
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Urol. , 19 January 2023
Sec. Pediatric, Adolescent and Developmental Urology
Volume 2 - 2022 | https://doi.org/10.3389/fruro.2022.1092192
This article is part of the Research Topic Women in Pediatric, Adolescent, and Developmental Urology: Volume I View all 11 articles
Introduction: Epididymitis, orchitis, and epididymo-orchitis (EO) are common disorders in pediatric patients which may be caused by infection, trauma, or inflammation. SARS-CoV-2 associated EO has been previously described, particularly in adults. However, no systematic reviews of these manifestations in pediatric patients yet exist. We present a systematic literature review of epididymitis, orchitis, and EO associated with SARS-CoV-2 in pediatric patients to shed light on these relatively rare, yet potentially severe, conditions to understand presentation, course of illness, management options, and outcomes.
Materials and Methods: Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, a systematic review was performed using specified key terms to search PubMed, Cumulative Index to Nursing and Allied Health Literature, Web of Science, and Embase. Articles were independently screened by two reviewers. Manuscripts with detailed descriptions of SARS-CoV-2 associated epididymitis, orchitis, or EO in pediatric patients were included. Exclusion criteria included: no clear diagnosis of the target diseases and no detailed clinical course described. Quality and bias were assessed using the Joanna Briggs Institute Critical Appraisal Checklist for Case Reports.
Results: 60 records were initially identified, with 6 case reports included in the systematic review. All 6 patients included presented with fever and genitourinary symptoms. Four patients were also diagnosed with multisystem inflammatory syndrome in children (MIS-C). One patient underwent surgical exploration for presumed testicular torsion, though intraoperatively there was no evidence of torsion. All patients recovered without documented long-term sequelae.
Discussion: While observational studies are prone to bias, this systematic review suggests that epididymitis, orchitis, and EO are significant manifestations of SARS-CoV-2 that may mimic urologic emergencies (i.e., testicular torsion). Providers should suspect these conditions in pediatric COVID-19 patients with scrotal symptoms, particularly with associated MIS-C. The long-term genitourinary sequelae of SARS-CoV-2 should be investigated, including the effects on pediatric patients undergoing reproductive development.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for the Coronavirus Disease 2019 (COVID-19) pandemic, is associated with a wide variety of pathologic manifestations across multiple organ systems (1–4). Although it is most known for its pulmonary involvement with potential for severe pneumonia and acute respiratory distress syndrome, SARS-CoV-2 also commonly affects the gastrointestinal and cardiovascular systems and can cause widespread systemic inflammatory conditions (1–4). In pediatric patients, these systemic conditions include a Kawasaki Disease-like syndrome with characteristic cutaneous involvement (5, 6). This condition was eventually termed multisystem inflammatory syndrome in children (MIS-C) (5, 6). Several mechanisms for these inflammatory syndromes have been presented including widespread microvascular damage and thrombosis, increased inflammatory mediators (angiotensin II), and extensive immune cell activation (4, 6).
COVID-19 is associated with a variety of urologic manifestations in adult patients. The most common urologic complication of COVID-19 is acute kidney injury with a prevalence of 7.58%, while other less common genitourinary sequelae in adults include ischemic priapism, lower urinary tract dysfunction, and epididymo-orchitis (EO) (7–9). However, the current literature is lacking with respect to the viruses’ urologic effect in pediatric COVID-19 patients. Recently published case reports of ischemic priapism in a 12-year-old boy and torsion of appendix testis in an 8-year-old boy provide some insight into the genitourinary manifestations of SARS-CoV-2 (10, 11). Additionally, there have been some reports of EO associated with SARS-CoV-2 in pediatric patients. However, no systematic reviews of the genitourinary manifestations of SARS-CoV-2 within the pediatric patient, specifically EO, currently exist.
Epididymitis is defined as inflammation of the epididymis, orchitis is defined as inflammation of the testis, and EO is defined as the presence of both epididymitis and orchitis (12–14). These conditions most commonly present with scrotal pain, redness, and swelling, and ultrasound findings characteristically include enlargement of the testis and/or epididymis, thickening of the tunica albuginea, and increased flow on Doppler ultrasound (12–15). The incidence of EO has been estimated at 1.2 out of 1,000 annually in boys aged 2-14 years old, while a recent review of retrospective studies on epididymitis and EO indicated a mean incidence of 37.3% in pediatric patients presenting with an acute scrotum (16, 17). EO may be caused by a variety of etiologies, including infection (Chlamydia trachomatis, Neisseria gonorrhea, tuberculosis, mumps), medications (amiodarone), and systemic inflammatory conditions such as Kawasaki Disease, Henoch-Schoenlein Purpura, and, most recently, SARS-CoV-2 related MIS-C (12–14, 18, 19). In addition to acute and systemic inflammation, SARS-CoV-2 may also directly infect cells of the testis via its functional receptor angiotensin converting enzyme 2 (ACE2) (20). ACE2 is also expressed in testicular tissue, suggesting a potential novel pathophysiologic mechanism of EO (20).
