
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Trop. Dis., 21 November 2024
Sec. Neglected Tropical Diseases
Volume 5 - 2024 | https://doi.org/10.3389/fitd.2024.1372267
This article is part of the Research TopicMorbidity Management of Lymphatic Filariasis: A Focus on Filarial Hydrocele and LymphoedemaView all 4 articles
Morbidity Management and Disability Prevention (MMDP) remains a key aspect of the Global project for the Elimination of Lymphatic Filariasis (GPELF) a program launched by WHO in the year 2000. In line with this mandate the Ministry of Health in Kenya having already achieved 95% Mass Drug Administration (MDA) by use of door-to-door drug administration (DA-albendazole and diethylcarbamazine) yearly for 5 years. The dosages used were albendazole 400mg and diethylcarbamazine citrate 6mg/Kg orally. Three drug combination by adding ivermectin (150ug/Kg) have been used in areas where the success of DA was suboptimal following the recommendation by WHO to speed up the elimination of lymphatic filariasis and areas endemic with onchocerciasis. A training workshop for surgeons and medical officers was organized in May 2023 for the surgical management of lymphatic hydroceles in the Coastal region of Kenya which is an endemic area for lymphatic filariasis. During the index training workshop in Kilifi, we encountered and managed an 83-year-old male who lived with a large grade 4 hydrocele and a right inguinal hernia for over six decades. We share our experience with this case report in this manuscript (large bilateral filarial hydrocele and right inguinal hernia for a period of sixty years. The objective of writing this report is to share our experience and the progress of MMDP program in Kenya.
Filarial hydrocele remains a neglected tropical disease in various parts of the world. It is caused by Wuchereria bancrofti and spread by the anopheles or culex mosquito. The prevalence of hydroceles in the coastal region of Kenya is not documented despite the many cases that we encounter in this region. In the coastal region of Kenya Mwobobia et, al looked at the proportion of major surgeries in some hospitals as a proxy for hydrocele prevalence and found that hydrocelectomies constituted up to 27% of all the surgical cases between 1991-1993 (1). Lymphatic filariasis leading to hydrocele formation remains to be a chronic condition with significant morbidity that can be quite debilitating to the patient (2, 3). In 1997 the World Health Agency (WHA) in a resolution 50.29 recommended the formation of Global Project for Elimination of Lymphatic Filariasis (GPELF). There were two components of this project, to stop the spread of the infection by interrupting transmission by Mass Drug Administration (MDA) and alleviate the suffering of affected populations (controlling morbidity)-MMDP-Morbidity Management and Disability Prevention. Despite this campaign, the goals of this project have not been realized in many endemic countries. MMDP remains a key aspect in the management of these patients (4, 5) but has just begun in Kenya in the last one year. Diagnosis using clinical examination by transillumination and scrotal ultrasonography usually demonstrates fluid accumulation in the scrotum and rules out other causes of scrotal swelling. While ultrasonography can reveal characteristics like size, shape, and echogenic material that might suggest infection, it cannot confirm or exclude it on its own. Additional evaluations, such as blood tests (e.g., white blood cell count, CRP), urine tests for pyuria, and hydrocele fluid aspiration for culture, are necessary to rule out or confirm infection. In terms of surgical management there has been a move towards standardizing an approach that is best suited to manage filarial hydrocele (6, 7). Surgery to correct this condition results in improved quality of life for these patients and rapid reintegration back into society (8–10). Total excision of the sac is deemed the best technique with minimal post operative complications and recurrence (7). Training of medical personnel has been ongoing in various endemic countries (11, 12).
In Kenya, training for healthcare professionals was started during a recent workshop with a second one being held in October 2023. Over 114 surgeries were performed during these two workshops in endemic areas of the coastal region of Kenya. Many more patients await surgery but due to lack of funding they continue to suffer.
