- School of Public Health, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
Background: Podoconiosis, one of the neglected tropical diseases (NTDs), affects barefoot people in impoverished regions and contributes to poverty by having negative impacts on economic output, education, and disability. Podoconiosis has enormous social, psychological, and economic implications for the affected individuals. Social stigmatization of people with the disease is widespread, and patients are restricted from schools, local meetings, mosques, and churches and not allowed to marry into unaffected families. Therefore, this study aimed to systematically review the stigma related to podoconiosis in Ethiopia.
Methods: The Preferred Items for Systematic Reviews and Meta-analysis (PRISMA-2020) guidelines were followed. PubMed/Medline, Scopus, Web of Science, Google Scholar, and Google databases were searched. Articles published in the English language from inception to 2023 were included. Data were extracted by using a pre-prepared Excel sheet, and a narrative synthesis of the findings was done. This review was registered in the PROSPERO International Prospective Register of Systematic Reviews with registration number CRD42024510091.
Results: A total of 19 studies were included in this systematic review. This systematic review identified different types of stigmas reported from individuals with podoconiosis. The types of stigmas identified were enacted, felt, and internalized stigma and social stigmas, including exclusion from different social occurrences such as idir, meetings, funerals, and churches/mosques. Stigma also prevented patients with podoconiosis from visiting health institutions for the treatment of the disease and using health services for other cases.
Conclusions: Stigma among podoconiosis patients is widely distributed in Ethiopia. Different types of stigmas were identified among the patients. Extensive work needs to be done to prevent the disease and stigma. Strengthening works on community awareness about the disease help to ensure that it does not get transmitted from affected individuals to others.
Systematic review registration: PROSPERO, identifier CRD42024510091.
Introduction
Podoconiosis is a condition of non-infectious geochemical leg swelling (lymphoedema) caused by the long-term exposure of bare feet to red clay soil (1). The disease is characterized by severe disability, episodes of excruciating pain, and lower limb lymphoedema (2). It is a crippling neglected tropical disease (NTD) that is linked to severe stigma (3), which leads to social exclusion and isolation, relationship problems like fewer chances for marriage, negative emotions like shame and low self-esteem, and co-occurring mental health disorders (4). Approximately 4 million individuals worldwide suffer from podoconiosis in 32 countries that have the potential to become endemic: 18 of these countries are in Africa, three are in Asia, and 11 are in Latin America (5). Ethiopia shares the highest burden of podoconiosis globally; more than 35 million people are at risk of the disease, and more than 1.5 million people live with the disease in 345 districts of the country (6). In the country’s endemic areas, the disease’s prevalence ranges from 5% to 10% (7, 8).
Stigma is a social process or related personal experience characterized by exclusion, rejection, blame, or devaluation that results from experience or reasonable anticipation of an adverse social judgement about a person or group identified with a particular problem (9). In endemic places, podoconiosis is regarded as the health issue that causes the greatest social stigma. Numerous factors contribute to the stigma attached to podoconiosis, including the progressive physical disability that makes it impossible for those who have it to earn a living (10, 11), the misunderstandings held by locals regarding the disease’s causes and available treatments (3, 12–14), the burden that the disease brings on family members through treatment costs, and perceived fear of public identification of familial disease (3) as well as the deformity brought on by the disease’s progression (15, 16).
Patients with podoconiosis frequently face stigma (17), including exclusion from schools, churches, and mosques as well as restrictions on their ability to marry non-affected people (18). Stigma from the community members, health professionals, and non-affected people on podoconiosis patients due to the disease leads to instilled self-stigma and lack of self-confidence among people with podoconiosis, which ultimately discourage them from looking for proper healthcare and rather limit them to poor medical care (12, 14, 19–21). Patients are nearly seven times more likely to have quality-of-life scores that are below average and have 11 times the likelihood of depression than their healthy neighbors (22). Given this context, it is not unexpected that people with podoconiosis have high levels of mental discomfort and a generally lower quality of life (22, 23).
The social stigma associated with podoconiosis negatively impacts the overall health and wellbeing of patients, prompting different coping mechanisms with unfavorable results (3). This stigma further influences both healthcare-seeking behavior and the success of treatment. In an attempt to avoid unwanted responses from others, some podoconiosis sufferers choose to conceal their illness, potentially exacerbating their symptoms (3, 24). The embarrassment surrounding the disease often discourages those with podoconiosis from seeking help from potentially biased medical professionals (20). Research has shown that individuals with podoconiosis are often denied full societal acceptance, are excluded from social activities, are subjected to discrimination in mate selection and marriage, and have limited opportunities for decision-making and leadership roles within the community (3, 18).
