
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Trop. Dis., 27 February 2025
Sec. Neglected Tropical Diseases
Volume 6 - 2025 | https://doi.org/10.3389/fitd.2025.1544842
This article is part of the Research TopicClinical Review of Neglected Tropical DiseasesView all 8 articles
 India Hotopf1*
India Hotopf1* Shahreen Chowdhury1
Shahreen Chowdhury1 Guillermo Robert2
Guillermo Robert2 Mary Ellen Sellers2
Mary Ellen Sellers2 Maneesh Phillip2
Maneesh Phillip2 Anil Fastenau3,4,5
Anil Fastenau3,4,5 Maria del Mar Marais6
Maria del Mar Marais6 Constanze Vettel3
Constanze Vettel3 Mijanur Rahman6
Mijanur Rahman6 Rajni Kant Singh7
Rajni Kant Singh7 Becks Hill6
Becks Hill6 Ahmed Bekere8
Ahmed Bekere8 Laura Dean1
Laura Dean1Skin neglected tropical diseases (NTDs) cause physical impairments, and socioeconomic and mental health impacts, often exacerbated by social stigma. The WHO 2030 road map calls for integrated, person-centred care; community-based groups (CBGs) present a community-led solution. However, evidence is limited and CBGs are not consistently being operationalised across health systems. The UPLIFT study is developing and piloting a harmonised CBG tool. This scoping review aimed to identify preferred practices in existing skin-NTD CBG models and recommend a holistic framework for best practice. We searched four peer-reviewed databases and key organisations’ websites, for terms related to CBGs and skin-NTDs. Eligible studies explored community models and skin NTDs and were published in English from 2000 onwards. Studies with quantitative, qualitative, or mixed method approaches, and secondary analysis or evidence synthesis were eligible. Studies failing to fulfil the criteria, opinion pieces, cross-sectional surveys, editorials, and case studies were excluded. Outcomes on key CBG domains were thematically identified and explored from literature and discussions with subject matter experts: self-care, mental health, livelihood, and governance. Data were compiled in Excel and charted according to CBG domain and other key information (e.g., outcome and method of measurement), before writing up findings thematically. Fifty-four eligible citations were identified, including 38 peer-reviewed papers. Most studies were pretest/posttests conducted in Asia, targeting mainly leprosy, with heterogeneity in study designs and evaluative measures. Only four studies explored all CBG domains, with few CBGs including formal mental health support, livelihood activities and advocacy and awareness activities. Current research on the burden of skin-NTDs is predominantly focused on leprosy, leaving a significant gap in research on other skin-NTDs, particularly in the African region. Most CBGs are failing to integrate into health systems and mainstream important programmatic components such as sustainability and gender considerations. To address these gaps and work towards a harmonised CBG approach, we present a framework of best practice and recommend further research, targeting multiple skin-NTDs in unison.
Neglected tropical diseases (NTDs) impact nearly 1.7 billion people globally, prevailing in the most marginalised communities and perpetuating poverty and inequality (1). Skin NTDs are a subset of NTDs which impact the skin and subcutaneous tissues and include leprosy (Hansen’s Disease), Buruli ulcer (BU), lymphatic filariasis (LF), onchocerciasis, scabies, podoconiosis, yaws and cutaneous leishmaniasis (CL) (2). Skin NTDs are among the top 10 causes of disability and the third most common cause of illness globally (3). Whilst manifestations and treatments vary, skin-NTDs are unified in causing severe long-term consequences, including irreversible physical impairment, socio-economic impacts, mental distress and social stigma (3).
The WHO NTD Road map 2030 (4) calls for person-centred care and treatment approaches that prioritises country ownership and integration of services to address the long-term needs of people affected. Early case detection, disease management, disability and inclusion (DMDI) interventions should be designed to improve access to inclusive, holistic healthcare and mental health support at local (community and primary health care) levels. Additionally, the strategic framework for the integrated control and management of skin NTDs recommends that programmes should actively collaborate with people affected to acknowledge their expertise and potential and support empowerment initiatives, including peer support initiatives (5).
Community based groups (CBGs, Figure 1), also known as self-care, peer-support, self-support, self-care practice groups or self-help groups, are person-centred approaches which empower people affected by skin-NTDs to regain control of their health, increasing social participation and inclusion, resulting in “positive mental and physical health outcomes as well as belonging to society” (5). CBGs aim to empower people affected to become active participants in the management of their condition, as well as serving as forums which foster a culture of trust to support and advocate for its members on their disease journey, enhancing social participation. As Figure 2 indicates, there are two core domains of CBGs: 1) the self-management of the disease/morbidity focused on immediate outcomes; and 2) social participation and inclusion focused on mid/long term outcomes.
Figure 1. The WHO’s definition of CBGs (source: 5).
Prevention of disability (POD) related to NTDs has mainly been studied in leprosy and LF, although non-governmental organisations (NGOs) are increasingly implementing, supporting, or sustaining self-care activities through CBGs, integrating other skin NTDs. Several self-care guidelines have already been published and adopted for leprosy and LF (6–9). The importance of addressing self-awareness, people-centred approaches, livelihoods, mental well-being, advocacy, and the social and broader drivers of health are increasingly recognised (10). Some interventions have adopted integrated approaches for lower limb disorders, caused by leprosy, LF and podoconiosis in CBG models (11), whereas others have demonstrated the importance of introducing mental health peer counsellors to community interventions (12). An extensive literature review on the relationship between stigma, mental health and NTDs is now available (13). Despite this review highlighting that further information is needed to understand the most appropriate intervention approaches that can be implemented at scale to improve mental health of people affected by NTDs, peer support is emphasised as a critical option (13). Finally, organisational principles and behavioural theories have also been documented in the context of self-care planning (14, 15). Overall, CBGs present a powerful and widely recognised bottom-up intervention model that aligns with the WHO’s recent strategic framework for integrating skin NTDs and show potential for enhancing the upwards accountability of health systems through the empowerment of people affected. This may also allow for the development of core competencies and indicators that could be embedded within the NTD road map to support countries and programmes to attain road map goals.
Despite their evident importance, within and across countries, the operationalisation of CBG approaches is not yet integrated across health systems and their NGO implementing partners. Whilst contextual differences should be recognised and addressed in CBG models, it would be beneficial to formalize, harmonise and operationalise both cross-cutting theories and preferred practices to enhance effectiveness and improve sustainability. Such efforts would allow for harmonisation of impact measures, presenting the potential for cross-sectoral analysis and learning, contributing to enhanced programme planning, delivery, and monitoring, in the longer term.
The Unlocking the Potential of Leprosy & NTD affected people, to pursue Inclusive, Fulfilling and Transformational lives, through a harmonised Community Based Group model (UPLIFT) study aims to explore the function of CBGs with a view to develop a harmonised operational model for piloting across Bangladesh, Ethiopia, and India. To inform the development of a harmonised operational model, we conducted a scoping review to identify preferred practices and areas for improvement in existing CBG models, particularly those focused on leprosy, and or other skin-NTDs. We were particularly focused on understanding; CBG structure, member dynamics, needs, priority areas and approaches to self-care, mental health, livelihoods; and any other relevant consideration for operationalising harmonised CBG models.
Scoping reviews are appropriate when there is limited evidence available as they include a breadth of topics and study designs and do not assess the quality of evidence (16). Given that we were focused on ascertaining a broad understanding of the multiple and varied ways in which CBGs have been designed, implemented and evaluated, a scoping review was deemed appropriate. Our scoping review follows the methodological framework of Arksey and O’Malley (16) and is presented according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (17).
The search strategy included keywords and Medical Subject Headings (MeSH) terms related to two concepts: 1) community-based groups (CBGs) (including other common synonyms e.g., self-help groups) and 2) skin-NTDs. The strategy was developed through consultation with Alison Derbyshire, an Academic Liaison & Training Specialist at LSTM. The search strategy was piloted and refined using Medline Complete and the finalised strategy (Table 1) was run on the 2nd of March 2023 on the following databases: Medline Complete, Psycinfo, CINHAL Complete and Global Health.
Once the peer reviewed literature gathering was complete, we searched for grey literature from key organisations’ websites, including Infolep, InfoNTD, the WHO and several other institutions, on the 24th of April 2023, as well as hand searching reference lists.
Eligible studies explored community models, investigated skin-NTDs and were published in English from 2000 onwards, since the WHO published a draft 2021-2030 road map for NTDs in April 2020, increasing attention, and potentially evidence, surrounding NTDs. Studies were also eligible if they used quantitative, qualitative, or mixed method approaches, or if they entailed secondary analysis or evidence synthesis. Studies that did not explore community models through the lens of skin NTDs and were published prior to 2000 in a language other than English were excluded. As were opinion pieces, cross-sectional surveys, editorials, and individual case studies.
Study outcomes of interest were those related to the core domains deemed as critically important based on the literature and informed by ongoing discussions with subject matter experts within the UPLIFT consortium and the DMDI working group of the NGDO Network on NTDs (Figure 2). Additionally, we also considered variations in outcome related to age, gender, and socio-economic status, where reported.
Citations from peer-reviewed literature were imported into Endnote 20 and duplicates were removed automatically and then manually, before being exported into an Excel sheet for screening. Grey literature was entered into an Excel sheet and duplicates were removed manually. Titles were also entered into Endnote to check for duplicates with existing peer-reviewed literature.
Eligible citations were identified through a two-stage screening process. First, titles and abstracts were screened to assess whether the citations were related to; 1) CBGs and 2) skin-NTDs. IH and LD double screened the first 20% and compared agreement. As a good level of agreement was achieved (defined as an inter-rater agreement of >90% (18), IH completed the rest of screening independently. Next, full texts were screened according to the eligibility criteria. IH and LD double screened the first 20% and achieved good agreement. Hence, IH screened the remainder of citations independently, with SC providing a third review to determine eligibility in cases of any discrepancies.
