- 1College of Social Sciences, Addis Ababa University, Addis Ababa, Ethiopia
- 2Centre for Global Health Research, Brighton and Sussex Medical School, Brighton, United Kingdom
- 3School of Public Health, Addis Ababa University, Addis Ababa, Ethiopia
Introduction: Understanding contextual factors that influence the implementation and outcome of interventions is crucial to improving them. Outcome and process evaluation studies have to date focused on the successes and limitations of interventions with little consideration of external factors that could either facilitate or impede them. Guided by the Context and Implementation of Complex Intervention (CICI) framework, we evaluated the effect of contextual factors on a health intervention implemented against the neglected tropical disease (NTD) podoconiosis in Ethiopia.
Method: We purposefully selected a health intervention jointly implemented by two NGOs in podoconiosis-endemic districts in Northwestern Ethiopia. We employed an exploratory mixed methods approach, and data were collected between April and July 2022. We first conducted document analysis, observations, 4 focus group discussions, 32 in-depth interviews and 19 key informant interviews. Subsequently, we administered a survey to 369 rural residents, of whom 42 were affected by podoconiosis. The qualitative data were managed with NVivo version 12 software. The quantitative data were analyzed using Stata version 15 software.
Results: Most project activities were implemented as per the initial plan and the intervention reached patients that never had access to treatment services before. Contextual factors (geographical, epidemiological, socio-economic, socio-cultural, ethical, legal and political) and lived experience of patients influenced the implementation and outcome of the intervention. Most of the contextual factors pose constraints on implementation and affected the acceptability and sustainability of project activities. On the other hand, political context such the commitment of the government to rollout national programs and set up NTD structures at district level positively influenced the implementation of the intervention.
Conclusion: Health intervention implementors should be aware of the interactive effects of contextual factors wherein interventions are put into practice. Minimizing the constraining effects of these contextual factors while utilizing opportunities presented by them might help implement optimal strategies to improve the lives of individuals affected by podoconiosis and similar NTDs.
Introduction
Neglected Tropical Diseases are conditions whose epidemiology is often related to environmental factors and which mostly affect impoverished and vulnerable groups living in remote areas (1). The diseases cause debilitating physical consequences and impose social and economic burdens on about one billion people (WHO, 2020). Attempts have been made to control NTDs through mass drug administration (MDA), water, sanitation, and hygiene (WASH), vector control, health education, and micronutrient supplementation (1). Some studies reported that the interventions could not bear positive results due to reasons related to delivery strategy (2, 3). On the other hand, interventions that utilized community structures such as schools and religious organizations have been effective in reducing the impact of NTDs (4–6).
Some NTDs are not curable with drug therapy but require self- and continued care to manage the impact of the conditions and limit disability. Among these is podoconiosis, a disease that develops when naturally susceptible individuals walk barefoot on irritant soil (7).
Podoconiosis is a considerable public health problem in Ethiopia About 35 million Ethiopians are at risk through exposure to the irritant soil (8). It is highly disfiguring, causes severe swelling and chronic disability in patients. Affected individuals face acute adenolymphangitis (acute attack) characterized by swollen and red leg, chills and fever (9). Podoconiosis also limits patients’ mobility and poses a large economic burden on affected families (10). A study estimated that the total economic of podoconiosis in the country was US$213.2 million annually and over 91% of this cost resulted from productivity cost. Podoconiosis is accounted for the loss of 172, disability-adjusted years (DALYs) annually (11). The condition and the disability resulting from it are also associated with depression among patients (12). Studies have also shown that people with podoconiosis are severely stigmatized, and this is usually manifested through exclusion from community events, difficulties finding employment or gaining education, or through divorce or termination of marriage plans (13–15).
Podoconiosis is entirely preventable if individuals wear shoes and wash their feet with soap and water consistently (7). Thus, culturally tailored strategies to enhance individuals’ understanding about the disease and their ability to take preventive action could be highly effective prevention strategies (13, 16).
