
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Urol. , 31 August 2022
Sec. Pediatric, Adolescent and Developmental Urology
Volume 2 - 2022 | https://doi.org/10.3389/fruro.2022.950425
This article is part of the Research Topic Applications of Telehealth in Pediatric Urology View all 8 articles
 Zoe S. Gan1†
Zoe S. Gan1† Yash B. Shah2†
Yash B. Shah2† Natalie Plachter3
Natalie Plachter3 Dana A. Weiss3
Dana A. Weiss3 Jason Van Batavia3
Jason Van Batavia3 Stephen A. Zderic3
Stephen A. Zderic3 Aseem R. Shukla3
Aseem R. Shukla3 Arun K. Srinivasan3
Arun K. Srinivasan3 Thomas F. Kolon3
Thomas F. Kolon3 Mark R. Zaontz3
Mark R. Zaontz3 Douglas A. Canning3
Douglas A. Canning3 Christopher J. Long3*
Christopher J. Long3*Telemedicine utilization rapidly expanded throughout the coronavirus disease 2019 (COVID-19) pandemic and yielded numerous patient benefits. However, its future remains uncertain, limiting further institutional investments in telemedicine. We aimed to evaluate trends in the volume of telemedicine visits throughout the pandemic and patient factors associated with telemedicine usage to inform the future role of telemedicine in pediatric urology. An Institutional Review Board (IRB)-approved registry of pediatric urology outpatient visits was queried from June 2019 to November 2021 at a single institution. Variables of interest included patient demographics, travel distance for care, insurance status, primary visit diagnosis, and visit type (in-person visits, IPVs; or video visits, VVs). IPVs and VVs were further categorized as new patient visits (NPVs), return patient visits (RPVs), and post-operative visits (post-ops). Monthly trends in descriptive variables were summarized. A total of 51,605 pediatric urology outpatient visits occurred during the study period. Patients had a median age of 5 years [interquartile range (IQR), 1–11] and were predominantly male (71.6%), white (61.6%), and held private insurance (69%). VVs increased substantially from 0% in February 2020 to 100% in April 2020 and then subsequently declined through November 2021, although total visit volumes were increasing throughout the period. As the pandemic progressed, compared to IPVs, VVs were more likely to have an RPV visit type (80% vs. 50%–60%) and longer median travel distance (30+ vs. 14 miles). VVs were less frequently covered by subsidized insurance (20%–30% vs. 50%–70%). In summary, this study found that telemedicine usage has declined since the peak of the COVID-19 pandemic, although its use remains higher than pre-pandemic levels and appears to be associated with RPVs, longer travel distance, and private insurance coverage. Utilization has stabilized as we have emerged from peak pandemic restrictions. Further work is required to elucidate the optimal role of telemedicine and its effects on access to care in pediatric urology.
Telemedicine usage rapidly expanded throughout the coronavirus disease 2019 (COVID-19) pandemic to comply with pandemic lockdown restrictions. This change aimed to limit viral transmission between patients and providers, protect vulnerable populations from community spread, and redirect key healthcare infrastructure towards COVID-19 care. Pediatric urology was no exception, with a 75% increase in telemedicine utilization reported across urology practices internationally for May 2020 (1). As the pandemic progressed and utilization expanded, the benefits of telemedicine have become increasingly apparent. Telemedicine usage in pediatric urology has been shown to increase access to care by addressing cost and travel distance barriers, result in high satisfaction rates among families and providers, and maintain equivalent outcomes compared to in-person visits (IPVs) (2). Our previous report found that patient satisfaction analysis supports the continued use of VVs following the pandemic, along with expansion from post-operative visits to include new patient and returning patient visits (3).
Despite these benefits, the future of telemedicine remains uncertain due to reimbursement and physician concerns. Rapid VV adoption during the pandemic was largely attributable to temporary expansions of Medicare coverage and subsequent private insurance coverage during the pandemic’s onset (4). As society has moved towards post-pandemic normalcy, private insurance coverage for telemedicine has declined, and public coverage only remains due to periodic extensions of the public health emergency (5). The Centers for Medicare and Medicaid Services (CMS) has extended coverage of several telehealth services through the end of 2023 to allow time to further evaluate the permanent addition of these services to the Medicare telehealth services list (6). Additionally, pediatric urology providers have expressed concerns about the lack of best practices in pediatric telemedicine, barriers to scalability, and limited ability to establish rapport with patients and families virtually (7). Finally, telehealth can add up-front costs for institutions as they invest in the proper infrastructure, administrative personnel, technical personnel, and software technology (8). Given these concerns and uncertainties regarding future insurance coverage, institutions may be wary of further investments in telemedicine at this time.
