
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Vet. Sci. , 03 March 2022
Sec. Veterinary Humanities and Social Sciences
Volume 9 - 2022 | https://doi.org/10.3389/fvets.2022.775411
Veterinarians are established public health professionals, committing to promote public health when they take their veterinary oath. The issue of climate change and its impact on planetary health is vital to public health, and therefore, it is critical that climate change is regarded as within the veterinary scope of practice. However, climate change is a multi-faceted issue which requires interdisciplinary collaboration and integrated stakeholder involvement in order to establish effective solutions and impactful policies. As a result, in this perspective, we discuss how policy is critical to support veterinarians in the climate change space and argue that more explicit support is needed for veterinarians to take an active role in climate change adaption, resilience, and mitigation. We address the discrepancies between the human health and veterinary professions with respect to providing policy support and capacity for practitioners to be stewards to promote planetary health and shed light on the lack of veterinary capacity in this area. We stress that veterinary professional societies are well equipped to bolster their policies, expand education for veterinary professionals and students in policy and advocacy, and establish calls to action to address climate change and planetary health issues. Ultimately, as public health professionals, veterinarians are uniquely poised to be contributors to climate change solutions and they should be actively involved in policy decision-making and empowered to take active roles in interdisciplinary conversations surrounding this important issue.
Veterinarians are critical public health professionals. Veterinary practitioners in the United States (U.S.) and across the globe, regardless of sector, commit to promoting public health when they take their veterinary oath (1–3). The nature of veterinary training inherently promotes an interdisciplinary approach to solving global health problems, including integrated use of public health practices such as disease detection, reporting, and surveillance, as well as health education and prevention (1). It is well established that the health of animals contributes to the health of humans, and vice versa, in multiple notable areas, by protecting against zoonotic disease, bolstering a sustainable food supply, fostering the human-animal bond, and preserving ecological systems (4, 5). Involving veterinarians in decision making has significant advantages over tackling problems in health professional silos, as has been the case for coordinated human and animal vaccination efforts against zoonoses, integrated diagnostic laboratory infrastructure, and integrated surveillance and response to disease outbreaks (6). The importance of interdisciplinary collaboration, including veterinarians, to solve global health problems has been exemplified with COVID-19. The issue of climate change and its impact on planetary health is no different.
Recent commentary has stressed the need for veterinarians to acknowledge climate change as within their scope of practice, redefine their roles in the climate change space, and take ownership and active roles as stewards of climate change adaptation and resilience (7). As Figure 1 demonstrates, several aspects of climate change impact public health and veterinary practice. Ultimately, climate change is a public health problem, veterinarians are public health professionals, and, thus, climate change and the promotion of planetary health are veterinary issues. However, these kinds of activities cannot be conducted within a vacuum, and support from cross-sector collaborations, stakeholders, and policy are critical for veterinarians to be effective stewards in this area (4, 7). Gaps must be bridged between veterinary practice and policy decision-making to ensure veterinarians are supported in public health capacities. In this perspective, we discuss the importance of policy to support veterinarians in the climate space and argue that policies should more explicitly support the role of veterinarians and prepare them to take climate action.
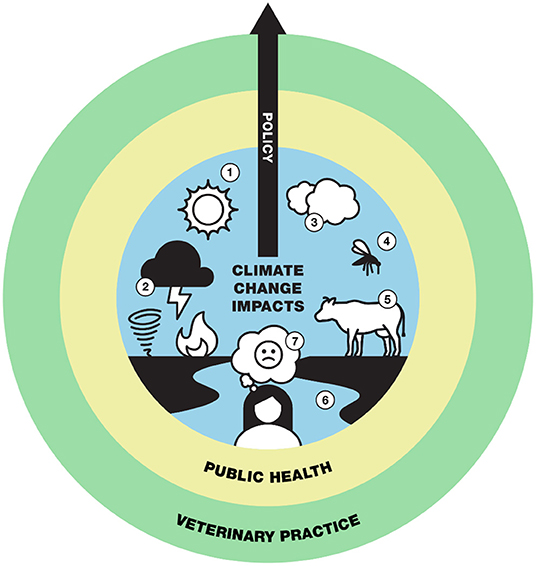
Figure 1. Policies already exist which highlight issues impacted by climate and which fall within a One Health and planetary health framework. These issues include (1) increasing temperature, (2) extreme weather events, (3) air quality, (4) vector-borne disease, (5) food safety/security, (6) water-related health issues, and (7) mental health. These issues are not independent and should be framed within policy as climate change issues. Further, climate change issues are within the scope of public health, which is within the scope of veterinary practice. Policy is a bridge and transcendent tool that spans all spheres and has the ability to build veterinary capacity and empower the profession to be climate change stewards and protect planetary health.
Policy is a vital tool for all health practitioners, including veterinarians. There are two explicit ways in which science and policy interface, science for policy and policy for science (8). Clinical knowledge, expertise in global public health issues, understanding of zoonotic disease transmission, and translational research efforts using animal models are all examples of areas in which the knowledge acquired through veterinary training can be used to help inform legislative decisions that require scientific and clinical expertise (science for policy). However, policy is also generated which impacts how veterinary practice is conducted (policy for science). Policy for science shapes how drugs are dispensed, the regulation of generated waste, drug compounding, tax laws for small businesses, employee healthcare programs, loan repayment programs, the nature of a veterinary-client-patient relationship, ethical responsibilities for a veterinarian, legal definitions of animals, occupational requirements, and modalities of practice, such as telemedicine. Spanning the practitioner-policy boundary is critical for veterinary medicine, ensuring policy decisions are rooted in evidence and are relevant to everyday practice. Effective, efficient, transparent, responsive, and proportionate policies require continuous evolution and evaluation based on current contexts (4). Through education and practice, veterinarians become competent and employ skills in clinical reasoning, individual animal and population health, public health, communication, collaboration, ethics, and workplace management. As a result, veterinary practitioners are uniquely equipped to provide the breadth of on-the-ground perspectives to inform policy affecting human, animal, and environmental health, or One Health. There is a clear, recognized need to establish and build capacity to support veterinarians in the policy space.
