- 1USAID Medicines, Technologies, and Pharmaceutical Services Program, Management Sciences for Health, Nairobi, Kenya
- 2State Department for Public Health & Professional Standards, Ministry of Health, Nairobi, Kenya
- 3State Department for Livestock Development, Ministry of Agriculture and Livestock Development, Nairobi, Kenya
- 4United States Agency for International Development (USAID) Medicines, Technologies, and Pharmaceutical Services Program, Management Sciences for Health, Arlington, VA, United States
Kenya has established a multisectoral national action plan (NAP) on antimicrobial resistance (AMR), which provides a common framework for action by all stakeholders from different sectors in implementing AMR containment activities. Monitoring and evaluation (M&E) of the NAP-AMR has been weak, however, necessitating the development of a multisectoral M&E framework in 2021. Using this M&E tool, Kenya’s highest level technical body charged with containing AMR—the National Antimicrobial Stewardship Interagency Committee (NASIC)—led a review of the NAP-AMR (2017–2022) implementation progress at the national and county levels. The review showed that 16 out of 47 counties had established County Antimicrobial Stewardship Interagency Committees mirroring the NASIC and that 93% (38 out of 41) of the activities listed in the NAP-AMR (2017–2022) and the 2021 M&E framework for human health were either completed or ongoing (compared to 64% [28 out of 44] that were completed or ongoing in the animal and crop sectors). Key challenges identified for the implementation of the NAP-AMR included lack of adequate funding; difficulties in effective collaboration across and within relevant sectors; weak laboratory-clinical interface; erratic supply of laboratory reagents, equipment, and supplies leading to underutilization of microbiology laboratories; and poor internet connectivity at the various facilities negatively affecting transmission of AMR data to the national level. Major learnings and recommendations from the review—strengthening governance arrangements at the national and county level; costing of the NAP-AMR; and ramping up advocacy efforts to political leadership to gather further support for actions on AMR—were integrated into the next iteration of the NAP-AMR (2023–2027), which was released during the World AMR Awareness Week in November 2023. Strengthening the process for monitoring the implementation of the NAP-AMR and cascading that process to the subnational (county) level were identified as critical for a robust operationalization of NAP-AMR.
Introduction
Antimicrobial resistance (AMR) is a global threat that requires urgent collaborative action within and among countries. Its effects are felt across the human health, animal health, and environment sectors.
Thus, successful implementation of the National Action Plan on AMR (NAP-AMR) requires strong government commitment and collaboration across the various sectors and with international partners. The Kenya NAP-AMR provides a common framework for efforts from different sectors, including the human health, animal health, agriculture, fisheries, and environment sectors, and from civil society and other stakeholders in managing and implementing appropriate AMR containment activities (1).
The Government of Kenya, through the Ministry of Health and the Ministry of Agriculture, Livestock, Fisheries, and Cooperatives, developed the joint National Policy on the Prevention and Containment of Antimicrobial Resistance under the One Health approach (2). To implement the policy, Kenya developed its 2017–2022 NAP-AMR, with various containment objectives aligned with the World Health Organization’s (WHO) 2015 Global Action Plan on AMR (3). During the period 2017-2022, the National Action Plan for AMR containment in Kenya was aligned to the global action plan that focused mainly across the human health and agriculture sectors. Hence the Kenya NAP-AMR only included these two sectors. Since the NAP-AMR monitoring and evaluation (M&E) framework was aligned to the 2017-2022 NAP-AMR, it excluded the environment sector. Having recognized the critical role of the environment sector in AMR containment, the UNEP formally joined the tripartite (WHO, WOAH and FAO) in March 2022. Thereafter, all global and national documents incorporated the environment sector. The new iteration of the Kenya NAP-AMR (2023-2027) had the environment sector under the authority of the Ministry of Environment and Forestry included in alignment to the global guidance. However, as in other low- and middle-income countries, the M&E component of the NAP-AMR has been weak (4) (5) M&E is critical to determining implementation progress and facilitating advocacy for support and funding. It also provides an avenue for generating and objectively assessing data on AMR containment implementation and serves countries by providing necessary facts and evidence (6) In 2021, Kenya developed its first M&E framework for the NAP-AMR, which was revised in 2023, concurrent with the NAP-AMR review. This paper provides a summary of our experience and an analysis on measuring progress in implementation of the NAP-AMR in Kenya—including the challenges and lessons learned—using the M&E framework.
