
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Vet. Sci. , 09 March 2023
Sec. Veterinary Regenerative Medicine
Volume 10 - 2023 | https://doi.org/10.3389/fvets.2023.1117829
This article is part of the Research Topic Rising Stars in Veterinary Regenerative Medicine: 2022 View all 14 articles
In equine medicine, the use of regenerative therapeutics has gained growing attention, but is still a new and complex field with room for improvement. Platelet lysate (PL) can be used as therapeutic agent but is also a promising supplement for the culture of multipotent mesenchymal stromal cells. To enable a targeted use of PL both in clinic and laboratory, it is crucial to learn more details on its effective ingredients. While so far, mainly growth factor components have been analyzed in platelet-based products such as PL, the current study focuses on the content of cytokines in serum, plasma, platelet concentrate and PL. Blood was harvested from 20 clinically healthy horses and subjected to blood count and chemistry analysis, as well as to further processing to PL. Plasma and platelet concentrate were produced by a buffy-coat-based method and PL was produced from the concentrate by freeze-thawing. Samples from each horse were analyzed regarding interleukin (IL)-1β, −4, −6 and −10, interferon-γ and tumor necrosis factor-α concentrations using sandwich ELISAs. Cytokine concentrations in serum, plasma, concentrate and PL were similar and correlated significantly. However, there was a large inter-individual variability in cytokine concentrations between the different donor horses. The samples from some donor animals had overall very high cytokine concentrations, while samples from other donors had no measurable cytokine ingredient. This pattern was observed for all cytokines. There was a noticeable link between high cytokine concentrations in the blood products and abnormal findings in blood chemistry. Cytokine concentrations in samples from horses with abnormal findings were significantly higher than in samples from the remaining horses. The interindividual differences in cytokine concentrations could be highly relevant when using PL for therapy and cell culture, as the mode of action of the PL is likely changed depending on the presence of pro- and anti-inflammatory cytokines. Blood chemistry might be useful to predict cytokine concentrations in blood products.
Platelets play a crucial role in hemostasis and contain various cytokines, chemokines and growth factors, which are released after activation (1). These messenger substances cause a further release of soluble mediators, initiating signaling cascades e.g., for inflammation regulation, angiogenesis or tissue regeneration (2, 3). Besides their biological functions in the body, platelets are being harvested for biomedical purposes, which includes their use in regenerative medicine in the form of platelet concentrate or platelet lysate (PL).
Platelet concentrate is mainly being used for therapeutic purposes (4, 5). However, when further processed to PL by using freeze-thaw cycles to disrupt the platelets (6, 7), their contents are released (6, 8–10), and shelf life and storability of the blood product are improved (11). Therefore, PL can not only be used as a direct therapeutic agent for various indications such as tendon disorders, corneal defects or to support wound healing in horses and humans (12–14), but also as a cell culture supplement (15) which can replace the ethically critical fetal bovine serum (16, 17).
PL as cell culture supplement is particularly useful for the culture of multipotent mesenchymal stromal cells (MSC), which are being explored as therapeutic agent in their own right. MSC culture with addition of PL not only preserves their proliferation and basic properties, such as plastic adherence, expression of specific surface antigens, and trilineage differentiation potential (18), but also has a positive impact on their efficacy. Overall, PL supports the unfolding of diverse biological activities of MSC so that they can exert proregenerative, anti-inflammatory, antifibrotic, and immunomodulatory effects (10). Accordingly, we have previously demonstrated that equine PL, produced by a scalable buffy-coat method, supports equine MSC proliferation and increases their pro-angiogenic potency (19). However, it has not been fully elucidated which PL components contribute to these beneficial effects.
To date, PL has been analyzed predominantly regarding its growth factor contents, while the possible presence of inflammation mediators in platelet-based blood products has been widely disregarded so far. This is surprising, considering the discussion on platelet rich plasma leukocyte contents and considering that the mode of action of other blood products such as conditioned serum relies on (anti-)inflammatory mediators. Knowledge on the cytokine ingredients of platelet-based blood products would be tremendously helpful for their targeted therapeutic use (20, 21). Moreover, the presence of cytokines in PL could play a crucial role for MSC culture, as it could affect their mode of action, for example by inflammatory licensing (22).
To close this gap of knowledge, in this study, we aimed to characterize and quantify different cytokines in equine PL. We show that the cytokine levels vary heavily between individual horses and that abnormal findings in blood chemistry might be indicative of high cytokine levels.