Podoconiosis-related stigma experienced by affected individuals has a huge impact on reproductive health-related issues: poor marriage prospects, unwillingness to marry affected individuals and their family members, discrimination of marriage, and poor medical care (3, 12, 18, 20, 25). Thus, the purpose of this systematic review was to address the stigma related to podoconiosis among Ethiopian patients at all stages of the disease.
Methods
Studies’ grouping for evidence synthesis
A thorough search was conducted across various databases to get literature about the stigma associated with podoconiosis in Ethiopia. From the beginning until March 31, 2024, we have searched databases such as PubMed/Medline, Scopus, Web of Science, Embase, Google Scholar, and Google for published and unpublished publications. For the purpose of synthesizing the evidence, papers that met the inclusion criteria were categorized as “source of stigma explaining articles”, “impact of stigma on the general health”, “impact of stigma on quality of life”, and “impact of stigma on patients’ reproductive health”.
Search strategy
The Preferred Items for Systematic Reviews and Meta-analysis guidelines were followed. An electronic search for published articles was performed using different databases for primary articles. We systematically searched PubMed/Medline, Scopus, Web of Science, Embase, Google Scholar, and Google databases by using the terms “stigma”, “discrimination”, “exclusion”, ‘shame”, “negative attitude”, “bad perception”, “disgrace”, “disfigure”, “self-stigma”, “social consequences”, “stereotype”, “label avoidance”, “psychosocial burden”, “podoconiosis”, and “Ethiopia” combined by “and” (Supplementary S1 Text). Articles published in the English language and unpublished data from inception to 31/03/2024 were searched. The protocol for this review was published (with registration number CRD42023392583) in the PROSPERO International Prospective Register of Systematic Reviews (Supplementary S1 File). This systematic review followed the PRISMA guidelines for literature search strategy, selection of studies, data extraction, and result reporting (26). EndNote (version X7) reference management software for Windows was used to download, organize, review, and cite related articles.
Research question
We have conducted this systematic review to seek an answer for the following questions: What is the extent and impact of stigma related to podoconiosis on reproductive health, general health, social health, and quality of life?
Criteria for article selection
Inclusion criteria
Articles published in the English language that address the stigma and discrimination associated with podoconiosis among affected individuals were incorporated. Publications and unpublished data released from the inception of the field until 31/03/2024 within the context of Ethiopia were considered. All research investigations evaluating stigma, discrimination, exclusion, and any variant of stigma among podoconiosis patients across all stages of the disease were included.
Exclusion criteria
This review did not include tool verification studies, case reports, reviews, or articles published in languages other than English.
Quality assessment of the included studies
The modified Newcastle–Ottawa Scale (NOS) for cross-sectional studies was used to evaluate each study’s quality (27). Eight sections make up the scale, which assesses the included articles according to selection, comparability, exposure assessment, and result. The point scores were as follows: 0–5 represented low quality, 6–7 represented moderate quality, and 8–10 represented high quality (Supplemetary File 2). Articles with a minimum NOS score of 6 were included. Each study’s quality was evaluated independently by two authors (TL and AA) using the NOS. The titles and abstracts of the identified studies were evaluated for review relevance by two authors (MM and EW), and the relevant articles’ full texts were retrieved and examined by the primary author before NOS quality assessment.
Data extraction and synthesis
Before the actual data extraction began, a pilot extraction of the data using Microsoft Excel was conducted. The first author’s name, publication year, study location, design, sample size, response rate, type of stigma, and participants were all included in the data extraction template (S1 Excel sheet). Two authors carefully read each study (AA and EW), and any type of stigma reported is identified and extracted to a pre-prepared data extraction Excel sheet. The two authors (AA and EW) separately extracted the data, and a third author (MM) participated in discussing and reexamining the original articles in order to decide on unresolved disputes. After extracting the data by using Excel, detailed narration was done.
Definition of terms
Stigma: “a social process or related personal experience characterized by exclusion, rejection, blame, or devaluation that result from experience or reasonable anticipation of an adverse social judgment about a person or group identified with a particular problem” (9).
Data analysis
Data were extracted and compiled in Excel. Four authors (TL, AA, EW, and MM) discussed and synthesized the data in several cycles. A narrative synthesis was done to compile the data.
