- 1Department of Urology, Peking University People’s Hospital, Beijing, China
- 2Department of Pathology, Peking University People’s Hospital, Beijing, China
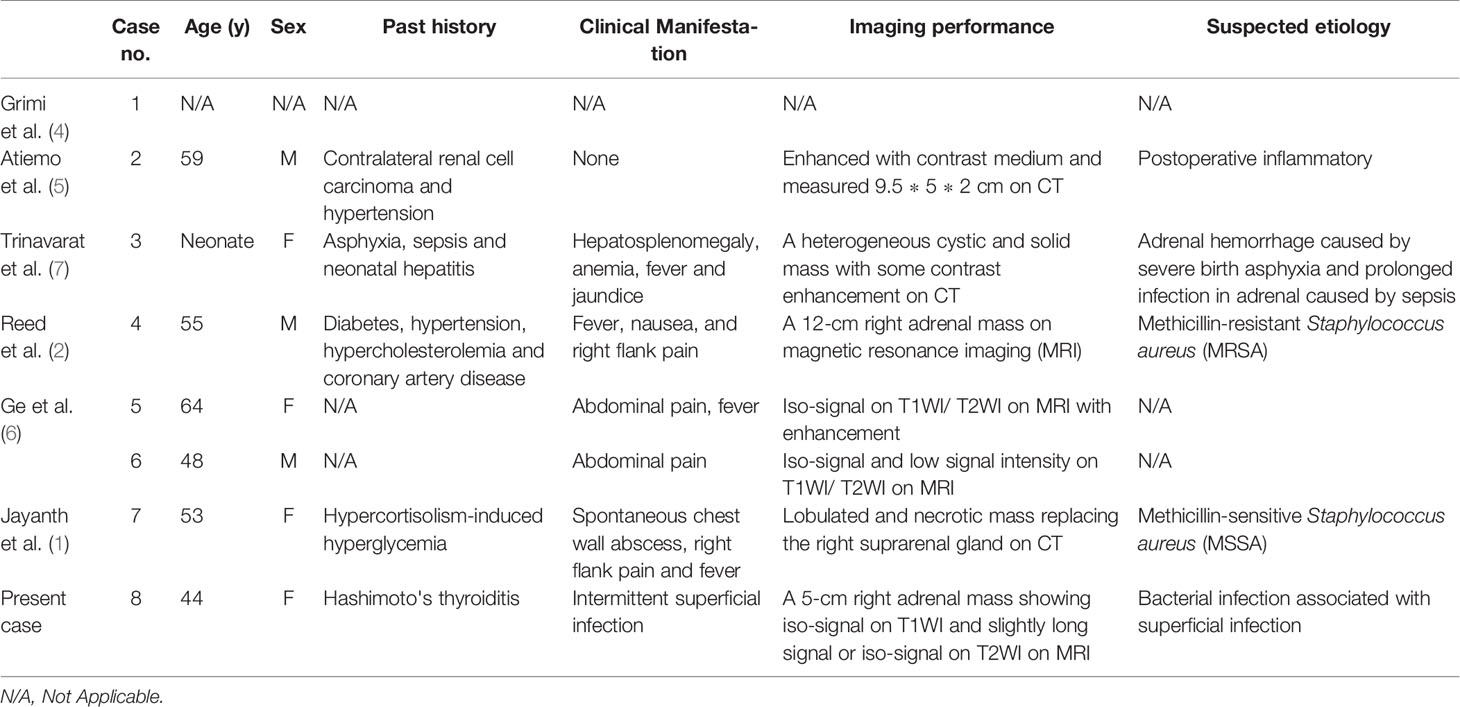
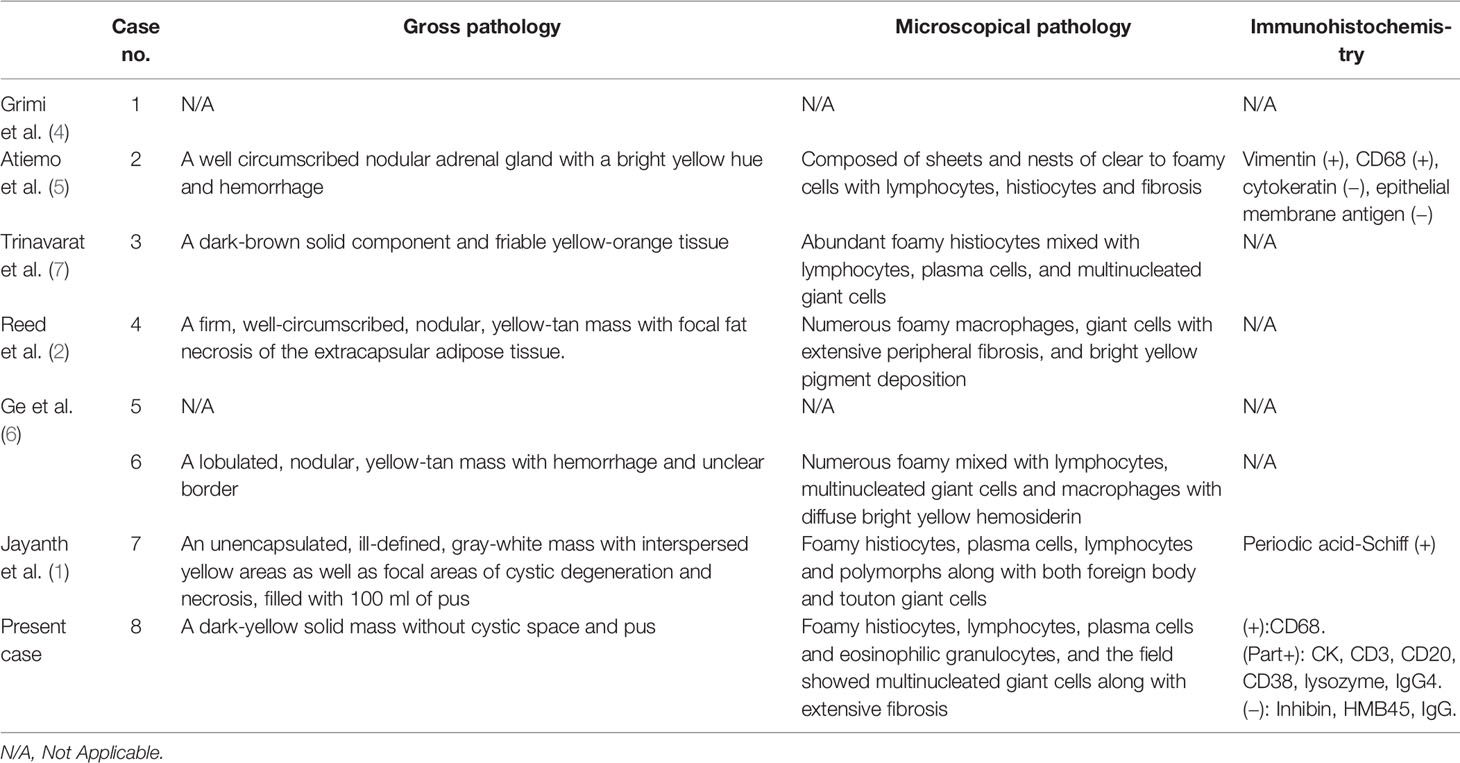
Xanthogranulomatous adrenalitis (XGA) is a rare inflammatory condition of the adrenal glands, probably resulting from a combination of chronic infection and local bleeding. Herein, we present an exceedingly rare case of functional xanthogranulomatous adrenalitis occurring in a 44-year-old Chinese female patient. With a history of intermittent superficial infection and a high level of C-reactive protein for 6 months, she presented to the hospital without fever or flank pain. Magnetic resonance imaging revealed a 5-cm right adrenal mass, which showed iso-signal on T1WI and a slightly long signal or iso-signal on T2WI. The preoperative basal serum renin level of the patient was decreased and the aldosterone-to-renin ratio was increased. After laparoscopic radical adrenalectomy, the adrenal mass was diagnosed as xanthogranulomatous adrenalitis, which was confirmed by histological examination and immunohistochemical staining for CD68. One month after surgery, the serum renin and aldosterone to renin ratio of the patient dropped to normal levels. Our case shows that xanthogranulomatous adrenalitis may resemble functional adrenal neoplasms, both biochemically and radiologically. The most likely cause of xanthogranulomatous adrenalitis is chronic infection, especially gram-positive coccus infection. Xanthogranulomatous adrenalitis should be considered when clinical and radiological manifestations are not typical for other inflammatory diseases or adrenal neoplasms.