The Excel data charting form was developed according to the key CBG domains previously identified (Figure 2): basic information; study setting; participants; intervention; CBG components of intervention (self-care, mental health, livelihood, monitoring and governance); outcomes and method of measure; evaluation and findings. Once an eligible pool of studies was identified, IH and LD double extracted the first 10% of papers before comparing. As good agreement was achieved, IH and SC extracted the remainder independently.
Following data extraction, study findings were synthesised and presented according to domains of CBGs identified within the UPLIFT framework in a Word document, applying the thematic analysis approach (Figure 2) (19). Additional emerging domains were also considered. The findings were written up thematically by IH and SC and reviewed by LD. Finally, the findings were explored during a set of online dissemination workshops with subject matter experts.
The searches identified 2,359 citations for review, of which, 54 were deemed eligible for inclusion. The majority (n=38) were peer-reviewed papers and 17 were grey literature. Figure 3 presents a flow chart of the search, screening process and application of the eligibility criteria.
Studies were conducted across Asia (n=20), Africa (n=16) and South America (n=2), with some focused on multiple countries (n=3) and others having a global focus (n=8). Five studies did not describe a specific geographical focus, and most were conducted in a single country (n=38). Ethiopia was the most common country (n=8), followed by Nepal (n=7) and India (n=6). Included studies demonstrated a high degree of heterogeneity, with 17 different study designs identified. The majority were pretestt/posttest designs (n=11), followed by reports (n=8) and reviews (n=7) and most used mixed methods (n=24). Most studies targeted a single disease (67%), with leprosy (n=29) being most common, followed by studies targeting LF alone (n=5) and leprosy, LF and podoconiosis simultaneously (n=5). See Table 2 for an overview of study characteristics.
Table 2 includes information on the type of CBG domain covered and the type of formal evaluation tool used, demonstrating that across all studies, tools are not standardised and not all domains are covered. Advocacy and awareness emerged as an additional critical domain based on the evidence. Overall, just four studies discussed all five domains, including advocacy and awareness (27, 46, 48, 62) and eight studies did not discuss any of the key domains. Tools evaluated self-support, self-care and self-help structures (n=37), including outcomes related to physical impacts: skin and wound care (n=28), health literacy (n=3) and other outcomes e.g., referrals (n=7). Mental health was also evaluated (n=29), including tools exploring the impact of mental health and counselling (n=17) and changes in stigma reduction and social participation (n=11). Tools were largely quantitative, with only four studies using qualitative methods, such as FGDs, interviews and photovoice to evaluate numerous outcomes (27, 39, 57, 62).
Self-care typically focused on skin/wound care and health education and was highlighted by most papers (39/54), illustrating that it is often the primary focus of CBGs.
Wound management activities involve basic training, typically from health providers, with demonstrations on how to clean wounds using soap and water and perform self-care at home (6, 27, 39, 50, 57). For leprosy-specific CBGs, some studies highlighted inspection of hands and feet for signs of damage as central and typically entailing soaking one’s hands/feet in water for 30 min, often using mud pots and a stone to gently scrape over callouses; dressing wounds using local materials and oiling the skin (50). One study reported provision of treatment such as antibiotics, ointments and painkillers, though it noted that such treatment is considerably less common (44). Where treatment is not provided, members are typically referred to government clinics where they can access medicines, as described by Yahathugoda et al. (70).
According to Noordende et al. (57), CBG members typically receive self-care kits to practice self-care, such as soap, bandages, Vaseline, and buckets. CBGs focused on leprosy, LF and podoconiosis also provide protective footwear, which is occasionally custom-made, as highlighted by a few studies (35, 44, 45).
Where CBGs cannot provide medication, the focus is on prevention using local material(s) (including soap and oil); Benbow and Tamiru (24) places emphasis on finding local solutions through the self-provision of materials where group members are required to provide their own wound management materials. This self-reliant approach encourages individuals to take ownership of their healing process and prevents reliance on external sources (24). Local materials included the core from a maize corncob as a scraping tool and cellulose strips from the stem of the banana leaf as bandages (24).
Health education includes information on conditions, symptoms, and environmental factors, as well as treatment, hygiene, and exercise and is key in achieving behaviour change – a domain of interest in the NTD community. Some CBGs use Information Education Communication (IEC) materials to educate patients on management procedures to be followed up at home; it is recommended that IEC materials on conditions, skin and wound care are pictorial and written in local languages (27, 44, 62). Yoga exercises were facilitated in LF camps in India focusing on flexion of toes, ankle joints and breathing exercises (20). As Noordende et al. (57) highlights, facilitation of self-support techniques is often cascaded; for example, the first meetings are often facilitated by health workers, who then supervise members and carers on techniques. Several studies described how family members and caregivers are often involved in training on self-care highlighting their key role in the support and recovery of CBG members (10, 23, 28, 39, 42).
Despite a growing recognition of the importance of addressing stigma and mental health through CBGs, only 16 studies included mental health components, typically focused on uniting people affected and their communities and providing mental health support, such as counselling (5, 10, 22, 25, 27, 33, 35, 37, 44, 46, 48–50, 53, 58, 62, 69).
We have included all references to any form of counselling or talk therapy within this section as we recognise that understanding of disease causation is critical to supporting good mental health amongst people affected (71). The content of CBG counselling activities reported by studies varied and included providing accurate disease knowledge, addressing misconceptions around the cause of conditions (e.g., that skin NTDs are caused by witchcraft or curses which are self-inflicted), as well as facilitating discussions around emotions and relationships in relation to stigma and coping mechanisms (25, 33, 35, 46). Typically, encouraging members to share their personal experiences and success stories, fosters belonging and strengthens social connections between group members, as highlighted by Bhat et al. (25) and Chowdhury et al. (27).
According to the WHO (5), CBGs and peer supporters play a crucial role in addressing mental health and stigma, due to their deep understanding from lived experience. Individuals can be educated in basic techniques like psychological first aid (PFA) and facilitating prompt referrals to specialised services, enabling early identification of mental health conditions (5). According to Noordende et al. (57), people affected and families learn about receiving and providing psychosocial support. In Ethiopia (EnDPoINT study), a mental health professional conducted assessments for all patients, treatment (e.g., counselling and antidepressants) were administered if required, and caregivers received guidance on administering medication (37). Follow-up consultations with mental health experts were also scheduled. Prescribers, local nurses and health officers also received a 5-day training course in DMDI and mental health (37). Mental health training was guided by the WHO Mental Health Gap Action Program resources and involved a 5-day practical in a hospital, facilitated by a psychiatrist, as well as supervision and mentorship (37). Studies in Nepal also emphasised that integrating mental health services improves the efficiency and cost-effectiveness of community-based groups, strengthening wellbeing and adherence (5).
Twenty-five studies included livelihood and economic empowerment (5, 22, 25, 27, 28, 30, 31, 33, 34, 36, 40, 41, 45, 46, 48, 49, 55–59, 62, 63, 67, 72). The WHO (5) highlights livelihood activities, specifically financial activities, as a key form of self-help for people affected and their family members. According to Cornielje et al. (28), socioeconomic empowerment stops the cycle of poverty, dependence, and isolation, through improving self-perception and social status, though CBGs should refrain from focusing solely on socioeconomic rehabilitation as such programmes would fail to address other key domains. Twenty (20) of the studies included livelihood components.
According to ILEP (46), CBGs typically act as “micro credit unions” wherein members make small financial contributions (e.g., 10 taka/month or 0.08 USD/month) into a communal pot of money, which NGOs might also contribute to. Whilst the facilitator (see section on Facilitation: roles and responsibilities below) typically safeguards funds, decisions on who obtains loans and interest rates tend to be a group decision, potentially dependent on members fulfilling pre-requisites e.g., financially contributing for 6 months, as described by Dahiru et al. (34). Alternatively, in Ethiopia, implementers established Organisations for People with Disabilities (OPDs) for each skin-NTD, providing microfinance via member contributions (57).
One typical use of micro-loans is seed money for micro-enterprise development (30); with support from CBGs, people affected launch businesses such as traditional handicraft shops; fish or chicken farms and traditional medicine stores, as described by a few studies (34, 46, 62). This is achieved through vocational training and skills programmes on topics such as literacy, bamboo weaving, farming, marketing and packaging production, as well as general business skills, in some studies (27, 34, 46, 52, 62, 67). As Muldoon et al. (52) described, CBGs also provide training to family members, on the basis that “income generation will benefit the whole family”. Micro-enterprise development typically occurs in the maturation phase, once the CBG has achieved significant improvements in health and hygiene practices, according to Dahiru et al. (34). Some papers assert that aside from improving the financial and social status of people affected and their families, these activities support the local economy and enable people to re-train in professions which are less physically demanding, also improving family relationships (34, 67, 72). In addition to encouraging new business formation, organisations such as The Leprosy Mission India focus on nurturing existing enterprises through adoption of innovative approaches e.g., rainwater harvesting (67). Additionally, CBGs might support people affected to seek appropriate employment from existing businesses (67).
Another key livelihood activity is community development, which generally occurs in the CBG growth phase (~five years in, when there is a shift towards community interventions and participation and self-advocacy) (41). Grounded in concepts of civic responsibility, some studies describe CBGs encouraging participation in community enhancement activities, such as road repair and improving water, sanitation and hygiene (WASH) infrastructure (30, 33, 46). Additionally, members might organise informal education and health promotion activities, such as street dramas, as well as supporting community development activities for other marginalised groups, as described by Cross et al. (33) and Kiran et al. (49). Such activities might entail engaging community leaders and government to conduct formal needs assessments, as in the case of TLMTI’s CBGs, federations and cooperatives (67). As Ebenso et al. (41) highlight, the level of success is largely dependent on the planning stage and active participation of communities of people affected.
