
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Trop. Dis. , 13 February 2025
Sec. Antimicrobial Resistance
Volume 5 - 2024 | https://doi.org/10.3389/fitd.2024.1497220
This article is part of the Research Topic Antimicrobial Resistance Response Perspectives in Africa View all 5 articles
 Nkatha Gitonga1*
Nkatha Gitonga1* Mitchel Okumu2
Mitchel Okumu2 Oscar Agoro3
Oscar Agoro3 Ndinda Kusu1
Ndinda Kusu1 Joseph Mukoko1
Joseph Mukoko1 Helen Wangai1
Helen Wangai1 Tamara Hafner4
Tamara Hafner4 Mohan P. Joshi4
Mohan P. Joshi4Background: Antimicrobial resistance (AMR) is a growing concern globally and is notably prevalent in Kenya. The World Health Organization (WHO) Global Action Plan (GAP) and the Kenya National Action Plan (NAP) on AMR emphasize the need for effective antimicrobial stewardship (AMS) programs to combat AMR. The USAID-funded Medicines, Technologies, and Pharmaceutical Services (MTaPS) program has supported AMS implementation in 20 healthcare facilities (HCFs) in Nyeri, Kisumu, Murang’a, and Kilifi counties since 2019, focusing on developing and operationalizing AMS programs based on national, WHO, and Centres for Disease Control and Prevention (CDC) guidelines. However, there is paucity of information on how the AMS programs have been implemented in Nyeri and Kisumu Counties. This study evaluates the progress in AMS program implementation in these two counties between 2019 and 2023.
Methods: Baseline and follow up assessments were conducted using a 33-item AMS questionnaire adapted from the CDC’s Core Elements of Hospital Antibiotic Stewardship Programs (CEHASP) and WHO guidelines. The assessment evaluated 13 thematic areas.
Results: AMS implementation showed significant improvements, with Nyeri county increasing from 12% to 76% and Kisumu from 17% to 78%. Several elements achieved 100% implementation in both counties, including core governance structures, accountability, and medical expertise. Education programs reached 88% implementation in Kisumu and 100% in Nyeri. Leadership support improved from 0% to 54% in Nyeri and from 0% to 60% in Kisumu. However, tracking antimicrobial use (AMU) and AMR through process measures remained the lowest implemented element (33% in Kisumu, 19% in Nyeri). Other challenges included limited microbiology services affecting antibiogram production, inadequate monitoring of adherence to treatment guidelines (0-7% implementation), and suboptimal implementation of policies and guidelines (48-58%).
Conclusions: These findings suggest that the implementation of antimicrobial stewardship programs (ASP) in resource-limited settings can be successful, as evidenced by the improvements in core governance, accountability, and medical expertise observed in the selected healthcare facilities. However, critical gaps remain in tracking antimicrobial use and resistance and monitoring treatment guideline adherence. To strengthen ASPs, we recommend establishing standardized national protocols for tracking and monitoring, developing regional laboratory networks to improve microbiology services access, and implementing electronic health records systems.
Rates of AMR have been increasing worldwide, and this picture is mirrored in Kenya (1, 2). The World Health Organization (WHO) released its Global Action Plan (GAP) to combat AMR in 2015, a key component of which is the development and implementation of antimicrobial stewardship (AMS) programs (ASPs) (3). In alignment with the GAP on AMR, the Kenyan National Action Plan on AMR (NAP-AMR), released in 2017 and revised in 2023, also emphasizes the need for optimal use of antimicrobials in human and animal health sectors (4). The NAP-AMR further recommends establishing ASPs in healthcare facilities (HCFs) to ensure prudent use of antimicrobials.
WHO released a practical toolkit for ASPs in HCFs in low and middle-income countries (LMICs) in 2019, which provides guidance on the stepwise approach of setting up ASPs (5). In addition, in the same year, the United States (US) Centers for Disease Control and Prevention (CDC) published a document on the Core Elements of Hospital Antibiotic Stewardship Programs (CEHASP), the document targets hospital settings, providing guidance on how to implement ASPs (6). The Kenyan National AMR Secretariat, in collaboration with its partners, developed the "National Antimicrobial Stewardship Guidelines for Health Care Settings" in 2020, outlining AMS interventions for optimizing antimicrobial use at different HCF levels in Kenya (7). These guidelines advocate for the leadership of medicine and therapeutics committees (MTCs), which work to ensure patient safety, optimal treatment outcomes, and reduced treatment costs.