Introduction
Xanthogranulomatous adrenalitis (XGA) is an extremely rare type of retroperitoneal xanthogranuloma that is histologically defined as chronic xanthogranulomatous inflammation. Fewer than 10 reports have been reported on XGA worldwide since 1987, when XGA was first described, and all of them were individual cases. The mechanism underlying its pathogenesis remains unknown. It has been reported that XGA often occurs in patients with an underlying condition, such as infection or hemorrhage. Some cases have evidence of bacterial infection, namely, methicillin-resistant Staphylococcus aureus (MRSA) and methicillin-sensitive S. aureus (MSSA) (1, 2), which are rare in xanthogranulomatous pyelonephritis. Uniquely, Jayanth et al. reported a case masquerading as a functioning adrenocortical malignancy with elevated cortisol levels (1). To the best of our knowledge, this is the first reported case of XGA associated with superficial infection and low renin levels which could resemble a functional adrenal neoplasm. In this report, we describe our clinical, radiological, and pathological observations and review the previous literature to decrease the risk of misdiagnosis and provide more clinical data for the diagnosis and treatment of XGA.
Case Presentation
A 44-year-old woman with a right adrenal mass noted during a routine ultrasound examination presented to the hospital without fever or flank pain. The patient had been diagnosed with Hashimoto’s thyroiditis 3 years prior and was currently on oral euthyroxine (levothyroxine sodium) maintenance therapy, without any other comorbidities. Six months earlier, the patient had intermittent superficial subcutaneous nodules 5-cm in diameter accompanied by mild tenderness, with local redness and swelling, which subsided spontaneously after 1 month. The subcutaneous lumps appeared in several areas without fever, namely, the forearms, abdomen, and back, so the patient ignored these conditions and did not seek medical help.
After admission, we found a subcutaneous lump on the back of the patient on physical examination, and the subsequent CT examination confirmed this. CT scan detected a subcutaneous soft tissue density nodule on the left dorsum. In preliminary investigations, her white blood cell count was normal at 5.8 × 109/L (normal range 4.0–10.0 × 109/L), but her C-reactive protein level was elevated at 30 mg/L (normal range <5 mg/L). Serum renin level was decreased at 0.5 uIU/ml in supine position (normal range 2.8–39.9 uIU/ml) and 0.8 uIU/ml in erect position (normal range 4.4–46.1 uIU/ml), and aldosterone to renin ratio (ARR) raised at 8.2 in supine position (normal range <3.7) and 6.25 in erect position (normal range <3.7). Other hematologic parameters, biochemical investigations, and blood pressure were within the normal limits. Magnetic resonance imaging (MRI) revealed a 5-cm right adrenal mass, which showed iso-signal on T1WI, slightly long signal or iso-signal on T2WI, and slightly high signal on DWI. The mass showed heterogeneous enhancement within some non-enhancing lesions on contrast-enhanced scan (Figure 1). A subcutaneous soft tissue mass on the right flank and multiple para-aortic lymph nodes were also detected. The patient underwent laparoscopic radical adrenalectomy; the cut surface of the mass was dark-yellow and solid, without cystic spaces or pus. Microscopically, the adrenal nodule was composed of foamy histiocytes, accompanied by dense aggregation of lymphocytes, plasma cells, eosinophilic granulocytes, and multinucleate giant cells along with extensive fibrosis (Figure 2). The normal architecture of the adrenal tissue was lost, with only a small remnant of normal adrenal tissue seen in the adjacent adipose tissue. The diagnosis of XGA was further supported immunohistochemical positivity for CD68, without any evidence of neoplasm. The follow-up duration was 9 months. The subcutaneous mass that had appeared preoperatively did not recur after surgery, and CT examination also did not reveal any mass in the surgical area or adjacent subcutaneous tissue. The serum renin and ARR levels of the patient dropped to normal levels 1 month after surgery and remained normal on follow-up.