Implementation of the NAP AMR (2017–2022) at the national and county levels and monitoring and evaluation exercise conducted
To ensure the effective implementation of the NAP-AMR at the national level, Kenya established a multisectoral National Antimicrobial Stewardship Interagency Committee (NASIC) that provides leadership and coordination for monitoring implementation of the NAP-AMR. Additionally, given Kenya’s devolved government, the NAP-AMR provided for the establishment and operationalization of County Antimicrobial Stewardship Interagency Committees (CASICs) that mirror NASIC to oversee the implementation of AMR interventions at the county level. In the period 2019–2024, the US Agency for International Development (USAID) Medicines, Technologies, and Pharmaceutical Services program (henceforth referred to as the program), in collaboration with national stakeholders in Kenya, has been supporting national- and county-level government in NAP-AMR implementation, including strengthening multisectoral coordination. At the national level, the program provided technical support to the NASIC to implement and review the NAP-AMR. Moreover, based on the Ministry of Health’s recommendation, the program supported Nyeri, Murang’a, Kilifi, Kisumu, Kiambu, and Nairobi on the county level in establishing and institutionalizing CASICs and developing and implementing associated AMR workplans.
To measure the progress in implementing the 2017–2022 NAP-AMR, the program in 2021 collaborated with national stakeholders to develop an M&E framework using a multisectoral consultative process under the leadership of the One Health AMR Secretariat (7). The M&E framework was developed with a focus on key measurable results and indicators based on the outcome areas aligned with the five objectives of the NAP-AMR (2017–2022). The framework had five strategic objectives namely a) awareness and understanding of AMR improved through effective communication, education, and training; b) knowledge and evidence base strengthened through surveillance and research; c) incidence of infection reduced through effective sanitation, hygiene, and IPC measures; d) use of antimicrobials in human and animal health optimized; and e) an economic case for sustainable investment that takes account of the needs of Kenya developed, and investment in new medicines, diagnostic tools, vaccines, and other interventions increased. The framework comprised a total of 85 indicators based on the 85 activities contained in the NAP-AMR and M&E framework—41 for the human health sector and 44 for the animal and crop sectors. This activity aligned with two actions recommended as part of the indicator “Multisectoral coordination on AMR (P.3.1.),” which is part of the AMR technical area in the 2019 WHO Benchmarks for International Health Regulations Capacities: develop and implement an AMR national action plan monitoring framework (capacity level 4 action) and ensure regular monitoring of progress with data submitted to the regional and global levels (capacity level 5 action) (8).
Using the newly developed M&E framework, NASIC in 2022 led a review of the implementation of the NAP-AMR (2017–2022) with the objectives of assessing progress at the national level, identifying and addressing gaps, and developing insights and recommendations to inform the next iteration of the NAP-AMR (2023–2027). That effort incorporated desktop reviews and two focus group discussions—the initial one comprising the smaller NASIC Secretariat team of eight persons and a second one comprising 30 participants who conducted in-depth reviews. This review process also separately collected information from 37 One Health institutions and partners drawn from across the different sectors at national and county levels of government. These institutions provided feedback on the status of NAP-AMR implementation using questionnaires (Supplementary File 1). To help objectivize the process of reviewing, recording, and summarizing the NAP-AMR implementation progress as much as possible, the One Health AMR Secretariat, other multisectoral AMR stakeholders, and the program collaborated to develop a scorecard with standardized indicators within the M&E framework (Supplementary File 2). The analysis summarized the progress made in implementing the 85 activities contained in the NAP-AMR and placed them in three categories: activities achieved or completed; activities in progress; and activities not initiated. This structured approach to undertaking the review that included desk review to compile progress made across all the five NAP-AMR objectives, use of questionnaires to solicit feedback, review of implementation status using the score card, and summarization of progress to establish extent of implementation facilitated quick consensus among stakeholders on the final status of the implementation of the 2017–2022 NAP-AMR.
The M&E framework development and use of the structured approach for the review enabled the country to track its progress and assess the effectiveness, efficiency, and relevance of various NAP-AMR interventions with respect to attaining the overall goal. This process informed the subsequent revision of the NAP-AMR for the period 2023–2027.
