
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Vet. Sci. , 26 April 2022
Sec. Veterinary Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fvets.2022.830098
This article is part of the Research Topic Sports Medicine and Physical Rehabilitation, Volume II View all 19 articles
 Conny Mosley1,2*
Conny Mosley1,2* Tara Edwards3
Tara Edwards3 Laura Romano4
Laura Romano4 Geoffrey Truchetti5
Geoffrey Truchetti5 Laurie Dunbar6
Laurie Dunbar6 Teresa Schiller7
Teresa Schiller7 Tom Gibson8
Tom Gibson8 Charles Bruce9
Charles Bruce9 Eric Troncy10
Eric Troncy10The Canadian consensus guidelines on OA treatment were created from a diverse group of experts, with a strong clinical and/or academic background in treating OA in dogs. The document is a summary of the treatment recommendations made by the group, with treatments being divided into either a core or secondary recommendation. Each treatment or modality is then summarized in the context of available research based support and clinical experience, as the treatment of OA continues to be a multimodal and commonly a multidisciplinary as well as individualized approach. The guidelines aim to help clinicians by providing clear and clinically relevant information about treatment options based on COAST defined OA stages 1–4.
Osteoarthritis (OA) is a challenging disease for veterinarians, patients, and pet owners. The chronicity and disease complexity require extensive education of the pet owner and a willingness to begin a treatment plan for their pet requiring multiple re-assessments over a pet's life dependent on disease progression. The situation is further challenged for veterinarians, as there are a multitude of potential OA treatments, but there is no clear differentiation or priority based on OA stage. It is these understood challenges that led to the specific aim behind the guideline development, to provide prioritized treatment guidance based on clinical experience, with consideration of the available scientific evidence, enabling the Canadian veterinary practitioner to treat and discuss OA based on the different OA stages.
The guidelines are the result of a consensus among a group of Canadian experts in the field of OA including board certified surgeons, anesthesiologists, sports medicine and rehabilitation practitioners, pharmacologist, and general practitioner. The panel members were asked by the lead author to participate in this project based on their clinical expertise, academic knowledge, and active participation in OA education in Canada. A focus for the selection of Canadian members was placed on diversity of fields of interest within OA treatment to represent the clinical, academic and collaborate approach. In the spring of 2021, the panel members virtually met with the goal of creating Canadian specific, OA treatment guidelines based on OA stage. To help frame the initial conversations of the panel, 5 different sample cases were provided ahead of the meeting, with each case representing a typical clinical presentation for the different COAST stage of OA. Each panel member reviewed the cases independently and submitted their approach prior to the meeting. During the meeting, the cases were used to focus the conversation on where treatment approaches were similar or different among the members, discuss specific aspects of the treatment and evaluate the treatment based on scientific support and clinical experience. In addition, topics or challenges that are encountered when treating patients with OA were discussed, i.e., how the panelists approach lowest effective dose, challenges in pain assessment.
After the case discussions finished, the panel moved on to discuss more generally, how to adjust the treatment approach based on the different COAST stage. Each treatment was then evaluated and voted on. In order for a treatment to be classified as “core” it required 9/9 agreement. Therefore, core treatment recommendations were unanimously agreed on to be included in any case with OA with specific nuances adjusted to the different stages and individual patient. If a treatment did not receive unanimous support, it was classified as secondary, and then further discussions occurred as to at what stage, and when the treatment should be considered. The secondary treatments received varying levels of support due to the often lack of available research for a particular treatment, and instead those in favor of the treatment, provided their clinical knowledge and experience. A consensus was reached for when to start the secondary treatment options based on the COAST stage, however, there was no priority assigned (which order to start treatment A, then B, etc.) and instead the treatments were simply grouped. Overall, the authors focused on available or soon to be available treatment options in Canada.
In human medicine, chronic pain guidelines are based on evidenced based medicine and therefore backed up by extensive scientific studies, that provide appropriate evidence. In veterinary medicine such work with clear evidence is unfortunately not available in chronic pain management. The limitations are mainly due to inadequate objective pain assessments, and knowledge gaps remain within most treatment options, despite many efforts from well-performed studies.
This review article summarizes the consensual guideline results, that were based on the shared opinions of the Canadian experts using evidence-considered treatment information and their own clinical experience. Compared to the classical evidence based approach adopted in human clinical guidelines, the scope of this review is therefore more narrow in focus, documenting the scientific, and clinical insights of the panel members. Within the description of each treatment option, a focus was placed on explaining the mechanism of actions and pharmacology of each treatment to increase the reader's knowledge and understanding of its benefits or limitations as a potentially effective treatment in canine OA. The literature citing reflected this focus.
Osteoarthritis is the most common joint disease affecting dogs. Most papers reference that ~1 in 4 dogs are affected (1–3), although it has been suspected that this number may be an underestimation due to this disease being underreported until later stages (3). It has to be mentioned that the actual original studies that continue to be referenced are either older, have a small sample size, or represent a very specific regional selection, among other limitations, and show a variety of OA prevalence results (4–6). Osteoarthritis is a disease of the entire joint organ with loss and dysfunction of the articular cartilage and is usually highly inflammatory in nature. Resulting changes will progressively impact all structures within the joint, including a thickened joint capsule with inflamed synovium and reduced viscosity of synovial fluid, damage to cartilage and subchondral bones, and development of osteophytes. The etiology of OA is complex with local mechanical as well as systemic and metabolic contributing factors (7–9). The chronic and progressive characteristics make it a challenging disease for clinicians to control. In addition, the treatment recommendations in the literature can be inconsistent and vague, and the clinical approach often varies among veterinarians. The individual case response, including both patient and client variability, adds to the complexity when making decisions for a treatment plan. The age of the dog and the different stages of the disease further impact treatment decisions and create more confusion due to inconsistencies in recommendations. When left untreated, OA can progress to a severe debilitating disease with significant functional impairment and pain sensitization. Early detection of OA and early treatments are considered important aspects in slowing down the progression of the disease and enhancing the quality of life (QoL) of the pet.
Regarding identifying the patient's stage of OA, the Canine OsteoArthritis Staging Tool (COAST) is a helpful diagnostic tool to assist veterinarians -with input from pet owners-, in recognizing and treating canine OA from its earliest stages (10). The tool provides clear guidance on how to decide on a dog's current OA stage based on owner input, orthopedic exam, and radiographic findings. The COAST stages include 0 (clinically normal, no risk factors), 1 (clinically normal, but OA risk factors present), 2 (mild OA), 3 (moderate OA), 4 (severe OA) (Figure 1). The descriptions of each stage are included in the category discussions below.
With OA, it is important to identify risk factors early in the disease and intervene before significant clinical signs occur, with the goal of preventing and/or slowing the progression (11). For consistency and to ensure clear definitions of each stage, these treatment guidelines are based on the COAST definitions of OA stages 1–4. We have not included Stage 0 as a stage that requires treatments but recognize that due to the high prevalence of OA in dogs, it is important for veterinarians to provide OA risk factor and prevention education at an early age even in this stage. The general education and Stage 1 discussion points also apply to Stage 0.
For all stages of OA, client education is fundamental. The veterinarian's role to educate owners on the disease (including pathology, risk factors, progression, stages, and identification and recognition of pain behaviors) is crucial. Education also includes relevant components like nutrition, specific diets, weight management, regular assessments, and therapeutic options (pharmaceutical, nutraceutical, physical medicine modalities, importance of exercise, lifestyle changes, and home improvements).
Osteoarthritis is a painful disease that results in limitations to the dog's ability and can progress to being severely debilitating. Education and empowering owners to recognize and identify the early signs of pain will help with early detection and treatment of the disease. Signs of pain in the later stages can help evaluate treatment response as well as its impact on the QoL of the pet. Signs in the early stages (Stages 1 and 2) can be subtle like asymmetric posture when standing or sitting, slight difficulties in rising or laying down, reluctance to jump into car, reluctance to play, young dogs not able to keep up with others, and difficulties with stairs. Pain in the later stages of OA is described below in their specific stage (Stage 3 and 4).
For general treatment recommendations, one common denominator in all OA stages is weight management (reaching and maintaining an ideal body condition score) (12–15). Obesity has been considered a high-risk factor for the development and progression of OA. Historically, this was ascribed to the excessive biomechanical joint loading on the articular cartilage, because of increased body weight, causing micro injuries and subsequent wear and faster breakdown. However, the association between obesity and OA in non-weight-bearing joints suggests a more complex etiology for obesity-induced OA. A more important part of the pathogenesis of OA could be the systemic and metabolic effects of obesity (inflamed adipose, dyslipidemia) (16, 17). Fat produces systemic inflammatory factors (cytokines and adipokines), which are specific adipose tissue-produced factors with significant inflammatory properties (18), which we presume from other species' extrapolation is also the case in dogs. The influence of adipose tissue attributing to low-grade systemic inflammation has been recognized and a weight loss program has shown both in humans and dogs to have general health benefits and potentially decrease and slow down the progression of OA in humans (19) and dogs (15), and is therefore considered by many an actual treatment option (20). Thus, an increase in body weight has been demonstrated to have negative effects on the osteoarthritic joint load (21) and maintaining optimal body condition should be one of the most important goals for any patient at any OA stage in the opinion of the panel. A specific effort should be made to educate and support owners in a weight reduction plan for their pet. This includes nutrition counseling for the right diet (weight or joint health focused or both), including both caloric and omega 3 fatty acid (FA) dose recommendations. This can also be used for a weight maintenance plan throughout the patient's life.
Dogs with OA require regular exercise. This is an important aspect of OA management for dogs. Exercise may be modified depending on the disease stage, but it is crucial that dogs with OA maintain a regular exercise plan that limits high impact and torsion to minimize joint trauma to help keep the joints mobile, cartilage healthy, and maintain muscle strength to support the joint (22–25). Historically “prolonged rest” was prescribed in cases with OA pain. This approach has the disadvantage that when a joint lacks movement, it will stiffen further (fibrosis) and decline cartilage health (26). A lack of exercise will contribute to muscle atrophy, thereby further reducing joint stability and contributing to pain (27, 28). The practice of severe activity restriction or rest is generally not recommended, instead regular, low impact exercise is an important part of pain management in OA. Regular physical activity is crucial to slow down the progression of sarcopenia and maintain physical fitness in dogs with OA (29), including the geriatric population. The specific type and frequency of exercise is dependent on the different stage of disease as well as the joints affected. Examples of low impact exercises could be frequent daily leash walks and a program with specific or targeted therapeutic exercises.
Recommendations for specific stages of the disease will be presented below and are useful starting points for most animals at each stage.
Serial monitoring of these patients is necessary, and treatment should be adapted according to the patient's response. Please note that multiple joints can be affected, and each joint may be in a different OA stage. There was agreement among the expert panel that targeting the joint with the worst OA stage will ensure an appropriate treatment plan for the patient. This was in agreement with the COAST reference of OA staging (10).
Please note, when reviewing the treatment guidelines, the below considerations may require adjustment of the therapeutic approach:
• Multiple joints affected requiring specific targeted therapies for an individual joint.
• Additional co-morbidities or concurrent medications present.
• Adverse events encountered in response to therapy.
• Surgical therapies were beyond the scope of the guidelines, please consider surgical interventions as appropriate for the patient.
Some of the suggested treatments are not licensed for the use in dogs or may have limited scientific evidence specifically for OA in dogs. It is the veterinarian's duty to make a risk:benefit assessment for each patient prior to administering any treatment and provide all relevant information related to the treatment.
Stage 1 refers to a patient that is currently normal (preclinical) but has risk factors for developing OA (10). Based on the COAST literature, our panel identified that risk factors may include a genetic predisposition, extensive, and longterm participation in injury prone activity, a joint injury or surgery, and excess body weight or age. A typical COAST Stage I dog would be a specific breed with atypical limb conformation either breed related (i.e., Basset Hound, Bulldog, German Shephard etc.) or congenital/traumatic deformities (elbow/hip dysplasia; giant breed dogs) that could cause abnormal joint loading. The treatment is focused on the prevention of the disease.
Provide adequate education to owners about the high prevalence and risks of canine OA as well as early recognition and clear prevention measures. Maintaining joint health is a priority in this stage. If a joint injury or surgery are contributing factors, the importance of effectively controlling inflammation and pain in the peri-and post surgical/injury time is imperative.
For Stage 1, client education begins with a strategy for growing puppies, including nutrition, weight management and exercise, as stated above. More specific education for this stage include education on the risk factors, as well as guidance for specific training and exercises for injury prevention. Owners of working and sporting dogs may especially need a reminder about the importance of regular musculoskeletal assessments for early recognition of OA.
In dogs with a higher risk factor for OA, a diet with focus on joint health is ideal to ensure that the dietary ingredients included support the musculoskeletal system. In particular, omega 3 FAs have shown to be effective in reducing the signs and progression of OA (30–38), although it is important to provide adequate dosing (39). Most joint health focused diets have omega 3 FAs at varying dosing ranging from 0.59 to 10.11 g/1,000 kcal, with many brands being under 3.5 g/1,000 kcal (40). It is imperative to identify the actual eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) concentrations in the food, as not uncommonly alpha lipoic acid (ALA) is used in foods for its omega 3 FA content. As described below ALA is not an adequate substitute and food should quantify actual levels of DHA and EPA. In most cases, additional DHA/EPA supplementation is required to reach the scientifically recommended minimum dose of 100 mg/kg daily DHA/EPA (32). The type of omega 3 FA supplementation for adequate conversion to DHA/EPA should be based on current scientific evidence. The precursor of DHA/EPA in plants is ALA. The conversion rate from plant-based ALA to EPA is significantly less than from fish/marine based oil and a full conversion from ALA to DHA does not occur, only to its precursor docosapentaenoic acid (DPA) (41, 42). Higher conversion rates with significantly more reduction of inflammatory markers were found with fish/marine based oils. In some patients, the joint health focused diet may need to be assessed for calories to reflect weight management goals and activity levels. Weight optimization is recommended throughout the patient's life as mentioned above.
Depending on the risk factors for the dog, a rehabilitation veterinarian can be sought out to discuss disease prevention, strategies to slow down progression of disease, and recommend therapeutic exercises to promote strengthening of muscles supporting joints. For an athletic or service dog, adequate training tips for injury prevention may be beneficial (i.e., focusing on strength, endurance, proprioception, limiting repetitive, and concussive activity). For a dog with a genetic or breed specific predisposition, specific exercises could be useful to implement into daily activities (43).
These consults by a veterinarian or rehabilitation practitioner may also include lifestyle and household modifications, for example, daily exercises (including walks, swims) or household modifications (early teaching of a young Dachshund not to jump on and off a sofa, adding in a step stool, improving flooring traction, etc.).
A summary of stage 1 treatment recommendations is provided in Table 1.
Stage 2 refers to the early clinical stage of osteoarthritis that results in mild clinical signs. Those signs can be inconsistent and subtle, can occur with some activities or after activities, may affect the gait and show subtle changes/shifting in body weight distribution and limb loading. Range of motion (ROM) of a certain limb/joint may be minimally reduced, but crepitus is unlikely at this stage. Minimal osteophytes and early signs of OA may be visible on diagnostic imaging (10).
The treatment goals at this stage are supporting the preservation of healthy cartilage and treating flare ups promptly and effectively. Providing owner education on recognizing signs of OA and importance of early as well as longterm treatment can be teadious, but is needed for the desired compliance.
Client education encompasses all points mentioned in the general treatment recommendation section as well as the Stage 1 specific education points.
A joint health focused diet and weight optimization are recommended as mentioned in the general section. DHA/EPA at a minimum of 100 mg/kg daily dose should be included within the diet or additionally supplemented.
Further important Stage 2 discussion topics include the progression of OA from mild to moderate stages, the importance of regular orthopedic assessments and monitoring response to therapy, as well as developing an exercise program suited for the patient. Daily exercise is necessary and should be low to moderate impact, for example walks, swims or specific physical exercises as recommended (43, 44). Exercises with high impact or torsion, like ball throwing, should be avoided. A specific fitness and exercise plan is necessary to be set in place for working dogs that require to return to work. This plan would be based on the type of work, the type of joint/dog concerns, and should focus on further injury prevention.
A consultation with a rehabilitation practitioner (when possible) would be beneficial to identify factors that may contribute to the faster progression of the disease and help with tips on how to decrease risk factors and optimize muscle strength, posture, proprioception, and gait. An initial assessment of gait, weight bearing, transitions, posture, body condition score, muscle condition score, ROM, and pain scoring provides a baseline evaluation of musculoskeletal health. Understanding what areas need improvement allows for a more individualized treatment plan. Targeted therapeutic exercises may focus on core strength and posture, maintaining or gaining ROM, improving overall physical fitness, and strengthening the musculature that is required to provide stability for arthritic joints (28, 45). Specific exercises should be prescribed depending on location of arthritis, concurrent illness, pain level, temperament/trainability of the dog, physical limitations of the owner, physical strength and endurance of the dog, home environment (i.e., condo vs. farm dog) and it is beyond the scope of this paper to address the multitude of situations. In addition, there are many options including manual therapy, physical medicine modalities, and rehabilitation equipment that can be utilized to treat and manage the arthritic patient. A rehabilitation program at this stage may include a combination of both specific home exercises and a formal in-clinic rehabilitation program.