Policy for veterinary medicine in the U.S. originates from multiple avenues, including at the federal, state, and local level. The American Veterinary Medical Association (AVMA) is the professional society whose mission includes advocating for its members to advance the science and practice of veterinary medicine including supporting stewardship and promotion of public health (9). The AVMA closely monitors all federal and state legislation currently being discussed and comes to consensus positions to support, watch, or oppose proposed legislation. The AVMA relies heavily on volunteer committees and councils to inform policy decision-making and to inform how the Government Relations Division advocates for veterinary medicine on Capitol Hill in Washington, D.C. AVMA brokers critical meetings with stakeholder organizations, including government agencies, trade organizations, industry, and professional societies to ensure that policy most accurately supports its veterinary membership. Policies created by the AVMA cover the breadth of veterinary medicine, including licensure and accreditation, euthanasia, animal welfare, and mass depopulation. Government agencies, varied stakeholders, and veterinary practitioners look to these policies for guidance, especially in uncharted territory. A recent example highlights this influence when the United States Department of Agriculture and the swine industry needed to undergo mass depopulation during the COVID-19 pandemic, demonstrating how policy coordination across organizations could be leveraged for other pertinent global issues such as climate change (10). Federal laws, such as the Animal Welfare Act and the Humane Slaughter Act, regulate standards of care, along with practice regulations set by State Boards of Veterinary Medicine. Additionally, state Veterinary Medical Associations provide specific legislative updates and expertise for community-based issues. Ultimately, professional societies have unique roles and responsibilities, which include bridging gaps between practitioners and policy and providing support and guidance on taking active roles in the policy space for relevant issues, including climate change (11).
A brief scoping review (12) was conducted in March 2021 to better understand the policy landscape that supports veterinarians in this space. The authors conclude that policies that formally support veterinarians in the climate space and articles on the need for veterinarians to be climate change leaders are virtually nonexistent. The current AVMA Committee on Environmental Issues priorities (13) and joint statements with the Canadian Veterinary Medical Association and the Federation of Veterinarians of Europe on the role of veterinarians in protecting public and environmental health fail to mention climate change (14). The only AVMA policy mentioning climate change, called “Global climate change and One Health,” has no action guidance or capacity building for veterinarians to be leaders in this space. Rather, the policy only encourages research, education, and stakeholder collaboration (15). Recently, the World Veterinary Association published a position statement declaring global climate change as an emergency, encouraging increased collaborations amongst stakeholders, and emphasizing the importance of building veterinary capacity to prevent and address climate change concerns (16). This is the only major veterinary position statement on this issue.
The human medical profession, including specialist doctors and nurses, have established calls to action and incorporated climate change as an important issue into their professional society policies (Table 1). These groups have created coalitions and subsequent policy action agendas, excluding any representation from animal health sectors. Guides to support practitioners in climate change and its impact on human and planetary health have been published in the human medical field (Table 1). For example, The American College of Physicians has developed a Climate Change Action Plan and Toolkit, included in Table 1, which not only provides a freely accessible presentation to explain the impacts of climate change on health, but provides talking points for regional U.S. climate change issues. This resource includes fact sheets to facilitate discussions about climate change directly with patients, and guides on how to create more sustainable hospital environments. Medical professionals have acknowledged the importance of incorporating climate education into training programs (17), showcasing active movement to create change in this space and a clear recognition of the professional need. Additionally, the human medical profession views climate change and sustainability as a public health issue (18–24). This is true across physicians (25–30), nurses (31–38), and dentists (39, 40). The need for these professionals to use their voices for change, be powerful advocates, and be agents of action in this space has been emphasized (41–44). The veterinary profession can adapt human health coalition policy agendas and practitioner guides within their own organizations.
As public health professionals, veterinarians should be viewed as keystone contributors to climate change solutions. The impact of heat stress on livestock health provides an illustrative example of how veterinarians can play critical roles in climate change action. Rising temperatures lead to reduced livestock productivity and immune suppression, making livestock more vulnerable to disease and impacting food security (45). Veterinarians who provide care to livestock have the ability to inform early interventions that protect animals from heat stress and services to aid in the recovery from heat events (adaptation), bolster the overall health of populations to be better equipped to handle subsequent climate change threats (resilience), and guide dietary and other management actions that reduce cattle emissions, which contribute to warming (mitigation) (45). Similar veterinary insight can be brought to other climate change issues outlined in Figure 1. Based on this, it is unclear why veterinarians are out of the conversation surrounding climate change action. Veterinarians may not think they belong in the space, may view it as a “political” issue, or may be hesitant without supportive professional society leadership. Additionally, other professions may have excluded veterinarians in discussions of climate change, maintaining silos that would benefit from interdisciplinary expertise. As an example, veterinarians are more trusted than physicians and viewed positively by the public (46), which can be beneficial in being part of these important topics. There are guides for other health professions on having conversations about politicized topics which have major impacts on patient health (47). Human health professionals have already emphasized the need to teach patients about the relevance of climate change to direct patient care (48). By utilizing guides already created, an opportunity exists for veterinarians to be educators on how climate change impacts the health of their patients, clients, and the environment. The veterinary profession should rise to meet other healthcare professions and lead in providing policy to support climate action.