There remains a need to further assess the effects of telemedicine on total healthcare costs, patient access to technology, and the quality of care delivery in order to inform insurance policies and ultimately shape the future provision of VVs in medical care (9). As part of an evaluation of access to care, we explore trends in the volume of telemedicine visits throughout the pandemic and patient factors associated with telemedicine usage. Our primary hypothesis is that the proportion of VVs increased during the height of the pandemic through mid-2020 and then decreased afterwards. Our secondary hypothesis is that as the pandemic progressed, compared to patients undergoing IPVs, patients undergoing VVs were more likely to have government-subsidized insurance, post-op visit type, and increased median travel distance for non-post-op visits. By determining trends in VVs conducted during the pandemic, we hope to identify which patients have been most commonly receiving telemedical care and inform recommendations for its future use in pediatric urology.
An Institutional Review Board (IRB)-approved registry of pediatric urology outpatient visits was queried from June 2019 through November 2021 to identify patients who completed any type of visit within the urology division at the Children’s Hospital of Philadelphia. For each visit, the following characteristics were extracted: age, sex, race, ethnicity, home ZIP code, ZIP code of the place of service, insurance type, visit type, and primary visit diagnosis. The following visit types were excluded from further analysis (1): IPVs that could only be completed in person by the nature of the visit and therefore did not have the option to be converted to VVs during the pandemic (clean intermittent catheterization training, office circumcision, urodynamics, etc.) and (2) VVs for which new, return, or post-op status could not be determined. The remaining in-person visits (IPVs) and virtual visits (VVs) were included for analysis and further stratified into new patient visits (NPVs), return patient visits (RPVs), and post-operative visits (post-ops). Travel distance was calculated using the geodetic distance between home ZIP code and the ZIP code of the place of service. Insurance types were stratified into private, subsidized (by Medicare, the Children’s Health Insurance Program, or the state), and other.
During the early pandemic, a federal mandate was enacted to allow equal billing for both IPVs and VVs. Our institution bills separately for VVs, and as private insurance have waned, we have continued VV for patients whose insurances permit them while switching IPV for the remaining patients.
Descriptive statistics were utilized to summarize demographic, travel distance, insurance type, and visit type data for all included visits during the study period. For each month during the study period, data regarding visit type, insurance type, and median travel distance were summarized. Categories for which there were fewer than 10 patients (e.g., IPV post-ops during April 2020) were excluded to avoid skewing the data. For VVs (NPVs, RPVs, and post-ops), the top 5 most common visit diagnoses were identified for the first half of the study period (June 2019–August 2020) and the second half of the study period (September 2020–November 2021). For comparative and discussion purposes, the peak of the COVID-19 pandemic was defined as March–April 2020, as the COVID-19 outbreak was declared a national emergency on March 13, 2020 (10).
A total of 51,605 pediatric urology outpatient visits occurred from June 2019 through November 2021. Most patients were male (71.6%) and white (61.6%) with private insurance (69.4%), and the median age was 5 years [interquartile range (IQR), 1–11) (Table 1). A total of 2,333 visits (4.5%) were excluded, leaving 49,272 included visits, of which 9.7% were VVs. Of the included IPVs, 39.2% were NPVs, 53.5% were RPVs, and 7.3% were post-ops. Of the included VVs, 17.6% were NPVs, 68.2% were RPVs, and 14.2% were post-ops.
The proportion of visits that were VVs increased substantially from 0% in February 2020 up to 100% by April 2020, coinciding with the peak of the COVID-19 pandemic (Figure 1). The proportion of VVs subsequently decreased to approximately 10%–15% and further decreased to <10% since March 2021. Overall visit volume dropped by roughly 50% during April and May 2020, then increased by June 2020 to pre-pandemic levels. Of note, overall visit volumes since March 2021 were overall slightly higher than pre-pandemic levels.
