
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Urol., 24 February 2023
Sec. Male Urology
Volume 3 - 2023 | https://doi.org/10.3389/fruro.2023.1100386
This article is part of the Research TopicWomen in Male Urology: 2022View all 4 articles
 Valentina Lorenzoni1
Valentina Lorenzoni1 Ilaria Palla1*
Ilaria Palla1* Guglielmo Manenti2†
Guglielmo Manenti2† Pasquale Ditonno3
Pasquale Ditonno3 Theo M. de Reijke4
Theo M. de Reijke4 Giuseppe Turchetti1
Giuseppe Turchetti1Introduction: Benign prostatic hyperplasia (BPH) is a common diagnosis among the ageing male population over 60 years and it is associated with the development of lower urinary tract symptoms (LUTS): dysuria, nocturia, increased frequency of urination, etc. LUTS negatively affect the patient’s daily activities and the quality of life. Patients with severe and persisting symptoms, not responding to pharmacological therapy, are candidates for surgical intervention. Transurethral resection of the prostate (TURP) has been the gold standard for surgical approach despite it can be associated with significant complications. Indeed, laser vaporization or enucleation are today the most broadly used surgical techniques and other minimally invasive surgical therapies (MISTs) have been introduced to reduce some complications during- and post-surgery. Moreover, a new micro-invasive approach for LUTS is represented by EchoLaser SoracteLite™ transperineal laser ablation (TPLA), an innovative, safe and feasible approach that can be performed under local anaesthesia and in an outpatient setting.
Objective: The paper aims to analyse and discuss the economic implications of standard surgical techniques and innovative approaches with a focus on TPLA thought a literature review.
Results: The literature review highlights that at present there are few studies related to the economic implications of surgical therapies for LUTS. Preliminary results show that the TPLA is a promising technique in terms of clinical and economic benefit for the treatment of obstructive LUTS. Furthermore, TPLA can be performed in an outpatient setting implying an advantage from an economic and also organizational point of view, in particular in a health emergency situation.
Conclusions: Economic literature on minimally invasive techniques and surgical approaches for the treatment of BPH is still lacking. Multicentre and long-term economic studies are needed to assess the estimated disease burden. However, direct and indirect costs associated with TPLA are minimized vs TURP and laser vaporization/enucleation.
Benign prostatic hyperplasia (BPH) is a non-cancerous enlargement of the prostate affecting more than 50% of men above 60 years (1). BPH is linked to the development of lower urinary tract symptoms (LUTS): dysuria, nocturia, increased frequency of urination etc. The obstructive symptoms can lead to complications such as urinary retention, urinary tract infection, haematuria and hydronephrosis. LUTS negatively affect the patient’s daily activities and Quality of Life (QoL), also including psychological stress due to anxiety (2). LUTS are strongly associated with ageing and several modifiable risk factors (3, 4). Therefore, prevalence of the disease and associated costs are likely to increase with future demographic changes (5).
Treatment of BPH-related LUTS depends on the severity of the problem that is usually defined based on the International Prostate Symptom Score (IPSS) which distinguishes mild (score from 0 to 7), moderate (score from 8 to 19) and severe symptoms (scores from 20 to 35) (6).
Common clinical practice foresees initial treatment of patients with moderate to severe symptoms with pharmacotherapy (α-blocker, 5α-reductase inhibitor or combined therapy). Low compliance, intolerance or allergy, and costs to maintain therapy are major disadvantages that have a negative impact on effectiveness of this approach. Moreover, there is recent evidence that medical therapy for LUTS due to BPH increases the risk of cardiac failure and stroke (7), the risk of suicide and psychological adverse events (8) and dementia (9).
Patients with severe and persisting symptoms, not responding to pharmaceutical therapy, are candidates for surgical intervention. Among these, transurethral resection of the prostate (TURP) has long been considered the gold standard; it can however be associated with significant complications such as bleeding, urinary incontinence and retrograde ejaculation (10) and it is performed under regional or general anaesthesia which requires the patient be treated in inpatient setting. Laser therapy such as Holmium Laser Enucleation of the prostate (HoLEP), Thulium and Greenlight laser therapy are implemented with the aim to reduce perioperative bleeding (and post-op blood transfusions) and are emerging as a new standard for BPH surgery (11).
Other minimally invasive surgical therapies (MISTs) have been introduced in the past years being nowadays available and recognized (although as “investigational”) also by the American Urology Association (AUA) and the European Association of Urology (EAU) (11). In detail, thermo-ablative strategies such as transurethral microwave therapy (TUMT) and transurethral vaporization of the prostate (TUVP), mechanical therapy as Urolift and intra-prostatic stent (iTIND), water based treatment as Aquablation, Rezūm system, an ablative system, prostatic artery embolization (PAE) and the use of Intraprostatic Injectables could be considered depending on the availability of the procedure, patient risk, prostate volume, patients’ preference and the sustainability of the approaches. New techniques such as Aquablation use a transurethral approach implying similar complications as TURP; furthermore, Aquablation needs general anaesthesia. Rezūm, which is a thermal therapy based on a transurethral approach, leads to high risk of urethral damage with irritative symptoms in the post-operative period and haematuria. A large-scale analysis of real-world healthcare data for enlarged prostate procedures presented at the American Urological Association 2021 Annual Meeting, revealed that surgical re-treatment rates are comparable among the UroLift System, TURP and GreenLight, while highest for Rezūm (12).