At the heart of sustained interactions between policy-makers and practitioners is communication and relationships (49). Veterinarians are trained in these skills, as this type of engagement is central to successful veterinary-client-patient relationships. Veterinarians can serve as “knowledge brokers” using cross-disciplinary communication skills, coupled with their unique perspective on climate change vulnerabilities, to establish strong relationships and trust with policy-makers early (50). In this way, veterinarians can continue to be long-term stewards for issues related to climate change and planetary health. To be successful, these types of networks and information exchange between policy-makers and veterinarians must be formally supported and facilitated (50). Within the U.S., the AVMA has the opportunity to enhance policy capacity and support reframing the scope of practice to include issues related to climate change and planetary health. Policy support available to tackle climate change issues should be equivalent between human and animal health sectors. As a model for the U.S., the Health Environment Network in Europe creates and fosters collaborative, interdisciplinary health networks to solve environmental health problems and provide policy guidance (51).
Veterinary policies are already in place that address issues that are impacted by climate (Figure 1, Supplementary Table 1). However, these policies are often not framed within climate change but rather as independent factors. There is ample literature linking medical and public health issues to climate change, including increasing global temperature (52–57), extreme weather events (58–63), air quality (64–71), vector-borne disease (72–79), food safety/security (80–87), water-related health issues (88–94), and mental health (95–102). Health concerns have also been directly attributed to climate change (103). Yet, the disconnect within policy still exists, and a critical gap needs to be addressed to provide veterinarians with the roles, responsibilities, and support to be effective climate change advocates alongside their human medical counterparts.
There is a clear path forward for veterinarians to take an active role in promoting planetary health in the fight to mitigate climate change impacts. Veterinarians have the opportunity to serve as “boundary-spanners” and “honest brokers”(104) using their roles as practitioners to share their knowledge about public health issues with policy-makers, educate the public on the impacts of climate change on planetary health, and bolster capacity for climate change resilience, adaptation, and mitigation. The role of veterinarians in climate change must be recognized as critical by professional societies, such as the AVMA. Programs that allow veterinarians to gain experience at the science-policy interface, such as the AVMA Fellowship Program, must be strengthened. Specific training opportunities, such as fellowships in climate change and health policy and creating climate-specific advocacy toolkits and practitioner guides, would empower veterinarians to act (105–108). Professional society leadership are well poised to develop and teach these skills to practitioners (105, 106). More effort is needed from veterinary professional societies to publish calls to action and take an overt stand that puts veterinarians in the forefront of climate change efforts. While some advocacy programming exists at both state and federal levels, they are limited in their breadth and depth. Creating continuing education modules for advocacy and policy is one way to enhance this knowledge among veterinarians. The AVMA could take a more active role in surveying practitioners about how policy directly impacts their practice, to better emphasize the role policy plays in shaping their ability to promote public health (109). Veterinarians can look to other scientific societies that are leaders in the human health and scientific space, including the Union of Concerned Scientists and the American Association for the Advancement of Science, which have ample tools, resources, and training available for scientists to effectively navigate the policy space.
The desire to cross-train health professionals in policy, including knowledge of the legislative process, policy-writing, and understanding how policy shapes global topics of concern, is not new, and has been undertaken by some university programs (110). However, these types of opportunities are limited within the U.S., particularly for current veterinarians, and are not incorporated as core curricular programs. While not all veterinarians need to have explicit roles in the policy space, all should understand how their work fits into the broader, global context to promote planetary health and take action to inform policy-decision making in their area. Courses to engage current veterinary students in public policy topics that are already established (110) should be expanded as core curricula or be incorporated and integrated into already existing coursework. Integrating climate and health education is critical for fostering future generations of informed healthcare leaders (111). Veterinarians should be trained in global perspectives to allow them to be stewards for global problems, such as preserving planetary health and mitigating climate change (112). Empowering veterinarians and veterinary students to envision how policy fits into their careers and utilize their expertise to impact policy decisions from the local to international level, regardless of their chosen specialty, is critical. Public health education already views knowledge about policy as a core educational domain and competency (113). The AVMA Council on Education and the American Association of Veterinary Medical Colleges should enhance public health related professional competencies to encompass this aspect of knowledge and make a commitment to including public policy and the practitioner-policy interface as key skillsets.
Policy to support veterinarians as climate change leaders will not only benefit veterinarians but will contribute to the overall effort to improve planetary health. The next generation of veterinarians, veterinary technicians, and clients all care about the changing climate. To stay socially relevant as veterinarians, it is critical for the veterinary profession to address climate change as a need (7). Veterinary students across the U.S. agree that climate change is a problem, believe veterinarians have a responsibility to be leaders in this space, that veterinary professional societies should take an active role, and that educational opportunities should be expanded (114). Veterinary medicine should re-consider its curricular foci and priorities to incorporate policy and advocacy at the forefront of translatable skillsets. The importance of incorporating project-based, experiential learning opportunities that model real-world, complex problems has been demonstrated for the related area of sustainability education (115). This type of applied learning helps prepare students to be change leaders and ensures that they have the capacity to translate curricular knowledge into practice and policy settings. Federal agencies, senior leaders in higher education administration, program directors, department faculty, and private sector organizations all have roles to play in fostering the development of core competencies, researching curricular effectiveness, encouraging interdisciplinary program building, using problem-based learning approaches, enhancing mentorship and advising capacity, and promoting cross-sector collaborations to build a comprehensive educational program in climate change and policy (115).