As part of the client education or the rehabilitation consult, lifestyle and household modifications should be included at this stage. These may incorporate modifications in the house (stairs, flooring) or car (adjusted jumping out or in) to prevent high impact injuries and start learning/switching habits for future mobility concerns.
For pain management, the use of non-steroidal anti-inflammatory drugs (NSAIDs) is warranted for this stage, as a patient is demonstrating clinical signs. Due to the inflammatory nature of OA especially at the early stage (46, 47), NSAIDs play a significant role in decreasing the pathogenesis of peripheral sensitization. Prostaglandins (PG), in particular PGE2, are one of the main inflammatory mediators in arthritis and will contribute to the transition from acute to a maladaptive chronic pain state when untreated (48, 49). Therefore, NSAIDs are considered to be the cornerstone of rheumatoid arthritis and OA treatment, providing effective pain relief, especially in this initial clinical stage by inhibiting cyclooxygenase (COX) activity and subsequently blocking the production of prostanoids, including PGE2 (50, 51). When the production of this prostaglandin is increased in response to an inflammatory event, PGE2 is more readily available to bind to its specific receptor [E-type prostanoid receptor 4 (EP4 receptor)] on the presynaptic side at the site of inflammation, resulting in a pain signal to be sent across the synapse and subsequently travel up the pain pathway. Without interference and continuing phasic and/or static nociceptive input, the constant stimulation from PGE2 via the EP4 receptor pathway will lead over time to an increase in the sensitization of sensory neurons. The EP4 receptor will be upregulated in a prolonged state of inflammation (52). Upregulation means that the receptors are in a higher state of alert and increase in number. This constant activation results in further pain and increased inflammation. The ability to dampen the receptors (piprant class NSAID) or decrease available inflammatory prostaglandins (COX-2 selective inhibitory NSAIDs) will decrease the pain sensitivity and contribute to limiting sensitization (49), that could lead to chronic maladaptive pain.
The response to NSAIDs can be individual and the right fit regarding efficacy, adverse events, and predicted duration of use should determine the choice of a specific NSAID for the patient. Considering the importance of NSAIDs in the disease of OA, sometimes a patient may need to switch to a more suitable NSAID after the appropriate washout period (53, 54).
For dogs, this panel all agreed on a NSAID trial for a minimum of 4 weeks at product's labeled dose. The minimum of 4 weeks is recommended to allow for an adequate decrease of inflammation (55). Improvements of clinical signs may show earlier than 4 weeks, but the consensus is to treat for the full duration of the NSAID trail to resolve the inflammation on a cellular level. As most adverse events commonly occur in the early phase of initial treatment, a “check-in” call after 1 week to discuss the patient's tolerance and acceptance of the medication is recommended. After the 4-week trial, the patient should be reassessed clinically and, based on therapeutic response, the treatment can be continued or discontinued as appropriate. Not uncommonly it is recommended to continue NSAID therapy long-term to allow for effectively treating the underlying inflammatory nature of OA at this stage. With long-term NSAID use, bloodwork is recommended with a baseline CBC/Chemistry prior to initiating NSAID treatment and then every 3–6 months as needed, unless concerns about the health of the dog arise earlier.
“Flare-ups” (also known as “acute-on-chronic-episodes”) can occur because of activity, injury, weather, and should aim to be minimized (56). In the occurrence of a flare up with clinical signs, if NSAIDs are not currently being used in the patient, a trial should be most strongly considered to keep the inflammation at a minimum as currently the only product proven to be effective to achieve this are NSAIDs. Median duration of flare-ups was reported in humans to last 5 days (56). In dogs, our recommendations for the NSAID treatment during an aggravated, more obvious painful period, would be at a minimum of 3–5 days -or longer- until resolved, with the oversight of a veterinarian. A patient with re-occuring flare-ups should remain on long-term administration of NSAIDs to reduce inflammation, that will lead to sensitization and maladaptive pain. The benefits of a more chronic NSAID dose regimen outweighs the perceived risks (54). Owner education on this aspect is necessary to negate potential reservations and increase compliance.
Similar to the above, patients should always be assessed for improvement and monitored for any potential adverse events.
Within stage 2, there is a high variability in case presentation. Depending on the presenting clinical signs, secondary treatment options should be tailored to each individual patient on a case-by-case basis. No consensus was reached among the panel members on specific treatment recommendations due to limited evidence and differing clinical approaches resulting from the inconsistency of case presentations. Nevertheless, due to the progression of OA, the development of chronic pain, or acute on chronic flare ups, adjunctive pain medications or treatment modalities may be required. Physical medicine modalities that focus on reducing inflammation and managing pain are suggested to be considered on an individual basis (i.e., photobiomodulation, pulsed-electromagnetic field therapy (PEMF), acupuncture, cryotherapy). Implementing a long-term joint health plan with chondroprotective products is aiming to slow down the progression of the disease, but scientific evidence of efficacy for canine OA is currently still limited. The choice of recommeded chondroprotective product is dependent on the specific case presentation.
A summary of stage 2 treatment recommendations is provided in Table 2.
Stage 3 refers to the clinical stage of OA that results in moderate clinical signs and moderate signs of discomfort. Those signs are more consistent and obvious at all gaits and activities, with consistent clinical abnormalities. There are noticeable changes in body weight distribution and limb loading and obvious reduction in use of affected limb(s). Some difficulties in rising or laying down are present. A decrease in ROM is present and muscle atrophy can be seen. Joint thickening may be noticeable. Obvious osteophytes and signs of OA are likely evident on diagnostic imaging (10). This is the stage that most dogs are presented for orthopedic and/or pain evaluation.
At Stage 3, the treatment goals are an individualized and effective treatment of these multi-facetted pain states and maintaining a tailored level of mobility for the specific patient based on both patient and client. This includes specific interventions aimed at slowing the OA progression and mobility decline.
Client education includes all the topics mentioned in the general treatment recommendations for nutrition, weight management, exercise, and regular reassessments.
Specific focus points for education at Stage 3 would be the progression of disease, impact on quality of life, and appropriate pain management. The importance of regular assessments should be emphasized to allow for tracking musculoskeletal changes and response to treatment. Individualized home exercise programs, lifestyle adjustments, and household modifications will require adjustments over time.
At Stage 3, a formal rehabilitation program designed by a rehabilitation practitioner is highly recommended if logistics allow. Rehabilitation can ensure appropriate assessment and treatment of pain on a regular basis, aiming to slow down the disease progression with a focus on mobility. A rehabilitation partnership provides support to owners for their dog's debilitating disease. This support can include QoL assessments and discussions. A rehabilitation team will create an individualized program for the patient that may include targeted therapeutic exercises which focus on core strength and posture, maintaining or gaining range of motion, improving overall physical fitness, and strengthening the musculature that is required to provide stability for arthritic joints (44). A rehabilitation team should use the fundamentals of rehabilitation to create a long-term rehabilitation plan that considers the dog's and owner's desired lifestyle. The plan should be patient-centric and based on canine physiological and scientific principles. The dog's initial presentation and progress is based on individual assessment. It must address the degree of tissue damage and healing, pain experienced in rest and during exercise, strength, and desired functional goals. An understanding of the phases of tissue healing, frequent patient reassessments, and clinical reasoning skills to progress treatments appropriately for the individual patient are the cornerstones of a successful rehabilitation program (57). A rehabilitation program at this stage often includes a combination of a home exercise plan in addition to a formal in-clinic rehabilitation program. Effective pain management is the fundamental basis for a successful rehabilitation program and contributes to patient compliance and owner motivation.
Lifestyle and household modifications play an important role at this stage to prevent injury and improve QoL by simplification of obstacles. Examples may include ramps for easier access to stairs/car, baby gates to block off stairs for prevention of falls/injuries, carpet runners or yoga mats over slippery floor to prevent slipping, well-padded dog beds for easier comfort, improved traction with nail covers or grips to prevent slipping and dragging toes, assistive devices such as special harnesses (Help'emUp harness) for improved mobility. Adequate nail trimming is also an underestimated tool to assist with proper biomechanics and appropriate alignment. Improving traction and reducing risk of slipping is further achieved by appropriate trimming of foot fur to allow for pads contacting the floor.
For pain management, the use of NSAIDs is highly recommended at this stage. NSAIDs are the cornerstone of providing adequate anti-inflammatory therapy for OA (54). The initial protocol is very similar to the stage 2 NSAID description. However, if the response of the 4-week trial is showing favorable results for the pet, the use of NSAIDS will most likely be required on a long-term basis. Most dogs tolerate the long-term use of NSAIDs well, although regular wellness visits, bloodwork, and treatment reassessments are needed.
Long-term use of NSAIDs may produce some questions or concerns from both owners and veterinarians (54, 58). NSAIDs have proven the most effective medication for OA but administration does carry the potential risk for adverse events (gastrointestinal, renal) in particular with patients with pre-existing risk factors. Most common adverse events described in dogs appear to be gastrointestinal related and that is a common cause of concern for veterinarians and pet owners alike (53, 54, 58). In human medicine, it has been recommended to use the lowest effective dose for the shortest time possible (59), but the challenge with this recommendation is the risk for suboptimal pain relief with non-verbal patients in veterinary medicine. One study evaluated the efficacy of ketoprofen at lower than label dose in an acute experimental inflammatory model using a weight bearing assessment tool with results showing analgesic efficacy compared to the control group (60), but overall clinical studies are limited addressing the dose reduction approach. Concerns are that lowering the dose can be quite problematic, considering the limitations of owners (and veterinarians in clinic settings) to adequately assess pain, specifically subtle changes. The need for studies assessing if using concurrent medications that may work synergistically with NSAIDs due to similar pathways are needed to evaluate the potential for dose reductions. A canine study on the non-selective COX inhibitor ketoprofen (61) showed that reducing the recommended NSAID dose by 75%, significantly reduced the measured side effects (glomerular filtration rate, gastro-intestinal lesions) but not platelet aggregation changes, and the reduced dose did provide some OA pain relief, although this was improved in conjunction with tramadol (5 mg/kg/day PO, slow-release formulation). The comparison of pain scores to the group given ketoprofen at the label dose was unfortunately not presented. A similar dose-reducing study compared a reduced dose of meloxicam (62) to the recommended label dose, and it concluded that the adequacy of pain control was lower with the reduced dose. This study gradually reduced the dose over time (15% reduction) every 2 weeks. Only the first 15% reduction was tolerated by the majority of the dogs (87%), while further reduction revealed inadequate pain control in some dogs (62). This led the authors to conclude that a small dose reduction may maintain efficacy but does not seem to be consistent and appears to be based on individual responses. This may be difficult to differentiate clinically and will require the owners' ability to appropriately assess pain. The study found minimal adverse events in the recommended label dose group of the study over a period of 100 days. See Table 3 for OA approved NSAIDs in Canada.
Although all approved NSAIDs in Canada provide recommendations to utilize the lowest effective dose, assessing the adequate efficacy for appropriate pain control remains a significant challenge. Utilizing client-based questionnaires, e.g., Liverpool Osteoarthritis in Dogs (LOAD), can help raise owner's pain recognition awareness and aid in assessing the response to treatment (63).
Secondary treatment options are often needed at stage 3 and 4 due to the difficult characteristics of OA pain. Depending on the presenting clinical signs, secondary treatment should be tailored to each individual patient on a case-by-case basis. The pain experience is unique for every individual, as is their response to treatment(s). Factors including a patient's personality, receptor genetics, metabolism, and degree of peripheral and central sensitization, which all serve to emphasize the importance of tailoring treatments to an individual patient.
The multimodal approach can be confusing due to the multitude of options, limited evidence in some instances, and the high variation in individual response in efficacy.
No unanimous consensus was reached among the panel members on secondary treatment recommendations due to limited or variability in evidence, therapy available and differing clinical experiences.
Instead, a summarized review of the most common secondary treatment options are provided.
The order of what, when and how to introduce a new secondary medication or modality to the multimodal approach is dependent on the individual dog, owner, veterinarian, and availability (of modality). In this following section a brief summary of options for Stage 3 specific is provided (with more detailed description of those treatment options listed below the Stage 4 category as all options may be relevant for both Stages 3 and 4).
• Gabapentin or pregabalin are usually added as a second line treatment based on the clinical experience of some panel members, when the core treatments are not sufficient to control the patients clinical signs. The evidence for the use of gabapentin (or pregabalin) for OA is limited to non-existent, although it is considered a good additional medication when a neurogenic/neuropathic component is expected (see detailed description in appendix, including the advantages of pregabalin over gabapentin).
• Photobiomodulation (64) and acupuncture (65) are considered appropriate modalities to support the multimodal therapy approach based on subjective outcome measures and clinical experience of some panelists; see detailed description in appendix.
• Some panelists would consider joint injections with platelet rich plasma (PRP) or hyaluronic acid (HA)/triamcinolone at this time if a particular joint is refractory to treatment (66–68).
• Some panelists would consider cannabinoids at this time with veterinary oversight for close monitoring and appropriate selection of a suitable quality product (69, 70).
A summary of stage 3 treatment recommendations is provided in Table 4.
Stage 4 refers to the advanced stage of OA in which patients demonstrate significant clinical signs and a higher level of dysfunction and pain. The signs are obvious, constantly present, and are significantly affecting the QoL of the dog. Those signs include severely abnormal limb loading and shifting of weight distribution with a reluctance and restlessness when standing; significant lameness with a reluctance to move and marked difficulties in rising and laying down. A limited ROM with crepitus, joint thickening, anatomical misalignment, and advanced muscle atrophy can be seen. Diagnostic imaging will show advanced osteophytes and signs of bone remodeling (10).
At Stage 4, the treatment goals are often very individual to effectively treat the multi-facetted pain states and often require a tailored level or expectation of mobility for the specific patient based on both the patient and client. The focus in this stage is the continuing assessment and adequate improvements/maintenance of QoL, including support for both owners and patient.
Client education includes all the topics mentioned in the general treatment recommendations for nutrition, joint health focused diet, omega 3 FA, weight optimization, exercise, and regular reassessments. Stage 3 specific education recommendations also apply. Specific Stage 4 focus points for education would be the impact on QoL as the disease progresses, as well as the importance of appropriate pain management and pain assessments. Regular orthopedic assessments should be emphasized to allow for tracking musculoskeletal changes and treatment results. Muscle wasting is a large concern especially for seniors that are already challenged with sarcopenia (29). Maintaining and possibly building muscle mass is one of the priorities for these patients. Creating a regular exercise and activity schedule that can be modified depending on the health of the dog is crucial. Regular, short, but frequent, low impact walks, and exercise (to tolerance of patient) even at this advanced stage are very important for preservation of mobility, physical and mental health.
At Stage 4, a formal rehabilitation program designed by a rehabilitation practitioner is highly recommended if logistics allow. Rehabilitation can provide assessments and discussions about QoL as well as appropriately assess and revise the pain management plan in collaboration with the family veterinarian. The owner often requires advanced lifestyle and home modifications to adjust to their pet's level of disability. Based on the same principles described in Stage 3, a rehabilitation team will create an individualized program for the patient that may include targeted therapeutic exercises which focus on core strength and posture, maintaining or gaining range of motion, improving overall physical fitness, and strengthening the musculature that is required to provide stability for osteoarthritic joints. This often includes a combination of a home exercise plan in addition to the formal in-clinic rehabilitation program and considers the lifestyle and ability of the owners.
Lifestyle and household modifications play an important role at this advanced stage and are similar to the modifications mentioned in Stage 3. These modifications focus on preventing any slipping and injuries and providing more comfort for the dog to ensure that QoL is maintained. Examples are the same as in Stage 3 with the addition of assistive mobility devices that may be helpful based upon the individual case situation. Supporting ongoing environmental enrichment and promoting the human-animal bond plays a role here.
For pain management the use of NSAIDs continues to be most highly recommended at this stage to keep the patient comfortable. If no co-existing diseases are present, lifelong administration is necessary. As patients are often older at this stage of disease, it is important to continue to monitor for the development of other diseases (kidney, liver, cancer) by regular bloodwork assessments and physical examinations. When NSAIDs are initiated, the same protocol as described in stage 2 and 3 applies. Other anti-inflammatory options may need to be discussed when dogs at this advanced stage have co-existing disease that prevent regular NSAID use. A discussion with owners may be initated to address QoL with aspect of efficacy of NSAIDs over risks of adverse events when no other treatment options provide adequate pain relief to prevent suffering of the animal.
