
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Vet. Sci. , 14 June 2022
Sec. Veterinary Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fvets.2022.921471
This article is part of the Research Topic Sports Medicine and Physical Rehabilitation, Volume II View all 19 articles
Physical rehabilitation is frequently recommended in dogs recovering from acute thoracolumbar intervertebral disc extrusion (TL-IVDE), but protocols vary widely. The objective of this study was to evaluate the feasibility of incorporating sensory-integrated neurorehabilitation strategies into a post-operative rehabilitation protocol in dogs with TL-IVDE. Non-ambulatory dogs with acute TL-IVDE managed surgically were prospectively recruited to this unblinded cross-over feasibility study. Eligible dogs were randomized to start with tactile-enhanced (artificial grass) or auditory-enhanced (floor piano) basic rehabilitation exercises performed twice daily for the first 4 weeks before switching to the opposite surface for the subsequent 4 weeks. Neurologic examination, open field gait scoring, girth measurements and an owner-completed feasibility questionnaire were performed at baseline and 2, 4, 6, and 8 weeks post-operatively. Twenty-four dogs were enrolled, 12 randomized to each order of exercises. Gait scores did not differ between the two groups at baseline, 4 or 8 week visits. All modified exercises could be performed and compliance was high. Adverse events potentially attributable to the study surface were mild, self-limiting and occurred in 2/24 dogs. The most common surface-related limitations were that the piano was slippery and that both surfaces were too short. The artificial grass was preferred by owners and dogs compared to the floor piano surface, but this was influenced by which surface was utilized first. Auditory and tactile modifications were feasible and safe to incorporate into a standardized rehabilitation protocol. This pilot study could prompt larger efficacy studies investigating the benefit of sensory-integrated rehabilitation in dogs with TL-IVDE.
Acute spinal cord injury (SCI) occurs frequently in dogs, commonly due to thoracolumbar intervertebral disc extrusion (TL-IVDE) (1, 2). A successful outcome after TL-IVDE in dogs is typically defined as resolution of pain and regaining independent ambulation and reasonable continence (3). Physical rehabilitation is frequently recommended to facilitate improvement (4, 5) with basic rehabilitation exercises consisting of cryotherapy, passive range of motion, massage, assisted standing and assisted walking (6–17). A variety of more intensive or multimodal protocols have been described in dogs with SCI, but the primary target of most rehabilitation therapy is the motor system (8, 11–23).
Sensory stimulation as a component of rehabilitation protocols in dogs is occasionally mentioned with descriptions of toe pinching, hair brushing, and utilizing different flooring surfaces (7, 10–12, 16, 19). However, details are limited regarding how they are incorporated and evidence to support such sensory-stimulating exercises is lacking in veterinary patients. In human stroke and SCI patients, sensory integration training has been shown to improve motor outcomes (24–29). This includes preferential stimulation of sensory fibers of peripheral nerves which promotes improved somatosensory processing and augments the effects of massed practice of motor skills (25, 26). Vibratory stimulation of specific muscle groups also provides enhanced proprioceptive feedback and improves motor function in people with incomplete tetraplegia (24) and stroke (28), and can be combined with other strategies such as using visual cues (30). Rhythmic auditory stimulation during gait training improves walking performance as does real-time auditory feedback of motor errors (27, 31–33). Visual strategies such as mirroring specific actions by an unaffected limb or providing real-time visual feedback during exercises appear to similarly promote improved motor learning and execution (27, 34). The benefit of sensory-based neurorehabilitation strategies in dogs with acute SCI is unknown.
The objective of this study was to evaluate the feasibility of incorporating tactile- and auditory-enhanced exercises into a standardized, post-operative basic rehabilitation protocol in dogs with TL-IVDE. We hypothesized that sensory-enhanced exercises would be simple to perform and well-tolerated by dogs recovering from acute TL-IVDE.
Client-owned dogs were prospectively recruited from the existing patient pool of the Purdue University Veterinary Hospital. Dogs had to have an acute SCI secondary to TL-IVDE resulting in non-ambulatory paraparesis or paraplegia with or without pain perception, be aged 1 to 10 years and weigh between 5 and 25 kg. The minimum weight limit was to ensure dogs were sufficiently large enough to produce sounds on the surface utilized for the auditory-enhanced exercises. The upper weight limit was chosen to facilitate adequate participation in exercises given length limitations of the study surfaces. Duration of neurologic signs had to be ≤7 days from onset of pain or pelvic limb deficits. Confirmation of TL-IVDE between the third thoracic and third lumbar vertebrae (T3-L3) was required based on computed tomography or magnetic resonance imaging. Decompressive hemilaminectomy was performed followed imaging confirmation of extruded disc material. The number of sites decompressed and whether durotomy or prophylactic fenestration were performed was at the discretion of the neurosurgeon.
Exclusion criteria included deafness, severe orthopedic or systemic disease, signs consistent with progressive myelomalacia on presentation, temperament (i.e., dogs not amenable to handling), or unwillingness to return for study rechecks. The study was approved by the Purdue Animal Care and Use Committee (protocol #201200210) and all owners provided informed consent at enrollment.
This study was a prospective, randomized, unblinded, cross-over design clinical trial. At 48 h post-operatively, eligible dogs were enrolled, stratified based on whether or not they had deep pain perception (deep pain positive or deep pain negative) and then assigned to one of two treatment groups in a 1:1 ratio using block randomization (groups of 4) with a cross-over design. Stratification ensured an even distribution of the most severely affected dogs (i.e., deep pain negative) between the treatment groups. Group 1 participated in tactile-enhanced neurorehabilitation for 4 weeks, then auditory-enhanced exercises for 4 weeks while group 2 participated in the opposite order of exercises. Dogs were evaluated at enrollment (baseline visit) and at 2-, 4-, 6-, and 8-weeks post-operatively.
