- 1Medical School, University of Texas Southwestern Medical Center, Dallas, TX, United States
- 2Department of Urology, University of Texas Southwestern Medical Center, Dallas, TX, United States
Background: Type 2 diabetes mellitus is considered a risk factor for developing recurrent urinary tract infections. This review examined current knowledge on the incidence rates, bacterial strains, risk factors, treatments, and outcomes of recurrent urinary tract infections in type 2 diabetes, predominantly in women.
Methods: A systematic review was conducted for all English language articles from inception to June 2022 utilizing the Cochrane and Preferred Reporting Items for Systematic Reviews and Meta-Analyses standards in the databases PubMed, OVID Embase, and Cochrane Library. References were cross-examined for further articles. Data collected described the prevalence, characteristics, and management of recurrent urinary tract infections. Risk of bias assessments were performed for all studies.
Results: From 3342 identified articles, 597 met initial study criteria. Fifteen studies from 10 countries were included after full-text reviews. Four studies found higher recurrent urinary tract infection rates in diabetics versus non-diabetics meanwhile others reported recurrence rates from 23.4% to 37%. Four of five studies found diabetes to be a risk factor for recurrent urinary tract infection. E. coli was the most frequent causative pathogen. Antibiotic prescription results varied; however, multiple studies determined that longer treatment (≥ 5 days) did not correlate with lower recurrence rates. Risk of bias assessments found the most frequent study weakness to be identification of confounding variables.
Conclusion: This review covered multiple subtopics, with few comprehensive or generalizable results, suggesting a need for more research on how recurrent urinary tract infections can be better evaluated and managed in women with type 2 diabetes.
Introduction
Urinary tract infection (UTI) is the most common adult bacterial infection in the world, affecting over 60% of women at least once in their lifetime and becoming a recurrent urinary tract infection (rUTI) in more than a quarter of women (1–5). With the growing issue of antibiotic resistance, there is an urgent need to expand our understanding of UTIs, especially recurrent infections (6). Unfortunately, there are few published studies on rUTIs to guide clinical diagnosis and treatment (2, 5, 6).
Patients with type II diabetes mellitus (T2DM) are of special interest to researchers as many studies have shown that individuals with T2DM suffer from UTIs at a higher rate than those without T2DM (7–9). The incidence of diabetes in the US is rapidly increasing, therefore, UTIs are likely to become even more prevalent (10). A 2021 systematic review summarized the current literature on UTIs and diabetes (11). However, there is limited literature that focuses on rUTIs in women with T2DM.
Until recently, there were multiple limitations on rUTI research which contributed to the lack of rUTI studies in various populations. Criteria for rUTI diagnosis were not well defined and studies in humans were lacking (12). In a 2018 study, various diagnostic criteria for rUTIs were compared across studies, highlighting the need for one clearly defined, uniform diagnostic criteria (13). With the increase in both antibiotic resistant infections and T2DM across the world, understanding the relationship between recurrent urinary tract infections and diabetes is crucial (1, 14). Given this context and several gaps in knowledge, our goal was to analyze current literature to understand where rUTI research in T2DM populations stands. We aimed to identify all English language articles on the topic of recurrent urinary tract infections in adult, type II diabetic women and compare research outcomes across studies on rUTI diagnostic criteria, rUTI incidence rates, characterization of rUTIs, risk factors for rUTIs, workup and diagnostic methods, UTI treatment durations, antibiotic prescription rates, antibiotic resistances, and the correlation of SGLT2 inhibitor use with rUTIs. We hypothesized that rUTI incidence rates would be higher in T2DM women than non-T2DM women.
Methods
Study design
We aimed to collect all studies with relevant information on the workup, characteristics, and treatment of rUTIs in women with T2DM including data on rUTI incidence rates, common bacterial strains, symptoms of infection, risk factors for rUTI, rUTI treatments, and post-treatment outcomes.
Systematic review
A systematic review was performed in accordance with Cochrane and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) standards (15). We reviewed articles published from inception to June 2022 in PubMed/MEDLINE, OVID Embase, and Cochrane Library. The references of relevant articles were hand searched by the reviewers to identify any additional articles. The study criteria outlined below were used in this review:
Inclusion criteria
- Full text, English-language, prospective cohort, retrospective cohort, and randomized control trial studies of adult female patients.