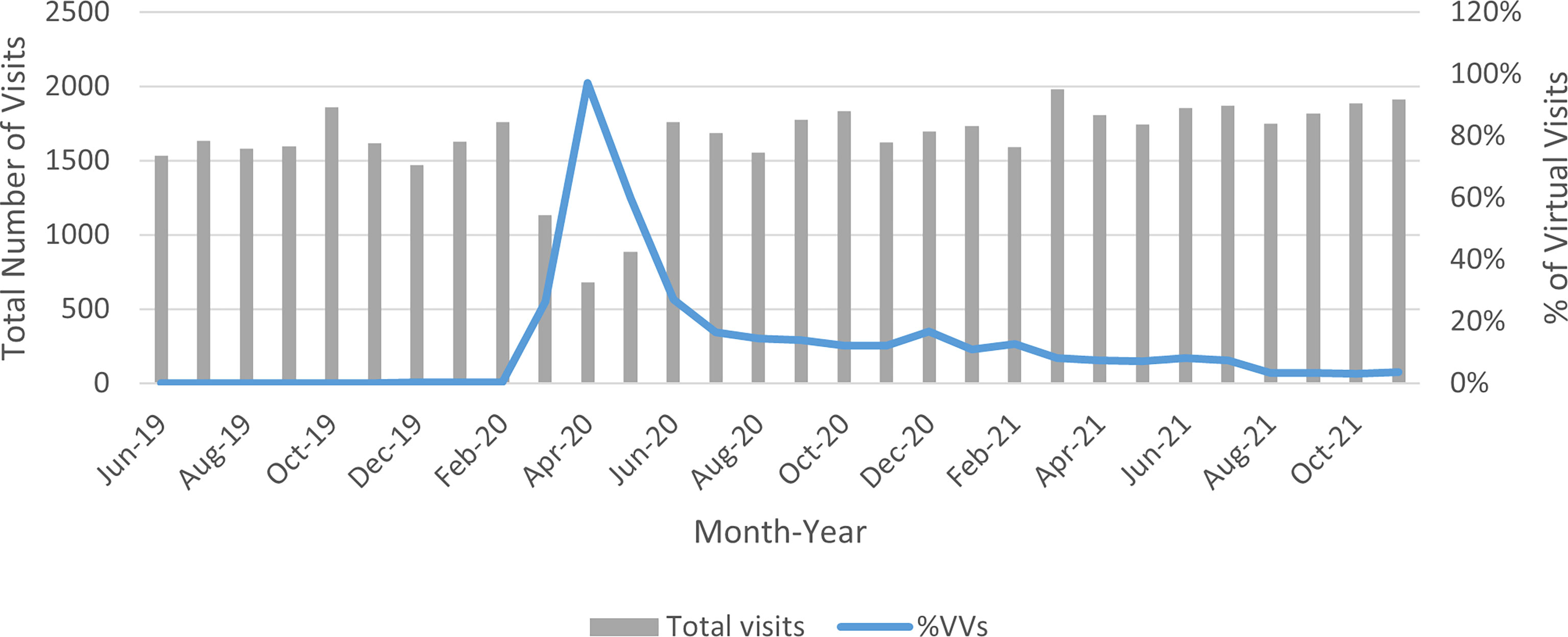
Figure 1 Variation in virtual visit usage over the study period. VVs, virtual visits. The blue line indicates the percentage of total monthly visits that were VVs.
Several differences in visit characteristics were noted between IPVs and VVs. Prior to March 2020, about 30% of IPVs were covered by subsidized insurance (no VV data was included during this period due to low volumes). After March 2020, approximately 50%–70% of IPVs and 20%–30% of VVs were covered by subsidized insurance, and these increases remained sustained over the study period (Figure 2). The few VVs prior to March 2020 were post-ops; thereafter, RPVs became the most common VV type, increasing from approximately 60% in March 2020 to approximately 80% by the end of the study period (Figure 3). NPVs initially