
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Trop. Dis. , 08 August 2024
Sec. Neglected Tropical Diseases
Volume 5 - 2024 | https://doi.org/10.3389/fitd.2024.1421522
This article is part of the Research Topic Women in Science - Emerging, Major & Neglected Tropical Diseases View all 5 articles
 Nafiisah Chotun1*
Nafiisah Chotun1* Julian Eaton2
Julian Eaton2 Ifeoma Ajegbo Anagbogu3
Ifeoma Ajegbo Anagbogu3 Hanna Amanuel Tesfahunei1
Hanna Amanuel Tesfahunei1 Sheila Shawa4
Sheila Shawa4 Carol Karutu5
Carol Karutu5 Akeem Bolarinwa6
Akeem Bolarinwa6 Abdulaziz Mohammed1
Abdulaziz Mohammed1The elimination of Neglected Tropical Diseases (NTDs) has seen significant progress, with 22 African Union Member States having successfully eliminated at least one NTD. However, post-elimination management of NTDs remains a challenge. This article provides important insights into the challenges faced by African Union Member States after eliminating NTDs, including potential financial support withdrawal and risk of disease reemergence. We also discuss comprehensive strategies for post-elimination management, emphasising the importance of robust surveillance systems, capacity building, community engagement, and the integration of mental health services. We also advocate for a multisectoral approach to sustain elimination gains, aligning with global and regional health strategies. Our analysis underscores the necessity of continuous innovation in surveillance, the critical role of community health workers, the integration of NTD post-elimination management into broader health and development frameworks such as Universal Healthcare Coverage, and the need for innovative financing and partnerships to ensure the long-term success of NTD elimination efforts.
The journey to controlling and eliminating Neglected Tropical Diseases (NTDs) has been one of great strides, where globally, by June 2024, 51 countries had eliminated at least one NTD successfully, of which 22 were African Union (AU) Member States (MS). Notably, Togo is the only country in the world that has eliminated four NTDs (1). Ghana and Benin have eliminated three NTDs, whilst most other countries have eliminated one or two diseases (Figure 1). Although these achievements highlight the progress that has been made to eliminate NTDs, elimination comes with a new set of challenges. As countries graduate to a post-elimination status, they will likely lose financial support during the transition phase. Yet most countries are unprepared to sustain the elimination status and gains made. This situation is further exacerbated by cross-border re-infection and re-introduction of eliminated NTDs by endemic neighbouring countries. Climate change also poses challenges to post-elimination efforts for vector-borne NTDs as the rise in temperature creates a conducive environment for transmission of infection and reemergence of diseases. Changes in temperature, humidity and rainfall allow some vectors to thrive in environments where they could not previously (2, 3). Besides, urbanisation trends and encroachment on wildlife territories tend to increase exposure risks to zoonotic and vector-borne NTDs, making it necessary for continued efforts to check such diseases.