Blood was collected from 20 horses (4–15 years; 14 mares, 5 geldings, 1 stallion) as approved by the responsible authority (regional council Giessen, A14/2019). Beforehand, the donor health status was evaluated by general clinical examination and only animals that were free of abnormal clinical findings were included. In addition to the whole blood intended for platelet lysate production, blood was drawn into EDTA and lithium heparin as well as serum blood collection tubes and analyzed in the laboratory. This included complete blood counts and blood chemistry analysis using an ADVIA 2120i with Multispecies software MS 5.9 (Siemens Healthcare GmbH, Erlangen, Germany). With the latter, electrolytes, urea, creatinine, total protein, albumin, globulins, bilirubin, alkaline phosphatase, glutamate dehydrogenase, γ-glutamyltransferase, aspartate aminotransferase, creatine kinase and lactate dehydrogenase were measured.
Whole blood was collected and processed to produce PL as described in detail previously (6). Briefly, using a buffy-coat based approach, platelet concentrate was produced from whole blood collected in CPD-loaded blood collection bags by centrifugation and blood separation steps. The PL was then produced from this concentrate by freeze-thaw cycles, centrifugation and filtration. Samples from plasma, platelet concentrate and PL were frozen and stored at −80°C for cytokine analyses. Additionally, serum samples were handled accordingly.
Cytokine concentrations were analyzed in serum, plasma, platelet concentrate and PL from each horse using Equine DuoSet ELISA kits (R&D Systems, Minneapolis, MN, USA) for IFN-γ, TNF-α, IL-1β, IL-4, IL-6 and IL-10. The plates were read in an Infinite F50 plate reader and raw data were processed with the corresponding Magellan software (Tecan Ltd., Maennedorf, Switzerland).
First, different serum dilutions were tested for all horses in order to establish the experimental setup. The results showed considerable inter-individual differences in cytokine concentrations demonstrating the need to adjust the dilution factor for each donor. To estimate the possible influence of serum matrix effects in different serum dilutions, spiking experiments were performed. For this purpose, serum from horses with no detectable cytokine content was pooled and a dilution series (1:1, 1:10, 1:100, 1:1,000 in RD buffer) was prepared. These diluted serum samples were then spiked with cytokine standard, corresponding to the second highest concentration of the assay standard curve for each respective cytokine. The spiked samples were subjected to the remaining assay procedure according to the manufacturer's instructions.
The cytokine measurements in all blood products were performed for all cytokines using the ELISA assays according to the manufacturer's instructions. Blood product dilutions were adjusted individually, aiming to use the highest dilutions yielding results within the standard curve ranges in each case. Nevertheless, some samples had to be measured with no or low dilution. Samples with no detectable cytokine content in undiluted samples were assigned the value 0 for graphical presentation. The overall study design is shown in Figure 1.
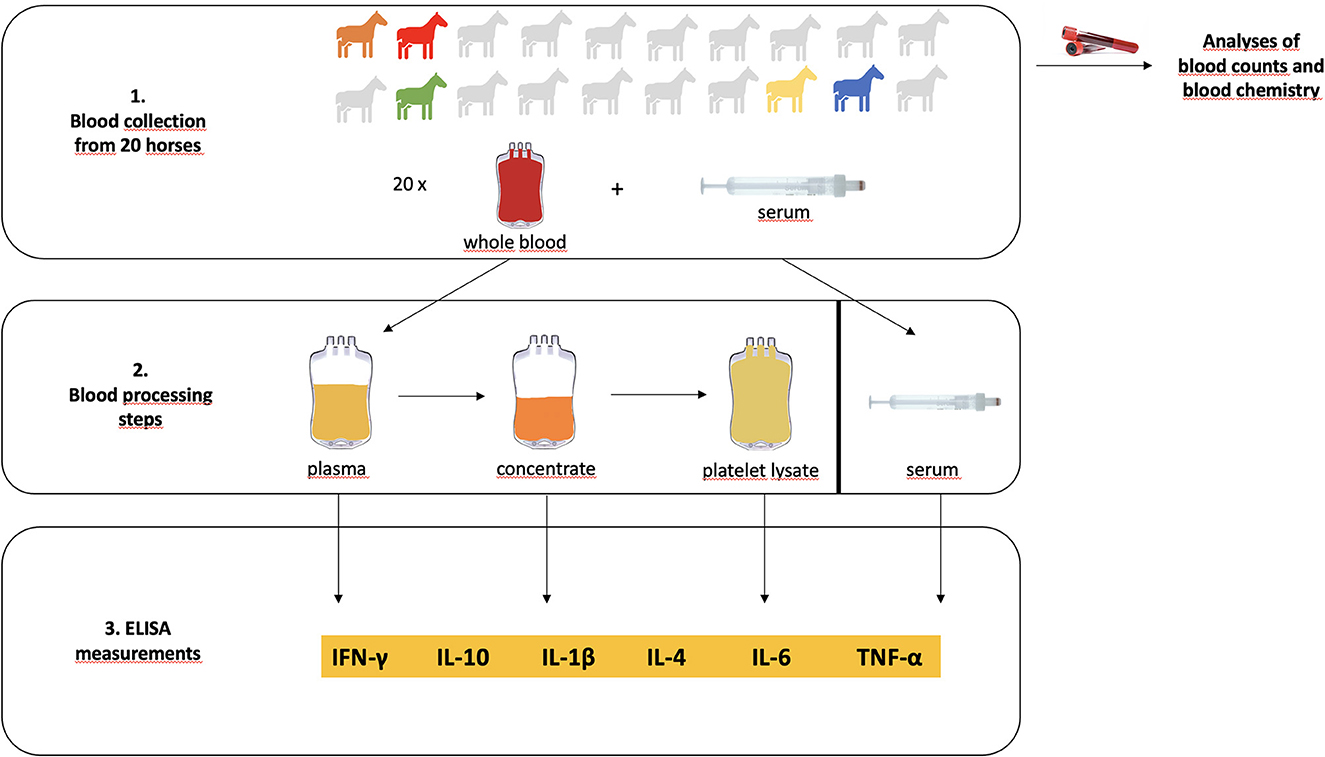