Given that SARS-CoV-2 may directly infect the genitourinary tract and may cause systemic inflammation, particularly within the pediatric population, epididymitis, orchitis, and EO are uncommon but significant manifestations in pediatric patients. Herein, we present a systematic review of the known pediatric cases of epididymitis, orchitis, and EO associated with COVID-19. Our objective is to investigate the clinical presentations of cases, including initial signs and symptoms, subsequent management, and outcomes in pediatric patients with concurrent COVID-19 infection and epididymitis, orchitis, and EO.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were utilized to systematically query databases from inception through April 2022. Databases searched were PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Web of Science, and Embase, to access cases of epididymitis, orchitis, and EO associated with COVID-19 (21). Key terms utilized for PubMed, CINAHL, Web of Science, and Embase were “((epididymitis) OR (orchitis) OR (Orchiepididymitis) OR (epididymorchitis) OR (epidiymo*)) AND ((covid*) OR (coronavirus) OR (SARS-CoV-2)) AND ((pediatric*) OR (paediatric*) OR (child*) OR (adolesc*))”. No additional filters or restrictions were utilized for any of the databases. Additional references deemed relevant to our systematic review were obtained through cross-references. For a more detailed description of our search strategies, please see Supplementary Table 1 which details our search criteria for each database, as well as our protocol in the supplementary files.
For this systematic review, inclusion criteria consisted of articles that provided a detailed description of epididymitis, orchitis, or EO associated with COVID-19 in pediatric patients aged 18 years and under. The target outcomes and data collected for comparison are detailed in Table 1 and include the presenting symptoms, examination findings, diagnostic results, therapeutic management, and clinical outcomes. Manuscripts were excluded if: a) there was no clear diagnosis epididymitis, orchitis, or EO, b) there was no association with COVID-19, c) the relevant patients were greater than 18 years old, or d) the study in question did not contain a detailed description of the patient’s clinical course including initial presentation, management, and clinical outcome.
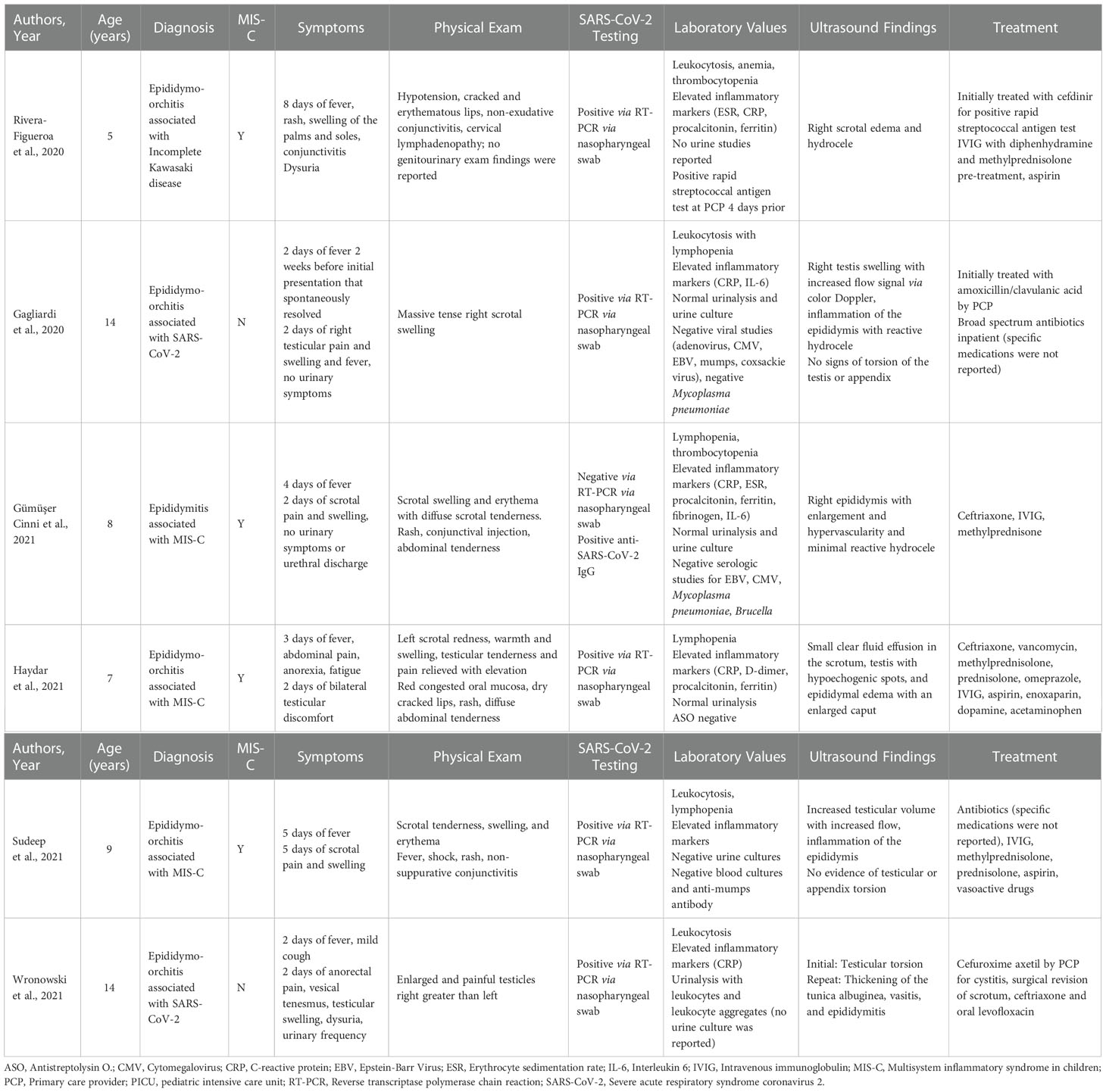
Table 1 Included cases of epididymitis, orchitis, and epididymo-orchitis associated with COVID-19 in pediatric patients.