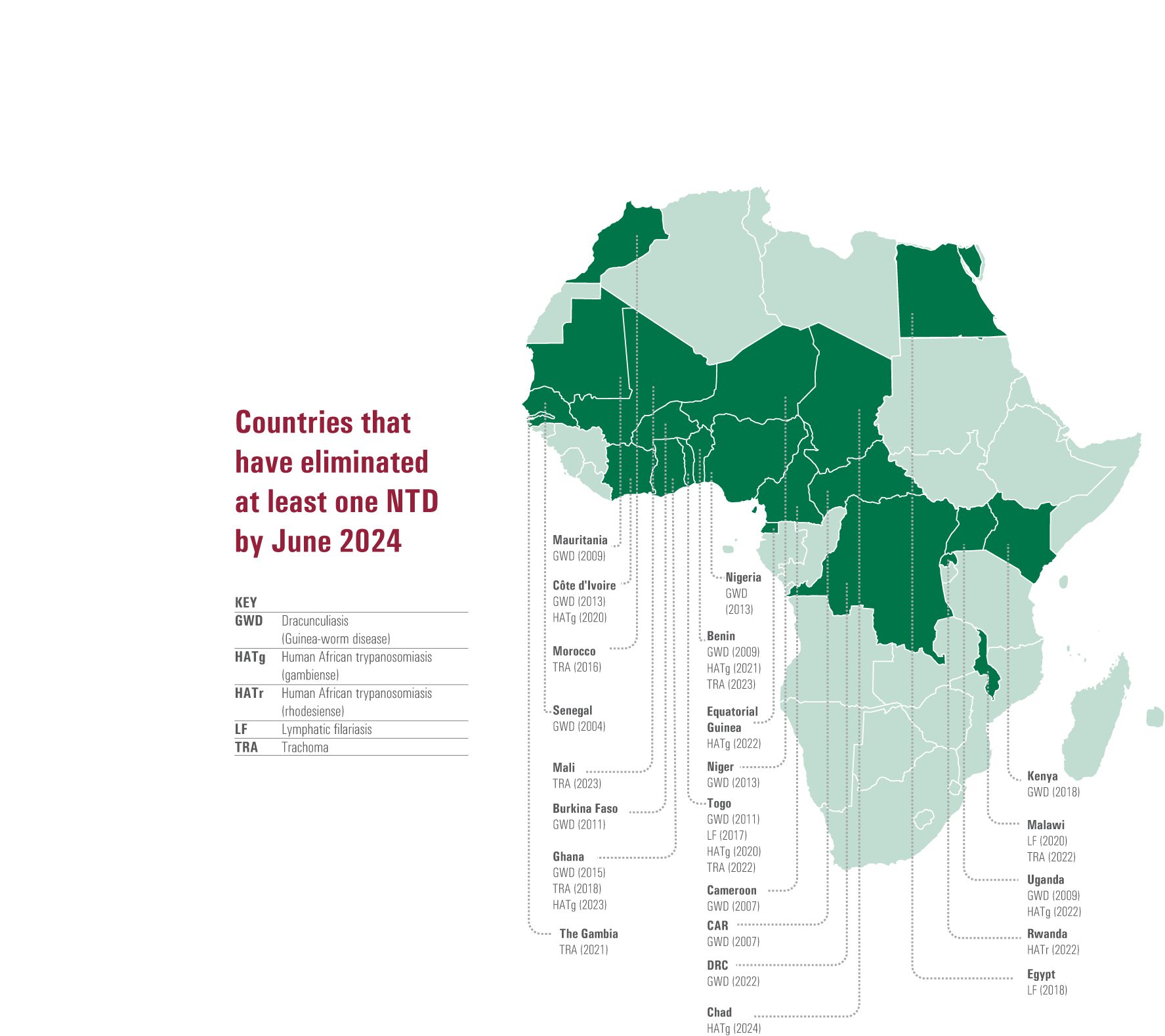
Figure 1 African Union Member States that have eliminated at least one neglected tropical disease (NTD) as of December 2023. Adapted from WHO Global report on neglected tropical diseases 2023 (1).
In this paper, we investigate key strategies for proper post-elimination management of NTDs within AU MS and highlight the importance of resilient integrated surveillance systems, continuous capacity strengthening, risk communication and community engagement, and integration of mental health services in changing environmental and socio-economic landscapes. We underscore the integration of NTD programmes into broader health and socio-economic development frameworks to ensure sustenance of post-elimination gains. The strategies discussed align with the aspirations of the AU Agenda 2063 (4), which seeks to promote healthy and well-nourished citizens, the Africa Health Strategy (5), the Sustainable Development Goals (SDGs) (6), the AU Continental Framework for Elimination of NTDs by 2030 (7) and the Africa CDC Strategic Plan 2023-2027. Notably, the latter now includes a pillar to tackle high-burden diseases, including NTDs (8). We share essential insights from extensive collaboration with the MS that have succeeded in eliminating NTDs and share general considerations for the countries on the path to eliminating NTDs.
Sustaining gains from elimination requires continued surveillance to detect any resurgence of NTDs and involves regular monitoring, data collection, and analysis to identify and address potential outbreaks (9). Others have presented key considerations in conducting post-elimination active surveillance (10) by integrating surveillance for NTDs into existing structures such as Integrated Disease Surveillance and Response (IDSR) and population-based surveys such as the Demographic Health Surveys (DHS), sentinel surveillance and the need for specific diagnostic tools adapted for post-elimination surveillance (11).
In addition to laboratory testing for proxy-biomarkers for continued monitoring for NTDs post-elimination, we propose integrated and community-based approaches using event-based surveillance (EBS) using the One Health approach (12) for those with identifiable and visible symptoms (e.g. Guinea Worm Disease (GWD) that can be identified in humans and dogs through the emergence of worms from ulcers in their limbs) (13). During the COVID-19 pandemic, Africa CDC supported Member States in scaling up event-based surveillance through community healthcare workers (CHWs) to ensure rapid identification of cases and contact tracing through simple signals that community members could report. The latest Africa CDC EBS framework incorporates a One Health approach and cross-border EBS, key to preventing the reemergence of NTDs (14).