- Studies focused on rUTI and T2DM; studies with an initial focus on UTI with relevant, clearly defined rUTI data, were included.
Exclusion criteria
- Abstract-only texts, individual case reports, review articles, non-human studies. Review articles were not excluded until full-text examination and reference screening to ensure comprehensive article identification.
- Studies with strictly male or pediatric populations; due to the limited dataset, studies including men or pediatric patients were not excluded if the study included a significant proportion of women. Such studies were reported separately.
- Asymptomatic bacteriuria, pyelonephritis, and unspecified genitourinary infections.
- Type I diabetic populations only; due to the limited dataset, groups with both Type I and Type II diabetes were included and independently analyzed.
The search was conducted using the keywords [recur*] AND [urinary tract infection*] AND [diabetes] including MeSH terms. Alternative spellings, names, and abbreviations, such as “rUTI”, “chronic”, cystitis”, “T2DM” and “adult-onset diabetes” were thoroughly searched in all combinations. Additional keywords for diabetes medications such as “metformin,” “Ozempic,” and “sodium-glucose co-transporter 2 inhibitor” were used as alternative terms to find all possible additional diabetic populations. Keywords appeared at least once in the title, abstract, keywords, or full text. Findings were compared between reviewers and differences were reconciled after careful examination and discussion.
Results