Figure 1. Overview of the study design. Blood was collected from 20 clinically healthy horses, of which 5 turned out to have mildly to moderately abnormal findings in blood chemistry (designated by the colored icons). Whole blood was processed to platelet lysate. Serum, plasma, concentrate and platelet lysate were then subjected to ELISA measurements of their cytokine contents.
Statistical analyses and graphical presentation of data were performed using IBM SPSS Statistics 26. Based on the results of the spiking experiment, we considered that the cytokine concentrations measured in blood product samples with low to medium cytokine content might be underestimated to some extent, as these samples could not be diluted enough to overcome the anticipated matrix effects. Therefore, for the statistical comparisons, cytokine concentrations were transformed into categories to circumvent calculations with inaccurate values. Category 1 corresponds to no detectable cytokine content, category 2 corresponds to the clusters with low to medium cytokine content, and category 3 reflects the clusters with high cytokine content. Non-parametric tests for paired samples were run to compare the different blood products, and non-parametric tests for unpaired samples were run to compare the donors with physiological blood chemistry and those with abnormal blood chemistry findings. In addition, possible correlations were evaluated according to Spearman.
With respect to the general clinical findings, all horses were considered as healthy. Measurements of blood cells were within the reference range, except for very mild changes in two animals (18 and 19). Blood chemistry measurements were within the reference range in 11 horses, showed very mild changes in four horses (4, 5, 13 and 17) and mild to moderate elevations of either alkaline phosphatase, creatinine, lactate dehydrogenase in five horses (horses 1 and 18, horse 2, horses 12 and 19, respectively) (Table 1). The latter were considered as abnormal in the further analyses.
Putative matrix effects were observed for IFN-γ, TNFα, IL-4, IL-6 and, to a lesser extent, IL-10. For IL-1β, matrix effects appeared to be only marginal. In IFN-γ, TNF-α-, IL-4- and IL-6-spiked serum, the measured absorbance was reduced to <50% of the absorbance of the corresponding spiked reagent diluent assay buffer sample. In IL-10-spiked serum, the absorption was reduced to approximately 65%. Diluting the serum decreased this effect, but it was still evident in serum diluted 1:10 (Supplementary Figure 1).
The concentrations of cytokines in the blood products were highly variable between individual horses. For each cytokine, there were a number of blood donors with no measurable concentration (category 1), donors with medium concentrations (category 2), as well as donors with very high concentrations (category 3). Yet interestingly, the number of donors with no detectable cytokine content was reduced during blood processing to PL, suggesting some cytokine release during freeze-thawing of the concentrates in these samples (Figure 2). Nevertheless, considering all donors, cytokine concentrations remained similar between the different blood products, with no significant differences in concentration categories in the post-hoc tests. Instead, the cytokine concentration categories correlated between the different blood products. These correlations were very strong between serum, plasma and concentrate, and more moderate when these were compared with PL (Table 2).