EchoLaser SoracteLite™ transperineal laser ablation (TPLA) represents an innovative, safe and feasible micro-invasive approach for LUTS treatment (13, 14) that can be performed under local anaesthesia in an outpatient setting using thin introducer needles (21G). Furthermore, a recent study (15) shows that the TPLA ensures good and stable results after three years from the treatment.
The present paper aims to review and discuss the economic implications of standard surgical techniques and innovative approaches with a focus on TPLA.
TURP has been considered the gold standard for the management of LUTS secondary to benign prostatic hyperplasia. In the last years, several techniques have been developed as safe and effective alternatives [2022 EAU Guidelines].
Despite invasiveness of the procedure that involves the insertion of a resectoscope through the urethra to remove obstructing tissue, surgical and follow-up complications have been shown to be reduced over years with increasing experience. Moreover, alternatives have been developed and made available for patients depending on the prostate volumes even if long-term effects on relapses and complications of those alternatives are still lacking (16).
Endoscopic enucleation of the prostate (EEP) is a laser-based (Holmium, Thulium, Greenlight-PVP) and non-laser-based (monopolar, bipolar, and plasmakinetic) transurethral approach, able to enucleate completely the prostatic adenoma similar to an open prostatectomy without the side effects of an open surgery. HoLEP is emerging as a new gold standard for the surgical management of the high-volume BPH, but it is a difficult technique with a high learning curve (15). Thulium laser therapy is similar in terms of complications and re-interventions after surgery compared to HoLEP (17).
Prostate vaporization is achieved by heating the prostatic adenoma trough high-energy application. This can be accomplished by either a bipolar electrical system (TUVP) or laser energy with Greenlight. These procedures demonstrated the safety and efficacy for treatment of prostates up to 70 grams while the durability of the outcome remains a concern.
Short-term studies showed efficacy and safety of the above mentioned procedures that could be comparable with TURP, with generally a reduced hospital length of stay (18).
Main characteristics of the available approaches are detailed in Table 1.
Patelli et al. (14) presented the first data on TransPerineal Laser Ablation with a good efficacy and safety profile that should be confirmed in larger studies. For a TPLA procedure the patient is positioned in the lithotomy position and a three-way 18-F Foley catheter is inserted to permit cooling irrigation during the whole lasing period in order to prevent injuries to the urethral wall. Some users prefer to place normal 2 way catheter. Following local anaesthesia of the perineal region and periprostatic plexus, the procedure is carried out under transrectal ultrasound (US) guidance. One or two 21 G introducer needles (EchoLaser introducer needle, Elesta SpA, Calenzano) for each lobe are simultaneously inserted transperineally in the adenoma and placed as parallel as possible in the longitudinal plane of the prostate (Figure 1A). In order to facilitate the insertion of the needles, the transrectal US biplanar probe is combined with a multi-channel needle guide, with a dedicated planning tool device (Echolaser Smart Interface, Elesta SpA, Calenzano) with a software displaying needle trajectories and safety area overlying the US image in the longitudinal plane (Figure 1B) and transverse plane (Figure 1C).