Through a multi-database and cross-reference search, 3342 records were identified. The titles of the articles were reviewed by two independent reviewers and were excluded if they did not meet study criteria or were duplicates. This step yielded 597 abstracts which were then further reviewed. 153 full-text studies were assessed for initial eligibility and were excluded based on format and topic exclusions. A total of 15 articles met all eligibility criteria.
Fifteen studies were included in the final review (Figure 1). This included 4 prospective studies, 10 retrospective studies, and 1 study that was both prospective and retrospective. The countries of origin were the United States (n = 3), Netherlands (n = 2), Taiwan (n = 2), India (n = 2), Germany (n = 1), Greece (n = 1), Spain (n = 1), Israel (n = 1), Japan (n = 1), and Italy (n = 1).
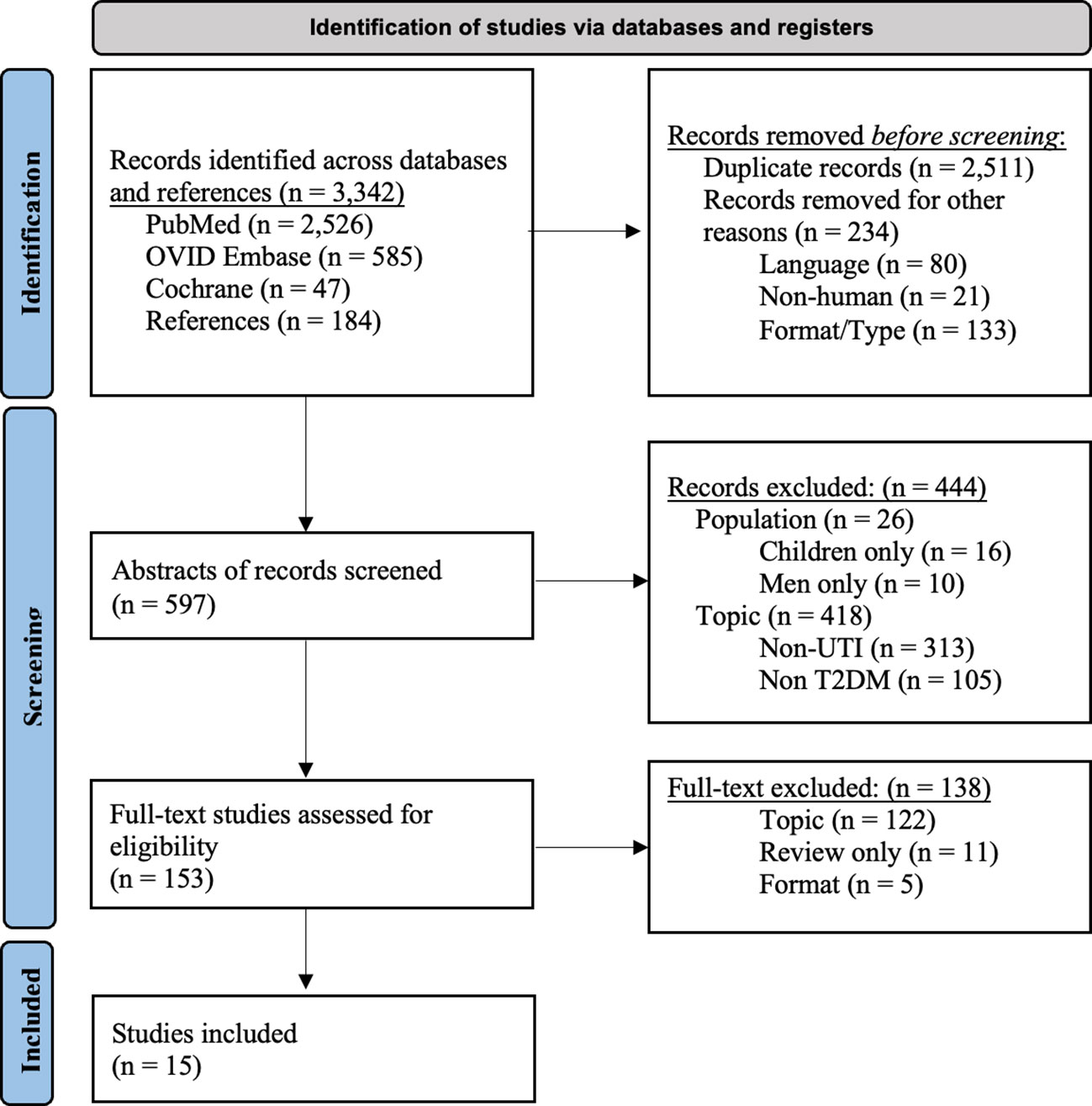
Figure 1 PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only. Adapted from: Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. UTI, urinary tract infection; rUTI, recurrent urinary tract infection; T2DM, type II diabetes mellitus.
RUTI diagnosis criteria and incidence rates
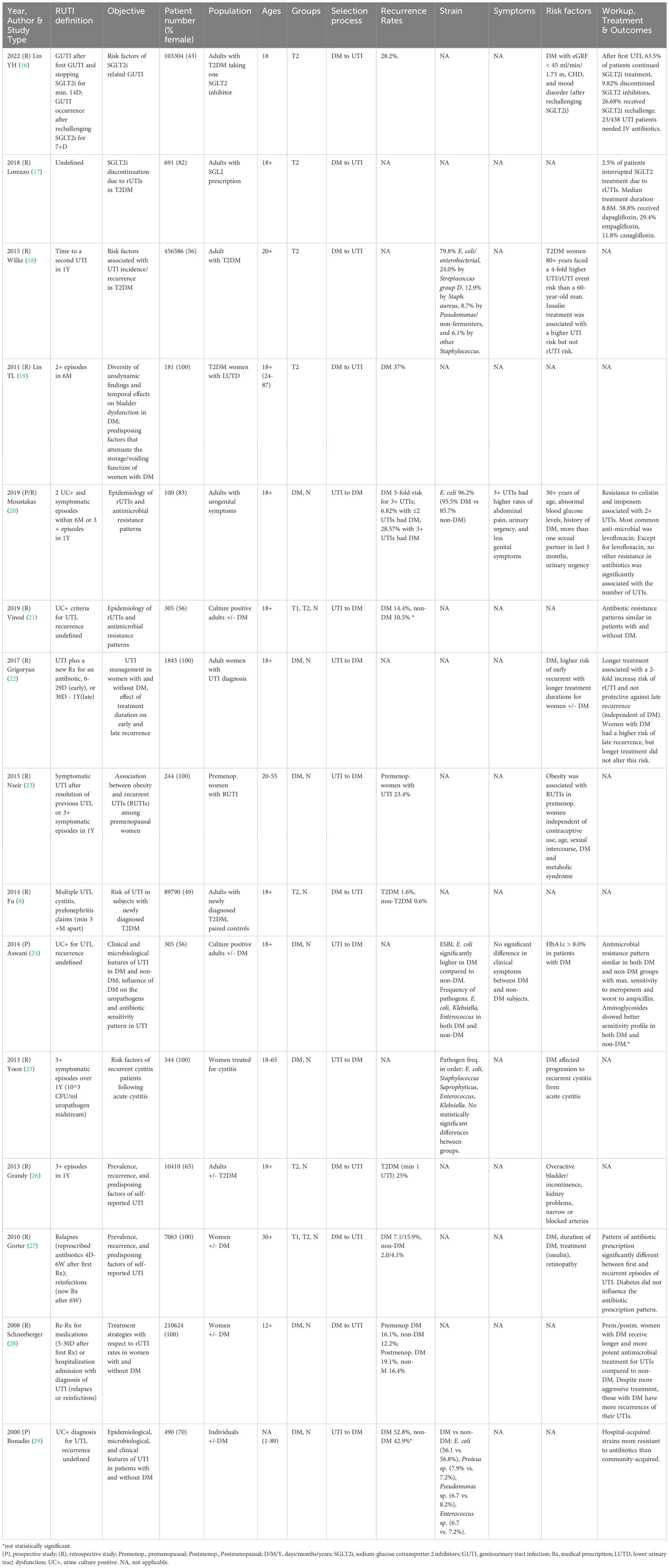
The definitions and diagnostic criteria of recurrent UTI are included for each study (Table 1). Ten studies defined rUTI with a combination of symptomatology, urine culture, and prescription patterns and five studies used only one criterion. Nine studies set time frames in which multiple UTI diagnoses had to be made to consider the infection “recurrent”, most commonly 1 year.