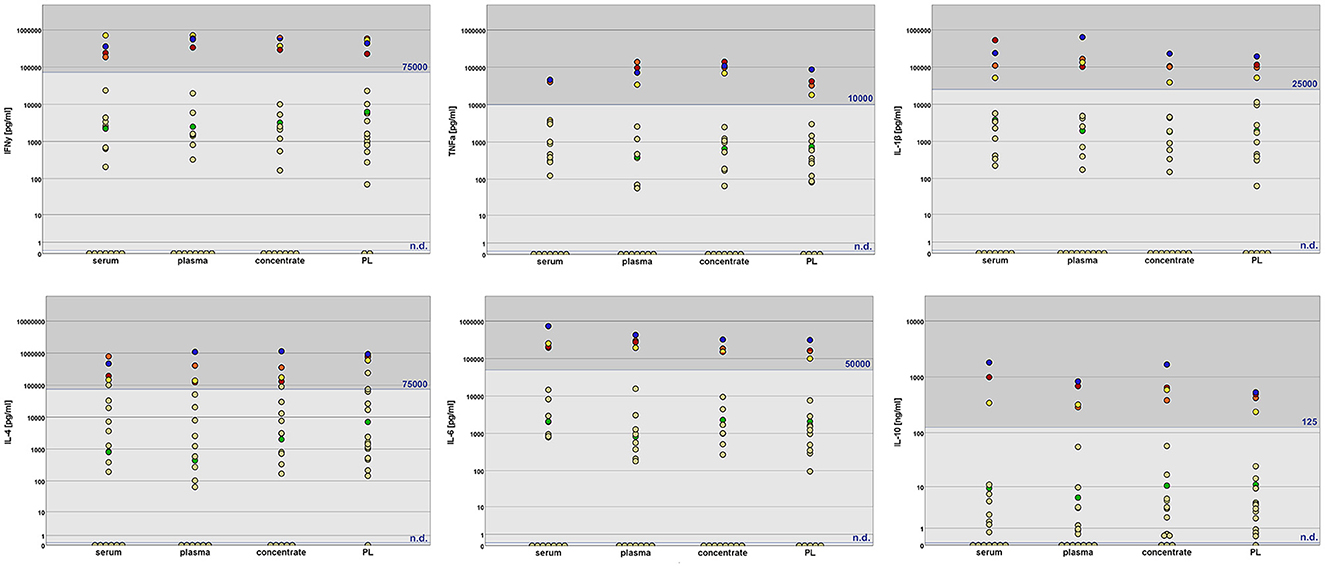
Figure 2. Cytokine concentrations in equine serum, plasma, platelet concentrate and platelet lysate (PL) as measured by sandwich ELISA. The assigned concentration categories are indicated by dark gray (category 3), gray (category 2) and light gray (category 1) background. The thresholds between category 2 and 3 are given in blue letters; category 1 corresponds to no detectable cytokine content (n.d.). Data from donors with abnormal findings in blood chemistry are highlighted in different colors (horse 1: orange; horse 2: red; horse 12: green; horse 18: yellow; horse 19: blue). The cytokine concentration categories were significantly higher in these animals as compared to the others (p < 0.01, except for IL-4 in PL).
Furthermore, the concentration categories of the different cytokines compared with each other correlated significantly, revealing that specific donors had either low, medium or high overall cytokine levels, widely irrespective of the type of cytokine. Again, these correlations were very strong in serum, plasma and concentrate, but more moderate in PL (Table 3).
To find reasons and predictors for the high inter-individual variability in the blood product cytokine concentrations, we searched for links between cytokine contents and health status. Clearly higher cytokine concentrations (category 3 for most cytokines) had been detected in horses 1, 2, 18 and 19 as compared to the other horses. Interestingly, these were 4 out of the 5 horses that had shown elevated readings in the blood chemistry parameters, namely alkaline phosphatase, creatinine and lactate dehydrogenase (Table 1). The remaining horse (horse 12) with an abnormal blood chemistry finding, however, had middle range cytokine concentrations in its blood products (category 2). Nevertheless, cytokine concentration categories were significantly higher in the donor group with abnormal blood work results than in the donor group with physiological blood work results (p < 0.01 for all cytokines and blood products analyzed, except for IL-4 in PL).
The primary aim of this study was to gain insight into the cytokine content of PL and related blood products. Anticipating the high inter-individual differences, we also aimed to identify putative predictors for cytokine content.
The high inter-individual differences in cytokine concentrations between the horses were the most conspicuous finding of the current study, which illustrated that it will be difficult to establish robust reference ranges for serum analysis or quality control thresholds for platelet concentrate and PL products. For serum, such variations are described in the literature, especially regarding IFN-γ concentrations due to vaccination or viral antigen exposure (24). In the current study, however, at the time of blood sampling, none of the horses had received any vaccinations or other medications in the last 2 weeks, and all had received standard vaccinations over the past years.