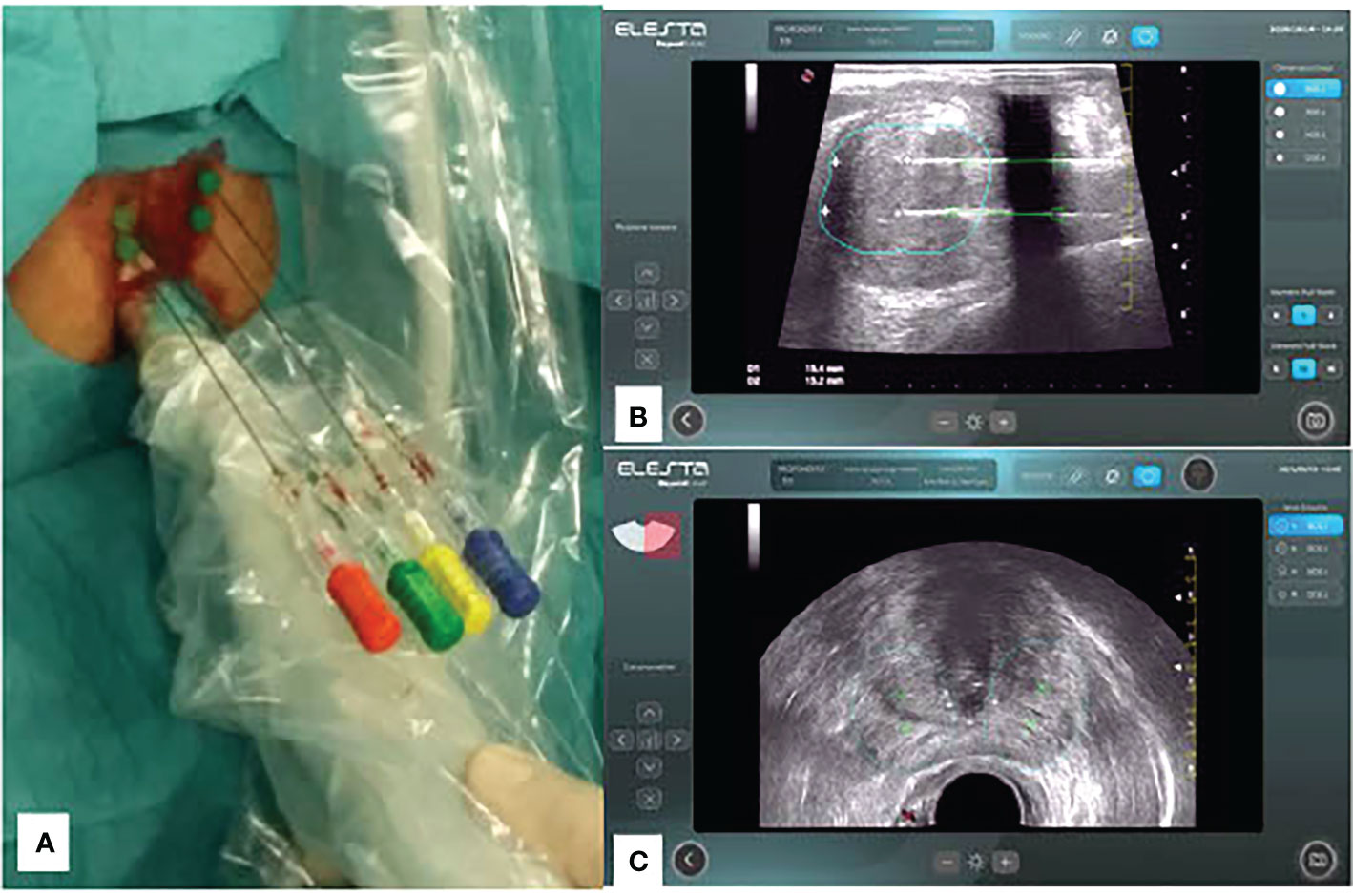
Figure 1 (A) Transperineal approach with 4 fibers placed in position and monitored by US images coming from Biplane probe; (B) Treatment Planning: longitudinal plane with two fibers positioned at fair safety distances from prostate capsule (@1800J) including 1 Pull-Back of 10mm; (C) Treatment Planning: transverse plane with planning of needle/fiber position according safety distances at 1800J.
Subsequently, one 272µm flat-tip optical fiber (EchoLaser Fiber Optic for PLA, Elesta SpA, Calenzano) per needle is introduced. The safety area is determined after introduction of the laser fibers. The optical fibers are then connected with a continuous wave diode laser source (EchoLaser, Elesta SpA, Calenzano) (Figure 2) and energy delivery is performed with a fixed power (3W, 1800 J - however it has been observed by some users that optimal outcome might be achieved with higher power, up to 5W, which in their experience was shown to be well tolerated by non-anaesthetized patients) (19).The number of applicators per prostatic lobe and the number of pull-back are chosen according to prostate shape and volume taking into account safety distance from urethra, prostatic capsule and bladder neck. The use of Echolaser Smart Interface device for the treatment planning helps in positioning the optical fibers through a graphical representation of a safety area even in the case of multiple applicators. Correct positioning of the fiber tips preserve the anatomical structures such as bladder neck, verumontanum, urethra and sphincter and thus preserving antegrade ejaculation and urinary continence (19) and reducing post-op complications and side effects.

Figure 2 EchoLaser consists of a multisource laser and a touch panel for treatment planning (Echolaser Smart Interface).
Several retrospective and prospective series with intermediate term of follow-up demonstrated that TPLA is a safe and feasible procedure for the treatment of LUTS due to BPH, with a good safety profile. Cai et al. (20) and Pacella et al. (21) retrospectively and Frego et al. (22), De Rienzo et al. (23) prospectively demonstrated a significant improvement in IPSS score, in peak urinary flow rate (Qmax), post void residual, a reduction in prostate volume at 3 months and improvement in QoL at follow-up. The study performed by Cai et al. (20) shows that the IPSS score improved from 22.7 ± 5.3 (baseline) to 9.1± 3.2 (after 6 months); the Qmax improved from 8.5 ± 3.0 to 15.2 ± 4.8 mL/s (P < 0.001), the PVR increased from 78.7± 58.8 to 30.3 ± 34.2 (P<0.05), and the mean prostate volume ranged from 70.8 ± 23.8 to 54.7± 20.9 mL (P<0.05). In the study of Pacella et al. (21), at 12 months the mean IPSS score improved from 22.5 ± 4.5 to 7.0 ± 2.9 (P < 0.001); the PVR from 71.7 ± 93.9 to 17.8 ± 51.0 ml (P < 0.001), Qmax from 8.6 ± 5.2 to 15.0 ± 4.0 ml/s (P < 0.001) and the QoL from 4.2 ± 0.6 to 1.6 ± 0.9 (P < 0.001).