The Ethiopian government has identified podoconiosis as one of the Neglected Tropical Diseases (NTDs) to be prioritized. The country’s Master Plan for Neglected Tropical Diseases (2012-15) called for efforts to disseminate health education through local administration offices, religious institutions and schools to prevent the disease and reduce the stigma against individuals affected by podoconiosis.
In parallel, a handful of interventions have been implemented by non-government organizations (NGOs) to prevent and control podoconiosis, notably by International Orthodox Christian Charities (IOCC) and the National Podoconiosis Action Network (NaPAN), an umbrella organization that coordinates the work of its member organizations working on preventing and controlling podoconiosis in Ethiopia (NaPAN, nd). These and other organizations have been implementing population-level interventions in podoconiosis-endemic areas of Ethiopia (17).
There is some evidence from implementing organizations which suggests that health intervention activities help improve treatment for patients and enhance people’s understanding of the disease in Ethiopia (18). A recent study also indicated that health education, skin care training and foot hygiene supplies could reduce the burdens of the disease; thereby increasing patients’ mobility, economic productivity and quality of life (19). A holistic care package helped to improve the physical health, quality of life and social support among individuals affected by LF, podoconiosis and leprosy in Ethiopia (20).
However, little academic evaluation of the process of implementation of social interventions exists. Studying critical factors such as contexts that may either promote or restrain social interventions from a social science perspective is still largely uncharted territory in Low and middle income countries (LMICs). Indeed, assessing interventions in such a comprehensive manner is relatively new in the field of health program evaluation (21). Designing complex social interventions requires assessing the process of implemented interventions, their setting and contextual factors in order to draw lessons from their success and failures. Such a view helps us consider social interventions together with the system they attempt to change (22, 23).
With this gap in mind, we selected the Context and Implementation of Complex Intervention (CICI) framework to evaluate a social intervention known as “Next steps for podoconiosis patients in Amhara region” that aimed to improve the lives of patients in Ethiopia. The CICI framework emphasizes contextual factors, the setting and the implementation process in an integrated way to evaluate the success of a given intervention in reaching targeted populations (21). Conducting evaluation in this manner will help provide inputs to social interventions to end the suffering of people with podoconiosis. Blacklock and colleagues (24) argued that although the success of an intervention depends very much on local contexts, only a few trials have been conducted in sub-Saharan Africa and even fewer have adopted methodologies which allow the effect of context to be assessed. In this manuscript, we focused on the CICI’s seven contextual domains including geographical, epidemiological, socio-cultural, socio-economic, ethical, legal and the political domain. The geographical context includes the physical environment and resources (21). The epidemiological context refers to the distribution and the attributable burden of a disease [Rychetnik et al., cited in (25)]. Socio-cultural and socioeconomic contexts encompass beliefs, values, norms and material aspect of culture that constitute people’s way of life (21, 26–28). Ethical context comprises reflection of morality and standards of conduct that guide the behavior of intervention agents (29). The legal domain on the other hand includes rules and regulations that aim to protect the target population’s rights (30). The political context refers to the range of organizations and their interest that could influence health interventions (31).
Materials and methods
Study setting and population
We purposefully selected an intervention known as “Next steps for podoconiosis patients in Amhara region” from among social interventions being implemented against the neglected tropical lymphoedema, podoconiosis. Funded by IZUMI Foundation, the intervention was jointly implemented by International Orthodox Christian Charities (IOCC) and the National Podoconiosis Action Network (NaPAN). The intervention included enhancing the capacity of health professionals to deploy them as trainers for community health workers [mostly known as Health Extension Workers (HEWs)]. The NGOs also distributed supplies to affected individuals. The trained health professionals trained community health workers and provided lymphedema services to affected individuals at healthcare facilities over a three-month period. The health professionals washed affected individuals’ feet with water and soap, bandaged their wounds and showed them elevation exercise to improve lymphatic function. The intervention required affected individuals to attend services at healthcare center at least three times (once in every month). Upon the completion of the three services, affected individuals graduate from the intervention are expected to continue self-care procedure at home. To enhance understanding of podoconiosis and reduce stigmatizing attitudes against patients, the intervention implementors also trained and deployed local health professionals to conduct health education intervention for affected and unaffected members of the communities at healthcare centers and churches. We intentionally selected this intervention since it was active during the evaluation period and was complex in nature with a range of different components and target groups.