The Department of Surgery at the University of Nairobi Faculty of Health Sciences organized a training workshop for the Kenya Ministry of Heath with funding from the African Medical and Research Foundation (AMREF). Two training camps were organized in May and October 2023 lasting 5 days in each session and successfully managed to operate on 114 patients. Trainings were also done for the local surgeons and medical officers with the aim of building capacity and transferring Knowledge. We present a case of an 83-year-old male patient, a resident of Kilifi County in the coastal region of Kenya who presented with over six decades of bilateral scrotal and right inguinal swellings. The scrotal swelling had been progressively increasing in size up to the level of the knee since his early twenties. He noticed subsequent reduction in the size of the penis. He complained of a feeling of heaviness and occasional pain. The patient also reports that he noticed a right inguinal swelling that reduced spontaneously on lying down. He had no associated lower limb swelling but reports occasional episodes of fever on and off which had resolved after treatment with oral medications in a previous consultation. He reported an episode of attempted aspiration of the fluid in the early 70s by some traditional healers. He reported that he did not seek treatment from health facilities before presenting to us due to the long distance to the nearest health facility and financial constraints. He learned of the surgical camp from Neglected Tropical Disease coordinators employed by the Ministry of Health who visit remoted villages to ensure the success of the MDA and MMDP programs He had no known comorbidities. He is married with nine children, an avid tobacco chewer and consumed local brew. On examination he had a reducible, non-tender right inguinal swelling. The scrotum was markedly swollen bilaterally measuring 62cm wide, non-tender with a buried penis with Capuano and Capuano classification Grade 4, and Stage 4 (13). The transillumination test was positive and the swelling was noted to contain fluid with the ultrasound confirming the diagnosis (Figure 1).