Touch (i.e., Artificial grass1) or sound (i.e., Floor piano mat2) modifications were incorporated into a standardized post-operative rehabilitation regimen which included: passive range of motion (PROM), assisted standing and weight-shifting and assisted walking. A 2-foot-wide by 6-foot-long strip of artificial grass and a 29-inch-wide and 70-inch-long child's floor piano were utilized as the tactile- and auditory-enhancements, respectively (Figure 1). The floor piano had a smooth surface. Passive range of motion was performed in a standing position where each pelvic limb was manually manipulated through range of motion (bicycling) at each joint to simulate limb movement during walking (Supplementary Video 1). The plantar surface of the paw was brought in contact with the study surface with each repetition, either touching the grass or touching and producing a sound on the floor piano. This was repeated 20 times per leg at each session. Assisted standing and weight shifting consisted of supporting the dog to stand squarely with all four limbs positioned on the study surface (Supplementary Video 2). The hips were then gently shifted from left to right and front to back for 5 min at each session. For PROM and assisted standing and weight shifting exercises, the use of the owner's hands, a sling, a physiopeanut or modified foam roller were utilized to provide hindquarter support as needed until dogs were able to support their own weight against gravity. Assisted walking was performed by repeatedly walking the dog on a leash across the study surface for 5 min per session (Supplementary Videos 3, 4). Hindquarter support was provided with the use of a sling or harness until dogs were independently ambulatory. When utilizing the floor piano for standing and walking exercises, the goal was to produce a sound each time the body weight was shifted or a step was taken, respectively.
All exercises were performed two times per day throughout the 8-week study period, including during initial hospitalization, starting 48-h post-operatively. Owners were sent home with the assigned study surface at the time of discharge from initial hospitalization and provided with the new study surface at the 4-week study visit. At the time of discharge and the 4-week recheck, owners were instructed verbally and via demonstrations on how to perform each exercise including how to use and incorporate each study surface.
At each study visit, the following procedures were performed: physical and neurologic examinations, open field gait scoring, body and limb circumference measurements, and an owner-completed questionnaire. Neurologic examination consisted of evaluation of mentation, gait, cranial nerves, postural reactions, spinal reflexes, presence of spinal hypersthesia, pain perception and continence. Gait was classified as normal, ambulatory paraparesis, non-ambulatory paraparesis or paraplegia. Ambulation was defined as being able to take at least 10 consecutive weight-bearing steps without falling. Gait was also scored using the validated 0-12-point open field gait scale (OFS) (35, 36). A Gulick-type 2 tape measurement device3 was utilized for all circumference measurements and performed by trained personnel. Three circumference measurements were performed in triplicate as previously reported including caudal trunk girth and right and left thigh girth (37). Briefly, the caudal trunk measurement was performed in a standing position with girth measured around the abdomen just cranial to the inguinal folds. Limb girth measurements were performed in lateral recumbency with the circumference of the upper limb measured at 50% of the length of the femur from the greater trochanter. A questionnaire was completed by owners at each study visit (Supplementary Figure 1). The questions focused on compliance and feasibility regarding the ease of completion, patient tolerance and any adverse effects associated with the rehabilitation exercises or the study surface.
As a pilot, feasibility study, a power analysis was not performed. A minimum sample size of 20 dogs was planned with the aim of providing sufficient preliminary data on our methods. Descriptive statistics were utilized to summarize enrollment and feasibility data acquired in this study. Triplicate girth measurements were averaged to provide a mean value for each dog at each visit. To account for dogs of varying size and conformation, these measurements were expressed as a percentage of the baseline values. Mean OFS scores and girth measurements at baseline, 4 and 8 weeks post-operatively were compared using a t-test to look for any differences between groups. P < 0.05 was considered significant.
Twenty-four dogs were enrolled with a mean age of 4.4 years (SD 2.2) and mean body weight of 9.4 kg (SD 4.5) at baseline. Breeds included 12 dachshunds, four mixed breed dogs, three French bulldogs, and five breeds represented by two or fewer dogs. Mean duration of neurologic signs prior to enrollment was 3.2 days (SD 1.2), accounting for a 48-h interval from presentation and surgery to enrollment. Twelve dogs including twoparaplegic with absent pain perception were randomized to start with exercises incorporating the artificial grass (Group 1). This group had a mean age of 3.8 years (SD 2), mean body weight 11 kg (SD 4.9) of and mean duration of signs of 3.2 days (SD 1.1). Twelve dogs including 3 paraplegic with absent pain perception were randomized to start with the floor piano (Group 2). This group had a mean age of 5 years (SD 2.4), a mean body weight of 7.7 kg (SD 3.6) and a mean duration of signs of 3.2 days (SD 1.2). Group 1 was significantly heavier than group 2 (p = 0.04), but no significant differences were identified between groups with regard to age or duration of signs (p > 0.05).
All dogs were diagnosed with TL-IVDE between T10 and L3 and underwent decompressive surgery. Surgical plan including number of sites decompressed and prophylactic fenestration varied between cases. No intra-operative complications were encountered. One dog required a second decompressive surgery 3 days after the first due early re-herniation of disc material resulting in paraplegia with intact pain perception. This dog was enrolled in the study 48 h after the second surgery (with a neurologic status of paraplegia with intact pain perception) and no physical rehabilitation exercises were performed (of any kind) until enrollment and randomization. Nineteen dogs completed all study visits (nine in group 1, 10 in group 2), one dog completed three of the four rechecks (missed 6-week visit), two dogs completed two of four rechecks (missing 6- and 8-week rechecks), one dog completed only the 2-week recheck. One additional dog was euthanized within 1 week after the baseline visit (due to lack of neurologic improvement).