In 2023, the four entities that comprise the One Health Quadripartite—the WHO, the Food and Agriculture Organization of the United Nations (FAO), the United Nations Environment Program, and the World Organization for Animal Health—published a guidance document to facilitate M&E for NAPs (9). That document provides countries with advice for establishing M&E plans for their NAP-AMRs that build on existing national reporting systems and recommended indicators from the WHO Global Action Plan AMR M&E framework. The guidelines stress the importance of governance and well-established systems for monitoring and evaluating a NAP-AMR to track progress, prioritize actions, appropriately allocate resources, and capture lessons learned to correct the course of action with respect to the country’s efforts to tackle AMR.
That global guidance validates the process Kenya went through in reviewing its NAP-AMR and will facilitate the development of future editions of the NAP-AMR and its M&E framework. Kenya’s 2021 NAP-AMR M&E framework largely addressed the key points of this global guidance, focusing on the context of the country and developing indicators that monitor and evaluate NAP-AMR implementation, tracking progress and capturing lessons learned to correct gaps and address challenges experienced during the implementation of the country’s first NAP-AMR.
Following the review, a one-day hybrid National AMR Consultative Forum with 102 AMR One Health stakeholders (49 females) physically present was held to disseminate the findings on the progress made in implementing the NAP-AMR and to generate lessons learned, best practices, and recommendations to be considered in the next iteration of the NAP-AMR. The findings from the scorecard analysis and the discussions and recommendations from the National AMR Consultative Forum informed the review of the next iteration of the NAP-AMR (2023–2027) by identifying priorities for inclusion. Through the review of the M&E plan for the 2023–2027 NAP-AMR, clear targets were developed to further inform implementation. Additionally, the NAP-AMR prioritized strengthening the governance and coordination arrangements and costed the activities.
To drive similar initiatives at the subnational level, the program subsequently supported the county teams in Nyeri, Kilifi, and Murang’a to apply a similar approach to reviewing progress made in implementing their CASIC AMR workplans. Prior to the county consultative review process, a standard template was shared with participants from the county teams to summarize progress made on implementing their CASIC workplans. The progress was also summarized using a scorecard, with the lessons learned informing the next iteration of their CASIC workplans.
Key achievements
The NASIC-led review of the implementation of the 2017—2022 NAP-AMR showed that of the 85 national-level activities, 29 (34%) were completed, 37 (44%) were ongoing, and 19 (22%) were not initiated. When disaggregated by sector, 93% (38 out of 41) of the activities in human health were either completed or ongoing, compared to 64% (28 out of 44) that were completed or ongoing in the combined animal and crop sectors (Figure 1). These findings show that the implementation of NAP-AMR in the human health sector was more advanced than in the animal/crop sectors.