This study demonstrated that there is a relationship between high cytokine concentrations in blood products, including PL, and increased values in blood chemistry parameters (lactate dehydrogenase, alkaline phosphatase and creatinine). In accordance with this, previous studies showed that there are correlations for the cytokines IFN-γ and TNF-α with the levels of alkaline phosphatase and lactate dehydrogenase (25–27). Probably, the increase in cytokine concentration can be explained by inflammatory processes in the organs such as liver, kidney, muscle or bone, for which these enzymes are considered as indicators.
Cytokines serve as messengers in the regulation of immune response and inflammation. Traditionally, they are divided into pro- (IFN-γ, IL-1β, IL-6 and TNF-α) and anti-inflammatory cytokines (IL-4 and−10), which interact with each other (28, 29). Cytokines are mainly produced by TH1 and TH2 lymphocytes, natural killer as well as mast cells and macrophages, as a result of stimulation by antigens or signaling molecules (24). Due to their contribution to pathological processes, they are being explored as biomarkers for various diseases (30). The exact relationship of cytokine levels and blood chemistry changes in horses will need to be further explored. However, the findings of this study suggest the possibility that blood chemistry measurement might be a convenient tool to estimate the level of cytokines in donor blood and thus facilitate the targeted use of PL.
So far, there are two different operational areas for PL. One is the direct local therapeutic application, e.g., for treatment of osteoarthritis in humans (31, 32) and horses (33), for tendon lesions in humans (34), to promote healing of corneal ulcers (35–37) or for wound healing (38, 39). All beforementioned publications describe an improved outcome compared to control populations. The decisive factors for clinical efficacy are presumably the growth factors contained in the PL, as well as anti-inflammatory cytokines, which can locally influence the inflammatory process (40). On the other hand, PL is already successfully used as a medium additive for cell culture of MSC, which can promote the cellular potency (6, 19, 41, 42). While this has been largely attributed to the growth factors contained in the PL, e.g., VEGF (19), other mediators should be considered as well. As already described by Barrachina et al. (43), stimulation with IFN-y or TNF-α in culture improves the immunomodulatory potency of MSC. Therefore, local application of primed MSC can be expected to yield better therapeutic results. The appropriate amount of pro-inflammatory cytokines is important, because an excess of them impairs the differentiation potential and proliferative capacity of MSC (44). At this point, cytokines contained in the PL may also play a crucial role. With specific levels of pro-inflammatory cytokines, PL alone could possibly serve as a medium additive for priming.
In this study, cytokine levels were measured by sandwich ELISA in different blood products, such as serum, plasma, concentrate and PL. It became apparent that this method has its shortcomings regarding the exact quantification of low cytokine concentrations, as matrix effects occurred in samples measured at low dilutions. We aimed to overcome this on the one hand by repeated measurements at different dilutions and using the highest possible dilution for further analysis, and on the other hand by grouping the cytokine concentrations into categories, the latter to circumvent statistical analysis with inaccurate numbers. Transforming the continuous results data into ordinal data, however, limited the opportunities of inductive statistical analysis. To account for possible confounding variables and interactions of different factors, a generalized linear mixed model would have been more suitable than the analysis approach presented. However, only a multinomial model considering sample type and health status was applicable based on the given data set. This model confirmed that there was no interaction between sample type and health status, but it strongly misestimated the probabilities for the different cytokine categories in different groups, due to their uneven distribution between groups and the relatively small sample sizes per group. Therefore, although this model overall revealed the same trends, namely a significant influence of the health status but no major influence of the sample type on cytokine concentrations, we choose to present a data analysis based on basic group comparisons. While the shortcomings of the ELISA assay and the resulting statistical simplification represent limitations of the current study, it is important to note that the measurements of high cytokine concentrations can still be considered as reliable, as these could be performed with high dilution factors, preventing matrix effects.
In conclusion, this study illustrates that blood products, including PL, are subject to wide variations in cytokine content, which makes careful consideration regarding their use important. It is possible that blood chemistry parameters may provide clues to cytokine content in blood products in individual horses. If this can be confirmed and specified in future research, it would provide a prerequisite to targeted use of PL in clinic and laboratory.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The animal study was reviewed and approved by Regierungspräsidium Gießen. Written informed consent was obtained from the owners for the participation of their animals in this study.
JM: conception of the study and complete experimental design (together with JB), blood collection, sample and data analysis, data interpretation, and drafting of the manuscript. AH: substantial contribution to the experimental design, blood collection, and processing and analysis. SN: substantial contribution to the experimental design and data interpretation. KB: data analysis and interpretation (together with JB and JM). JB: conception of the study and complete experimental design (together with JM), data interpretation, and drafting of the manuscript (together with JM). All authors have critically revised the manuscript for important intellectual content and approved the publication of its content.