At baseline, seven dogs were non-ambulatory paraparetic (two in group 1, five in group 2), 12 were paraplegic with intact pain perception (eight in group 1, four in group 2) and five were paraplegic with absent pain perception in their pelvic limb toes and tail base (two in group 1, 3 in group 2). Of the dogs with available follow-up data, 16 dogs were ambulatory by 2 weeks, 17 dogs were ambulatory by 4 weeks and 18 dogs were ambulatory by 8 weeks or sooner. At study completion, 4 dogs remained non-ambulatory, of which 3 had persistently absent pain perception with varying degrees of pelvic limb motor. Gait scores across study visits are outlined in Table 1. There were no significant differences identified in OFS scores between groups at baseline, 4 and 8-week study rechecks (p > 0.05).
Proprioception (paw placing) was absent in all dogs at baseline. By study completion, proprioceptive placing had completely normalized in five dogs, including two dog from group 1 and three dogs in group 2, but remained delayed or absent in the remainder. Mean girth measurements expressed as a percentage of baseline values are outlined in Table 2. Caudal trunk girth was decreased at 4 weeks compared to baseline in both groups; by 8 weeks post-operatively, this had returned to baseline in group 2 but remained lower in group 1. Left and right thigh circumference measurements did not demonstrate clear trends. Changes were generally small and no significant differences between groups over time were identified (p > 0.05).
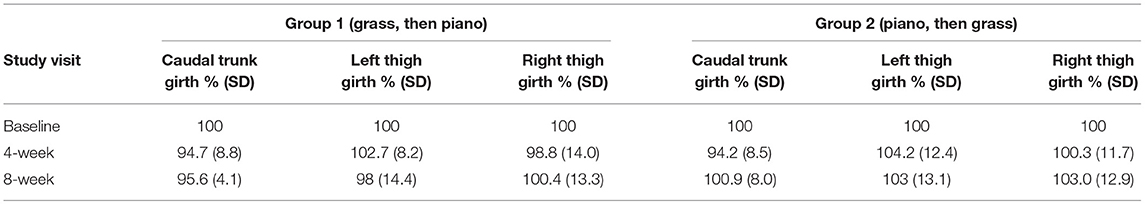
Table 2. Mean thigh and body girth measurements at the 4- and 8-week study visits, expressed as a percentage of baseline values.
Adverse events during the course of the study occurred in 5/24 (21%) dogs, including two dogs in which it was considered attributable to the tactile or auditory modifications. In one dog, the piano noise was noted to be particularly aversive and another dog developed a superficial abrasion on the dorsum of the right pelvic limb paw during the study period when using the artificial grass. Neither event required intervention and the exercises were continued by both owners. Additional adverse events reported by owners in three dogs were related to their neurologic status. This included one dog initially paraplegic deep pain negative that regained pain perception by discharge but was euthanized at 1 week post-operatively due to lack of recovery of function. Another dog initially recovered uneventfully but had a recurrence of paraplegia at 4.5 weeks post-operatively due to a presumptive re-herniation. This dog was managed conservatively and had regained independent ambulation by the next study visit. A third dog was noted by the owner to be intermittently, mildly painful when performing the daily exercises during the first 2 weeks post-operatively. No adjustments to the dog's analgesic protocol were required.
In 20/24 (83%) dogs, all modified exercises were performed as instructed, while owners of four dogs reported that they were unable to perform all of the exercises twice daily at some point during the study period. In 3 dogs, this was reported for a single 2-week period while one owner reported incompletely performing the exercises over a duration of 4 weeks. The reasons cited included being busy or other scheduling conflict in 3 dogs and fear of worsening status in one dog that suffered a presumptive re-herniation.
All exercises were able to be performed with the modifications. However, ease of use varied between dogs and surfaces. Summarizing owner-reported feasibility across all study visits in which data was available, 13/22 (59%) owners reported that the grass was easy to use while 9/22 (41%) owners reported at least once that use was associated with mild difficulty. Six of 20 (30%) dog owners reported that the piano was easy to use while 14/20 (70%) owners rated on at least one occasion that this surface was mildly difficult (12/20, 60%) or hard to use (2/20, 10%). No trends over time during the 8-week study period regarding ease of use for each surface were identified.
Feedback relayed via the questionnaire could be subdivided into comments that were related vs. unrelated to the surfaces. Positive experiences related to the the artificial grass were reported in two dogs including one dog that ‘loved the grass' and another where it ‘reminded the dog of being outside.' Positive experiences related to the floor piano were also reported in two dogs including one dog that ‘liked making noises' and another where it ‘seemed like a game.' The most common surface-related limitations or negative experiences reported were that the piano was too slippery and both the grass and piano were too short, especially when performing the walking exercises. These were noted in ~25 and 15% of questionnaire responses, respectively. Less than 10% of responses indicated that dogs initially disliked or were scared of the artificial grass texture or the piano noises, though all were reported to get used to it on subsequent responses. One dog weighing 6.4 kg was noted to be too small to consistently make noise on the floor piano when performing the exercises, though this was not specifically reported in the seven other dogs weighing the same or less (5.4–6.4 kg) than this dog.
There were non-surface related comments provided in about 27% of questionnaire responses and these were generally attributable to behavioral limitations associated with performing the exercises. The most commonly reported behavioral difficulties included that the dog got distracted or tried to move away from the owner and the designated surface/exercise area, that the dog was not cooperative when performing the exercises, that the dog became bored or frustrated during the 5-min sessions for each exercise, and that the duration of the exercises was too long. Owners also noted that these limitations became more frequent or problematic to overcome as their dogs improved and regained more pelvic limb function.
