, so the treatment effect was judged using the reference values from previous reports. The reference values used in this study may not necessarily be appropriate, as they may vary depending on the size and breed of the dog. It is also known that the results can vary depending on the echo device used and the analysis software (32).
For this reason, it may be important to focus on the change in values before and after MVP.
In addition, the small number of cases in each stage means that it may not be possible to draw strong conclusions about the evaluation of cardiac function after surgery based on this study alone. However, it has become statistically clear that the therapeutic effect of MVP manifests in the same way in all cases.
This is thought to be a result that strongly supports the idea that MVP is one of the beneficial treatments, even with a small sample size.
Furthermore, in Stage B2, there were cases where diuretics were used in the absence of heart failure, and it is unclear whether the case was Stage B2 or Stage C.
In addition, as this study is a short-term follow-up survey of up to 3 months after surgery, it is impossible to deny the possibility that the trend of improvement in various parameters will disappear if the patient’s condition is followed over a long period of time.
6 Conclusion
Our study highlights 2D-STE analysis as a valuable tool for assessing the efficacy of MVP in treating MMVD, showing improvements in myocardial function. According to our knowledge, our study presents the first report of postoperative enhancement in twist, GCS, and GRS with a notable trend towards improvement even in severe cases, although statistical significance was not achieved. Moreover, our findings indicate that changes in the ventricular septum influence both cardiac systems. These results collectively underscore the promising potential of MVP in improving cardiac function and warrant further investigation into its clinical applicability and long-term benefits for MMVD patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The requirement of ethical approval was waived by Dolphin Animal Hospital Urawamisono for the studies involving animals because this is a retrospective study that compiles data from cases. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent was obtained from the owners for the participation of their animals in this study.
Author contributions
SF: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Validation, Writing – original draft. AM: Writing – original draft, Writing – review & editing. AF: Writing – original draft, Writing – review & editing. TY: Data curation, Writing – review & editing. AN: Data curation, Investigation, Writing – review & editing. HY: Investigation, Writing – review & editing. YY: Investigation, Writing – review & editing. KM: Project administration, Writing – review & editing, Conceptualization. RT: Supervision, Writing – review & editing, Project administration.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Oyama, MA, Elliott, C, Loughran, KA, Kossar, AP, Castillero, E, Levy, RJ, et al. Comparative pathology of human and canine myxomatous mitral valve degeneration: 5HT and TGF-β mechanisms. Cardiovasc Pathol. (2020) 46:107196. doi: 10.1016/j.carpath.2019.107196
2. Matsuura, K, Yoshida, T, Yamada, S, Aboshi, Y, Yotsuida, H, Yaginuma, Y, et al. The outcome of surgical mitral valve repair with loop-in-loop technique in dogs with different stage myxomatous mitral valve disease. J Vet Cardiol. (2022) 42:74–82. doi: 10.1016/j.jvc.2022.06.001
3. Yoshida, T, Matsuura, K, Chieh-Jen, C, Aboshi, Y, Yamada, S, Yotsuida, H, et al. Surgical treatment for left atrial rupture due to myxomatous mitral valve disease in three dogs: a case report. Vet Med Sci. (2022) 8:2261–7. doi: 10.1002/vms3.915