Seventeen (17) studies included advocacy and awareness focused on: 1) the rights of people affected by skin-NTDs, as well as other members who may be vulnerable to discrimination and exclusion, such as older people; 2) improving access to healthcare and infrastructure; and 3) evidence based NTD action and equal access to opportunities, such as employment and essential services (5, 27, 30, 36, 41, 44–46, 49, 53, 55–57, 61–63, 68). Advocacy objectives were achieved through holding forums and public functions with social and political leaders in India (53), school visits in Bangladesh (46), district department visits in Indonesia (46) or through providing advocacy training to patient advocacy groups (46). One prime example of successful advocacy efforts is in Nigeria, where the growth phase of an intervention witnessed the formation of the Nigerian International Association for Integration, Dignity and Economic Advancement (IDEA) – groups which advocate for the rights of people affected by leprosy (41). Through self-advocacy campaigns, IDEA have achieved “chapters” or groups in almost all states (41).
Advocacy typically involves collaboration with numerous intersectional stakeholders, such as the Ministry of Health (MoH), community and religious leaders, national NTD programmes, NGOs/international MGOs, female community volunteers, healthcare staff, organisations of people with disabilities and schools, as described by a few studies (27, 46, 61, 63).
Awareness raising amongst communities and affected populations was identified as crucial in addressing stigma, increasing acceptance and ensuring early diagnosis of skin-NTDs by Noordende (56) and the WHO (5). Activities typically included: the design and distribution of IEC materials including posters, videos, mass media and comics; training for community volunteers; community awareness workshops and exhibitions in health centres and communities (36, 44, 46, 62). Awareness topics included the early signs of skin-NTDs, myth busting and promoting positive attitudes during ‘contact events’ with community members, as described by Noordende (56). One example of groups setting expectations regarding awareness raising was seen in Ethiopia, where members are expected to deliver health information to a minimum of five community members each month, via community social events (68).
The exact structural organisation of CBGs and the various roles and committees was shaped by the group’s purpose, e.g., whether focused on self-care or livelihoods (73). Key considerations identified in the literature were group size, meeting schedules, meeting venue and facilitation process. Some authors emphasised that contextual factors such as geographic barriers, lack of resources, and political instability could impact the success of support groups (28, 45, 56).
From the literature, group size varied from 5-10 members (21, 24, 34, 45, 46, 69) and 20-30, which was less common (27, 43). As Dahiru et al. (34) highlights, groups should be big enough to encourage discussions, but not so big that members grow bored waiting for their turn to speak or be examined. Size depends on numerous factors, including location - Benbow and Tamiru (24) found groups in rural areas were typically half the size of urban areas, potentially due to transportation barriers. Husada (45) identifies that if group size becomes too large, reorganisation to sub-groups based on geographic location, profession and disability status is advisable. Nonetheless, it is important to ensure inclusion of women during group formation and establishing group leadership as women are often neglected due to their “less visible role in society” – for instance, Shrestha et al. (63) recommend ensuring that at least 50% of leadership are women (45, 63). According to Noordende et al. (57), many CBGs also invite family members or neighbors to participate.
The frequency and timing of meetings is dictated by members, and ranges from weekly to trimonthly, with monthly sessions being most common (8/19 studies reporting the frequency) (24, 27, 33, 45, 54, 58, 59, 62). As Husada (45) highlights, meeting more frequently initially helps build rapport quickly and using dates like “every first Thursday of the month” is most memorable and holding meetings on market days supports members to combine trips, saving on travel. Weekend meetings may need revision if members are employed (45). Moreover, the timing of meetings might need to be adjusted seasonally – for instance, Dahiru et al. (34) asserts that evening meetings will be preferable during farming session.
Meetings typically last 1-2 hours, and CBG duration spans from weeks-years, depending on funding availability, disease severity, group demand and meeting frequency (24, 45, 63). Husada (45) reports that once the group has reached the end of its planned duration, there are several options for next steps, including a) terminating the group b) continuing with a reduced frequency or c) continuing in the same fashion. The latter may require groups to seek alternative funding sources.
According to the literature, meeting places are generally selected by group members; typical locations include health centres, people’s homes and public or private community locations (24, 33, 34, 46). Whilst the latter fosters a sense of community and encourages involvement from family and neighbors, Husada (45) warns that holding meetings publicly may expose members to stigma. Venues must be accessible, central (members are seldom willing to pay for transport), private and large enough for everyone to sit in a circle, according to Dahiru et al. (34) and Husada (45). The same papers also suggest that venues be private, sheltered and have a water supply, as well as being close to a referral hospital (34, 45).
Facilitation within CBGs refers to the role of leaders (elected group member with lived experience) and facilitators (non-group member, e.g., staff of NGO or research team implementing CBGs) in guiding and managing group dynamics, ensuring effective communication and engagement of members. The specific roles and responsibilities of facilitators and leaders varied depending on the context and the type of support group. However, leadership qualities, including an understanding of self-care, ability to assess members’ abilities, empathy, good listening skills, and a commitment to engaging members are consistently highlighted in several papers (10, 14, 30, 45, 60). Deepak (36) notes a shortage of mid-level healthcare workers skilled in Community Based Rehabilitation (CBR), defined as an “approach and an attitude towards rehabilitation whereby people with disabilities and caregivers define their own needs and negotiate with rehabilitation workers and policymakers to improve their living circumstances and to play their full part in society” (28, 74) as a key challenge when assigning roles and responsibilities. Benbow and Tamiru (24) and Husada (45) warn that facilitators may face challenges in maintaining group dynamics, dealing with dominant members, and addressing competing priorities.
The literature highlights two primary methods for selecting or electing group leaders: 1) at point of group formation based on leadership skills; and 2) once the group has been established (58). Some studies emphasise that groups consider gender, particularly in relation to women’s representation in leadership roles; groups should strive to elect female facilitators and empower women through providing education and job training (48, 64, 75). Doing so may address the phenomenon where gender norms, cultural beliefs, and gender dynamics can pose barriers to participation and empowerment, especially for women, as highlighted in a few studies (48, 64).
Facilitators are chosen by group leaders and members; they must possess the skills and knowledge to deliver tailored awareness and stigma reduction workshops on key topics (e.g., wound management) in the local language (14, 34, 44, 63). According to Dahiru et al. (34), facilitators often receive training on their roles, wound management, group facilitation, and self-care functioning, via presentations, discussions, group work, and role play. The exact role varies, but facilitators typically bridge the gap between the leprosy programme and community, through advocating for group members and engaging community leaders, religious figures, and volunteers (21, 63). Crucially, facilitators help group members to identify problems and develop solutions, emphasising self-reliance and problem-solving within the group. Finally, they ensure understanding of the group’s objectives, monitor attendance, and guide discussions on relevant topics, as highlighted by Darlong (10).
Groups also invite external facilitators from NTD and community programmes, typically chosen by group leaders and members, to deliver training and awareness, as described in a few papers (22, 25, 27, 37).
The end goal is for people affected to eventually adopt the facilitator role entirely, no longer needing external facilitators. Therefore, external facilitators must assess the stage of the group and respond appropriately; for example, in a study in Indonesia, the district leprosy supervisor and leprosy field worker led facilitation for 2-3 meetings then facilitated election of a group leader amongst members (22, 61).
Twenty-one (21) studies included information on monitoring and evaluation (M&E) (10, 14, 21, 23, 24, 27, 29, 33, 34, 37, 38, 42, 44–46, 50, 52, 53, 61, 62, 68, 75, 76). Across studies, the frequency of monitoring activities varied; Dahiru et al. (34) warns that M&E activities should be limited to avoid sustainability issues, suggesting that facilitators conduct monthly visits, whilst coordinators and project leaders visit quarterly and annually.
Dahiru et al. (34) and Husada (45) identified that monitoring activities consider a range of outcomes, such as group dynamics, social participation, group size, development stage, governance structures, self-worth, and social status. Compliance and attitudes towards self-care practices are other key outcomes which can be measured via meetings and household visits, as described in a few studies (21, 33, 34). Physical improvements are often monitored via regular measurement check-ups and completion of monitoring forms or participant files by facilitators, according to Benbow and Tamiru (24) and Narahari et al. (53). Alternatively, Tora et al. (68) highlights that facilitators might directly report to an NTD focal person or there may be an elected health worker who attends meetings and monitors patient data. Hounsome et al. (44) also monitored the quality of care provided via a community advisory board formed of various stakeholders, including health professionals.
Formal evaluations, typically conducted by facilitators or medical professionals, are key in ensuring CBGs are effective and adapt to the needs of affected populations, as highlighted by Celiktemur et al. (14) and Dahiru et al. (34). Dahiru et al. (34) also cautions that activities must be constructive, focusing on identifying solutions, rather than finding fault, asserting that evaluations focus on ulcers, referrals, the group development stage, the effectiveness of the leader and members’ attitudes towards the group, among other factors.
Formal evaluation approaches vary; in Thailand, evaluations occurred at the 5- and 12-month mark and involved stakeholder engagement, capacity building to assess skills and knowledge, meetings with healthcare staff and process management and structure assessments, to evaluate participants’ understanding of tasks and roles, as well as the coordinators competency (62). In Indonesia, facilitators evaluated the impact of the CBG at 6- and 12-months, collecting data on indicators including “proportion of members who demonstrate a positive change in self-care” (45). Higher level evaluations might also include meetings between project coordinators and managers to assess CBG’s ongoing challenges and successes, as described by Dahiru et al. (34).
Formal supervisions, typically provided by NGO staff or experienced facilitators, are another important component highlighted in the literatures, which provide opportunities for facilitators to seek support and raise issues, as well as enabling DMDI knowledge assessments (23, 24).
Thirty (30) of the studies explicitly referred to sustainability (4, 5, 15, 21, 24, 27, 28, 34–36, 40–43, 45–47, 50, 51, 54–58, 60, 61, 63, 67, 69, 77), whilst an additional 13 studies included information related to sustainability without being explicit. Finkenflügel and Rule (42) argue that the movement towards CBR, specifically CBGs, presents a sustainable, person-centred approach to supporting people affected by skin-NTDs (42). Within CBGs, professionals take on a facilitative role, imparting skills and knowledge to members and their families/caregivers, enabling long-term DMDI. This, combined with the shift of decision-making power from professionals to people affected, strengthens empowerment and self-efficacy, enabling genuine participation of people affected – key to sustainability (30, 33, 36, 60). However, some argue that self-care groups are fundamentally unsustainable in the long-term, citing accessibility challenges, such as financial and geographical constraints (39, 51, 56). According to Bassey Ebenso et al. (39), long-term sustainability of CBGs is dependent on three concepts: 1) continuity of impact; 2) participation of affected populations; and 3) mobilisation of multisectoral partnerships to achieve continuity of CBR services – we explore these below.