We also propose enhanced cross-border surveillance as a critical requirement for post-elimination surveillance as this will ensure that as countries are validated for elimination, neighbouring countries are encouraged to continue working towards elimination. Moreover, the constant movement of people between countries, whether for economic or conflict reasons, necessitates monitoring these migrant populations post-elimination to prevent re-emergence (15). Coordinated efforts between countries have proven effective. For example, the border crossing between Ethiopia and Sudan at Galabat-Metema was targeted for onchocerciasis elimination, and the two countries ensured coordinated approaches that led to the elimination of onchocerciasis and continued surveillance (16). In West Africa, the Mano River Union, encompassing Liberia, Sierra Leone, Guinea, and Côte d’Ivoire, broadened its focus to health, initially targeting onchocerciasis and then extending to lymphatic filariasis, schistosomiasis, trachoma, and soil-transmitted helminthiasis (STH). This Union was pivotal in coordinating cross-border efforts during the 2014 Ebola outbreak and has significantly facilitated cross-border health collaborations through advocacy and streamlined administrative processes (17).
With advancements in technology, mobile health (mHealth) tools and digital reporting systems have become more accessible (18, 19) and could help improve health equity (20) and facilitate the implementation of EBS for NTDs in remote or underserved areas that cannot be easily reached and are often close to the borders of neighbouring countries. Additionally, improvement in data collection mechanisms will ensure accuracy in reporting, which will prevent challenges currently faced with NTDs, such as leprosy, where the disease was initially certified as eliminated. Still, the number of cases has increased recently due to improved surveillance and data collection.
At a side-event on post-elimination surveillance for NTDs at the Conference on Public Health in Africa (CPHIA) 2024, one of the panellists (IAA) shared Nigeria’s experience in monitoring GWD after its elimination through a comprehensive, integrated system that was operational even during the active transmission phase, ensuring a seamless transition and continued vigilance in disease monitoring. The strategies included incorporating GWD queries into Immunisation Plus Days’ tally sheets, distributing GWD information during mosquito net campaigns, and including GWD searches in the 2011 DHS. Such strategies could also be adapted for diseases like schistosomiasis and STH during national health school surveys. Many NTDs, including GWD, are monitored through IDSR forms used by health facilities and the public and any available opportunities to promote surveillance activities. Cross-border surveillance and targeted case searches target urban areas where NTDs like GWD are prevalent, often linked to the mobility of groups like farmers, traders, and local security personnel (‘mai guards’) from neighbouring countries and internally displaced people due to insecurity.
Knowledge and awareness of NTDs among healthcare workers and communities are low (21, 22), necessitating ongoing education for personnel, including CHWs, especially in resource-limited settings where NTDs are prevalent, and CHWs often serve as the primary source of health information and services for the community (23). Many healthcare workers lack sufficient training to identify and treat NTDs, leading to missed diagnoses. Adequate staffing for control programmes and the use of digital tools can enhance NTD diagnosis and contribute to health equity, particularly benefiting women who often have less access to healthcare services yet are disproportionately affected by NTDs (19, 20).
The African Union has committed to training 2 million CHWs on the continent; WHO has highlighted the importance of capacity building for health workers in NTD-endemic countries and advocated for ongoing education programmes that include updates on disease management, surveillance techniques, and community engagement strategies (14). Ongoing education is crucial to keep healthcare providers skilled in managing NTDs, particularly in resource-scarce, endemic regions. Furthermore, as NTD control strategies evolve and new treatment or diagnostic tools are developed, disseminating this knowledge to frontline workers is vital (14). There is also a risk of losing specific disease knowledge in regions where an NTD has been eliminated, as areas with no history of NTD interventions often exhibit misconceptions and incorrect knowledge about the treatability of these diseases, typically recognising only late-stage symptoms.
In Nigeria, regular training on NTD case definitions has improved surveillance and response at all administrative levels. Public engagement, financial incentives, and media, along with education for migratory populations, have enhanced case reporting and investigation. Misunderstandings and stigma around NTDs can hinder health-seeking behaviours, notably where NTDs may re-emerge in previously eliminated areas (24). Education for lasting behavioural change is vital in regions with persistent NTD vectors, as demonstrated by the successful eradication of Guinea Worm Disease (13).