Of the 20 dogs that completed an 8-week study visit, owners of 14 dogs preferred the grass, three preferred the piano, two indicated an equal preference for both and one did not provide an answer. Eleven owners indicated that their dog preferred the grass, two thought their dog preferred the piano, five indicated their dog liked both surfaces equally, 1 owner reported that their dog disliked both surfaces equally, and one owner did not provide an answer. The surface preferences varied by group (Table 3). When starting with the piano first (group 2), 9/10 owners and 9/10 dogs preferred the grass. However, when starting with the grass first (group 1), 5/9 owners and 2/9 dogs preferred the grass.
This is the first study specifically investigating sensory-enhanced rehabilitation exercises in dogs recovering from acute TL-IVDE. Our results demonstrated that simple auditory and tactile modifications were feasible and safe to incorporate into a standardized rehabilitation protocol. While both surfaces were generally well-tolerated, dog behaviors independent of the surface contributed to challenges in performing the exercises during the study period. This preliminary information could be used to design larger efficacy studies investigating the benefit of sensory-enhanced neurorehabilitation and to continue to optimize rehabilitation protocols in this population.
Incorporating two different, readily accessible surfaces, a piece of artificial grass or a child's floor piano, we provided a simple means to enhance sensory feedback as part of a basic post-operative rehabilitation protocol consisting of PROM, assisted weight shifting and assisted walking. There is very limited detail from prior studies in veterinary patients regarding how exercises with a sensory component are incorporated (8, 10–12, 16, 19). Importantly, sensory stimulation exercises in the post operative veterinary neurologic patient typically center on the owner or rehabilitation professional stimulating the patient's feet, with activities like toe pinching, tickling or rubbing having been described (6, 8, 10, 11). This study was different in that the sensory stimulation was initiated by the patient's foot landing on the artificial grass or floor piano surface, and therefore, incorporated into the exercises themselves. Specific sensory-integrated techniques are utilized in people with SCI as well as other conditions such as stroke (24–28). These approaches allow intact sensory systems (e.g., auditory system) to provide appropriate input in the form of specific sensory cues during various motor training tasks to aid in recovery or compensation of an impaired sense (e.g. propioeption) after injury (38, 39). Music, through its ability to stimulate memories and the so-called memory-movement connection, has also been described as a rehabilitation strategy to promote muscle memory and enhance movement (40). A variation on this, known as cognitive multisensory rehabilitation, uses multisensory input to restore brain connectivity relating to awareness and pain perception that is impaired after SCI (41). Reported benefits include rebuilding the mind-body connection, improving body awareness and reducing neuropathic pain (41). Sensory-integrated neurorehabilitation approaches have also been associated with improved motor outcomes and enhanced overall functional recovery (24–28, 34, 38, 39).
Given the potential benefits demonstrated by human neurorehabilitation studies combined with the dearth of information in veterinary SCI patients, our rationale was to explore novel sensory stimulation integrated into a standardized rehabilitation protocol. We demonstrated that the tactile or auditory adaptations were simple to apply and that the modified exercises could be performed by veterinary professionals and owners with no specific training or skills. Additionally, the dogs of this study with severe SCI secondary to TL-IVDE were amenable to both the tactile and auditory sensory stimulation, regardless of their neurologic status or recovery trajectory. Patients who were paralyzed or severely paretic and also those who regained independent walking tolerated both types of sensory stimulation. In addition to feasibility, no substantial adverse events directly attributable to the surfaces or exercise modifications were encountered. Initiation of exercises at 48 h post-operatively was well-tolerated which is consistent with other clinical trials of post-operative physical rehabilitation (8, 17).
While this study was not designed to evaluate efficacy, we utilized open field gait scoring, proprioceptive placing and caudal trunk and thigh girth measurements to evaluate outcomes. No significant differences were identified in these measures between the two treatment groups at 4 or 8 weeks post-operatively, but there was no control group. In addition to incorporating controls and blinding evaluators, outcome measures that can quantify the potential influence of a sensory-integrated approach would help to evaluate the efficacy of our methods. For example, quantitative sensory thresholds have been established in dogs with acute SCI (42–45) and could be used to evaluate if sensory stimulation aids in re-establishing more normal thresholds after injury. Additionally, the F-response and H-reflex provide information on motor neuron pool excitability in dogs with acute and chronic SCI (46, 47). These electrodiagnostic tests could help to objectively determine if sensory enhanced exercises provide appropriate afferent input to positively impact motor neuron pool excitability and, in turn, contribute to motor recovery. Body weight distribution has also been quantified in dogs after SCI (37) and could be used with girth measurements and proprioception to determine if sensory interventions intended to improve limb awareness affect pelvic limb weight distribution and muscle mass. Evaluation of nuanced gait parameters such as velocity, cadence and stride length are utilized in human stroke patients undergoing rehabilitation (48, 49). Treadmill-based stepping and coordination scores are validated in dogs with SCI and could be similarly utilized to objectively measure rehabilitation progress (50). Tailored outcome measures could provide important evidence of a link between an enhanced, integrated sensory environment and improved functional recovery after SCI in dogs.