In Frego et al. (22), IPSS score decreases from 22 at 6 points; the median postoperative Qmax improved by +57.8%, +98%, and +115.8%, at 3, 6, and 12 months; the post void residual decreases from 60 ml a 30 ml; the median prostate volume significantly decreased by a − 21.3%, − 29%, and − 41%, respectively at 3, 6 and 12 months. In De Rienzo et al. (23), the IPSS score amounts to 18.3 ± 3.9 in the preoperative phase and to 6.1 ± 2.6 at 6 months; the Qmax improved from 9.2 ± 3.4 (preoperative) to 13.9 ± 6.2 (6 months); the post void residual decreases from 81.8 ± 62.6 (preoperative) to 14.0 ± 16.7 (6 months). Furthermore, the ejaculatory function is maintained at all follow up visits up to 12 months (21) and the sexual function is preserved in all sexually active patients (19).
The study performed by Manenti et al. (24) assessing the impact of ultrasound-guided TPLA shows that the procedure is a safe, manageable and effective treatment for LUTS. The patients had an improvement in urinary symptoms, preserve the sexual and erectile function. The results at 12 months in terms of IPSS score, PVR, Qmax and QoL are comparable with the other cited studies in the paper.
The recent study performed by Sessa et al. (25) aimed to assess the early functional and sexual outcomes in 38 patients underwent to TPLA between April and February 2022 in a single center. The study showed that the median time of procedure was 31 minutes (IQR 28-37) and 37/38 patients were discharged within 8 hours of hospital stay. Qmax improved from 9.1 (8.0-11.5) at baseline to 10.6 (9.0-13.6) at 1 month, 11 (9.4-13.6) at 12 (9.5-15.0) at last follow up (range 4-12 months). The median postoperative IPSS decreased by -14%, -36% and -35% at 1 month, 3 months and at last follow up. Ejaculation was preserved in all patients.
From the study perfomed by Gerbasi et al. (15) emerged that 20/21 patients submitted to TPLA from September 2018 to March 2019 presented a significant improvement in IPSS (-37.2%) and QMax (+45.8%) after three years of the treatment. The authors underlined that the ultra-minimally invasive surgical approach could be an alternative to medical therapy and more invasive surgical approaches. Furthermore, from the study emerged that the improvement of the functional outcomes is maintained stable over the time after 3 years1.
In January 2023, Sessa et al. (26) have published a review with the aim to revise the current evidence on surgical and functional outcomes related to TPLA for LUTS due to BPH. The review included 7 studies of which 6 we have presented. The review empathizes the promising results in terms of functional outcomes and patient safety; but highlights the need to implement prospective studies to compare the results of TPLA versus other techniques. Recently, it was published the protocol of a randomized clinical trial comparing TPLA versus TURP aims to analyze the impact in terms of relief in benign prostatic obstruction and preservation of ejaculatory function at 1, 3 and 6 months (27).
However, randomized clinical trials in multicenter settings are desirable to demonstrate the advantages over a long period (22). Currently, it is published the study protocol of the first multicenter randomised clinical trial including 16 participating centres in China, Italy, Switzerland, and Poland aims to compare the efficacy and safety of TPLA respect to TURP (28).
With respect to the health economic implications, literature data showed that pharmacological treatment is less costly with respect to surgical treatment, but those approaches were also shown to be not cost-effective (16). To provide an overview about currently available non-pharmacological treatments, a literature review was performed as part of the present study. A review of the English language literature was perfomed using two databases (PubMed and Scopus) from 2011 to 2021 (Additional File 1 for details about the methods and searching strategy used). An additional research was performed in February 2023 to research the latest evidence.
Table 2 summarizes the results of 10 studies included in the literature review. Six of them performed a formal health economic evaluation, either a cost-utility (CUA) or a cost-effectiveness analysis (CEA) (29–31, 33, 34); 4 were simple cost-analyses (32, 35–37) and just one study also reported a budget impact analysis (BIA) (30). Almost all the studies performed a comparison just between Greenlight PVP (Photoselective Vaporization of the Prostate) and TURP (29–32, 34, 36). Ulchaker et al. (33) considered different available treatments including medical treatment, convective Radiofrequency (RF), prostatic urethral lift (UroLift®), PVP and TURP; Brown et al. (38) considered PAE, PVP and TURP and Ahn et al. (35) compared medical treatment versus surgery. Finally, Noble et al. (38) compared TURP and ThuVARP (Thulium laser transurethral vaporesection). Time period considered in the studies varied from 1-month to 2-years. In almost all studies only direct health costs were considered.
Despite TURP is considered the gold standard according to a clinical perspective, novel alternatives such as PVP (GreenLight laser) were shown to be cost-effective compared to TURP in almost all studies considering those alternatives (27, 31, 33, 34). In detail, PVP has been shown to be performed mainly as an outpatient procedure or day-surgery thus reducing costs associated with hospital stay, but also imply lower readmissions and post-operative complications (ie, bleeding) possibly. The study comparing PAE, PVP and TURP showed that PAE was less costly compared to TURP and PVP; PAE has fewer complications and a shortened length of hospital stay (37). ThuVARP has been shown to be not a cost-effective alternative to TURP (Table 2) (38).
Studies related to the economic impact of TPLA as a micro-invasive technique are scarce.