rose to 28.4% of all VVs by April 2020, but have since plateaued under 10% by the end of the study period. Post-ops were as low as 5.5% of all VVs in June 2020 after the pandemic’s peak and since stabilized approximately 10%–20%. On the other hand, IPVs had a relatively stable distribution over the study period, with approximately 40% NPVs, 50%–60% RPVs, and just under 10% post-ops; April 2020 was an exception, when over 80% of IPVs were RPVs, and only 10% were NPVs (Figure 4).
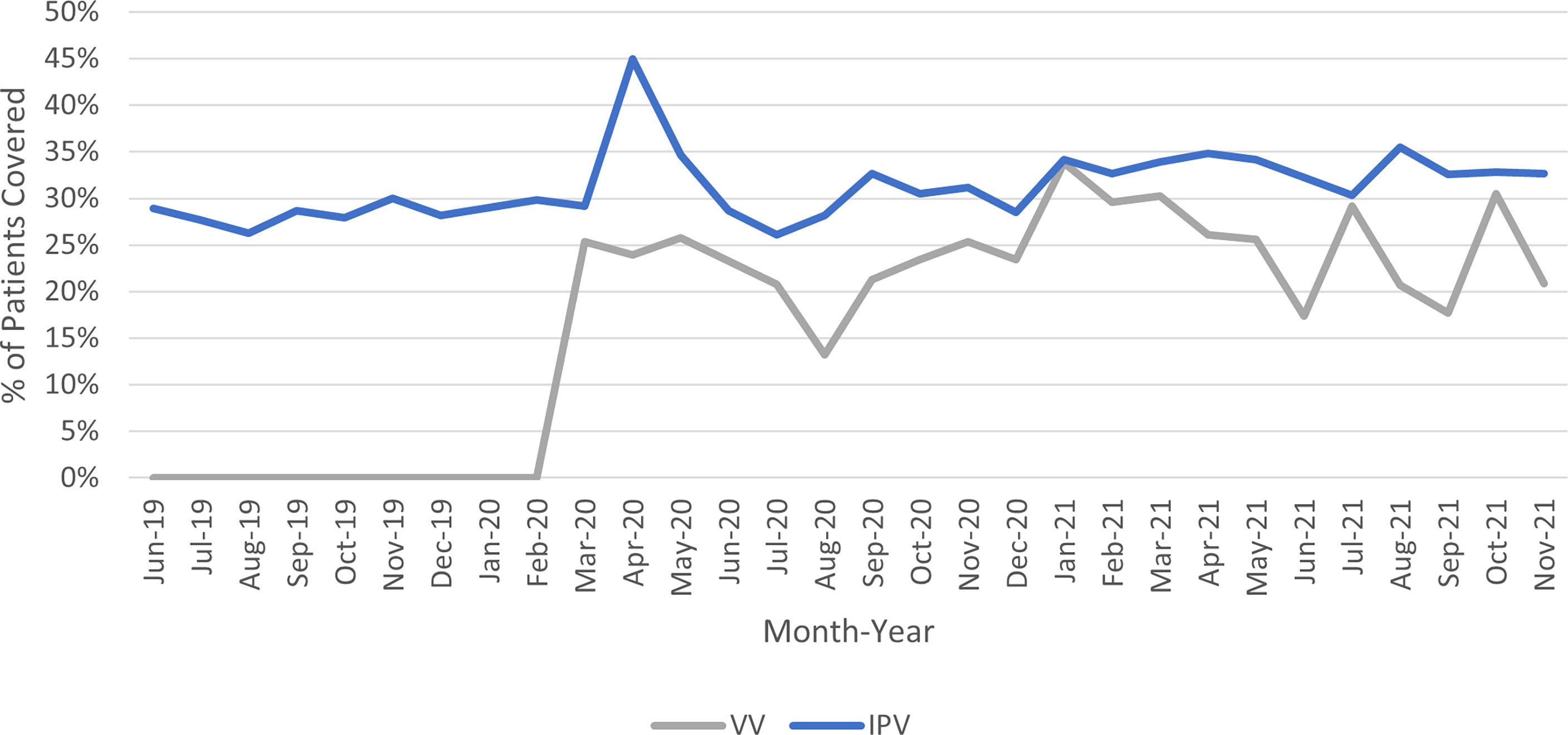
Figure 2 Variation in subsidized insurance coverage over the study period. IPV, in-person visit; VV, virtual visit.
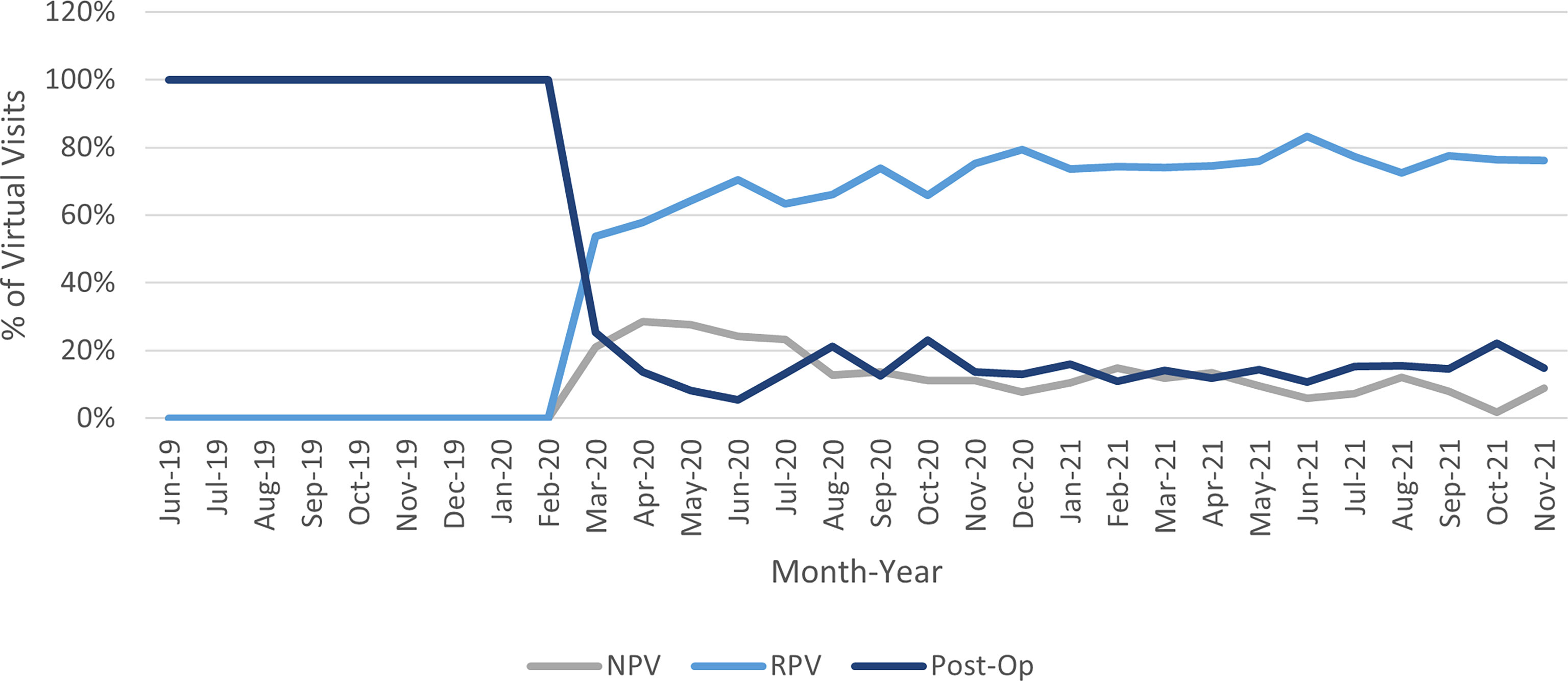
Figure 3 Variation in VV types over the study period. NPV, new patient visit; RPV, return patient visit; Post-Op, post-operative visit.