Amhara region is the second largest and most populous regional state in Ethiopia. The region was projected to have 22.8 million people in 2022 (32). Amhara region is roughly located between latitude 90 21’ to 140 0’ North and longitude 360 20’ to 400 20’ East (33). The estimated average annual rainfall is 1,150 mm (34). About 4% of the adult population in the region is affected by podoconiosis and 64 of 164 districts are identified as podoconiosis-endemic areas (35). The selected intervention was implemented in seven districts between August 2020 and March 2023 in Amhara region, Ethiopia. We purposefully selected two districts, Yilmana Densa from West Gojjam and Dera from South Gondar Zones of Amhara region, as they were among the districts with the highest number of cases of podoconiosis in Ethiopia (16). Red clay soils are the most dominant soil in the districts (33). The two districts are homogeneous in terms of economic activities and cultural contexts. Both districts were reported to have about 10% podoconiosis prevalence. From these districts, we purposefully selected four kebeles (smallest administrative units) considering higher prevalence of the disease. We selected Shime kebele (with 145 affected individuals) from Dera district and Agita, Fetlo and Abika kebeles in Yilmana Densa district (with 62, 56 and 51 affected individuals, respectively).
Study design
We employed an exploratory sequential mixed methods design. There were two distinct phases: qualitative followed by quantitative (36).
The study team conducted situational analysis to obtain a broader understanding of podoconiosis in Ethiopia. We then conducted a desk review to examine the socioeconomic, political, legal and ethical contexts that might influence the effectiveness of the selected intervention.
We conducted in depth interviews (IDIs) with 32 purposefully selected affected individuals to the point of data saturation between May and June 2022. Lists of affected individuals were obtained from health posts. Of the affected individuals, 28 were above the age of 30 and 14 were females. Five affected individuals were divorced while another five were never married. Most of the affected individuals had persistent swelling, warty lesions and nodules above their ankles. Only four of the IDI participants had formal education. We studied their lived experience and their views about the outcomes of the intervention. We included affected individuals who took part in the intervention and those who were not part of the intervention. All interviews were conducted privately in the respondents’ compound.
We also conducted four Focus Group Discussions (FGD) in the two districts between April and May 2022: two with women and two with men, to elicit their views about the context and members’ participation in the intervention. Six men took part in the FGD at Yilmana Densa district; and eight individuals participated in each of the remaining three FGDs. Group discussion guides were prepared in line with the CICI framework. Group discussions were conducted in healthcare facilities on Sundays.
We also conducted 20 Key Informant Interviews (KII) with policy makers, the staff of the implementing NGOs, health workers and local administrators to understand the political and socio-economic context, the intervention components and the execution of project activities. The interviews were conducted in the offices of the key informants.
Following the qualitative phase, we administered a survey with 369 respondents. We conducted a census of households prior to selecting samples and administering the survey. We identified 6,439 household representatives in the kebeles. Assuming +/- 5 confidence interval and 95% confidence level, the minimum sample size was estimated at 363. Considering 10% podoconiosis prevalence rate in the districts, we allocated 10% of the sample (36) for affected household representatives. We decided to oversample the affected population, anticipating refusal. We surveyed 369 household representatives. 42 of the respondents were affected by podoconiosis. We included patients at different stage of podoconiosis as identified by local health professionals. Local health professionals classified the disease stage as ‘mild’, ‘medium’ and ‘severe’ based on the swelling and severity of leg wounds. 257 of the respondents were from Yilmana Densa district, and the remainder from Dera district. The survey assessed the socioeconomic and socio-cultural context, including knowledge about podoconiosis and shoe wearing behaviour, involvement of rural residents in the intervention and the acceptability of the intervention.
The questionnaire was developed in English, translated into Amharic (the main language used in this setting), checked for accuracy and back translated to English. We recruited interviewers (N=8) who had first degrees in social science and related studies using informal networks. The interviewers received four days’ training on the objectives of the study, the items included in the survey questionnaire, REDCap software, and how to carry out the survey using tablet computers. The data collectors conducted interviews in respondents’ homes between July 15 and 29, 2022.