The patient was admitted the day before surgery and kept nil by mouth from midnight. Cardiac assessment by Echocardiogram and ECG were done. Shaving was done on the table and a social wash with liquid soap was done after spinal anesthesia was given. Skin preparation was done with povidone iodine and draped to ensure sterility. A median raphe incision, 2 cm below the penoscrotal junction was made. Layer by layer dissection was done to the tunica vaginalis which was dissected and delivered after draining the fluid by electro suction (Figure 2). A total of three liters of straw-colored filarial fluid was drained bilaterally (Figure 3). Complete resection of the parietal layer of the tunica vaginalis was done leaving a 2cm margin all round. A 3/0 round body vicryl suture was used to stitch the resected margin in an interlocking manner 1 cm apart (Figure 2). The same procedure was replicated on the other side. This ensured hemostasis and closing of the lymphatic channels. This prevents recurrence of the hydrocele and formation of a hematoma. The testes were repositioned back into the scrotum and closed in two layers without a drain. A right herniorrhaphy was done with a prolene mesh (Figure 4).
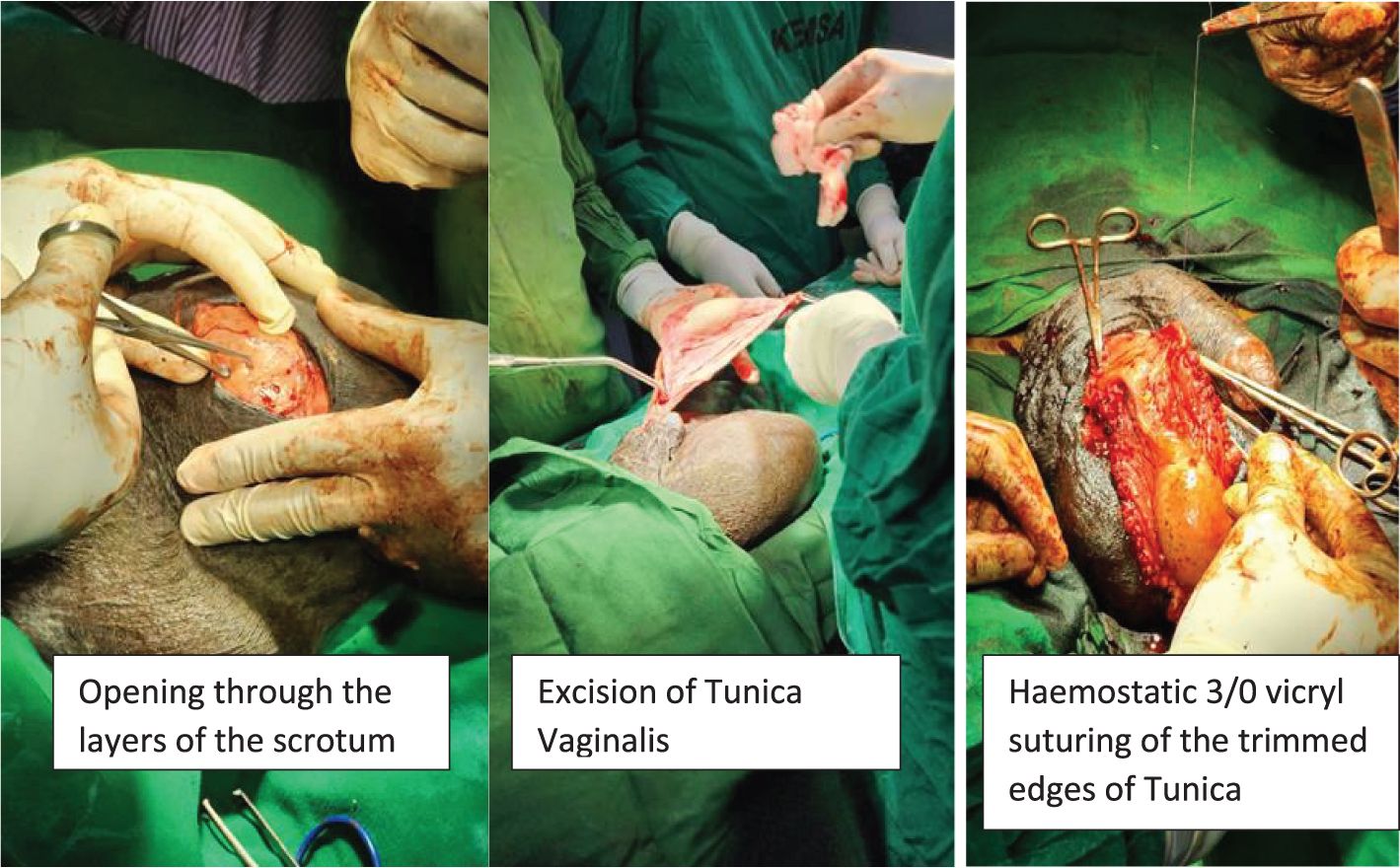
Figure 2. Median raphe incision with opening of the layers of the scrotum, tunica identified and fluid drained. Total excision of the sac with attention to hemostasis an interlocking vicryl 3/0 suture was used. (photos taken with consent).
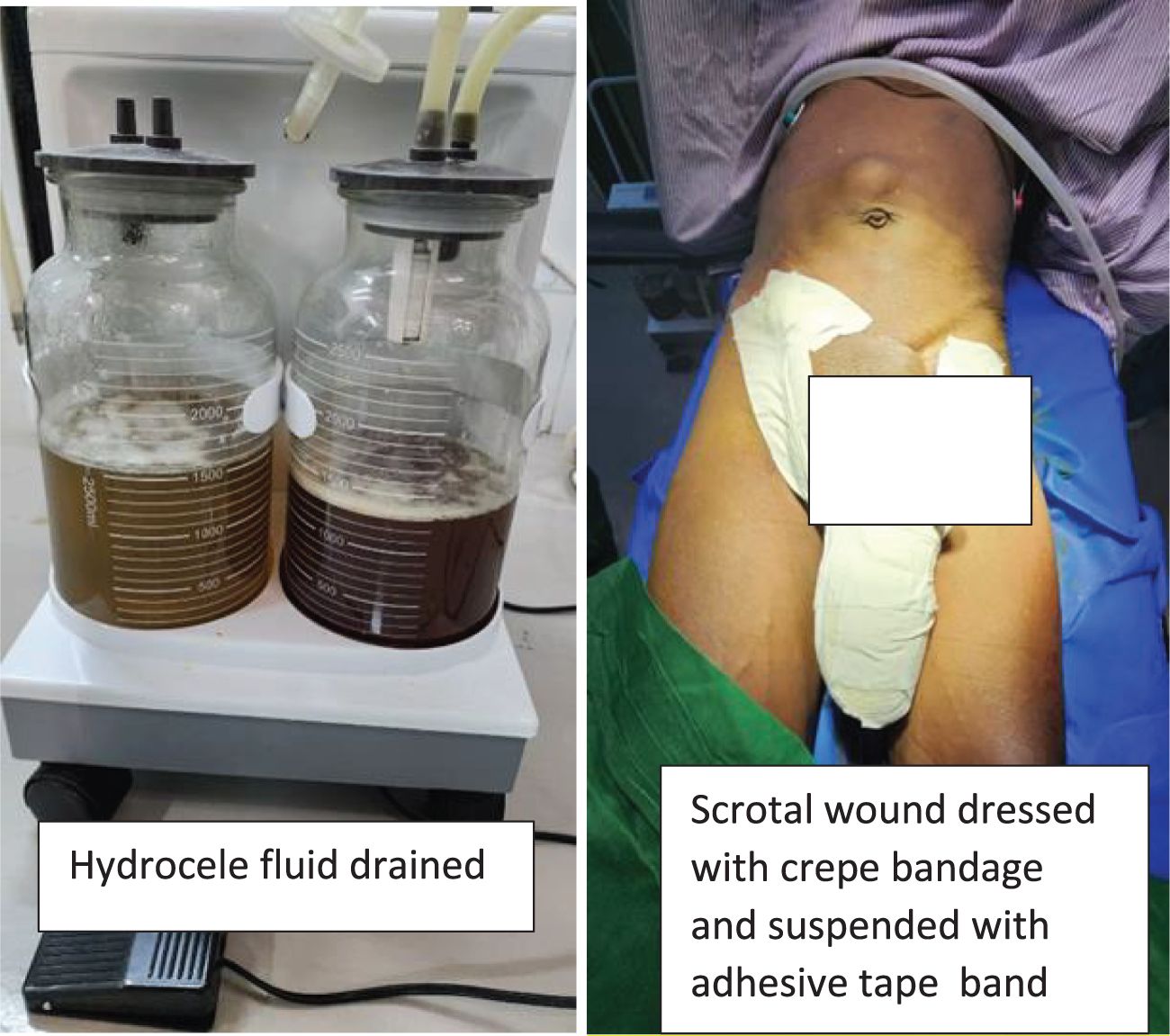
Figure 3. Fluid drained from both hydroceles approximately three liters bilaterally and dressing applied post operatively. (photos taken with consent).
Patient did well postoperatively and discharged to continue with the pressure dressing at the nearest health facility. He later developed a hematoma that was subsequently evacuated with follow-up scrotoplasty owing to the redundant skin that persisted three months later. The cost of this patient’s treatment including the surgical camp was sponsored by the END fund through AMREF.