One abstract presented at the European Congress of Radiology in 2020 provided a preliminary evaluation of the economic implications of the TPLA (39).
An assessment was performed according to several therapeutic options available for the treatment of LUTS due to BPH. They were identified in: Open Surgery, TURP, HoLEP and TPLA.
The therapeutic process is divided into two macro-phases, each of which has been coded as follows:
- Treatment activities (TA);
- Post-treatment activities (PTA);
In detail the Treatment Activities include: preparation of the room and of the patient and the treatment. Post-treatment activities include mainly costs of post-operative hospitalizations (Table 3).
TPLA costs were compared to those of open prostatectomy (OP), TURP, HoLEP and PVP showing that TPLA has lower perioperative costs with respect to the other techniques (TPLA: €2496, OP: €6406, TURP: €4804, HoLEP: €3194 and PVP: €4090).
Despite the paucity of economic evidence available about TPLA, given the characteristics of the technology and the available preliminary clinical data, some potential economic implications related to the use of the technology could be delineated. On one hand, the acquisition costs of the technology may weigh on the costs of intervention as compared to less costly options such as TURP. However, in the above mentioned abstract a lease cost of 600€ for the capital equipment was factored in, along with an average use of three consumable fiber kits per procedure (at 600€ each, for a total of 1800€). On the other hand, the possibility to perform the procedure in an outpatient setting, the micro-invasive nature of the intervention and the claimed benefit on QoL and complications, if confirmed in future studies, may reduce both direct health costs in the postoperative phase and during follow-up but also direct non-health and indirect costs (20–23).
The present study provides an overview of the economic and health economic implications of procedures for LUTS secondary to BPH.
First of all, the literature review highlights that at present there is not an abundance of studies related to the economic implications of surgical therapies for LUTS. Moreover, most of the evidence available is related to the comparison of TURP versus PVP but recently some studies explore the economic dimensions of MISTs. Recently, a cost-minimization and budget impact analysis showed that over 4 years the costs per patient with Rezūm were €2072 versus €2836 withTURP and the Rezūm is highly to be cost-saving approach compared with TURP from an Italian hospital healthcare perspective (40). From the study performed by Wu et al. (41) emerged that PAE compared with TURP resulted a cost-effectiveness strategy: the outcomes were comparable in terms of QALY (2.845 versus 2.854, respectively) but the PAE had lower costs respect to TURP ($2,934 vs $6,038). A comprehensive analysis (42) comparing several options in terms of clinical, quality of life and cost-effectiveness outcomes, generic combination therapy (CT), PUL, water vapor thermal therapy (WVTT), PVP and TURP, showed that water vapor thermal therapy could be the more convenient option over a short (1 year) and long time horizon (5 years). From the costs point of view, the least expensive treatment was WVTT whereas the most expensive was PUL ($2,019 versus $9,580, respectively).
NHS guidelines “UroLift for treating lower urinary tract symptoms of benign prostatic hyperplasia” highlighted that the UroLift System was likely to be cost saving respect the traditional approaches: over 5 years UroLift was estimated to save per person £981 respect to bipolar TURP, £1,242 compared with monopolar TURP and £1,230 respect to HoLEP. The cost savings were attributed to reduced length of stay and procedure time of UroLift respect to the other techniques (43).
At the present, we don’t not know studies evaluating the full spectrum of costs potentially associated with the treatment of LUTS, in particular exploring the dimensions of direct non-health costs and indirect costs and exploring a long-term horizon.
This translates into the lack of guidance for clinicians and healthcare providers, particularly for what concerns alternatives for PVP and TURP. As a consequence, TURP, despite implying higher costs and being limited to the inpatient setting, remains the preferred option and costs associated with LUTS and BPH still remain a challenge (16, 18).
Despite pharmacological treatment seems to hold the promise for lower costs in comparison with TURP, drug adherence, side-effects and lower degree of perception about symptoms improvements are all factors that limit its clinical and cost effectiveness (44, 45). Also, progression to invasive procedures should be taken into account. This is an important point, because TPLA might not only be an alternative to TURP or PVP (after pharmacological treatment fails), but also to pharmacological treatment itself, earlier in what is generally known as “patient journey”.
In the last years, several new MISTs emerged for the treatment of symptoms due to BPH aiming to improve the patient’s quality of life with similar efficacy compared to standard treatment. Clinical studies showed some degree of benefits associated with them although duration of follow up is still short to intermediate (16, 20–23). Moreover, many studies underline that the physician’s decision related to the treatment is also based on the patient’s preference.
TPLA minimally invasive technique is an emerging promising approach to be used in treatment of obstructive LUTS while preliminary results are promising both in terms of clinical and economic benefit. Also, as other MIST'S, the fact that the treatment could be delivered in an outpatient setting is of paramount importance not only to reduce costs, but also to avoid interruption or delay of care during a health emergency like eg the COVID-19 pandemic (24).
Solid evidence about the economic implications about MIST'S and surgical approaches (like PVP or others) for the treatment of BPH are still lacking thus not providing guidance for clinically effective and sustainable choice among alternatives available for those patients. In particular, multicenter and long-term economic studies on all available treatment modalities are urgently needed to better assess the estimated disease burden. However, direct and indirect costs associated with EchoLaser TPLA are minimized versus TURP and laser vaporization/enucleation.