Twelve studies reported rUTI incidence rates. Grandy et al. reported both UTI and rUTI rates for their T2DM group, meanwhile Fu et al. studied general rUTI diagnosis rates in newly diagnosed T2DM patients. Other studies looked at recurrence rates in diabetic vs non-diabetic populations after a UTI diagnosis. Schneeberger et al. and Gorter et al. both found that women with DM had higher recurrence rates than their non-DM counterparts, however, neither of these studies distinguished between Type I and Type II diabetic patients. In contrast, two studies did not find significant differences in diabetic vs non-diabetic rUTI rates; once again, these studies did not differentiate Type 1 Diabetes Mellitus (T1DM) from T2DM.
Characterization of RUTI
Of the five studies that reported specific strains, all 5 found Escherichia coli (E. coli) to be the most frequent causative agent for UTI (56.1% - 96.2%) both in diabetics and non-diabetics. None of the studies reported a significant difference between the two groups. Two studies reported pathogen rates in their studies specific to rUTI, both of which found E. coli to be the most frequently rUTI pathogen. Aswani et al. reported a higher prevalence of extended-spectrum beta-lactamase (ESBL) E. coli in diabetics vs. non-diabetics; in contrast, Yoon et al. found no significant differences in pathogen distribution between groups.
Risk factors for RUTI
Diabetes has been shown to be a risk factor for UTI across many former studies (11). Of the 15 studies included in this review, five studies sought out to determine if diabetes was a risk factor for developing recurrent UTI, specifically. Yoon et al. found that having diabetes was significantly associated with the progression of acute to recurrent cystitis while Moustakas et al. found that DM was a risk factor for rUTI. Similarly, Grigoryan et al. found that the presence of DM was a determinant of late recurrence of UTI. For studies looking at risk factors for rUTI in diabetic populations, results varied greatly. Gorter et al. reported several risk factors for rUTI in women, including insulin treatment. Contrary to this finding, Wilke et al. reported that insulin treatment was not associated with rUTI risk.
Workup, diagnosis, and treatment durations
Eight studies discussed the diagnosis, treatment, or outcomes of rUTIs in diabetes. Grigoryan et al. reported that women with diabetes and acute cystitis were less likely to receive workup for new cystitis events but were more likely to receive longer durations of antibiotics. They also found that treating UTI episodes for longer did not correlate with lower rates of recurrence. Similarly, Schneeberger et al. reported that women with DM received longer and more potent antimicrobial treatment for UTIs but had higher recurrence rates than non-DM women.
Antibiotic prescription rates
Gorter et al. found that both women with and without DM received significantly different antibiotic prescriptions between their first episode of UTI and their recurrent episodes, but that diabetes did not influence antibiotic prescription patterns. Moustakas and Grigoryan et al. both reported that fluoroquinolones were the most prescribed antibiotic class; the latter also found that there was no clinically meaningful difference in prescription patterns between DM status groups. Similarly, Schneeberger et al. found no statistically significant difference in fluoroquinolone prescription between groups but reported that postmenopausal patients with DM were more likely to receive norfloxacin with longer treatment duration.