4. Uechi, M, Mizukoshi, T, Mizuno, T, Mizuno, M, Harada, K, Ebisawa, T, et al. Mitral valve repair under cardiopulmonary bypass in small-breed dogs: 48 cases (2006–2009). J Am Vet Med Assoc. (2012) 240:1194–201. doi: 10.2460/javma.240.10.1194
5. Hamabe, L, Mandour, AS, Shimada, K, Uemura, A, Yilmaz, Z, Nagaoka, K, et al. Role of two-dimensional speckle-tracking echocardiography in early detection of left ventricular dysfunction in dogs. Animals. (2021) 11:2361. doi: 10.3390/ani11082361
6. Reisner, SA, Lysyansky, P, Agmon, Y, Mutlak, D, Lessick, J, and Friedman, Z. Global longitudinal strain: a novel index of left ventricular systolic function. J Am Soc Echocardiogr. (2004) 17:630–3. doi: 10.1016/j.echo.2004.02.011
7. de Boer, JM, Kuipers, IM, Klitsie, LM, Blom, NA, and Ten Harkel, AD. Decreased biventricular longitudinal strain shortly after congenital heart defect surgery. Echocardiography. (2017) 34:446–52. doi: 10.1111/echo.13456
8. Suzuki, R, Matsumoto, H, Teshima, T, and Koyama, H. Clinical assessment of systolic myocardial deformations in dogs with chronic mitral valve insufficiency using two-dimensional speckle-tracking echocardiography. J Vet Cardiol. (2013) 15:41–9. doi: 10.1016/j.jvc.2012.09.001
9. Suzuki, R, Matsumoto, H, Teshima, T, and Koyama, H. Noninvasive clinical assessment of systolic torsional motions by two-dimensional speckle-tracking echocardiography in dogs with myxomatous mitral valve disease. J Vet Intern Med. (2013) 27:69–75. doi: 10.1111/jvim.12024
10. Zois, NE, Olsen, NT, Moesgaard, SG, Rasmussen, CE, Falk, T, Haggstrom, J, et al. Left ventricular twist and circumferential strain in dogs with myxomatous mitral valve disease. J Vet Intern Med. (2013) 27:875–83. doi: 10.1111/jvim.12114
11. Cheng, CJ, Mandour, AS, Yoshida, T, Watari, T, Tanaka, R, and Matsuura, K. Changes in renin-angiotensin-aldosterone system during cardiac remodeling after mitral valvuloplasty in dogs. J Vet Intern Med. (2022) 36:397–405. doi: 10.1111/jvim.16346
13. Gomez-Doblas, JJ, Schor, J, Vignola, P, Weinberg, D, Traad, E, Carrillo, R, et al. Left ventricular geometry and operative mortality in patients undergoing mitral valve replacement. Clin Cardiol. (2001) 24:717–22. doi: 10.1002/clc.4960241106
14. Stendahl, JC, Parajuli, N, Lu, A, Boutagy, NE, Guerrera, N, Alkhalil, I, et al. Regional myocardial strain analysis via 2D speckle tracking echocardiography: validation with sonomicrometry and correlation with regional blood flow in the presence of graded coronary stenoses and dobutamine stress. Cardiovasc Ultrasound. (2020) 18:2. doi: 10.1186/s12947-019-0183-x
15. Hamabe, L, Fukushima, R, Kawamura, K, Shinoda, Y, Huai-Che, H, Suzuki, S, et al. Evaluation of changes in left ventricular myocardial function observed in canine myocardial dysfunction model using a two-dimensional tissue tracking technique. J Vet Sci. (2013) 14:355–62. doi: 10.4142/jvs.2013.14.3.355
16. Morita, T, Nakamura, K, Osuga, T, Yokoyama, N, Khoirun, N, Morishita, K, et al. The repeatability and characteristics of right ventricular longitudinal strain imaging by speckle-tracking echocardiography in healthy dogs. J Vet Cardiol. (2017) 19:351–62. doi: 10.1016/j.jvc.2017.05.001
17. Avierinos, JF, Gersh, BJ, Melton, LJ 3rd, Bailey, KR, Shub, C, Nishimura, RA, et al. Natural history of asymptomatic mitral valve prolapse in the community. Circulation. (2002) 106:1355–61. doi: 10.1161/01.cir.0000028933.34260.09
18. Brener, MI, Uriel, N, and Burkhoff, D. Left ventricular volume reduction and reshaping as a treatment option for heart failure. Struct Heart. (2020) 4:264–83. doi: 10.1080/24748706.2020.1777359
19. Giordano, P, Scrascia, G, D'Agostino, D, Mastro, F, Rotunno, C, Conte, M, et al. Myocardial damage following cardiac surgery: comparison between single-dose celsior cardioplegic solution and cold blood multi-dose cardioplegia. Perfusion. (2013) 28:496–503. doi: 10.1177/0267659113486827