To enable continuity of impact, Cornielje et al. (28) assert that solutions must be manageable and financially sustainable for people affected. Instead of distributing medical provisions, many CBGs take sustainable approaches to wound management, using locally available materials, such as banana leaves and old clothes, as described by Benbow and Tamiru (24) and Narahari et al. (53). Doing so reduces financial strain and dependence on hospitals and ensures that self-care practices are sustainable and culturally relevant (24, 43). Similarly, Oktavian et al. (59) reports that many CBGs use locally available materials for producing crafts, such as recycling rubbish for income generation. Financial sustainability is also key; through livelihood projects, member contribution fees and community driven financial opportunities, CBGs can fund activities such as microloans and transport costs, as described in a few studies (5, 46, 58). Similarly, PAHO (60) emphasise that actors consider the potential impacts of external funding on long-term sustainability. In terms of potential challenges, Sermrittirong et al. (62) warned that funding for support groups may be insufficient and asserted a lack of ownership and accountability in some formal support groups might hinder the continuity of impact. Some studies also emphasised that moving towards a CBR approach requires collaboration among various ministries and stakeholders, and low awareness of morbidity management and disability prevention also poses challenges (36, 42).
Numerous approaches to achieving participation of people affected by NTDs were identified in the review, united by an emphasis on achieving bottom-up participation from the outset through transferring power to affected populations (29, 47). Four studies identified that this could be achieved through using participatory action research during programme design; employing people affected; co-designing training and encouraging active participation in analysing findings (14, 27, 29, 63). Providing training in areas such as public speaking and note-taking also encourages ownership, as described by TLMTI (67). According to Husada (45), the long-term goal of all CBGs should be complete independence. As Cross and Choudhary (30) highlight, once self-care groups have matured, they can transform to self-help groups, which typically entails integration of livelihood activities and other marginalised groups, as well as engaging in community development and potentially transforming to an NGO. In Bangladesh, ILEP self-help groups successfully transformed to community-based organisations, legitimising the group and enabling formation of formal programmes, ultimately increasing influence (46).
PAHO (60) emphasise the importance of harnessing existing structures and resources to strengthen coverage and sustainability, of CBR, as well as mobilising invaluable contextual knowledge. As Ebenso et al. (41) highlight, CBGs do not operate in isolation and hence, “continuity of activities is dependent on building stable stakeholder partnerships”. According to a few papers, to be successful, actors must foster partnerships with key stakeholders, such as OPDs, government, community- based actors, NGOs and religious institutes (30, 36, 44). Many papers suggest that participation should be supported through system strengthening activities; for example, providing capacity strengthening for MoH staff, supporting patient advocate groups and strengthening referral routes (50, 61). Integration is also key and may entail integrating NTDs with other developmental areas, such as gender and WASH or integrating other marginalised groups into CBGs, as described by Pronk et al. (61) and Shrestha et al. (63). Some studies advocated for the integration of other disabilities within skin-NTD CBGs, and skin-NTD specific services, with the aim that doing so will reduce stigma and strengthen sustainability (35, 60). Cornielje et al. (29) asserts that this “twin track approach” could enrich mainstream programmes and vice versa, with the added value strengthening sustainability. In terms of potential challenges, Cornielje et al. (29) warns that government programmes may be fragmented, with limited integration between sectors and high turnover of staff, affecting commitment and coordination, in addition to competing priorities from other developmental programmes, also highlighted by Shrestha et al. (63). Pronk et al. (61) recommends targeting multiple diseases based on commonalities between diseases (e.g., LF and leprosy) or in terms of which diseases are most prevalent in target populations.
Despite its evident importance, many CBGs fail to fully consider sustainability, as highlighted in reviews from Noordende et al. (55) and (51), which both found that sustainability was scarcely considered and called for programmes to strengthen sustainability outcomes.
Thirty-one (31) studies referenced establishing linkages with the healthcare system in multiple ways, including: collaborating with healthcare professionals and institutions to provide training, counselling, and support to group members (36); referrals to healthcare facilities, including for mental health support (44); accessing patient lists to invite them to join CBGs; and enlisting health workers, including community health workers (CHWs), as supervisors or facilitators (27, 33, 43–45, 59). For example, in a study in India, Accredited Social Health Activists (ASHAs) played a key role in bridging the local community and public health system, receiving training on administration of assessment tools and self-care techniques (20). Whilst health staff have a role within CBGs, some papers emphasised that their roles should shift to become facilitative, rather than prescriptive (40, 58).
Similarly, linkages with government NTD programmes were highlighted in 19 studies, with MoH and NTD programmes typically being implementing partners (24, 27, 41). The roles of NTD or Leprosy-TB programmes was mainly to support referrals; emphasise government commitment to the inclusion of people affected in wider society (24, 27, 43) and to facilitate monitoring activities within routine supervision structures (23).
This scoping review sought to map existing practices in the delivery of CBG models for skin-NTDs, with an aim to develop recommendations for a more harmonised, holistic person-centred approach to peer-support group interventions. Current approaches to CBG delivery present a powerful, person-centred approach to attaining the WHO’s strategic plan for the road map for NTDs 2021-2030, which includes strategic plan to improving morbidity, enhancing participation and inclusion of people affected by skin-NTDs, as well as presenting opportunities for case identification/control/elimination of skin-NTDs. However, we highlight that further evidence is needed to understand best practices that can support sustainability, health systems integration, gender mainstreaming, mental health, stigma reduction and advocacy/awareness within current CBG approaches. Whilst most studies included components on DMDI and education and the review highlights the positive impact of CBGs on mental health, only 30% (n=16) included formal mental health support. There is growing evidence on the impact of providing talk therapy, basic PFA and facilitating mental health referrals among other NTDs. Skin-NTDs, acknowledged as one of the most stigmatised NTDs impacting populations with inadequate access to services, should follow suit and incorporate formal mental health services in CBGs (78, 79). Livelihood and economic rehabilitation activities are vital in breaking the cycle of poverty, isolation and dependence and achieving participation and inclusion of people affected; whilst there were some strong examples of micro-enterprises and credit unions, they were only in 37% of studies (n=20). Similarly, advocacy and awareness activities which are integral in driving acceptance, empowerment and case detection, were only described in 31% (n=17). This implies that components integral in reducing the burden of skin NTDs and achieving meaningful participation and inclusion of people affected are not being considered in most CBGs. Therefore, we propose an integrated CBG model that can be operationalised to overcome these gaps and drive progress towards achieving the WHO’s 2030 NTD road map.
Below we present a theory of change for the framework of best practice with the hypothesised outcome of each domain, its associated outputs and related activities (Figure 4). The framework is informed by the scoping review findings as well as subsequent discussions with subject matter experts during dissemination workshops, wherein the findings and implications of the review were explored.
Most studies were conducted in Asia and focused on a single country, with India, Nepal and Ethiopia being most common. Whilst there is a considerable burden of skin NTDs in these countries, especially Ethiopia, our review highlights a lack of research in the African region which accounts for the highest global burden of skin-NTDs (2). The coast of Western Africa and parts of Central Africa, the horn of Africa and Yemen, are all co-endemic for 5+ skin-NTDs. However, only 16 of the 54 studies were conducted within these regions. Moreover, there was an uneven distribution within these regions, with most conducted in Nigeria and or Ethiopia (n=10), two in Mozambique and only one study in Liberia, Côte d’Ivoire, DRC, Tanzania, and Ghana, demonstrating gaps in the evidence-base. This speaks to well-known pattern of skin-NTDs sitting low on research agendas and scientific research in Africa being consistently under-represented, due to inequitable funding, inflexible institutional frameworks, and publication bias, among other factors, which may hinder the WHO’s road map progress (80–82).
Similarly, most studies focused on leprosy alone, which illustrates a lack of integration and does not reflect the burden of leprosy relative to other skin NTDs (2). This disparity is likely due to leprosy having a deep historical focus on these types of approaches, which may reflect the geographical distribution of papers (83). Regardless, it is critical that we think beyond leprosy to achieve integration and reflect the true burden of skin-NTDs, to achieve the WHO’s global road map targets.
Integration is central in maximising impact and achieving the WHO’s road map targets; pillar 2 specifically calls for enhanced cross-cutting approaches through integrating interventions for multiple NTDs and mainstreaming of programmes into the national health system and existing programmes, to enable scaling of interventions (2). Integration enables implementation of centralised, sustainable, holistic programmes which achieve more effective use of resources, improved coverage and encourage holistic integrated approaches through harnessing synergies across existing programmes (4, 84). Moreover, integration overcomes issues of duplication and competition over resources, commonly associated with vertical programmes – ultimately, strengthening impact and health outcomes (82). Despite this, our review found that only 10 of the 54 studies targeted multiple skin-NTDs, with Leprosy, LF and podoconiosis most integrated, since these lower limb disorders share similar care needs (11, 85). Moreover, whilst the majority did collaborate with health systems and government NTD programmes, for instance through arranging two-way referrals (between CBGs and the formal health system) and enlisting health workers as external facilitators, none of the CBGs appeared to collaborate with the informal sector, such as traditional and faith healers and many relied on NGO partners to kick-start or fund such initiatives. This presents a missed opportunity for collaboration, as the role of traditional and faith-based healers in healthcare provision has gained increasing recognition over the last decade, particularly in Africa, where the burden of skin-NTDs is most severe (84, 86). There is a growing pool of literature which demonstrates how CBGs can offer useful platforms for other NTD interventions (e.g., mass drug administration and bed net distribution), enhancing equity of delivery, particularly if they are well established within the community health system (77, 87). However, very few studies discussed this concept; where it was mentioned, it was limited to recommendations for future research, with no examples of integration in practice identified, suggesting a knowledge gap (4, 29, 35, 61).