The call to action from health professions is clear. A pledge has been proposed to incorporate the protection of planetary health, including mitigating climate change, into the ethos and framework of healthcare professions and to incorporate planetary health into educational offerings (17, 116). This call to action should include the veterinary profession. Veterinarians must be empowered to protect planetary health and have a sense of ownership and stewardship about protecting the planet against the impacts of climate change. In order to do this, veterinarians need to be supported in a professional capacity to do work in this space, and policy is a critical piece of this puzzle. Climate change policy is relevant to all veterinary practitioners, whether they work in clinical practice settings or elsewhere, because climate change is a public health issue (Figure 1). Advocacy skills are key, and veterinarians can be involved with the policy-making process and build these skills at all levels, from the local level via county public health boards to the state and national levels through professional societies and relationships with policy-makers. Veterinarians can serve as critical community leaders to advocate for concerns relating to climate change and health of their patients and clients (117).
Ultimately, when veterinarians take their veterinary medical oath, they vow to promote and protect public health, and medical professionals agree that climate change is currently the greatest public health threat (118). If veterinarians want to maintain their commitment to promoting public health, they must be able to address climate change (119), be actively included in conversations as key stakeholders for policy decision-making, and be formally supported and trained in public policy and advocacy.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
DK and CD initiated the study. DK conducted the scoping review, organized resources, wrote the first draft of the manuscript, and designed the initial figure. WS, CD, and DK reviewed results and contributed to interpretation. All authors contributed to manuscript revision, read, and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflictof interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2022.775411/full#supplementary-material
1. Trevejo RT. Public health for the twenty-first century: what role do veterinarians in clinical practice play? Vet Clin North Am Small Anim. (2009) 39:215–24. doi: 10.1016/j.cvsm.2008.10.008
2. Veterinarian's Oath. American Veterinary Medical Association. Available online at: https://www.avma.org/resources-tools/avma-policies/veterinarians-oath
3. WSAVA Global Oath. WSAVA. Available online at: https://wsava.org/global-guidelines/wsava-global-oath/
4. Evans B, MacInnes T. Shaping veterinary health policies in a global and evolving context. Rev Sci Tech. (2012) 31:431–7. doi: 10.20506/rst.31.2.2129
5. Kelly A, Osburn B, Salman M. Veterinary medicine's increasing role in global health. Lancet Global Health. (2014) 2:e379–80. doi: 10.1016/S2214-109X(14)70255-4
6. Zinsstag J, Crump L, Schelling E, Hattendorf J, Maidane YO, Ali KO, et al. Climate change and One Health. FEMS Microbiology Letters. (2018) 365:fny085. doi: 10.1093/femsle/fny085
7. Stephen C, Carron M, Stemshorn B. Climate change and veterinary medicine: action is needed to retain social relevance. Can Vet J. (2019) 60:1356−8.
8. The intersection of science public policy. American Association for the Advancement of Science. Available online at: https://www.aaas.org/intersection-science-and-public-policy
9. Vision mission values. American Veterinary Medical Association. Available online at: https://www.avma.org/about/vision-mission-and-values
10. COVID-19 impacts on food production medicine. American Veterinary Medical Association. Available online at: https://www.avma.org/resources-tools/animal-health-and-welfare/covid-19/covid-19-impacts-food-production-medicine
11. Scott JM, Rachlow JL, Lackey RT. The Science-policy interface: what is an appropriate role for professional societies. BioScience. (2008) 58:865–9. doi: 10.1641/B580914
12. Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. JBI Evidence Implementation. (2015) 13:141–6. doi: 10.1097/XEB.0000000000000050
13. CEI roadmap for environmental leadership priorities. American Veterinary Medical Association. Available online at: https://www.avma.org/resources-tools/avma-policies/cei-roadmap-environmental-leadership-priorities
14. Joint Joint AVMA-FVE-CVMA statement on the essential role of veterinarians in protecting animal human public environmental health—A global public good. American Veterinary Medical Association. Available online at: https://www.avma.org/resources-tools/avma-policies/joint-avma-fve-cvma-statement-essential-role-veterinarians-protecting-animal-human-public
15. Global Climate Change One Health. American Veterinary Medical Association. Available online at: https://www.avma.org/resources-tools/avma-policies/global-climate-change-and-one-health
16. WVA News. Available online at: https://www.worldvet.org/news.php?item=460
17. Shaw E, Walpole S, McLean M, Alvarez-Nieto C, Barna S, Bazin K, et al. AMEE Consensus statement: planetary health and education for sustainable healthcare. Med Teach. (2021) 0:1–15. doi: 10.1080/0142159X.2020.1860207
18. Haines A, Scheelbeek P, Abbasi K. The health case for urgent action on climate change. BMJ. (2020) 368. doi: 10.1136/bmj.m1103
19. Farrell A. Mitigating the effects of the climate crisis through health policy. HSI. (2020) 11:103–7. doi: 10.29173/hsi287
20. Buse CG, Patrick R. Climate change glossary for public health practice: from vulnerability to climate justice. J Epidemiol Community Health. (2020) 74:867–71. doi: 10.1136/jech-2020-213889
21. Graham R, Compton J, Meador K. A systematic review of peer-reviewed literature authored by medical professionals regarding US biomedicine's role in responding to climate change. Prev Med Rep. (2019) 13:132–8. doi: 10.1016/j.pmedr.2018.11.014
22. Peters JL. Mitigating the impact of climate change on human health: the role of the medical community. AMA J Ethics. (2017) 19:1153–6. doi: 10.1001/journalofethics.2017.19.12.fred1-1712
23. Norling A. AMA code of medical ethics' opinions related to climate change. AMA J Ethics. (2017) 19:1183–5. doi: 10.1001/journalofethics.2017.19.12.coet1-1712
24. Yidan Lu MDCM F. Climate change and health – concrete steps for physicians and health professionals. Can Journ Gen Int Med. (2016) 11. doi: 10.22374/cjgim.v11i4.187
25. Storz MA. Mitigating climate change: using the physician's tool of the trade. Br J Gen Pract. (2019) 69:557. doi: 10.3399/bjgp19X706313