20. Gercek, M, Faber, L, Rudolph, V, Fox, H, Puehler, T, Omran, H, et al. Myocardial adaptation as assessed by speckle tracking echocardiography after isolated mitral valve surgery for primary mitral regurgitation. Int J Cardiovasc Imaging. (2021) 37:913–20. doi: 10.1007/s10554-020-02065-3
21. Streeter, DD Jr, Spotnitz, HM, Patel, DP, Ross, J Jr, and Sonnenblick, EH. Fiber orientation in the canine left ventricle during diastole and systole. Circ Res. (1969) 24:339–47. doi: 10.1161/01.res.24.3.339
22. Keller, M, Heller, T, Lang, T, Patzelt, J, Schreieck, J, Schlensak, C, et al. Acute changes of global and longitudinal right ventricular function: an exploratory analysis in patients undergoing open-chest mitral valve surgery, percutaneous mitral valve repair and off-pump coronary artery bypass grafting. Cardiovasc Ultrasound. (2020) 18:32. doi: 10.1186/s12947-020-00218-x
23. Poser, H, Berlanda, M, Monacolli, M, Contiero, B, Coltro, A, and Guglielmini, C. Tricuspid annular plane systolic excursion in dogs with myxomatous mitral valve disease with and without pulmonary hypertension. J Vet Cardiol. (2017) 19:228–39. doi: 10.1016/j.jvc.2017.03.007
24. Caivano, D, Dickson, D, Pariaut, R, Stillman, M, and Rishniw, M. Tricuspid annular plane systolic excursion-to-aortic ratio provides a bodyweight-independent measure of right ventricular systolic function in dogs. J Vet Cardiol. (2018) 20:79–91. doi: 10.1016/j.jvc.2018.01.005
25. Raina, A, Vaidya, A, Gertz, ZM, Susan, C, and Forfia, PR. Marked changes in right ventricular contractile pattern after cardiothoracic surgery: implications for post-surgical assessment of right ventricular function. J Heart Lung Transplant. (2013) 32:777–83. doi: 10.1016/j.healun.2013.05.004
26. Del Rio, JM, Grecu, L, and Nicoara, A. Right ventricular function in left heart disease. Semin Cardiothorac Vasc Anesth. (2019) 23:88–107. doi: 10.1177/1089253218799345
27. Tamborini, G, Muratori, M, Brusoni, D, Celeste, F, Maffessanti, F, Caiani, EG, et al. Is right ventricular systolic function reduced after cardiac surgery? A two- and three-dimensional echocardiographic study. Eur J Echocardiogr. (2009) 10:630–4. doi: 10.1093/ejechocard/jep015
28. Addetia, K, Maffessanti, F, Muraru, D, Singh, A, Surkova, E, Mor-Avi, V, et al. Morphologic analysis of the normal right ventricle using three-dimensional echocardiography-derived curvature indices. J Am Soc Echocardiogr. (2018) 31:614–23. doi: 10.1016/j.echo.2017.12.009
29. van Dalen, BM, Kauer, F, Vletter, WB, Soliman, OI, van der Zwaan, HB, Ten Cate, FJ, et al. Influence of cardiac shape on left ventricular twist. J Appl Physiol. (2010) 108:146–51. doi: 10.1152/japplphysiol.00419.2009
30. Ljungvall, I, Hoglund, K, Carnabuci, C, Tidholm, A, and Haggstrom, J. Assessment of global and regional left ventricular volume and shape by real-time 3-dimensional echocardiography in dogs with myxomatous mitral valve disease. J Vet Intern Med. (2011) 25:1036–43. doi: 10.1111/j.1939-1676.2011.0774.x
31. Kazui, T, Niinuma, H, Tsuboi, J, and Okabayashi, H. Changes in left ventricular twist after mitral valve repair. J Thorac Cardiovasc Surg. (2011) 141:716–24. doi: 10.1016/j.jtcvs.2010.05.004
Keywords: mitral valve repair, 2D-STE, twist, GLS, GCS, GRS, ventricular interaction
Citation: Fukuzumi S, Mandour AS, Farag A, Yoshida T, Nishiura A, Yotsuida H, Yaginuma Y, Matsuura K and Tanaka R (2024) Speckle tracking echocardiography for evaluation of myocardial functions before and after mitral valvuloplasty in dogs. Front. Vet. Sci. 11:1463889. doi: 10.3389/fvets.2024.1463889
Edited by:
Micaela Sgorbini, University of Pisa, ItalyCopyright © 2024 Fukuzumi, Mandour, Farag, Yoshida, Nishiura, Yotsuida, Yaginuma, Matsuura and Tanaka. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katsuhiro Matsuura, a21hdHN1dXJhQHVmbC5lZHU=; Ryou Tanaka, cnlvQHZldC5uZS5qcA==
 Sho Fukuzumi
Sho Fukuzumi Ahmed S. Mandour
Ahmed S. Mandour Ahmed Farag
Ahmed Farag Tomohiko Yoshida
Tomohiko Yoshida Akitsugu Nishiura5
Akitsugu Nishiura5 Ryou Tanaka
Ryou Tanaka