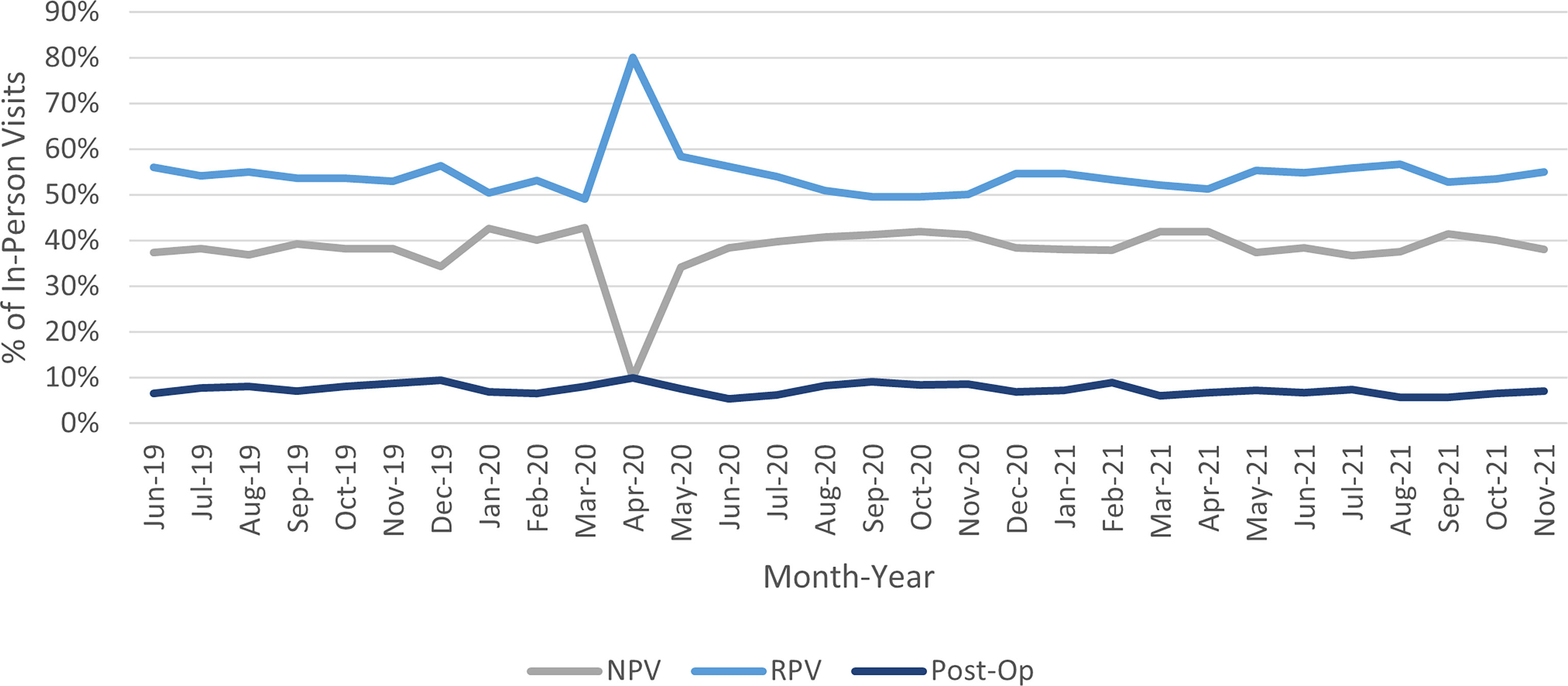
Figure 4 Variation in IPV types over the study period. NPV, new patient visit; RPV, return patient visit; Post-Op, post-operative visit.