Lymphatic filariasis is a debilitating parasitic infection caused primarily by Wuchereria bancrofti and transmitted by mosquitoes such as the Anopheles and Culex species. One of the most common clinical manifestations of lymphatic filariasis is the development of hydroceles. Lymphatic filariasis (LF) hydrocele primarily results from lymphatic dilation rather than obstruction. Research by Noroes and Dreyer shows that filarial parasites, particularly Wuchereria bancrofti, lodge in the lymphatic system, causing inflammation and dysfunction. This leads to vessel dilation, increased permeability, and lymphatic leakage, which contributes to hydrocele formation. While obstruction was once considered the main cause, lymphatic dilation and failure are now recognized as the key factors, shaping more effective treatment and prevention strategies (14). The morbidity associated with lymphatic hydroceles can be profound, often leading to significant physical discomfort, social stigma, and economic burden for affected individuals and their families.
The Global Program to Eliminate Lymphatic Filariasis (GPELF), launched by the World Health Organization (WHO) in 2000, includes two main components: interrupting the transmission of the disease through mass drug administration (MDA) and managing morbidity and preventing disability through the Morbidity Management and Disability Prevention (MMDP) strategy. While Kenya has achieved high coverage in MDA, MMDP efforts have only recently begun, with significant challenges remaining in many endemic areas.
The patient described in this report, an 83-year-old male from Kilifi County, presented with a large, longstanding bilateral scrotal swelling and a right inguinal hernia. The condition had persisted for over six decades, illustrating the chronic nature of filarial hydroceles when left untreated. The surgical intervention performed included complete excision of the tunica vaginalis bilaterally and herniorrhaphy for the associated inguinal hernia. This approach aligns with current best practices that recommend complete removal of the hydrocele sac to prevent recurrence and reduce the risk of postoperative complications (11).