While all modified exercises were feasible, owner feedback highlighted several limitations regarding ease of completion. The short length of both the artificial grass and floor piano as well as the slippery surface of the piano were recurrent comments. This suggests that additional refinement of our techniques for incorporating sensory modifications is needed to improve feasibility, ensure appropriate compliance and optimize the potential benefit. Future adjustments to the tactile-enhanced exercises could include using a textured surface of longer length or incorporating expanded tactile modifications, including taking advantage of natural outdoor surface variations on assisted walks. Providing varied terrain (e.g., tall grass, gravel, etc.) has been mentioned for dogs with recovering from disc herniation (12), but specific protocols have not been established. Providing auditory feedback via an alternative method other than the floor piano might eliminate the body size restrictions and the need to utilize a slippery surface in non-ambulatory dogs. Sound, delivered in the form of musical notes with beat and rhythm, might also be most advantageous in the later stages of gait refinement and coordination as compared to earlier stages of regaining movement after SCI (32, 33, 51). Rhythmic auditory stimulation has been incorporated into rehabilitation programs following a variety of conditions in people including SCI, stroke and movement disorders (48, 51–54). Rhythmic auditory stimulation is based on the idea of entrainment, in which rhythmic patterns produced by sounds or music directly improve movement timing and efficiency (55). This sensory technique can be combined with treadmill training to improve gait speed and balance and could be adapted for dogs. Therefore, it is possible that timing of certain types of sensory stimulation is important and that auditory integration might be more useful once a dog is more functional or even ambulatory. Another alternative strategy could be utilizing auditory cues to highlight mistakes. This has been used to improve motor performance in people with stroke (31). Future larger scale efficacy studies are warranted comparing different types of tactile and auditory stimulation to each other in an ongoing effort to optimize rehabilitation protocols, including how best to incorporate sensory integration in both the hospital and home-care settings.
Owner reported compliance was generally high throughout the study, but owner feedback also commonly focused on non-surface related issues. This included things such as dog boredom, distractability or lack of cooperation for performing the exercises, which were reported to worsen as pelvic limb function improved. In prior studies in which at-home rehabilitation regimens are recommended (10–12, 17), sparse information is provided regarding if there was adherence to protocols or if any challenges were encountered in the proper execution of the exercises by owners. We do not have baseline data on compliance in performing these exercises without the sensory modifications. However, our results underscore that dog behavior could substantially impact proper performance of prescribed exercises and owner perception of the recovery process and willingness to engage in at-home protocols. In people with SCI, explicitly outlining daily tasks and recommended exercises provides clear expectations, structure and consistency which in turn improves compliance with rehabilitation participation (56). While there are obvious differences between motivating a dog vs. onself to participate in at-home rehabilitation, our findings support that behavioral factors should be considered when developing an at-home therapy regimen. Additionally, dynamically acquiring and responding to owner feedback might improve both owner and dog participation.
At study completion, 70% of owners preferred the grass and 55% of owners thought their dogs also preferred the grass while just 15% of owners and 10% of dogs preferred the piano. While this might support a true preference for the artificial grass surface, there was a discrepancy based on whether dogs were randomized to group 1 (grass first) or group 2 (piano first). When rehabilitation exercises were initially performed on the piano, the vast majority of the dogs and owners preferred grass as compared to the piano. The opposite, however, was not the case; when dogs used grass for the first half of the study, owner preference for grass over the piano was less decisive and dog preference was essentially equally spread between the surfaces. Therefore, the role of the order of surfaces and the dogs' neurologic status during the recovery period must be considered as factors impacting this preference. Similar to previously published data on recovery rates (57), the majority of dogs in this study regained independent ambulation within the first 4 weeks post-operatively. Thus, when pelvic limb motor function was worse during the first half of the study, the smooth surface of the floor piano likely made it more difficult to perform the exercises while the textured surface of the artificial grass could have provided better traction. This might help to explain why owners of dogs randomized to group 2 (piano first) more strongly favored the artificial grass. Once greater functional status was achieved, the slippery nature of the piano might have been less of a detractor and could account for the more even distribution of preference in dogs randomized to group 1 where the piano was not utilized until the latter half of the study. Another potential contributing factor is that group 2 was significantly lighter than group 1. Being lighter makes it harder to make noise on the floor piano and could exacerbate the lack of traction further influencing the preference toward the artificial grass.
Similarly, all owners whose dogs completed the study but did not regain ambulation during the 8 weeks of follow-up, preferred the grass to piano. In these more severely affected dogs, traction and support from the artificial grass might have facilitated more easily performing exercises compared to the smooth surface of the piano. While pelvic limb tone and ability to bear weight against gravity improved over the course of the study among the dogs that remained non-ambulatory, this might not have been enough to improve the ease of completion of exercises on the floor piano (relative to the grass) and influenced the owner's preferred surface.
Overall, this pilot project demonstrated that sensory integrated rehabilitation was feasible in dogs recovering from severe SCI and provides a framework to continue to investigate multisensory rehabilitation protocols incorporating visual, auditory, tactile, or somatosensory stimulation, or a combination of approaches. These preliminary results will be useful to design future, larger scale efficacy studies on sensorimotor integration into intensive, staged rehabilitation protocols in dogs recovering from SCI.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The animal study was reviewed and approved by Purdue University Institutional Animal Care and Use Committee (protocol # 201200210). Written informed consent was obtained from the owners for the participation of their animals in this study.
MJL and SAT participated in study design, data acquisition and analysis, manuscript preparation, and editing and review. JB, BL, NP, and RY participated in data acquisition and analysis and manuscript editing and review. All authors contributed to the article and approved the submitted version.
This project was funded by a grant from the American Association of Rehabilitation Veterinarians (AARV) and the Purina Institute.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2022.921471/full#supplementary-material
1. ^Greenline Jade 50 15ft Wide x Cut to Length Artificial Grass, Home Depot, homedepot.com.
2. ^Click N' Play Gigantic Keyboard Play Mat 70 x 29 inches, Amazon, amazon.com.
3. ^Gulick II Tape Measure, Fitness Mart, GaysMills, WI.