Results
Study selection
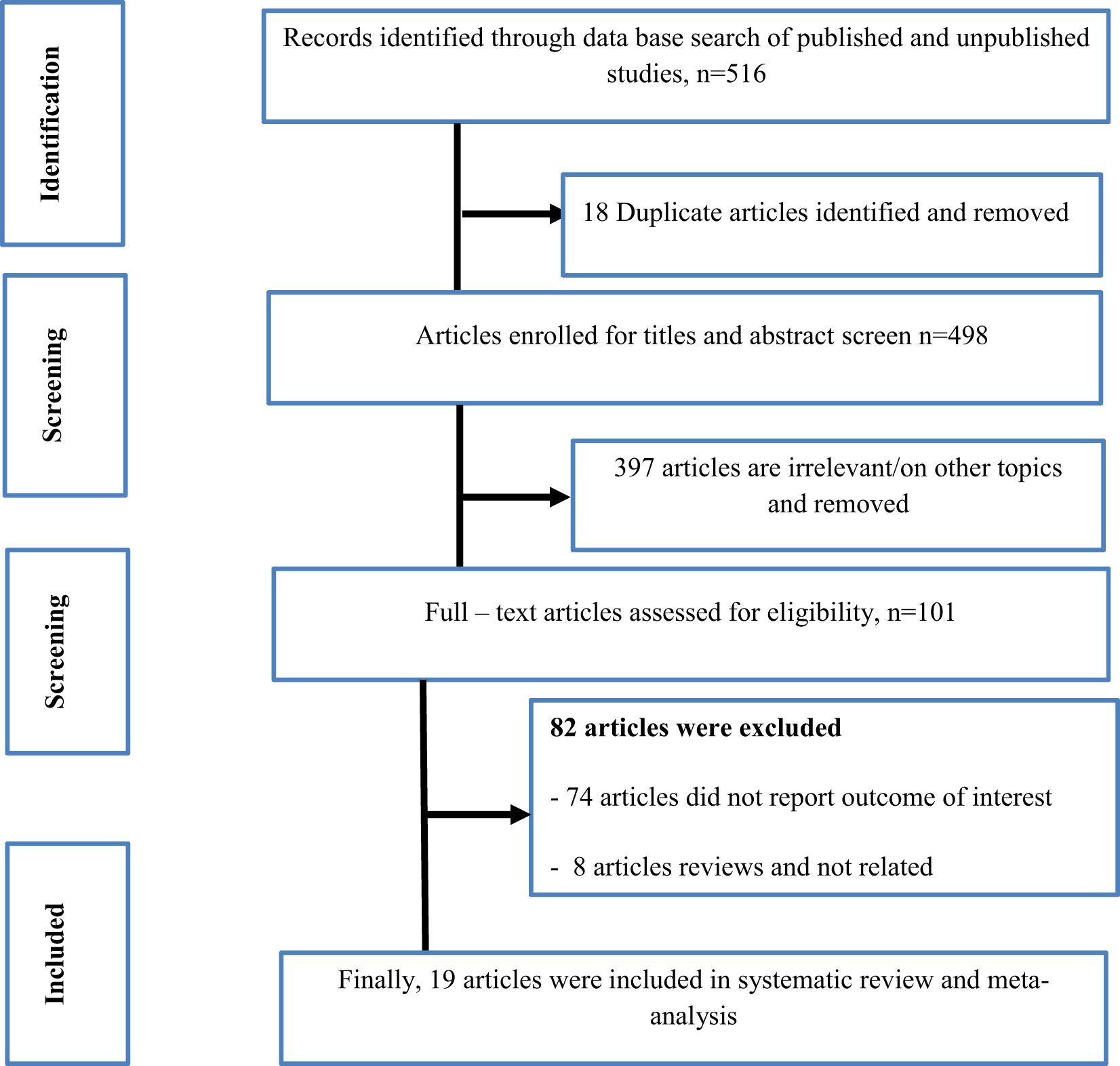
A comprehensive search of different databases was done to get articles on stigma related to podoconiosis in Ethiopia. We have searched databases including PubMed/Medline, Scopus, Web of Science, Embase, Google Scholar, and Google for published and unpublished articles from inception to 31/03/2024. In the beginning, 516 studies were first gathered via database searches. A total of 19 duplicates were detected from this and eliminated. Subsequently, 399 studies were eliminated after screening based on their title and abstract. The remaining 98 articles were evaluated for eligibility, and 80 of them were excluded for not reporting the desired outcome and not being primary studies. At the end, 19 articles that met the inclusion criteria were included in the study (Figure 1).
Study participants
A total of 19 articles with 4,796 respondents from Ethiopia were included in this systematic review. From the total of 19 included articles, 12 of the studies are observational (cross-sectional) (12, 14, 16, 20, 22, 24, 28–34) studies, two are mixed studies (18, 31), and the remaining five are qualitative studies (3, 13, 35–37) that assessed the stigma among podoconiosis patients. There were 14 of the studies that identified stigma among podoconiosis patients, and the remaining five tried to identify and explore health professionals’, communities’, and youth’s stigma on podoconiosis patients. The sample size across the studies ranged from 14 (35) from the Amhara region to 1,319 (14) from the same region. There were 11 studies (3, 12, 13, 16, 18, 20, 24, 28, 29, 35, 36) included that were from the south region, and the remaining eight studies (14, 22, 30–34, 37) included were from Amhara Region, North Ethiopia. We could not get any studies from the rest of the regions in Ethiopia, which might indicate that the disease prevalence is high in the two regions, and most of the studies on podoconiosis-related issues were concentrated on the two specified regions of Ethiopia (Table 1).