Anti-NGF monoclonal antibody (mAb) is not yet available in Canada at the time of the preparation of this document, however we have included it in the guidelines due to its recent Canadian label approval (Feb 2021). Anti-NGF mAb has demonstrated potential in research and there has been clinical experience in the European market for use in late-stage OA (71–75). Nerve Growth Factor (NGF) and inflammatory mediators (cytokines, prostaglandins, etc.) play an important role as pain initiators and nerve sensitization in chronic pain (50, 76, 77). NGF is largely responsible for the neurogenic inflammation component in chronicity and severity of pain and, it regulates pain through nociceptor sensitization. The mechanisms of NGF on the pain signaling pathway are complex, involving various other receptors and are in parts responsible for the development of neuropathic pain and pain modulation peripherally and in dorsal root ganglion. Anti-NGF mAb blocks NGF from binding to the tropomyosin-related kinase receptor (TrkA) and p75 neurotropin receptor (NTR), subsequently inhibiting the pain signaling pathway potentially treating and slowing down peripheral nerve sensitization (78–80). It has shown to provide OA pain relief over the period of about 4 weeks after a single subcutaneous injection. The safety profile of bedinvetmab, the first anti-NGF mAb to be commercialized for dogs, appears to be high (75). Mild reactions at the injection site (e.g., swelling and heat) may uncommonly be observed. There are no safety data on the concurrent long-term use of NSAIDs and bedinvetmab in dogs. In clinical trials in humans, this has been reported as a potential source of rapidly progressive OA, the incidence increasing with high doses and in those human patients that received long-term (more than 90 days) NSAIDs concomitantly with an anti-NGF mAb (81). Dogs have no reported equivalent of the human rapidly progressive OA.
Once available, Anti-NGF mAb would be recommended as a core treatment for Stage 4 in particular (and possibly earlier) if the pain is refractory to treatment, suggesting that a neurogenic component from nerve hypersensitivity is present. The potential for Anti-NGF mAb to specifically treat the neuropathic or neurogenic component is promising and can be well-incorporated into a multimodal approach. A recent multicentre prospective efficacy study in clinical canine OA patients showed promising results as an additional option in the treatment of pain with seemingly remarkable safety profile. After 3 months of comparative study between a placebo (n = 146) and bedinvetmab (n = 141) with a treatment success rate (as defined by study criteria) varying from 50% (day 14) to 67.9% (day 56), the treatment success rate stabilized at about 75% over the continuation phase (up to day 252) (75). Clinical experience in the future will give more insights into this medication for OA in dogs as part of a multimodal treatment plan.
Secondary treatment options are usually needed at Stage 3 and 4 due to the difficult characteristics of OA pain. The pain experience is unique for every individual, and accordingly as is their response to treatment(s). Factors including a patient's personality, receptor genetics, metabolism, degree and mechanisms of peripheral and central sensitization, which all serve to emphasize the importance of tailoring treatments to an individual patient.
However, the multimodal approach can be confusing due to a number of factors. Often the sheer number of treatment options can present challenges, the wrong application of therapies, a lack of understanding of the mechanismus of pain or modality, limited evidence, and the high variation in individual response in efficacy.
Most of the secondary treatment options could be considered in stage 3 or 4, as the order on what, when and how to introduce a new medication or modality to the multimodal approach is dependent on the individual dog, owner, veterinarian, and availability (of modality).
As mentioned previously, the secondary therapies did not receive unanimous support from the panel, the lack of support or difference in opinion often arose due to concerns in prioritization, variability or lack of scientific evidence, lack of experience with therapy and lack of clinical experience. Thus, each treatment below is presented in the context that limitations are present, and thus using clinical judgement to conduct a risk:benefit analysis for therapy is important prior to using it in a patient.
In this section a brief summary of options for Stage 4 specific is provided. The secondary treatment options recommended at Stage 3 apply and may have already been introduced.
• If gabapentin has been ineffective, a switch to pregabalin can be made based on clinical experience.
• After introducing pregabalin/gabapentin in Stage 3 in cases with presumed neurogenic/neuropathic hyperexcitability component of the pain, some panelists turn to amantadine as a third line treatment option. Evidence for efficacy in OA is limited, the only paper available provides questionable evidence of its effectiveness (82). Nevertheless, the mechanism of action of blocking the NMDA receptor may warrant its use in cases with pain hypersensitivity in conjunction with other pain medications. With similar evidence, tramadol can also be considered in association with an NSAID (61). See detailed description below.
• Some panelists would maintain photobiomodulation, acupuncture and PEMF therapy as supportive modality in the multimodal approach. See detailed description below.
• Some panelists would consider joint injections for joints that are refractory to treatment. See detailed description below.
• Some panelists would consider steroid epidural if indicated, especially for severe lumbosacral pain in conjunction with significant hind-end weakness. See detailed description below.
• Some panelists would consider starting or continuing cannabinoid medicine with appropriate veterinary oversight. See detailed description below.
• Some panelists would consider shockwave therapy (83, 84) as an added physical therapy modality. See detailed description below.
• Even though surgical intervention (arthroscopy, arthrodesis, etc.) was beyond the scope of this article, it is important to note that it may be warranted and considered in some cases of both Stage 3 and 4 to provide the needed relief of discomfort, following full recovery from said surgery. An informed discussion of the impact of surgery on both advantages and potential risks and disadvantages (including slower and less comfortable recovery period) is necessary, when performing surgery on an already heavily sensitized joint in a COAST OA stage 4 dog.
A summary of stage 4 treatment recommendations is provided in Table 5.
The below information entails Stage 3 and 4 secondary treatment options with more detailed information including MOA, supporting literature and dosing information. They are grouped in categories and not ranked in preference of treatment.
Gabapentin is often used as a second line treatment in chronic pain, including OA, in conjunction with NSAIDs, and is commonly added when a neuropathic pain component is suspected (85). The complete mechanism of action of gabapentinoids (gabapentin and pregabalin) has not been fully elicited, but its primary mechanism of action involves the presynaptic inhibition of voltage-gated calcium channels, which in turn blocks calcium influx, that would have led to the release of excitatory neurotransmitters. Due to the inhibition of the excitatory neurotransmitters, there is a decrease in pain signaling across the synapsis. Voltage gated calcium channels (VGCC) are upregulated in a chronic neuropathic state and gabapentin may influence the number of available and active calcium channels. Gabapentin has other, less understood mechanisms of action. These mechanisms are the antagonism of (but not direct binding to) the N-methyl-D-aspartate (NMDA) receptor, also known to be a calcium channel when activated. The antinociceptive effects of gabapentinoids have further been described to be associated with the noradrenergic and serotonergic activity via the descending pain pathway (86, 87). For dogs, there are no currently licensed veterinary products in Canada. Studies on efficacy of gabapentin for pain have been disappointing, as the evidence that gabapentin is efficacious to treat pain, in particular inflammatory pain, is low. Clinically it has been noted that gabapentin seems to show better effects when the patient has a neuropathic hyperexcitability component to their pain (significant central upregulation or nerve related pain). Dogs in late-stage OA commonly have a neurogenic inflammatory and central sensitization component and may exhibit back pain due to posture abnormalities and muscle atrophy related to the ongoing OA. The role of both gabapentin and pregabalin would theoretically reduce those components (88), but the evidence for the clinical efficacy has yet to be proven for OA. Recommended dosing is controversial and may depend on age and health status of the dog as well as co-administered medications. A pharmacokinetic (PK) study in greyhounds after a single dose administration concluded a dose of 10–20 mg/kg TID is required to reach plasma levels that compare to adequate levels for pain relief in humans (89), but no canine studies have been able to establish the plasma levels that provide analgesia or the PK results after long-term use. Clinically a 5–10 mg/kg TID dose prevents the unwanted side effects of significant ataxia, sedation, and urinary incontinence. Even though these side effects may be transient, they commonly affect an owner's compliance, and the panel members generally refrain from escalating doses beyond this, in particular in older dogs with pre-existing hind end weakness. Gabapentin is rarely used as a sole analgesic in veterinary medicine, and until there is better efficacy data, it should be used based on an individual assessment as part of a multimodal regimen.
Pregabalin is the gabapentinoid, that has preferable PK and pharmacodynamic (PD) profile over gabapentin (90). The oral bioavailability and duration of action is superior to gabapentin, and the binding to the delta subunit of the voltage-gated calcium channel is stronger, showing higher efficacy in humans (91). The recommended dose based on a canine PK study is 3–5 mg/kg BID (90). In conjunction with an NSAID, pregabalin (and presumably gabapentin) appears to be more effective in human OA studies addressing both the inflammatory and central neuropathic aspects of chronic OA (92). Beyond the recommended dose, pregabalin can have similar side effects as Gabapentin in older dogs.
Amantadine was considered as a third line treatment in refractory pain cases by the panel. Amantadine is an NMDA receptor antagonist and has the potential to be effective in reducing the wind-up effect in patients that show signs of central sensitization (refractory pain despite treatment, sensitive to touch). However, based on the current understanding of the mechanism of action, it does not likely work as a sole analgesic, and is usually recommended to be used in conjunction with an NSAID. Currently there is only one study assessing the efficacy of amantadine in OA pain in dogs (in addition to meloxicam, at a dosage of 3–5 mg/kg SID PO), and it showed incomplete and questionable beneficial treatment effects with a 3 week delay in onset (82). The current dose recommendations for dogs are 3–5 mg/kg BID which are based on a combination of a PK study that involved five Greyhounds (93) and extrapolations from human data. Due to the shorter T1/2life in dogs, the historically suggested once daily dose has been adjusted to twice daily (every 12 h) in dogs (93, 94). The PD effects, in particular the efficacy for pain, and adequate plasma levels that would be needed for analgesia have not been established and therefore the evidence for the use of amantadine as a pain medication in dogs with OA is low to non-existent. A study to determine the effectiveness of amantadine for pain in veterinary species is needed. Side effects are usually reduced appetite or vomiting, which in parts may be due to the bad taste of the formulation.
Acetaminophen has been infrequently suggested as a pain medication for dogs with OA. Under the name paracetamol it is more commonly used in Europe. Acetaminophen has a unique mechanism of action related to the endocannabinoid system (ECS). It produces a metabolite (N-arachidonoylphenolamine), which inhibits the enzymatic (FAAH) breakdown of anandamide, inhibits COX1 & 2, and is a TRPV1 agonist. This metabolism pathway may be species-specific and dose dependent but is a promising therapeutic avenue and reflects the interaction of the ECS in a variety of mechanisms of action of pain medications. Clinically human studies repeatedly suggest NSAIDs are superior for pain relief in OA (95) concluding acetaminophen to only play a role in the early-stage mild OA pain relief. Experimental research with induced synovitis study in dogs confirmed that the NSAID carprofen was superior to an acetaminophen-codeine product and that both the PK and PD of acetaminophen may not be sufficient for adequate pain relief and improvement of function (lameness) (96). It has to be noted that the study focused on the anti-inflammatory capacity of both treatments over a very short period of time (9 h) in a chemically-induced model. A long-term clinical study in dogs with OA would be needed to gain more insights, including its side effects and potential long-term effects on liver.
Tramadol. The role of tramadol in treatment of chronic pain has been controversial. Its mechanism of action in dogs is mainly via the descending pathway by means of norepinephrine and serotonin re-uptake inhibition. This descending pathway does play an important role in modulating the ascending pain signals. Tramadol seems to have a lack of measurable efficacy for OA in dogs as a sole agent (97, 98). In both studies, the duration of treatment was unusual short and the OA stage advanced (radiographically present) [10 days: Budsberg et al. (98); 14 days: Malek et al. (97)]. The analgesic efficacy of a NSAID-tramadol combination looked more advantageous over a 4-month period, including a 4-week daily initial regimen administration (61). The PK profile of tramadol is also not ideal in dogs (99), making a slow-release formulation (5–10 mg/kg PO daily) more attractive. Long-term use has been reported to have a decrease in effect (94). The concerns of gastric adverse effects in conjunction with NSAIDs due to the serotonin modulating gastric acid secretion and contributing to gastric lesions, have been assessed with no evidence to detect any deleterious effects (61, 100). Further studies are needed to investigate the effects of tramadol, as there may be emotional benefits contributing to pain control and QoL through the serotonin/dopamine and norepinephrine pathways (requiring more exposure to treatment to induce changes). These pathways on the other hand may also contribute to the negative behavioral side effects that one may see in some (senior) dogs. Based on current literature, tramadol plays a minimal role in the treatment of OA in dogs. More research is needed to further assess tramadol and its role in chronic pain in dogs.
With the recognition that pet owners are increasingly looking for botanical and “more natural” treatment options, as well as an increase in interest from the scientific veterinary community in the nutritional and medicinal use of herbal medicinal products, the expert group felt it important to include products and ingredients that have appropriate studies and evidence for OA treatment (101, 102). The list is not complete but includes some of the more common product groups.
It is important to recognize that nutraceutical combination products fall under the category of Animal Health Products, which are very differently regulated than the pharmaceutical industry (103), currently not requiring research or safety studies, but also cannot claim therapeutic benefits. When considering a specific product, it is important to assess specific ingredients and their concentrations. A certificate of analysis can be obtained, that shows a product is free of contaminants like residual solvents, heavy metals, microbials, pesticides, or fungus. Ideally a company can also be transparent about quality of product, source of ingredients and manufacturing standards. A natural product number (NPN), that is provided for a licensed natural health product assessed by Health Canada to be deemed safe, effective and of high quality, adds to assurance of quality. To date there is little information about the stability of products, ingredient interaction, bioavailability or PK profile, including dosing for most natural health products (103). Another area of needed research is the effects of using certain nutraceutical products together with other nutraceutical or pharmaceutical products, especially when the mechanism of actions works on similar pathways or receptors, or the metabolism is impacted. In general, a synergistic or additive effect is presumed, but scientifically not established for most products. Close monitoring for efficacy and adverse events is recommended as has been previously suggested for multimodal pain management.
b.1 Cannabinoids. The endocannabinoidome system is involved in almost all aspects of the ascending and descending pain pathway at all major signaling points including the periphery, spinal cord and CNS. The endocannabinoidome system extends from the ECS system (receptors (CB1 and 2), enzymes and ligands) to other classic receptor systems that are part of the pain pathway (opioid, TRPV, serotonin, prostaglandins, etc.). Cannabinoids have been shown to play a role in neurogenic and inflammatory pain by a variety of mechanism of actions on various receptors and pathways (104). The use of cannabinoids in veterinary medicine is still relatively new, nevertheless there have been multiple clinical trials published that show promising results for its efficacy for pain relief of OA (70, 105–110). The existing studies conducted have been product specific, in that the researched product has a specific cannabinoid and terpenoid profile. Unfortunately, this makes it challenging to extrapolate and interpret the results of PK and PD toward other comparable products (69, 70, 107, 111). The safety profile needs further investigation, particularly with regards to causes of liver enzyme elevation and its effects on liver function (107, 110). Current regulations in veterinary medicine make it difficult for veterinarians to support owners with finding a consistent product that can be safely used in their pet. From clinical experience, a cannabidiol (CBD) isolate product may not provide adequate pain relief in moderate to severe OA cases but can be useful in mild cases (110, 112). A full spectrum CBD|THC product has been shown to be more effective in advanced pain cases based on the nature of pain (inflammatory, immune-mediated, neurogenic). The role of THC/THCA and CBD/CBDA as a CB2 receptor agonist in more severe or immune mediated pain is still to be further investigated in dogs but would presume to play a role based on research from other species (113–115). Like other medications, cannabinoids used for OA pain should be accompanied by regular wellness evaluations, blood work and monitoring for patient response or adverse events, as synergistic effects can be noted when used together with other medications due to overlapping mechanism of actions and changes in metabolism (112).
b.2.Chondroprotective agents:
Due to the destruction of cartilage as part of the disease process in OA, the search for biological substances with the ability to restore the damaged connective tissues and protect the cartilage and chondrocytes is ongoing. These substances are considered chondroprotective agents and if effective are termed disease-modifying osteoarthritis drugs (DMOADs) (116). Currently there is still a discrepancy between in-vitro and in-vivo studies, in parts due to the lack of medications that have proven adequate oral bioavailability and distribution to site of cartilage. Commonly considered chondroprotective agents that have been assessed in clinical trials and research studies, although with often limited conclusive results, include glucosamine hydrochloride (or sulfate), chondroitin sulfate, avocado soybean unsaponifiables (ASUs), egg-shell membrane extract, sodium pentosan polysulfate (PPS), green lipped mussel extract, type II Collagen (UC-II), and elk antler velvet extract among others.