The included studies were assessed for quality and bias utilizing the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Case Reports (22). Missing data was recorded as “not reported” and excluded from the syntheses when appropriate. Two authors independently completed the systematic review to determine article eligibility, collect data, and perform initial qualitative synthesis. Any discrepancies between the two reviewers were discussed among the study team to reach a consensus. While this study was not registered through PROSPERO as data collection began prior to registration, a protocol detailing the methodology of this systematic review was created and is available in the supplementary files.
Our initial query using the previously described search criteria produced 60 results (Figure 1). After 21 duplicates were removed, the remaining 39 results were screened based on title and abstract for the inclusion criteria, resulting in 7 manuscripts appropriate for full text review. An additional 4 manuscripts were found based on cross-referencing, resulting in a total of 11 manuscripts for full text review. Of the 11 reviewed, 5 articles were excluded resulting in 6 case reports for subsequent synthesis (Table 1) (23–28). Two manuscripts were excluded due to no clear diagnosis in a case series, and 3 manuscripts were excluded as they described retrospective cohorts without detailed clinical courses (5, 19, 29–31).
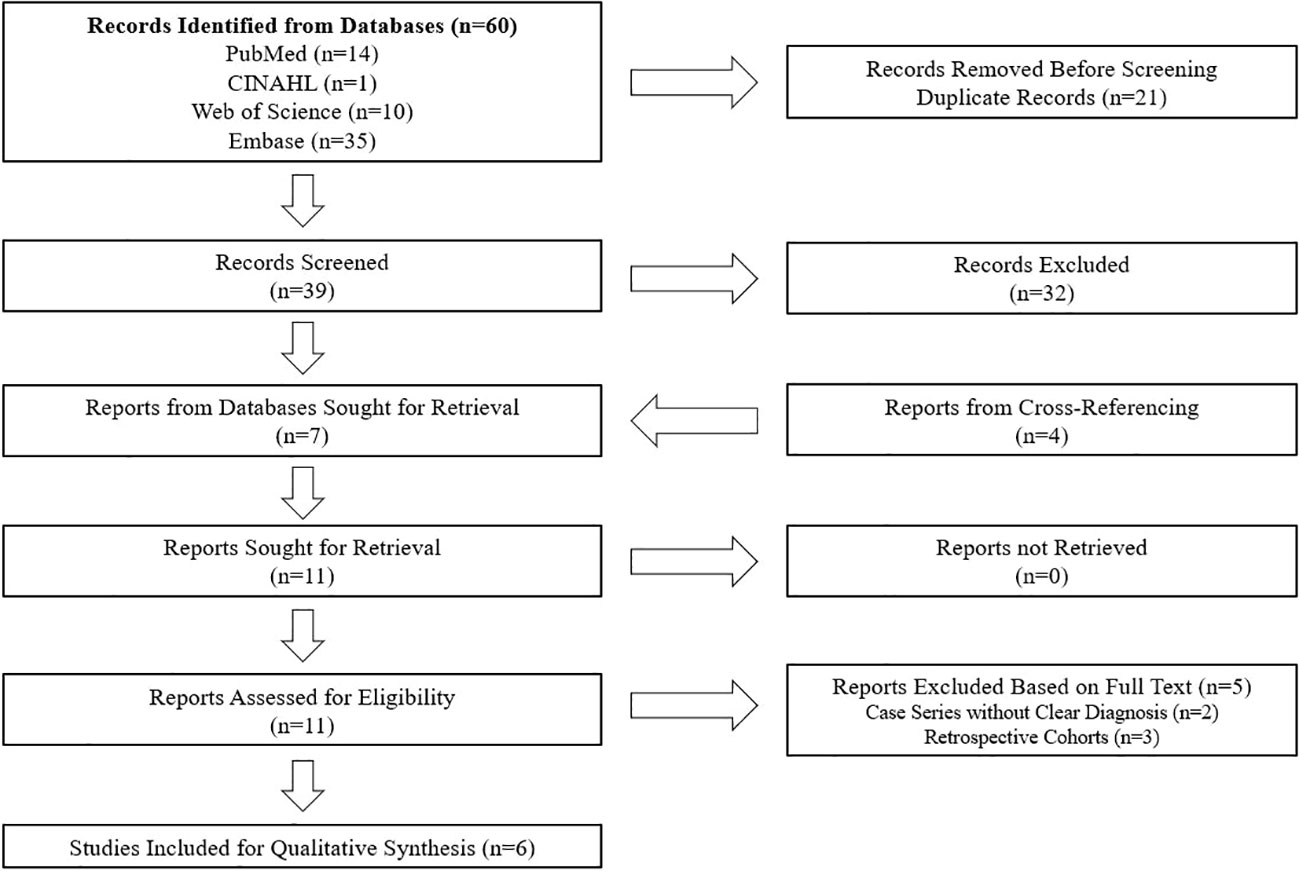
Figure 1 PRISMA flowchart for systematic review process. CINAHL, Cumulative Index to Nursing and Allied Health Literature.