Data analysis
The systemization and analysis of the qualitative data was conducted with NVivo version 12 Qualitative Data Analysis software. In depth Interviews, FGDs and key informant interviews were audio-recorded in Amharic, transcribed and translated into English. We then imported the translated transcripts and selected documents into NVivo software and did structural coding. Structural coding applies a content-based or conceptual phrase representing a topic of inquiry to a segment of data that relates to a specific research question used to frame the interview (37, p. 124). The large data were structured into small pieces in line with the contextual domains of the CICI framework. To capture the lived experiences of affected individuals, we conducted process and values coding (38).
Quantitative data were collected using tablets and the REDCap application. The data were then exported to Stata version 17. Data were checked carefully for missing values and inconsistencies. Univariate and bivariate were executed on survey responses. These included respondents’ demographic and socio-economic background, knowledge about podoconiosis and involvement in the social intervention. Both qualitative and quantitative data were integrated at the analysis stage.
Ethical considerations
The study obtained ethical clearance from the Research Governance and Ethics Committee (RGEC) of Brighton and Sussex Medical School (BSMS) (Reference: ER/BSMS9E3G/8) and the Ethiopian Society of Sociologists, Social Workers and Anthropologists (ESSSWA) (Reference: ESSSWA 019/21). The Amhara Public Health Institute, regional and zonal health bureaus granted permission to conduct the study in the selected areas.
Participant information sheets were written in simple lay language and were translated into Amharic, enabling participants to understand the aims, procedures, and potential risks of participation. Data collectors read out the participant information sheets. Thumbprints or signatures were taken after the completion of interviews. Each participant received 200 ETB ($4) to compensate for their time. Confidentiality and anonymity were assured by not collecting personal identification information such as names, ID numbers, phone number, or house numbers. Data were accessible only to necessary research staff. Participants were identified only by questionnaire ID number. The data were transferred to the BSMS 5S Foundation data repository under the supervision of the project’s Data Manager according to the General Data Protection Regulations (GDPR).
Results
Respondents’ socio-economic characteristics
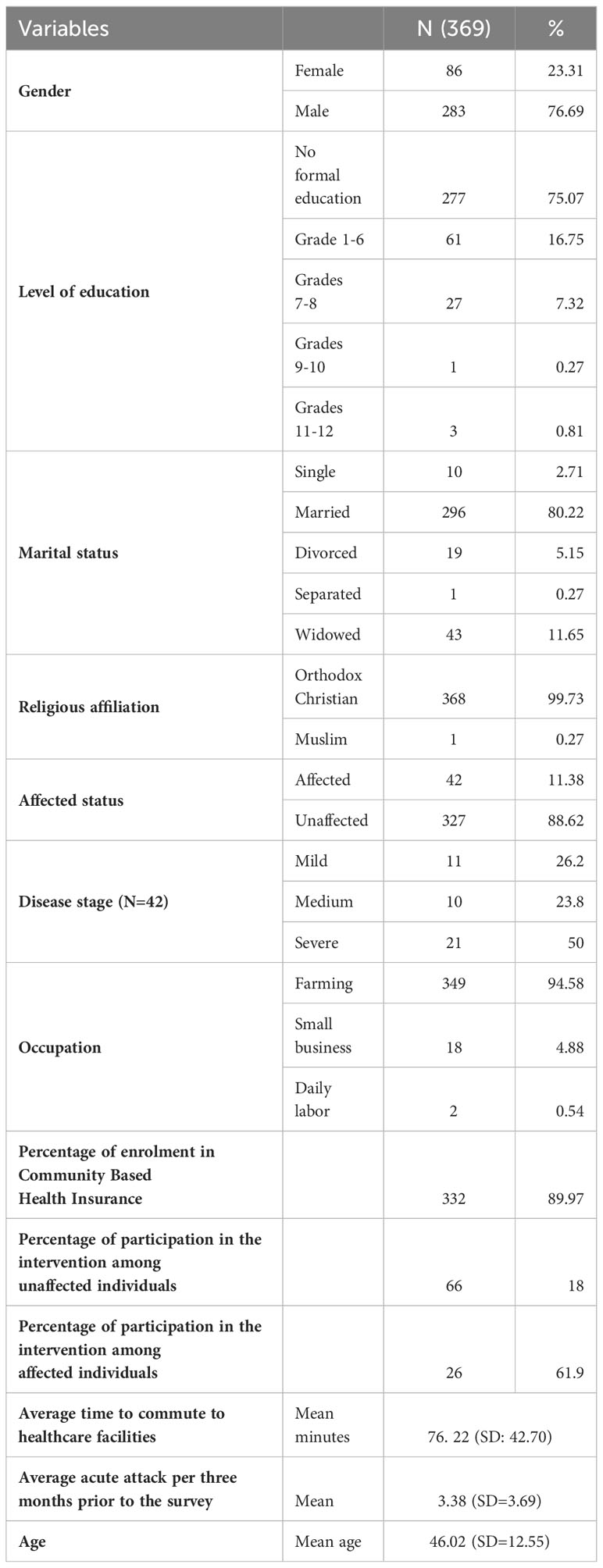