The US Agency for International Development (USAID) Medicines, Technologies, and Pharmaceutical Services (MTaPS) program supported the government with AMS guideline implementation in 20 HCFs across four counties, that is, in Nyeri (8 HCFs) and Kisumu (7 HCFs) from 2019 to 2023, and in Murang'a (2 HCFs) and Kilifi (3 HCFs) from 2021 to 2024. The support included the establishment and operationalization of their governance mechanisms, capacity building and development through provision of training, supportive supervision, and mentorship for the facility MTCs and AMS committees and teams, as well as providing assistance with monitoring and evaluating (M&E) of ASPs. The WHO toolkit, CEHASP, and the Kenya National AMS Guidelines all recommend that the HCFs set up systems to measure AMS activities. In this paper, we present the status of ASP implementation across fifteen facilities in Kisumu and Nyeri counties, where MTaPS support concluded in 2023.
A 33-item AMS questionnaire was developed to assess the implementation of AMS programs. The questionnaire was adapted from the CDC CEHASP tool, with modifications made to suit the local context of Kenyan HCFs. The questionnaire comprised 33 questions spanning 13 thematic areas: core governance structures, MTC governance, AMS governance, leadership support, accountability, medicines expertise, key support for the AMS program, actions to improve optimal antimicrobial use (AMU) through policy and guidelines, actions to improve optimal AMU through interventions, tracking and monitoring AMU and AMR with process measures, tracking and monitoring AMU and AMR with outcome measures, reporting information, and education. Additionally, several process indicators of AMU from the WHO toolkit were included. The questionnaire included both closed (31) and open-ended questions (2) (Annex 1). The closed-ended questions were scored as 1, 0.5, or 0 corresponding to yes/completed, in progress, or no/not started, respectively, with higher scores indicating better adherence. An abbreviated version of the questionnaire was administered to facilities not providing inpatient services, specifically level 3 HCFs. The facilities were assessed across the thirteen thematic areas.
A three-part training program was used to equip the MTC and AMS committee members with essential knowledge and skills for AMS implementation. Training materials covered establishing MTCs and AMS programs, prescription reviews, developing AMS policies, guidelines, treatment protocols, and AWaRe categorization (Access, Watch, and Reserve categories for antibiotics).
Each facility created a facility-based continuous quality improvement (CQI) action plan, guided by the findings from the baseline AMS assessment, and outlined the steps for implementing AMS interventions. These action plans were based on the National AMS Guidelines and included strategies for monitoring antimicrobial use and improving AMS practices over the course of one year.
Quarterly monitoring and mentorship activities included the use of site visit reports, supportive supervision checklists, and on-the-job training materials to track the progress of AMS interventions. These tools were employed to ensure the ongoing implementation and evaluation of AMS programs at participating HCFs.
This study adopted a longitudinal study design to evaluate the implementation of AMS programs in selected HCFs in Kenya. The study was conducted in two phases: a baseline assessment in 2019 and a follow-up assessment in 2023. The longitudinal design was selected as it would enable the evaluation of changes in AMS implementation over a four-year period. Data were collected using a quantitative approach through a 33-item questionnaire adapted from the CDC’s CEHASP and WHO toolkit, focusing on 13 thematic areas related to AMS practices. The study was conducted in two counties in Kenya: Nyeri and Kisumu, both of which were supported by the USAID MTaPS program in their efforts to implement AMS programs between 2019 and 2023. The healthcare facilities selected for the study included faith-based organizations, public and private institutions, ensuring a diverse sample that represents the challenges faced in various healthcare settings across the country.
Seven HCFs were supported in Kisumu County, including six public hospitals and one faith-based organization (FBO), representing six of the seven sub-counties. Eight HCFs in Nyeri County were supported, including six public hospitals, one FBO and one private hospital, representing six of the eight sub-counties. Key AMS interventions were determined based on the baseline assessment and designed using the National AMS Guidelines and were outlined in the one-year AMS CQI action plans. The facilities systematically implemented the interventions using the CQI approach. The MTC and AMS committee members participated in a three-part training program focused on key AMS activities such as prescription reviews; developing AMS policies, guidelines, and treatment protocols; and implementing AWaRe categorization. Following the training and the development of the facility-based CQI action plan, on-site technical and financial support was offered to the facilities to implement and monitor their AMS interventions. The key interventions implemented across the facilities included cascade training for healthcare workers, patient sensitizations, antimicrobial consumption and use data generation and analysis, antibiotic restrictions based on AWaRe categorization, implementation of AMS ward rounds, and prescription reviews, among others. The facilities were monitored and mentored on a quarterly basis through activities that included supportive supervision and mentorship site visits, and on-the-job training on how to conduct these key AMS interventions and actions.
A baseline assessment of AMS implementation in July 2019 in the selected HCFs was done in conjunction with the County leadership and AMS focal persons in Nyeri and Kisumu counties. The service level of HCFs included county referral hospitals (level 5), sub-county hospitals (level 4), and health centers (level 3) (Table 1). It is noteworthy that one health centre in Nyeri County was upgraded to a sub-county hospital after the implementation was completed. Table 1 is a summary of the MTaPS supported facilities in the study areas.