The 6 case reports included in this systematic literature review described a total of 6 male patients with a mean age of 9.5 years (range 5-14). All 6 reports fulfilled all 8 items of the JBI Critical Appraisal Checklist for Case Reports. Table 1 describes the clinical characteristics of the 6 patients included in this systematic review. All 6 patients had fever and genitourinary symptoms on initial presentation, while 5 patients had documented testicular or scrotal swelling subjectively. Onset of any symptom of SARS-CoV-2 to presentation was on average 4 days (range 2-8), while onset of genitourinary symptoms to presentation was on average 3.5 days (range 2-8) (Table 2). One patient experienced possible prodromal symptoms with 2 days of high fever that spontaneously resolved 2 weeks prior to admission. One patient was diagnosed with acute epididymitis and 5 patients were diagnosed with EO. Physical exam findings commonly included scrotal swelling, erythema, and tenderness. All patients were admitted to the hospital for their conditions.
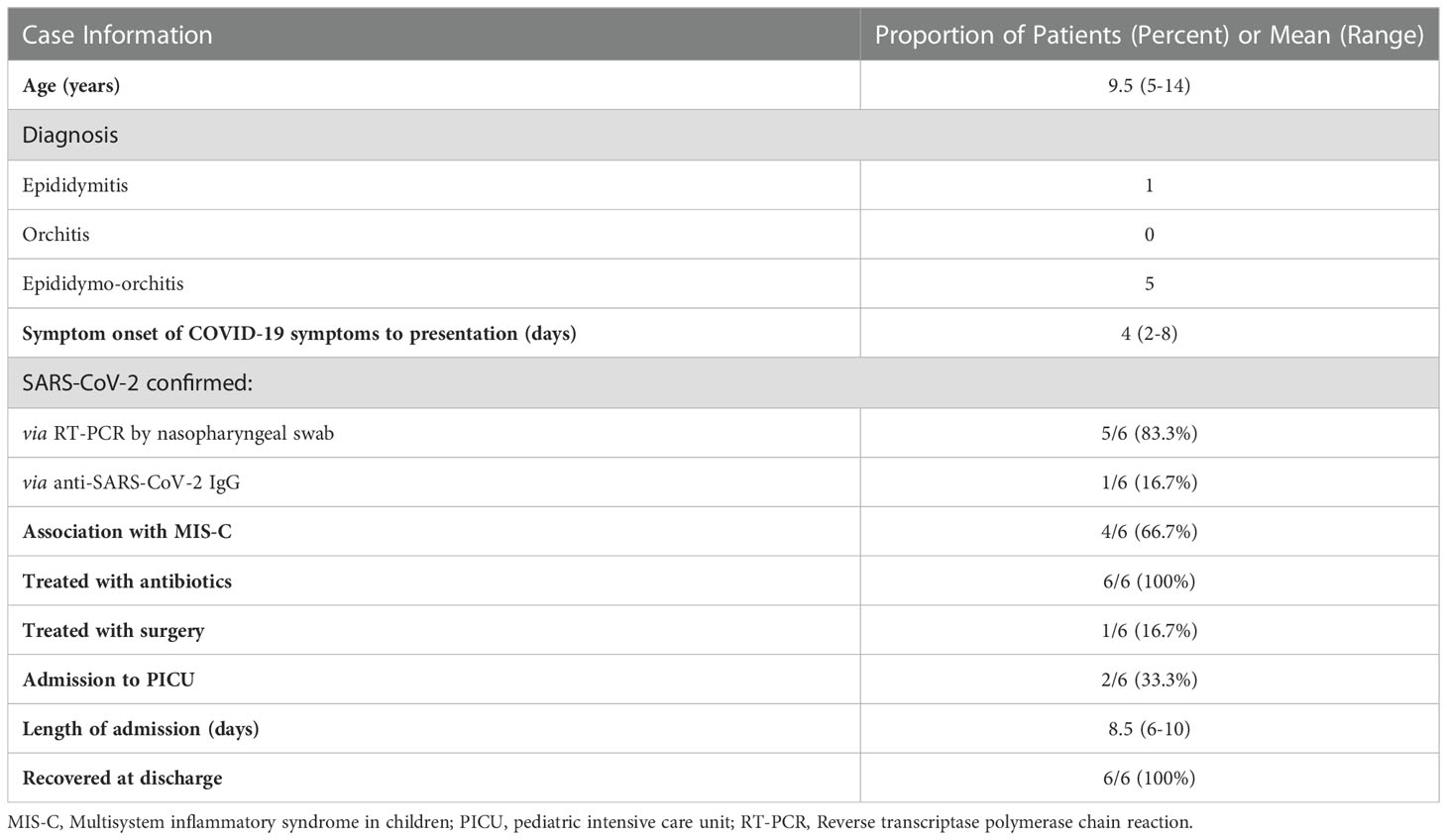
Table 2 Clinical features of epididymitis, orchitis, and epididymo-orchitis associated with COVID-19 in pediatric patients.