Whilst the elimination of NTDs offers an exciting opportunity for the reduction of disability and suffering, those already affected must be provided suitable care and support to deal with the physical, social, and mental impacts of these conditions. For skin NTDs in particular, which are often highly stigmatised, focusing on mental health is a critical factor that has been largely neglected. Addressing population attitudes can reduce stigma against people affected and support uptake of elimination strategies as recommended by the WHO NTD Roadmap (2021–2030) as part of a person-centred approach to integrated services. The substantial adverse effects of NTDs on the mental well-being of affected people have an impact that often remains even after physical disease control has been attained (14, 25). Mechanisms linking NTDs with a high prevalence of mental and neurological symptoms (and an increased suicide rate) include persistent pain and itch (both associated with depression in other health conditions), functional loss like blindness, and direct neurological effects (for example, in human African trypanosomiasis and onchocerciasis with nodding syndrome). However, by far, the strongest causal mechanism seems to be stigma, social exclusion, and discrimination associated with disfiguring skin conditions. This could not only lead to depression and anxiety but reinforce already high levels of poverty through reduced economic opportunities and catastrophic health expenditure. Emerging evidence from across Africa is supporting integrating mental health services within primary healthcare systems (26, 27), with development and testing of practical models that can start to reduce the negative impact of social exclusion and mental distress on those affected (28, 29). With this, we have the prospect of comprehensive systems for improving mental well-being, social reintegration, and quality of life for people affected by NTDs as we move into a post-elimination phase. In Nigeria, for example, mental health is an integral part of the NTD Masterplan. The Mental Health and NTD Programmes at the Federal Ministry of Health and Social Welfare are collaborating with civil society to scale integration of mental health into health and other systems for people affected by NTDs (28).
The AU Continental Framework on the elimination of NTDs, The Africa Health Strategy, and the WHO 2021-2030 Roadmap for NTDs advocate for a multisectoral approach to prevent the reemergence of NTDs, highlighting the necessity to address the socio-economic dimensions that underlie their resurgence. This strategy emphasises integrating interventions across sectors to tackle poverty-related factors deeply embedded in social, economic, and environmental conditions, such as water supply, sanitation, health education, and vector control.
Addressing malnutrition is crucial, as it often perpetuates a cycle of increased susceptibility to infection and nutritional deficiencies, as seen in NTDs such as Noma. Consequently, dietary education and access to nutritious food are fundamental in the NTD elimination and post-elimination strategy, necessitating collaboration across physical and mental health, water and sanitation, education, economic development, and nutrition sectors.
The African Programme for Onchocerciasis Control (APOC) exemplifies effective multisectoral collaboration, uniting communities, policymakers, health workers, the UN, donors, and NGOs to foster sustainable community capacities for onchocerciasis control through Community-Directed Treatment with Ivermectin (CDTI). APOC’s success in promoting community ownership and empowering individuals to take charge of their health underscores the importance of such collaboration for maintaining NTD elimination.
In terms of vector control, targeted approaches have been effectively used to combat NTDs. For example, the Guinea Worm Eradication Programme utilises insecticides, such as Temephos, to manage the cyclops population. Similarly, the Onchocerciasis Control Programme employs insecticides in some countries to target blackflies. Strategies like Insecticide-Treated Nets (ITNs) and Indoor Residual Spraying (IRS) have proven effective against lymphatic filariasis. These prevention strategies are also utilised by malaria programmes, underscoring the interconnection between various disease control activities and the need for better coordinated multisectoral strategies.
During the African Union Commission (AUC)-Africa CDC joint meeting on mobilising domestic resources and strengthening programmes to combat NTDs conducted in Zambia in December 2023, NTD experts recommended adopting the One Health approach for better coordination between the different ministries, including Education, Agriculture, Community and social development, Finance, Tourism, and Information, and development partners, etc. They proposed a strategic plan involving a Technical Working Group (TWG) for NTDs, with each Ministry providing a focal point to participate in regular TWG multisectoral meetings, showcasing the integrated approach needed to maintain elimination gains for NTDs effectively.
Whilst promoting a multisectoral approach is essential for preventing the reemergence of NTDs, it alone may not be sufficient. Given the uncertain future environment related to climate change, demographic shifts, and population movements, effective disease control interventions must be designed with sustainability in mind. This involves integrating NTD management into national health systems, securing ongoing financial and political support, and fostering community ownership of health initiatives. Sustainable interventions should be adaptable to changing socio-economic and environmental conditions and built upon robust surveillance systems, continuous capacity building, and strong cross-sectoral collaborations. Additionally, addressing main determinants such as poverty, poor sanitation, and lack of access to healthcare is critical. Understanding risk factors, gaps, and challenges in current strategies will help redesign interventions to be more resilient and self-sustaining, creating a lasting impact in the fight against NTDs.