1. Dewey CW, da Costa RC. Myelopathies: disorders of the spinal cord. In: Dewey CW, da Costa RC, eds. Practice Guide to Canine and Feline Neurology. 3rd ed. Oxford: Wiley Blackwell (2016) p. 329–403.
2. Granger N, Carwardine D. Acute spinal cord injury tetraplegia and paraplegia in small animals. Vet Clin Small Anim. (2014) 44:1131–56. doi: 10.1016/j.cvsm.2014.07.013
3. Olby NJ, da Costa RC, Levine JM, Stein VM, CANSORT SCI. Prognostic factors in canine acute intervertebral disc disease. Front Vet Sci. (2020) 3:6059. doi: 10.3389/fvets.2020.596059
4. Frank LR, Roynard PFP. Veterinary neurologic rehabilitation: the rationale for a comprehensive approach. Topic in Compan An Med. (2018) 33:49–57. doi: 10.1053/j.tcam.2018.04.002
5. Moore SA, Early PJ, Hettlich BF. Practice patterns in the management of acute intervertebral disc herniation in dogs. J Small Anim Pract. (2016) 57:409–15. doi: 10.1111/jsap.12496
6. Drum MG. Physical rehabilitation of the canine neurologic patient. Vet Clin Small Anim. (2010) 40:181–93. doi: 10.1016/j.cvsm.2009.09.009
7. Thomas WB, Olby NJ, Sharon L. Neurologic conditions and physical rehabilitation of the neurologic patient. In: Millis DL, Levine D, Taylor R, eds. Canine Rehabilitation and Physical Therapy. 2nd ed. Philadelphia: WB Saunders Co (2004) 609–27. doi: 10.1016/B978-1-4377-0309-2.00034-X
8. Bennaim M, Porato M, Jarleton A, Hamon M, Carroll JD, Gommeren K, et al. Preliminary evaluation of the effects of photobiomodulation therapy and physical rehabilitation on early postoperative recovery of dogs undergoing hemilaminectomy for treatment of thoracolumbar intervertebral disc disease. Am J Vet Res. (2017) 78:195–206. doi: 10.2460/ajvr.78.2.195
9. Bruno E, Canal S, Antonucci M, Bernardini M, Balducci F, Musella V, et al. Perilesional photobiomodulation therapy and physical rehabilitation in post-operative recovery of dogs surgically treated for thoracolumbar disk extrusion. BMC Vet Res. (2020) 16:120. doi: 10.1186/s12917-020-02333-3
10. Draper WE, Schubert TA, Clemmons RM, Miles SA. Low-level laser therapy reduces time to ambulation in dogs after hemilaminectomy: a preliminary study. J Small Anim Pract. (2012) 53:465–9. doi: 10.1111/j.1748-5827.2012.01242.x
11. Hady LL, Schwarz PD. Recovery times for dogs undergoing thoracolumbar hemilaminectomy with fenestration and physical rehabilitation: a review of 113 cases. J Vet Med An Health. (2015) 7:278–89. doi: 10.5897/JVMAH2015.0398
12. Hodgson MM, Bevan JM, Evans RB, Johnson TI. Influence of in-house rehabilitation on the postoperative outcome of dogs with intervertebral disk herniation. Vet Surgery. (2017) 46:566–73. doi: 10.1111/vsu.12635
13. Jadeson W. Rehabilitation of dogs with intervertebral disk lesions by physical therapy methods: 1. Basic aspects of disk lesions in dogs. J Am Vet Med Assoc. (1961) 138:411–3. doi: 10.1136/bmj.1.5223.411-a
14. Jadeson W. Rehabilitation of dogs with intervertebral disk lesions by physical therapy methods: 2. Review of treatment methods. J Am Vet Med Assoc. (1961) 138:414–5.
15. Jadeson W. Rehabilitation of dogs with intervertebral disk lesions by physical therapy methods: 3. A pilot study of the effect of physical therapy. J Am Vet Med Assoc. (1961) 138:415–23.