b.2.1 Glucosamine and chondroitin have been suggested to have chondroprotective effects and are commonly used for OA patients in both human and veterinary medicine. Yet, inconsistent study design among studies has resulted in limited and conflicting results (117), causing questioning of their actual efficacy in veterinary species. In brief, based on in-vitro data, glucosamine is partly responsible for the regulation of collagen synthesis in cartilage and it contributes to glycosaminoglycan and proteoglycan synthesis (118, 119). Chondroitin sulfate is a sulfated glycosaminoglycan and contributes to extracellular matrix of cartilage and adds resistance and elasticity to the cartilage (120). The role of chondroitin sulfate is the inhibition of specific destructive enzymes in joint fluid and cartilage and, like glucosamine, contributes to the synthesis of glycosaminoglycans and proteoglycans (119, 120). The biggest challenge that both chondroitin sulfate and glucosamine face are low oral bioavailability and inconsistencies in product formulation (strength, form for glucosamine as sulfate vs. hydrochloride, and other ingredients added to the product), both contribute to the inconsistent results found in efficacy evaluation in literature and clinics. Most veterinary products contain glucosamine hydrochloride, which has significantly less bioavailability in humans than glucosamine sulfate. Pharmacokinetic studies are limited (121, 122) and the dosing recommendations of 15–30 mg/kg seem arbitrary and have not been established based on pharmacological evidence. The study performed by Adebowale et al. (123) demonstrated an oral bioavailability of 12% for glucosamine hydrochloride and 5% for chondroitin sulfate. Despite the differences in clinical studies from a point of view of design, products and results, there have been some well-conducted studies that provide more insight into the use of glucosamine and chondroitin (124–131). These studies evaluated joint function, comfort of the patient, and the overall safety profile of the supplement. The various outcome measures were aimed at establishing the potential anti-inflammatory and presumed mechanical improvements due to advanced cartilage function, with some positive results. The follow-up ranged from 2 to 6 months, with dosing around 40–62.5 mg/kg/d for glucosamine hydrochloride and 12–50 mg/kg/d for chondroitin sulfate in dogs, doubled for cats (132). No improvement was observed with objective outcomes in any study, and mild improvement was observed with non-validated subjective clinical scoring at three time-points in one study [Day 90, 120, and 150 (129)] and in one time-point in another study [Day 70 (127)]. Little is known about the actual effects of glucosamine and chondroitin at the level of the joint in either late or early stages of OA (133, 134). Canapp et al. showed evidence of protective effects of glucosamine hydrochloride with chondroitin sulfate at the level of joint, when given preemptively in an induced synovitis study (135), which would be different from OA. Despite the concerns about the lack of evidence in this category, owners and veterinarians alike continue to use or recommend products that contain glucosamine and chondroitin, often due to the high safety profile of most products. Education is important to clarify understanding and expectations of these products, in addition further studies including systematic review and metanalysis are required, to help resolve concerns of bioavailability and ultimately, efficacy.
b.2.2 Avocado soybean unsaponifiable (ASUs) is a mixture of the unsaponifiable fractions of one-third avocado oil and two-third soybean oil, that had promising effects for OA as a nutraceutical (136). The mechanism of action has been suggested to be inhibitory on interleukin-1 (IL-1) and stimulating on collagen synthesis based on in-vitro articular chondrocyte culture study (137). A potent inhibition of IL-8 and PGE2 has also been suggested (138). Cartilage repair may be promoted by its action on subchondral bone osteoblasts by preventing the osteoarthritic osteoblast-induced inhibition of matrix molecule production. Clinical studies in human OA with a focus on pain reduction outcomes show positive but limited evidence (139). A structural assessment study was done in a canine cruciate model, which demonstrated that ASUs reduce the development of early osteoarthritic cartilage and subchondral bone lesions. The suggested mode of action was mediated by the inhibition of inducible nitric oxide synthase and matrix metalloproteinase 13 (MMP-13), both key mediators of structural changes in canine OA (140). Dosing used in this study was 10 mkg/kg/day over 8 weeks. A study by Altinel et al. (141) evaluated ASU administration based on joint fluids and saw an increased levels of transforming growth factor beta 1 and 2 (TGF-ß1 and 2), both considered to be associated with the chondrocyte production of collagen and proteoglycans. Dosing for this study was 300 mg/dog SID, which translated to about 12 mg/kg. One clinical trial was conducted to assesses the efficacy of ASU in conjunction with glucosamine and chondroitin (131), not showing a significant difference in results, which may possibly be due to relatively low dosing (2.5–4.5 mg/kg/d). Overall, the evidence for ASU having beneficial effects in canine OA is limited but so far positive for both symptom relief and potential chondroprotective effects, although product differences need to be considered.
b.2.3. Egg-shell membrane (ESM) is the mesh-like bilayered substance that is found between the calcified shell and the albumin in chicken eggs. It is primarily composed of fibrous proteins such as collagen type I, keratin and elastin and glycosaminoglycans (142, 143). Egg-shell membrane extract has been evaluated in-vitro and showed an inhibition of IL1 β and tumor necrosis factor alpha (TNFα) (142, 144). A clinical study with a commercial product showed some positive effects on symptom relief that was detectable after 1 week and lasted throughout the study period of 6 weeks but lacked the statistical significance. The study further detected a change in serum levels of the cartilage degradation biomarker, c-terminal cross-linked telopeptide of type-II collagen (CTX-II) and concluded to a chondroprotective aspect (145). Dosing in the study was 300 mg/dog daily (equivalent to about 13.5 mg/kg daily), extrapolated from the effective studied human dose of 500 mg/day). Another study that examined the effect of a commercial ESM product in dogs with hip dysplasia found a clinical benefit of symptom relief at 15 mg/kg/day (143). Finally, another commercial ESM product was recently tested (146), and the dosing regimen was as per package (soft chews) recommendations, but a mg/kg dosing information was not made available. If the changes were in favor of the treated group, the differences did not reach statistical significance. Egg shell membrane supplements may be an option for symptom relief, however its role in chondroprotective measures and its pharmacokinetic profile require future studies to be completed.
b.2.4. Systemic DMOADs – Pentosan polysulfate sodium (PPS) is a polysulfate ester of xylan, prepared semi synthetically from beechwood plant material and is structurally similar to glycosaminoglycan (147). The mechanism of action may be a stimulation of hyaluronic acid and glycosaminoglycan synthesis, inhibition of proteolytic enzymes including metalloproteinases, and free radical scavenging as well as reduction of cytokine activity and osteoclast differentiation (147–149). The sodium derivative of PPS [sodium pentosan polysulphate (NaPPS)] has been available in veterinary medicine, is administered in the form of a subcutaneous injection and has been approved as a DMOAD, but its efficacy has not been fully established in the literature and remains controversial among clinicians. A canine post cruciate surgery study saw a faster recovery in one outcome measure compared to the placebo (150) and a clinical human study with knee OA found significant improvements in symptom relief compared to the placebo group (147). Yet clinically the results in dogs are inconsistent. Some patients demonstrate mild to moderate improvement, while others show no response. More studies are needed to assess the clinical and chondroprotective effects in dogs.
b.3. Boswellia Serrata (also known as “true” frankincense) has been included in many anti-arthritic joint supplements and has been shown to have anti-inflammatory properties in published studies (151). It has been traditionally used for centuries for this purpose (152). The active ingredient from the tree is the oleo-gum resin, and it is harvested by collecting the sap of the tree, then it is processed for use (stored, solidified and graded) (151). Boswellia resin is a traditional remedy for multiple ailments, but its anti-inflammatory properties held therapeutic interest and have been further explored. One of the mechanisms of action for its anti-inflammatory property is the inhibition of leukotrine (5HETE and leukotrine B4) synthesis by blocking the 5-lipoxygenase. It also has been shown to reduce glycosaminoglycan degradation, inhibition of TNF α and IL-1 β in-vitro (153). As with many of the other nutraceutical ingredients, the oral bioavailability in dogs can be challenging and species-specific PK studies are needed (154). Product formulation and manufacturing techniques also play a role in efficacy and safety. There have been some clinical studies in dogs (155) and humans (156), and Boswellia seems to have a wide safety range, based on acute and chronic toxicity and safety studies. However, dose determination research is needed, as the dose in one canine study was 40 mg/kg, but others have suggested 50–100 mg/kg once daily (155).
Other and combination products: Products that combine different nutraceuticals are available and popular among pet owners. There are commercially available products as well as veterinary specific products that have been scientifically assessed with promising results: omega-3 FA, including green-lipped mussel, products are the most recognized (34, 35). Curcuma efficacy alone (157), or in combination with collagen and green tea extract in an enriched therapeutic diet (158) did not show clear results. However, multi-herbal, omega-3, glucosamine combination in two different formulations (124, 159) was more convincing. Specific ingredients in combination products with promising efficacy shown in studies include epiitalis (160, 161), undenatured type II collagen (UC-II) either alone (128, 162–164) or in combination with other chondroprotective ingredients (128, 129, 163), and warrant mentioning and further research.
Finally, promising natural health products, such as elk-velvet antler (165) or the Brachystemma calicinum D. don Chinese plant (166, 167), that have attractive analgesic benefits currently have a minor role in commercialization due to their controversy in safety and quality control production.
Under this category, there are specific modalities that are commonly used clinically in OA patients and have been scientifically evaluated (Table 6). We provided a summary but encourage the reader to further their own knowledge with additional research on available studies, bias, risks, side effects, techniques, required level of training or certification process, and benefits. These details were beyond the scope of this paper, but are important information, when considering the different modalities. The list of OA related modalities presented in these guidelines is not exhaustive, additional modalities may be considered by experienced and trained practitioners (including osteopathy, chiropractice, canine massages, cryotherapy, therapeutic ultrasound among others), and should also be based on available evidence that results from appropriate study design.
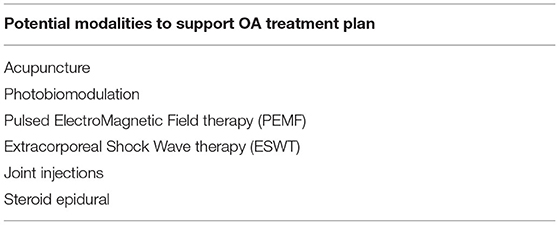
Table 6. Potential modalities discussed in this paper that may be added to an OA treatment plan to support the individual patient.
Photobiomodulation (Laser) treatments can potentially be beneficial for some patients, using appropriate settings for specific tissues or conditions. There have been significant knowledge gains in the field of laser therapy over the last 10 years and it is important to understand the technicalities to assure that the targeted tissue depth is reached, as it will vary depending on tissue (168, 169). The mechanism of action of Laser (light amplification by stimulated emission of radiation) is on a cellular level via photobiomodulation. Investigators have shown that laser application on tissue has multiple effects including an increase in angiogenesis, neurite extension, normalization of ion channels, stabilization of the cellular membrane, and other cellular changes (170), but the most recognized mechanism is the nitric oxide (NO) interaction in the cytochrome C system leading to improved ATP utilization and production. Reducing inflammation and edema through means of IL-1 reduction, acceleration of leucocyte, and inhibition of PG synthesis have also been discussed. In veterinary medicine Low Level Laser therapy (LLLT) can be useful in the treatment of musculoskeletal pain (170) using either a class IIIB or IV laser. Usually, wavelengths in the therapeutic window between 600 and 1,100 nm are used, with adequate penetration into tissue requiring a minimum of 800 nm. Laser therapy can reduce muscle tension when used for surface area application, however treatment of OA via intra-articular penetration of the laser beam requires a higher power (higher than 4–8 J cm2) or a longer duration of treatment. The risk of burns at the higher wavelengths are avoided by constant movement of the probe, extra precautions with darker skin/fur animals as the absorbed light in these patients may produce warm energy. At times shaving thicker fur may improve wavelength penetration. Laser therapy is used as an integral part of rehabilitation protocols (64, 170, 171) and is commonly used as an add on modality to an overall sound treatment plan. It appears that with better understanding of laser therapy and better designed studies, the knowledge for its usefulness in the treatment of OA has improved (64, 169, 171–174) but it is not yet conclusive (175). It will require further extensive and appropriate investigations to answer its benefits, risks, limitations and settle the strong controversy surrounding this modality.
Acupuncture can be an effective conservative treatment for neuro- and musculoskeletal pain conditions including OA and is recommended as an adjunct therapy within the multimodal approach (176). Various studies have been published in dogs with OA with different outcome measures and assessments, as well as acupuncture techniques and results. The changes that have been noted seem subtle but positive, although not always statistically significant. Acupuncture is a modality that seems to have an individual response irrelevant of whether a Western or Eastern approach is used. Extensive human studies have shown a beneficial effect of acupuncture in the treatment of OA (177), but metanalyses are not always conclusive and the claimed small analgesic effect cannot be clearly distinguished from bias (178). Veterinary studies are not different (65), in parts due to the difficulties in pain assessment and the challenges of standardizing a treatment protocol. The differentiation of electroacupuncture vs. dry needle acupuncture is one of the questions that would be interesting to have answered. Acupuncture is a highly individualized therapy that is commonly used within a rehabilitation program or as part of palliative care, continues to gain popularity within the veterinary community.
Mechanical stimulation: Pulsed ElectroMagnetic Field therapy (PEMF) and Extracorporeal Shock Wave Therapy (ESWT). PEMF is an emerging area of interest for OA treatment in both human and veterinary medicine (179). PEMF utilizes frequencies at the low end of the electromagnetic spectrum (6–500 zH), which stimulate biological effects on a cellular level. The mechanism of action remains not fully understood but potential mechanism of actions of PEMF are the stimulation of chondrocyte proliferation and differentiation, as well as extracellular matrix synthesis. PEMF can cause a decrease in inflammatory cell infiltration, reduction in immuno-positive cells to IL-1β, decrease in TNF-α, and increase TGF-β 1 (promoting cartilage repair). PEMF shows promising results in both in-vitro and in-vivo studies to provide pain relief, improved function and slowing down the progression of OA (180, 181). Although literature is readily available, the quality of veterinary studies on PEMF are still limited (182) and more research needs to be conducted. As an adjunct, non-invasive therapy, this modality will likely play an increasing role in clinics and, especially for in-home use in form of commercially available loops, discs, and mats (182). ESWT is a special, non-linear type of pressure wave with a short rise time (around 10 μs) and a frequency ranging from 16 to 20 MHz. Different ESWT units are available with different wave forms (radial, piezioelectric and electrohydraulic) which will lead to different tissue penetration of the acoustic wave. Extensive knowledge and training is needed for appropriate application of this modality. In particular the electrohydraulic waves will require sedation of the patient, potentially part of the reasons why this modality is less mainstream in veterinary practice. Several studies have demonstrating attractive value of ESWT in managing canine musculoskeletal alterations, mostly OA, either for stifle (183), shoulder (184) or hip (83, 185) joints.
As part of “regenerative medicine,” joint injections of “orthobiologics” or drugs have been explored for local pain relief of a specific joint. Severe OA in the elbow, shoulder or hip can be difficult to treat to provide adequate comfort. Injections of hyaluronic acid (HA), mesenchymal stem cells (MSC) or platelet-rich plasma (PRP), autologous protein solution (APS) have been proposed and investigated. This panel has agreed that as of now, most of the research in canines has been published with PRP injections (see below) and is therefore currently the recommended choice, if a joint injection is considered. Stem cell injections have some chondroprotective and regenerative potential, however, are still considered to be in their infancy. Injections of HA and steroids are usually reserved for palliative cases as the pain relief may show benefits for symptom relief, but the chondro-destructive potential remains controversial for steroid injections (186). The use of HA/steroid joint injections in human OA appears to be favorable in the literature due to the improvement of symptoms as well as the joint lubricating effects of HA but has a relative short duration and a limited number of injections per year. It remains quite uncommon in canine medicine (187, 188). The use of HA has been studied either in experimental models (189) or in clinical use in OA dogs (190) with positive outcomes over an appropriate (several months) length of time (67, 68, 191). It has been previously suggested that intraarticular HA would be more effective in dogs with mild to moderate OA than in those with severe OA (189). The combination of intraarticular HA and triamcinolone looks efficient too (187).
Platelet-rich plasma (PRP) is an orthobiologic composed mainly of platelets, which in turn will release growth factors to then stimulate other cytokines and chemokines. Derivatives include autologous platelets concentrate (APC) and APS. The growth factors (platelet-derived growth factor (PDGF), transforming growth factor β 1 &2 (TGF-β 1 &2), vascular endothelial growth factor (VEGF), basic fibroblastic growth factor (bFGF) and epidermal grow factor (EGF) among others) are the driving forces as important bioactive compounds contributing to wound healing by enhancing cellular migration, cellular proliferation, angiogenesis, and matrix deposition, which in turn may counteract cartilage destruction (192, 193). Platelet preparation systems vary in their ability to concentrate platelets, as well as select beneficial cells over unwanted cells like RBC, leukocytes, neutrophiles (193, 194). The ideal concentrations of platelets and WBCs are unknown, and likely depend on the type and chronicity of the injury. In the literature, the high variability in PRP preparations may be the reason for inconsistent results, but emerging clinical and in vitro studies, and clinical experience seem promising. PRP preparation can be done by specific systems (commercial gravity systems or centrifuge systems), that can be acquired. The protocol involves a blood draw from the patient which in turn is spun down in a centrifuge to separate RBC and plasma from the platelet/WBC layer. In some instances, a second centrifugation is recommended for further platelet concentration. The final product is then injected meticulously aseptically into the joint to avoid any infection. Duration of pain relief may last from 3 to 12 months and has been reported in OA dogs for PRP alone (195–199) or associated to HA (67) or physical therapy, showing longer duration of analgesia (197), APC (200, 201), APS (187, 202, 203). Most interestingly, PRP may have the potential to slow the progression of the disease, as suggested by a recent metanalysis including 1,251 animals (19 studies on rodents, 13 on rabbits, 4 on horses, one on goats, and 7 on dogs) (204). The disease-modifying effects (DMOAD) were present in 68% of the studies (beneficial clinical effects in 80%) and included attenuating cartilage damage progression, and reducing synovial inflammation, coupled with changes in biomarker levels.
