
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Trop. Dis., 28 February 2025
Sec. Antimicrobial Resistance
Volume 6 - 2025 | https://doi.org/10.3389/fitd.2025.1425042
This article is part of the Research TopicInnovative Strategies for Overcoming Drug Resistance in Tropical DiseasesView all articles
Background: Antibiotic resistance poses a significant threat to healthcare services and Methicillin-Resistant Staphylococcus aureus (MRSA) is common among hospital workers. Currently, there is no research on MRSA and its prevalence in Somalia. This study sought to determine the prevalence of nasal Staphylococcus aureus carriage and the susceptibility pattern of healthcare workers’ MRSA isolates.
Methods: This cross-sectional, descriptive study involved nasal swab collection from healthcare workers at Banadir Teaching Hospital. Cefoxitin discs were used to identify methicillin-resistant strains, and their antimicrobial susceptibility was evaluated using the Kirby–Bauer (disc diffusion) method. Based on specialty, e.g., pediatrics, obstetrics, gynecology, laboratory, and intensive care unit (ICU), participants were recruited from different wards. Nasal swabs from 215 participants were inoculated on mannitol salt agar, and yellow colonies were aseptically transferred into blood agar, inoculated on DNase agar, and subjected to catalase, coagulase, and gram staining tests. Next, bacterial suspensions were prepared and aseptically inoculated on Mueller–Hinton agar plates, followed by cefoxitin antibiotic (30 μg) disc testing. Staphylococcus aureus was categorized/interpreted based on the zone diameter (nearest whole millimeter) of the cefoxitin discs. Samples with diameters of ≤21 mm were considered to be MRSA) while those with diameters of ≥22 mm were regarded as methicillin-sensitive Staphylococcus aureus.
Results: Some locations had higher MRSA isolation rates. Ward 16 (postnatal care and neonatal ICU) had the highest MRSA prevalence (n=9, 26.5%), followed by pediatric isolation (n=6, 33.3%), emergency (n=5, 17.9%), and pediatric malnutrition (n=4, 44.4%) wards. A total of 27 (23.70%) MRSA cases were isolated and were susceptible to vancomycin and linezolid.
Conclusion: Some hospital locations had higher MRSA prevalence, with the postnatal care, neonatal ICU, and isolation wards having the highest isolation rates.
Antibiotic resistance is a critical global health challenge and a pressing public health and socioeconomic concern. In modern medicine, effective antimicrobials are essential. However, rising antibiotic resistance rates have been observed in various microorganisms across all World Health Organization regions (1). Globally, in 2019, bacterial antibiotic resistance was associated with 4.95 million deaths and directly attributed to 1.27 million deaths, underscoring its serious impact on public health. A study estimated that by 2050, up to 3.8% of the global gross domestic product will be at risk of being lost because of antimicrobial resistance. Despite a lower per-person antibiotic consumption in low- and middle-income countries compared with high-income countries, several low- and middle-income countries have higher antimicrobial resistance rates. Although antibiotic overuse or misuse is the primary antimicrobial resistance driver, various interconnected factors contribute to its dissemination and prevalence (1). MRSA, a well-known nosocomial pathogen that causes severe morbidity and mortality globally, is a growing contributor to infection control management failure and has become one of the most common causes of hospital-acquired infections. Nasal carriage is thought to have a pivotal role in Staphylococcus aureus epidemiology and pathogenesis. Healthcare workers (HCWs) can introduce MRSA into hospital and community settings (2).