26. Wellbery C. Climate change health impacts: a role for the family physician. AFP. (2019) 100:602–3.
27. Crowley RA. Climate change and health: a position paper of the american college of physicians. Ann Intern Med. (2016) 164:608–10. doi: 10.7326/M15-2766
28. McCoy D, Hoskins B. The science of anthropogenic climate change: what every doctor should know. BMJ. (2014) 349. doi: 10.1136/bmj.g5178
29. Gill M, Godlee F, Horton R, Stott R. Doctors and climate change. BMJ. (2007) 335:1104–5. doi: 10.1136/bmj.39412.488021.80
30. Woodward A. Climate change and the surgeon: what is the problem? Why is it so hard? What can be done? ANZ Journal of Surgery. (2019) 89:1358–63. doi: 10.1111/ans.15562
31. Nicholas PK, Breakey S, Tagliareni E, Tuck I, Neal-Boylan L, Ladd E, et al. Advancing a school of nursing center for climate change, climate justice, and health. Annu Rev Nurs Res. (2020) 38:145–58. doi: 10.1891/0739-6686.38.145
32. Levin KL, Chandler T. Climate Change the Nurse's Role in Policy Practice. Springer Publishing Company. (2020). Available online at: https://connect.springerpub.com/content/book/978-0-8261-0865-4/part/part04/chapter/ch18
33. Kalogirou MR, Olson J, Davidson S. Nursing's metaparadigm, climate change and planetary health. Nurs Inq. (2020) 27:e12356. doi: 10.1111/nin.12356
34. Lilienfeld E, Nicholas PK, Breakey S, Corless IB. Addressing climate change through a nursing lens within the framework of the United Nations Sustainable Development Goals. Nursing Outlook. (2018) 66:482–94. doi: 10.1016/j.outlook.2018.06.010
35. Leffers J, Butterfield P. Nurses play essential roles in reducing health problems due to climate change. Nurs Outlook. (2018) 66:210–3. doi: 10.1016/j.outlook.2018.02.008
36. Leffers J, Levy RM, Nicholas PK, Sweeney CF. Mandate for the nursing profession to address climate change through nursing education. J Nurs Scholarship. (2017) 49:679–87. doi: 10.1111/jnu.12331
37. Cook C. Climate change and health: nurses as drivers of climate action. IJPS. (2018) 5:8–8. doi: 10.24926/ijps.v5i1.914
39. Duane B, Harford S, Ramasubbu D, Stancliffe R, Pasdeki-Clewer E, Lomax R, et al. Environmentally sustainable dentistry: a brief introduction to sustainable concepts within the dental practice. Br Dent J. (2019) 226:292–5. doi: 10.1038/s41415-019-0010-7
40. Duane B, Stancliffe R, Miller FA, Sherman J, Pasdeki-Clewer E. Sustainability in dentistry: a multifaceted approach needed. J Dent Res. (2020) 99:998–1003. doi: 10.1177/0022034520919391
41. Bennett H, Macmillan A, Jones R, Blaiklock A, McMillan J. Should health professionals participate in civil disobedience in response to the climate change health emergency? Lancet. (2020) 395:304–8. doi: 10.1016/S0140-6736(19)32985-X
42. Macpherson CC, Wynia M. Should health professionals speak up to reduce the health risks of climate change? AMA J Ethics. (2017) 19:1202–10. doi: 10.1001/journalofethics.2017.19.12.msoc1-1712
43. Patrick K. Physicians and climate change policy: We are powerful agents of change. CMAJ. (2015) 187:307–307. doi: 10.1503/cmaj.150139
44. Kemple T. The climate emergency: are the doctors who take non-violent direct action to raise public awareness radical activists, rightminded professionals, or reluctant whistleblowers? The New Bioethics. (2020) 26:111–24. doi: 10.1080/20502877.2020.1775390
45. Stephen C, Soos C. The implications of climate change for veterinary services. Rev Sci Tech. (2021) 40:421–30. doi: 10.20506/rst.40.2.3234
46. Kedrowicz AA, Royal KD, A. Comparison of public perceptions of physicians and veterinarians in the United States. Veterinary Sci. (2020) 7:50. doi: 10.3390/vetsci7020050
47. Alame D, Truog RD. How should clinicians weigh the benefits and harms of discussing politicized topics that influence their individual patients' health? AMA J Ethics. (2017) 19:1174–82. doi: 10.1001/journalofethics.2017.19.12.ecas3-1712
48. Verner G, Schütte S, Knop J, Sankoh O, Sauerborn R. Health in climate change research from 1990 to 2014: positive trend, but still underperforming. Global Health Action. (2016) 9:30723. doi: 10.3402/gha.v9.30723
49. More SJ. Perspectives from the science-policy interface in animal health and welfare. Front Vet Sci. (2019) 6:382. doi: 10.3389/fvets.2019.00382
50. Boden L, Auty H, Goddard P, Stott A, Ball N, Mellor D. Working at the science-policy interface. Veterinary Record. (2014) 174:165–7. doi: 10.1136/vr.g1430