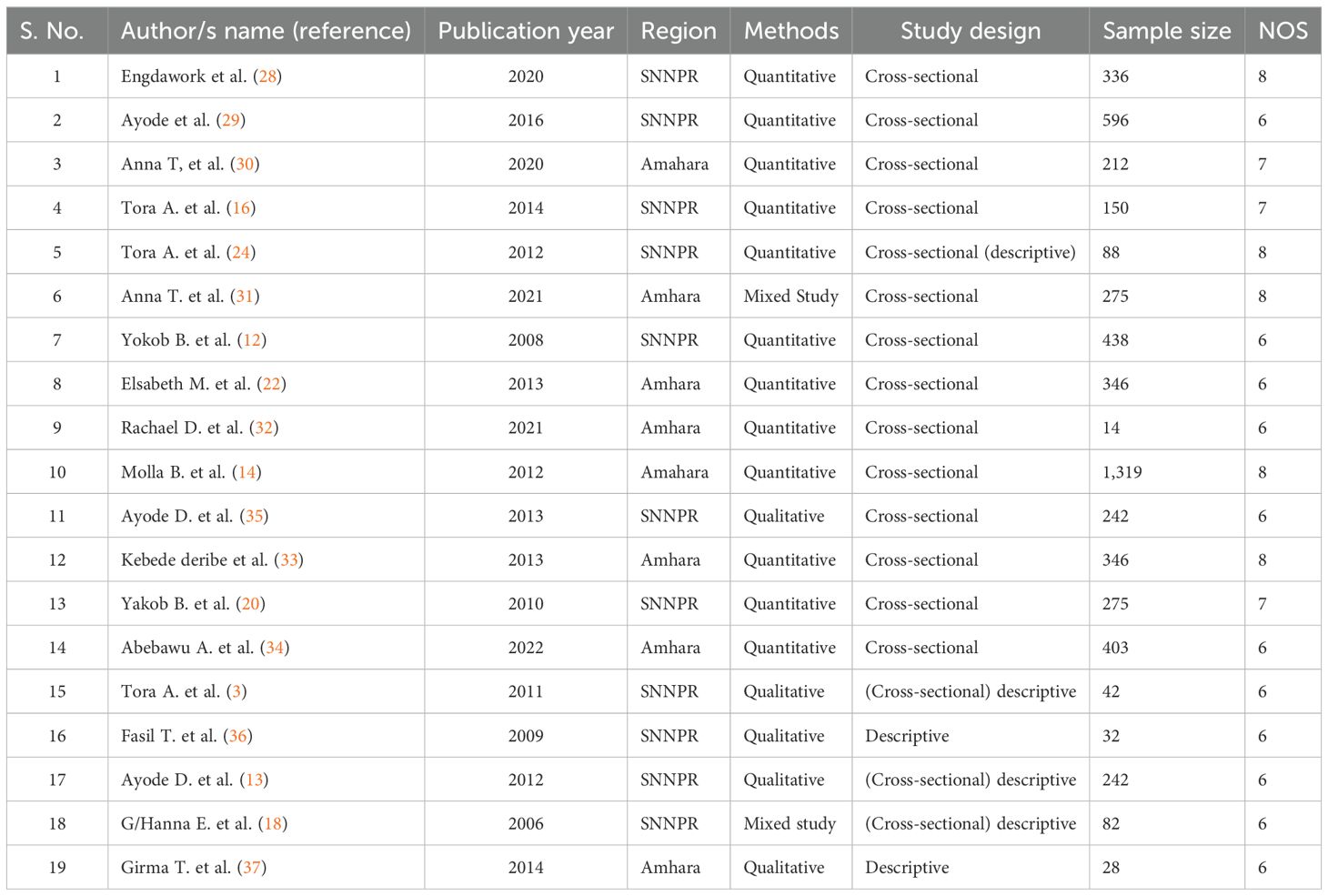
Table 1. Characteristics of the included studies in the systematic review for stigma related to podoconiois among the patients in Ethiopia, 2024.