Advocacy plays a pivotal role in securing funding and sustainability for public agendas, crucial for the sustained vigilance needed in the fight against NTDs. Particularly in low- and middle-income countries where health budgets are constrained, advocacy ensures that eliminating NTDs remains a priority amidst competing health issues. It is essential to engage key stakeholders at all levels, from local communities to international partners, to coordinate efforts against the reemergence of these diseases. The AUC-Africa CDC joint meeting on NTDs underscored the importance of political support at the Heads of State level, advocating using continental NTD scorecards to mobilise resources for long-term sustainability.
We advocate for integrating NTDs into Universal Health Coverage (UHC) to ensure equitable healthcare for all, especially as these diseases predominantly impact communities with limited access to affordable care. Incorporating a dedicated NTD package within UHC, focusing on post-elimination surveillance, supports the most vulnerable and marginalised groups, expediting the enhancement of health systems and the achievement of comprehensive UHC. This integration guarantees comprehensive health services for everyone, irrespective of economic status, which is vital for breaking the poverty-disease cycle and sustaining NTD elimination.
Policy-wise, post-elimination strategies necessitate high-level consideration of approaches like cross-border collaborations. The collaborative efforts between Ethiopia, Sudan, and South Sudan in eliminating onchocerciasis and lymphatic filariasis, as outlined in Ethiopia’s Third National NTDs Strategic Plan 2021-2025, exemplify effective policy implementation. Formal agreements facilitate smooth joint surveillance and management of NTD reemergence. Additionally, policies must address the mental health needs of NTD survivors, ensuring funding and resource allocation for mental health services in post-elimination phases.
In the post-elimination phase of NTDs, financing and resource allocation are crucial to sustain surveillance and prevent disease resurgence. The shift from donor-driven support to more diversified sources, including national health budgets and innovative financing mechanisms like public-private partnerships, is vital, as funding often decreases post-elimination (15). This approach is emphasised in the Africa CDC New Public Health Order (30). Integrating NTD surveillance into broader health systems can enhance cost efficiencies by utilising existing infrastructure. Furthermore, the integration of vertical NTD programmes offers opportunities for joint campaigns and simultaneous screening of populations, reducing campaign fatigue (31). GLIDE has presented some interesting instruments to garner innovative financing for NTDs by presenting models that have worked for other disease programmes, debt swaps, milestone-based funding, etc. (32).
The AUC-Africa CDC joint meeting in December 2023 focused on the need for clear requests for specific NTD budget lines, increased allocations, efficient resource use, and transparent expenditure tracking to bolster NTD funding. Diversifying funding sources through in-kind donations and corporate social responsibility initiatives and advocating for tax and user fee exemptions on NTD-related drugs were highlighted as a means to lower financial barriers. The integration of resource mobilisation with other health and development programmes and high-level advocacy involving AU Nutrition Champions and African Leaders for Nutrition were recommended to secure political support and prioritise NTDs.
Nonetheless, international funding remains pivotal, providing financial and technical assistance, as demonstrated by models like the Global Polio Eradication Initiative. International funding for financial and technical support should be strategically allocated to targeted surveillance, rapid response, mobile health technologies, and digital reporting, enhancing decision-making. This includes training for healthcare workers, community initiatives, research and development, and environmental management like vector control, aligning with country objectives and ensuring cost-effective, multisectoral, and flexible use of resources.
The enthusiasm of donors and investors for disease elimination has increased funding and investment in activities aligned with elimination goals, like mass drug administration (MDA), surveys to assess whether MDA can be stopped, disease transmission assessments, and the development of elimination dossiers. The Reaching the Last Mile Fund’s expansion, with a $777.2 million boost, aims to extend elimination efforts for diseases like lymphatic filariasis and river blindness. AU MS are encouraged to leverage these resources, integrating post-elimination management activities and fostering new partnerships with the private sector, philanthropists, the diaspora, and NGOs to bolster NTD post-elimination efforts.
Maintaining elimination of NTDs in AU Member States requires a multifaceted approach that transcends achieving elimination targets, addressing health system challenges and broader socio-economic issues. Our analysis underscores the importance of continuous surveillance and integrated health frameworks for monitoring and managing potential NTD reemergence post-elimination. Integrating NTD surveillance with current health systems, like IDSR, using population-based surveys and sentinel surveillance, and developing post-elimination diagnostic tools are vital.
The proposed strategic interventions are designed to address the complex challenges posed by climate change, cross-border migration, urbanisation, and increased exposure to zoonotic and vector-borne NTDs. Robust surveillance systems, enhanced cross-border collaboration, and event-based surveillance frameworks can help detect and respond to disease reemergence quickly, particularly in areas with high mobility and varying endemicity. Integrating NTD management into broader health systems ensures that interventions are adaptable to environmental changes and urban growth. Moreover, fostering community engagement and capacity building strengthens local resilience and enhances the effectiveness of vector control measures, thereby reducing the risk of zoonotic and vector-borne diseases.