Antibiotic resistance
Antibiotic resistance patterns were discussed in three studies. Aswani et al. reported similar patterns in both DM and non-DM populations; similarly, Bonadio et al. reported slight differences that did not reach statistical significance. Neither of these studies specified the impact of antibiotic resistance on rUTIs. Moustakas et al. looked at how resistance to antimicrobials was associated with multiple UTIs. They found that resistance to colistin and imipenem was associated with a history of >2 UTI episodes but observed only in a few patients.
SGLT2 inhibitors
Two studies focused on the effects of sodium-glucose co-transporter 2 inhibitors (SGLT2i) on UTIs and their recurrences. The study by Lin YH et al. investigated the risk factors related to genitourinary tract infections with SGLT2i use. The authors found a 28.2% recurrence rate. The other study, Lorenzo et al. found that 10 out of 691 patients interrupted their SGLT2i use due to rUTIs.
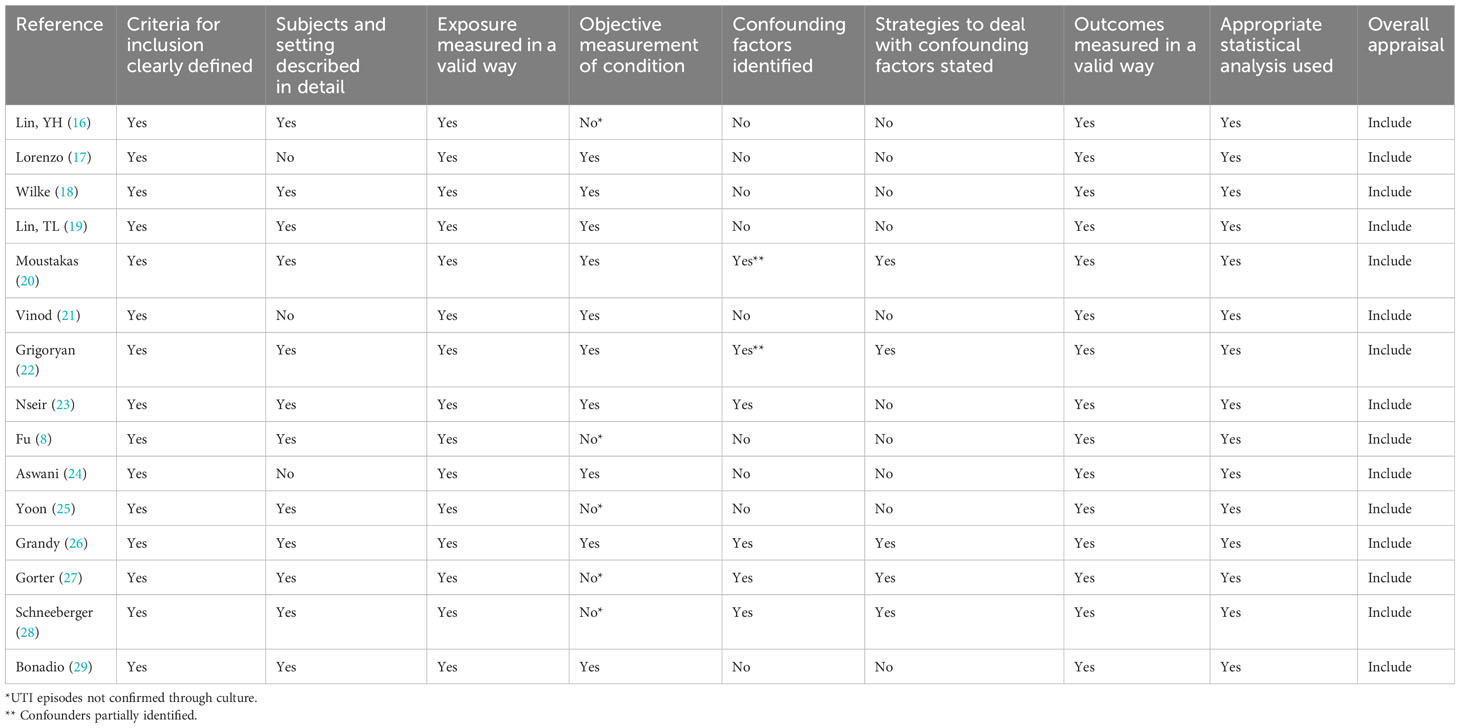
Risk of bias assessment
The Joanna Briggs Institute (JBI) critical appraisal checklist was used to analyze the risk of bias for the thirteen cohort studies and two cross-sectional analyses in this review. The results are summarized in (Table 2). The studies included in this review were not focused on acute treatment of a single UTI infection, and as a result, certain criteria for the risk of bias assessment categories were not applicable. The articles otherwise scored highly for similarities in the groups, exposure measurement, and statistical analysis. Some of the studies did not identify and/or address confounding variables, however, these studies were still high enough quality for inclusion.