A progress review was conducted in October 2023 in Kisumu County and in October/November 2023 in Nyeri County to evaluate the status of ASP institutionalization in these HCFs (Table 1). Similar assessments were planned for Murang’a and Kilifi counties in 2024 at the conclusion of MTaPS’ support for these counties.
Microsoft Excel™ 2021 was used to tabulate the responses and compute descriptive statistics to compare changes between baseline and at progress review. Based on the scoring parameters, each facility was awarded a score out of 48 for level 4-5 healthcare facilities and 40 for level 3 facilities. Data was summarized using descriptive statistics on Microsoft Excel™ 2021. Additionally, identified themes from the open-ended responses provided further context to the quantitative findings.
We examined the overall implementation across all the facilities as an average and across all assessed AMS elements. In Nyeri county, 12% of the AMS elements were implemented at baseline in 2019 compared to 76% at progress review in 2023. Kisumu county showed similar improvements, increasing implementation of AMS elements from 17% in 2019 at baseline to 78% at the progress review in 2023. Below we describe the findings in more detail for each county.
Figure 1 is a description of the progress in the implementation of the 13 AMS elements in Nyeri County between baseline (2019) and at progress review (2023).
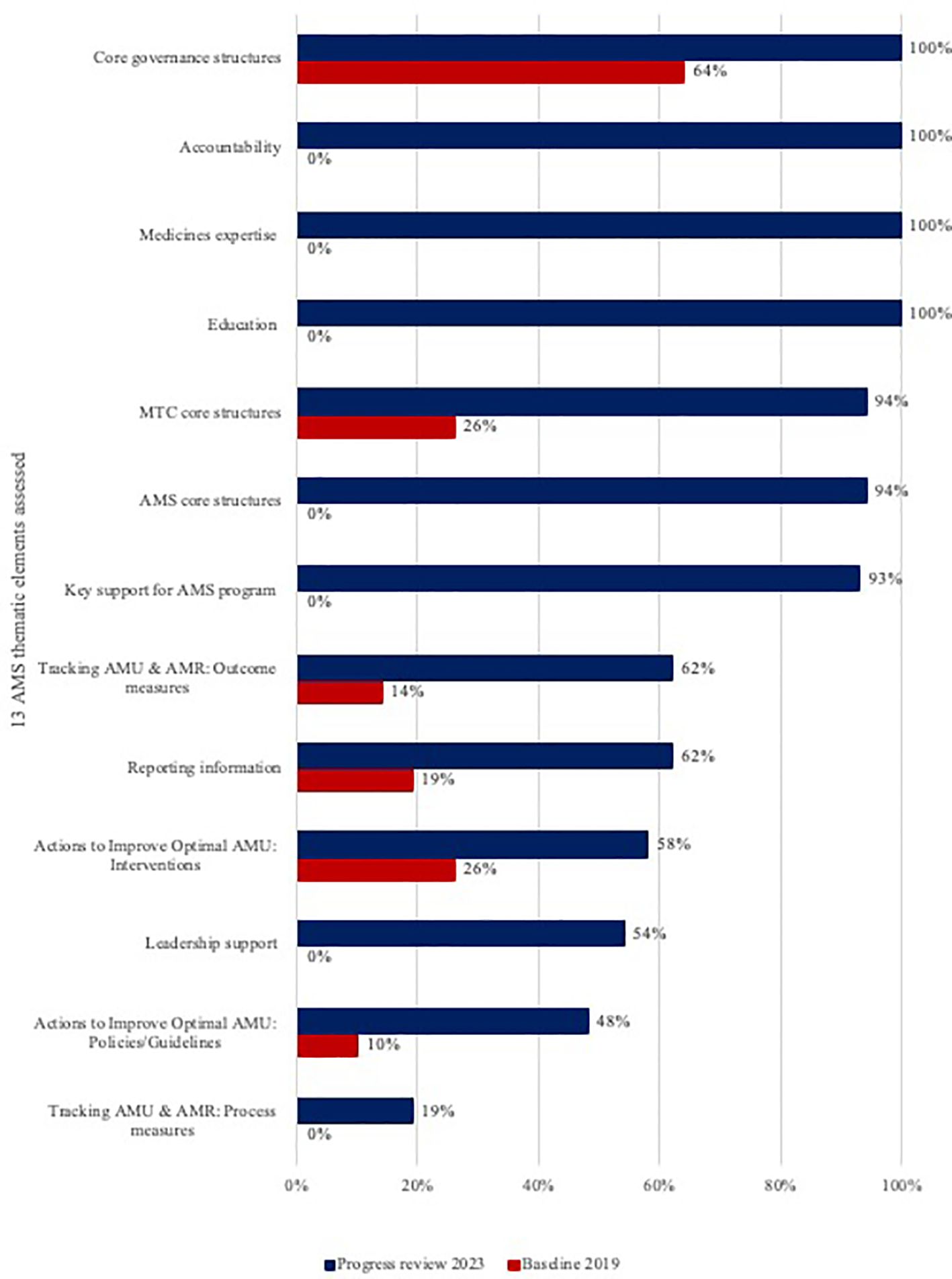
Figure 1. Progress in implementation of the thirteen AMS elements in Nyeri County from baseline (2019) to progress review (2023).