Africa CDC’s leadership in establishing event-based surveillance is crucial for swiftly detecting and responding to NTD reemergence. This initiative and Africa CDC’s comprehensive community healthcare worker programme are pivotal in addressing outbreaks and emerging diseases and can support AU MS in post-elimination NTD management. Enhancing CHW training to cover surveillance and management of eliminated NTDs is essential for quick response to potential reemergence. Africa CDC is also developing its internal Strategic Priorities for Endemic and NTDs using a bottom-top consultative approach with MS and other stakeholders to support MS with the elimination efforts of these diseases following an integrated and multisectoral approach.
We also highlight the necessity of cross-border surveillance and international collaboration, acknowledging the risk of NTD reemergence due to easy cross-border population movements. Successful coordination efforts in West Africa exemplify maintaining disease elimination. The persistence of NTDs is linked to socio-economic factors, necessitating multisectoral approaches and policies that support cross-border collaborations. Emphasising the inclusion of NTDs in UHC and allocating adequate resources for post-elimination surveillance and management, we advocate for diversified funding sources to maintain an effective NTD fight.
Our article advocates for a paradigm shift in post-elimination NTD management, promoting a proactive, integrated, and resource-efficient approach. Integrating mental health services into post-elimination strategies is crucial for addressing stigma and mental distress linked to NTDs. Africa CDC’s mental health unit, in collaboration with CBM Global, has launched a Mental Health Leadership Programme to emphasise the importance of mental health care, highlighting the mental health dimension in comprehensive NTD management post-elimination.
Another critical component is financial sustainability. A shift is required from donor-driven funding to diversified funding streams, including, but not limited to, integration of NTD-related budgets into national government budgets and other sources of innovative financing mechanisms that would keep the programmes going even after elimination has been achieved. A multisectoral strategy encompassing health, environmental management, and socio-economic development is crucial to avoid reemergence of NTDs. Supporting integrated policies at national and international levels is vital for securing necessary support and resources. Sustaining NTD elimination successes depends on strategic planning, resource allocation, continuous innovation, and strengthening partnerships, community engagement, and ongoing investment.
Nonetheless, although we outlined general strategies for post-elimination management of NTDs, we also recognise the heterogeneity in settings across AU MS concerning NTD distribution and the socioecological, political, and economic contexts, which may affect the prevalence or chances of reemergence of NTDs. For example, climatic variations, health infrastructure, political stability, and economic health of the country can affect how diseases are managed and controlled. Additionally, the progress a particular country has made towards eliminating or eradicating an NTD will also influence the strategies adopted. It is, therefore, essential to have context-specific tailored approaches with community-specific interventions. In this manner, flexible strategies shall be developed to suit the unique conditions of each Member State, ensuring that the management of NTDs is more efficient and sustainable post-elimination. This approach will be further enhanced by involving local stakeholders and utilising ndigenous knowledge to adapt such interventions for relevance and acceptance.
In conclusion, the feasibility of these interventions highly depends on political will, resource availability, and the ability to integrate NTD management into broader health and development frameworks. However, we strongly believe that sustainability can be achieved by leveraging and streamlining existing health systems and structures. Implementing simple, cost-effective interventions focused on preventing re-emergence is more economical than addressing an outbreak of a previously eliminated NTD. Promoting community ownership and ensuring that interventions are adaptable to local contexts are also crucial for long-term success.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
NC: Conceptualization, Writing – original draft, Writing – review & editing. JE: Writing – review & editing. IA: Writing – review & editing. HT: Writing – review & editing. SS: Writing – review & editing. CK: Writing – review & editing. AB: Writing – review & editing. AM: Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We extend our heartfelt thanks to the Africa CDC leadership for their unwavering support of the institution’s infectious disease programme. We are also grateful to Mr. Dickson Amanya, Communications and Graphics Design Officer at Africa CDC, for his invaluable assistance in developing the figure included in this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization. Global report on neglected tropical diseases 2023(2023). Available online at: https://www.who.int/publications/i/item/9789240067295 (Accessed March 31, 2024).