Five patients had confirmed COVID-19 via nasopharyngeal reverse transcription polymerase chain reaction (RT-PCR). 1 patient was negative for SARS-CoV-2 on nasopharyngeal RT-PCR though had a positive anti-SARS-CoV-2 IgG with a confirmed positive sick-contact (Table 2). Four of the 6 cases were associated with MIS-C. All 6 patients had documented hematologic derangements, including either leukocytosis, lymphopenia, or lymphopenic leukocytosis. Additionally, all 6 patients had elevated inflammatory markers, most commonly C-reactive protein and erythrocyte sedimentation rate, though procalcitonin, ferritin, and D-dimer were also elevated in some patients. Of the 5 cases with documented urine studies (urinalysis or urine culture), only 1 urinalysis was positive for leukocytes and leukocyte aggregates in a patient experiencing dysuria and urinary frequency; no urine culture results were reported for this patient and SARS-CoV-2 RT-PCR of his urine was negative. Five out of 6 patients had additional infectious studies documented including viral serologies (Epstein-Barr Virus, Cytomegalovirus, Mycoplasma pneumoniae), antistreptolysine O, and blood cultures. Other than one patient with a positive outpatient rapid streptococcal antigen test, all other infectious studies were negative. For all 6 patients, no sexually transmitted infection testing was reported (i.e., Chlamydia trachomatis, Neisseria gonorrhoeae), and there were no comments documented on the patients’ sexual activity. Scrotal ultrasounds were performed on all 6 patients to support the diagnoses, with common findings including increased testicular volume, hypervascularity, and reactive hydrocele. Interestingly, 1 patient had an initial ultrasound which revealed “testicular torsion” prompting surgical intervention, though during scrotal exploration, no torsion was found (28). The initial ultrasound findings to suggest torsion were not described in the case report, and repeat ultrasound showed findings more consistent with EO with thickening of the tunica albuginea and vasitis.
Treatment for all cases of epididymitis, orchitis, and EO included antibiotics most commonly with a third-generation cephalosporin (cefdinir, ceftriaxone), though other antibiotics utilized include cefdinir, vancomycin, and levofloxacin (Table 1). Two patients were treated prior to admission with antibiotics prescribed by their primary care physicians (cefuroxime and amoxicillin/clavulanic acid). All cases associated with MIS-C were treated with intravenous immunoglobulin (IVIG) and methylprednisolone, though other medications included aspirin, proton pump inhibitors (omeprazole), vasoactive medications (dopamine), and anti-coagulants (enoxaparin, heparin). All patients were hospitalized with a mean hospital stay of 7.5 days (range 3-10). 2 patients reportedly required admission to the pediatric intensive care unit (PICU) for hemodynamic instability, and all patients eventually recovered from their illness with no mortalities. Only 2 cases indicated any follow-up after admission, with Gagliardi et al. describing “progression to normality” at 8 days after discharge and Sudeep et al. reporting their patient was asymptomatic at 1 month follow-up.
To our knowledge, this is the first systematic review to critically evaluate the published cases of epididymitis, orchitis, and EO associated with COVID-19 in pediatric patients. Along with the 6 cases described in this systematic review, our literature search also resulted in 1 case of epididymitis, 2 cases of orchitis, and 1 case of EO documented across three retrospective cohorts of pediatric patients with COVID-19, though these cases were excluded in the present systematic review due to lack of detailed information regarding symptomatology, management, and outcomes (5, 30, 31). Although relatively few cases have been reported since the beginning of the COVID-19 pandemic, the cases included in this systematic review were severe and associated with complex COVID-19, each requiring at least 6 days of admission. Additionally, given the nature of case reports which typically describe the most severe cases, there may be many children who experience relatively mild symptoms at home without contacting their health care providers. All patients survived and were discharged in significantly improved conditions.
The majority of the cases included in our systematic review were associated with MIS-C. Additionally, all 4 of the previously mentioned cases excluded (due to insufficient data) were associated with MIS-C (5, 30, 31). Furthermore, we also reviewed 2 pediatric case series in MIS-C patients which described 2 patients with signs and symptoms of epididymitis, orchitis, and EO. This included scrotal pain in one patient and signs of hyperemia of the testes and epididymes in the other patient (19, 29). In consideration of these factors, male patients with MIS-C should be carefully monitored for genitourinary symptoms. Epididymitis, orchitis, and EO should be considered as possible diagnoses in COVID-19 patients with urinary or scrotal symptoms.