Integration and mainstreaming are essential in achieving sustainable, locally-led CBGs and align with WHO’s road map indicator of 40 countries adopting and implementing integrated skin-NTD strategies by 2030 – thus, future CBG interventions must be integrated (4). To achieve integration, further research is needed to evidence different approaches for integration and the roles and responsibilities of different actors across the health system. The latter is particularly important, since skin-NTDs have far reaching impacts beyond the physical and psychological symptoms, which interact with virtually all aspects of people affected lives (e.g., livelihoods). Thus, cross-sectoral collaboration is key in delivering complex development interventions.
Globally, skin-NTD data is insufficient; a recent conference uniting researchers and WHO members prioritised producing strong evidence on the cost-effectiveness of DMDI for skin NTDs to support national implementation and attract donors, as well as collecting more robust data on skin-NTDs to map disease distributions and overlaps to support advocacy efforts and resource allocation (88). These aims align with WHO’s road map targets of integrating M&E efforts, which remain fragmented (2). We found a high degree of heterogeneity in the study designs and measures used to evaluate the impact and effectiveness of CBGs, with very few harnessing participatory methods to capture the views and experiences of people affected. This is problematic given the limited evidence currently available on preferred practices and pathways to empowerment for people affected by NTDs. Given the centrality of DMDI, and the inclusion and participation of people affected by NTDs within WHO’s NTD road map, establishing indicators of best practice/impact of CBGs is essential to enable national programmes to measure gains in these areas, and is critical to ensuring equitable and sustainable attainment of road map goals. Only one of the papers identified within this review used a randomised controlled trial (RCT) design. Going forward, we need more CBG evaluations which use robust, homogenous study designs, with standardised evaluative approaches aligned with WHO indicators to enable comparison and ensure transparency, adaptability, and accountability to affected populations.
Gender is a key consideration for skin-NTDs, as it interacts with other identity factors and forms of discrimination to influence the degree of vulnerability to- and experiences of- skin NTDs, with women and girls bearing a disproportionate burden (89–91). For instance, women and girls face heightened rates of stigma and mental health issues, combined with lower educational attainment, relative decision-making power and socioeconomic inequities. These barriers significantly hinder their participation, including within CBGs. (92, 93). Thus, gender equity is a key consideration within pillar 1 of the road map for NTDs 2021-2030 ‘Accelerating programmatic action’ (2). Very few studies explored the gender dimension of CBGs; those that did emphasised the need for gender equity, including recruiting women facilitators in CBGs, offering education, job training, and basic services to empower women (48, 51, 64, 75). This aligns with the gap in intersectional, gender-sensitive NTD evidence described by the WHO (2) – therefore, further research is needed into the best approaches to mainstream intersectional, gendered considerations within CBG models.
56% of the studies referred to sustainability, with some practical examples of sustainable approaches to CBGs given, for example using locally available materials, cascading training to people affected and family members and transfer of facilitator role. The WHO repeatedly emphasise the importance of sustainability throughout their road map (2). However, just under half of the studies did not mention sustainability at all, aligning with the gaps highlighted by other scoping reviews (51, 55). Moreover, even where studies did mention sustainability, none of them included outcomes related to sustainability and it was only central in a few papers (judged by whether or not it was discussed in the abstract) (23, 40, 55).
The sustainability of CBGs relies on ensuring the continuity of impact, fostering active participation of people affected and mobilising multisectoral partnerships (Bassey 39). Continuity of impact involves maintaining and expanding the positive changes initiated by CBGs. To achieve this, dependence on external facilitators must be reduced, and processes should be designed to be attainable and financially sustainable for CBG members (28). Active participation is a prerequisite to ensure CBG ownership and legitimates the formalisation of independent CBG structures that evolve to maximise impact and influence (29, 46, 47). Therefore, mobilising multisectoral partnerships and empowering CBGs to dialogue with key stakeholders, including community structures, is vital for accessing knowledge, resources and networks needed to enhance CBG capacity to achieve the group´s purpose and improve their impact within the broader system (41, 61, 63).
In practice, these three concepts – continuity of impact, active participation, and multisectoral partnerships- are intrinsically linked to the empowerment of CBG members, achieved through skill development and the progressive shift in decision-making power (28, 30, 33, 36, 47, 60). After groups are formed and initial governance structures are established, external facilitators must assist members so they take ownership of their groups, moving from passive engagement to active leadership. This shift not only builds trust and fosters a sense of responsibility within CBGs, but also ensures that activities are aligned with the needs and objectives of group members, enhancing long-term commitment and sustainability.
When CBG members gather, it is crucial that they reach autonomy as soon as possible, and that other parallel core activities such as psychosocial support is led by group members in the early stages. As groups mature, activities evolve to encompass wider community and advocacy initiatives (41). At this stage, the purpose and governance structure of CBGs may change to address the needs for such growth, shifting the focus to mid and long-term outcomes. Early planning and integrated participatory approaches such as feedback mechanisms within CBG structures are therefore crucial for successful transitions. Partnerships and networks are instrumental in integrating CBGs into the broader health and social systems, ensuring that they are supported and recognised at multiple levels (35, 41, 60, 61, 63). These also help reducing stigma and foster a more inclusive environment, where the needs of people affected are understood by the wider community and different stakeholders (24, 27, 43).
Financial sustainability is key to ensure the continuity of CBGs. Although several activities have been proposed to support this, further research is needed to better understand the factors and drivers that contribute to success. Activities such as community development, livelihoods and micro-credits schemes develop over time as the group builds skills and ownership, but they require early planning and active member participation from the beginning to be sustained in the long-term (41). Based on these findings, we propose a sustainability framework for CBGs, illustrated in Figure 5.
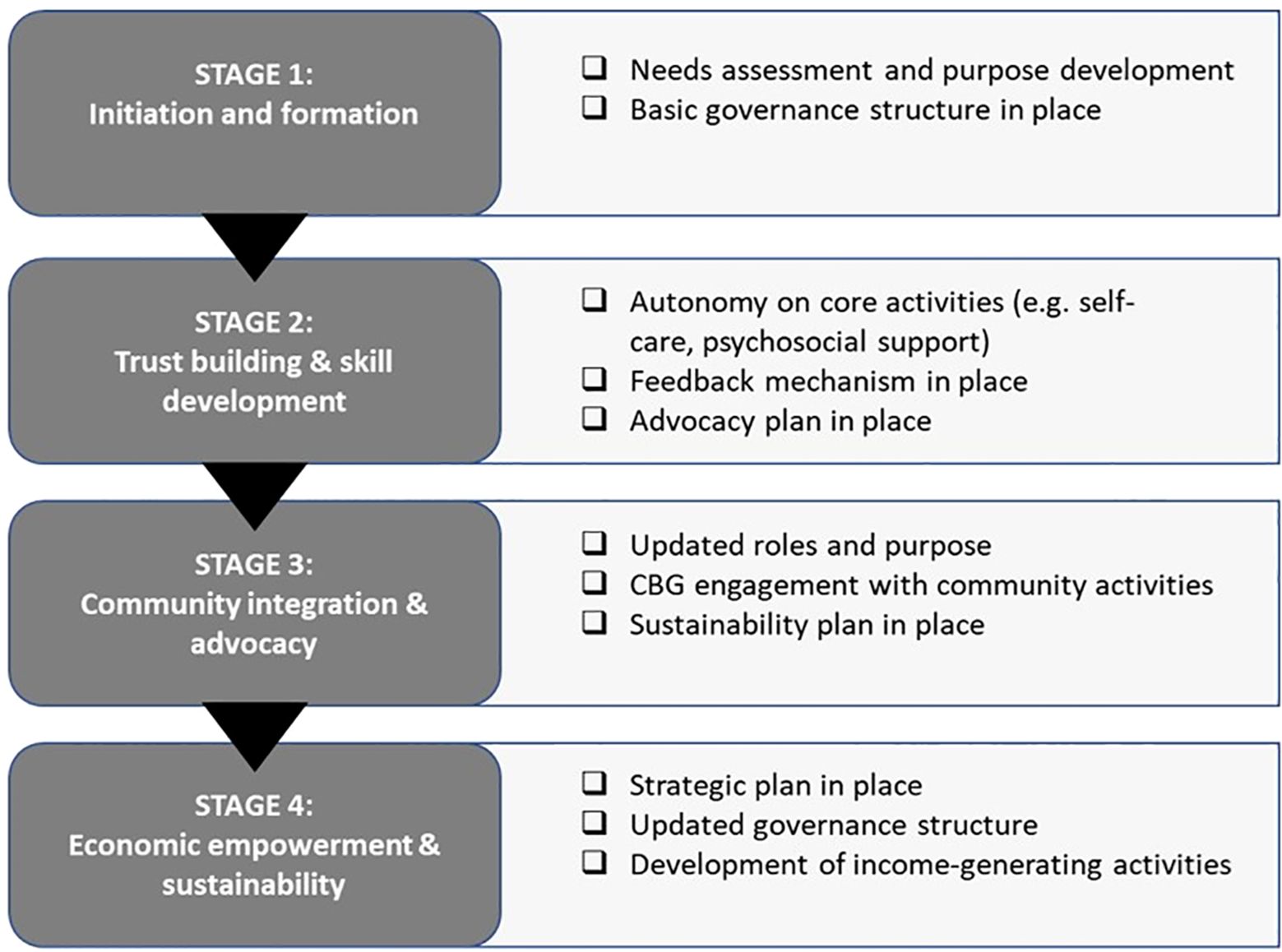
Figure 5. Sustainability framework for CBGs of people affected by NTDs gathering primarily for their self-care needs.
The strengths of our study include the fact that we incorporated both peer-reviewed and grey literature, and developed and implemented a relatively broad search strategy in collaboration with a librarian. Aside from contributing to the evidence-base on CBGs for skin-NTDs, the findings from this review have shaped international consultation workshops with professionals working on the ground on skin-NTDs and will ultimately shape the development of the UPLIFT consortium’s CBG framework which will be operationalised and evaluated within Ethiopia, Bangladesh and India.