VL and IP contributions include selecting studies, analyzing and presenting results. All authors contribute to write and revise the manuscript. All authors read and approved the final manuscript.
This work was supported by Elesta SpA. The funding body was not involved in the study design, data extraction, analysis, and description, or manuscript writing.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2023.1100386/full#supplementary-material
BPH, Benign prostatic hyperplasia; LUTS, Lower urinary tract symptoms; TURP, Transurethral resection of the prostate; TPLA, Transperineal laser ablation; QoL, Quality of Life; IPSS, International Prostate Symptom Score; HoLEP, Holmium Laser Enucleation of the prostate; MISTs, minimally invasive surgical therapies; AUA, American Urology Association; EAU, European Association of Urology; TUMT, transurethral microwave therapy; TUVP, transurethral vaporization of the prostate; iTIND, intra-prostatic stent; PAE, prostatic artery embolization; EEP, Endoscopic enucleation of the prostate; CUA, cost-utility analysis; CEA, cost-effectiveness analysis; BIA, budget impact analysis; RF, Radiofrequency; TA, Treatment activities; PTA, Post-treatment activities.
1. Bengtsen M, Heide-Jørgensen U, Sandfeld Blichert-Refsgaard L, Johannesson Hjelholt T, Borre M, Nørgaard M. Positive predictive value of benign prostatic hyperplasia and acute urinary retention in the Danish national patient registry: A validation study. Clin Epidemiol (2020) 12:1281–85. doi: 10.2147/CLEP.S278554
2. Park S, Ryu JM, Lee M. Quality of life in older adults with benign prostatic hyperplasia. Healthcare (2020) 8(2):158. doi: 10.3390/healthcare8020158
3. Martin SA, Haren MT, Marshall VR, Lange K, Wittert Gary A. Prevalence and factors associated with uncomplicated storage and voiding lower urinary tract symptoms in community-dwelling Australian men. World J Urol. (2011) 29:179–84. doi: 10.1007/s00345-010-0605-8
4. Gacci M, Corona G, Vignozzi L, Salvi M, Serni S, De Nunzio C, et al. Metabolic syndrome and benign prostatic enlargement: a systematic review and meta-analysis. BJU Int (2015) 115:24–31. doi: 10.1111/bju.12728
5. Taub DA, Wei JT. The economics of benign prostatic hyperplasia and lower urinary tract symptoms in the united states. Curr Urol Rep (2006) 7:272–81. doi: 10.1007/s11934-996-0006-0
6. Barry MJ, Fowler FJ Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American urological association symptom index for benign prostatic hyperplasia. the measurement committee of the American urological association. J Urol (1992) 148:1549. doi: 10.1016/S0022-5347(17)36966-5
7. Lusty A, Siemens DR, Tohidi M, Whitehead M, Tranmer J, Nickel JC. Cardiac failure associated with medical therapy of benign prostatic hyperplasia: A population based study. J Urol. (2021) 205(5):1430–37. doi: 10.1097/JU.0000000000001561
8. Nguyen DD, Marchese M, Cone EB, Paciotti M, Basaria S, Bhojani N, et al. Investigation of suicidality and psychological adverse events in patients treated with finasteride. JAMA Dermatol (2021) 157(1):35–42. doi: 10.1001/jamadermatol.2020.3385
9. Coupland CAC, Hill T, Dening T, Morriss R, Moore M, Hippisley-Cox J. Anticholinergic drug exposure and the risk of dementia: A nested case-control study. JAMA Intern Med (2019) 179(8):1084–93. doi: 10.1001/jamainternmed.2019.0677
10. Magistro G, Chapple CR, Elhilali M, Gilling P, McVary KT, Roehrborn CG, et al. Emerging minimally invasive treatment options for Male lower urinary tract symptoms. Eur Urol. (2017) 72(6):986–99. doi: 10.1016/j.eururo.2017.07.005
11. Gravas S (Chair), Cornu JN, Gacci M, Gratzke C, Herrmann TRW, Mamoulakis C, et al. EAU guidelines on management of non-neurogenic male lower urinary tract symptoms (LUTS), incl. benign prostatic obstruction (BPO). Eur Assoc Urol (2022).
12. Teleflex announces Large-scale analysis of real-world healthcare claims data for enlarged prostate procedures at the American urological association 2021 annual meeting (2021) Las Vegas.