This work received partial funding by a scholarship (AH) from the Animal Health Academy [Akademie fuer Tiergesundheit (AfT)].
The authors thank Dr. Hendrik Lehmann, formerly Justus-Liebig-University, Department of Veterinary Clinical Sciences, Small Animal Clinic, and Prof. Dr. Natali Bauer, Justus-Liebig-University, Department of Veterinary Clinical Sciences, Small Animal Clinic, for their intellectual contribution to blood processing, and their support with blood work. The authors further acknowledge all members of the research group for their help and input.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2023.1117829/full#supplementary-material
1. Golebiewska EM, Poole AW. Platelet secretion: from haemostasis to wound healing and beyond. Blood Rev. (2015) 29:153–62. doi: 10.1016/j.blre.2014.10.003
2. Scully D, Naseem KM, Matsakas A. Platelet biology in regenerative medicine of skeletal muscle. Acta Physiol. (2018) 223:e13071. doi: 10.1111/apha.13071
3. Jiang P, Zhang Y, Ru B, Yang Y, Vu T, Paul R, et al. Systematic investigation of cytokine signaling activity at the tissue and single-cell levels. Nat Methods. (2021) 18:1181–91. doi: 10.1038/s41592-021-01274-5
4. Burnouf T, Goubran HA, Chen TM, Ou KL, El-Ekiaby M, Radosevic M. Blood-derived biomaterials and platelet growth factors in regenerative medicine. Blood Rev. (2013) 27:77–89. doi: 10.1016/j.blre.2013.02.001
5. Santos S, Sigurjonsson ÓE, Custódio CA, Mano J. Blood plasma derivatives for tissue engineering and regenerative medicine therapies. Tissue Eng Part B Rev. (2018) 24:454–62. doi: 10.1089/ten.teb.2018.0008
6. Hagen A, Lehmann H, Aurich S, Bauer N, Melzer M, Moellerberndt J, et al. Scalable production of equine platelet lysate for multipotent mesenchymal stromal cell culture. Front Bioeng Biotechnol. (2021) 8:613621. doi: 10.3389/fbioe.2020.613621
7. Strandberg G, Sellberg F, Sommar P, Ronaghi M, Lubenow N, Knutson F, et al. Standardizing the freeze-thaw preparation of growth factors from platelet lysate. Transfusion. (2017) 57:1058–65. doi: 10.1111/trf.13998
8. Altaie A, Owston H, Jones E. Use of platelet lysate for bone regeneration - are we ready for clinical translation? World J Stem Cells. (2016) 8:47–55. doi: 10.4252/wjsc.v8.i2.47
9. Burnouf T, Strunk D, Koh MB, Schallmoser K. Human platelet lysate: replacing fetal bovine serum as a gold standard for human cell propagation? Biomaterials. (2016) 76:371–87. doi: 10.1016/j.biomaterials.2015.10.065
10. Bieback K. Platelet lysate as replacement for fetal bovine serum in mesenchymal stromal cell cultures. Transfus Med Hemother. (2013) 40:326–35. doi: 10.1159/000354061
11. Fekete N, Gadelorge M, Furst D, Maurer C, Dausend J, Fleury-Cappellesso S, et al. Platelet lysate from whole blood-derived pooled platelet concentrates and apheresis-derived platelet concentrates for the isolation and expansion of human bone marrow mesenchymal stromal cells: production process, content and identification of active components. Cytotherapy. (2012) 14:540–54. doi: 10.3109/14653249.2012.655420
12. Zamani M, Yaghoubi Y, Movassaghpour A, Shakouri K, Mehdizadeh A, Pishgahi A, et al. Novel therapeutic approaches in utilizing platelet lysate in regenerative medicine: Are we ready for clinical use? J Cell Physiol. (2019) 234:17172–86. doi: 10.1002/jcp.28496
13. Abu-Ameerh MA, Jafar HD, Hasan MH, Al Bdour MD, Msallam M, Ababneh OH, et al. Platelet lysate promotes re-epithelialization of persistent epithelial defects: a pilot study. Int Ophthalmol. (2019) 39:1483–90. doi: 10.1007/s10792-018-0968-1
14. Textor JA, Clark KC, Walker NJ, Aristizobal FA, Kol A, LeJeune SS, et al. Allogeneic stem cells alter gene expression and improve healing of distal limb wounds in horses. Stem Cells Transl Med. (2018) 7:98–108. doi: 10.1002/sctm.17-0071