Whilst our scoping review revealed a wealth of research on CBGs, there are several limitations to consider. Firstly, our review only included studies published in English – this may have contributed to the geographical distribution of studies and potentially risked excluding valuable research from the field conducted in languages other than English. We also acknowledge the limitations due to the heterogeneity in study designs and outcomes. We chose a scoping review design, which includes all studies regardless of the quality, there was no form of evaluation; it may have been useful to examine the quality of the evidence-base beyond commenting on the types of designs. As new evidence emerges, a systematic review and or realist evaluations which consider what works for who and in what context, might be appropriate. Finally, whilst we did search for grey literature, the search could have been more comprehensive and whilst this scoping review focused only on the NTD sector, other wider disability sectors, e.g., HIV could have contributed to further insights on best practices and sustainability.
Community-based groups (CBGs) present a viable solution to delivering sustainable, integrated, person-centred care to people affected by skin NTDs and achieving empowerment and active participation and ownership of people affected by skin-NTDs. Our review identifies significant gaps in current CBGs, particularly the narrow focus on leprosy, the limited research in the African region, and the lack of emphasis on mental health support, livelihoods, and advocacy and awareness activities. Furthermore, evaluative measures are inconsistent, and aspects such as integration, mainstreaming, sustainability, and gender dynamics are seldom formally addressed.
To address these challenges and work towards a harmonised CBG approach, further research must be conducted, especially in the African region, targeting multiple skin-NTDs in unison. Strategies such as presenting successful models, conducting training sessions, and organising visits to successful CBGs should also be delivered to facilitate effective scale up of CBG interventions, with support from our framework of best practice to inform programmatic design.
IH: Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. SC: Data curation, Formal analysis, Investigation, Project administration, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. GR: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Writing – original draft, Writing – review & editing. MS: Funding acquisition, Project administration, Resources, Writing – original draft, Writing – review & editing. MP: Writing – original draft, Writing – review & editing. AF: Writing – original draft, Writing – review & editing. Md: Writing – original draft, Writing – review & editing. CV: Writing – original draft, Writing – review & editing. MR: Writing – original draft, Writing – review & editing. RS: Writing – original draft, Writing – review & editing. BH: Writing – original draft, Writing – review & editing. AB: Writing – original draft, Writing – review & editing. LD: Conceptualization, Project administration, Resources, Supervision, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This scoping review was funded by the ILEP Reserve Fund, Effect Hope, Lepra and German Leprosy and Tuberculosis Relief Association (GLRA/DAHW) under the following UPLIFT study numbers: Bangladesh: Registration number 529 09 03 2023 (National Research Ethics Committee of the Bangladesh Medical Research Council) India: Identification number 09/LEPRA-IEC/2023 (Institutional Ethics Committee of Blue Peter Public Health & Research Centre, LEPRA Society) Ethiopia: Ref. number BFO/113TEH/1-16/80063 (Oromia Regional Health Bureau research ethics review board).
We give thanks to all ILEP members and those who contributed in the consultation process which shaped this scoping review and production of the CBG framework of best practice, as well as implementing partners who put time into facilitating local consultation workshops. The search strategy was developed through consultation with Alison Derbyshire, Academic Liaison & Training Specialist at the Liverpool School of Tropical Medicine. Finally, we give thanks to persons affected for their participation in focus group discussions during the consultation process.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. END. The Impact of Neglected Tropical Diseases. New York, USA: The END Fund (2023). Available at: https://end.org/ntds-in-focus/ (Accessed February 5, 2024).
2. WHO. Global report on neglected tropical diseases 2023. New York, USA (2023). Available online at: https://iris.who.int/bitstream/handle/10665/365729/9789240067295-eng.pdf?sequence=1 (Accessed February 5, 2024).
3. WHO. Global meeting on skin-related neglected tropical diseases (skin NTDs). Geneva, Switzerland: WHO (2023). Available at: https://www.who.int/news-room/events/detail/2023/03/27/default-calendar/global-meeting-on-skin-related-neglected-tropical-diseases-skin-ntds (Accessed October 9, 2023).
4. WHO. Ending the neglect to attain the Sustainable Development Goals: A road map for neglected tropical diseases 2021–2030 (2021). Available online at: https://www.who.int/publications/i/item/9789240010352 (Accessed October 9, 2023).
5. WHO. Ending the neglect to attain the sustainable development goals: a strategic framework for integrated control and management of skin-related neglected tropical diseases (2022). Available online at: https://www.who.int/publications/i/item/9789240051423(Accessed October 9, 2023).
6. ALM. Ten steps a guide for health promotion and empowerment of people affected by neglected tropical diseases (2015). Available online at: https://leprosy.org/wp-content/uploads/2022/02/ALM-10Steps-FULLGUIDE-021816.pdf (Accessed November 15, 2023).
7. Deribe K, Kebede B, Tamiru M, Mengistu B, Kebede F, Martindale S, et al. Integrated morbidity management for lymphatic filariasis and podoconiosis, Ethiopia. Bull World Health Organ. (2017) 95(9):652–6. doi: 10.2471/BLT.16.189399
8. Ilozumba O, Lilford RJ. Self-care programmes for people living with leprosy: a scoping review. Leprosy Rev. (2021) 92:317–37. doi: 10.47276/lr.92.4.317
9. WHO. Lymphatic filariasis - managing morbidity and preventing disability: An aide-mémoire for national programme managers. 2nd ed. Geneva, Switzerland: World Health Organisation (2021).
10. Darlong J. Self-care in leprosy at the front line. Leprosy Rev. (2021) 92:356–65. doi: 10.47276/lr.92.4.356
11. Davies B, Mersha K, Ali O, Asrat M, Abraham T, Mossie Tamiru W, et al. Stakeholder perspectives on an integrated package of care for lower limb disorders caused by podoconiosis, lymphatic filariasis or leprosy: a qualitative study. PloS Negl Trop Dis. (2022) 16:e0010132. doi: 10.1371/journal.pntd.0010132
12. Netten WJV, Dorst MMARv, Waltz MM, Pandey BD, Aley D, Choudhary R, et al. Mental wellbeing among people affected by leprosy in the Terai region, Nepal. Leprosy Rev. (2021) 29:59–74. doi: 10.47276/lr.92.1.59
13. Koschorke M, Al-Haboubi Y, Tseng P-C, Semrau M, Eaton J. Mental health, stigma, and neglected tropical diseases: A review and systematic mapping of the evidence. Front Trop Dis. (2022) 3:808955. doi: 10.3389/fitd.2022.808955
14. Celiktemur B, Choudhury SM, Lilford R. Organizing and managing a programme for self-care in leprosy. Leprosy Rev. (2021) 92:338–43. doi: 10.47276/lr.92.4.338
15. Choudhury SM, Kudrnaa L, Celiktemurb B, Lilford RJ. Application of behavioural psychology principles to self-care programmes for people living with leprosy. Leprosy Rev. (2021) 92:344–55. doi: 10.47276/lr.92.4.344
16. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Method. (2005) 8:19–32. doi: 10.1080/1364557032000119616
17. Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PloS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
18. Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ psychol Measurement. (1973) 33:613–9. doi: 10.1177/001316447303300309
19. Clarke V, Braun V. Thematic analysis. J Positive Psychol. (2017) 12:297–8. doi: 10.1080/17439760.2016.1262613
20. Aggithaya MG, Narahari SR, Sudha V, Mohammed S, Jacob NK, Sushma KV. Self care integrative treatment demonstrated in rural community setting improves health related quality of life of lymphatic filariasis patients in endemic villages [Journal Article. Acta Tropica. (2013) 126:198–204. doi: 10.1016/j.actatropica.2013.02.022
21. Akogun OB, Badaki JA. Management of adenolymphangitis and lymphoedema due to lymphatic filariasis in resource-limited North-eastern Nigeria. Acta Tropica. (2011) 120:S69–75. doi: 10.1016/j.actatropica.2010.10.006
22. Arief F. Self care group in leprosy control program in Indonesia. Amsterdam: Royal Tropical Institute (2008). Available at: http://www.bibalex.org/search4dev/files/351089/185295.pdf (Accessed January 20, 2024).
23. Atinbire SA, Marfo B, Alomatu B, Ahorlu C, Saunderson P, Weiland S. The development of a capacity-strengthening program to promote self-care practices among people with lymphatic filariasis-related lymphedema in the Upper West Region of Ghana. Infect Dis Poverty. (2021) 10. doi: 10.1186/s40249-021-00846-z
24. Benbow C, Tamiru T. The experience of self-care groups with people affected by leprosy: ALERT, Ethiopia. Leprosy Rev. (2001) 72:311–21. https://lstmed.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=sso&db=lhh&AN=20013158807&site=ehost-live&scope=site.
25. Bhat L, Khan N, Vaida N, Hassan I, Banday MT. Assessing the anticipated stigma among leprosy affected persons and its reduction through counselling: a case study. Indian J Leprosy. (2021) 93:241–54. https://www.ijl.org.in/article-detail/93/382.
26. Chowdhury S, Mccollum R, Rogers E, Zaizay Z, Dean L. Intervention manual supporting health workers to identify, diagnose, treat and support persons affected by NTDs that affect the skin (2022). Liverpool: REDRESS. Available at: https://www.redressliberia.org/news/integrated-management-of-skin-ntds-co-developing-an-operational-manual-for-use-within-national-health-systems/ (Accessed March 5, 2024).
27. Chowdhury S, Adekeye O, McRae A, Olorunfemi T, Dubukumah L, Makinde O, et al. A holistic approach to well-being and neglected tropical diseases: evaluating the impact of community-led support groups in Nigeria using community-based participatory research. Int Health. (2023) 15:i87–99. doi: 10.1093/inthealth/ihac084
28. Cornielje H, Nicholls PG, Velema J. Making sense of rehabilitation projects: classification by objectives. Leprosy Rev. (2000) 71:472–85. doi: 10.5935/0305-7518.20000049
29. Cornielje H, Piefer A, Khasnabis C. Inclusion of persons affected by leprosy in CBR. Leprosy Rev. (2008) 79:30–5. https://www.leprosy-information.org/resource/inclusion-persons-affected-leprosy-cbr.