Evidence synthesis on stigmas related to podoconiosis
Different studies have explored different types of stigmas related to podoconiosis. In this synthesis, stigmas reported by different studies were comprehensively presented. The types of stigmas identified in the included studies were enacted and anticipated (13, 24, 28, 30, 32, 33, 35), enacted and internalized (14, 29), enacted, anticipated, and internalized (3, 16, 18, 22, 23, 31, 34, 36), and enacted (12, 20, 37). The different forms of stigmas identified include exclusion, discrimination, and negative attitudes toward the patients, pinching their nose, not buying products, insulting, pointing at them, dropping from school, and preventing them from involvement in social affairs; social stigmatizations such as forced exclusion and exclusion from wedding, funerals, and marketplace are the felt stigma, enacted stigma, and experienced stigma that were identified (3, 12, 14, 16, 18, 20, 22, 24, 28–37). This systematic review indicated that there is the stigma of unwillingness to marry affected individuals, unwillingness to marry from the affected family, low willingness to help affected individuals, low willingness to be friends with affected persons, and unwillingness to care for podoconiosis patients (12, 13, 16, 20, 28, 37). The current review showed that experienced stigma among podoconiosis patients is common in Ethiopia. Most of the patients living with podoconiosis experienced stigma in their day to day activities (14, 16, 22, 24, 29, 33). This review identified that different studies reported stigma among podoconiosis in different social life situations. People with podoconiosis experience one or more forms of social stigmatization at school, church, or in the marketplace (14, 22, 32, 34, 36). The current study also showed that self-stigma among patients is evident as a result of pervasive stigmatizing beliefs in the community, which show up as poor self-esteem, suicidal thoughts, and avoiding relationships with non-affected community members (16, 24, 36). Similarly, stigma from family members was frequently reported from individuals living with podoconiosis (3).
Sources of stigma among podoconiosis patients
Common sources of stigma among podoconiosis patients include the progressive physical disability that prevents affected individuals from making a living, the misconceptions among community members about the causes of the disease and treatment options (3, 12–14), fear of public identification of a disease that is known to be familial (3, 37), and the physical disfigurement caused as the disease advances (36).
Impact of stigma on the general health of podoconiosis patients
This study identified that the impact of stigma on the healthcare service utilization of patients is critical. It showed that the stigma experienced by the patients in different places and daily situations prevented them from utilizing healthcare services in health facilities, which eventually led them to a poor heath outcome, dropping out from treatment follow-up, and poor quality of life (1, 12, 20, 24, 32, 37).
Impact of stigma on the quality of life
The current review also stated that the stigma faced by the individuals living with podoconiosis was highly related to the quality of life. The review showed that experiencing high levels of stigma compromised the quality of life of the individuals because patients were excluded from community activities such as meetings, funerals, markets, schools, and churches. Most of the patients were restricted and unable to generate their income, which further worsen their quality of life in health, psychological, and social aspects (22, 30, 34).
Impact of stigma on the reproductive health of patients
Even though the impact of stigma on the reproductive health of the patients is not well stated in the included studies in this review, the right of individuals to marry partners whom they choose is violated due to stigma. This study showed that stigma from different individuals prevents the patients from marrying unaffected individuals and those from unaffected families (12, 13, 16, 28, 36), and forced divorce and dissolution of marriage were identified (3, 13, 16, 18, 24).
The current review also showed that there is a gender difference in stigma among the patients (12). The level/extent of stigma was higher among female patients than in male patients (14, 28, 29).
Discussion
This systematic review was conducted to determine the stigma related to podoconiosis in Ethiopia. Different types of stigma were identified among podoconiosis patients in this study. The review included both quantitative and qualitative studies conducted on stigma among podoconiosis patients. The results from 19 included articles in this review revealed the evidence of stigma among podoconiosis patients. A total of 12 of the studies are observational (cross-sectional) (12, 14, 16, 20, 22, 24, 28–34) studies, two are mixed studies (18, 31), and the remaining five are qualitative studies (3, 13, 35–37) that assessed stigma among podoconiosis patients.
There was evidence of widespread stigma related to podoconiosis among the patients in Ethiopia (16, 20, 24).
The current review showed that experienced stigma, felt stigma, enacted stigma, and social stigmatization (forced exclusion, forced divorce, dissolution of marriage, exclusion from marriage prosper, not buying products, inability to participate in wedding ceremonies, funerals, markets, meetings, insulting, nose pinching, and stigmatizing attitudes) were reported in the current study (3, 12, 16, 18, 20, 21, 24, 29, 32, 33, 36).
This study also showed that from inception to 31/03/2024, stigma persisted among podoconiosis patients, indicating that consistent, comprehensive, collaborative, and efficient disease prevention and stigma prevention programs need to be strengthened.
This study also identified that there are still existing beliefs that podoconiosis is caused by contagious agents and that it can be transmitted, which is one of the common sources of stigmas among patients. The finding is similar to a systematic review conducted among countries globally (38). This might be due to the persistent lack of awareness about the disease and its causes among the communities and healthcare professionals.