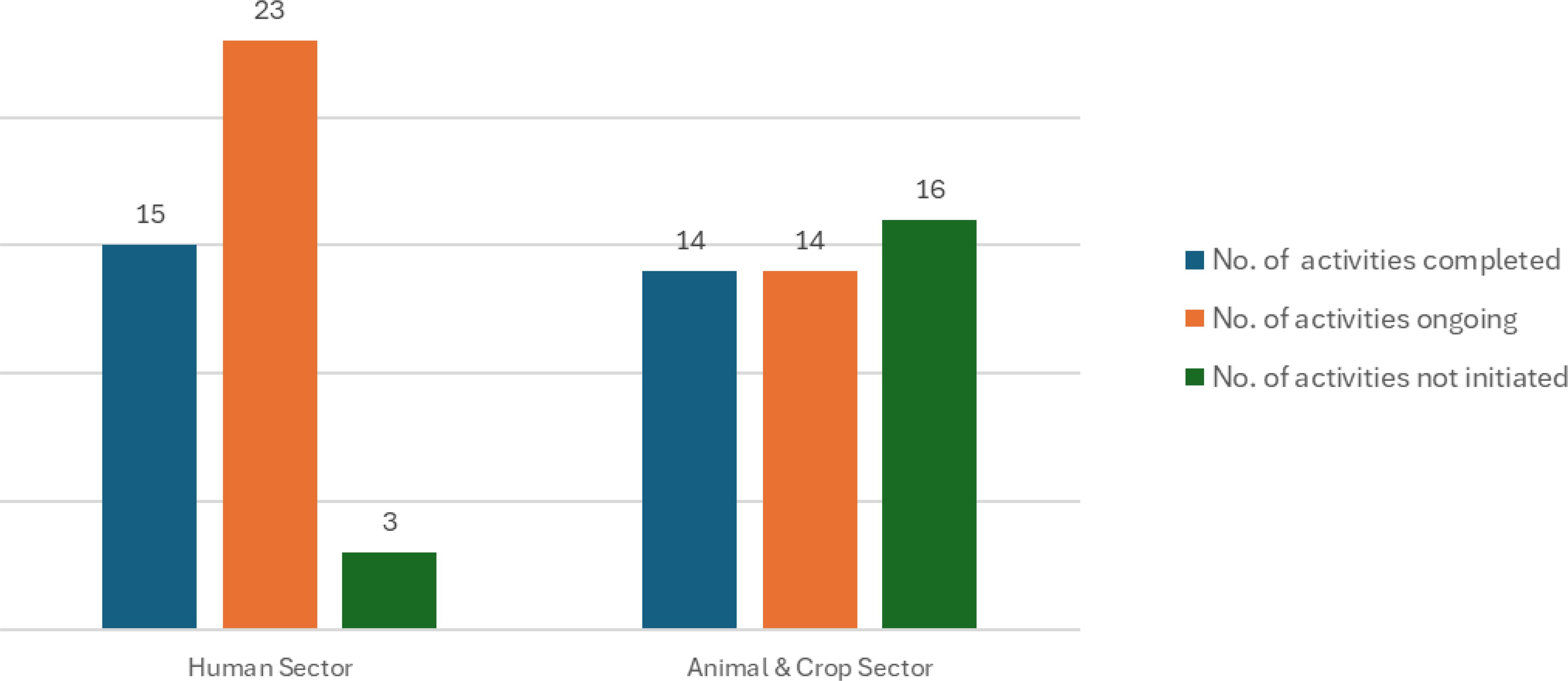
Figure 1. Summary of the implementation status of the activities contained in Kenya’s NAP-AMR 2017–2022.
Some notable achievements from the implementation of the Kenya NAP-AMR (2017–2022) include the following:
a. Establishment and inauguration of a One Health NASIC team.
b. Development and implementation of an AMR communication strategy and an AMR surveillance strategy.
c. Establishment of 22 AMR surveillance sentinel sites that submit data to the central data warehouse.
d. Development and implementation of AMR stewardship guidelines for health settings and guidelines on prudent use of antimicrobials in animals.
e. Implementation of a national policy, strategy, guidelines, and basic training course for infection prevention and control (IPC) as well as development of the national M&E framework and reporting system through the Kenya Health Information System for AMR, IPC, and patient safety.
f. Establishment of a One Health dashboard to visualize AMR trends across the country.
g. Compilation of a scoping report on the investment incentives for local production of essential antibiotics in Kenya in light of mitigating AMR.
h. Development of farm biosafety and biosecurity guidelines.
i. Development of the NAP-AMR M&E framework.
In addition to this national or central level progress in containing AMR, subnational (county) level initiatives also expanded rapidly. Jointly with the FAO, the program helped pioneer the NAP-AMR (2017–2022) mandate on “practically establishing the initial CASICS”. By the end 2023, 34% (16/47) of the counties had established CASICs, and 20/47 (42.5%) had done so by mid-November 2024. Only 10/47 (21%) have costed One Health AMR workplans, and 60% of those workplans (6/10) were supported by the program. Motivated by the experiences from the program supported counties, 14 other counties established their CASICs though their own funds or through other partners’ support. Thus, the program’s initial support sparked a much wider subnational expansion of multisectoral coordination on AMR. Despite these achievements, several challenges hindered implementation of the NAP-AMR (2017–2022) at both the national and county level. These include the following:
a. Lack of adequate funding to implement interventions across all policies at all levels coupled with a limited understanding of AMR at high policy levels and difficulties in forging effective collaboration across and within relevant sectors.
b. Issues of weak laboratory-clinical interface and erratic supply of laboratory reagents, equipment, and supplies leading to the underutilization of microbiology laboratories.
c. Poor internet connectivity at the various facilities negatively affecting transmission of AMR data to the national level.
These challenges also are consistent with the results of studies that have been conducted in other countries, particularly in Africa (10–13).