16. Martins Â, Gouveia D, Cardoso A, Carvalho C, Coelho T, Silva C, et al. A controlled clinical study of intensive neurorehabilitation in post-surgical dogs with severe acute intervertebral disc extrusion. Animals. (2021) 11:3034. doi: 10.3390/ani11113034
17. Zidan N, Sims C, Fenn J, Williams K, Griffith E, Early PJ, et al. A randomized, blinded, prospective clinical trial of postoperative rehabilitation in dogs after surgical decompression of acute thoracolumbar intervertebral disc herniation. J Vet Intern Med. (2018) 32:1133–44. doi: 10.1111/jvim.15086
18. Gandini G, Cizinauskas S, Lang J, Fatzer R, Jaggy A. Fibrocartilaginous embolism in 75 dogs: clinical findings and factors influencing recovery rate. J Sm Anim Pract. (2003) 44:76–80. doi: 10.1111/j.1748-5827.2003.tb00124.x
19. Gallucci A, Dragone L, Menchetti M, Gagliardo T, Pietra M, Cardinali M, et al. Acquisition of involuntary spinal locomotion (Spinal Walking) in dogs with irreversible thoracolumbar spinal cord lesion: 81 dogs. J Vet Intern Med. (2017) 222:762–6. doi: 10.1111/jvim.14651
20. Gordon-Evans WJ, Johnson AL, Knap KE, Griffon DJ. The effect of body condition on postoperative recovery of dachshunds with intervertebral disc disease treated with postoperative physical rehabilitation. Vet Surg. (2019) 48:159–63. doi: 10.1111/vsu.13142
21. Jeong IS, Piao Z, Rahman M, Kim S, Kim NS. Canine thoracolumbar intervertebral disk herniation and rehabilitation therapy after surgical decompression: a retrospective study. J Adv Vet Anim Res. (2019) 6:394–402. doi: 10.5455/javar.2019.f359
22. Martins A, Gouveia D, Cardoso A, Viegas I, Gamboa O, Ferreira A, et al. comparison between body weight supported treadmill training and conventional over-ground training in dogs with incomplete spinal cord injury. Front Vet Sci. (2021) 8:597949. doi: 10.3389/fvets.2021.597949
23. Mojarradi A, De Decker S, Bäckström C, Bergknut N. Safety of early postoperative hydrotherapy in dogs undergoing thoracolumbar hemilaminectomy. J Small Anim Pract. (2021) 62:1062–9. doi: 10.1111/jsap.13412
24. Backus D, Cordo P, Gillott A, Kandilakis C, Mori M, Raslan AM. Assisted movement with proprioceptive stimulation reduces impairment and restores function in incomplete spinal cord injury. Arch Phys Med Rehabil. (2014) 95:1447–53. doi: 10.1016/j.apmr.2014.03.011
25. Beekhuizen KS, Field-Fote EC. Massed practice versus massed practice with stimulation: effects on upper extremity function and cortical plasticity in individuals with incomplete cervical spinal cord injury. Neurorehabil Neural Repair. (2005) 19:33–45. doi: 10.1177/1545968305274517
26. Beekhuizen KS, Field-Fote EC. Sensory stimulation augments the effects of massed practice in persons with tetraplegia. Arch Phys Med Rehabil. (2008) 89:602–8. doi: 10.1016/j.apmr.2007.11.021
27. Bolognini N, Russo C, Edwards DJ. The sensory side of post-stroke motor rehabilitation. Restor Neurol Neurosci. (2016) 34:571–86. doi: 10.3233/RNN-150606
28. Cordo P, Lutsep H, Cordo L, Wright G, Cacciatore T, Skoss R. Assisted movement with enhanced sensation (AMES): coupling motor and sensory to remediate motor deficits in chronic stroke patients. Neurorehabil Neural Repair. (2009) 23:67–77. doi: 10.1177/1545968308317437
29. Smania N, Picelli A, Gandolfi M, Fiaschi A, Tinazzi M. Rehabilitation of sensorimotor integration deficits in balance impairment of patients with stroke hemiparesis: a before/after pilot study. Neurol Sci. (2008) 29:313–9. doi: 10.1007/s10072-008-0988-0
30. Tzorakoleftherakis E, Bengstron MC, Mussa-Ivaldi FA, Scheidt RA, Murphey TD. Tactile proprioceptive input in robotic rehabilitation after stroke. IEEE I. 2015 IEEE International Conference on Robotics and Automation (ICRA). (2015) 6475–81. doi: 10.1109/ICRA.2015.7140109
31. Secoli R, Milot MH, Rosati G, Reinkensmeyer DJ. Effect of visual distraction and auditory feedback on patient effort during robot-assisted movement training after stroke. J Neuro Eng Rehabil. (2011) 8:1–10. doi: 10.1186/1743-0003-8-21
32. Thaut MH, Leins AK, Rice RR, Argstatter H, Kenyon GP, McIntosh GC, et al. Rhythmic auditory stimulation improves gait more than NDT/Bobath training in near-ambulatory patients early poststroke: a single-blind, randomized trial. Neurorehabil Neural Repair. (2007) 21:455–9. doi: 10.1177/1545968307300523
33. LaGrasse AB, Knight A. Rhythm and music in rehabilitation: a critical review of current research. Physical Rehabil Med. (2011) 23:49–67. doi: 10.1615/CritRevPhysRehabilMed.v23.i1-4.40
34. Sayenko DG, Alekhina MI, Masani K, Vette AH, Obata H, Popvic MR, et al. Positive effect of balance training with visual feedback on standing balance abilities in people with incomplete spinal cord injury. Spinal Cord. (2010) 48:886–93. doi: 10.1038/sc.2010.41
35. Olby NJ, De Risio L, Munana KR, Wosar MA, Skeen TM, Sharp NJH, et al. Development of a functional scoring system in dogs with acute spinal cord injuries. Am J Vet Res. (2001) 62:1624–8. doi: 10.2460/ajvr.2001.62.1624
36. Olby NJ, Muguet-Chanoit AC, Lim JH, Davidian M, Mariani CL, Freeman AC, et al. A placebo-controlled, prospective, randomized clinical trial of polyethylene glycol and methylprednisolone sodium succinate in dogs with intervertebral disk herniation. J Vet Intern Med. (2016) 30:206–14. doi: 10.1111/jvim.13657
37. Amaral-Marrero NP, Thomovsky SA, Linder JE, Bowditch J, Lind M, Kazmierczak KA, et al. Static body weight distribution and girth measurements over time in dogs after acute thoracolumbar intervertebral disc extrusion. Front Vet Sci. (2022) 388:7402. doi: 10.3389/fvets.2022.877402
38. Jang SH, Lee JH. Impact of sensory integration training on balance among stroke patients. Open Med. (2016) 11:330–5. doi: 10.1515/med-2016-0061
39. Yen SC, Landry JM, Wu M. Augmented multisensory feedback enhances locomotor adaptation in humans with incomplete spinal cord injury. Human Mov Sci. (2014) 35:80–93. doi: 10.1016/j.humov.2014.03.006
40. Thaut M. Neurologic music therapy in sensorimotor rehabilitation. In: Rhythm, Music, and the Brain: Scientific Foundations and Clinical Applications. New York, NY: Taylor and Francis Group (2005). p. 137–64.