Seven of the 13 elements —AMS core structures, leadership support, accountability, key support for AMS program, medical expertise, tracking AMU and AMR through process measures, and education— had 0% implementation (Figure 1). By the progress review in 2023, 100% implementation was observed for core governance structures, accountability, medical expertise, and education. Key support for AMS program, MTC core structures, and AMS core structures recorded a score of over 90%. Notably, leadership support and tracking AMU and AMR through process, which both had 0% implementation at baseline, improved to 54% and 19%, respectively. Tracking AMU and AMR through process measures (19% implementation), and actions to improve optimal AMU through policies and guidelines (48% implementation) were the least implemented elements.
Table 2 shows disaggregation of the areas assessed that recorded the least implementation and the number of facilities in Nyeri County that implemented the specific AMS element.

Table 2. Disaggregation of specific areas assessed within the least implemented core AMS elements and the number of facilities implementing these areas for Nyeri county.
In Kisumu County at baseline, six of the 13 elements —AMS core structures, leadership support, accountability, key support for AMS program, medical expertise, and tracking AMU and AMR through process measures — had 0% implementation at baseline (Figure 2). There was 100% implementation for five of the thirteen elements by 2023. These elements included core governance structures, MTC core structures, AMS core structures, accountability, and medical expertise. Key support for AMS program and education achieved 92% and 88% implementation, respectively in the same period. Moreover, leadership support and tracking AMU and AMR through process improved to 60% and 33% at the time of progress review up from 0% at baseline.
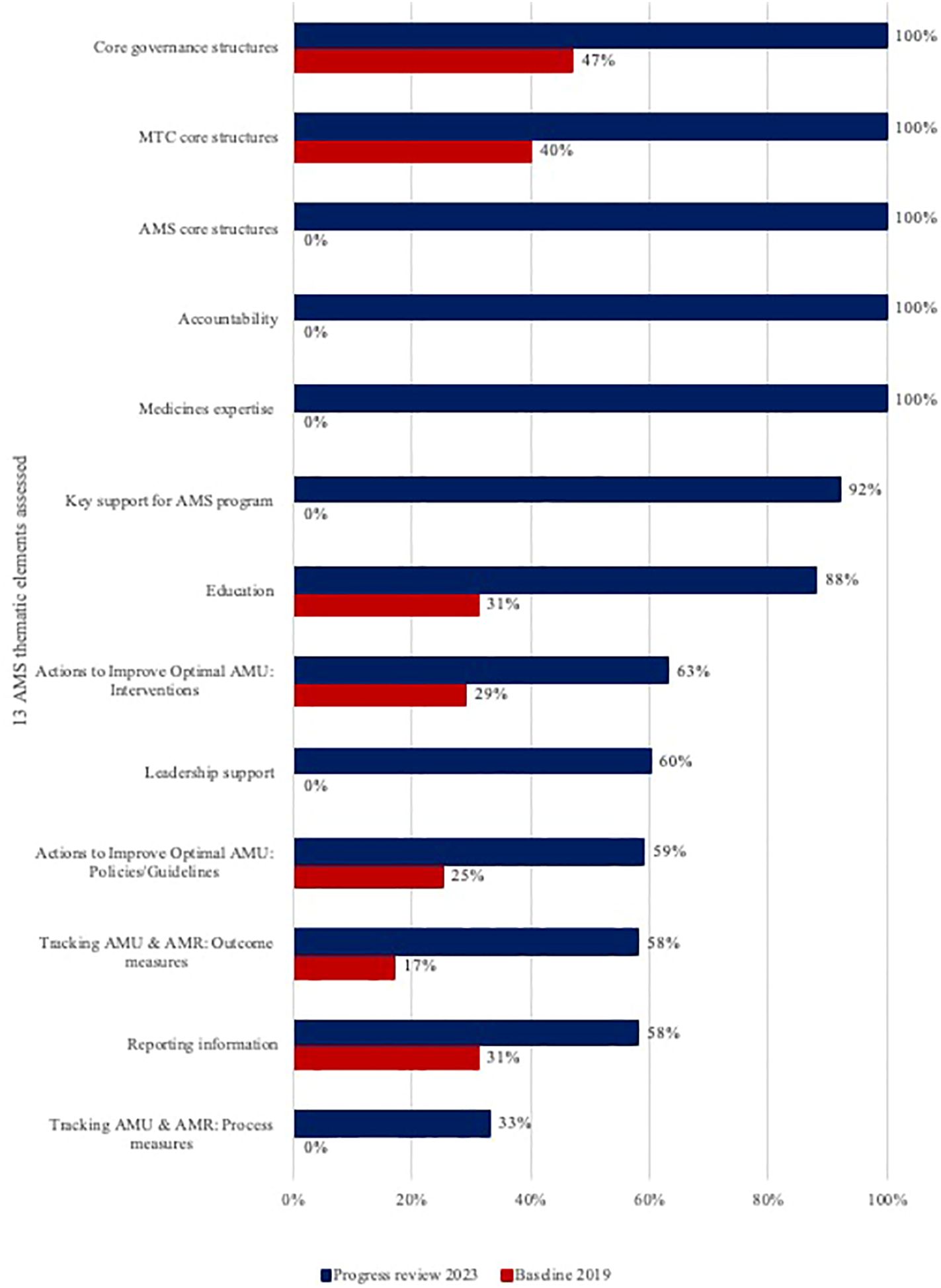
Figure 2. Progress in implementation of the thirteen AMS elements in Kisumu County from baseline (2019) to progress review (2023).