Staphylococcus aureus is a Gram-positive pathogen of the Staphylococcaceae family and different strains are resistant to every other beta-lactam drug. Some S. aureus strains, known as epidemic strains, are very infectious, and are likely to spread across hospitals and countries (3). S. aureus is one of the many bacteria that colonize the mouth, skin, and nasal passages well. About 20%–40% of people have S. aureus bacteria without negative consequences. A sign of antibiotic resistance to all beta-lactams is methicillin-resistant Staphylococcus aureus (MRSA). Infection risk is higher in those under intensive care, those who have recently undergone surgery, those with open wounds or intravascular devices, or those who are immunocompromised. All colonized or infected patients must be considered as possible infection sources (4). Over 90% of S. aureus strains have lactamase-encoding plasmids, which confer resistance to penicillins like methicillin and nafcillin through penicillin-binding protein modification in their cell membranes. In the United States, MRSA accounts for >50% of the S. aureus strains isolated from hospital patients (5) and it is associated with numerous illnesses, including small skin lesions and life-endangering infections. It is one of the most common causes of hospital-acquired illnesses worldwide. Bacterial antibiotic resistance raises infection risk, decreases antibiotic effectiveness, and heavily strains healthcare systems (6).
By curtailing efforts to successfully treat and prevent the spread of bacterial infection, antibiotic resistance has emerged as a serious public health problem. After their original detection in a British hospital in the 1960s, MRSA clones rapidly spread worldwide. Like penicillin-resistant bacteria, MRSA isolates frequently have genes that confer resistance to additional antimicrobial drugs and methicillin-resistant clone propagation is similar to the appearance of penicillin resistance in the 1940s (7).
Several MRSA strains have special characteristics that boost their patient-to-patient transmission in hospitals across broad geographical regions, which led to MRSA-associated hospital-acquired infections spread between the 1980s and 1990s. This was also discovered through the genetic analysis of MRSA from patients in hospitals worldwide (3).
MRSA is a global public health challenge that causes community- and hospital-acquired infections (8). Furthermore, several countries, including China, Italy, and Uganda, have reported increased milk contamination with MRSA. Several Ethiopian studies have investigated the prevalence of S. aureus nasal carriage in HCWs, with one reporting a nasal carriage rate of 28.8%, and of these cases, 12.7% were MRSA (9). Another study found an S. aureus nasal carriage rate of 23.3% among healthcare personnel (10). A Kenyan study reported that among HCWs, the S. aureus nasal carriage rate was 25.0% (11). However, there is a shortage of research on S. aureus nasal carriage prevalence in Somalia. This lack of data is further compounded by Somalia being one of the world’s lowest-income countries, making it difficult to determine the extent of healthcare-associated infections caused by MRSA and other bacteria. This study’s main aim was to determine MRSA prevalence among HCWs in Banadir Hospital, Mogadishu, Somalia. By understanding MRSA prevalence in healthcare settings, appropriate measures can be taken to prevent the spread of MRSA and other healthcare-associated infections.
A cross-sectional study was conducted to determine the prevalence of Methicillin-resistant Staphylococcus aureus (MRSA) nasal carriage among healthcare workers (HCWs) at Banadir Hospital. The study spanned from August to December 2022.
The study population included healthcare workers employed at Banadir Hospital during the study period.
Participants were selected using a random sampling method to ensure representativeness. All participants were required to provide informed consent after being given a detailed explanation of the study’s purpose and procedures. Those who consented completed a structured questionnaire and underwent nasal swab collection. Privacy and confidentiality were maintained throughout the study.
All healthcare workers employed at Banadir Hospital during the study period and individuals who were present and agreed to participate after providing informed consent were included in the study while.
Healthcare workers who were absent during the study period, participants who refused to participate or did not complete the questionnaire were not included in the study.
The sample size was calculated using the Krejcie and Morgan formula:
● n = required sample size
● Z = Z-value (1.96 for 95% confidence level)
● p = estimated prevalence (0.5 for maximum variability)
● q = 1 - p
● N = population size (417 HCWs)
● e = margin of error (0.05)
Based on the calculation, a minimum of 200 participants was required. However, to account for non-responses, 215 participants were recruited.
Sterile swabs moistened with sterile saline were used to collect samples from each nostril, rotating the swab at least five times in each. Swabs were then placed in sterile transport media, labeled with unique identifiers, and transported to the Al Jazeera Diagnostic and Research Center. Samples were processed within 2-4 hours of collection; if immediate processing was impossible, samples were stored at 4°C for a maximum of 6 hours to maintain bacterial viability.