Discussion
This systematic review of existing literature on rUTIs in women with diabetes was done according to PRISMA guidelines. In addition to a relative dearth of publications, we observed that only two studies reported exclusively on rUTIs in T2DM women. The others included UTI data as well as information on diabetic men. RUTI definitions were heterogeneous and most did not comply with the more recently adopted criteria of two symptomatic UTIs in six months of three in a year (13). In the end, fifteen articles were identified as relevant to this topic, covering various subtopics including rUTI incidence rates, characteristics, symptoms, risk factors, treatments, and outcomes.
RUTI incidence rates in diabetic populations were the most reported findings across the studies. Overall, four studies reported non-comparative recurrence rates ranging from 23.4% to 37% in different diabetic populations. Six studies compared rUTI rates between populations, most commonly diabetics vs. non-diabetics. Four of these yielded statistically significant differences between groups, although not all studies fully addressed possible confounding variables. Two studies found differences in rUTI rates between diabetics and non-diabetics that were not statistically significant. These differences between studies are possibly the result of variable diabetes groups (T2DM vs all diabetics), small study populations, short study durations, and a lack of rUTI focus.
Another aim of this review was to assess the risk factors for rUTI. Four of five studies found that diabetes was a determining risk factor for rUTI, but no specific conclusion can be drawn regarding T2DM as a risk factor, specifically. Additional risk factors for rUTI in diabetic patients mentioned across the studies included retinopathy, overactive bladder, incontinence, kidney problems, narrow/blocked arteries, insulin treatment, age, and duration of diabetes. However, many of these findings were inconsistent across studies. This is again likely the result of the differences in study populations, methodology, and rUTI definitions.
Antibiotic usage and resistance were the focus of treatment data across studies. Due to the varying geographical locations of the studies included in this review, guidelines for antibiotic prescriptions varied greatly, limiting our ability to compare antibiotic prescription findings. Despite these differences, it was reported that longer durations of antibiotic treatment in diabetic patients does not correlate with less UTI recurrences. Otherwise, no significant findings were reported for antibiotic resistance patterns between diabetic and non-diabetic groups.
E. coli was found to be the most frequent causative agent of both UTI and rUTI across studies, both for diabetic and non-diabetic groups. Only one study found a significant difference between the causative agent of UTI/rUTI in diabetic and non-diabetic groups; ESBL was determined to be higher in diabetics. For symptoms of rUTI specifically, only one study reported relevant findings. Moustakas et al. found that urinary urgency, abdominal pain, and the absence of genital symptoms were correlated with having ≥3 UTIs in a year.
Areas of gaps of knowledge
As underscored by this review, several gaps in knowledge in the field of rUTI research in diabetics were identified. To our knowledge, this review is the first formal systematic review of the limited literature available on the topic of recurrent urinary tract infections in type II diabetics, with a focus on female populations. This project was initiated to better understand the gaps in knowledge in this growing field and aging population. Although there has been a recent suggestion for a standardized definition of rUTI, many of the studies in this review used different diagnostic criteria. In addition, there were so few rUTI studies in T2DM women specifically, that studies with unspecified types of diabetes (T1DM and T2DM not separated) and studies that included some men had to be included. Due to these large differences in study populations, methodologies, and aims, performing a valuable statistical comparison between studies, such as a meta-analysis, was not possible. UTI recurrence and incidence rates were difficult to compare. Additionally, treatment options varied greatly between countries because of guidelines as well as high rates of antibiotic-resistant organisms and antibiotic allergies (6, 13, 18, 20–22, 28). This resulted in an inability to compare treatment results across studies. Lastly, patients with diabetes often had several comorbidities that were difficult to control for, and multiple studies did not identify confounding variables.