Similar to Nyeri County, Kisumu county also showed that the least implemented element was tracking AMU and AMR through process measures (33% implementation). In Kisumu, the next least implemented elements were tracking AMU and AMR through outcome measures and reporting information, both with implementation rates of 58% (see Table 3).
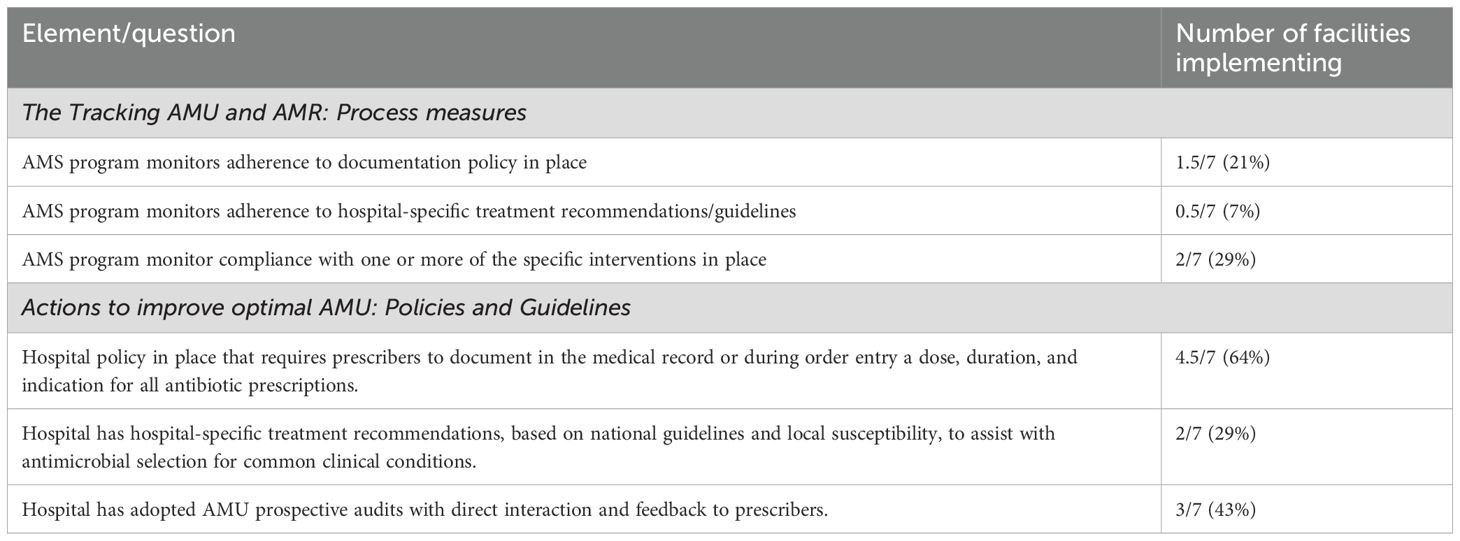
Table 3. Disaggregation of specific areas assessed within the least implemented core AMS elements and the number of facilities implementing these areas for Kisumu County.
Aggregated data from the two counties revealed that the least implemented elements were tracking AMR and AMU through process measures (26%). This low implementation rate likely reflects systemic challenges within healthcare facilities, such as inadequate resources and a lack of standardized data collection and reporting protocols. This underscores the need for targeted interventions and support. The challenges are expected, as effective tracking and reporting of AMU and AMR require substantial investment in IT infrastructure and time for technical experts. Additionally, collecting detailed data on antimicrobial prescriptions, consumption, and resistance patterns is both complex and resource intensive.