Median travel distances remained stable approximately 10–20 miles for IPV post-ops and non-post-ops throughout the study period (Figure 5). Conversely, the median travel distances for VVs have largely increased from March 2020 to the end of the study period, with VV post-ops rising from approximately 20 miles to around 30–50 miles, and VV non-post-ops demonstrating a parallel increase from approximately 15 miles to approximately 30–65 miles. Of note, IPV visits during April 2020 were excluded due to inadequate visit numbers, as were VVs prior to March 2020.
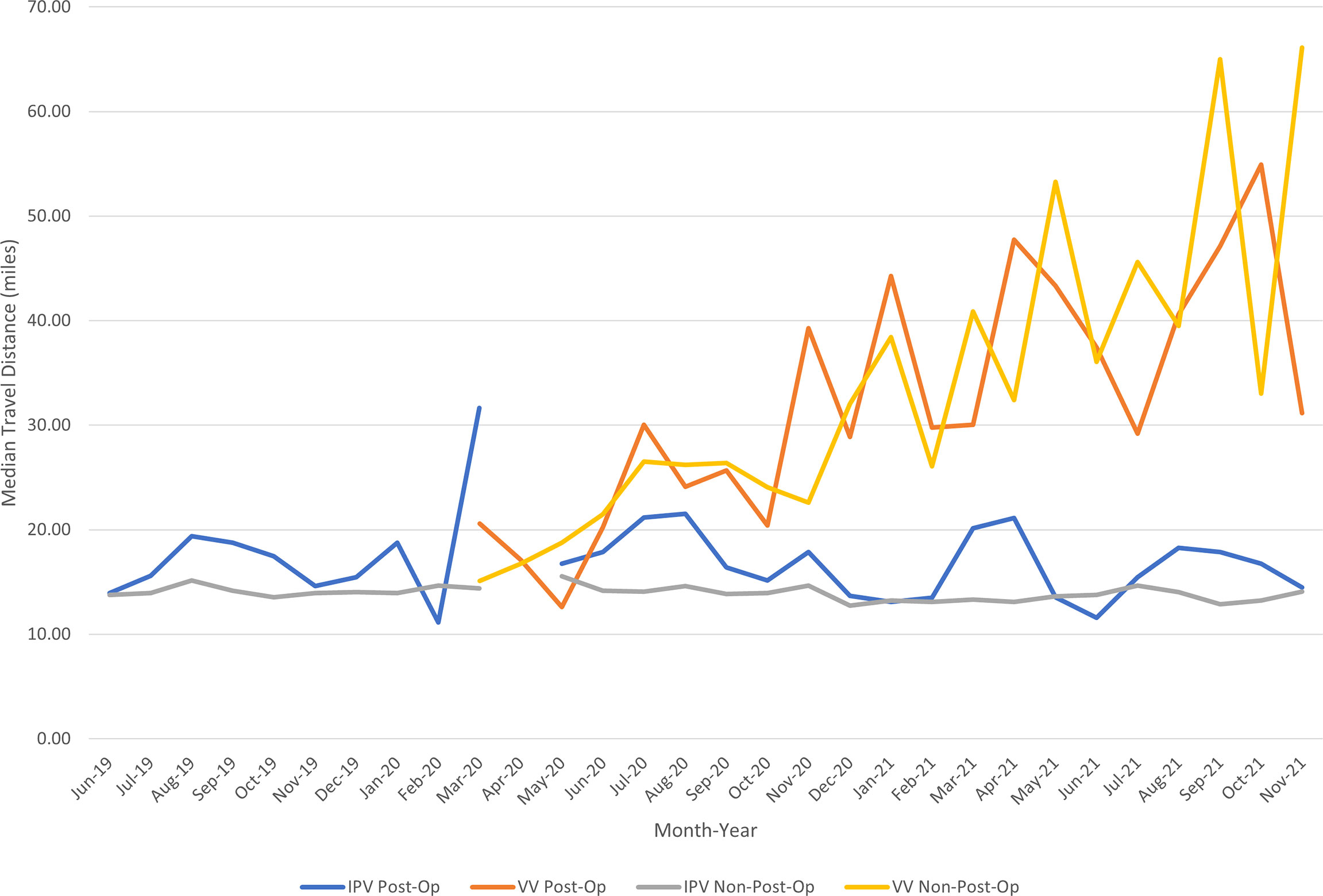
Figure 5 Median travel distance by visit type. IPV, in-person visit; Post-Op, post-operative visit; VV, virtual visit. Due to inadequate visit numbers, IPVs are excluded for April 2020, and VVs are excluded prior to March 2020.
Top VV diagnoses stratified by visit type (NPV, RPV, and post-op) are listed in Table 2. These diagnoses generally remained stable between the first (June 2019–August 2020) and the second (September 2020–November 2021) halves of the study period, regardless of visit type. However, in the second half of the study period, the top diagnosis for VV NPVs was antenatal screening, which was not otherwise a top diagnosis for the first half or the entire study period.