The comparison between intraarticular HA, APC, triamcinolone, and stanozolol supports more prolonged analgesic benefits, with lower variation in results for HA and APC (205). Several reports of beneficial analgesia exist after intraarticular MSC injection (206–212). However, these reports present methodological drawbacks, such as absence of standardization in MSC preparation, either limited power of analysis, and/or subjective outcome measures, or most often lack of a placebo control, to really state about the interest of intraarticular MSC injection. Finally, some anecdotal publications mention the use of intraarticular botulinum toxin A for pain management in OA dogs (213, 214), of Tin-117m (117mSn-colloid) isotope radiopharmaceutical in canine elbow OA (215), and of intraarticular resiniferatoxin for long-term analgesia (216).
Steroid epidural: Senior dogs especially, but also young working dogs (i.e., German Shephard military or police dogs) may exhibit severe lumbosacral pain. This can be a primary disease, as some dog breeds are predisposed to it, but it also can be part of posture changes related to late-stage OA in hips or knees. The resulting progressive hind-end weakness due to avoidance of muscle usage caused by pain leads to significant mobility issues. An epidural injection of long-acting steroid can provide relief of a duration from 4 to 12 months (217, 218). For an epidural injection, the patient is heavily sedated, or in case of health-related concerns briefly anesthetized. The lumbosacral area is aseptically prepared and 0.1 mg/kg methylprednisolone acetate injected sterile. Complications appear to be rare in veterinary medicine and may relate primarily to sterility and trauma but have also been linked to the formulation (including preservatives and particulation). In human chronic spinal pain management, complications can be severe, and concerns have been raised specifically regarding the use of particulate steroids -like methylprednisoline- when applied epidurally (219).
The Canadian OA treatment guidelines were created from a diverse group of experts, driven by the shared understanding of the need for providing direction for veterinarians on selecting appropriate therapies based on COAST stage for a patient experiencing OA. Due to the inflammatory nature, chronicity, potential neurogenic component and continued progression of the disease, OA requires a multimodal approach. The treatment options for OA are constantly evolving as new therapies and research emerge, and this document captures the current or soon to be arriving options for Canadian veterinarians in 2022. It aims to provide insights into the treatment choices of experts and is grouped based on consensus into core and secondary treatments.
The panel felt that for every OA patient, their multimodal plan should involve client education, a weight management plan, optimized nutrition including omega 3 fatty acids, exercise, and beginning in stage 2, pain management. Additional secondary therapies or modalities can then be layered on, based on OA stage, individual patient need and veterinarian or pet owner preference. A cautious and rigorous characterization of the pain syndrome affecting the patient must guide the veterinarian to the best choice of therapeutics. With the fundamental understanding that the multimodal approach should always be aimed at slowing the progression of OA, maintaining patient mobility and above all, maximizing patient comfort and QoL.
CM wrote the first draft of the manuscript. All authors contributed to the discussion for the content of this manuscript, wrote sections of the manuscript and contributed to the correctness of the content (in order of their authorship, besides ET, who added significant amount and is considered senior author on this manuscript), and manuscript revision, read, and approved the submitted version.
Elanco Canada Limited supported the development of these OA guidelines as part of their commitment to education and the orthopedic health and pain management of dogs.
These guidelines and recommendations should not be construed as dictating an exclusive protocol, course of treatment, or procedure. They are considered to be a helpful informational summary of available treatment options with a consensus from experts with a critical evaluation of the literature and clinical expertise. Although every effort has been made to ensure the completeness and accuracy of the information provided herein, neither the authors nor Elanco Canada Limited assume any responsibility for the completeness or accuracy of the information. All information is provided “as is” without any warranties, either expressed or implied. As each case is different, veterinarians must base their decisions on the best available scientific evidence in conjunction with their own knowledge and experience.
CM is currently a Veterinary Consultant for Orthopedic Health and Pain for Elanco Canada Limited.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ALA, alpha lipoic acid; APC, autologous platelets concentrate; APS, autologous protein solution; ASU, avocado soybean unsaponifiables; bFGF, basic fibroplastic growth factor; CB1+2, cannabinoid receptor 1 and 2; CBD, cannabidiol; CBDa, acid form of cannabidiol; COAST, canine osteoarthritis staging tool; COX, cyclooxygenase enzyme; CTX-II, c-terminal cross-linked telopeptide of type-II collagen; DHA, docosahexaenoic acid; DMOAD, disease-modifying osteoarthritis drug; DPA, docosapentaenoic acid; ECS, endocannabinoid system; EGF, epidermal grow factor; EPA, eicosapentaenoic acid; EP4, E-type prostanoid receptor 4; ESM, eggshell membrane; ESWT, Extracorporeal Shock Wave Therapy; FA, fatty acids; FAAH, Fatty acid amide hydrolase; HA, hyaluronic acid; IL-1 or 8, interleukin-1 or 8; Laser, light amplification by stimulated emission of radiation; LLLT, Low Level Laser therapy; LOAD, Liverpool osteoarthritis in dogs questionnaire; mAb, monoclonal antibody; MMP-13, matrix metalloproteinase 13; MSC, mesenchymal stem cells; NGF, nerve growth factor; NMDA, N-methyl-D-aspartate receptor; NO, nitric oxide; NPN, natural product number; NSAID, non-steroidal anti-inflammatory drug; NTR, neurotropin receptor; OA, osteoarthritis; PD, pharmacodynamics; PDGF, platelet-derived growth factor; PEMF, pulsed-electromagnetic field therapy; PG, prostaglandin; PK, pharmacokinetic; PPA, pentosan polysulfate sodium; PRP, platelet rich plasma; QoL, quality of life; ROM, range of motion; T1/2, half life; TGF-ß1 and 2, transforming growth factor beta; THC, tetrahydrocannabinol; THCa, acid form of tetrahydrocannabinol; TNFα, tumor necrosis factor alpha; TrkA, tropomyosin-related kinase receptor; TRPV, transient receptor potential cation channel—vanilloid; UC-II, type II Collagen; VEGF, vascular endothelial growth factor; VGCC, voltage gated calcium channel.
1. Johnston SA. Osteoarthritis. joint anatomy, physiology, and pathology. Vet Clin North Am Small Anim Pract. (1997) 27:699–723. doi: 10.1016/S0195-5616(97)50076-3
2. Anderson KL, O'Neill DG, Brodbelt DC, Church DB, Meeson RL, Sargan D, et al. Prevalence, duration and risk factors for appendicular osteoarthritis in a UK dog population under primary veterinary care. Sci Rep. (2018) 8:5641. doi: 10.1038/s41598-018-23940-z
3. Anderson KL, Zulch H, O'Neill DG, Meeson RL, Collins LM. Risk factors for canine osteoarthritis and its predisposing arthropathies: a systematic review. Front Vet Sci. (2020) 7:220. doi: 10.3389/fvets.2020.00220
4. Johnson JA, Austin C, Breur GJ. Incidence of canine appendicular musculoskeletal disorders in 16 veterinary teaching hospitals from 1980 through 1989. Vet Comp Orthop Traumatol. (1994) 7:56–69. doi: 10.1055/s-0038-1633097
5. Lamani TSD, Ranganath L, Nagaraja BN, Satyanarayana ML, Jamuna KV, Kamran A. Incidence of osteoarthritis in dogs – a clinical study of 64 patients. Int J Sci Environ Technol. (2019) 8:559–64.
6. Areshkumar M, Prasad A, Shafiuzama M, Jeyaraja K. Studies on the incidence of osteoarthritis of hip joint in dogs of Chennai. Sci Ocean. (2018) 1:18–23.
7. Pinho-Ribeiro FA, Verri WA Jr, Chiu IM. Nociceptor sensory neuron-immune interactions in pain and inflammation. Trends Immunol. (2017) 38:5–19. doi: 10.1016/j.it.2016.10.001
8. Van den Bosch MHJ. Inflammation in osteoarthritis: is it time to dampen the alarm(in) in this debilitating disease? Clin Exp Immunol. (2019) 195:153–66. doi: 10.1111/cei.13237
9. Chen O, Donnelly CR, Ji RR. Regulation of pain by neuro-immune interactions between macrophages and nociceptor sensory neurons. Curr Opin Neurobiol. (2020) 62:17–25. doi: 10.1016/j.conb.2019.11.006
10. Cachon T, Frykman O, Innes JF, Lascelles BDX, Okumura M, Sousa P, et al. COAST development group. face validity of a proposed tool for staging canine osteoarthritis: Canine OsteoArthritis Staging Tool (COAST). Vet J. (2018) 235:1–8. doi: 10.1016/j.tvjl.2018.02.017
11. Marcellin-Little DJ,. Managing Canine Osteoarthritis in All Stages Ages. Veterinary Practice News. (2020). Available online at: https://www.veterinarypracticenews.com/osteoarthritis-june-2020/ (accessed October 20, 2021)
12. Kealy RD, Lawler DL, Ballam JM, Lust G, Biery DN, Smith GK, et al. Evaluation of the effect of limited food consumption on radiographic evidence of osteoarthritis in dogs. J Am Vet Med Assoc. (2000) 217:1678–80. doi: 10.2460/javma.2000.217.1678
13. Impellizeri JA, Tetrick MA, Muir P. Effect of weight reduction on clinical signs of lameness in dogs with hip osteoarthritis. J Am Vet Med Assoc. (2000) 216:1089–91. doi: 10.2460/javma.2000.216.1089
14. Marshall W, Bockstahler B, Hulse D, Carmichael S. A review of osteoarthritis and obesity: current understanding of the relationship and benefit of obesity treatment and prevention in the dog. Vet Comp Orthop Traumatol. (2009) 22:339–45. doi: 10.3415/VCOT-08-08-0069
15. Marshall WG, Hazewinkel HA, Mullen D, De Meyer G, Baert K, Carmichael S. The effect of weight loss on lameness in obese dogs with osteoarthritis. Vet Res Commun. (2010) 34:241–53. doi: 10.1007/s11259-010-9348-7
16. Koonce RC, Bravman JT. Obesity and osteoarthritis: more than just wear and tear. J Am Acad Orthop Surg. (2013) 21:161–9. doi: 10.5435/JAAOS-21-03-161
17. Frank L, Mann S, Levine CB, Cummings BP, Wakshlag JJ. Increasing body condition score is positively associated interleukin-6 and monocyte chemoattractant protein-1 in Labrador retrievers. Vet Immunol Immunopathol. (2015) 167:104–9. doi: 10.1016/j.vetimm.2015.07.010
18. Richter M, Trzeciak T, Owecki M, Pucher A, Kaczmarczyk J. The role of adipocytokines in the pathogenesis of knee joint osteoarthritis. Int Orthop. (2015) 39:1211–7. doi: 10.1007/s00264-015-2707-9
19. Vincent HK, Heywood K, Connelly J, Hurley RW. Obesity and weight loss in the treatment and prevention of osteoarthritis. PM R. (2012) 4(5 Suppl):S59–67. doi: 10.1016/j.pmrj.2012.01.005
20. German AJ, Holden SL, Wiseman-Orr ML, Reid J, Nolan AM, Biourge V, et al. Quality of life is reduced in obese dogs but improves after successful weight loss. Vet J. (2012) 192:428–34. doi: 10.1016/j.tvjl.2011.09.015
21. Moreau M, Troncy E, Bichot S, Lussier B. Influence of changes in body weight on peak vertical force in osteoarthritic dogs: a possible bias in study outcome. Vet Surg. (2010) 39:43–7. doi: 10.1111/j.1532-950X.2009.00621.x
22. Jurvelin J, Kiviranta I, Tammi M, Helminen HJ. Effect of physical exercise on indentation stiffness of articular cartilage in the canine knee. Int J Sports Med. (1986) 7:106–10. doi: 10.1055/s-2008-1025743
23. Greene LM, Marcellin-Little DJ, Lascelles BD. Associations among exercise duration, lameness severity, and hip joint range of motion in Labrador Retrievers with hip dysplasia. J Am Vet Med Assoc. (2013) 242:1528–33. doi: 10.2460/javma.242.11.1528
24. Buckwalter JA. Sports, joint injury, and posttraumatic osteoarthritis. J Orthop Sports Phys Ther. (2003) 33:578–88. doi: 10.2519/jospt.2003.33.10.578
25. Hunter DJ, Eckstein F. Exercise, and osteoarthritis. J Anat. (2009) 214:197–207. doi: 10.1111/j.1469-7580.2008.01013.x
26. Jurvelin J, Kiviranta I, Tammi M, Helminen HJ. Softening of canine articular cartilage after immobilization of the knee joint. Clin Orthop Res. (1986) 207:246–52. doi: 10.1097/00003086-198606000-00042
27. Herrmann M, Engelke K, Ebert R, Müller-Deubert S, Rudert M, Ziouti F, et al. Interactions between muscle and bone-where physics meets biology. Biomolecules. (2020) 10:432. doi: 10.3390/biom10030432
28. Adrian CP, Haussler KK, Kawcak C, Reiser RF 2nd, Riegger-Krugh C, Palmer RH, et al. The role of muscle activation in cruciate disease. Vet Surg. (2013) 42:765–73. doi: 10.1111/j.1532-950X.2013.12045.x
29. Freeman LM. Cachexia and sarcopenia: emerging syndromes of importance in dogs and cats. J Vet Intern Med. (2012) 26:3–17. doi: 10.1111/j.1939-1676.2011.00838.x
30. Roush JK, Dodd CE, Fritsch DA, Allen TA, Jewell DE, Schoenherr WD, et al. Multicenter veterinary practice assessment of the effects of omega-3 fatty acids on osteoarthritis in dogs. J Am Vet Med Assoc. (2010) 236:59–66. doi: 10.2460/javma.236.1.59
31. Roush JK, Cross AR, Renberg WC, Dodd CE, Sixby KA, Fritsch DA, et al. Evaluation of the effects of dietary supplementation with fish oil omega-3 fatty acids on weight bearing in dogs with osteoarthritis. J Am Vet Med Assoc. (2010) 236:67–73. doi: 10.2460/javma.236.1.67
32. Moreau M, Troncy E, del Castillo JRE, Bédard C, Gauvin D, Lussier B. Effects of feeding a high omega-3 fatty acids diet in dogs with naturally occurring osteoarthritis. J Anim Physiol Anim Nutr. (2013) 97:830–7. doi: 10.1111/j.1439-0396.2012.01325.x
33. Mehler SJ, May LR, King C, Harris WS, Shah Z. A prospective, randomized, double blind, placebo-controlled evaluation of the effects of eicosapentaenoic acid and docosahexaenoic acid on the clinical signs and erythrocyte membrane polyunsaturated fatty acid concentrations in dogs with osteoarthritis. Prostaglandins Leukot Essent Fatty Acids. (2016) 109:1–7. doi: 10.1016/j.plefa.2016.03.015
34. Hielm-Björkman A, Tulamo RM, Salonen H, Raekallio M. Evaluating complementary therapies for canine osteoarthritis part i: green-lipped mussel (Perna canaliculus). Evid Based Complement Alternat Med. (2007) 6:365–73. doi: 10.1093/ecam/nem136
35. Hielm-Björkman A, Roine J, Elo K, Lappalainer A, Junnila J, Laitinen-Vapaavuori O. An un-commissioned randomized, placebo-controlled double-blind study to test the effect of deep sea fish oil as a pain reliever for dogs suffering from canine OA. BMC Vet Res. (2012) 8:157. doi: 10.1186/1746-6148-8-157
36. Rialland P, Bichot S, Lussier B, Moreau M, Beaudry F, del Castillo JR, et al. Effect of a diet enriched with green-lipped mussel on pain behavior and functioning in dogs with clinical osteoarthritis. Can J Vet Res. (2013) 77:66–74.
37. Soontornvipart K, Mongkhon N, Nganvongpanit K, Kongtawelert P. Effect of PCSO-524 on OA biomarkers and weight-bearing properties in canine shoulder and coxofemoral osteoarthritis. Thai J Vet Med. (2015) 45:157–65.