Surgical management of lymphatic hydrocele, particularly in endemic regions, has been shown to significantly improve the quality of life for affected patients by alleviating symptoms and reducing the associated stigma (10). The technique used in this case, complete excision of the parietal layer of the tunica vaginalis with meticulous hemostasis and closure of lymphatic channels, has been associated with favorable outcomes, including reduced rates of recurrence and minimized postoperative complications such as hematoma formation.
Hydrocelectomy in filarial hydroceles can prove difficult due to the chronicity of the condition and the subsequent anatomical changes encountered. Care must be taken to prevent injury to the neurovascular structures. Attention to hemostasis is very important to prevent the attendant post operative complications. Patients are advised to wear scrotal support during the recovery period. Total excision of the sac has shown promising results in preventing complications and recurrence. Other methods for hydrocelectomy used in Kenya include Jaboulay and the lord’s procedure, aspiration of fluid and instillation of a sclerosing agent. These methods have been traditionally used in Kenya but have a very high recurrence rate. Psychological counselling is also an important aspect of patient care due to the stigma associated with the condition to reintegrate the patients back into society and long-term follow-up (15).
However, challenges such as postoperative complications, including hematomas and redundant scrotal skin requiring further surgical intervention (as seen in this case), highlighting the need for ongoing refinement of surgical techniques and postoperative care protocols. Additionally, the limited access to surgical care and the need for capacity building among healthcare workers in endemic regions remain significant barriers (16). This underscores the importance of training workshops and surgical camps, such as those conducted by the University of Nairobi in collaboration with AMREF, which aim to enhance local surgical capacity and ensure sustainable MMDP interventions.
The case underscores the importance of integrating surgical care into broader MMDP programs, as the elimination of lymphatic filariasis requires not only the interruption of transmission but also the management of morbidity among affected populations. As Kenya continues to scale up its MMDP activities, including the provision of surgical services for hydrocele management, there is a need for continued support, funding, and health system strengthening to address the needs of patients who remain untreated due to resource limitations.
Expanding access to surgical management and building local capacity are critical steps toward alleviating the burden of lymphatic filariasis and improving the quality of life for patients in endemic regions. Future efforts should focus on the integration of MMDP services into primary healthcare systems, ensuring that surgical care is available, accessible, and affordable for all patients in need.
The case of the 83-year-old male patient from Kilifi County underscores the critical role of surgical management in addressing the morbidity associated with lymphatic filariasis, particularly large hydroceles. Despite global efforts through the GPELF, including mass drug administration, the burden of chronic manifestations such as hydrocele remains significant in endemic regions like coastal Kenya. This case highlights the importance of comprehensive MMDP strategies that include not only drug interventions but also accessible and effective surgical care.
Successful management of large hydroceles through surgery significantly improves patients’ quality of life, reduces stigma, and facilitates their reintegration into society. However, challenges such as limited resources, insufficient training, and the need for ongoing postoperative care highlight the importance of capacity building and sustainable health interventions.
The recent training workshops conducted in Kenya represent a positive step towards building local capacity and improving surgical outcomes for patients with lymphatic filariasis. To achieve the full elimination of the disease, continued investment in MMDP programs, including surgical management and healthcare worker training, is essential. Addressing these needs will require a concerted effort from national health authorities, international organizations, and local communities to ensure that all affected individuals receive the care and support they need.
Standardization of the surgical procedure for filarial hydrocele is key in minimizing the expected complications. In cases of longstanding cases with more advanced stages, scrotoplasty may be considered to deal with the resultant redundant skin and the dead space that may result in hematoma formation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval was not required for the studies involving humans because it is not mandatory to get one in Kenya if a patient provides a written informed consent for a case report. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
CW: Data curation, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. SG: Writing – original draft. ES: Data curation, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Mwobobia IK, Muniu EM, Kombe Y, Wamae CN. Hydrocelectomy: a proxy for hydrocele prevalence in coastal Kenya. Ann Trop Med Parasitol. (2000) 94:479–84. doi: 10.1080/00034983.2000.11813566
2. Mackenzie CD, Mante S. Caring for patients in the global program to eliminate lymphatic filariasis. Int Health. (2020) 13:S48–54. https://academic.oup.com/inthealth/article/13/Supplement_1/S48/6043674.