Epididymitis, orchitis, and EO in pediatric patients are relatively common conditions potentially caused by infection, reflux or stasis of urine, trauma, or systemic inflammatory conditions. SARS-CoV-2 may be another causative virus due to a combination of cellular susceptibility to infection and systemic inflammation. Similar to its predecessor SARS-CoV-1, SARS-CoV-2 uses ACE2 as its functional receptor and transmembrane serine protease 2 (TMPRSS2) for priming its spike protein (32, 33). In human tissues, ACE2 is highly expressed in the lungs, oral and nasal mucosae, and within the gastrointestinal tract, suggesting potential sites of initial infection and routes of transmission (32, 33). Furthermore, the distribution of ACE2 and TMPRSS2 expression correlates with common sequelae of COVID-19, including within the respiratory system (cough, rhinorrhea, pneumonia) and gastrointestinal system (vomiting, diarrhea) (32). ACE2 and TMPRSS2 have been shown to be expressed within the testis including in Sertoli cells, Leydig cells, and spermatogonia, suggesting potential susceptibility of these cells to direct COVID-19 (20, 34).
Along with the biomolecular susceptibility of the male reproductive system, several objective laboratory and radiologic findings are associated with COVID-19. In a cohort of adult male patients with confirmed COVID-19 at single center in Wuhan, China, 32/142 (22.5%) met ultrasonographic diagnostic criteria of epididymitis, orchitis, or EO (15). Autopsy studies of patients infected with SARS-CoV-2 showed findings consistent with interstitial orchitis as well evidence of germ cell infection with scarcity of Sertoli and Leydig cells and decreased spermatogenesis (35, 36). Several studies have found hormonal derangements in patients infected with SARS-CoV-2, with increasing severity of infection associated with increasing magnitude of hormonal change (37, 38). Furthermore, certain etiologies of epididymitis, orchitis, and EO are associated with chronic and irreversible sequelae including infertility due to germ cell destruction and damage to the seminiferous tubules including mumps and chronic C. trachomatis and N. gonorrhoeae (12, 14, 39). While SARS-CoV-2 is not known to cause irreversible infertility, it has demonstrated an ability to alter sperm analyses with effects on sperm motility and sperm count (40). In light of this, within the pediatric population, the potential for COVID-19 to adversely affect sexual development and puberty should be considered, and future investigations assessing long-term outcomes in this developing population are warranted.
Along with the previously published cases of ischemic priapism and torsion of the appendix testis, SARS-CoV-2 may present with multiple acute genitourinary symptoms and may even mimic acute urologic emergencies, as exemplified by the case in this systematic review who underwent surgical exploration for suspected testicular torsion. Providers should be cognizant of the urologic manifestations of SARS-CoV-2 in pediatric patients and have a high suspicion for epididymitis, orchitis, or EO in pediatric SARS-CoV-2 patients with genitourinary symptoms, particularly in the setting of MIS-C. Future investigations should be directed towards exploring the long-term sequelae of COVID-19 within the genitourinary tract, including the potential effects on male fertility. Furthermore, consideration of these factors may be taken when counseling pediatric patients and their families regarding immunization against SARS-CoV-2.
Limitations of this study include the descriptive observational nature of case reports and case series which are, by nature, prone to biases. Furthermore, as previously described, case reports and case series often display the most severe clinical courses seen at academic centers, and it is possible that more benign cases of epididymitis, orchitis, and EO are occurring in the general population without medical evaluation. This systematic review also includes a relatively small number of included articles which may limit the generalizability. However, the complications investigated in this study are relatively rare and the long-term effects of COVID-19 on sexual development in pediatric patients still need to be elucidated; therefore, this systematic review of the published cases is warranted to assemble and synthesize the limited data regarding this clinically significant manifestation. Our systematic review was also not registered through PROSPERO as data collection had begun prior to registration, though we followed the guidelines to the best of our ability and have uploaded our PRISMA checklist and protocol in the supplementary files.
SARS-CoV-2 may increase the risk of epididymitis, orchitis, and EO due to its capacity to cause systemic inflammation as well as the biomolecular mechanisms involving ACE2 and TMPRSS2. In pediatric patients with COVID-19 who are experiencing genitourinary symptoms, clinicians should have a high suspicion for epididymitis, orchitis, and EO, especially in those with concurrent MIS-C. Further research regarding the urologic sequelae of SARS-CoV-2 is warranted, particularly with respect to the long-term reproductive health of infected pediatric patients who are undergoing reproductive development.