13. van Kollenburg RAA, van Riel LAMJG, Bloemen PR, Oddens Jorg R, de Reijke Theo M, Beerlage Harrie P, et al. Transperineal laser ablation treatment for lower urinary tract symptoms due to benign prostatic obstruction: Protocol for a prospective In vivo pilot study. JMIR Res Protoc (2020) 9(1):e15687. doi: 10.2196/15687
14. Patelli G, Ranieri A, Paganelli A, Mauri G, Pacella CM. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: A feasibility study. Cardiovasc Intervent Radiol (2017) 40(9):1440–46. doi: 10.1007/s00270-017-1662-9
15. Gerbasi S, Minafra DR, Gaetano L, Rella L, Lippolis G, Ditonno P. Three years outcomes of transperineal laser ablation of the prostate. Eur Urol Open Sci (2022) 44(Suppl.1). doi: 10.1016/S2666-1683(22)01164-8
16. Smith C, Craig P, Taleb S, Young S, Golzarian J. Comparison of traditional and emerging surgical therapies for lower urinary tract symptoms in men: A review. Cardiovasc Intervent Radiol (2017) 40(8):1176–84. doi: 10.1007/s00270-017-1575-7
17. Lokeshwar SD, Harper BT, Webb E, Jordan A, Dykes Thomas A, Neal Durwood E Jr, et al. Epidemiology and treatment modalities for the management of benign prostatic hyperplasia. Transl Androl Urol. (2019) 8(5):529–39. doi: 10.21037/tau.2019.10.01
18. Gill BC, Ulchaker JC. Costs of managing benign prostatic hyperplasia in the office and operating room. Curr Urol Rep (2018) 19(9):72. doi: 10.1007/s11934-018-0822-z
19. Bianco F, Lopez-Prieto A, Luna E, Luis A, Gheiler E, Kaufman A, et al. Transperineal laser ablation for benign prostatic hyperplasia (bph): feasibility and safety. J Urol (2021) 206(3S). doi: 10.1097/JU.0000000000002021.05
20. Cai HJ, Fang JH, Kong FL, Xu CK, Chen CH, Wang W, et al. Ultrasound-guided transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a new minimally invasive interventional therapy. Acta Radiol (2021) 63(4). doi: 10.1177/02841851211003289
21. Pacella CM, Patelli G, Iapicca G, Manenti G, Perretta T, Ryan Colleen P, et al. Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study. results at 6 and 12 months from a retrospective multi-centric study. Prostate Cancer Prostatic Dis (2020) 23(2):356–63. doi: 10.1038/s41391-019-0196-4
22. Frego N, Saita A, Casale P, Diana P, Contieri R, Avolio Pier P, et al. Feasibility, safety, and efficacy of ultrasound-guided transperineal laser ablation for the treatment of benign prostatic hyperplasia: a single institutional experience. World J Urol (2021) 39:3867–73. doi: 10.1007/s00345-021-03685-7
23. de Rienzo G, Lorusso A, Minafra P, Zingarelli M, Papapicco, Lucarelli G, et al. Transperineal interstitial laser ablation of the prostate, a novel option for minimally invasive treatment of benign prostatic obstruction. Eur Urol. (2021) 80(1):95–103. doi: 10.1016/j.eururo.2020.08.018
24. Manenti G, Perretta T, Calcagni A, Ferrari D, Ryan Colleen P, Fraioli , et al. 3-T MRI and clinical validation of ultrasound-guided transperineal laser ablation of being prostatic hyperplasia. Eur Radiol exp. (2021) 5:41. doi: 10.1186/s41747-021-00239-9
25. Sessa F, Polverino P, Bisegna C, Siena G, Lo Re M, Spatafora P, et al. Transperineal laser ablation of the prostate with EchoLaserTM system: perioperative and short-term functional and sexual outcomes. Front Urol. (2022) 2:969208. doi: 10.3389/fruro.2022.969208
26. Sessa F, Polverino P, Siena G, Bisgna C, Lo Re M, Spatafora P, et al. Transperineal laser ablation of the prostate (TPLA) for lower urinary tract symptoms due to benign prostatic obstruction. J Clin Med (2023) 12:793. doi: 10.3390/jcm12030793
27. Transperineal laser ablation of prostate versus transurethral prostate resection for benign prostatic obstruction: A randomized clinical trial (2021). Available at: https://clinicaltrials.gov/ct2/show/NCT04781049.
28. Zhang W, Guo Q, Chen L, Chen L, Meng Z, Xu Y, et al. The design and rationale of a multicentre randomised controlled trial comparing transperineal percutaneous laser ablation with transurethral resection of the prostate for treating benign prostatic hyperplasia. Front Surg (2021) 8:755957. doi: 10.3389/fsurg.2021.755957
29. Whelan JP, Bowen JM, Burke N, Woods EA, McIssac GP, Hopkins RB, et al. A prospective trial of GreenLight PVP (HPS120) versus transurethral resection of the prostate in the treatment of lower urinary tract symptoms in Ontario, Canada. Can Urol. Assoc J (2013) 7(9-10):335. doi: 10.5489/cuaj.180
30. Bowen JM, Whelan JP, Hopkins RB, Burke N, Woods EA, McIsaac GP, et al. Photoselective vaporization for the treatment of benign prostatic hyperplasia. Ont Health Technol Assess Ser (2013) 13(2):1–34.