The present study provides an assessment of the evolution of telemedicine usage at a single high-volume, tertiary referral pediatric urology center as COVID-19 pandemic-era restrictions have softened. We found that telemedicine usage at our institution has declined since the peak of the COVID-19 pandemic, although its use by the end of 2021 has stabilized and remains higher than pre-pandemic levels. Continued telemedicine usage appears to be more commonly associated with RPVs, longer travel distance, and private insurance coverage. There are several insights to be gained from these findings regarding the future role of telemedicine in pediatric urology.
While we anticipated VVs would be most commonly utilized for post-op visits as was the case pre-pandemic, we found that VVs over the course of the study period were largely dominated by RPVs, even more so than the IPVs. This finding may be due in part to the lack of physical exam needed for most of the top VV RPV diagnoses, which remained stable over the study period and included congenital hydronephrosis, nocturnal enuresis, urinary tract infection, and unspecified neuromuscular bladder dysfunction. For NPVs, the relatively lower usage of VVs compared to IPVs may reflect parent preferences for a physical exam at the initial encounter, and physician concerns about establishing rapport virtually and subsequent preference for an in-person meeting (3, 7). However, even in the second half of the study period, which reflects a post-peak pandemic era, VV NPVs were still performed for common diagnoses such as antenatal screening, congenital hydronephrosis, and nocturnal enuresis, suggesting a new role for virtual NPVs in select situations. Post-op patients contributed a small but consistent proportion of visits for both VVs and IPVs, suggesting that they may be appropriate for either modality depending on patient factors and/or family and provider preferences. Sample diagnoses that have been previously identified as most appropriate for IPVs include cryptorchidism, meatal stenosis after hypospadias repair, and urethrocutaneous fistula (11). However, one study used a combination of in-person and virtual evaluation for undescended testes, with specifically trained advanced practice providers evaluating the patient in-person while a pediatric urologist evaluates virtually (12). If the patient was booked for surgery, the surgeon would examine the patient in the preoperative holding area to confirm the diagnosis. Overall, this approach was successful and particularly useful in a rural setting with limited access to a pediatric urologist. The efficacy and satisfaction rates for this hybrid approach or something similar to advance the telemedicine experience are not yet determined for alternative diagnoses in pediatric urology.
Telemedicine plays an increasingly significant role in expanding care to patients who would otherwise travel long distances for care. We found that travel distance was not only higher for VVs compared to IPVs regardless of visit purpose, but has also been up-trending since the peak of the pandemic. Given that the time involved in travel and waiting for care can account for up to 98.4% of the total time spent for in-person visits and that opportunity costs for pediatric urology IPVs have been calculated at 20 times higher per minute than those of VVs, patients living far away greatly benefit from the increased efficiency of telemedicine and decreased missed time from work or school (13). Further investigation is warranted to determine if these patients are from underserved areas, such as rural areas that may benefit most from expansion of telemedicine in pediatric urology, and whether telemedicine at our institution is reaching socioeconomically disadvantaged patients who may benefit most from these cost savings (14).
Despite the potential for telemedicine to increase access to care across disparity domains by overcoming travel distance and opportunity cost barriers, VVs across the study period were less frequently covered by subsidized insurance compared to IPVs. This difference was observed despite the maintenance of peak pandemic-era CMS coverage for telehealth services and anecdotal decreases in private insurance coverage. The lower proportion of VVs covered by subsidized insurance may perhaps be explained by prior work in pediatric urology demonstrating that public insurance status was associated with increased connectivity issues, and private insurance status increased the odds of having a successful VV (11). While concerns may be raised that limited access to technology and the Internet may exacerbate disparities in access to care, factors such as general neighborhood deprivation and generalized mistrust of the medical system (especially in African-Americans) may play a larger role in telehealth usage than technology alone (15). Furthermore, it is possible that patients with subsidized insurance may be more likely to attend local IPVs than choose a VV with a provider farther away. Thus, it is likely that multiple factors, not just adequate coverage by CMS, contribute to telemedicine utilization in patients with subsidized insurance. These factors may be further explored to clarify the role of telemedicine for these patients as expanded CMS telehealth coverage continues for the near foreseeable future.
This study has several limitations. We performed this analysis of practice patterns within a single large, academic center, and results may not be generalizable to all pediatric urologic practices or clinical settings. Our institution modified our telemedicine capabilities to accommodate increased VV volumes. Moreover, patient populations, insurance policies, and telemedicine protocols and workflows vary on institutional and regional bases, although the basic principles of telemedicine remain consistent. Evaluation of clinical outcomes and patient and provider satisfaction are beyond the scope of the current study. Analyses are primarily descriptive with the intention of identifying broader trends to direct future research. Finally, due to the monthly nature of the analysis, certain time points lacked an adequately number of visits for analysis. Nevertheless, this study has notable strengths, including the large overall number of visits, concurrent analysis of both IPVs and VVs, and the broad study period encompassing not only the peak pandemic period but also the post-pandemic months up to late 2021.