All individuals approached for the survey were willing to take part. As shown in Table 1, a total of 369 individuals took part in the survey, of whom 11.4% were affected by podoconiosis. About three quarters of respondents were male and had no formal education; their mean age was 46.02 (SD=12.5) years. The overwhelming majority (94.6%) reported farming as their occupation. Nearly 90 percent of the respondents were enrolled in Community Based Health Insurance (CBHI). On average, the respondents spent 76 minutes for two-ways commutes to and from healthcare facilities. About 18% of unaffected members of the community and 62% of affected individuals took part in the intervention. On average, affected individuals had faced acute attacks 3.38 (SD=3.69) times in the three months prior to the survey.
The “next steps for podoconiosis patients in Amhara region” intervention: process, fidelity and acceptability
We first looked at the implementation process, fidelity and acceptability of the selected intervention. The implementors were of the opinion that they had executed all of the intervention activities in line with the initial plans. A member of implementing staff noted “We found that most of the health centers were doing well … Cascaded trainings have been implemented in most of the health centers. In many of the health centers some patients show up regularly for follow up visits. High attendance means there is good linkage with the health extension workers” (KII, staff of intervention implementing organization). However, while the intervention was designed to cascade training activities through existing health structures, in real life, the intervention was mainly concentrated at the health center settings. Trained health professionals did not train the HEWs as oriented. A key informant said, “We provided training to the health staff of each healthcare facility in a nearby district town. However, after the training, the trained staff were not actively engaged in training HEWs and documenting the intervention activities” (KII, NTD officer, Dera district). The study further noted that HEWs showed little interest in engaging in NTD interventions that do not provide incentives. Key informants reported that some health professionals preferred working on health conditions that bring personal benefits. An NTD officer noted, “Some health workers lacked motivation to engage themselves in podoconiosis treatment as we do not pay incentives during health education campaigns” (KII, Dera District). Failure to fulfil these responsibilities has disrupted the fidelity of intervention activities and by extension, attempts to prevent and treat podoconiosis.
About 18% of the unaffected community members had engaged in health education programs. Of the 42 affected individuals that took part in the survey, 61.9% of them had taken part in the intervention. However, only 45.2% of affected individuals had completed the intervention activities.
We assessed affected individuals’ attitudes towards the project activities. Table 2 shows that nearly all (96.2%) reported they fully comprehended the message, and the intervention had improved their foot condition and self-confidence. Additionally, about 88% reported continuing to implement intervention lessons after completing the three months training.