The AMS assessments explored here provides an implementation progress of ASPs in the MTaPS focus facilities in two counties (Nyeri and Kisumu) in Kenya, from the baseline conducted in July 2019 to the progress review conducted between October-November 2023 (4-year implementation period). The participating facilities represent different regions in Kenya, various service delivery levels and ownership.
Interventions to track AMR and AMU were the least implemented across HCFs in the two counties. Specifically, monitoring adherence to policies on documentation and adherence to hospital-specific treatment recommendations/guidelines was inadequately done. In addition, in Nyeri County, no antibiograms were developed and distributed, and in Kisumu County, there was inadequate development and adoption of hospital-specific treatment recommendations to assist with antimicrobial selection for common clinical conditions.
Possible reasons include inadequate data collection and management capacity in health facilities characterized by limited technical capacity, competing tasks for officers, and paper-based data management systems. In addition, the lack of standardized data collection and reporting systems, and the fact that HCFs are not mandated to report on AMS intervention indicators led to reduced motivation for AMS and AMR data collection and use. Corrective interventions to improve the collection and use of data on AMU and AMR should be embedded in CQI plans specific to each health facility. System-level interventions to develop and roll out standardized reporting systems and to mandate the reporting of key AMU and AMR indicators should be put in place. More advocacy and engagement of stakeholders should be conducted to ensure continued investment in AMU and AMR data management and use systems.
Commendably, the findings revealed that all facilities had in place core governance structures, including the presence of functional MTCs and AMS committees, accountability for AMS, and medical expertise. Only two facilities obtained lower scores on the functionality of their MTCs and AMS committees due to lack of appointment letters with terms of reference issued to their new members. Furthermore, the findings highlight commendable efforts by HCFs in implementing interventions across all 13 assessed thematic areas, as evidenced by improvements in each area compared to baseline findings.
The findings reveal that several ASP elements remain inadequately implemented in hospitals. The analysis highlights which elements need focused efforts for improvement. Tracking AMR and AMU through process measures—such as monitoring adherence to policies on documentation and hospital-specific treatment guidelines—emerged as the weakest performer. This poor performance is likely exacerbated by the absence of these specific local and national policies and updated treatment guidelines. Compounding this issue is the sub-optimal implementation of actions to improve AMU through policies and guidelines, which include medical documentation, treatment recommendations, and prospective audits of AMU.
Even facilities with existing policies and guidelines struggled with tracking and monitoring, likely due to the lack of national or county mandates for reporting and monitoring, leading to reduced commitment and buy-in from healthcare facilities. However, within the action to improve AMU, many focused HCFs successfully implemented prospective audits, highlighting their value as demonstrated in previous studies (8–10). Despite this notable progress from the focus HCFs, institutionalization and a wider national rollout of these audits is necessary for larger benefits.
Tracking AMU and AMR through outcome measures also performed poorly, primarily due to the lack of microbiology services in most facilities, which impeded antimicrobial susceptibility testing (ASTs) and the production of antibiograms. While level 5 facilities had microbiology services, low utilization also limited their ability to produce antibiograms.
Despite these challenges, notable improvements from baseline findings were observed. Resource mobilization remains a pervasive issue affecting all assessed elements and their implementation. Similar issues with the least performing elements have been reported in other studies (11–13). To ensure optimal ASP implementation, challenges such as complex data collection, financial constraints, and institutional resistance must be addressed. The absence of standardized national and county protocols, policies, and treatment guidelines further complicates matters. Adopting or adapting these standards could alleviate the burden on individual HCFs, enhancing consistency and improving antimicrobial prescription quality (14). Additionally, integrating ASP tracking and monitoring actions into existing IT systems could minimize workflow disruptions. Effective tracking of adherence to ASP interventions allows facilities to identify compliance gaps and focus efforts on mitigating these issues.
Some encouraging findings were noted including leadership commitment, implementation of interventions to improve AMU, and enhanced support for AMS programs, all of which were either not present at baseline or very weak. Additionally, the HCFs were found to have implemented regular sessions to educate prescribers and healthcare workers on AMS, AMR and infection prevention and control practices. These improvements, including the ones earlier mentioned, place the HCFs on a strong footing for acceleration to achieving full implementation of all ASP elements.