31. Benejam-Gual JM, Sanz-Granda A, Garcia-Miralles Gravalos R, Severa-Ruiz de Velasco A, Pons-Viver J. Cost-effectiveness analysis at 2 years of surgical treatment of benign prostatic hyperplasia by photoselective vaporization of the prostate with GreenLight-photo vaporization 120 W versus transurethral resection of the prostate. Actas Urologicas Espanolas. (2014) 38(4):238–43. doi: 10.1016/j.acuroe.2014.02.007
32. Hsu YC, Lin YH, Chou CY, Hou CP, Chen CL, Chang PL, et al. Economic evaluation study (Cheer compliant) laser prostatectomy for benign prostatic hyperplasia. Medicine (2016) 95(5):e2644. doi: 10.1097/MD.0000000000002644
33. Ulchaker JC, Martinson M. Cost-effectiveness analysis of six therapies for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia. ClinicoEconom. Outcom. Res (2018) 10:29–43. doi: 10.2147/CEOR.S148195
34. Erman A, Masucci L, Krahn MD, Elterman DS. Pharmacotherapy vs surgery as initial therapy for patients with moderate-to-severe benign prostate hyperplasia: a cost-effectiveness analysis. BJU Int (2018) 122(5):879–88. doi: 10.1111/bju.14520
35. Ahn HS, Kim SJ, Choi JB, Choo SH, Shim KH, Kim SI. Long-term cost comparison between surgical and medical therapy for benign prostatic hyperplasia: a study using hospital billing data. BJU Int (2019) 123(5A):E79–85. doi: 10.1111/bju.14584
36. Masucci L, Erman A, Krahn MD, Elterman D. Cost analysis of greenlight photoselective vaporization of the prostate compared to transurethral resection of the prostate for benign prostatic hyperplasia. Can Urol Assoc J (2018) 12(12):382–7. doi: 10.5489/cuaj.5267
37. Brown AD, Stella SF, Simons ME. Minimally invasive treatment for benign prostatic hyperplasia: Economic evaluation from a standardized hospital case costing system. Cardiovasc Intervent Radiol (2019) 42(4):520–27. doi: 10.1007/s00270-018-2132-8
38. Noble SM, Ahern AM, Worthington J, Hashim H, Taylor H, Young GJ, et al. The cost-effectiveness of transurethral resection of the prostate vs thulium laser transurethral vaporesection of the prostate in the UNBLOCS randomised controlled trial for benign prostatic obstruction. BJU Int (2020) 126(5):595–603. doi: 10.1111/bju.15138
39. Manenti G, Perretta T, Ryan CP, Fraioli F, Vidali S, Porena M, et al. Diagnostic Imaging and Interventional Radiology. In European Conference on Interventional Oncology (2021):P-102 Clinical and economic impact of transperineal laser ablation (TPLA) for treating focal unilateral prostate cancer. Rome, IT: Policlinico tor Vergata. Available at: https://link.springer.com/content/pdf/10.1007/s00270-021-02819-z.pdf
40. Blissett R, Blissett D, Oselin M, Demaire C, Woodward E, Siciliano M, et al. Transurethral water therapy for treatment of lower urinary tract symptoms secondary to benign prostatic hyperplasia: a cost-minimization and budget impact analysis from an Italian healthcare perspective. Minerva Urol Nephrol (2022) 74:1–10. doi: 10.23736/S2724-6051.22.05020-0
41. Wu X, Zhou A, Heller M, Kohlbrenner R. Prostatic artery embolization versus transurethral resection of the prostate for benign prostatic hyperplasia: a cost-effectiveness analysis. J Vasc Interv Radiol (2022) 33(12):1605–15. doi: 10.1016/j.jvir.2022.08.006
42. Chugtai B, Rojanasarot S, Neeser K, Gultyaev D, Fu S, Samir. Bhattacharyya SK, et al. A comprehensive analysis of clinical, quality of life, and cost-effectiveness outcomes of key treatment options for benign prostatic hyperplasia. PloS One (2022) 17(4):e0266824. doi: 10.1371/journal.pone.0266824
43. Knight L, Dale M, Cleves A, Charlotte Pelekanou C, Morris R. UroLift for treating lower urinary tract symtoms of benign prostatic hyperplasia. Medical technology guidance update. Appl Health Econ Health Policy (2021) 20(5):669-680.
44. Cindolo L, Pirozzi L, Fanizza C, Romero M, Tubaro A, Autorino R, et al. Drug adherence and clinical outcomes for patients under pharmacological therapy for lower urinary tract symptoms related to benign prostatic hyperplasia: population-based cohort study. Eur Urol. (2015) 68(3):418–25. doi: 10.1016/j.eururo.2014.11.006
Keywords: benign prostatic hyperplasia (BPH), quality of life, innovative, lower urinary tract symptoms, TPLA, EchoLaser, Cost analysis
Citation: Lorenzoni V, Palla I, Manenti G, Ditonno P, de Reijke TM and Turchetti G (2023) Standard approach and future perspective for the management of benign prostatic hyperplasia from a health-economics point of view: the role of transperineal laser ablation. Front. Urol. 3:1100386. doi: 10.3389/fruro.2023.1100386
Received: 16 November 2022; Accepted: 09 February 2023;
Published: 24 February 2023.
Edited by:
Gian Maria Busetto, University of Foggia, ItalyReviewed by:
Daniele D’Agostino, Villa Salus Mestre Hospital, ItalyCopyright © 2023 Lorenzoni, Palla, Manenti, Ditonno, de Reijke and Turchetti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ilaria Palla, aWxhcmlhLnBhbGxhQHNhbnRhbm5hcGlzYS5pdA==
‡ORCID: Guglielmo Manenti, orcid.org/0000-0002-7659-5392
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.