Conclusions
This systematic review summarizes the literature on recurrent urinary tract infections in diabetic women. Fifteen studies from 10 countries met study criteria, providing a heterogenous population. The included articles covered subtopics from recurrent UTI rates, risk factors, symptoms, characteristics, treatments, and disease outcomes. Several studies focused on UTIs and diabetes as their primary goal, and recurrent UTIs only as their secondary target. Hence, rUTI specific results included in this review were limited and not generalizable. However, multiple studies found diabetes to be a risk factor for rUTI, supporting our initial hypothesis that rUTI rates are higher in diabetics than non-diabetics. The findings of this review indicate an urgent need for more research, specifically well-structured prospective studies to determine how best to evaluate and manage recurrent urinary tract infections in diabetic patients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Author contributions
SP: Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. PZ: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Foxman B. Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med (2002) 113(1):5–13. doi: 10.1016/S0002-9343(02)01054-9
2. Klein RD, Hultgren SJ. Urinary tract infections: microbial pathogenesis, host–pathogen interactions and new treatment strategies. Nat Rev Microbiol (2020) 18(4):211–26. doi: 10.1038/s41579-020-0324-0
3. De Nisco NJ, Neugent M, Mull J, Chen L, Kuprasertkul A, de Souza Santos M, et al. Direct detection of tissue-resident bacteria and chronic inflammation in the bladder wall of postmenopausal women with recurrent urinary tract infection. J Mol Biol (2019) 431(21):4368–79. doi: 10.1016/j.jmb.2019.04.008
4. Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol (2015) 13(5):269–84. doi: 10.1038/nrmicro3432
5. Glover M, Moreira CG, Sperandio V, Zimmern P. Recurrent urinary tract infections in healthy and nonpregnant women. Urol Sci (2014) 25(1):1–8. doi: 10.1016/j.urols.2013.11.007
6. Öztürk R, Murt A. Epidemiology of urological infections: A global burden. World J Urol (2020) 38(11):2669–79. doi: 10.1007/s00345-019-03071-4
7. Patterson JE, Andriole VT. Bacterial urinary tract infections in diabetes. Infect Dis Clinics (1997) 11(3):735–50. doi: 10.1016/S0891-5520(05)70383-4
8. Fu AZ, Iglay K, Qiu Y, Engel S, Shankar R, Brodovicz K. Risk characterization for urinary tract infections in subjects with newly diagnosed type 2 diabetes. J Diabetes its Complications (2014) 28(6):805–10. doi: 10.1016/j.jdiacomp.2014.06.009
9. Hirji I, Guo Z, Andersson SW, Hammar N, Gomez-Caminero A. Incidence of urinary tract infection among patients with type 2 diabetes in the UK General Practice Research Database (GPRD). J Diabetes its complications (2012) 26(6):513–6. doi: 10.1016/j.jdiacomp.2012.06.008
10. American Diabetes Association. Economic costs of diabetes in the US in 2017. Diabetes Care (2018) 41(5):917–28. doi: 10.2337/dci18-0007
11. Kamei J, Yamamoto S. Complicated urinary tract infections with diabetes mellitus. J Infection Chemotherapy (2021) 27(8):1131–6. doi: 10.1016/j.jiac.2021.05.012
12. Murray BO, Flores C, Williams C, Flusberg DA, Marr EE, Kwiatkowska KM, et al. Recurrent urinary tract infection: a mystery in search of better model systems. Front Cell Infection Microbiol (2021) 11. doi: 10.3389/fcimb.2021.691210
13. Malik RD, Wu YR, Zimmern PE. Definition of recurrent urinary tract infections in women: which one to adopt? Female pelvic Med reconstructive Surg (2018) 24(6):424–9. doi: 10.1097/SPV.0000000000000509
14. Stamm WE, Norrby SR. Urinary tract infections: disease panorama and challenges. J Infect Dis (2001) 183(Supplement_1):S1–4. doi: 10.1086/318850
15. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (2021) 372:n71. doi: 10.1136/bmj.n71