Discussion
Applying lessons learned from the implementation of NAP-AMR (2017–2022) to the development of NAP-AMR (2023–2027)
The development of the first Kenya NAP-AMR (2017–2022) did not cover certain relevant sectors, such as the environment and fisheries sectors. Additionally, the activities were not properly costed, the roles and responsibilities were unclear, and the targets were overly ambitious or unrealistic. Therefore, based on the lessons learned from the review of the 2017–2022 NAP-AMR, the new iteration of the NAP-AMR (2023–2027) incorporated all sectors—including environment, fisheries, and plants—and thereby more comprehensively implemented the One Health approach. The 2023–2027 NAP-AMR was costed at Kshs 2.035 billion (USD 13.69 million) (14) using the WHO costing tool (15), which provided clear guidance for resource mobilization. The 2023–2027 NAP-AMR incorporated a new strategic objective on governance and coordination to support system strengthening and multisectoral coordination. The activities and targets are clear and realistic and the responsibilities unambiguous. Alongside the development of the new iteration of the NAP-AMR (2023–2027), an updated M&E framework was concurrently developed that includes a clear performance indicator tracking table and performance indicator reference sheet to facilitate monitoring of progress in the implementation of NAP-AMR on a regular basis.
Crucial lessons were learned with the implementation of Kenya’s first NAP-AMR, which include the following:
a. Strong governance and leadership at national and county levels is vital for successful implementation. The program’s support to NASIC to provide overall stewardship in implementation, coordinate with various partners, and review and develop the next NAP-AMR iteration showed the value of governance and the need to further strengthen it. Additionally, strengthening the CASICs to enable them to coordinate and review NAP-AMR activity implementation progress was instrumental for success at the sub-national (county) level.
b. A structured review using the approved M&E framework helped track progress on NAP-AMR implementation and helped identify the need to further focus on a multisectoral One Health approach, which was incorporated in the second iteration of the NAP-AMR.
c. Scale-up of AMR containment efforts is needed in all 47 counties of Kenya through the establishment of county-level AMR coordination governance structures.
d. Revision of the NAP-AMR and the M&E framework concurrently allows for alignment of activities to realistic targets and timelines for successful implementation.
e. Costing of the NAP-AMR and its M&E plan is important for ensuring that resources are identified and mobilized for implementation. Strong advocacy and the mobilization of sufficient and sustained domestic funding is crucial for a sustainable implementation of the country’s NAP-AMR at the national and county levels.
f. Sustained advocacy efforts for NAP-AMR operationalization is critical, as demonstrated by the increased participation of counties, youth, communities, and other stakeholders through the years. The program engaged youth during pre-service training on AMR and anti-microbial stewardship at the University of Nairobi and during awareness-creation activities, trainings, and continuing professional development webinars that were implemented by health professional associations. The public and communities were engaged during NASIC and CASIC activities, including through AMR awareness-creation events at the national and county levels.
Future considerations for the sustainable implementation of the NAP-AMR
Affirming the six strategies for implementing the NAP-AMR, as highlighted by the WHO working paper (2.0) on implementation and coordination (16), and based on lessons learned from the implementation of the Kenya NAP-AMR (2017–2022), Kenya is on a path toward the successful implementation of its next iteration of the NAP-AMR (2023–2027) by:
a. Prioritizing the establishment and operationalization of CASICs with clear roles, responsibilities, and terms of reference in the remaining counties to oversee the implementation of the NAP-AMR in line with national efforts, thereby ensuring governance at all levels.
b. Incorporating the AMR agenda into various sectors of the country (e.g., animal, crop, environment, education, and health) and aligning the AMR interventions within existing health programs (e.g., HIV, TB, malaria, family health) to leverage available resources.
c. Ensuring the incorporation of AMR plans into existing national-level and county-level strategic documents, such as strategic plans and annual budgets, to ensure that the AMR agenda is well funded with domestic resources beyond donors’/partners’ support.
d. Engaging key AMR stakeholders from different sectors, including health, agriculture, livestock, fisheries, environment, treasury, research, academia, education, implementing partners, and the private sector, to ensure proper One Health implementation of the NAP-AMR.
e. Developing an economic case for investment and carrying out vigorous advocacy and sensitization efforts to secure political and leadership buy-in for the AMR agenda.
f. Ensuring the implementation and review of the multisectoral AMR communication strategy to tailor comprehensive messages to create awareness and action on AMR among various target audiences.