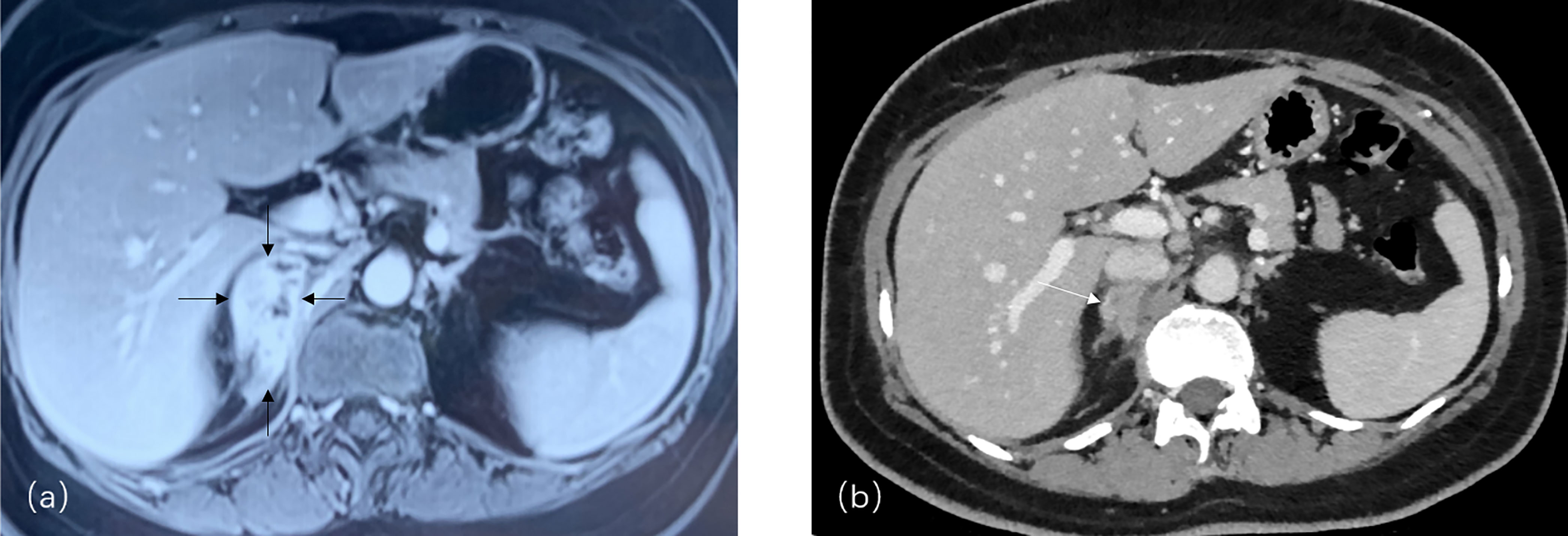
Figure 1 (A) A 5.2*4.3*2.0 cm right adrenal mass (arrows) showing heterogeneously enhancement within some non-enhancement lesions in contrast enhanced scan on MRI; (B) Adrenal mass with heterogeneously enhancement and multiple para-aortic lymph nodes on CT imaging (arrow).