2. Caminade C, McIntyre KM, Jones AE. Impact of recent and future climate change on vector-borne diseases. Ann N Y Acad Sci. (2019) 1436:157–73. doi: 10.1111/nyas.13950
3. Kaseya J, Alimi Y, Aluso A, Habtemariam MK, Crowell TA, Ngongo AN, et al. Tackling the twin threats of pandemics and climate change: An agenda for action. J Public Health Afr. (2023) 14:2868. doi: 10.4081/jphia.2024.2868
4. African Union Commission. Agenda 2063: The Africa We Want(2015). Available online at: https://au.int/en/Agenda2063/popular_version (Accessed April 9, 2024).
5. African Union Commission. Africa Health Strategy 2016 – 2030(2016). Available online at: https://au.int/sites/default/files/documents/24098-au_ahs_strategy_clean.pdf (Accessed April 9, 2024).
6. United Nations. Transforming our world: the 2030 Agenda for Sustainable Development(2015). Available online at: https://wedocs.unep.org/20.500.11822/9814 (Accessed March 31, 2024).
7. African Union. Continental Framework on the Control and Elimination of Neglected Tropical Diseases in Africa by the Year 2030(2022). Available online at: https://unitingntds.cdn.ngo/media/documents/CF_EN.pdf (Accessed March 31, 2024).
8. Africa Centres for Disease Control and Prevention. Africa CDC Strategic Plan 2023 – 2027(2023). Available online at: https://africacdc.org/download/africa-cdc-strategic-plan-2023-2027/ (Accessed March 31, 2024).
9. Ortu G, Williams O. Neglected tropical diseases: exploring long term practical approaches to achieve sustainable disease elimination and beyond. Infect Dis Poverty. (2017) 6:147. doi: 10.1186/s40249-017-0361-8
10. Hatherell H-A, Simpson H, Baggaley RF, Hollingsworth TD, Pullan RL. Sustainable surveillance of neglected tropical diseases for the post-elimination era. Clin Infect Dis. (2021) 72:S210–6. doi: 10.1093/cid/ciab211
11. Lammie P, Solomon A, Secor E, Peeling R. Diagnostic needs for NTD programs, in: The Causes and Impacts of Neglected Tropical and Zoonotic Diseases: Opportunities for Integrated Intervention Strategies (2011). Washington (DC: National Academies Press (US. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK62529/ (Accessed March 31, 2024).
12. Mercy K, Balajee A, Numbere T-W, Ngere P, Simwaba D, Kebede Y. Africa CDC’s blueprint to enhance early warning surveillance: accelerating implementation of event-based surveillance in Africa. J Public Health Afr. (2023) 14:2827. doi: 10.4081/jphia.2023.2827
13. Cairncross S, Muller R, Zagaria N. Dracunculiasis (Guinea worm disease) and the eradication initiative. Clin Microbiol Rev. (2002) 15:223–46. doi: 10.1128/CMR.15.2.223-246.2002
14. World Health Organization. Ending the neglect to attain the Sustainable Development Goals: A road map for neglected tropical diseases 2021–2030(2020). Available online at: https://www.who.int/publications/i/item/9789240010352 (Accessed March 31, 2024).
15. Dorkenoo MA, Tchankoni MK, Yehadji D, Yakpa K, Tchalim M, Sossou E, et al. Monitoring migrant groups as a post-validation surveillance approach to contain the potential reemergence of lymphatic filariasis in Togo. Parasit Vectors. (2021) 14:134. doi: 10.1186/s13071-021-04644-2
16. Katabarwa MN, Zarroug IMA, Negussu N, Aziz NM, Tadesse Z, Elmubark WA, et al. The Galabat-Metema cross-border onchocerciasis focus: The first coordinated interruption of onchocerciasis transmission in Africa. PloS Negl Trop Dis. (2020) 14:e0007830. doi: 10.1371/journal.pntd.0007830
17. Gustavsen K, Sodahlon Y, Bush S. Cross-border collaboration for neglected tropical disease efforts—Lessons learned from onchocerciasis control and elimination in the Mano River Union (West Africa). Global Health. (2016) 12:44. doi: 10.1186/s12992-016-0185-5
18. Tilahun B, Gashu KD, Mekonnen ZA, Endehabtu BF, Angaw DA. Mapping the role of digital health technologies in the case detection, management, and treatment outcomes of neglected tropical diseases: a scoping review. Trop Med Health. (2021) 49:17. doi: 10.1186/s41182-021-00307-1
19. The Lancet Digital Health. Technology for world elimination of neglected tropical diseases. Lancet Digit Health. (2023) 5:e51. doi: 10.1016/S2589-7500(23)00003-1
20. World Health Organization. Advancing the management of skin-related neglected tropical diseases in Ghana: Exploration of gender-related factors and mobile technology (2022). News release. Available online at: https://tdr.who.int/newsroom/news/item/14-12-2022-advancing-the-management-of-skin-related-neglected-tropical-diseases-in-Ghana-exploration-of-gender-related-factors-and-mobile-technology (Accessed March 31, 2024).