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
All authors conceptualized the study design. DI and ZB conducted the review with oversight from EV and AP. DI was primarily responsible for writing the manuscript, with additional input from ZB and AP and revisions from EV. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fruro.2022.1092192/full#supplementary-material
1. Yazdanpanah F, Hamblin MR, Rezaei N. The immune system and COVID-19: Friend or foe? Life Sci (2020) 256:117900. doi: 10.1016/j.lfs.2020.117900
2. Patel KP, Patel PA, Vunnam RR, Hewlett AT, Jain R, Jing R, et al. Gastrointestinal, hepatobiliary, and pancreatic manifestations of COVID-19. J Clin Virol (2020) 128:104386. doi: 10.1016/j.jcv.2020.104386
3. Azevedo RB, Botelho BG, de Hollanda JVG, Ferreira LVL, de Junqueira Andrade LZ, Oei SSML, et al. Covid-19 and the cardiovascular system: A comprehensive review. J Hum Hypertens (2021) 35:4–11. doi: 10.1038/s41371-020-0387-4
4. Sakir A, Olena Z, Armen Yuri G. COVID-19 and the clinical course of rheumatic manifestations. Clin Rheumatol (2021) 40:2611–9. doi: 10.1007/s10067-021-05691-x
5. Pouletty M, Borocco C, Ouldali N, Caseris M, Basmaci R, Lachaume N, et al. Paediatric multisystem inflammatory syndrome temporally associated with SARS-CoV-2 mimicking Kawasaki disease (Kawa-COVID-19): A multicentre cohort. Ann Rheum Dis (2020) 79:999–1006. doi: 10.1136/annrheumdis-2020-217960
6. Kabeerdoss J, Pilania RK, Karkhele R, Kumar TS, Danda D, Singh S. Severe COVID-19, multisystem inflammatory syndrome in children, and Kawasaki disease: immunological mechanisms, clinical manifestations and management. Rheumatol Int (2021) 41:19–32. doi: 10.1007/s00296-020-04749-4
7. Chan VW-S, Chiu PK-F, Yee C-H, Yuan Y, Ng C-F, Teoh JY-C. A systematic review on COVID-19: Urological manifestations, viral RNA detection and special considerations in urological conditions. World J Urol (2021) 39:3127–38. doi: 10.1007/s00345-020-03246-4
8. Alsaedi SM, Alsarwani RM, Ali AI, Aladhrai SA. Ischemic priapism progressing to penile gangrene in a patient with COVID-19 infection: A case report with literature review. Case Rep Med (2022) 2022:8408216. doi: 10.1155/2022/8408216
9. Creta M, Sagnelli C, Celentano G, Napolitano L, La Rocca R, Capece M, et al. SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review. J Med Virol (2021) 93:3133–42. doi: 10.1002/jmv.26883
10. Brönimann S, Thalhammer F, Springer A, Tonnhofer U, Shariat SF, D’Andrea D. Ischemic priapism in a 12 year old patient associated with coronavirus disease 2019 (COVID-19): A case report. Urology (2022) 165:316–8. doi: 10.1016/j.urology.2022.01.022
11. Hamzavi SS, Derakhshan D, Askari A, Haghshenas H, Hajiani Ghotbabadi S. Torsion of the appendix testis as a presenting feature of multisystemic inflammatory syndrome in children. Pediatr Infect Dis J (2021) 40:e526–7. doi: 10.1097/INF.0000000000003283
12. Banyra O, Shulyak A. Acute epididymo-orchitis: Staging and treatment. Cent Eur J Urol (2012) 65:139–43. doi: 10.5173/ceju.2012.03.art8
13. Street EJ, Justice ED, Kopa Z, Portman MD, Ross JD, Skerlev M, et al. The 2016 European guideline on the management of epididymo-orchitis. Int J STD AIDS (2017) 28:744–9. doi: 10.1177/0956462417699356
15. Chen L, Huang X, Yi Z, Deng Q, Jiang N, Feng C, et al. Ultrasound imaging findings of acute testicular infection in patients with coronavirus disease 2019. J Ultrasound Med (2021) 40:1787–94. doi: 10.1002/jum.15558
16. Somekh E, Gorenstein A, Serour F. Acute epididymitis in boys: Evidence of a post-infectious etiology. J Urol (2004) 171:391–4. doi: 10.1097/01.ju.0000102160.55494.1f
17. Cristoforo TA. Evaluating the necessity of antibiotics in the treatment of acute epididymitis in pediatric patients: A literature review of retrospective studies and data analysis. Pediatr Emergency Care (2017) 37:1675–80. doi: 10.1097/PEC.0000000000001018
18. Dalpiaz A, Schwamb R, Miao Y, Gonka J, Walzter W, Khan SA. Urological manifestations of henoch-schonlein purpura: A review. Curr Urol (2015) 8:66–73. doi: 10.1159/000365692
19. Kurz H, Gombala T. Multisystem inflammatory syndrome in children (MIS-C)–a case series in December 2020 in Vienna, Austria. Front Pediatr (2021) 9:656768. doi: 10.3389/fped.2021.656768
20. Wang Z, Xu X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, leydig and sertoli cells. Cells (2020) 9:920. doi: 10.3390/cells9040920
21. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ (2021) 372:n71. doi: 10.1136/bmj.n71