This review showed that beliefs that podoconiosis is hereditary, belief that contagion causes podoconiosis, and being female are factors associated with stigma among podoconiosis patients (13, 28, 29, 37). This finding is similar to primary studies conducted among podoconiosis patients in different parts of Ethiopia (13, 16, 24, 29, 37).
Stigma related to podoconiosis impacts on healthcare service utilization, quality of life, and reproductive health of individuals. This finding is consistent with a review on stigma among NTD patients (39–41). This indicates that a violation of the sexual and reproductive health rights of podoconiosis patients is evident in Ethiopia, which needs to be addressed by organizations working on podoconiosis prevention.
This study showed that enacted, felt, and experienced stigma were common among podoconiosis patients in Ethiopia. This finding is consistent with a systematic review of stigma associated with cutaneous and mucocutaneous leishmaniasis (40). This might be due to a stagnant change in the families’ and communities’ awareness, beliefs, and attitudes toward podoconiosis.
The current review showed that stigma related to podoconiosis is known to be a challenge for patients to utilize treatments and other prevention methods. This finding is similar to studies in Ethiopia and other countries (39, 41). This might be because attitudes from families, communities, and health professionals make things difficult for patients to get treatment.
Limitations of the study
This systematic review provides up-to-date evidence regarding the stigma related with podoconiosis in Ethiopia; however, there are some limitations that need to be considered. We could not obtain primary studies from other regions of Ethiopia except for the two regions where the disease is most prevalent. The review reported data from two regions, which might lack representativeness. Despite this limitation, an extensive search was conducted to minimize all possible risks of bias.
Conclusions
Stigma is a persisting issue that needs due attention from government and non-government organizations. This systematic review showed that the stigma faced by patients with podoconiosis is widely distributed. The review identified that different types of stigmas occurred among patients, such as felt, enacted, and experienced, and patients were excluded from different social happenings like meetings, churches, markets, and funerals and hindered from using health service care in health facilities due to fear of stigma. Therefore, strengthening disease prevention, stigma prevention, awareness creation among the community, and working with national and local media to expand information, education, and communication are needed for the prevention and mitigation of stigma.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
TA: Conceptualization, Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft. AA: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. EW: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. MK: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Wolaita Sodo University, College of Health Sciences and Medicine, for facilitating the Internet connections. We also thank all authors and participants of the primary study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fitd.2024.1483407/full#supplementary-material
Abbreviations
NTDs, neglected tropical disease; NOS, Newcastle−Ottawa Scale; PRISMA, Preferred Items for Systematic Reviews and Meta-analysis; WHO, World Health Organization.
References
2. Negussie H, Molla M, Ngari M, Berkley JA, Kivaya E, Njuguna P, et al. Lymphoedema management to prevent acute dermatolymphangioadenitis in podoconiosis in northern Ethiopia (GoLBeT): a pragmatic randomised controlled trial. Lancet Global Health. (2018) 6:e795–803. doi: 10.1016/S2214-109X(18)30124-4
3. Tora A, Davey G, Tadele G. A qualitative study on stigma and coping strategies of patients with podoconiosis in Wolaita zone, Southern Ethiopia. Int Health. (2011) 3:176–81. doi: 10.1016/j.inhe.2011.06.006
4. Bartlett J, Deribe K, Tamiru A, Amberbir T, Medhin G, Malik M, et al. Depression and disability in people with podoconiosis: a comparative cross-sectional study in rural Northern Ethiopia. Int Health. (2016) 8:124–31. doi: 10.1093/inthealth/ihv037
5. Deribe K, Cano J, Trueba ML, Newport MJ, Davey G. Global epidemiology of podoconiosis: A systematic review. PloS Negl Trop Diseases. (2018) 12:e0006324. doi: 10.1371/journal.pntd.0006324