15. Sovkova V, Vocetkova K, Rampichova M, Mickova A, Buzgo M, Lukasova V, et al. Platelet lysate as a serum replacement for skin cell culture on biomimetic PCL nanofibers. Platelets. (2018) 29:395–405. doi: 10.1080/09537104.2017.1316838
16. Jochems CEA, van der Valk JBF, Stafleu FR, Baumans V. The use of fetal bovine serum: ethical or scientific problem? Altern Lab Anim. (2002) 30:219–27. doi: 10.1177/026119290203000208
17. van der Valk J, Mellor D, Brands R, Fischer R, Gruber F, Gstraunthaler G, et al. The humane collection of fetal bovine serum and possibilities for serum-free cell and tissue culture. Toxicol In Vitro. (2004) 18:1–12. doi: 10.1016/j.tiv.2003.08.009
18. Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The international society for cellular therapy position statement. Cytotherapy. (2006) 8:315–7. doi: 10.1080/14653240600855905
19. Hagen A, Niebert S, Brandt V-P, Holland H, Melzer M, Wehrend A, et al. Functional properties of equine adipose-derived mesenchymal stromal cells cultured with equine platelet lysate. Front Vet Sci. (2022) 9:890302. doi: 10.3389/fvets.2022.890302
20. Gilbertie JM, Long JM, Schubert AG, Berglund AK, Schaer TP, Schnabel LV. Pooled platelet-rich plasma lysate therapy increases synoviocyte proliferation and hyaluronic acid production while protecting chondrocytes from synoviocyte-derived inflammatory mediators. Front Vet Sci. (2018) 5:150. doi: 10.3389/fvets.2018.00150
21. Mussano F, Genova T, Munaron L, Petrillo S, Erovigni F, Carossa S. Cytokine, chemokine, and growth factor profile of platelet-rich plasma. Platelets. (2016) 27:467–71. doi: 10.3109/09537104.2016.1143922
22. Hillmann A, Paebst F, Brehm W, Piehler D, Schubert S, Tárnok A, et al. A novel direct co-culture assay analyzed by multicolor flow cytometry reveals context and cell type-specific immunomodulatory effects of equine mesenchymal stromal cells. PLoS ONE. (2019) 14:e0218949. doi: 10.1371/journal.pone.0218949
23. Bauer N, Keresztes M. Blutuntersuchung. In:Brehm W, Gehlen H, Ohnesorge B, Wehrend A, , editors. Handbuch Pferdepraxis. 4th edition, Stuttgart: Enke (2016). p. 27–32.
24. Heinemann D,. Ex Vivo In Vitro Studies of the Impact of Zylexis® on the Immune Response Following Vaccination with Resequin® NN Plus with Special Consideration of the EHV-1/-4 Specific Antibody Response, the Immune Status the Cytokine Gene Expression Patterns in Horse Blood, Inaugural-Dissertation University of Berlin, Veterinary Medicine. (2008). Available online at: https://refubium.fu-berlin.de/handle/fub188/617 (accessed August 1, 2022).
25. Yoshihara R, Shiozawa S, Imai Y, Fujita T. Tumor necrosis factor alpha and interferon gamma inhibit proliferation and alkaline phosphatase activity of human osteoblastic SaOS-2 cell line. Lymphokine Res Spring. (1990) 9:59–66.
26. Le-Thi-Phuong T, Thirion G, Coutelier JP. Distinct gamma interferon-production pathways in mice infected with lactate dehydrogenase-elevating virus. J Gen Virol. (2007) 88:3063–6. doi: 10.1099/vir.0.83242-0
27. Peng M, Yin N, Chhangawala S, Xu K, Leslie CS, Li MO. Aerobic glycolysis promotes T helper 1 cell differentiation through an epigenetic mechanism. Science. (2016) 354:481–4. doi: 10.1126/science.aaf6284
28. Farrar MA, Schreiber RD. The molecular cell biology of interferon-gamma and its receptor. Annu Rev Immunol. (1993) 11:571–611. doi: 10.1146/annurev.iy.11.040193.003035
29. Jansen JE, Aschenbrenner D, Uhlig HH, Coles MC, Gaffney EA. A method for the inference of cytokine interaction networks. PLoS Comput Biol. (2022) 18:e1010112. doi: 10.1371/journal.pcbi.1010112
30. Liu C, Chu D, Kalantar-Zadeh K, George J, Young HA, Liu G. Cytokines: from clinical significance to quantification. Adv Sci. (2021) 8:e2004433. doi: 10.1002/advs.202004433
31. Samara O, Alajlouni J, Al Najar M, Saleh M, Ryalat N, Gharaibeh A, et al. Intra-articular autologous platelet lysates produce positive mri structural changes in early and intermediate knee osteoarthrosis. Pakistan J Radiol. (2017) 27:14–8.