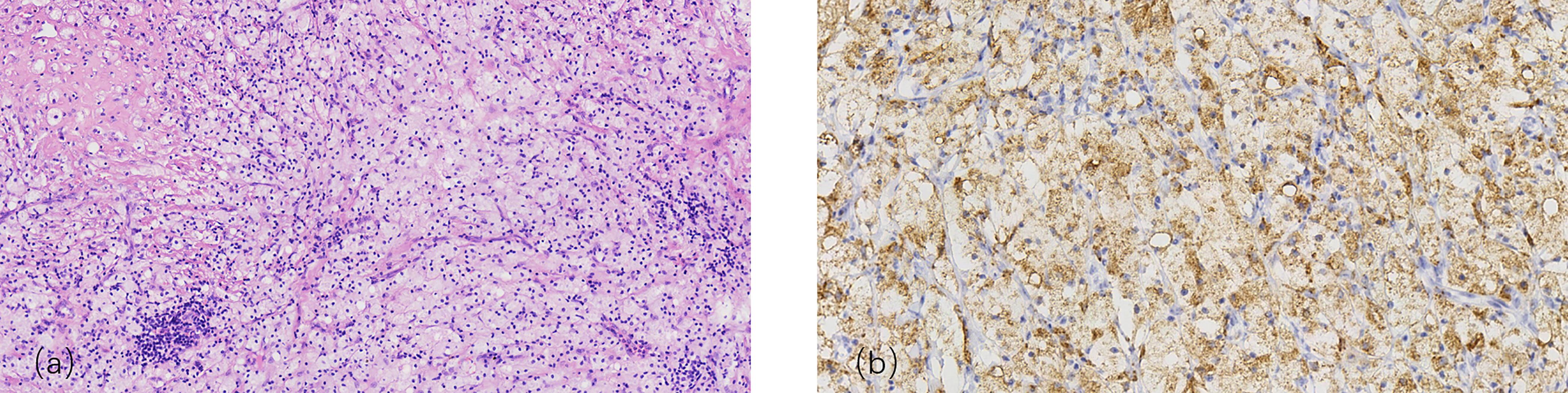
Figure 2 (A) Granulomas zone: composed of foamy cell, lymphocytes and normal adrenal parenchyma cell, H&E, reduced from ×200 (B) Immunohistochemical: CD68(+), H&E, reduced from x400.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Ethics Committee and with the Helsinki Declaration (revised in 2013). Written informed consent was obtained from all the patients. To date, the patient continues to visit the hospital for her long-term follow-up.
Discussion
Retroperitoneal xanthogranulomatous was first presented by Oberling in 1935 (3), and XGA, as an exceedingly rare type of xanthogranulomatous process, was first described in 1987 by Grimi (4) and considered as a new pathological entity in 2003 (5).
To review the known characteristics of XGA, we searched PubMed and Embase using the keywords “retroperitoneal xanthogranuloma”, “xanthogranulomatous adrenalitis”, and “functional adrenal mass”. A total of seven cases have been reported since 1987, namely, five cases in English literature and two cases in Chinese reports. Except for one case lacking detailed information, the remaining six cases included five cases of adults and one case of a neonate (three males and three females, mean age 46.5 years, range 0–64 years) (1, 2, 4–7). All patients underwent adrenalectomy and remained well on follow-up. The clinical and pathological features of the eight cases are summarized in Tables 1 and 2 (including the present case).