6. Deribe K, Negussu N, Newport MJ, Davey G, Turner HC. The health and economic burden of podoconiosis in Ethiopia. Trans R Soc Trop Med Hygiene. (2020) 114:284–92. doi: 10.1093/trstmh/traa003
7. Geshere Oli G, Tekola Ayele F, Petros B. Parasitological, serological and clinical evidence for high prevalence of podoconiosis (non-filarial elephantiasis) in Midakegn district, central Ethiopia. Trop Med Int Health. (2012) 17:722–6. doi: 10.1111/j.1365-3156.2012.02978.x
8. Desta K, Ashine M, Davey G. Predictive value of clinical assessment of patients with podoconiosis in an endemic community setting. Trans R Soc Trop Med Hygiene. (2007) 101:621–3. doi: 10.1016/j.trstmh.2006.12.002
9. Weiss MG, Ramakrishna J. Stigma interventions and research for international health. Lancet (London England). (2006) 367:536–8. doi: 10.1016/S0140-6736(06)68189-0
10. Destas K, Ashine M, Davey G. Prevalence of podoconiosis (endemic non-filarial elephantiasis) in Wolaitta, Southern Ethiopia. Trop doctor. (2003) 33:217–20. doi: 10.1177/004947550303300410
11. Tekola F, Mariam DH, Davey G. Economic costs of endemic non-filarial elephantiasis in Wolaita Zone, Ethiopia. Trop Med Int Health. (2006) 11:1136–44. doi: 10.1111/j.1365-3156.2006.01658.x
12. Yakob B, Deribe K, Davey G. High levels of misconceptions and stigma in a community highly endemic for podoconiosis in southern Ethiopia. Trans R Soc Trop Med Hygiene. (2008) 102:439–44. doi: 10.1016/j.trstmh.2008.01.023
13. Ayode D, McBride CM, de Heer H, Watanabe E, Gebreyesus T, Tadele G, et al. The association of beliefs about heredity with preventive and interpersonal behaviors in communities affected by podoconiosis in rural Ethiopia. Am J Trop Med Hygiene. (2012) 87:623–30. doi: 10.4269/ajtmh.2012.12-0204
14. Molla YB, Tomczyk S, Amberbir T, Tamiru A, Davey G. Patients’ perceptions of podoconiosis causes, prevention and consequences in East and West Gojam, Northern Ethiopia. BMC Public Health. (2012) 12:828. doi: 10.1186/1471-2458-12-828
15. Tekola F, Ayele Z, Mariam DH, Fuller C, Davey G. Development and testing of a de novo clinical staging system for podoconiosis (endemic non-filarial elephantiasis). Trop Med Int Health. (2008) 13:1277–83. doi: 10.1111/j.1365-3156.2008.02133.x
16. Tora A, Franklin H, Deribe K, Reda AA, Davey G. Extent of podoconiosis-related stigma in Wolaita Zone, Southern Ethiopia: a cross-sectional study. SpringerPlus. (2014) 3. doi: 10.1186/2193-1801-3-647
17. Tora A, Franklin H, Deribe K, Reda AA, Davey G. Extent of podoconiosis-related stigma in Wolaita Zone, Southern Ethiopia: a cross-sectional study Vol. 3. SpringerPlus (2014). p. 647. Available at: http://wwwspringerpluscom/content/3/1/647.
18. Ewenat G. The social burden of podoconiosis in Wolayita zone. Southern Nation Nationality People’s Region, Ethiopia (2005).
19. Alemu G, Tekola Ayele F, Daniel T, Ahrens C, Davey G. Burden of podoconiosis in poor rural communities in Gulliso woreda, West Ethiopia. PloS Negl Trop Diseases. (2011) 5:e1184. doi: 10.1371/journal.pntd.0001184
20. Yakob B, Deribe K, Davey G. Health professionals’ attitudes and misconceptions regarding podoconiosis: potential impact on integration of care in southern Ethiopia. Trans R Soc Trop Med Hygiene. (2010) 104:42–7. doi: 10.1016/j.trstmh.2009.07.021
21. Tora A, Mengiste A, Davey G, Semrau M. Community involvement in the care of persons affected by podoconiosis-A lesson for other skin NTDs. Trop Med Infect Disease. (2018) 3. doi: 10.3390/tropicalmed3030087
22. Mousley E, Deribe K, Tamiru A, Davey G. The impact of podoconiosis on quality of life in Northern Ethiopia. Health Qual Life Outcomes. (2013) 11:122. doi: 10.1186/1477-7525-11-122
23. Mousley E, Deribe K, Tamiru A, Tomczyk S, Hanlon C, Davey G. Mental distress and podoconiosis in Northern Ethiopia: a comparative cross-sectional study. Int Health. (2015) 7:16–25. doi: 10.1093/inthealth/ihu043
24. Tora A, Davey G, Tadele G. Factors related to discontinued clinic attendance by patients with podoconiosis in southern Ethiopia: a qualitative study. BMC Public Health. (2012) 12:902. doi: 10.1186/1471-2458-12-902
25. Molla YB, Tomczyk S, Amberbir T, Tamiru A, Davey G. Patients’ perceptions of podoconiosis causes, prevention and consequences in East and West Gojam, Northern Ethiopia. BMC Public Health. (2012) 12:828. http://wwwbiomedcentralcom/1471-2458/12/828.
26. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. (Clinical research ed). doi: 10.1136/bmj.n71
27. Wells GA, Wells G, Shea B, Shea B, O’Connell D, Peterson J, et al eds. The newcastle-ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute (2014).