51. Bartonova A. How can scientists bring research to use: the HENVINET experience. Environ Health. (2012) 11:S2. doi: 10.1186/1476-069X-11-S1-S2
52. Lou J, Wu Y, Liu P, Kota SH, Huang L. Health effects of climate change through temperature and air pollution. Curr Pollution Rep. (2019) 5:144–58. doi: 10.1007/s40726-019-00112-9
53. Sorensen C, Garcia-Trabanino R. A new era of climate medicine — addressing heat-triggered renal disease. N Engl J Med. (2019) 381:693–6. doi: 10.1056/NEJMp1907859
54. Kingsolver JG, Diamond SE, Buckley LB. Heat stress and the fitness consequences of climate change for terrestrial ectotherms. Funct Ecol. (2013) 27:1415–23. doi: 10.1111/1365-2435.12145
55. Hanna EG, Kjellstrom T, Bennett C, Dear K. Climate change and rising heat: population health implications for working people in Australia. Asia Pac J Public Health. (2011) 23:14S−26S. doi: 10.1177/1010539510391457
56. Teixeira EI, Fischer G, van Velthuizen H, Walter C, Ewert F. Global hot-spots of heat stress on agricultural crops due to climate change. Agric For Meteorol. (2013) 170:206–15. doi: 10.1016/j.agrformet.2011.09.002
57. Kjellstrom T, Holmer I, Lemke B. Workplace heat stress, health and productivity – an increasing challenge for low and middle-income countries during climate change. Glob Health Action. (2009) 2:2047. doi: 10.3402/gha.v2i0.2047
58. Curtis S, Fair A, Wistow J, Val DV, Oven K. Impact of extreme weather events and climate change for health and social care systems. Environ Health. (2017)16:128. doi: 10.1186/s12940-017-0324-3
59. Ebi KL. Resilience to the health risks of extreme weather events in a changing climate in the United States. Int J Environ Res Public Health. (2011) 8:4582–95. doi: 10.3390/ijerph8124582
60. Greenough G, McGeehin M, Bernard S M, Trtanj J, Riad J, Engelberg D. The potential impacts of climate variability and change on health impacts of extreme weather events in the United States. Environmental Health Perspectives. (2001) 109:191–8. doi: 10.1289/ehp.109-1240666
61. Medicine I of, Health B on G, Threats F on M. Global Climate Change and Extreme Weather Events: Understanding the Contributions to Infectious Disease Emergence: Workshop Summary. Washington, DC: National Academies Press (2008). p. 302.
62. Mills DM. Climate change, extreme weather events, and us health impacts: what can we say? J Occup Environ. (2009) 51:26–32. doi: 10.1097/JOM.0b013e31817d32da
63. De Sario M, Katsouyanni K, Michelozzi P. Climate change, extreme weather events, air pollution and respiratory health in Europe. Eur Respir J. (2013) 42:826–43. doi: 10.1183/09031936.00074712
64. ApSIMON H, AMANN M, ÅSTRÖM S, OXLEY T. Synergies in addressing air quality and climate change. Climate Policy. (2009) 9:669–80. doi: 10.3763/cpol.2009.0678
65. Bernard S M, Samet J M, Grambsch A, Ebi K L, Romieu I. The potential impacts of climate variability and change on air pollution-related health effects in the United States. Environmental Health Perspectives. (2001) 109:199–209. doi: 10.1289/ehp.109-1240667
66. Fiore AM, Naik V, Leibensperger EM. Air quality and climate connections. J Air Waste Manag Assoc. (2015) 65:645–85. doi: 10.1080/10962247.2015.1040526
67. Nazaroff WW. Exploring the consequences of climate change for indoor air quality. Environ Res Lett. (2013) 8:015022. doi: 10.1088/1748-9326/8/1/015022
69. Campbell-Lendrum D, Prüss-Ustün A. Climate change, air pollution and noncommunicable diseases. Bull World Health Organ. (2019) 97:160–1. doi: 10.2471/BLT.18.224295
70. Kinney PL. Interactions of climate change, air pollution, and human health. Curr Envir Health Rpt. (2018) 5:179–86. doi: 10.1007/s40572-018-0188-x
71. D'Amato G, Vitale C, Lanza M, Molino A, D'Amato M. Climate change, air pollution, and allergic respiratory diseases: an update. Curr Opin Allergy Clin Immunol. (2016) 16:434–40. doi: 10.1097/ACI.0000000000000301
72. Bartlow AW, Manore C, Xu C, Kaufeld KA, Del Valle S, Ziemann A, et al. Forecasting zoonotic infectious disease response to climate change: mosquito vectors and a changing environment. Veterinary Sci. (2019) 6:40. doi: 10.3390/vetsci6020040
73. Campbell-Lendrum D, Manga L, Bagayoko M, Sommerfeld J. Climate change and vector-borne diseases: what are the implications for public health research and policy? Philos Trans R Soc Lond, B Biol Sci. (2015) 370:20130552. doi: 10.1098/rstb.2013.0552
74. Brisbois BW, Ali SH. Climate Change, Vector-borne Disease and Interdisciplinary Research: Social Science Perspectives on an Environment and Health Controversy. EcoHealth. (2010) 7:425–38. doi: 10.1007/s10393-010-0354-6