22. Moola S, Munn Z, Tufanaru C, Aromataris EK, Sfetcu R, Currie M, et al. Chapter 7: Systematic reviews of etiology and risk. In: Joanna Briggs Institute reviewer’s manual. The Joanna Briggs Institute (2017). Available at: https://jbi-global-wiki.refined.site/space/MANUAL/4687372/Chapter+7%3A+Systematic+reviews+of+etiology+and+risk
23. Rivera-Figueroa EI, Santos R, Simpson S, Garg P. Incomplete Kawasaki disease in a child with COVID-19. Indian Pediatr (2020) 57:680–1. doi: 10.1007/s13312-020-1900-0
24. Gagliardi L, Bertacca C, Centenari C, Merusi I, Parolo E, Ragazzo V, et al. Orchiepididymitis in a boy with COVID-19. Pediatr Infect Dis J (2020) 39:e200–2. doi: 10.1097/INF.0000000000002769
25. Gümüşer Cinni R, Polat M, Seyrek H, Kaynak Şahap S, Öz FN, Tanır G. Acute epididymitis associated with multisystem inflammatory syndrome in children. J Paediatrics Child Health (2021) 57:594–5. doi: 10.1111/jpc.15441
26. Haydar M, Baghdadi S, Taleb M, Al-Dali B, Badr H, Ghanem Y. Orchiepididymitis in the context of multisystem inflammatory syndrome in a child with covid-19 from Syria: A very rare presentation for SARS-Cov-19 in children. Oxf Med Case Rep (2021) 2021:omab052. doi: 10.1093/omcr/omab052
27. Sudeep KC, Muthuvel R, Hussain N, Awasthi P, Angurana SK, Bansal A. Epididymo-orchitis: A rare manifestation of MIS-c. Indian J Pediatr (2022) 89:209. doi: 10.1007/s12098-021-03996-y
28. Wronowski M, Wozniak W, Wanke-Rytt M, Jazdzewski K, Kuchar E, Kloc M, et al. Orchiepididymitis in a 14-year-old boy with concurrent SARS-CoV-2 infection. South Afr J Child Health (2021) 15:227–8. doi: 10.7196/SAJCH.2021.v15i4.1869
29. Riollano-Cruz M, Akkoyun E, Briceno-Brito E, Kowalsky S, Reed J, Posada R, et al. Multisystem inflammatory syndrome in children related to COVID-19: A new York city experience. J Med Virol (2021) 93:424–33. doi: 10.1002/jmv.26224
30. Alkan G, Sert A, Oz SKT, Emiroglu M, Yılmaz R. Clinical features and outcome of MIS-c patients: An experience from central Anatolia. Clin Rheumatol (2021) 40:4179–89. doi: 10.1007/s10067-021-05754-z
31. Ucan B, Kaynak Sahap S, Cinar HG, Tasci Yildiz Y, Uner C, Polat M, et al. Multisystem inflammatory syndrome in children associated with SARS-CoV-2: extracardiac radiological findings. Br J Radiol (2022) 95:20210570. doi: 10.1259/bjr.20210570
32. Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell (2020) 181:271–280.e8. doi: 10.1016/j.cell.2020.02.052
33. Hamming I, Timens W, Bulthuis M, Lely A, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. a first step in understanding SARS pathogenesis. J Pathol (2004) 203:631–7. doi: 10.1002/path.1570
34. Fan C, Lu W, Li K, Ding Y, Wang J. ACE2 expression in kidney and testis may cause kidney and testis infection in COVID-19 patients. Front Med (2021) 7. doi: 10.3389/fmed.2020.563893
35. Duarte-Neto AN, Teixeira TA, Caldini EG, Kanamura CT, Gomes-Gouvêa MS, dos Santos ABG, et al. Testicular pathology in fatal COVID-19: A descriptive autopsy study. Andrology (2021) 10:13–23. doi: 10.1111/andr.13073
36. Ma X, Guan C, Chen R, Wang Y, Feng S, Wang R, et al. Pathological and molecular examinations of postmortem testis biopsies reveal SARS-CoV-2 infection in the testis and spermatogenesis damage in COVID-19 patients. Cell Mol Immunol (2021) 18:487–9. doi: 10.1038/s41423-020-00604-5
37. Salciccia S, Del Giudice F, Gentile V, Mastroianni CM, Pasculli P, Di Lascio G, et al. Interplay between male testosterone levels and the risk for subsequent invasive respiratory assistance among COVID-19 patients at hospital admission. Endocrine (2020) 70:206–10. doi: 10.1007/s12020-020-02515-x
38. Tian Y, Zhou L. Evaluating the impact of COVID-19 on male reproduction. Reproduction (2021) 161:R37–44. doi: 10.1530/REP-20-0523
39. Masarani M, Wazait H, Dinneen M. Mumps orchitis. J R Soc Med (2006) 99:573–5. doi: 10.1258/jrsm.99.11.573
Keywords: epididymitis, orchitis, epididymo-orchitis, pediatric, SARS-CoV-2, multisystem inflammatory syndrome in children, MIS-C
Citation: Inouye D, Baker Z, Peña A and Vasquez E (2023) Epididymitis, orchitis, and epididymo-orchitis associated with SARS-CoV-2 infection in pediatric patients: A systematic review. Front. Urol. 2:1092192. doi: 10.3389/fruro.2022.1092192
Received: 07 November 2022; Accepted: 21 December 2022;
Published: 19 January 2023.
Edited by:
Emilie K. Johnson, Ann & Robert H. Lurie Children’s Hospital of Chicago, United StatesReviewed by:
Daniel E. Nassau, Nicklaus Children’s Health System, United StatesCopyright © 2023 Inouye, Baker, Peña and Vasquez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zoë Baker, em9lYmFrZXJAdWNsYS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.