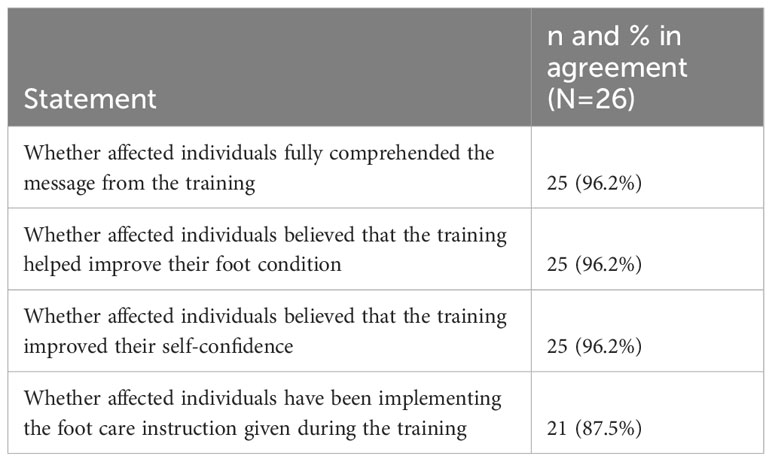
Table 2 Attitude of affected individuals about the message and perceived outcomes of the intervention.
Contextual factors that embed the intervention
Geographical context
Geographical contexts such as soil type, rurality and remoteness affected the intervention. The two districts’ surfaces are mainly covered by red clay soil, putting residents at higher risk of developing podoconiosis. In addition, residents in the two communities live in remote areas. Long distances between home and healthcare stations discouraged affected individuals from taking part in the intervention. The survey showed that participants travel on average, spent about 76 minutes (SD=42.70) for a round trip to and from the nearest health station on foot. As the intervention was conducted at healthcare facilities, the outreach target of the intervention was hindered by lack of accessibility for geographically isolated residents.
Epidemiological and clinical contexts
Podoconiosis is among the most prevalent health conditions in the study areas. However, unaffected community members did not consider podoconiosis a priority health problem as FGD participants ranked TB, trachoma and malaria as the most prevalent health conditions needing attention. The physical and socioeconomic burdens of podoconiosis affected participation in the intervention activities. Our qualitative interviews indicated that affected individuals faced frequent acute attacks manifested through high fever and chills. As shown in Table 1, the average number of acute adenolymphangitis attacks (ALA) in the three months prior to the survey was 3.38 (SD=3.69). Podoconiosis also affected the mobility of patients. One of the affected individuals said, “I was frequently suffering from an acute attack. When acute attack arises, I feel cold inside and pain around the groin. I also sleep the whole day or a couple of days until the acute attack subsides” (IDI, affected male, age 64).
The socio-cultural context
Involvement in and acceptability of the intervention was affected by the socio-cultural context, as manifested by misconceptions, gender inequality and lack of shoe wearing norms.
Several individuals associated the causes of podoconiosis with external factors such as stepping on goat blood or urine. These participants believed that goats eat poisonous plants and stepping on goats’ blood eventually results in developing podoconiosis. Some individuals in both communities also believed that podoconiosis was a hereditable condition. A participant in FGD noted, “The other causes of podoconiosis is heredity. In some families more than two people get sick without experiencing any accident. This shows that the children get the disease from their parents” (FGD, men, Dera district). Such beliefs led to wrong perceptions about the preventability of podoconiosis. One participant highlighted, “If the person is exposed to accidents due to sharp objects, the swelling subsides very soon. The swelling caused due to heredity cannot be cured and it is not reversible. This is what we observed among podoconiosis patients” (FGD, men, Dera district).
Further noted by the study was the community’s belief about the transmissibility of podoconiosis through personal contact. One example includes, “If many people within the same family are affected, it could be due to sharing a washing tool or when they sleep on the same bed it might be transmitted through physical contact with patients” (FGD, women, Yilmana Densa district)”. Our qualitative data revealed that skepticism about the treatability of podoconiosis using modern medicine is rife. Beliefs about traditional and spiritual treatment were present in the communities and influenced health seeking behaviour and adherence to modern treatment procedures. One participant said, “It is not worth spending money for medical treatment on such a disease which cannot be cured without the interference of God. I should wait for God’s response to my prayer” (IDI, affected female, 38).
Figure 1 shows that respondents simultaneously held accurate and inaccurate understanding. The overwhelming majority hold accurate beliefs that foot hygiene (94.3%) and regular shoe wearing (94%) prevent podoconiosis. However, major misconceptions with regards to the cause and transmission of podoconiosis were simultaneously reported. About nine in ten believed that wearing the shoes of a person with podoconiosis transmits podoconiosis, while 87% reported that sharing water and soap with patients transmits podoconiosis. About 72.4% believed that the disease was caused by insects in the soil, stepping on goat blood or snake poison and punishment or curse from God.