How do these findings compare to what is observed elsewhere in Sub-Saharan Africa? A study by Abejew et al. (2024) assessed the challenges and opportunities in antibiotic stewardship program implementation in NorthWest Ethiopia and reported that the status of ASP in hospitals was very poor. The study also observed that despite a lack of prior knowledge of ASPs, most participants did have a positive perception of AMR and the implementation of ASPs (15). Alabi et al. (2022) evaluated the effect of AMS measures in South-East Liberia on the quality of antimicrobial use in three regional hospitals and reported that adherence to local guidelines improved the selection of antimicrobial agents, following implementation of AMS ward rounds and improved microbiological analysis, which in turn reduced the rate of Ceftriaxone use (16).
The findings of these assessments, show great promise for implementing ASPs in LMICs and resource-limited HCFs. All elements assessed demonstrated implementation progress from the baseline findings. This provides the country, counties, and the HCFs with vital information on the areas of focus for the next years of implementation. The results show that there is commitment towards AMR containment efforts through the establishment of functional HCF ASPs and an increase in education and knowledge of AMR and AMS practices. Furthermore, findings from other regions in the continent shows the importance of developing local guidelines, implementing core AMS actions and investing in microbiology to support the prudent use of antimicrobials. These findings also underscore the need for coordinated cross-national policy strategies to address AMR.
The assessments provide a blueprint for other HCFs in similar settings, on what the low-hanging fruits for ASP implementation are and provide guidance on what areas may require more diligent planning for quicker implementation of required actions. It is evident that setting up robust tracking and monitoring of ASP implementation progress and outcomes is essential and should therefore be a priority at national and county levels. In addition, the lack of microbiology services in the HCFs to conduct ASTs is another area that will require focus, with counties exploring sample referral mechanisms within their counties to leverage off the services offered in higher-level facilities. The national team will need to look at developing standardized prospective audit tools and mandating these to be conducted across the country. It is also important to explore avenues for shifting documentation from manual to electronic systems this will support incorporating some AMS interventions within the system, encourage rollout of key AMS interventions in all clinical settings, and simplify monitoring and tracking exercises. Furthermore, as the sample size included in this study was small, the national team should aim at duplicating and extending similar studies across the country to monitor ASP implementation. Cross-country studies will support the acceleration of effective ASP implementation to mitigate AMR and provide local evidence to inform national strategies. Finally, these findings demonstrate implementation of the country’s NAP-AMR and the National AMS Guidelines.
The sample size analysed was small (15 HCFs) compared to the over 10,000 facilities in the country. The participating facilities that represented FBO and private ownership were minimal in comparison to the public HCFs, which prevented sub-analysis of AMS implementation by facility-ownership. The data only speaks to findings from HCFs in 2 out of the 47 counties in the country. However, these findings provide a first look at the achievement and gaps associated with operationalizing ASPs in HCFs in Kenya, in the facilities supported by USAID MTaPS.
This paper provides a detailed account of AMS program implementation in select facilities in Kenya, based on the assessments conducted in 2019 and 2023, using a pre-designed AMS assessment tool incorporating CDC core elements and WHO guidelines. The facilities showed progress in implementing the core AMS elements from baseline; however, the findings did reveal that not all elements were fully implemented at the end-term. The report highlights key strengths such as leadership commitment; the existence of core governance structures, including MTCs and AMS committees; accountability and medical expertise for ASPs; and the provision of education to healthcare workers. Some gaps were identified, including sub-optimal tracking, monitoring, and evaluating of AMS interventions and program outcomes, and inadequate implementation of some key AMS actions aimed at improving antimicrobial use.
The results provide the country with crucial information on the areas that require emphasis and coordinated effort to ensure ASP implementation, including securing financial support for the programs, digitalization of health systems, increasing access to and availability of microbiology services, and setting up well-structured and comprehensive tracking systems to monitor AMS interventions and program outcomes. The successes of the ASPs in the HCFs reported here can be attributed to leadership commitment at national, sub-national, and HCF levels, accountability, and collaboration among stakeholders. Monitoring ASP progress is an essential component that supports the review and evaluation of the country’s NAP-AMR and in setting priorities for the national and sub-national ASP efforts.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
NG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. OA: Data curation, Investigation, Methodology, Writing – review & editing. MO: Data curation, Investigation, Methodology, Writing – review & editing. NK: Methodology, Project administration, Resources, Supervision, Writing – review & editing. JM: Methodology, Project administration, Writing – review & editing. HW: Methodology, Project administration, Writing – review & editing. TH: Writing – review & editing. MJ: Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the US Agency for International Development (USAID) under contract number (7200AA18C00074). The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the US Government. The funder had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript.
The authors gratefully acknowledge the healthcare facility teams in Nyeri and Kisumu for their dedication to implementing antimicrobial stewardship programs and for their valuable support and participation in this study. We also extend our appreciation to Kenya’s Ministry of Health and the respective County governments and health departments for their continued support.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Murray CJ, Ikuta KS, Sharara F, Swetschinski L, Aguilar GR. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. (2022) 399:629–55. doi: 10.1016/S0140-6736(21)02724-0
2. Government of Kenya. National Antimicrobial Resistance Surveillance Report, 2023. National Antimicrobial Stewardship Interagency Committee Secretariat (2023).