38. Vijarnsorn M, Kwananocha I, Kashemsant N, Jarudecha T, Lekcharoensuk C, Beale B, et al. The effectiveness of marine based fatty acid compound (PCSO-524) and firocoxib in the treatment of canine osteoarthritis. BMC Vet Res. (2019) 15:349. doi: 10.1186/s12917-019-2110-7
39. Fritsch D, Allen TA, Dodd CE, Jewell DE, Sixby KA, Leventhal PS, et al. Dose-titration effects of fish oil in osteoarthritic dogs. J Vet Intern Med. (2010) 24:1020–6. doi: 10.1111/j.1939-1676.2010.0572.x
41. Bauer JE. Essential fatty acid metabolism in dogs and cats. Rev Bras Zootecn. (2008) 37:20–27. doi: 10.1590/S1516-35982008001300004
42. Waldron M,. (2004). Available online at: https://www.dvm360.com/view/role-fatty-acids-management-osteoarthritis (accessed October 26, 2021)
43. Krontveit RI, Nødtvedt A, Sævik BK, Ropstad E, Trangerud C. Housing- and exercise-related risk factors associated with the development of hip dysplasia as determined by radiographic evaluation in a prospective cohort of Newfoundlands, Labrador Retrievers, Leonbergers, and Irish Wolfhounds in Norway. Am J Vet Res. (2012) 73:838–46. doi: 10.2460/ajvr.73.6.838
44. Mlacnik E, Bockstahler BA, Müller M, Tetrick MA, Nap RC, Zentek J. Effects of caloric restriction and a moderate or intense physiotherapy program for treatment of lameness in overweight dogs with osteoarthritis. J Am Vet Med Assoc. (2006) 229:1756–60. doi: 10.2460/javma.229.11.1756
45. Jeong HS, Lee SC, Jee H, Song JB, Chang HS, Lee SY. Proprioceptive training and outcomes of patients with knee osteoarthritis: a meta-analysis of randomized controlled trials. J Athl Train. (2019) 54:418–28. doi: 10.4085/1062-6050-329-17
46. Berenbaum F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthritis Cartilage. (2013) 21:16–21. doi: 10.1016/j.joca.2012.11.012
47. Sokolove J, Lepus CM. Role of inflammation in the pathogenesis of osteoarthritis: latest findings and interpretations. Ther Adv Musculoskelet Dis. (2013) 5:77–94. doi: 10.1177/1759720X12467868
48. Kawabata A. Prostaglandin E2 and pain–an update. Biol Pharm Bull. (2011) 34:1170–3. doi: 10.1248/bpb.34.1170
49. St-Jacques B, Ma W. Peripheral prostaglandin E2 prolongs the sensitization of nociceptive dorsal root ganglion neurons possibly by facilitating the synthesis and anterograde axonal trafficking of EP4 receptors. Exp Neurol. (2014) 261:354–66. doi: 10.1016/j.expneurol.2014.05.028
50. McCoy JM, Wicks JR, Audoly LP. The role of prostaglandin E2 receptors in the pathogenesis of rheumatoid arthritis. J Clin Invest. (2002) 110:651–8. doi: 10.1172/JCI0215528
51. Griffiths R. Prostaglandins and inflammation. In: Gallin J and Snyderman R, editors. Inflammation: Basic Principles Clinical Correlates. Philadelphia, PA: Lippincott, Williams, & Wilkins (1999). p. 349–60.
52. Attur M, Al-Mussawir HE, Patel J, Kitay A, Dave M, Palmer G, et al. Prostaglandin E2 exerts catabolic effects in osteoarthritis cartilage: evidence for signaling via the EP4 receptor. J Immunol. (2008) 181:5082–8. doi: 10.4049/jimmunol.181.7.5082
53. KuKanich B, Bidgood T, Knesl O. Clinical pharmacology of nonsteroidal anti-inflammatory drugs in dogs. Vet Anaesth Analg. (2012) 39:69–90. doi: 10.1111/j.1467-2995.2011.00675.x
54. Innes JF, Clayton J, Lascelles BDX. Review of the safety and efficacy of long-term NSAID use in the treatment of canine osteoarthritis. Vet Record. (2010) 166:226–30. doi: 10.1136/vr.c97
55. Doig PA, Purbrick KA, Hare JE, McKeown DB. Clinical efficacy and tolerance of meloxicam in dogs with chronic osteoarthritis. Can Vet J. (2000) 41:296–300.
56. Thomas MJ, Rathod-Mistry T, Parry EL, Pope C, Neogi T, Peat C. Triggers for acute flare in adults with, or at risk of, knee osteoarthritis: a web-based case-crossover study in community-dwelling adults. Osteoarthritis Cartilage. (2021) 29:956–64. doi: 10.1016/j.joca.2021.04.007
57. Kirkby Shaw K, Alvarez L, Foster SA, Tomlinson JE, Shaw AJ, Pozzi A. Fundamental principles of rehabilitation and musculoskeletal tissue healing. Vet Surg. (2020) 49:22–32. doi: 10.1111/vsu.13270
58. Belshaw Z, Asher L, Dean RS. The attitudes of owners and veterinary professionals in the United Kingdom to the risk of adverse events associated with using non-steroidal anti-inflammatory drugs (NSAIDs) to treat dogs with osteoarthritis. Prev Vet Med. (2016) 131:121–6. doi: 10.1016/j.prevetmed.2016.07.017
59. Matthews ML. The role of dose reduction with NSAID use. Am J Manag Care. (2013) 19(14 Suppl):s273–7.
60. Hazewinkel HAW, van den Brom WE, Theijse LFH, Pollmeier M, Hanson PD. Reduced dosage of ketoprofen for the short-term and long-term treatment of joint pain in dogs. Vet Rec. (2003) 152:11–4. doi: 10.1136/vr.152.1.11
61. Monteiro BP, Lambert C, Bianchi E, Genevois JP, Soldani G, Troncy E. Safety and efficacy of reduced dosage ketoprofen with or without tramadol for long-term treatment of osteoarthritis in dogs: a randomized clinical trial. BMC Vet Res. (2019) 15:213. doi: 10.1186/s12917-019-1960-3
62. Wernham B, Trumpatori B, Hash J, Lipsett J, Davidson G, Wackerow P, et al. Dose reduction of meloxicam in dogs with osteoarthritis-associated pain and impaired mobility. J Vet Intern Med. (2011) 25:1298–305. doi: 10.1111/j.1939-1676.2011.00825.x
63. Walton MB, Cowderoy E, Lascelles D, Innes JF. Evaluation of construct and criterion validity for the ‘Liverpool Osteoarthritis in Dogs' (LOAD) clinical metrology instrument and comparison to two other instruments. PLoS ONE. (2013) 8:e58125. doi: 10.1371/journal.pone.0058125
64. Looney AL, Huntingford JL, Blaeser LL, Mann S. A randomized blind placebo-controlled trial investigating the effects of photobiomodulation therapy (PBMT) on canine elbow osteoarthritis. Can Vet J. (2018) 59:959–66.
65. Baker-Meuten A, Wendland T, Shamir SK, Hess AM, Duerr FM. Evaluation of acupuncture for the treatment of pain associated with naturally-occurring osteoarthritis in dogs: a prospective, randomized, placebo-controlled, blinded clinical trial. BMC Vet Res. (2020) 16:357. doi: 10.1186/s12917-020-02567-1
66. Sadabad HN, Behzadifar M, Arasteh F, Behzadifar M, Dehghan HR. Efficacy of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: a systematic review and meta-analysis. Electron Phys. (2016) 8:2115–22. doi: 10.19082/2115
67. Lee MI, Kim JH, Kwak HH, Woo HM, Han JH, Yayon A, et al. A placebo-controlled study comparing the efficacy of intra-articular injections of hyaluronic acid and a novel hyaluronic acid-platelet-rich plasma conjugate in a canine model of osteoarthritis. J Orthop Surg Res. (2019) 14:314. doi: 10.1186/s13018-019-1352-1
68. Pashuck TD, Kuroki K, Cook CR, Stoker AM, Cook JL. Hyaluronic acid versus saline intra-articular injections for amelioration of chronic knee osteoarthritis: a canine model. J Orthop Res. (2016) 34:1772–9. doi: 10.1002/jor.23191
69. Vaughn D, Kulpa J, Paulionis L. Preliminary investigation of the safety of escalating cannabinoid doses in healthy dogs. Front Vet Sci. (2020) 7:51. doi: 10.3389/fvets.2020.00051
70. Gamble L, Boesch JM, Frye CW, Schwark WS, Mann S, Wolfe L, et al. Pharmacokinetics, safety, and clinical efficacy of cannabidiol treatment in osteoarthritic dogs. Front Vet Sci. (2018) 5:165. doi: 10.3389/fvets.2018.00165
71. Lascelles BDX, Knazovicky D, Case B, Freire M, Innes JF, Drew AC, et al. A canine-specific anti-nerve growth factor antibody alleviates pain and improves mobility and function in dogs with degenerative joint disease-associated pain. BMC Vet Res. (2015) 11:101. doi: 10.1186/s12917-015-0413-x
72. Gearing DP, Virtue ER, Gearing RP, Drew AC. A fully caninised anti-NGF monoclonal antibody for pain relief in dogs. BMC Vet Res. (2013) 9:226. doi: 10.1186/1746-6148-9-226
73. Enomoto M, Mantyh PW, Murrell J, Innes JF, Lascelles BDX. Anti-nerve growth factor monoclonal antibodies for the control of pain in dogs and cats. Vet Rec. (2019) 184:23. doi: 10.1136/vr.104590
74. Webster RP, Anderson GI, Gearing DP. Canine Brief Pain Inventory scores for dogs with osteoarthritis before and after administration of a monoclonal antibody against nerve growth factor. Am J Vet Res. (2014) 75:532–35. doi: 10.2460/ajvr.75.6.532
75. Corral MJ, Moyaert H, Fernandes T, Escalada M, Kira S, Tena J, et al. A prospective, randomized, blinded, placebo-controlled multisite clinical study of bedinvetmab, a canine monoclonal antibody targeting nerve growth factor, in dogs with osteoarthritis. Vet Anaesth Analg. (2021) 4:943–55. doi: 10.1016/j.vaa.2021.08.001
76. Isola M, Ferrari V, Miolo A, Stabile F, Bernardini D, Carnier P, et al. Nerve growth factor concentrations in the synovial fluid from healthy dogs and dogs with secondary osteoarthritis. Vet Comp Orthop Traumatol. (2011) 24:279–84. doi: 10.3415/VCOT-10-04-0051
77. Aloe L, Rocco ML, Balzamino BO, Micera A. Nerve growth factor: a focus on neuroscience and therapy. Curr Neuropharmacol. (2015) 13:294–303. doi: 10.2174/1570159X13666150403231920
78. Bimonte S, Cascella M, Forte CA, Esposito G, Cuomo A. The role of anti-nerve growth factor monoclonal antibodies in the control of chronic cancer and non-cancer pain. J Pain Res. (2021) 14:1959–67. doi: 10.2147/JPR.S302004
79. Mantyh PW, Koltzenburg M, Mendell LM, Tive L, Shelton DL, Warner DS. Antagonism of nerve growth factor-TrkA signaling and the relief of pain. Anesthesiology. (2011) 115:189–204. doi: 10.1097/ALN.0b013e31821b1ac5
80. Chang DS, Hsu E, Hottinger DG, Cohen SP. Anti-nerve growth factor in pain management: current evidence. J Pain Res. (2016) 9:373–83. doi: 10.2147/JPR.S89061
81. Seah KTM, Rammanohar J, Sutton J, To K, Khan WS. The effectiveness of anti-nerve growth factor monoclonal antibodies in the management of pain in osteoarthritis of the hip and knee: a PRISMA systematic review and meta-analysis. Pain Med. (2021) 22:1185–204. doi: 10.1093/pm/pnaa441
82. Lascelles BDX, Gaynor JS, Smith ES, Roe SC, Marcellin-Little DJ, Davidson G, et al. Amantadine in a multimodal analgesic regimen for alleviation of refractory osteoarthritic pain in dogs. J Vet Intern Med. (2008) 22:53–9. doi: 10.1111/j.1939-1676.2007.0014.x
83. Mueller M, Bockstahler B, Skalicky M, Mlacnik E, Lorinson D. Effects of radial shockwave therapy on the limb function of dogs with hip osteoarthritis. Vet Rec. (2007) 160:762–5. doi: 10.1136/vr.160.22.762
84. Wang CJ, Weng LH, Ko JY, Sun YC, Yang YJ, Wang FS. Extracorporeal shockwave therapy shows chondroprotective effects in osteoarthritic rat knee. Arch Orthop Trauma Surg. (2011) 131:1153–8. doi: 10.1007/s00402-011-1289-2
85. Ruel HLM, Watanabe R, Evangelista MC, Beauchamp G, Auger J-P, Segura M, et al. Pain burden, sensory profile and inflammatory cytokines of dogs with naturally-occurring neuropathic pain treated with gabapentin alone or with meloxicam. PLoS ONE. (2020) 15:e0237121. doi: 10.1371/journal.pone.0237121
86. Fornasari D. Pharmacotherapy for neuropathic pain: a review. Pain Ther. (2017) 6(Suppl. 1):S25–33. doi: 10.1007/s40122-017-0091-4
87. Rose MA, Kam PCA. Gabapentin: pharmacology and its use in pain management. Anesthesia. (2002) 57:451–62. doi: 10.1046/j.0003-2409.2001.02399.x
88. Schmierer PA, Tünsmeyer J, Tipold A, Hartnack-Wilhelm S, Lesczuk P, Kästner SBR. Randomized controlled trial of pregabalin for analgesia after surgical treatment of intervertebral disc disease in dogs. Vet Surg. (2020) 49:905–13. doi: 10.1111/vsu.13411
89. Kukanich B, Cohen RL. Pharmacokinetics of oral gabapentin in greyhound dogs. Vet J. (2011) 187:133–5. doi: 10.1016/j.tvjl.2009.09.022
90. Salazar V, Dewey CW, Schwark W, Badgley BL, Gleed RD, Horne W, et al. Pharmacokinetics of single-dose oral pregabalin administration in normal dogs. Vet Anaesth Analg. (2009) 36:574–80. doi: 10.1111/j.1467-2995.2009.00486.x
91. Patel R, Dickenson AH. Mechanisms of the gabapentinoids and α 2 δ-1 calcium channel subunit in neuropathic pain. Pharma Res Per. (2016) 4:e00205. doi: 10.1002/prp2.205
92. Ohtori S, Inoue G, Orita S, Takaso M, Eguchi Y, Ochiai N, et al. Efficacy of combination of meloxicam and pregabalin for pain in knee osteoarthritis. Yonsei Med J. (2013) 54:1253–8. doi: 10.3349/ymj.2013.54.5.1253
93. Norkus C, Rankin D, Warner M, KuKanich B. Pharmacokinetics of oral amantadine in greyhound dogs. J Vet Pharmacol Ther. (2015) 38:305–8. doi: 10.1111/jvp.12190
94. KuKanich B. Outpatient Oral analgesics in dogs and cats beyond nonsteroidal Antiinflammatory drugs. an evidence-based approach. Vet Clin North Am - Small Anim Pract. (2013) 43:1109–25. doi: 10.1016/j.cvsm.2013.04.007
95. Towheed TE, Judd MJ, Hochberg MC, Wells G. Acetaminophen for osteoarthritis. Cochrane Database Syst Rev. (2003) 2:CD004257. doi: 10.1002/14651858.CD004257
96. Budsberg SC, Kleine SA, Norton MM, Sandberg GS, Papich MG. Comparison of the effects on lameness of orally administered acetaminophen-codeine and carprofen in dogs with experimentally induced synovitis. Am J Vet Res. (2020) 81:627–34. doi: 10.2460/ajvr.81.8.627
97. Malek S, Sample SJ, Schwartz Z, Nemke B, Jacobson PB, Cozzi EM, et al. Effect of analgesic therapy on clinical outcome measures in a randomized controlled trial using client-owned dogs with hip osteoarthritis. BMC Vet Res. (2012) 8:185. doi: 10.1186/1746-6148-8-185
98. Budsberg SC, Torres BT, Kleine SA, Sandberg GS, Berjeski AK. Lack of effectiveness of tramadol hydrochloride for the treatment of pain and joint dysfunction in dogs with chronic osteoarthritis. J Am Vet Med Assoc. (2018) 252:427–32. doi: 10.2460/javma.252.4.427
99. KuKanich B, Papich MG. Pharmacokinetics of tramadol and the metabolite O-desmethyltramadol in dogs. J Vet Pharmacol Ther. (2004) 27:239–46. doi: 10.1111/j.1365-2885.2004.00578.x
100. Eskafian H, Shojaee Tabrizi A, Ansari Lari M. Gastroscopic study of meloxicam, tramadol, and their combined administration on the development of gastric injuries in dogs. Top Companion Anim Med. (2017) 32:109–13. doi: 10.1053/j.tcam.2017.09.001
101. Vanderweerd JM, Coisnon C, Clegg P, Cambier C, Pierson A, Hontoir F, et al. Systematic review of efficacy of nutraceuticals to alleviate clinical signs of osteoarthritis. J Vet Intern Med. (2012) 26:448–56. doi: 10.1111/j.1939-1676.2012.00901.x
102. Comblain F, Serisier S, Barthelemy N, Balligand M, Henrotin Y. Review of dietary supplements for the management of osteoarthritis in dogs in studies from 2004 to 2014. J Vet Pharmacol Ther. (2016) 39:1–15. doi: 10.1111/jvp.12251
103. Helal NA, Eassa HA, Amer AM, Eltokhy MA, Edafiogho I, Nounou MI. Nutraceuticals' novel formulations: the good, the bad, the unknown and patents involved. Recent Pat Drug Deliv Formul. (2019) 13:105–56. doi: 10.2174/1872211313666190503112040
104. Russo EB, Hohmann AG. Role Of Cannabinoids In Pain Management. In: Deer TR, Leong MS, Buvanendran A, Gordin V, Kim PS, Panchal SJ, Ray AL, editors. Comprehensive Treatment of Chronic Pain by Medical, Interventional, and Integrative Approaches. New York, NY: Springer (2013). p. 181–97. doi: 10.1007/978-1-4614-1560-2_18
105. Kogan L, Hellyer P, Downing R. The use of cannabidiol-rich hemp oil extract to treat canine osteoarthritis-related pain: a pilot study. J Am Holistic Vet Med Assoc. (2020) 58:35–45.