The laboratory analysis utilized various materials including sterile swabs with transport media, sterile normal saline, Mannitol Salt Agar (MSA), Mueller-Hinton Agar, catalase reagent, blood agar, cefoxitin discs, EDTA plasma, Gram stain, an incubator, a microscope, sterile plastic loops, and an autoclave (Figures 1, 2).
Samples were inoculated onto MSA and blood agar plates, incubated aerobically at 35-37°C for 24-48 hours (Figures 3–6). Yellow colonies on MSA indicated Staphylococcus aureus (mannitol fermenting), while pink colonies suggested Staphylococcus epidermidis or other non-fermenting organisms.
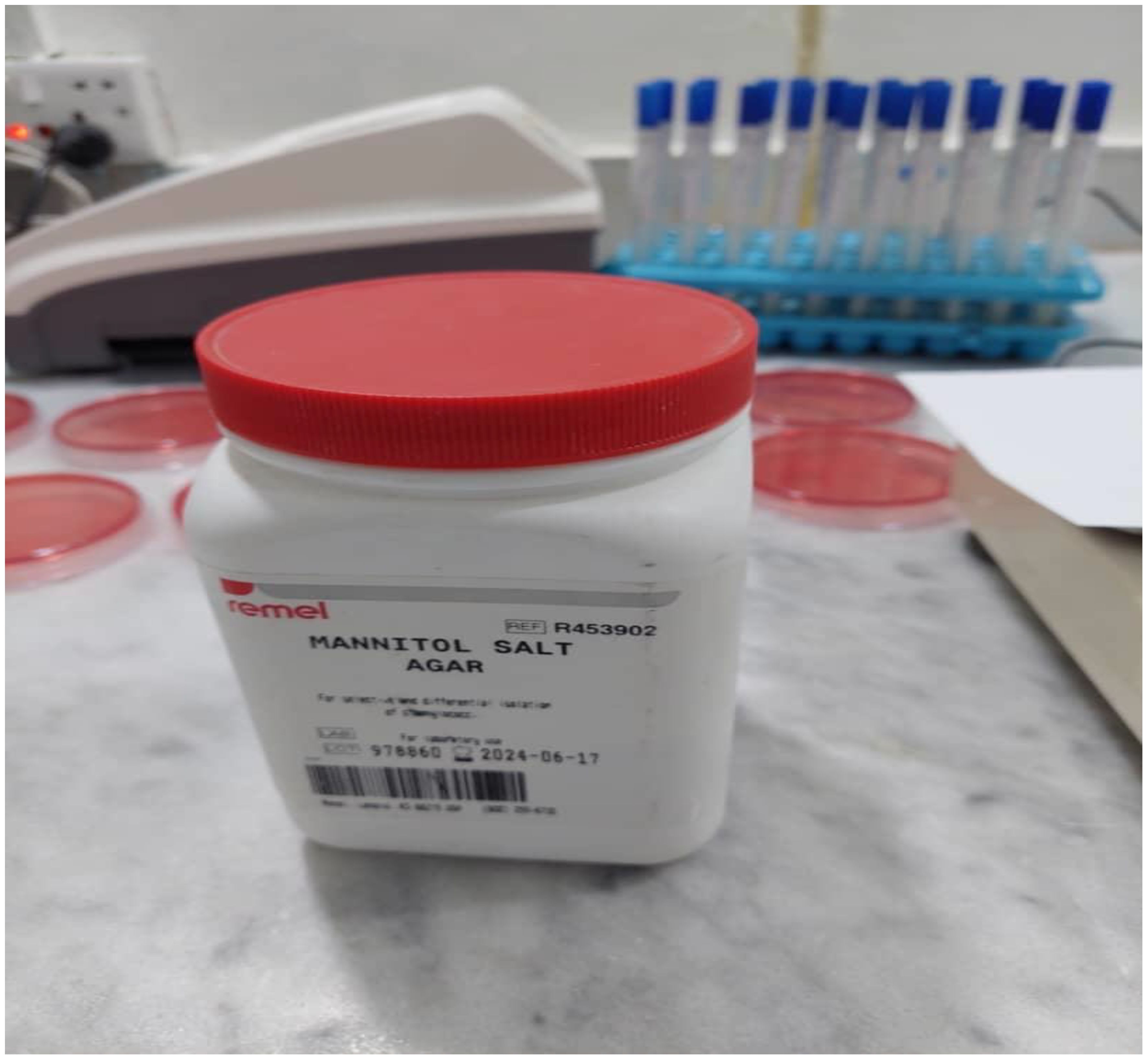
Figure 4. Mannitol salt agar for Staphylococcus aureus, selective and differential medium used to isolate and identify Staphylococcus aureus and collected swab from nasal.