These efforts together will be crucial for contributing to the achievement of the ambitious multisectoral One Health 2030 targets outlined in the political declaration made during the September 2024 United Nations General Assembly High-Level Meeting on AMR (17).
In conclusion, the experiences and lessons learned in Kenya in developing an M&E framework, using it to review implementation of the NAP-AMR and then cascading the review process to the sub-national (county) level, can provide useful insights to other low- and middle-income countries and provide a potential model for them to adapt to their own contexts. Countries must ensure that well-structured and implemented M&E plans are an integral part of their NAPs. As outlined in the Quadripartite M&E guidance document, such a process is essential for tracking progress, prioritizing actions, appropriately allocating resources, and capturing lessons learned to make any needed course corrections for containing AMR.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
JM: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing, Data curation. NKu: Project administration, Writing – review & editing. TH: Writing – review & editing. NG: Conceptualization, Formal analysis, Writing – original draft. NKo: Project administration, Supervision, Writing – review & editing. MJ: Writing – review & editing. CO: Data curation, Writing – original draft. EW: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing. ET: Data curation, Formal analysis, Validation, Writing – review & editing. AA: Conceptualization, Data curation, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing. RN: Conceptualization, Data curation, Formal analysis, Methodology, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The work and this paper were made possible by the generous support of the American people through USAID contract no. 7200AA18C00074. The work described in this article was supported by Global Health Security Agenda funding through USAID under the terms of contract no. 7200AA18C00074.
Acknowledgments
We thank the members of the NASIC for their contributions in validating the outputs of the NAP-AMR progress review; CASIC members from the USAID Medicines, Technologies and Pharmaceutical Services (MTaPS) program -supported counties of Kisumu, Nyeri, Kilifi, and Murang’a who provided critical inputs in validating the information collected; and other counties, including Bungoma, Kiambu, and Trans Nzoia, that were supported by other partners and made contributions to the work. We thank the US Centers for Communicable Disease Control and Prevention, the Fleming Fund, the FAO, the WHO, and USAID, which supported implementation of selected AMR activities. Additionally, we thank Dr. Rashid Aman, the Chief Administrative Secretary (MOH), and Mr. Harry Kimtai, the Permanent Secretary from the Ministry of Agriculture and Livestock Development, who together officiated at the AMR stakeholder meeting to disseminate the results of the NAP-AMR review in 2022. We acknowledge the great commitment and leadership by the AMR focal persons from the environment, animal, crop, and human sectors at the national level and in the USAID MTaPS focus counties of Nyeri, Kisumu, Murang’a, Kilifi, Nairobi, and Kiambu.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2025.1540713/full#supplementary-material
References
1. Ministry of Health. National action plan on prevention and containment of antimicrobial resistance, 2017 -2022. World Health Organization (2017). Available at: https://www.afro.who.int/publications/national-action-plan-prevention-and-containment-antimicrobial-resistance-2017-2022.
2. World Health Organization. Tackling antimicrobial resistance together working paper 1.0: Multisectoral coordination (2018). Available online at: https://www.who.int/publications/i/item/tackling-antimicrobial-resistance-together-working-paper-1.0-multisectoral-coordination.
3. World Health Organization. Global action plan on antimicrobial resistance. World Health Organization (2015). Available at: https://www.who.int/publications/i/item/9789241509763.
4. Wesangula E, Githii S. Implementing the national action plan on antimicrobial resistance in Kenya: Global expectations, national realities. Int J Infect Dis. (2020). https://www.ijidonline.com/article/S1201-9712(20)30856-0/fulltext.
5. Willemsen A, Reid S. A review of national action plans on antimicrobial resistance: strengths and weaknesses. BMC. (2022). doi: 10.1186/s13756-022-01130-x
6. World Health Organization, Food and Agriculture Organization of the United Nations, World Organization for Animal Health. Monitoring and evaluation of the global action plan on antimicrobial resistance: framework and recommended indicators (2019). Available online at: https://www.who.int/publications/i/item/monitoring-and-evaluation-of-the-global-action-plan-on-antimicrobial-resistance.