32. Al-Ajlouni J, Awidi A, Samara O, Al-Najar M, Tarwanah E, Saleh M, et al. Safety and efficacy of autologous intra-articular platelet lysates in early and intermediate knee osteoarthrosis in humans: a prospective open-label study. Clin J Sport Med. (2015) 25:524–8. doi: 10.1097/JSM.0000000000000166
33. Tyrnenopoulou P, Diakakis N, Karayannopoulou M, Savvas I, Koliakos G. Evaluation of intra-articular injection of autologous platelet lysate (PL) in horses with osteoarthritis of the distal interphalangeal joint. Vet Q. (2016) 36:56–62. doi: 10.1080/01652176.2016.1141257
34. Markazi R, Soltani-Zangbar MS, Zamani M, Eghbal-Fard S, Motavalli R, Kamrani A, et al. Platelet lysate and tendon healing: comparative analysis of autologous frozen-thawed PRP and ketorolac tromethamine in the treatment of patients with rotator cuff tendinopathy. Growth Factors. (2022) 40:163–74. doi: 10.1080/08977194.2022.2093198
35. Chen LW, Huang CJ, Tu WH, Lu CJ, Sun YC, Lin SY, et al. The corneal epitheliotrophic abilities of lyophilized powder form human platelet lysates. PLoS ONE. (2018) 13:e0194345. doi: 10.1371/journal.pone.0194345
36. Huang CJ, Sun YC, Christopher K, Pai AS, Lu CJ, Hu FR, et al. Comparison of corneal epitheliotrophic capacities among human platelet lysates and other blood derivatives. PLoS ONE. (2017) 12:e0171008. doi: 10.1371/journal.pone.0171008
37. Geremicca W, Fonte C, Vecchio S. Blood components for topical use in tissue regeneration: evaluation of corneal lesions treated with platelet lysate and considerations on repair mechanisms. Blood Transfus. (2010) 8:107–12. doi: 10.2450/2009.0091-09
38. Etulain J. Platelets in wound healing and regenerative medicine. Platelets. (2018) 29:556–68. doi: 10.1080/09537104.2018.1430357
39. Nurden AT, Nurden P, Sanchez M, Andia I, Anitua E. Platelets and wound healing. Front Biosci. (2008) 13:3532–48. doi: 10.2741/2947
40. Anitua E, Andia I, Ardanza B, Nurden P, Nurden AT. Autologous platelets as a source of proteins for healing and tissue regeneration. Thromb Haemost. (2004) 91:4–15. doi: 10.1160/TH03-07-0440
41. Naskou MC, Sumner SM, Chocallo A, Kemelmakher H, Thoresen M, Copland I, et al. Platelet lysate as a novel serum-free media supplement for the culture of equine bone marrow-derived mesenchymal stem cells. Stem Cell Res Ther. (2018) 9:75. doi: 10.1186/s13287-018-0823-3
42. Yaneselli K, Barrachina L, Remacha AR, Algorta A, Vitoria A, Cequier A, et al. Effect of allogeneic platelet lysate on equine bone marrow derived mesenchymal stem cell characteristics, including immunogenic and immunomodulatory gene expression profile. Vet Immunol Immunopathol. (2019) 217:109944. doi: 10.1016/j.vetimm.2019.109944
43. Barrachina L, Remacha AR, Romero A, Vázquez FJ, Albareda J, Prades M, et al. Priming equine bone marrow-derived mesenchymal stem cells with proinflammatory cytokines: implications in immunomodulation-immunogenicity balance, cell viability, and differentiation potential. Stem Cells Dev. (2017) 26:15–24. doi: 10.1089/scd.2016.0209
Keywords: platelet lysate, equine, IFN-γ, TNF-α, IL-1β, IL-4, IL-6, IL-10
Citation: Moellerberndt J, Hagen A, Niebert S, Büttner K and Burk J (2023) Cytokines in equine platelet lysate and related blood products. Front. Vet. Sci. 10:1117829. doi: 10.3389/fvets.2023.1117829
Received: 06 December 2022; Accepted: 09 February 2023;
Published: 09 March 2023.
Edited by:
Eleonora Iacono, University of Bologna, ItalyReviewed by:
Jorge U. Carmona, University of Caldas, ColombiaCopyright © 2023 Moellerberndt, Hagen, Niebert, Büttner and Burk. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Janina Burk, amFuaW5hLmJ1cmtAdmV0bWVkLnVuaS1naWVzc2VuLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.