Colonies suspected to be Staphylococcus aureus underwent further testing: a catalase test (positive for bubbles), a coagulase test (positive for clot formation), a DNAse test (positive for DNA hydrolysis), and Gram staining (revealing Gram-positive cocci in clusters).
The presence of MRSA was determined using the cefoxitin disk diffusion test. Mueller-Hinton agar was inoculated with a bacterial suspension, a cefoxitin (30 µg) disc was placed on the agar, and the plate was incubated at 35°C for 24 hours. Zone diameters were measured; ≥ 22 mm indicated methicillin-sensitive S. aureus (MSSA), while ≤ 21 mm indicated MRSA.
Antimicrobial susceptibility testing followed the standard Kirby-Bauer disk diffusion method, adhering to Clinical and Laboratory Standards Institute (CLSI) guidelines (Figure 7). A bacterial suspension was inoculated onto Mueller-Hinton agar, antibiotic discs were applied, and plates were incubated at 35°C for 24 hours. Zones of inhibition were measured and interpreted according to CLSI standards(M100 Performance Standards for Antimicrobial Susceptibility Testing, 31st Edition).
Data analysis was performed using SPSS software (version 25). Descriptive statistics (frequencies, percentages, and means) summarized the data, and the chi-square test (p < 0.05) assessed associations between categorical variables.
Of the 215 samples, 63 (29%) were S. aureus positive, and of these, 51 (81%) and 12 (19%) were MRSA and MSSA, respectively.
The results in Table 1 show that of the participants, 51 (23.7%) were MRSA carriers, while 164 (76.3%) were non-carriers. Of the MRSA carriers, 39 (25.8%) were females and 12 (18.7%) were male. Participants in the <30 age group accounted for the highest percentages (25.7% and 5.8%, respectively) of MRSA and MSSA carriers. Most participants (94.9%) were university-educated and of these, 24% were MRSA carriers. MRSA was also more common in female participants. However, further analysis may be needed to better understand the implications of these associations.
Table 2 shows the participants’ S. aureus methicillin sensitivity results. Of the doctors, seven (11%) had MRSA and two (22.2%) had MSSA. Of the nurses, 29 (46%) had MRSA, and three (9.4%) had MSSA. One (50.0%) medical laboratory technologist had MRSA and one (50.0%) had MSSA. Of the midwives, 11 (84.6%) had MRSA, and two (15.4%) had MSSA. Of the medical clerks, one (100.0%) had MSSA. Of the anesthesiologists, two (66.7%) had MRSA and one (33.3%) had MSSA. The pharmacist (n=1, 100.0%) had MSSA. There was a statistically significant difference between the various occupations (p = 0.047).
Both erythromycin and clindamycin had resistance and sensitivity rates of 38.1% and 61.9%, respectively (Table 3). Cotrimoxazole had a resistance of 22.2% and a sensitivity of 77.8%. For ciprofloxacin, the resistance and sensitivity rates were 60.3% and 39.7%, respectively. Gentamicin had a resistance of 27.0% and a sensitivity of 73.0%. Doxycycline had the lowest resistance rate (12.7%, sensitivity: 87.3%). Notably, all tested cases were sensitive to vancomycin and linezolid, indicating that these antibiotics were 100% effective against S. aureus infections.