In all cases reported, chronic inflammation was considered the most likely inciting factor in this process. In both previous studies and our case, potential factors associated with infection and bleeding were present, such as postsurgical inflammation after radical nephrectomy for renal cell carcinoma (5), neonatal adrenalitis triggered by sepsis and adrenal hemorrhage (7), local infection and bleeding due to trauma (2), spontaneous abscess due to immunosuppression possibly caused by diabetes (1) and intermittent superficial infections lasting six months in our case. MRSA and MSSA were detected in the cyst fluid of the mass or on blood culture, which was different from those in XGP. The pathogens of XGP are the same as those of urinary tract infections, mainly gram-negative bacteria such as Escherichia coli, Proteus mirabilis, and Klebsiella (8). Based on the above clinical data, we speculate that the main pathogen of XGA is gram-positive cocci such as S. aureus and Staphylococcus epidermidis.
Whether the parenchymal portion of XGA has a secretory function or it induces abnormal secretion in normal adrenal tissue, is unknown. A recent case reported that the preoperative basal serum cortisol and 24-hour urinary cortisol of a male patient were elevated with a positive result of dexamethasone suppression test and uncontrollable hyperglycemia (1). Hormone levels dropped to the normal range after adrenalectomy. In our case, although the cortisol rhythm of the patient was normal, she had a decreased level of serum renin and elevated levels of ARR. One month after surgery, her serum renin and ARR levels were within normal limits and remained normal on follow-up 9 months after surgery. On pathological examination of these cases, there was no evidence of cortical adenoma or aldosterone adenoma. To our knowledge, based on an extensive search, there is no research on the mechanism between the change in adrenal hormone levels and adrenalitis, and our findings may reveal a potential relationship between XGA and adrenal secretory function.
Radiologically, XGA may be easily misdiagnosed for two reasons. Since the parenchyma of the mass is easily obscured by cysts formed by local hemorrhage, XGA is often misdiagnosed as an adrenal hematoma or cyst. Also, XGA often shows extensive local invasion on imaging, which makes it indistinguishable from malignant adrenal tumors. Based on previous cases and our case, we found that CT lacked specificity for the diagnosis of XGA. It may manifest as a slightly dense and poorly defined mass with or without enhancement, which makes it difficult to differentiate between inflammation and other types of tumours. One study revealed that the parenchyma of XGA showed iso-signal on T2WI on MRI, supported by our case where XGA showed iso-signal on T1WI and a slightly long signal or iso-signal on T2WI. In contrast to XGA, some adrenal neoplasms, such as pheochromocytoma or adrenal adenocarcinoma, show a high signal on T2WI. We believe that MRI can better differentiate XGA from other adrenal diseases.
The preoperative diagnosis of XGA is confusing for clinicians because it does not have any specific clinical or radiological characteristic to differentiate it from other benign adrenal diseases. Even in our case, the preoperative abnormal levels of serum renin and ARR suggested an adrenocortical adenoma, but normal aldosterone levels and CT images where the mass exhibited unclear borders contradicted this diagnosis. Typical endocrinological manifestations, namely, high blood pressure, hypokalemia, and Cushing syndrome, may help differentiate hyperaldosteronism secondary to adrenocortical adenoma or hyperplasia of the gland. To date, all definite diagnoses of XGA are based on postoperative pathological examinations. Pathological examination showed granulomas composed of foamy cells, lymphocytes, and normal adrenal parenchyma cells, which was consistent with the manifestations of granulomatous inflammation reported in previous literature. On immunohistochemical examination, CD68 positivity and negativity for tumour markers such as inhibin, calretinin, and Melan-A also contribute to the diagnosis of XGA.
In the preoperative evaluation of XGA, given that XGA resembles invasive adrenal tumor on imaging, unilateral adrenalectomy is consistent with the treatment principle, similar to unilateral nephrectomy for xanthogranulomatous pyelonephritis (XGP). A recent study exploring whether the use of preoperative antibiotics is related to the incidence of complications after nephrectomy for XGP showed that prolonged (greater than 28 days) preoperative antibiotics were associated with fewer and less severe postoperative complications (9). Similarly, for XGA, the application of preoperative antibiotics has a good effect on the treatment of infection-related symptoms such as fever, pain, and even sepsis, but there is no standard or guideline for the term and type of antibiotics. Further research is needed to determine whether preoperative or postoperative antibiotic use is associated with a reduced risk of postoperative complications and recurrence in the future, but given the rarity of XGA, it may be difficult to develop a standard treatment protocol.