7. World Health Organization. Kenya national action plan on antimicrobial resistance: review of progress in the human health sector (2022). Available online at: https://iris.who.int/bitstream/handle/10665/364530/9789240062689-eng.pdf?sequence=1.
8. World Health Organization. WHO benchmarks for international health regulations (IHR) capacities (2019). World Health Organization (2019). Available at: https://apps.who.int/iris/handle/10665/311158.
9. World Health Organization, Food and Agriculture Organization of the United Nations, United Nations Environment Programme, World Organization for Animal Health, World Health Organization. Guidance to facilitate monitoring and evaluation for antimicrobial resistance national action plans (2023). Available online at: https://iris.who.int/bitstream/handle/10665/372142/9789240069763-eng.pdf?sequence=1.
10. Ahmed SM, Naher N, Tune SN, Islam BZ. The implementation of national action plan (NAP) on antimicrobial resistance (AMR) in Bangladesh: challenges and lessons learned from a cross-sectional qualitative study. Antibiotics. (2022) 11:690. doi: 10.3390/antibiotics11050690
11. Interagency coordination group for antimicrobial resistance. Antimicrobial resistance: national action plans. World Health Organization (2018). Available at: https://cdn.who.int/media/docs/default-source/antimicrobial-resistance/iacg-amr-national-action-plans-110618.pdf?sfvrsn=53e4eb22_4.
12. Shabangu K, Essack SY, Duma SE. Barriers to implementing National Action Plans on antimicrobial resistance using a One Health Approach: policymakers’ perspectives from South Africa and Eswatini. J Global Antimicrobial Resistance. (2023) 33:130–6. doi: 10.1016/j.jgar.2023.02.007
13. Charani E, Mendelson M. An analysis of existing national action plans for antimicrobial resistance—gaps and opportunities in strategies optimising antibiotic use in human populations(2023). Available online at: https://www.thelancet.com/action/showPdf?pii=S2214-109X%2823%2900019-0.
14. Government of Kenya. National action plan on prevention and containment of antimicrobial restance (2023). Available online at: http://guidelines.health.go.ke:8000/media/National_Action_Plan_for_AMR_2023-2027_-_KENYA.pdf.
15. World Health Organization. WHO costing and budgeting Tool for National Action Plans on Antimicrobial Resistance. World Health Organization (2021). Available at: https://www.who.int/teams/surveillance-prevention-control-AMR/who-amr-costing-and-budgeting-tool.
16. World Health Organization. Turning plans into action for antimicrobial resistance (AMR) Working Paper 2.0: Implementation and coordination. World Health Organization (2019). Available at: https://www.who.int/publications/i/item/turning-plans-into-action-for-antimicrobial-resistance-(-amr)-working-paper-2.0-implementation-and-coordination.
17. World Health Organization. (2024). Available online at: https://www.who.int/news/item/26-09-2024-world-leaders-commit-to-decisive-action-on-antimicrobial-resistance.
Keywords: National Action Plan, antimicrobial resistance, monitoring and evaluation, Kenya, one health
Citation: Mukoko J, Wesangula E, Gitonga N, Kusu N, Odhiambo C, Tanui E, Azegele A, Ndanyi R, Joshi MP, Hafner T and Konduri N (2025) Kenya’s National Action Plan on antimicrobial resistance: measuring implementation progress. Front. Trop. Dis. 6:1540713. doi: 10.3389/fitd.2025.1540713
Received: 06 December 2024; Accepted: 11 February 2025;
Published: 20 March 2025.
Edited by:
Sylvia Opanga, University of Nairobi, KenyaReviewed by:
Gerald Mboowa, Makerere University, UgandaCopyright © 2025 Mukoko, Wesangula, Gitonga, Kusu, Odhiambo, Tanui, Azegele, Ndanyi, Joshi, Hafner and Konduri. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joseph Mukoko, bXVrb2tvakBnbWFpbC5jb20=
†Present address: Evelyn Wesangula, East Central and Southern Africa Health Community, Arusha, Tanzania
 Joseph Mukoko
Joseph Mukoko Evelyn Wesangula
Evelyn Wesangula Nkatha Gitonga1
Nkatha Gitonga1 Ndinda Kusu
Ndinda Kusu Mohan P. Joshi
Mohan P. Joshi Niranjan Konduri
Niranjan Konduri