It is crucial to identify MRSA nasal carriage in hospital HCWs, particularly those working in critical care areas. These individuals can potentially spread infection to immunocompromised patients, which can prolong hospitalization (2, 29). This study’s main objective was to determine the prevalence of MRSA nasal carriage among HCWs in defense departments at Banadir Hospital. Globally, MRSA infection rates range from 13% to 74%, with the prevalence in Europe ranging from 0.9% to 56%. As per the Centers for Disease Control, in the U.S., MRSA is responsible for about 50% of the ICU S. aureus nosocomial infection cases (7).
Of the 215 samples, 51 (23.70%) and 12 (5.60%) were positive for MRSA and MSSA, respectively (total number of S. aureus isolates: 63). The number of samples without MRSA (the sum of the MSSA rate and the rate of samples without S. aureus) was 164/215 (76.3%).
In this study, among HCWs, the MRSA nasal carriage rate was 23.7% (51/215) and the MSSA prevalence rate was 5.6% (12/215). However, previous research has reported different MRSA nasal carriage prevalence rates in HCWs, ranging from 5.3% to 15.6%. Previous studies reported very similar findings for South-Western Uganda (28.8%) (30), Northeast Ethiopia (28.8%) (31), and the Gaza Strip (25.5%) (2). However, studies have reported different S. aureus nasal carriage prevalence rates in HCWs from various regions, such as 41.9% in Central Uganda, 18.3% in Kenya, 28.8% in Ethiopia, 64% in Nigeria, 31% in Iran and Palestine, 47.6% in Iraq, and 22% in India (Akujobi, Egwuatu, & Ezeanya, 2013; Askarian, Zeinalzadeh, &Japoni, 2009; Kateete et al., 2011; Nabil, Ali Al Laham, & Ayesh, 2017; Omuse, Kariuki, & Revathi, 2012; Shibabaw, Abebe, & Mihret, 2013; VaidyaRutvi, Sangeeta, Sima, & Piyush, 2016). This variability is attributable to S. aureus levels in the environments where the studies took place, such as the disparity between Central and Western Uganda (30, 32). Various factors contribute to the high nasal MRSA carrier prevalence among HCWs, including inadequate compliance with hand hygiene protocols, antibiotic overuse, and insufficient infection prevention and control measures (9, 32, 33).
Participant demographic data provide frequencies of various characteristics of survey respondents. Of the respondents, 64 (29.8%) identified as male and 151 (70.2%) as female. A total of 171 (79.5%) respondents were aged <30 years, 41 (19.1%) 31–50 years, and 3 (1.4%) >51 years. Of the respondents, 62 (28.8%) were married, 150 (69.8%) were single, and 3 (1.4%) were divorced. MRSA was isolated from 12 (18.8%) of the male participants and 39 (25.9%) of the female participants. However, 52 (81.3%) and 112 (74.2%) of the male and female participants, respectively, did not have MRSA. MRSA prevalence was highest in the <30 years age group (44 cases, 25.7%), followed by the 31–50 years age group (four cases, 13.3%), and the >51 years age group (three cases, 21.4%). In total, 51 MRSA cases were identified among the HCWs. Further analysis of the data may reveal possible correlations between age and MRSA infection risk or other factors that may contribute to MRSA spread in hospital settings. It is also important to note that the sample size (215 HCWs) may not be representative of the entire HCW population at Banadir Hospital. Therefore, a study involving a larger sample size might obtain more reliable MRSA infection rate estimates among HCWs at the hospital (12, 30).