30. Cross H, Choudhary R. STEP: an intervention to address the issue of stigma related to leprosy in Southern Nepal. Leprosy Rev. (2005) 76:316–24. https://lstmed.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=sso&db=mdc&AN=16411511&site=ehost-live&scope=site.
31. Cross H, Choudhury R. Self care: a catalyst for community development. Asia Pacific Disability Rehabil J. (2005) 16.
32. Cross H. A focus on the issues associated with implementing self-care as an intervention (2006). Available online at: https://leprosyreview.org/admin/public/api/lepra/website/getDownload/5f76007c2bea3014222a0f74 (Accessed March 5, 2024).
33. Cross H, Beise K, Ramesh C. A study of the linkage of poverty alleviation with self-care in South Central Nepal. Leprosy Rev. (2017) 88:306–17. https://www.lepra.org.uk.
34. Dahiru T, Iliyasu Z, Aliyu MH. Social participation restriction among persons with leprosy discharged from a multidrug therapy clinic in northern Nigeria. Trans R Soc Trop Med Hygiene. (2022) 116:694–703. doi: 10.1093/trstmh/trac056
35. De Bruin W, Dijkkamp E, Post E, Van Brakel WH. Combining peer-led self-care interventions for people affected by leprosy or diabetes in leprosy-endemic countries. What do health care professionals think? Leprosy Rev. (2013) 84:266–82. https://lstmed.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=sso&db=mdc&AN=24745126&site=ehost-live&scope=site.
36. Deepak S. Answering the rehabilitation needs of leprosy-affected persons in integrated setting through primary health care services and community-based rehabilitation. Indian J Leprosy. (2003) 75:127–42. https://lstmed.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=sso&db=mdc&AN=15255400&site=ehost-live&scope=site.
37. Dellar R, Ali O, Kinfe M, Mengiste A, Davey G, Bremner S, et al. Effect of a community-based holistic care package on physical and psychosocial outcomes in people with lower limb disorder caused by lymphatic filariasis, podoconiosis, and leprosy in Ethiopia: results from the endpoint pilot cohort study [Journal Article. Am J Trop Med Hygiene. (2022) 107:624–31. doi: 10.4269/ajtmh.21-1180
38. Douglass J, Hailekiros F, Martindale S, Mableson H, Seife F, Bishaw T, et al. Addition of lymphatic stimulating self-care practices reduces acute attacks among people affected by moderate and severe lower-limb lymphedema in Ethiopia, a cluster randomized controlled trial. J Clin Med. (2020) 9:4077. doi: 10.3390/jcm9124077
39. Ebenso B, Fashona A, Ayuba M, Idah M, Adeyemi G, S-Fada S. Impact of socio-economic rehabilitation on leprosy stigma in Northern Nigeria: findings of a retrospective study. Asia Pacific Disability Rehabil J. (2007) 18:98–119. https://lstmed.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=sso&db=ccm&AN=105970037&site=ehost-live&scope=site.
40. Ebenso J, Muyiwa LT, Ebenso BE. Self care groups and ulcer prevention in Okegbala, Nigeria. Leprosy Rev. (2009) 80:187–96. https://www.lepra.org.uk.
41. Ebenso B, Idah M, Anyor T, Opakunmi F. Lessons from the evolution of a CBR programme for people affected by leprosy in Northern Nigeria. Leprosy Rev. (2010) 81:318–31. https://www.lepra.org.uk.
42. Finkenflügel H, Rule S. Integrating community-based rehabilitation and leprosy rehabilitation services into an inclusive development approach. Leprosy Rev. (2008) 79:83–91. https://www.lepra.org.uk.
43. Gidado M, Obasanya J, Adesigbe C, Huji J, Tahir D. Role of positive deviants among Leprosy self-care groups in Leprosy settlement, Zaria, Nigeria. J Community Med Primary Health Care. (2010) 22:1–2. doi: 10.4314/jcmphc.v22i1-2.68320
44. Hounsome N, Kinfe M, Semrau M, Ali O, Tesfaye A, Mengiste A, et al. Economic assessment of a community-based care package for people with lower limb disorder caused by lymphatic filariasis, podoconiosis and leprosy in Ethiopia. Trans R Soc Trop Med Hygiene. (2020) 114:1021–34. doi: 10.1093/trstmh/traa111
45. Husada B. Self care groups in Indonesia: a manual for leprosy control programmes (2006). Available online at: https://www.leprosy-information.org/resource/self-care-groups-Indonesia-manual-leprosy-control-programmes (Accessed February 8, 2024).
46. ILEP. Good practices in strengthening participation of persons affected by leprosy in leprosy services (2018). Available online at: https://www.leprosy-information.org/resource/good-practices-strengthening-participation-persons-affected-leprosy-leprosy-services (Accessed February 8, 2024).
47. Jay S, Winterburn M, Jha K, Sah AK, Choudhary R, Muldoon OT. A resilience building collaboration: A social identity empowerment approach to trauma management in leprosy-affected communities. psychol Trauma: Theory Research Pract Policy. (2022) 14:940–7. doi: 10.1037/tra0001160
48. Jha K, Choudhary R, Shrestha M. An assessment of women’s empowerment in mixed Self-Help Groups in Dhanusha District of Nepal. Leprosy Rev. (2020) 91:155–72. https://www.leprosy-information.org/resource/assessment-womens-empowerment-mixed-self-help-groups-dhanusha-district-Nepal.
49. Kiran J, Choudhary RK, Mamesh S, Arbind S. An assessment of women’s empowerment in mixed Self-Help Groups in Dhanusha District of Nepal. Leprosy Rev. (2020) 91:155–72. https://leprosyreview.org/article/91/2/19-0082.
50. Madhavan K, Vijayakumaran P, Ramachandran L, Manickam C, Rajmohan R, Jacob M, et al. Sustainable leprosy related disability care within integrated general health services: findings from Salem District, India. Leprosy Rev. (2007) 78:353–61. https://www.lepra.org.uk.
51. Martos-Casado G, Vives-Cases C, Gil-González D. Scoping review: Community-based programmes with people affected by leprosy. Trop Med Int Health. (2020) 25:144–58. doi: 10.1111/tmi.13345
52. Muldoon OT, Jay S, O’Donnell AT, Winterburn M, Moynihan AB, O’Connell BH, et al. Health literacy among self-help leprosy group members reduces stereotype endorsement and stigma-related harm in rural Nepal. Health Soc Care Community. (2022) 30:2230–9. doi: 10.1111/hsc.13771
53. Narahari SR, Bose KS, Aggithaya MG, Swamy GK, Ryan TJ, Unnikrishnan B, et al. Community level morbidity control of lymphoedema using self care and integrative treatment in two lymphatic filariasis endemic districts of South India: a non randomized interventional study. Trans R Soc Trop Med Hygiene. (2013) 107:566–77. doi: 10.1093/trstmh/trt054
54. Negussie H, Meseret M, Ngari M, Berkley JA, Kivaya E, Njuguna P, et al. Lymphoedema management to prevent acute dermatolymphangioadenitis in podoconiosis in northern Ethiopia (GoLBeT): a pragmatic randomised controlled trial [Journal Article. Lancet Global Health. (2018) 6:e795–803. doi: 10.1016/S2214-109X(18)30124-4
55. Noordende ATvt, Kuipers P, Pereira ZBdS. Strengthening personal and family resilience: a literature review for the leprosy context. Leprosy Rev. (2019) 90:88–104. https://www.lepra.org.uk/Handlers/Download.ashx?IDMF=de663a37-5119-44d2-9168-d3f6903fdc4d.
56. Noordende A. The Perception of Leprosy. Studies on assessment, impact and interventions at individual, family and community level. Rotterdam: Erasmus University Rotterdam (2021). Available at: https://www.leprosy-information.org/resource/perception-leprosy-studies-assessment-impact-and-interventions-individual-family-and (Accessed February 19, 2024).
57. Noordende ATvt, Aycheh MW, Tadesse T, Hagens T, Haverkort E, Schippers AP. A family-based intervention for prevention and self-management of disabilities due to leprosy, podoconiosis and lymphatic filariasis in Ethiopia: a proof of concept study. PLoS Negl Trop Dis. (2021) 15:e0009167. doi: 10.1371/journal.pntd.0009167
58. Noordende ATvt, Aycheh MW, Moges NA, Tadesse T, Schippers AP. Family-based intervention for prevention and self-management of disabilities due to leprosy, podoconiosis and lymphatic filariasis versus usual care in Ethiopia: study protocol for a cluster-randomised controlled trial. BMJ Open. (2022) 12:e056620. doi: 10.1136/bmjopen-2021-056620
59. Oktavian A, Krismawati H, Arisanti Y. Rumah sobat: integrated self-care group for leprosy in Jayapura City, Papua province. Adv Health Sci Res. (2020) 22. https://www.leprosy-information.org/resource/rumah-sobat-integrated-self-care-group-leprosy-jayapura-city-papua-province.
60. PAHO. Consensus statement on prevention of disability (2006). Available online at: https://www.paho.org/es/file/33615/download?token=hczpyeg- (Accessed February 25, 2024).
61. Pronk M, Phillip M, Schaafsma A. Best practices in strengthening health systems for integrated care for people affected by leprosy and LF (2018). Available online at: https://www.leprosy-information.org/resource/best-practices-strengthening-health-systems-integrated-care-people-affected-leprosy-and-lf (Accessed February 26, 2024).