16. Lin YH, Lin CH, Huang YY, Tai AS, Fu SC, Chen ST, et al. Risk factors of first and recurrent genitourinary tract infection in patients with type 2 diabetes treated with SGLT2 inhibitors: A retrospective cohort study. Diabetes Res Clin Pract (2022) 186:109816. doi: 10.1016/j.diabres.2022.109816
17. Lorenzo MG, Romero LY, Lorenzo VT, Lara M. 4CPS-013 Discontinuation of sodium-glucose co-transporter 2 inhibitors due to recurrent genitourinary infections. Eur J Hosp Pharm (2018) 25(Suppl 1):A47. doi: 10.1136/ejhpharm-2018-eahpconf.104
18. Wilke T, Boettger B, Berg B, Groth A, Mueller S, Botteman M, et al. Epidemiology of urinary tract infections in type 2 diabetes mellitus patients: An analysis based on a large sample of 456,586 German T2DM patients. J Diabetes Complications (2015) 29(8):1015–23. doi: 10.1016/j.jdiacomp.2015.08.021
19. Lin TL, Chen GD, Chen YC, Huang CN, Ng SC. Aging and recurrent urinary tract infections are associated with bladder dysfunction in type 2 diabetes. Taiwan J Obstet Gynecol (2012) 51(3):381–6. doi: 10.1016/j.tjog.2012.07.011
20. Moustakas I, Dryllis G, Pouliakis A, Petrikos G, Daikos G, Pittaras T, et al. Emerging patterns of resistance in a cohort of Greek patients with recurrent UTIs: a pilot study. J Chemother (2019) 31(7-8):367–77. doi: 10.1080/1120009X.2019.1652013
21. Vinod C, Sayee S, Nareddy VA, Nagabhushana MV. A clinical study of urinary tract infections in diabetics and non-diabetics patients. Int J Adv Med (2019) 6(5):1421–9. doi: 10.18203/2349-3933.ijam20193683
22. Grigoryan L, Zoorob R, Wang H, Horsfield M, Gupta K, Trautner BW. Less workup, longer treatment, but no clinical benefit observed in women with diabetes and acute cystitis. Diabetes Res Clin Pract (2017) 129:197–202. doi: 10.1016/j.diabres.2017.05.005
23. Nseir W, Farah R, Mahamid M, Sayed-Ahmad H, Mograbi J, Taha M, et al. Obesity and recurrent urinary tract infections in premenopausal women: a retrospective study. Int J Infect Dis (2015) 41:32–5. doi: 10.1016/j.ijid.2015.10.014
24. Aswani SM, Chandrashekar U, Shivashankara K, Pruthvi B. Clinical profile of urinary tract infections in diabetics and non-diabetics. Australas Med J (2014) 7(1):29–34. doi: 10.4066/AMJ.2014.1906
25. Yoon BI, Kim SW, Ha US, Sohn DW, Cho YH. Risk factors for recurrent cystitis following acute cystitis in female patients. J Infect Chemother (2013) 19(4):727–31. doi: 10.1007/s10156-013-0556-2
26. Grandy S, Fox K, Hardy E. Prevalence and recurrence of urinary tract and genital infections among adults with and without type 2 diabetes mellitus in the general population: a longitudinal cohort study. J Diabetes Res Clin Metab (2013) 2:5. doi: 10.7243/2050-0866-2-5
27. Gorter KJ, Hak E, Zuithoff NP, Hoepelman AI, Rutten GE. Risk of recurrent acute lower urinary tract infections and prescription pattern of antibiotics in women with and without diabetes in primary care. Family Pract (2010) 27(4):379–85. doi: 10.1093/fampra/cmq026
28. Schneeberger C, Stolk RP, Devries JH, Schneeberger PM, Herings RM, Geerlings SE. Differences in the pattern of antibiotic prescription profile and recurrence rate for possible urinary tract infections in women with and without diabetes. Diabetes Care (2008) 31(7):1380–5. doi: 10.2337/dc07-2188
Keywords: diabetes, recurrent, UTI, urinary infection, type II diabetes
Citation: Papp SB and Zimmern PE (2023) Recurrent Urinary tract infections and type 2 diabetes mellitus: a systematic review predominantly in women. Front. Urol. 3:1275334. doi: 10.3389/fruro.2023.1275334
Received: 09 August 2023; Accepted: 22 November 2023;
Published: 12 December 2023.
Edited by:
Bassem S Wadie, Mansoura University, EgyptReviewed by:
Sakineh Hajebrahimi, Tabriz University of Medical Sciences, IranMeysam Sarshar, Bambino Gesù Children’s Hospital (IRCCS), Italy
Copyright © 2023 Papp and Zimmern. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Philippe E. Zimmern, cGhpbGlwcGUuemltbWVybkB1dHNvdXRod2VzdGVybi5lZHU=
 Sara B. Papp
Sara B. Papp Philippe E. Zimmern
Philippe E. Zimmern