3. Ton TGN, Mackenzie C, Molyneux DH. The burden of mental health in lymphatic filariasis. Infect Dis Poverty. (2015) 4:34. doi: 10.1186/s40249-015-0068-7
4. Lama Yonzon C, Padmawati RS, Subedi RK, Paudel S, Ghimire A, Murhandarwati EH. Exploring determinants of hydrocele surgery coverage related to Lymphatic Filariasis in Nepal: An implementation research study. PloS One. (2021) 16:e0244664. doi: 10.1371/journal.pone.0244664
5. Addiss DG, Brady MA. Morbidity management in the Global Programme to Eliminate Lymphatic Filariasis: a review of the scientific literature. Filaria J. (2007) 6:2. doi: 10.1186/1475-2883-6-2
6. Filarial hydrocele treatment & management: approach considerations, medical therapy, surgical therapy. (2024). Available online at: https://emedicine.medscape.com/article/438525-treatment?form=fpf (accessed November 8, 2024).
7. Mante SD, Gueye SM. Capacity building for the modified filarial hydrocelectomy technique in West Africa. Acta Trop. (2011) 120 Suppl 1:S76–80. doi: 10.1016/j.actatropica.2010.09.008
8. Sawers L, Stillwaggon E, Chiphwanya J, Mkwanda SZ, Betts H, Martindale S, et al. Economic benefits and costs of surgery for filarial hydrocele in Malawi. PloS Negl Trop Dis. (2020) 14:e0008003. doi: 10.1371/journal.pntd.0008003
9. Ahorlu CK, Dunyo SK, ASamoah G, Simonsen PE. Consequences of hydrocele and the benefits of hydrocelectomy: a qualitative study in lymphatic filariasis endemic communities on the coast of Ghana. Acta Tropica. (2001) 80:215–21. https://linkinghub.elsevier.com/retrieve/pii/S0001706X01001590.
10. Betts H, Martindale S, Chiphwanya J, Mkwanda SZ, Matipula DE, Ndhlovu P, et al. Significant improvement in quality of life following surgery for hydrocoele caused by lymphatic filariasis in Malawi: A prospective cohort study. PloS Negl Trop Dis. (2020) 14:e0008314. doi: 10.1371/journal.pntd.0008314
11. Available online at: https://hdi.no/wp-content/uploads/2018/03/lymphatic-filariasis-guide.pdf. (accessed October 29, 2024).
12. Beyene AD, Kebede F, Mammo BM, Negash BK, Mihret A, Abetew S, et al. The implementation and impact of a pilot hydrocele surgery camp for LF-endemic communities in Ethiopia. PloS Negl Trop Dis. (2021) 15:e0009403. doi: 10.1371/journal.pntd.0009403
13. Capuano GP, Capuano C. Surgical management of morbidity due to lymphatic filariasis: the usefulness of a standardized international clinical classification of hydroceles. Trop Biomed. (2012) 29:24–38.
14. Dreyer G, Norões J, Figueredo-Silva J, Piessens WF. Pathogenesis of lymphatic disease in bancroftian filariasis: a clinical perspective. Parasitol Today. (2000) 16:544–8. doi: 10.1016/S0169-4758(00)01778-6
15. Krishna Kumari A, Harichandrakumar KT, Das LK, Krishnamoorthy K. Physical and psychosocial burden due to lymphatic filariasis as perceived by patients and medical experts. Trop Med Int Health. (2005) 10:567–73. doi: 10.1111/j.1365-3156.2005.01426.x
Keywords: lymphatic filariasis, capacity building, filarial hydrocelectomy technique, filarial hydrocele, MMDP (Morbidity Management and Disability Prevention, MDA (Mass Drug Administration), coastal region of Kenya, Wuchereria bancrofti
Citation: Waihenya C, Githui S and Schouame E (2024) A large filarial hydrocele in Kenya: a case report. Front. Trop. Dis 5:1372267. doi: 10.3389/fitd.2024.1372267
Received: 17 January 2024; Accepted: 30 October 2024;
Published: 21 November 2024.
Edited by:
Sunny Doodu Mante, African Filariasis Morbidity Project, GhanaReviewed by:
Chiaka Anumudu, University of Ibadan, NigeriaCopyright © 2024 Waihenya, Githui and Schouame. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Charles Waihenya, Y2hhcmxlc3dhaWhlbnlhQHVvbmJpLmFjLmtl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.