106. Ruhaak LR, Felth J, Karlsson PC, Rafter JJ, Verpoorte R, Bohlin L. Evaluation of the cyclooxygenase inhibiting effects of six major cannabinoids isolated from Cannabis sativa. Biol Pharm Bull. (2011) 34:774–8. doi: 10.1248/bpb.34.774
107. Deabold KA, Schwark WS, Wolf L, Wakshlag JJ. Single-dose pharmacokinetics and preliminary safety assessment with use of CBD-rich hemp nutraceutical in healthy dogs and cats. Animals. (2019) 9:832. doi: 10.3390/ani9100832
108. Brioschi FA, Di Cesare F, Gioeni D, Rabbogliatti V, Ferrari F, D'Urso ES, et al. Oral transmucosal cannabidiol oil formulation as part of a multimodal analgesic regimen: effects on pain relief and quality of life improvement in dogs affected by spontaneous osteoarthritis. Animals. (2020) 10:1505. doi: 10.3390/ani10091505
109. Verrico CD, Wesson S, Konduri V, Hofferek CJ, Vazquez-Perez J, Blair E, et al. A randomized, double-blind, placebo-controlled study of daily cannabidiol for the treatment of canine osteoarthritis pain. Pain. (2020) 161:2191–202. doi: 10.1097/j.pain.0000000000001896
110. Meja S, Duerr FM, Griffenhagen G, McGrath S. Evaluation of the effect of cannabidiol on naturally occurring osteoarthritis-associated pain: a pilot study in dogs. J Am Anim Hosp Assoc. (2021) 57:81–90. doi: 10.5326/JAAHA-MS-7119
111. Bartner LR, McGrath S, Rao S, Hyatt LK, Wittenburg LA. Pharmacokinetics of cannabidiol administered by 3 delivery methods at 2 different dosages to healthy dogs. Can J Vet Res. (2018) 82:178–83.
112. Mosley C, Gaynor J, Cital S, Brassard J. Cannabinoids for pain management. In: Cital S, Kramer K, Hughston L, Gaynor JS, editors. Cannabis Therapy in Veterinary Medicine. Cham: Springer (2021). p. 117–41. doi: 10.1007/978-3-030-68317-7_5
113. Nagarkatti P, Pandey R, Rieder SA, Hegde VL, Nagarkatti M. Cannabinoids as novel anti-inflammatory drugs. Future Med Chem. (2009) 1:1333–49. doi: 10.4155/fmc.09.93
114. Nichols JM, Kaplan BLF. Immune responses regulated by cannabidiol. Cannabis Cannabinoid Res. (2020) 5:12–31. doi: 10.1089/can.2018.0073
115. Giorgi V, Marotto D, Batticciotto A, Atzeni F, Bongiovanni S, Sarzi-Puttini P. Cannabis and autoimmunity: possible mechanisms of action. Immunotargets Ther. (2021) 10:261–71. doi: 10.2147/ITT.S267905
116. Verbruggen G. Chondroprotective drugs in degenerative joint diseases. Rheumatology. (2006) 45:129–38. doi: 10.1093/rheumatology/kei171
117. Bhathal A, Spryszak M, Louizos C, Frankel G. Glucosamine and chondroitin use in canines for osteoarthritis: a review. Open Vet J. (2017) 7:36–49. doi: 10.4314/ovj.v7i1.6
118. Anderson CC, Cook JL, Kreeger JM, Tomlinson JL, Wagner-Mann CC. In vitro effects of glucosamine and acetylsalicylate on canine chondrocytes in three-dimensional culture. Am J Vet Res. (1999) 60:1546–51.
119. Beale BS. Use of nutraceuticals and chondroprotectants in osteoarthritic dogs and cats. Vet Clin North Am Small Anim Pract. (2004) 34:271–89. doi: 10.1016/j.cvsm.2003.09.008
120. Henrotin Y, Sanchez C, Balligand M. Pharmaceutical and nutraceutical management of canine osteoarthritis: present and future perspectives. Vet J. (2005) 170:113–23. doi: 10.1016/j.tvjl.2004.08.014
121. Altman R6D. Glucosamine therapy for knee osteoarthritis: pharmacokinetic considerations. Expert Rev Clin Pharmacol. (2009) 2:359–71. doi: 10.1586/ecp.09.17
122. Maxwell LK, Regier P, Achanta S. Comparison of glucosamine absorption after administration of oral liquid, chewable, and tablet formulations to dogs. J Am Anim Hosp Assoc. (2016) 52:90–4. doi: 10.5326/JAAHA-MS-6267
123. Adebowale A, Du J, Liang Z, Leslie JL, Eddington ND. The bioavailability and pharmacokinetics of glucosamine hydrochloride and low molecular weight chondroitin sulfate after single and multiple doses to beagle dogs. Biopharm Drug Dispos. (2002) 23:217–25. doi: 10.1002/bdd.315
124. Musco N, Vassalotti G, Mastellone V, Cortese L, della Rocca G, Molinari ML, et al. Effects of a nutritional supplement in dogs affected by osteoarthritis. Vet Med Sci. (2019) 5:325–35. doi: 10.1002/vms3.182
125. Dobenecker B, Beetz Y, Kienzle E. A placebo-controlled double-blind study on the effect of nutraceuticals (chondroitin sulfate and mussel extract) in dogs with joint diseases as perceived by their owners. J Nutr. (2002) 132:1690S−1S. doi: 10.1093/jn/132.6.1690S
126. Moreau M, Dupuis J, Bonneau NH, Desnoyers M. Clinical evaluation of a nutraceutical, carprofen and meloxicam for the treatment of dogs with osteoarthritis. Vet Rec. (2003) 152:323–9. doi: 10.1136/vr.152.11.323
127. McCarthy G, O'Donovan J, Jones B, McAllister H, Seed M, Mooney C. Randomized double-blind, positive-controlled trial to assess the efficacy of glucosamine/chondroitin sulfate for the treatment of dogs with osteoarthritis. Vet J. (2007) 174:54–61. doi: 10.1016/j.tvjl.2006.02.015
128. D'Altilio M, Peal A, Alvey M, Simms C, Curtsinger A, Gupta RC, et al. Therapeutic efficacy and safety of undenatured type ii collagen singly or in combination with glucosamine and chondroitin in arthritic dogs. Toxicol Mech Methods. (2007) 17:189–96. doi: 10.1080/15376510600910469
129. Gupta RC, Canerdy TD, Lindley J, Konemann M, Minniear J, Carroll BA, et al. Comparative therapeutic efficacy and safety of type-II collagen (UC-II), glucosamine and chondroitin in arthritic dogs: pain evaluation by ground force plate. J Anim Physiol Anim Nutr (Berl). (2012) 96:770–7. doi: 10.1111/j.1439-0396.2011.01166.x
130. Alves JC, Santos AM, Jorge PI. Effect of an oral joint supplement when compared to carprofen in the management of hip osteoarthritis in working dogs. Top Companion Anim Med. (2017) 32:126–9. doi: 10.1053/j.tcam.2017.10.003
131. Scott RM, Evans R, Conzemius MG. Efficacy of an oral nutraceutical for the treatment of canine osteoarthritis. Vet Comp Orthop Traumatol. (2017) 30:318–23. doi: 10.3415/VCOT-17-02-0020
132. Sul RM, Chase D, Parkin T, Bennett D. Comparison of meloxicam and a glucosamine-chrondroitin supplement in management of feline osteoarthritis. Vet Comp Orthop Traumatol. (2014) 27:20–6. doi: 10.3415/VCOT-12-11-0139
133. Meulyzer M, Vachon P, Beaudry F, Vinardell T, Richard H, Beauchamp G, et al. Comparison of pharmacokinetics of glucosamine and synovial fluid levels following administration of glucosamine sulphate or glucosamine hydrochloride. Osteoarthritis Cartilage. (2008) 16:973–9. doi: 10.1016/j.joca.2008.01.006
134. Johnson KA, Hulse DA, Hart RC, Kochevar D, Chu Q. Effects of an orally administered mixture of chondroitin sulfate, glucosamine hydrochloride and manganese ascorbate on synovial fluid chondroitin sulfate 3B3 and 7D4 epitope in a canine cruciate ligament transection model of osteoarthritis. Osteoarthritis Cartilage. (2001) 9:14–21. doi: 10.1053/joca.2000.0345
135. Canapp SO Jr, McLaughlin RM Jr, Hoskinson JJ, Roush JK, Butine MD. Scintigraphic evaluation of dogs with acute synovitis after treatment with glucosamine hydrochloride and chondroitin sulfate. Am J Vet Res. (1999) 60:1552–7.
136. Christensen R, Bartels EM, Astrup A, Bliddal H. Symptomatic efficacy of avocado-soybean unsaponifiables (ASU) in osteoarthritis (OA) patients: a meta-analysis of randomized controlled trials. Osteoarthritis Cartilage. (2008) 16:399–408. doi: 10.1016/j.joca.2007.10.003
137. Henrotin YE, Deberg MA, Crielaard JM, Piccardi N, Msika P, Sanchez C. Avocado/soybean unsaponifiables prevent the inhibitory effect of osteoarthritic subchondral osteoblasts on aggrecan and type II collagen synthesis by chondrocytes. J Rheumatol. (2006) 33:1668–78.
138. Henrotin YE, Labasse AH, Jaspar JM, De Groote DD, Zheng SX, Guillou GB, et al. Effects of three avocado/soybean unsaponifiable mixtures on metalloproteinases, cytokines and prostaglandin E2 production by human articular chondrocytes. Clin Rheumatol. (1998) 17:31–9. doi: 10.1007/BF01450955
139. Simental-Mendia M, Sanchez-Garcia A, Acosta-Olivo CA, Vichez-Cavazos F, Osuna-Garate J, Pena-Martinez VM, et al. Efficacy and safety of avocado-soybean unsaponifiables for the treatment of hip and knee osteoarthritis: a systematic review and meta-analysis of randomized placebo-controlled trials. Int J Rheum Dis. (2019) 22:1607–15. doi: 10.1111/1756-185X.13658
140. Boileau C, Martel-Pelletier J, Caron J, Msika P, Guillou GB, Baudouin C, et al. Protective effects of total fraction of avocado/soybean unsaponifiables on the structural changes in experimental dog osteoarthritis: inhibition of nitric oxide synthase and matrix metalloproteinase-13. Arthritis Res Ther. (2009) 11:R41. doi: 10.1186/ar2649
141. Altinel L, Saritas ZK, Kose KC, Pamuk K, Aksoy Y, Serteser M. Treatment with unsaponifiable extracts of avocado and soybean increases TGF beta1 and TGF beta2 levels in canine joint fluid. Tohoku J Exp Med. (2007) 211:181–6. doi: 10.1620/tjem.211.181
142. Ruff KJ, DeVore DP. Reduction of pro-inflammatory cytokines in rats following 7-day oral supplementation with a proprietary eggshell membrane-derived product. Mod Res Inflamm. (2014) 3:19–25. doi: 10.4236/mri.2014.31003
143. Aguirre A, Gil-Quintana E, Fenaux M, Sanchez N, Torre C. The efficacy of Ovopet® in the treatment of hip dysplasia in dogs. J Vet Med Anim Health. (2018) 10:198–207. doi: 10.5897/JVMAH2018.0687
144. Benson KF, Ruff KJ, Jensen GS. Effects of natural eggshell membrane (NEM) on cytokine production in cultures of peripheral blood mononuclear cells: increased suppression of tumor necrosis factor-α levels after in vitro digestion. J Med Food. (2012) 15:360–8. doi: 10.1089/jmf.2011.0197
145. Ruff KJ, Kopp KJ, Von Behrens P, Lux M, Mahn M, Back M. Effectiveness of NEM® brand eggshell membrane in the treatment of suboptimal joint function in dogs: a multicenter, randomized, double-blind, placebo-controlled study. Vet Med. (2016) 7:113–21. doi: 10.2147/VMRR.S101842
146. Muller C, Enomoto M, Buono A, Steiner JM, Lascelles BDX. Placebo-controlled pilot study of the effects of an eggshell membrane-based supplement on mobility and serum biomarkers in dogs with osteoarthritis. Vet J. (2019) 253:105379. doi: 10.1016/j.tvjl.2019.105379
147. Kumagai K, Shirabe S, Miyata N, Murata M, Yamauchi A, Kataoka Y, et al. Sodium pentosan polysulfate resulted in cartilage improvement in knee osteoarthritis–an open clinical trial. BMC Clin Pharmacol. (2010) 10:7. doi: 10.1186/1472-6904-10-7
148. Ghosh P. The pathobiology of osteoarthritis and the rationale for the use of pentosan polysulfate for its treatment. Semin Arthritis Rheum. (1999) 28:211–67. doi: 10.1016/S0049-0172(99)80021-3
149. Wijekoon H, Bwalya EC, Fang J, Kim S, Hosoya K, Okumura M. Inhibitory effects of sodium pentosan polysulfate on formation and function of osteoclasts derived from canine bone marrow. BMC Vet Res. (2018) 14:152. doi: 10.1186/s12917-018-1466-4
150. Budsberg SC, Bergh MS, Reynolds LR, Streppa HK. Evaluation of pentosan polysulfate sodium in the postoperative recovery from cranial cruciate injury in dogs: a randomized, placebo-controlled clinical trial. Vet Surg. (2007) 36:234–44. doi: 10.1111/j.1532-950X.2007.00256.x
151. Siddiqui MZ. Boswellia serrata, a potential antiinflammatory agent: an overview. Indian J Pharm Sci. (2011) 73:255–61. doi: 10.4103/0250-474X.93507
152. Kreck C, Saller R. Indischer Weihrauch und seine Zubereitungen einschliesslich H15 als traditionelles und modernes Therapeutikum. Internist Prax. (1998) 38:857–72.
153. Gayathri B, Manjula N, Vinaykumar KS, Lakshmi BS, Balakrishnan A. Pure compound from Boswellia serrata extract exhibits anti-inflammatory property in human PBMCs and mouse macrophages through inhibition of TNFalpha, IL-1beta, NO and MAP kinases. Int Immunopharmacol. (2007) 7:473–82. doi: 10.1016/j.intimp.2006.12.003
154. Sharma S, Thawani V, Hingorani L, Shrivastava M, Bhate VR, Khiyani R. Pharmacokinetic study of 11-keto beta-Boswellic acid. Phytomedicine. (2004) 11:255–60. doi: 10.1078/0944-7113-00290
155. Reichling J, Schmökel H, Fitzi J, Bucher S, Saller R. Dietary support with Boswellia resin in canine inflammatory joint and spinal disease. Schweiz Arch Tierheilk. (2004) 146:71–9. doi: 10.1024/0036-7281.146.2.71
156. Kimmatkar N, Thawani V, Hongorani L, Khiyani R. Efficacy and tolerability of Bosewellia serrata extract in treatment of osteoarthritis of knee—a randomized double blind placebo-controlled trial. Phytomedicine. (2003) 10:3–7. doi: 10.1078/094471103321648593
157. Innes JF, Fuller CJ, Grover ER, Kelly AL, Burn JF. Randomized, double-blind, placebo-controlled parallel group study of P54FP for the treatment of dogs with osteoarthritis. Vet Rec. (2003) 152:457–60. doi: 10.1136/vr.152.15.457
158. Comblain F, Barthélémy N, Lefèbvre M, Schwartz C, Lesponne I, Serisier S, et al. A randomized, double-blind, prospective, placebo-controlled study of the efficacy of a diet supplemented with curcuminoids extract, hydrolyzed collagen and green tea extract in owner's dogs with osteoarthritis. BMC Vet Res. (2017) 13:395. doi: 10.1186/s12917-017-1317-8
159. Moreau M, Lussier B, Pelletier J-P, Martel-Pelletier J, Bédard C, Gauvin D, et al. A medicinal herb-based natural health product improves the condition of a canine natural osteoarthritis model: a randomized placebo-controlled trial. Res Vet Sci. (2014) 97:574–81. doi: 10.1016/j.rvsc.2014.09.011
160. Whittem T, Richards L, Alexander J, Beck C, Knight C, Milne M, et al. A randomised controlled masked clinical trial of two treatments for osteoarthritis in dogs. Aust Vet J. (2021) 99:267–72. doi: 10.1111/avj.13066
161. Beths T, Munn R, Bauquier S, Mitchell P, Whittem T. A pilot study of 4CYTE™ Epiitalis® Forte, a novel nutraceutical, in the management of naturally occurring osteoarthritis in dogs. Aust Vet J. (2020) 98:591–5. doi: 10.1111/avj.13024
162. Deparle LA, Gupta RC, Canerdy TD, Goad JT, D'Altilio M, Bagchi M, et al. Efficacy and safety of glycosylated undenatured type-II collagen (UC-II) in therapy of arthritic dogs. J Vet Pharmacol Ther. (2005) 28:385–90. doi: 10.1111/j.1365-2885.2005.00668.x
163. Gencoglu H, Orhan C, Sahin E, Sahin K. Undenatured Type II Collagen (UC-II) in joint health and disease: a review on the current knowledge of companion animals. Animals. (2020) 10:697. doi: 10.3390/ani10040697
164. Stabile M, Samarelli R, Trerotoli P, Fracassi L, Lacitignola L, Crovace A, et al. Evaluation of the effects of Undenatured Type II collagen (UC-II) as compared to robenacoxib on the mobility impairment induced by osteoarthritis in dogs. Vet Sci. (2019) 6:72. doi: 10.3390/vetsci6030072
165. Moreau M, Dupuis J, Bonneau NH, Lécuyer M. Clinical evaluation of a powder of quality elk velvet antler for the treatment of osteoarthrosis in dogs. Can Vet J. (2004) 45:133–9.