75. Mills James N., Gage Kenneth L., Khan Ali S. Potential influence of climate change on vector-borne and zoonotic diseases: a review and proposed research plan. Environ Health Perspect. (2010) 118:1507–14. doi: 10.1289/ehp.0901389
76. Parham PE, Waldock J, Christophides GK, Michael E. Climate change and vector-borne diseases of humans. Philos Trans R Soc Lond, B Biol Sci. (2015) 370:20140377. doi: 10.1098/rstb.2014.0377
77. Ogden NH. Climate change and vector-borne diseases of public health significance. FEMS Microbiol Lett. (2017) 364. doi: 10.1093/femsle/fnx186
78. Rocklöv J, Dubrow R. Climate change: an enduring challenge for vector-borne disease prevention and control. Nat Immunol. (2020) 21:479–83. doi: 10.1038/s41590-020-0648-y
79. Hall RJ, Brown LM, Altizer S. Modeling vector-borne disease risk in migratory animals under climate change. Integr Comp Biol. (2016) 56:353–64. doi: 10.1093/icb/icw049
80. Al-Amin AQ, Ahmed F. Food security challenge of climate change: an analysis for policy selection. Futures. (2016) 83:50–63. doi: 10.1016/j.futures.2016.04.002
81. Beddington JR, Asaduzzaman M, Clark ME, Bremauntz AF, Guillou MD, Jahn MM, et al. The role for scientists in tackling food insecurity and climate change. Agric & Food Secur. (2012) 1:10. doi: 10.1186/2048-7010-1-10
82. Campbell BM, Vermeulen SJ, Aggarwal PK, Corner-Dolloff C, Girvetz E, Loboguerrero AM, et al. Reducing risks to food security from climate change. Global Food Security. (2016) 11:34–43. doi: 10.1016/j.gfs.2016.06.002
83. Dhankher OP, Foyer CH. Climate resilient crops for improving global food security and safety. Plant Cell Environ. (2018) 41:877–84. doi: 10.1111/pce.13207
84. Herrera M, Anadón R, Iqbal SZ, Bailly JD, Ariño A. Climate change and food safety. In: Selamat J, Iqbal SZ, editors. Food Safety: Basic Concepts, Recent Issues, and Future Challenges. Cham: Springer International Publishing. (2016). p. 149–60. doi: 10.1007/978-3-319-39253-0_8
85. Maggiore A, Afonso A, Barrucci F, Sanctis GD. Climate change as a driver of emerging risks for food and feed safety, plant, animal health and nutritional quality. EFSA Supporting Publications. (2020) 17:1881E. doi: 10.2903/sp.efsa.2020.EN-1881
86. Chen J, McCarl BA, Thayer A. Climate Change and Food Security: Threats and Adaptation. In: World Agricultural Resources and Food Security. Emerald Publishing Limited. (2017). p. 69–84. doi: 10.1108/S1574-871520170000017006
87. Schmidhuber J, Tubiello FN. Global food security under climate change. PNAS. (2007) 104:19703–8. doi: 10.1073/pnas.0701976104
88. Allan C, Xia J, Pahl-Wostl C. Climate change and water security: challenges for adaptive water management. Curr Opin Environ. (2013) 5:625–32. doi: 10.1016/j.cosust.2013.09.004
89. Cann KF, Thomas DR, Salmon RL, Wyn-Jones AP, Kay D. Extreme water-related weather events and waterborne disease. Epidemiol Infect. (2013) 141:671–86. doi: 10.1017/S0950268812001653
90. Arnell NW, van Vuuren DP, Isaac M. The implications of climate policy for the impacts of climate change on global water resources. Global Environmental Change. (2011) 21:592–603. doi: 10.1016/j.gloenvcha.2011.01.015
91. Charron DF, Thomas MK, Waltner-Toews D, Aramini JJ, Edge T, Kent RA, et al. Vulnerability of waterborne diseases to climate change in Canada: a review. J Toxicol Environ Health Part A. (2004) 67:1667–77. doi: 10.1080/15287390490492313
92. Döll P, Jiménez-Cisneros B, Oki T, Arnell NW, Benito G, Cogley JG, et al. Integrating risks of climate change into water management. Hydrological Sci J. (2015) 60:4–13. doi: 10.1080/02626667.2014.967250
93. Michalak AM. Study role of climate change in extreme threats to water quality. Nature News. (2016) 535:349. doi: 10.1038/535349a
94. Hales S. Climate change, extreme rainfall events, drinking water and enteric disease. Rev Environ Health. (2019) 34:1–3. doi: 10.1515/reveh-2019-2001
95. Berry HL, Waite TD, Dear KBG, Capon AG, Murray V. The case for systems thinking about climate change and mental health. Nat Clim Chang. (2018) 8:282–90. doi: 10.1038/s41558-018-0102-4
96. Berry HL, Bowen K, Kjellstrom T. Climate change and mental health: a causal pathways framework. Int J Public Health. (2010) 55:123–32. doi: 10.1007/s00038-009-0112-0
97. Berry H, Kelly B, Hanigan I, Coates J, McMichael A, Welsh J, et al. Rural mental health impacts of climate change. (2008).