28. Engdawork K, Davey G, Ayode D, McBride CM, Tadele G. A cross-sectional survey to assess the risk factors associated with stigmatizing attitudes towards patients with podoconiosis among rural youth in southern Ethiopia. Trans R Soc Trop Med Hygiene. (2020) 114:995–1002. doi: 10.1093/trstmh/traa091
29. Ayode D, Tora A, Farrell D, Tadele G, Davey G, McBride CM. Dual perspectives on stigma: reports of experienced and enacted stigma by those affected and unaffected by podoconiosis. J Public Health Res. (2016) 5:689. doi: 10.4081/jphr.2016.689
30. van’t Noordende AT, Aycheh MW, Schippers AP. An exploration of family quality of life in persons with leprosy-, lymphatic filariasis– and podoconiosis-related disabilities and their family members in Ethiopia. Trans R Soc Trop Med Hygiene. (2020) 114:1003–12. doi: 10.1093/trstmh/traa090
31. van’t Noordende AT, Wubie Aycheh M, Tadesse T, Hagens T, Haverkort E, Schippers AP. A family-based intervention for prevention and self-management of disabilities due to leprosy, podoconiosis and lymphatic filariasis in Ethiopia: A proof of concept study. PloS Negl Trop Dis. (2021) 15. doi: 10.1371/journal.pntd.0009167
32. Dellar R, Ali O, Kinfe M, Tesfaye A, Fekadu A, Davey G, et al. Knowledge, attitudes and practices of health professionals towards people living with lymphoedema caused by lymphatic filariasis, podoconiosis and leprosy in northern Ethiopia. Int Health. (2022) 14:530–6. doi: 10.1093/inthealth/ihab067
33. Deribe K, Tomczyk S, Mousley E, Tamiru A, Davey G. Stigma towards a neglected tropical disease: felt and enacted stigma scores among podoconiosis patients in Northern Ethiopia. BMC Public Health. (2013) 13:1178. doi: 10.1186/1471-2458-13-1178
34. Abebaw A, Atnafu A, Worku N, Hagos A. Health-related quality of life and associated factors among adult podoconiosis patients in Debre Elias district Northwest, Ethiopia. PloS Negl Trop Diseases. (2022) 16. doi: 10.1371/journal.pntd.0010673
35. Ayode D, McBride CM, de Heer HD, Watanabe E, Gebreyesus T, Tora A, et al. A qualitative study exploring barriers related to use of footwear in rural highland Ethiopia: implications for neglected tropical disease control. PloS Negl Trop Dis. (2013) 7. doi: 10.1371/journal.pntd.0002199
36. Tekola F, Bull S, Farsides B, Newport MJ, Adeyemo A, Rotimi CN, et al. Impact of social stigma on the process of obtaining informed consent for genetic research on podoconiosis: a qualitative study. BMC Med Ethics. (2009) 10:13. doi: 10.1186/1472-6939-10-13
37. Tsegay G, Wubie M, Degu G, Tamiru A, Cooper M, Davey G. Barriers to access and re-attendance for treatment of podoconiosis: a qualitative study in northern Ethiopia. Int Health. (2015) 7:285–92. doi: 10.1093/inthealth/ihu085
38. Hofstraat K, van Brakel WH. Social stigma towards neglected tropical diseases: a systematic review. Int Health. (2016) 8 Suppl 1:i53–70. doi: 10.1093/inthealth/ihv071
40. Nuwangi H, Agampodi TC, Price HP, Shepherd T, Weerakoon KG, Agampodi SB. Stigma associated with cutaneous and mucocutaneous leishmaniasis: A systematic review. PloS Negl Trop Diseases. (2023) 17:e0011818. doi: 10.1371/journal.pntd.0011818
Keywords: stigma, discrimination, neglected tropical disease, podoconiosis, Ethiopia
Citation: Abiso TL, Kerbo AA, Woticha EW and Koyira MM (2024) Stigma related to podoconiosis in Ethiopia: a systematic review. Front. Trop. Dis 5:1483407. doi: 10.3389/fitd.2024.1483407
Received: 19 August 2024; Accepted: 06 November 2024;
Published: 18 December 2024.
Edited by:
Alexander Yaw Debrah, Kwame Nkrumah University of Science and Technology, GhanaReviewed by:
Abdel Jelil Njouendou, University of Buea, CameroonSunny Doodu Mante, African Filariasis Morbidity Project, Ghana
Copyright © 2024 Abiso, Kerbo, Woticha and Koyira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Temesgen Lera Abiso, dGVtZWxlcmFAZ21haWwuY29t
 Temesgen Lera Abiso
Temesgen Lera Abiso Amene Abebe Kerbo
Amene Abebe Kerbo Eskinder Wolka Woticha
Eskinder Wolka Woticha Mengistu Meskele Koyira
Mengistu Meskele Koyira