Although the proportion of MRSA cases appears higher in those aged <30 years when compared with those aged 31–50 years and >51, the MRSA rates across the age groups may not be statistically significantly different because of the small sample sizes. Overall, MSSA cases were few, and there were none in the oldest age group. MRSA rates appear to differ statistically significantly between doctors and nurses, with doctors having a lower proportion of MRSA cases when compared with nurses (77.8% vs 90.6%, p = 0.047). However, because of the small sample sizes for some occupations, such as med clerks and pharmacists, whose sample sizes were only one per group, and med lab technologists, who had equal MRSA and MSSA rates but only two cases overall, it is difficult to draw conclusions about the relationship between occupation and MRSA/MSSA rates. Although the data suggest that midwives and anesthesiologists had a higher proportion of MRSA cases when compared with MSSA, larger sample sizes are needed to determine if these differences are statistically significant (13, 14, 28, 31).
The data suggest that MRSA isolation rates vary significantly across departments and wards (Table 4). Ward 16 (postnatal and neonatal ICU) had the highest number of MRSA isolates, probably because of factors like vulnerable newborn immune systems and the high interaction between patients and healthcare providers in these areas (15, 17, 18, 29). Pediatric ward 23 also had a significant number of MRSA cases, possibly because of close patient proximity and the increased cross-infection risk in confined spaces. To identify areas of concern and implement targeted infection control, healthcare facilities should track and analyze MRSA rates by department or ward. However, this simple analysis does not consider any confounding factors, and other variables may need to be considered when analyzing the relationship between MRSA and departments. A more thorough analysis would require statistical tests to determine whether there is a significant association between MRSA and departments (16, 19, 32).
The data suggests that being under antibiotics may significantly affect bacterial resistance since all participants under antibiotics were resistant to the bacteria being tested. However, further research may be needed to determine this trend’s consistency and identify the specific factors that contribute to this phenomenon. Additionally, the high resistance rate in participants who were not under antibiotics suggests that antibiotic resistance may be a widespread issue that requires attention and intervention (20, 21, 27, 33). The data revealed that resistance was highest for methicillin (81%), followed by ciprofloxacin, erythromycin, and clindamycin, each with rates of 38.1% to 60.3%. The bacteria samples exhibited 100% sensitivity rates to vancomycin and linezolid, indicating that these antibiotics are effective against the bacteria in this population. In comparison, resistance to gentamicin and cotrimoxazole was less common (27% and 22.2%, respectively), while resistance to doxycycline was least frequent (12.7%). This highlights the significance of antibiotic resistance and the need for appropriate and rational antibiotic use (22, 23). To slow the spread of antibiotic resistance, effective antibiotic stewardship is critical, including prudent antimicrobial use and infection control measures (25, 26, 34).
Although this study involved Banadir Hospital only, it should be emphasized that it is a referral hospital that serves the largest population in Mogadishu, Somalia (24). Furthermore, this study is the first active survey in decades, given that we primarily aimed to evaluate MRSA prevalence among HCWs.
The MRSA nasal carriage rate was high among HCWs, which requires applicable preventive measures.
The study’s limited sample size may have affected the accuracy of the prevalence detected in the population. Furthermore, the screening methods used to detect isolates were not highly sensitive, and there was a risk of obtaining false negative results.
To minimize MRSA spread, the adoption of various infection control measures, such as enforcing contact precautions, handwashing/hand rub protocols, active surveillance, promptly reporting MRSA laboratory results, and HCW education, training, and regular screening for relevant infections, is recommended.
The original contributions presented in the study are publicly available. This data can be found here: https://data.mendeley.com/datasets/ygp79kbcp4/1.
AA: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Writing – original draft. HG: Supervision, Writing – review & editing. DI: Supervision, Validation, Writing – review & editing. GH: Formal analysis, Methodology, Validation, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to thank all the healthcare workers who participated in this study and Banadir Hospital staff for their support. The authors also wish to acknowledge Timothy Kiprotich Kimutai and Hafsa Abdulrizak Ahmed for their efforts in data cleaning and proofreading.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. WHO. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report. World Health Organization (WHO). (2022).