98. Clayton S. The insidious impacts of climate change: mood, mental health, and psychosocial wellbeing. One Earth. (2020) 2:530–1. doi: 10.1016/j.oneear.2020.05.019
99. Bourque F, Willox AC. Climate change: The next challenge for public mental health? Int Rev Psychiat. (2014) 26:415–22. doi: 10.3109/09540261.2014.925851
100. Cunsolo A, Ellis NR. Ecological grief as a mental health response to climate change-related loss. Nature Clim Change. (2018) 8:275–81. doi: 10.1038/s41558-018-0092-2
101. Hayes K, Blashki G, Wiseman J, Burke S, Reifels L. Climate change and mental health: risks, impacts and priority actions. Int J Ment Health Syst. (2018) 12:28. doi: 10.1186/s13033-018-0210-6
102. Hrabok M, Delorme A, Agyapong VIO. Threats to mental health and well-being associated with climate change. J Anxiety Dis. (2020) 76:102295. doi: 10.1016/j.janxdis.2020.102295
103. Ebi Kristie L, Ogden Nicholas H, Semenza Jan C, Alistair W. Detecting and attributing health burdens to climate change. Environm Health Perspect. (2017) 125:085004. doi: 10.1289/EHP1509
104. Bednarek AT, Wyborn C, Cvitanovic C, Meyer R, Colvin RM, Addison PFE, et al. Boundary spanning at the science-policy interface: the practitioners' perspectives. Sustain Sci. (2018) 13:1175–83. doi: 10.1007/s11625-018-0550-9
106. Nielsen NO, Buntain B, Stemshorn B, Evans B. Public policy and veterinary medicine. Can Vet J. (2014) 55:389–90.
107. Long T, Chaiyachati KH, Khan A, Siddharthan T, Meyer E, Brienza R. Expanding health policy and advocacy education for graduate trainees. J Grad Med Educ. (2014) 6:547–50. doi: 10.4300/JGME-D-13-00363.1
108. Lemery J, Sorensen C, Balbus J, Newman L, Davis C, Reno E, et al. Science policy training for a new physician leader: description and framework of a novel climate and health science policy fellowship. AEM Educ Train. (2019) 3:233–42. doi: 10.1002/aet2.10323
109. Erwin PC. Sentinel public health practitioner surveillance group. Tracking the impact of policy changes on public health practice. Am J Public Health. (2017) 107:653–4. doi: 10.2105/AJPH.2017.303733
110. Herrmann JA, Johnson YJ, Troutt HF, Prudhomme T. a public-policy practicum to address current issues in human, animal, and ecosystem health. J Vet Med Educ. (2009) 36:397–402. doi: 10.3138/jvme.36.4.397
111. Shaman J, Knowlton K. The Need for Climate and health education. Am J Public Health. (2017) 108:S66–7. doi: 10.2105/AJPH.2017.304045
112. Blum N. Veterinary Students as Global Citizens: Exploring opportunities for embedding the global dimension in the undergraduate veterinary curriculum. Royal Veterinary College, University of London and Development Education Research Centre, Institute of Education: London, UK. London, UK: Royal Veterinary College, University of London and Development Education Research Centre, Institute of Education. (2012). Available online at: https://discovery.ucl.ac.uk/id/eprint/1475350/
113. Moreland-Russell S, Zwald M, Golden SD. Policy help needed, experience required: preparing practitioners to effectively engage in policy. Health Promotion Practice. (2016) 17:648–55. doi: 10.1177/1524839916650433
114. Pollard AE, Rowlison DL, Kohnen A, McGuffin K, Geldert C, Kramer C, et al. Preparing veterinarians to address the health impacts of climate change: student perceptions, knowledge gaps, and opportunities. J Vet Med Educ. (2020) 6:e20190080.
115. National Academies of Sciences E. Strengthening sustainability programs and curricula at the undergraduate and graduate levels. (2020). Available online at: https://www.nap.edu/catalog/25821/strengthening-sustainability-programs-and-curricula-at-the-undergraduate-and-graduate-levels
116. Wabnitz K-J, Gabrysch S, Guinto R, Haines A, Herrmann M, Howard C, et al. A pledge for planetary health to unite health professionals in the Anthropocene. The Lancet. (2020) 396:1471–3.
117. Kipp A, Cunsolo A, Gillis D, Sawatzky A, Harper SL. The need for community-led, integrated and innovative monitoring programmes when responding to the health impacts of climate change. Int J Circumpolar Health. (2019) 78:1517581. doi: 10.1080/22423982.2018.1517581
118. Atwoli L, Baqui AH, Benfield T, Bosurgi R, Godlee F, Hancocks S, et al. Call for emergency action to limit global temperature increases, restore biodiversity, and protect health. Lancet. (2021) 398:939–41. doi: 10.1016/S0140-6736(21)01915-2
Keywords: climate change, veterinary medicine, policy, public health, education
Citation: Kiran D, Sander WE and Duncan C (2022) Empowering Veterinarians to Be Planetary Health Stewards Through Policy and Practice. Front. Vet. Sci. 9:775411. doi: 10.3389/fvets.2022.775411
Received: 14 September 2021; Accepted: 09 February 2022;
Published: 03 March 2022.
Edited by:
Andrew Peters, Charles Sturt University, AustraliaReviewed by:
Elisabeth A. Stoddard, Worcester Polytechnic Institute, United StatesCopyright © 2022 Kiran, Sander and Duncan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Colleen Duncan, Y29sbGVlbi5kdW5jYW5AY29sb3N0YXRlLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.