21. Malaria Consortium. Strengthening primary healthcare for neglected tropical diseases in Ethiopia(2018). Available online at: https://www.malariaconsortium.org/media-download-file/201909030215/researchbriefstrengtheningprimaryhealthcareforntds.pdf (Accessed March 31, 2024).
22. Emeto DC, Salawu AT, Salawu MM, Fawole OI. Recognition and reporting of neglected tropical diseases by primary health care workers in Ibadan, Nigeria. Pan Afr Med J. (2021) 38:224. doi: 10.11604/pamj.2021.38.224.20576
23. Corley AG, Thornton CP, Glass NE. The role of nurses and community health workers in confronting neglected tropical diseases in sub-Saharan Africa: A systematic review. PloS Negl Trop Dis. (2016) 10:e0004914. doi: 10.1371/journal.pntd.0004914
24. Bukachi SA, Mumbo AA, Alak ACD, Sebit W, Rumunu J, Biéler S, et al. Knowledge, attitudes and practices about human African trypanosomiasis and their implications in designing intervention strategies for Yei county, South Sudan. PloS Negl Trop Dis. (2018) 12:e0006826. doi: 10.1371/journal.pntd.0006826
25. Koschorke M, Al-Haboubi YH, Tseng P-C, Semrau M, Eaton J. Mental health, stigma, and neglected tropical diseases: A review and systematic mapping of the evidence. Front Trop Dis. (2022) 3:808955. doi: 10.3389/fitd.2022.808955
26. World Health Organization. World Organization of Family Doctors. Integrating Mental Health into Primary Care: A Global Perspective(2008). Available online at: https://www.who.int/publications/i/item/9789241563680 (Accessed March 31, 2024).
27. Makin S. Mental health: The invisible effects of neglected tropical diseases. Nature. (2023). doi: 10.1038/d41586-023-02973-z
28. Eaton J, Afolaranmi T, Tsaku P, Nwefoh E, Ode P, Baird T, et al. Integration of services for Neglected Tropical Diseases and mental health in Nigeria: development of a practical model informed by international recommendations, contextual factors and service-user perspectives. Int Health. (2023) 15:iii47–58. doi: 10.1093/inthealth/ihad074
29. Davies B, Kinfe M, Ali O, Mengiste A, Tesfaye A, Wondimeneh MT, et al. Stakeholder perspectives on an integrated package of care for lower limb disorders caused by podoconiosis, lymphatic filariasis or leprosy: A qualitative study. PloS Negl Trop Dis. (2022) 16:e0010132. doi: 10.1371/journal.pntd.0010132
30. African Union. Call To Action: Africa’s New Public Health Order(2022). Available online at: https://africacdc.org/news-item/call-to-action-africas-new-public-health-order/ (Accessed April 9, 2024).
31. Koffi AP, Yao TAK, Barogui YT, Diez G, Djakeaux S, Zahiri MH, et al. Integrated approach in the control and management of skin neglected tropical diseases in three health districts of Côte d’Ivoire. BMC Public Health. (2020) 20:517. doi: 10.1186/s12889-020-08632-6
32. Global Institute for Disease Elimination. Innovative finance for neglected tropical diseases discussion paper(2023). Available online at: https://glideglobal.wpenginepowered.com/wp-content/uploads/2023/02/280223_IF-NTD-DISCUSSION-PAPER_final.pdf (Accessed March 31, 2024).
Keywords: neglected diseases, sustainable development, disease eradication, African Union, delivery of healthcare, integrated, mental health, universal health care
Citation: Chotun N, Eaton J, Anagbogu IA, Tesfahunei HA, Shawa S, Karutu C, Bolarinwa A and Mohammed A (2024) Sustaining success through strategies for post-elimination management of neglected tropical diseases in African Union Member States. Front. Trop. Dis 5:1421522. doi: 10.3389/fitd.2024.1421522
Received: 22 April 2024; Accepted: 12 July 2024;
Published: 08 August 2024.
Edited by:
Yenddy Carrero, Technical University of Ambato, EcuadorReviewed by:
Thuan Thi Nguyen, Institute of Tropical Medicine Antwerp, BelgiumCopyright © 2024 Chotun, Eaton, Anagbogu, Tesfahunei, Shawa, Karutu, Bolarinwa and Mohammed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nafiisah Chotun, bmFmaWlzYWguY2hvdHVuQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.