41. Carpentier S, Deng W, Bottale S, Hendrickson T, Zhang L, Wudlick R, et al. Cognitive multisensory rehabilitation for sensory and motor function in adults with spinal cord injury: proof of concept. Arch Phys Med Rehabil. (2022) 103: e21–22. doi: 10.1016/j.apmr.2022.01.059
42. Gorney AM, Blau SR, Dohse CS, Griffith EH, Williams KD, Lim JH, et al. Mechanical and thermal sensory testing in normal chondrodystrophoid dogs and dogs with spinal cord injury caused by thoracolumbar intervertebral disc herniations. J Vet Intern Med. (2016) 30:627–35. doi: 10.1111/jvim.13913
43. Moore SA, Hettlich BF, Waln A. The use of an electronic von Frey device for evaluation of sensory threshold in neurologically normal dogs and those with acute spinal cord injury. Vet J. (2013) 197:216–9. doi: 10.1016/j.tvjl.2012.11.003
44. Song RB, Basso DM, da Costa RC, Fisher LC, Mo X, Moore SA. Von Frey anesthesiometry to assess sensory impairment after acute spinal cord injury caused by thoracolumbar intervertebral disc extrusion in dogs. Vet J. (2016) 209:144–9. doi: 10.1016/j.tvjl.2015.07.028
45. Zidan N, Medland J, Olby NJ. Long-term postoperative pain evaluation in dogs with thoracolumbar intervertebral disk herniation after hemilaminectomy. J Vet Intern Med. (2020) 34:1547–55. doi: 10.1111/jvim.15800
46. Lewis MJ, Howard JF, Olby NJ. The relationship between trans-lesional conduction, motor neuron pool excitability, and motor function in dogs with incomplete recovery from severe spinal cord injury. J Neurotrauma. (2017) 34:2994–3002. doi: 10.1089/neu.2017.5012
47. Okuno S, Orito K. F-wave parameters for the tibial nerve in miniature dachshunds with and without naturally acquired thoracolumbar intervertebral disk herniation. Am J Vet Res. (2020) 81:422–7. doi: 10.2460/ajvr.81.5.422
48. Cha Y, Kim Y, Chung Y. Immediate effects of rhythmic auditory stimulation with tempo changes on gait in stroke patients. J Phys Ther Sci. (2014) 26:479–82. doi: 10.1589/jpts.26.479
49. Thaut MH, McIntosh G, Rice RR. Rhythmic facilitation of gait training in hemiparetic stroke rehabilitation. J of Neurol Sci. (1997) 151:207–12. doi: 10.1016/S0022-510X(97)00146-9
50. Olby NJ, Lim JH, Babb K, Bach K, Domaracki C, Williams K, et al. Gait scoring in dogs with thoracolumbar spinal cord injuries when walking on a treadmill. BMC Vet Research. (2014) 10:1–8. doi: 10.1186/1746-6148-10-58
51. Thaut MH, Abiru M. Rhythmic auditory stimulation in rehabilitation of movement disorders: a review of current research. Music Percep. (2010) 27:263–9. doi: 10.1525/mp.2010.27.4.263
52. de l'Etoile SK. The effect of rhythmic auditory stimulation on the gait parameters of patients with incomplete spinal cord injury: an exploratory pilot study. Int J Rehab Res. (2008) 21:155–7. doi: 10.1097/MRR.0b013e3282fc0f44
53. Mainka S, Wissel J, Voller H, Evers S. The use of rhythmic auditory stimulation to optimize treadmill training for stroke patients: a randomized controlled trial. Front in Neurol. (2018) 9:1–8. doi: 10.3389/fneur/2018.00755
54. Thaut MH, McIntosh GC, Rice RR, Miller RA, Rathbun J, Brault JM. Rhythmic auditory stimulation in gait training with Parkinson's disease patients. Mov Disord. (1996) 11:193–200. doi: 10.1002/mds.870110213
55. Thaut MH, McIntosh GC, Hoemberg V. Neurobiological foundations of neurologic music therapy: rhythmic entrainment and the motor system. Front Psycho. (2015) 5:1–6. doi: 10.3389/fpsyg.2014.01185
56. Gorski JA, Slifer KJH, Townsend V, Kelly-Suttka J, Amari A. Behavioral treatment of non-compliance in adolescents with newly acquired spinal cord injuries. Ped Rehabil. (2005) 8:187–98. doi: 10.1080/13638490400021438
57. Langerhuus L, Miles J. Proportion recovery and times to ambulation for non-ambulatory dogs with thoracolumbar disc extrusions treated with hemilaminectomy or conservative treatment: a systematic review and meta-analysis of case-series studies. Vet J. (2017) 220:7–16. doi: 10.1016/j.tvjl.2016.12.008
Keywords: thoracolumbar intervertebral disc extrusion (TL-IVDE), disc herniation, neurorehabilitation, tactile-enhanced exercises, auditory-enhanced exercises
Citation: Lewis MJ, Bowditch J, Laflen B, Perry N, Yoquelet R and Thomovsky SA (2022) Pilot Study on Feasibility of Sensory-Enhanced Rehabilitation in Canine Spinal Cord Injury. Front. Vet. Sci. 9:921471. doi: 10.3389/fvets.2022.921471
Received: 15 April 2022; Accepted: 16 May 2022;
Published: 14 June 2022.
Edited by:
David Levine, University of Tennessee at Chattanooga, United StatesReviewed by:
Theresa Elizabeth Pancotto, Virginia Tech, United StatesCopyright © 2022 Lewis, Bowditch, Laflen, Perry, Yoquelet and Thomovsky. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melissa J. Lewis, bGV3aXM0NDRAcHVyZHVlLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.