Conclusion
XGA is an extremely rare adrenal disease indistinguishable from malignant adrenal neoplasms. In this case, we summarized the characteristics of XGA based on the published cases and our case and tried to differentiate it from other adrenal diseases. However, its pathogenesis and early diagnosis require further research.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Peking University People’s Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
XD and YZ made equivalent contributions to the article. XD, YZ and LY designed the research. XD, YD, SL, GW, LY and XZ conducted the research. XD and YZ wrote the paper. XD, LY and TX had primary responsibility for the final content. All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jayanth KS, Balamurugan S, Sureshkumar S, Anandhi A, Sree Rekha J, Abdulbasith KM, et al. Xanthogranulomatous Adrenalitis Masquerading as a Functioning Adrenocortical Malignancy: A Case Report. Tumori (2020) 106(6):030089162094965. doi: 10.1177/0300891620949656
2. Reed CT, Adams K, Shenoy V. Xanthogranulomatous Adrenalitis: A Case Report of a Diabetic, 55-Year-Old Male. J Endocr Pathol (2015) 26(3):229–31. doi: 10.1007/s12022-015-9377-4
3. Oberling C. Retroperitoneal Xanthogranuloma. Am J Cancer (1935) 23(3):477–89. doi: 10.1158/ajc.1935.477
4. Grimi M, Nanni G, Sarro G, Luchetti P, Dipierdomenico M, Garbini A, et al. Retroperitoneal Xanthogranuloma of the Adrenal Gland. Rep Case (1987) 87(6):387. doi: 10.3760/cma.j.issn.1000-6702.2015.09.024
5. Atiemo HO, Nonaka D, Silverberg SG, Glassman DT, Jacobs SC. Xanthogranulomatous Adrenalitis. J Urol (2003) 170(1):177–7. doi: 10.1097/01.ju.0000067240.28097.bd
6. Ge C, Ni J. Radiographic Features of Xanthogranulomatous Adrenalitis. Chin J Urol (2015) 36(9):713. doi: 10.3760/cma.j.issn.1000-6702.2015.09.024
7. Trinavarat P, Sasiwimonphan K, Sansopha L, Vejchapipat P, Sosothikul D. Xanthogranulomatous Adrenalitis in a Neonate: CT and US Findings. Pediatr Radiol (2009) 39(3):286–9. doi: 10.1007/s00247-008-1075-7
8. Li L, Parwani AV. Xanthogranulomatous Pyelonephritis. Arch Pathol Lab Med (2011) 135(5):671–4. doi: 10.5858/2009-0769-RSR.1
Keywords: Xanthogranulomatous adrenalitis, functional adrenal neoplasm, superficial infection, case report, laparoscopic radical adrenalectomy
Citation: Dai X, Zhang Y, Du Y, Lai S, Wang G, Yu L, Zhang X and Xu T (2022) Xanthogranulomatous Adrenalitis: A Case Report and Literature Review. Front. Urol. 2:841002. doi: 10.3389/fruro.2022.841002
Received: 21 December 2021; Accepted: 02 February 2022;
Published: 25 February 2022.
Edited by:
Derek Hennessey, Mercy University Hospital, IrelandReviewed by:
Nikita Bhatt, Cambridge University Hospitals, United KingdomDonnacha Hogan, Mercy University Hospital, Ireland
Copyright © 2022 Dai, Zhang, Du, Lai, Wang, Yu, Zhang and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luping Yu, WUxQMDgyN0Bob3RtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Xiang Dai
Xiang Dai Yuanyuan Zhang2†
Yuanyuan Zhang2† Tao Xu
Tao Xu