3. World Health Organization. Global Action Plan on Antimicrobial Resistance (2015). Available online at: https://www.who.int/publications/i/item/9789241509763 (Accessed January 17, 2024).
4. Government of Kenya. National Action Plan on Prevention and Containment of Antimicrobial Resistance, 2023-2027. Nairobi (2023). Available at: https://www.afro.who.int/publications/national-action-plan-prevention-and-containment-antimicrobial-resistance-2017-2022 (Accessed January 17, 2024).
5. World Health Organization. Antimicrobial stewardship programmes in health-care facilities in low- and middle-income countries. A practical toolkit (2019). Available online at: https://iris.who.int/bitstream/handle/10665/329404/9789241515481-eng.pdf?sequence=1 (Accessed January 17, 2024).
6. Centers Disease Control, Prevention. Core Elements of Hospital Antibiotic Stewardship Programs (2019). Available online at: https://www.cdc.gov/antibiotic-use/healthcare/pdfs/hospital-core-elements-H.pdf (Accessed January 17, 2024).
7. Ministry of Health. National Antimicrobial Stewardship: Guidelines for Health Care settings (2020). Available online at: https://www.momanyink.com/wp-content/uploads/2020/07/National-AMS-Guidelines-for-Healthcare-Settings-in-Kenya.pdf (Accessed January 17, 2024).
8. Okoth C, Opanga S, Okalebo F, Oluka M, Kurdi AB, Godman B. Point prevalence survey of antibiotic use and resistance at a referral hospital in Kenya: findings and implications. Hosp Pract. (2018) 46:128–36. doi: 10.1080/21548331.2018.1464872
9. Maina M, Mwaniki P, Odira E, Kiko N, McKnight J, Schultsz C, et al. Antibiotic use in Kenyan public hospitals: Prevalence, appropriateness and link to guideline availability. Int J Infect Dis. (2020) 99:10–8. doi: 10.1016/j.ijid.2020.07.084
10. Versporten A, Zarb P, Caniaux I, Gros MF, Drapier N, Mille M. Global-PPS network. Lancet Glob Health. (2018) 6:619–29. doi: 10.1016/S2214-109X(18)30186-4
11. Raheem M, Anwaar S, Aziz Z, Raja SA, Saif-ur-Rehman N, Mubarak N. Adherence to the core elements of outpatient antibiotic stewardship: A cross-sectional survey in the tertiary care hospitals of Punjab, Pakistan. Infect Drug Resist. (2020) 13:3833–41. doi: 10.2147/IDR.S268574
12. Mubarak N, Khan AS, Zahid T, Ijaz UEB, Aziz MM, Khan R, et al. Assessment of adherence to the core elements of hospital antibiotic stewardship programs: A survey of the tertiary care hospitals in Punjab, Pakistan. Antibiotics. (2021) 10(8):906. doi: 10.3390/antibiotics10080906
13. Hassan SK, Dahmash EZ, Madi T, Tarawneh O, Jomhawi T, Alkhob W, et al. Four years after the implementation of antimicrobial stewardship program in Jordan: evaluation of program’s core elements. Front Public Health. (2023) 11. doi: 10.3389/fpubh.2023.1078596
14. Shrestha J, Zahra F, Cannady PJ. Antimicrobial Stewardship (2023). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK572068/.
15. Abejew AA, Wubetu GY, Fenta TG. Assessment of challenges and opportunities in antibiotic stewardship program implementation in Northwest Ethiopia. Heliyon. (2024) 10(11):e32663. doi: 10.1016/j.heliyon.2024.e32663
Keywords: antimicrobial stewardship (AMS), antimicrobial resistance (AMR), resource-limited settings, antimicrobial stewardship program (ASP) assessment, healthcare facilities
Citation: Gitonga N, Okumu M, Agoro O, Kusu N, Mukoko J, Wangai H, Hafner T and Joshi MP (2025) Assessment of the implementation of antimicrobial stewardship programs in selected healthcare facilities in Kenya. Front. Trop. Dis. 5:1497220. doi: 10.3389/fitd.2024.1497220
Received: 16 September 2024; Accepted: 20 December 2024;
Published: 13 February 2025.
Edited by:
Israel Abebrese Sefah, University of Health and Allied Sciences, GhanaReviewed by:
Gerald Mboowa, Makerere University, UgandaCopyright © 2025 Gitonga, Okumu, Agoro, Kusu, Mukoko, Wangai, Hafner and Joshi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nkatha Gitonga, bmthdGhhLmdpdEBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.