2. El Aila NA, Al Laham NA, Ayesh BM. Nasal carriage of methicillin resistant Staphylococcus aureus among health care workers at Al Shifa hospital in Gaza Strip. BMC Infect Dis. (2017) 17:1–7. doi: 10.1186/s12879-016-2139-1
3. Siegel JD, Rhinehart E, Cic RNMPH, Jackson M, Brennan PJ, Bell M. Management of Organisms in Healthcare Settings Vol. 2006. . Atlanta, GA: Centers for Disease Control and Prevention (2017).
4. Directorate IC. State of Kuwait ministry of health infection control directorate guidelines for the control and prevention of meticillin resistant staphylococcus aureus (MRSA) in health care facilities. (2011).
6. Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. (2022) 399:629–55. doi: 10.1016/S0140-6736(21)02724-0
7. Adam KM, Abomughaid MM. Prevalence of methicillin-resistant Staphylococcus aureus in Saudi Arabia revisited: a meta-analysis. Open Public Heal J. (2018) 11:584–91. doi: 10.2174/1874944501811010584
8. Shaba AA. Vancomycin susceptibility patterns of methicillin resistant staphylococcus aureus isolates from wounds at Madina hospital in Mogadishu, Somalia. (2018).
9. Shibabaw A, Abebe T, Mihret A. Nasal carriage rate of methicillin resistant Staphylococcus aureus among Dessie Referral Hospital health care workers; Dessie, Northeast Ethiopia. Antimicrob Resist Infect Control. (2013) 2:25. doi: 10.1186/2047-2994-2-25
10. Walana W, Bobzah BP, Kuugbee ED, Acquah S, Ezekiel VK, Yabasin IB, et al. Staphylococcus aureus nasal carriage among healthcare workers, inpatients and caretakers in the Tamale Teaching Hospital, Ghana. Sci Afr. (2020) 8:e00325. doi: 10.1016/j.sciaf.2020.e00325
11. Mogere AW. Carriage Rate of Methicillin Resistant Staphylococcus Aureus among Health Care Workers at The Kenyatta National Hospital Requirement for the Award of the Degree of Master of Medicine in Internal Medicine, University Of Nairobi. (2015).
12. Unakal T, Aureus S. National Library (2023). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK441868/.
13. Bush LM. Staphylococcus aureus infections. Rahway, NJ, USA: Merck &, Co, Inc. (2023). Available at: https://www.merckmanuals.com/home/infections/bacterial-infections-gram-positive-bacteria/staphylococcus-aureus-infections (Accessed October 23, 2024).
14. Coia JE, Wilson JA, Bak A, Marsden GL, Shimonovich M, Brooks J, et al. Joint Healthcare Infection Society (HIS) and Infection Prevention Society (IPS) guidelines for the prevention and control of meticillin-resistant Staphylococcus aureus (MRSA) in healthcare facilities. J Hosp Infect. (2021) 118:S1–S39. doi: 10.1016/j.jhin.2021.09.022
15. Harkins CP, Pichon B, Doumith M, Parkhill J, Westh H, Tomasz A, et al. Methicillin-resistant Staphylococcus aureus emerged long before the introduction of methicillin into clinical practice. Genome Biol. (2017) 18:1–11. doi: 10.1186/s13059-017-1252-9
16. Deverick J, Anderson M. Methicillin-resistant Staphylococcus aureus (MRSA) in adults: epidemiology (2022). Available online at: https://www.uptodate.com/contents/methicillin-resistant-staphylococcus-aureus-mrsa-in-adults-epidemiology (Accessed October 23, 2024).
17. CDC. Methicillin-resistant Staphylococcus aureus (MRSA) (2019). Available online at: https://www.cdc.gov/mrsa/index.html (Accessed October 23, 2024).
18. Plipat N. Methicillin-resistant staphylococcus aureus (MRSA) exposure assessment in hospital environment. (2012).
20. Lowy FD. Antimicrobial resistance: the example of Staphylococcus aureus. J Clin Invest. (2003) 111:1265–73. doi: 10.1172/JCI18535
22. World Health Organization. Preventing surgical site infections: implementation approaches for evidence-based recommendations. (2018).