Since the peak of the COVID-19 pandemic, pediatric urology telemedicine visits at a single high-volume institution have declined but remain more frequently utilized than before the pandemic. Telemedicine visits are most commonly RPVs and utilized by patients with longer travel distance and private insurance coverage. These findings provide insights into the evolution of telemedicine utilization beyond the peak restrictions of the pandemic. Future directions for research include further characterizing patient populations undergoing telemedicine visits and exploring reasons underlying differential utilization.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Mallenahalli S, Fifolt M, Gundeti M, Lakshmanan Y, Gargollo P, Ost MC, et al. Survey of covid-19 impact on pediatric urology services. Can J Urol (2021) 28(5):10834–40.
2. Pettit S, Young E, Jung I. Systematic review of telemedicine in pediatric urology. J Pediatr Urol (2022) 18(1):17–22. doi: 10.1016/j.jpurol.2021.09.024
3. Gan Z, Lee SY, Weiss DA, Van Batavia J, Siu S, Frazier J, et al. Single institution experience with telemedicine for pediatric urology outpatient visits: Adapting to covid-19 restrictions, patient satisfaction, and future utilization. J Pediatr Urol (2021) 17(4):480. doi: 10.1016/j.jpurol.2021.05.012
4. Center for Medicare & Medicaid services: Medicare telemedicine health care provider fact sheet (2020). Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet.
6. Center for Medicare & Medicaid services: Calendar year (Cy) 2022 Medicare physician fee schedule final rule (Accessed Apr 10, 2022).
7. Finkelstein JB, Tremblay ES, Van Cain M, Farber-Chen A, Schumann C, Brown C, et al. Pediatric clinicians' use of telemedicine: Qualitative interview study. JMIR Hum Factors (2021) 8(4):e29941. doi: 10.2196/29941
8. de Mooij M, Foss O, Brost B. Integrating the experience: Principles for digital transformation across the patient journey. Digit Health (2022) 8:20552076221089100. doi: 10.1177/20552076221089100
9. Koma W, Cubanski J, Neuman T. Medicare And telehealth: Coverage and use during the covid-19 pandemic and options for the future. kaiser family foundation (Accessed Apr 10, 2022).
10. Trump DJ. Proclamation 9994 - Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak. March 13, 2020. Office of the Federal Register, National Archives and Records Administration. College Park, MD. Available at: https://www.govinfo.gov/content/pkg/DCPD-202000156/pdf/DCPD-202000156.pdf
11. Winkelman AJ, Beller HL, Morgan KE, Corbett ST, Leroy SV, Noona SW, et al. Benefits and barriers to pediatric tele-urology during the covid-19 pandemic. J Pediatr Urol (2020) 16(6):840.e1–.e6. doi: 10.1016/j.jpurol.2020.09.028
12. Crigger C, Sholklapper T, Mitchell K, Eckert K, Zupper S, Bartlett M, et al. From start-to-Finish: A partnership with advanced practice providers in tele-consultation within pediatric urology. Front Urol (2022) 2:876560. doi: 10.3389/fruro.2022.876560
13. Finkelstein JB, Cahill D, Young K, Humphrey K, Campbell J, Schumann C, et al. Telemedicine for pediatric urological postoperative care is safe, convenient and economical. J Urol (2020), 204(1):144–148 101097ju0000000000000750. doi: 10.1097/ju.0000000000000750
14. Ferari C, Mitchell K, Crigger C, Zupper S, Wildasin A, Ost M, et al. Bridging the gap: Building surgical subspecialty telemedicine clinics in the rural setting. Urol Pract (2022) 9(2):126–33. doi: 10.1097/UPJ.0000000000000284
Keywords: telemedicine, COVID - 19, pediatric urology, virtual visit, telehealth
Citation: Gan ZS, Shah YB, Plachter N, Weiss DA, Van Batavia J, Zderic SA, Shukla AR, Srinivasan AK, Kolon TF, Zaontz MR, Canning DA and Long CJ (2022) Evolution of telemedicine utilization for pediatric urology during the COVID-19 pandemic and beyond: A single center experience. Front. Urol. 2:950425. doi: 10.3389/fruro.2022.950425
Received: 22 May 2022; Accepted: 01 August 2022;
Published: 31 August 2022.
Edited by:
Christopher Bayne, University of Florida, United StatesReviewed by:
Chad Crigger, Johns Hopkins Medicine, United StatesCopyright © 2022 Gan, Shah, Plachter, Weiss, Van Batavia, Zderic, Shukla, Srinivasan, Kolon, Zaontz, Canning and Long. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christopher J. Long, TG9uZ0MzQGNob3AuZWR1
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.