62. Sermrittirong S, Van Brakel WH, Bunders-Aelen JFG, Ariyothai N, Chaidee N. Addressing stigma related to leprosy: lessons from an intervention study in Thailand. Int J Trop Dis Health. (2014) 5:48–63. doi: 10.9734/IJTDH/2015/13295
63. Shrestha D, Napit IB, Ansari S, Choudhury SM, Dhungana B, Gill P, et al. Evaluation of a self-help intervention to promote the health and wellbeing of marginalised people including those living with leprosy in Nepal: a prospective, observational, cluster-based, cohort study with controls. BMC Public Health. (2021) 21:873. doi: 10.1186/s12889-021-10847-0
64. Souza NM, de Lima Belmonte M, Torres Alves MG, Delmondes do Nascimento R, Gomes MF, Moura dos Santos DC. Self-care in leprosy from the perspective of operative groups: a qualitative approach. Online Braz J Nurs. (2021) 20:6–6. https://lstmed.idm.oclc.org/login?url=https://search.ebscohost.com/login.aspx?direct=true&AuthType=sso&db=ccm&AN=150636689&site=ehost-live&scope=site.
65. Susanto T, Dewi EI, Rahmawati I. The experiences of people affected by leprosy who participated in self-care groups in the community: a qualitative study in indonesia(2017). Available at: https://www.lepra.org.uk (Accessed March 5, 2024).
66. TLM. Self-care. Retrieved 02.01.2024, 2024. (2024). Available at: https://www.leprosymission.org/our-work/healthcare/self-care/.
67. TLMTI. Self-Help Groups (SHGs). New Delhi, India: The Leprosy Mission Trust India (2022). Available at: https://www.leprosymission.in/what-we-do/thematic-programmes/community-empowerment/self-help-groups-shgs/:~:text=SHGs%20are%20federated%20at%20the,sustainable%20livelihoods%20to%20their%20members (Accesed October 9, 2023).
68. Tora A, Kinfe M, Ali O, Mengiste A, Ahimed A, Fekadu A, et al. A qualitative process evaluation of a community conversation intervention to reduce stigma related to lower limb lymphoedema in Northern Ethiopia. BMC Health Serv Res. (2022) 22:1043. doi: 10.1186/s12913-022-08335-1
69. WHO. Mental health of people with neglected tropical diseases: towards a person-centred approach (2020). Available online at: https://www.who.int/publications-detail-redirect/9789240004528 (Accessed February 26, 2024).
70. Yahathugoda TC, Weerasooriya MV, Samarawickrema WA, Kimura E, Itoh M. Impact of two follow-up schemes on morbidity management and disability prevention (MMDP) programme for filarial lymphedema in Matara, Sri Lanka. Parasitol Int. (2018) 67:176–83. doi: 10.1016/j.parint.2017.11.005
71. Dean L, Tolhurst R, Nallo G, Kollie K, Bettee A, Theobald S. Neglected tropical disease as a ‘biographical disruption’: Listening to the narratives of affected persons to develop integrated people centred care in Liberia. PloS Negl Trop Dis. (2019) 13:e0007710. doi: 10.1371/journal.pntd.0007710
72. Muldoon J. Chronic oedema: assessment, compression and monitoring. Independent Nurse. (2022) 2022:18–21. doi: 10.12968/indn.2022.8.18
73. COUNTDOWN. Establishing Community-Led Support Groups For People Affected by Skin NTDs (2021). Available online at: https://countdown.lstmed.ac.uk/sites/default/files/centre/Establishing%20community-led%20support%20groups%20for%20people%20affected%20by%20skin%20NTDs.pdf (Accessed February 26, 2024).
74. Wolffers I, Finkenflugel H. PHC and CBR: concepts for empowennent. In: Finkenflugel H, editor. The handicapped community. Amsterdam: Free University Press (1993).
75. Robert G. Mid-Term Evaluation Restoring the lives of forgotten people. Colchester, Lepra. (2018).
76. Robert. Impact of an enhanced Morbidity Management and Disability Prevention service package through community-based groups, on the physical, mental wellbeing and socio-economic outcomes of people affected by lymphatic filariasis, in two districts of Bihar, India: A two-arm before and after interventional study. Effect Hope.
77. Mensah EO, Aikins MK, Gyapong M, Anto F, Bockarie MJ, Gyapong JO. Extent of integration of priority interventions into general health systems: A case study of neglected tropical diseases programme in the western region of Ghana. PLoS Negl Trop Dis. (2016) 10(5):e0004725. doi: 10.1371/journal.pntd.0004725
78. Ali O, Mengiste A, Semrau M, Tesfaye A, Fekadu A, Davey D. The impact of podoconiosis, lymphatic filariasis, and leprosy on disability and mental well-being: A systematic review. PLoS Negl Trop Dis. (2018) 15:e0009492. doi: 10.1371/journal.pntd.0009492
79. Makin S. Mental health: The invisible effects of neglected tropical diseases. Nat Outlook. (2023). https://www.nature.com/articles/d41586-023-02973-z:~:text=NTDs%20that%20affect%20the%20skin,anxiety%20and%2085%25%20have%20depression (Accessed January 15, 2024).
80. Dosso M, Cassi L, Mescheba W. Towards regional scientific integration in Africa? Evidence from co-publications. Res Policy. (2023) 52:104630. doi: 10.1016/j.respol.2022.104630
81. Makoni M. African researchers’ work is being overlooked — here’s how to change that. Nat Index. (2023). doi: 10.1038/d41586-023-03322-w
82. Yotsu L, Fuller M, Murdoch W, van Brakel C, Revankar M, Barogui J, et al. A global call for action to tackle skin-related neglected tropical diseases (skin NTDs) through integration: An ambitious step change. PLoS Negl Trop Dis. (2023) 17:e0011357. doi: 10.1371/journal.pntd.0011357
83. Jung SH, Han HW, Koh H, Yu S-Y, Nawa N, Morita A, et al. Patients help other patients: Qualitative study on a longstanding community cooperative to tackle leprosy in India. PLoS Negl Trop Dis. (2020) 14:e0008016. doi: 10.1371/journal.pntd.0008016
84. Yotsu RR. Integrated management of skin NTDs-lessons learned from existing practice and field research. Trop Med Infect Dis. (2018) 3(4):120. doi: 10.3390/tropicalmed3040120
85. Deribe K, Cano J, Trueba M, Newport M, Davey G. Global epidemiology of podoconiosis: A systematic review. PLoS Negl Trop Dis. (2018) 12:e0006324. doi: 10.1371/journal.pntd.0006324
86. Olivier J, Tsimpo C, Gemignani R, Shojo M, Coulombe H, Dimmock F, et al. Understanding the roles of faith-based health-care providers in Africa: review of the evidence with a focus on magnitude, reach, cost, and satisfaction. Lancet Global Health. (2015) 386:1765–75. doi: 10.1016/S0140-6736(15)60251-3
87. Dean LA-O, Ozano K, Adekeye O, Dixon R, Fung EG, Gyapong M, et al. Neglected Tropical Diseases as a ‘litmus test’ for Universal Health Coverage? Understanding who is left behind and why in Mass Drug Administration: Lessons from four country contexts. (2019) 13(11):e0007847. doi: 10.1371/journal.pntd.0007847
88. Simpson H, Mengiste A, Mbonigaba J, Kollie K, Nganda M, Dean L, et al. Research priorities to support the development of integrated national strategies to control skin-neglected tropical diseases. Trans R Soc Trop Med Hygiene. (2023) 117:132–8. doi: 10.1093/trstmh/trac086
89. TDR. Advancing the management of skin-related neglected tropical diseases in Ghana: Exploration of gender-related factors and mobile technology (2022). Available online at: https://tdr.who.int/newsroom/news/item/14-12-2022-advancing-the-management-of-skin-related-neglected-tropical-diseases-in-Ghana-exploration-of-gender-related-factors-and-mobile-technology (Accessed February 2, 2024).
90. TDR. Skin NTD research. Geneva, Switzerland: TDR (2024). Available at: https://tdr.who.int/our-work/research-for-implementation/neglected-tropical-diseases-research/skin-ntd-research:~:text=Women%20and%20girls%20are%20disproportionally,healthcare%20services%20for%20skin%2DNTDs (Accessed February 2, 2024).
91. Theobald S, MacPherson E, Dean L, Jacobson J, Ducker C, Gyapong M, et al. 20 years of gender mainstreaming in health: lessons and reflections for the neglected tropical diseases community. BMJ Glob Health. (2017) 2:e000512. doi: 10.1136/bmjgh-2017-000512
92. Adekeye O, Chowdhury S, McRae A, Olorunfemi T, Ozokede E, Dubukumah L, et al. Exploring the well-being of people affected by skin NTDs in Kaduna and Kwara States, Nigeria: a photovoice and scoping review study. Int Health. (2023) 15:i100–9. doi: 10.1093/inthealth/ihad003
93. Seekles ML, Kadima J, Ding Y, Bulambo C, Kim J, Kukola J, et al. Mental health, stigma and the quality of life of people affected by neglected tropical diseases of the skin in Kasai Province, Democratic Republic of the Congo: a sex-disaggregated analysis. Int Health. (2023) 20:iii28–36. doi: 10.1093/inthealth/ihad084
Keywords: skin neglected tropical disease(s), peer support, self-care, mental health, equity, person-centred health system, sustainability, gender
Citation: Hotopf I, Chowdhury S, Robert G, Sellers ME, Phillip M, Fastenau A, del Mar Marais M, Vettel C, Rahman M, Singh RK, Hill B, Bekere A and Dean L (2025) Community-based models for neglected tropical diseases affecting the skin: a scoping review. Front. Trop. Dis. 6:1544842. doi: 10.3389/fitd.2025.1544842
Received: 13 December 2024; Accepted: 04 February 2025;
Published: 27 February 2025.
Edited by:
Emanuele Nicastri, National Institute for Infectious Diseases Lazzaro Spallanzani (IRCCS), ItalyReviewed by:
Elham Kazemirad, Tehran University of Medical Sciences, IranCopyright © 2025 Hotopf, Chowdhury, Robert, Sellers, Phillip, Fastenau, del Mar Marais, Vettel, Rahman, Singh, Hill, Bekere and Dean. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: India Hotopf, aW5kaWEuaG90b3BmQGxzdG1lZC5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.