23. Noskin GA, Rubin RJ, Schentag JJ, Kluytmans J, Hedblom EC, Smulders M, et al. The burden of Staphylococcus aureus infections on hospitals in the United States: an analysis of the 2000 and 2001 Nationwide Inpatient Sample Database. Arch Intern Med. (2005). doi: 10.1001/archinte.165.15.1756
24. Stone PW. Economic burden of healthcare-associated infections: an American perspective. Expert Rev Pharmacoecon Outcomes Res. (2009) 9:417–22. doi: 10.1586/erp.09.53
26. Du P, Superieur C, Sante DELA. Avis Intermédiaire Version Provisoire Soumise aux Professionnels de Terrain (plateformes d ‘ hygiène hospitalière) en vue d ‘ une amélioration (planifiée pour mai 2018). (2018), 1–129.
27. Price JR, Cole K, Bexley A, Kostiou V, Eyre DW, Golubchik T, et al. Transmission of Staphylococcus aureus between health-care workers, the environment, and patients in an intensive care unit: a longitudinal cohort study based on whole-genome sequencing. Lancet Infect Dis. (2017) 17:207–14. doi: 10.1016/S1473-3099(16)30413-3
28. Cheesbrough M. District Tropical Practice in Laboratory Countries, 2nd ed. Cambridge: University Press. (2006). p. 442.
29. Sa M, Taha AA. Faculty of Graduate Studies Prevalence of Methicillin – Resistant Staphylococcus aureus Nasal Carriage among Patients and Healthcare Workers in Hemodialysis Centers in North West Bank- Palestine. (2010).
31. Joachim A, Moyo SJ, Nkinda L, Majigo M, Rugarabamu S, Mkashabani EG, et al. Nasal carriage of methicillin-resistant Staphylococcus aureus among health care workers in Tertiary and Regional Hospitals in Dar es Salam, Tanzania. Int J Microbiol. (2018) 2018:5058390. doi: 10.1155/2018/5058390
32. Emaneini M, Jabalameli F, Rahdar H. Review article nasal carriage rate of methicillin resistant Staphylococcus aureus among Iranian healthcare workers: a systematic review and meta-analysis. (2017) 50:590–7. doi: 10.1590/0037-8682-0534-2016
33. Raut S, Bajracharya K, Adhikari J, Pant SS, Adhikari B. Prevalence of methicillin resistant Staphylococcus aureus in Lumbini Medical College and Teaching Hospital, Palpa, Western Nepal. BMC Res Notes. (2017) 10:187. doi: 10.1186/s13104-017-2515-y
34. Hasanpour AH, Sepidarkish M, Mollalo A, Ardekani A, Almukhtar M. The global prevalence of methicillin – resistant Staphylococcus aureus colonization in residents of elderly care centers: a systematic review and meta – analysis. Antimicrob Resist Infect Control. (2023) 6:1–11. doi: 10.1186/s13756-023-01210-6
Keywords: nasal swabs, MRSA, HCW’s, prevalence, Banadir Hospital, Jazeera University, Kalkaal Hospital, Somalia
Citation: Aweis ADH, Ga’al H, Ishaq Aweis DM and Hassan GD (2025) Nasal carriage of methicillin-resistant Staphylococcus aureus in healthcare workers at Banadir Hospital, Mogadishu, Somalia. Front. Trop. Dis. 6:1425042. doi: 10.3389/fitd.2025.1425042
Received: 29 April 2024; Accepted: 06 January 2025;
Published: 28 February 2025.
Edited by:
Arshad Islam, Lady Reading Hospital Peshawar, PakistanReviewed by:
Juan Pablo Escalera-Antezana, Secretaria Municipal de Salud, BoliviaCopyright © 2025 Aweis, Ga’al, Ishaq Aweis and Hassan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdullah Dahir H. Aweis, YXdlaXMyMDE2QGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.