166. Boileau C, Martel-Pelletier J, Caron J, Paré F, Troncy E, Moreau M, et al. Oral treatment with a Brachystemma calycinum D don plant extract reduces disease symptoms and the development of cartilage lesions in experimental dog osteoarthritis: inhibition of protease-activated receptor 2. Ann Rheum Dis. (2010) 69:1179–84. doi: 10.1136/ard.2009.110965
167. Moreau M, Lussier B, Pelletier J-P, Martel-Pelletier J, Bédard C, Gauvin D, et al. Brachystemma calycinum D. don effectively reduces the locomotor disability in dogs with naturally occurring osteoarthritis: a randomized placebo-controlled trial. Evidence-Based Compl Alt Med. (2012) 2012:646191. doi: 10.1155/2012/646191
168. Kampa N, Jitpean S, Seesupa S, Hoisang S. Penetration depth study of 830 nm low-intensity laser therapy on living dog tissue. Vet World. (2020) 13:1417–22. doi: 10.14202/vetworld.2020.1417-1422
169. Hochman-Elam LN, Heidel RE, Shmalberg JW. Effects of laser power, wavelength, coat length, and coat color on tissue penetration using photobiomodulation in healthy dogs. Can J Vet Res. (2020) 84:131–7.
170. Pryor B, Millis DL. Therapeutic laser in veterinary medicine. Vet Clin North Am Small Anim Pract. (2015) 45:45–56. doi: 10.1016/j.cvsm.2014.09.003
171. Hochman L. Photobiomodulation therapy in veterinary medicine: a review. Top Companion Anim Med. (2018) 33:83–8. doi: 10.1053/j.tcam.2018.06.004
172. Barale L, Monticelli P, Raviola M, Adami C. Preliminary clinical experience of low-level laser therapy for the treatment of canine osteoarthritis-associated pain: a retrospective investigation on 17 dogs. Open Vet J. (2020) 10:116–9. doi: 10.4314/ovj.v10i1.16
173. Barger BK, Bisges AM, Fox DB, Torres B. Low-level laser therapy for osteoarthritis treatment in dogs at missouri veterinary practice. J Am Anim Hosp Assoc. (2020) 56:139–45. doi: 10.5326/JAAHA-MS-6851
174. Hegedus B, Viharos L, Gervain M, Gálfi M. The effect of low-level laser in knee osteoarthritis: a double-blind, randomized, placebo-controlled trial. Photomed Laser Surg. (2009) 27:577–84. doi: 10.1089/pho.2008.2297
175. Stausholm MB, Naterstad IF, Joensen J, Lopes-Martins RÁB, Sæbø H, Lund H, et al. Efficacy of low-level laser therapy on pain and disability in knee osteoarthritis: systematic review and meta-analysis of randomised placebo-controlled trials. BMJ Open. (2019) 9:e031142. doi: 10.1136/bmjopen-2019-031142
176. Silva NEOF, Luna SPL, Joaquim JGF, Coutinho HD, Possebon FS. Effect of acupuncture on pain and quality of life in canine neurological and musculoskeletal diseases. Can Vet J. (2017) 58:941–51.
177. Selfe TK, Taylor AG. Acupuncture and osteoarthritis of the knee: a review of randomized, controlled trials. Fam Community Health. (2008) 31:247–54. doi: 10.1097/01.FCH.0000324482.78577.0f
178. Madsen MV, Gotzsche PC, Hrobjartsson A. Acupuncture treatment for pain: systematic review of randomized clinical trials with acupuncture, placebo acupuncture, and no acupuncture groups. BMJ. (2009) 338:a3115. doi: 10.1136/bmj.a3115
179. Wang T, Xie W, Ye W, He C. Effects of electromagnetic fields on osteoarthritis. Biomed Pharmacother. (2019) 118:109282. doi: 10.1016/j.biopha.2019.109282
180. Nelson FR, Zvirbulis R, Pilla AA. Non-invasive electromagnetic field therapy produces rapid and substantial pain reduction in early knee osteoarthritis: a randomized double-blind pilot study. Rheumatol Int. (2013) 33:2169–73. doi: 10.1007/s00296-012-2366-8
181. Wu Z, Ding X, Lei G, Zeng C, Wei J, Li J, et al. Efficacy and safety of the pulsed electromagnetic field in osteoarthritis: a meta-analysis. BMJ Open. (2018) 8:e022879. doi: 10.1136/bmjopen-2018-022879
182. Gaynor JS, Hagberg S, Gurfein BT. Veterinary applications of pulsed electromagnetic field therapy. Res Vet Sci. (2018) 119:1–8. doi: 10.1016/j.rvsc.2018.05.005
183. Dahlberg J, Fitch G, Evans RB, McClure SR, Conzemius M. The evaluation of extracorporeal shockwave therapy in naturally occurring osteoarthritis of the stifle joint in dogs. Vet Comp Orthop Traumatol. (2005) 18:147–52. doi: 10.1055/s-0038-1632954
184. Becker W, Kowaleski MP, McCarthy RJ, Blake CA. Extracorporeal shockwave therapy for shoulder lameness in dogs. J Am Anim Hosp Assoc. (2015) 51:15–9. doi: 10.5326/JAAHA-MS-6175
185. Souza ANA, Ferreira MP, Hagen SCF, Patricio GCF, Matera JM. Radial shock wave therapy in dogs with hip osteoarthritis. Vet Comp Orthop Traumatol. (2016) 29:108–14. doi: 10.3415/VCOT-15-01-0017
186. Hauser RA. The deterioration of articular cartilage in osteoarthritis by corticosteroid injections. J. Prolotherapy. (2009) 1:107–23.
187. Franklin SP, Franklin AL. Randomized controlled trial comparing autologous protein solution to hyaluronic acid plus triamcinolone for treating hip osteoarthritis in dogs. Front Vet Sci. (2021) 8:713768. doi: 10.3389/fvets.2021.713768
188. Alves JC, Santos A, Jorge P, Lavrador C, Carreira LM. The intra-articular administration of triamcinolone hexacetonide in the treatment of osteoarthritis. its effects in a naturally occurring canine osteoarthritis model. PLoS ONE. (2021) 16:e0245553. doi: 10.1371/journal.pone.0245553
189. Kuroki K, Cook JL, Kreeger JM. Mechanisms of action and potential uses of hyaluronan in dogs with osteoarthritis. J Am Vet Med Assoc. (2002) 221:944–50. doi: 10.2460/javma.2002.221.944
190. Hellström L-E, Carlsson C, Boucher JF, Michanek P. Intra-articular injections of high molecular weight sodium hyaluronate as a therapy for canine arthritis. Vet Rec. (2003) 153:89–90. doi: 10.1136/vr.153.3.89
191. Alves JC, dos Santos AMMP, Jorge P, Lavrador CFTVB, Carreira LM. Effect of a single intra-articular high molecular weight hyaluronan in a naturally occurring canine osteoarthritis model: a randomized controlled trial. J Orthop Surg Res. (2021) 16:290. doi: 10.1186/s13018-021-02423-4
192. Abrams GD, Frank RM, Fortier LA, Cole BJ. Platelet-rich plasma for articular cartilage repair. Sports Med Arthrosc Rev. (2013) 21:213–19. doi: 10.1097/JSA.0b013e3182999740
193. Carr BJ, Canapp SO Jr, Mason DR, Cox C, Hess T. Canine platelet-rich plasma systems: a prospective analysis. Front Vet Sci. (2016) 2:73. doi: 10.3389/fvets.2015.00073
194. Braun HJ, Kim HJ, Chu CR, Dragoo JL. The effect of platelet-rich plasma formulations and blood products on human synoviocytes. Am J Sports Med. (2014) 42:1204–10. doi: 10.1177/0363546514525593
195. Franklin SP, Cook JL. Prospective trial of autologous conditioned plasma versus hyaluronan plus corticosteroid for elbow osteoarthritis in dogs. Can Vet J. (2013) 54:881–4.
196. Vilar JM, Manera MA, Santana A, Spinella G, Rodriguez O, Rubio M, et al. Effect of leukocyte-reduced platelet-rich plasma on osteoarthritis caused by cranial cruciate ligament rupture: a canine gait analysis model. PLoS ONE. (2018) 13:e0194752. doi: 10.1371/journal.pone.0194752
197. Cuervo B, Rubio M, Chicharro D, Damiá E, Santana A, Carrillo JM, et al. Objective comparison between platelet rich plasma alone and in combination with physical therapy in dogs with osteoarthritis caused by hip dysplasia. Animals. (2020) 10:175. doi: 10.3390/ani10020175
198. Alves JC, Santos A, Jorge P. Platelet-rich plasma therapy in dogs with bilateral hip osteoarthritis. BMC Vet Res. (2021) 17:207. doi: 10.1186/s12917-021-02913-x
199. Catarino J, Carvalho P, Santos S, Martins Â, Requicha J. Treatment of canine osteoarthritis with allogeneic platelet-rich plasma: review of five cases. Open Vet J. (2020) 10:226–31. doi: 10.4314/ovj.v10i2.12
200. Fahie MA, Ortolano GA, Guercio V, Schaffer JA, Johnston G, Au J, et al. A randomized controlled trial of the efficacy of autologous platelet therapy for the treatment of osteoarthritis in dogs. J Am Vet Med Assoc. (2013) 243:1291–7. doi: 10.2460/javma.243.9.1291
201. Alves JC, Santos A, Jorge P, Lavrador C, Carreira LM. A report on the use of a single intra-articular administration of autologous platelet therapy in a naturally occurring canine osteoarthritis model - a preliminary study. BMC Musculoskelet Disord. (2020) 21:127. doi: 10.1186/s12891-020-3140-9
202. Wanstrath AW, Hettlich BF, Su L, Smith A, Zekas LJ, Allen MJ, et al. Evaluation of a single intra-articular injection of autologous protein solution for treatment of osteoarthritis in a canine population. Vet Surg. (2016) 45:764–74. doi: 10.1111/vsu.12512
203. King W, Cawood K, Bookmiller M. The use of autologous protein solution (Pro-Stride®) and leukocyte-rich platelet-rich plasma (Restigen®) in canine medicine. Vet Med Res Rep. (2021) 12:53–65. doi: 10.2147/VMRR.S286913
204. Boffa A, Salerno M, Merli G, De Girolamo L, Laver L, Magalon J, et al. Platelet-rich plasma injections induce disease-modifying effects in the treatment of osteoarthritis in animal models. Knee Surg Sports Traumatol Arthrosc. (2021) 29:4100–21. doi: 10.1007/s00167-021-06659-9
205. Alves JC, Santos A, Jorge P, Lavrador C, Carreira LM. Intraarticular triamcinolone hexacetonide, stanozolol, Hylan G-F 20 and platelet concentrate in a naturally occurring canine osteoarthritis model. Sci Rep. (2021) 11:3118. doi: 10.1038/s41598-021-82795-z
206. Black LL, Gaynor J, Gahring D, Adams C, Aron D, Harman S, et al. Effect of adipose-derived mesenchymal stem and regenerative cells on lameness in dogs with chronic osteoarthritis of the coxofemoral joints: a randomized, double-blinded, multicenter, controlled trial. Vet Ther. (2007) 8:272–84.
207. Black LL, Gaynor J, Adams C, Dhupa S, Sams AE, Taylor R, et al. Effect of intraarticular injection of autologous adipose-derived mesenchymal stem and regenerative cells on clinical signs of chronic osteoarthritis of the elbow joint in dogs. Vet Ther. (2008) 9:192–200.
208. Vilar JM, Batista M, Morales M, Santana A, Cuervo B, Rubio M, et al. Assessment of the effect of intraarticular injection of autologous adipose-derived mesenchymal stem cells in osteoarthritic dogs using a double blinded force platform analysis. BMC Vet Res. (2014) 10:143. doi: 10.1186/1746-6148-10-143
209. Kriston-Pal É, Czibula A, Gyuris Z, Balka G, Seregi A, Sükösd F, et al. Characterization and therapeutic application of canine adipose mesenchymal stem cells to treat elbow osteoarthritis. Can J Vet Res. (2017) 81:73–8.
210. Zeira O, Scaccia S, Pettinari L, Ghezzi E, Asiag N, Martinelli L, et al. Intra-articular administration of autologous micro-fragmented adipose tissue in dogs with spontaneous osteoarthritis: safety, feasibility, and clinical outcomes. Stem Cells Transl Med. (2018) 7:819–28. doi: 10.1002/sctm.18-0020
211. Shah K, Drury T, Roic I, Hansen P, Malin M, Boyd R, et al. Outcome of allogeneic adult stem cell therapy in dogs suffering from osteoarthritis and other joint defects. Stem Cells Int. (2018) 2018:7309201. doi: 10.1155/2018/7309201
212. Cabon Q, Febre M, Gomez N, Cachon T, Pillard P, Carozzo C, et al. Long-term safety and efficacy of simgle or repeated intra-articular injection of allogeneic neonatal mesenchymal stromal cells for managing pain and lameness in moderate to severe canine osteoarthritis without anti-inflammatory pharmacological support: pilot clinical study. Front Vet Sci. (2019) 6:10. doi: 10.3389/fvets.2019.00010
213. Heikkilä HM, Hielm-Bjökman AK, Morelius M, Larsen S, Honkavaara J, Innes JF, et al. Intra-articular botulinum toxin A for the treatment of osteoarthritic joint pain in dogs: a randomized, double-blinded, placebo-controlled clinical trial. Vet J. (2014) 200:162–9. doi: 10.1016/j.tvjl.2014.01.020
214. Nicacio GM, Luna SPL, Cavaleti P, Cassu N. Intra-articular botulinum toxin A (BoNT/A) for pain management in dogs with osteoarthritis secondary to hip dysplasia: a randomized controlled clinical trial. J Vet Med Sci. (2019) 81:411–7. doi: 10.1292/jvms.18-0506
215. Aulakh KS, Lopez MJ, Hudson C, Gaschen L, Fabiani M, Beale B, et al. Prospective clinical evaluation of intra-articular injection of Tin-117m (117mSn) radiosynoviorthesis agent for management of naturally occurring elbow osteoarthritis in dogs: a pilot study. Vet Med. (2021) 12:117–28. doi: 10.2147/VMRR.S295309
216. Iadarola MJ, Sapio MR, Raithel SJ, Mannes AJ, Cimino Brown D. Long-term pain relief in canine osteoarthritis by a single intra-articular injection of resiniferatoxin, a potent TRPV1 agonist. Pain. (2018) 159:2105–14. doi: 10.1097/j.pain.0000000000001314
217. Liotta AP, Girod M, Peeters D, Sandersen C, Couvreur T, Bolen G. Clinical effects of computed tomography-guided lumbosacral facet joint, transforaminal epidural, and translaminar epidural injections of methylprednisolone acetate in healthy dogs. Am J Vet Res. (2016) 77:1132–1139. doi: 10.2460/ajvr.77.10.1132
218. Janssens L, Beosier Y, Daems R. Lumbosacral degenerative stenosis in the dog. the results of epidural infiltration with methylprednisolone acetate: a retrospective study. Vet Comp Orthop Traumatol. (2009) 22:486–91. doi: 10.3415/VCOT-08-07-0055
Keywords: osteoarthritis, physical rehabilitation, weight management, non-steroidal anti-inflammatories, nutra- ceuticals, canine, treatment guidelines
Citation: Mosley CI, Edwards T, Romano L, Truchetti G, Dunbar L, Schiller T, Gibson T, Bruce C and Troncy E (2022) Proposed Canadian Consensus Guidelines on Osteoarthritis Treatment Based on OA-COAST Stages 1–4. Front. Vet. Sci. 9:830098. doi: 10.3389/fvets.2022.830098
Received: 06 December 2021; Accepted: 21 March 2022;
Published: 26 April 2022.
Edited by:
Denis J. Marcellin-Little, University of California, Davis, United StatesReviewed by:
Joseph Wakshlag, Cornell University, United StatesCopyright © 2022 Mosley, Edwards, Romano, Truchetti, Dunbar, Schiller, Gibson, Bruce and Troncy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Conny Mosley, Y29ubnltb3NsZXlAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.