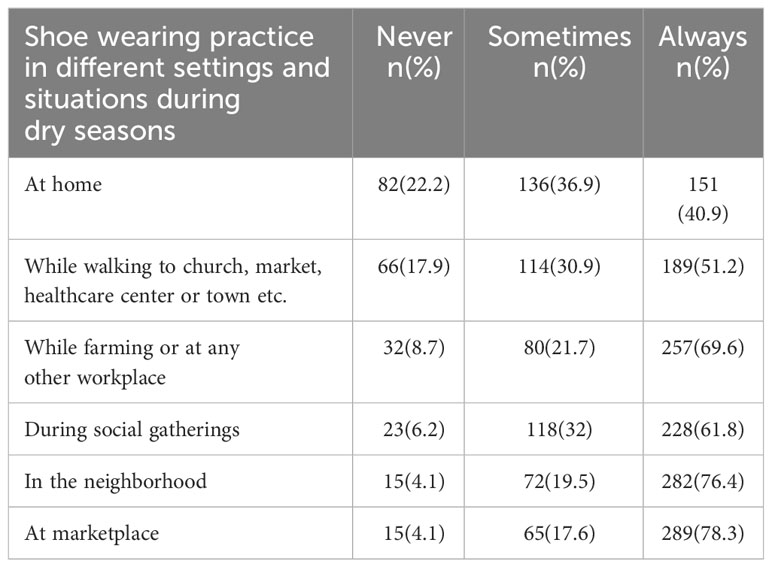
Table 3 shows patterns of footwear use varied across settings and situations, with the following proportion of respondents reporting that they always wore shoes at home (40.9%), while walking to church, market, healthcare center (51.2%), while farming or at any other workplace (69.6%), during social gatherings (61.8%), in the neighborhood (76.4%) or at the market (78.3%).
The qualitative data also suggested that shoe wearing practices in these communities are intermittent. Farming barefoot continues as a longstanding norm among adults and the elderly due to its perceived comfortability. However, the respondents believed that there had been a significant change in shoe wearing norms in the communities A key respondent said, “Nowadays most people in the community wears shoes. In my view, about 80-85% of the people in our community wear shoes. In fact, this is a recent phenomenon due to the advances in technology, education and people are now getting more profit from their production and have better savings to fulfil their needs…” (KII, local official Yilmana Densa District). Another key informant said, “There is improvement with regards to the shoes wearing practices among young people. Except during the rainy season where almost all people opt to walk bare feet when it is muddy, assuming not comfortable to work” (KII, HEW, Dera District). An affected person also said, “When I was a kid, we used to walk barefoot everywhere. Wearing shoe is a recent practice. I started wearing shoes after being affected. Now I have shoes, but I often wear open plastic shoes. Closed shoes are not comfortable for work (IDI, Affected female age 34 to 36).
We also found gender to be one of the socio-cultural factors that affected the intervention. Women in the two communities experienced hardship throughout their lives. FGD discussants revealed that women’s work includes carrying heavy loads over long distances, selling and buying items from the market, cooking, grinding grain at mills, cleaning and taking care of family members and cattle. The women in the two communities are responsible for fetching water and manure preparation. In the two communities, men usually own cattle and horses, and women own sheep and chickens.
Due to their status and household roles, women find it difficult to take part in health interventions conducted at health care facilities. Gender appears to be an important influencer of health as husbands mostly make treatment-seeking related decisions. A woman participant said, “…husbands remain [to be] the leaders of the family … So females go to healthcare stations and buy medicine when husbands give permission” (IDI, affected female, age 64).
As shown in Table 4, although the associations are of borderline statistical significance, men’s involvement in the intervention was higher than females (χ2(1) (3.23), p =0.07). Additionally, more men than women completed the intervention activities. However, the difference was not statistically significant (χ2(1) (0.16) p =0.68).
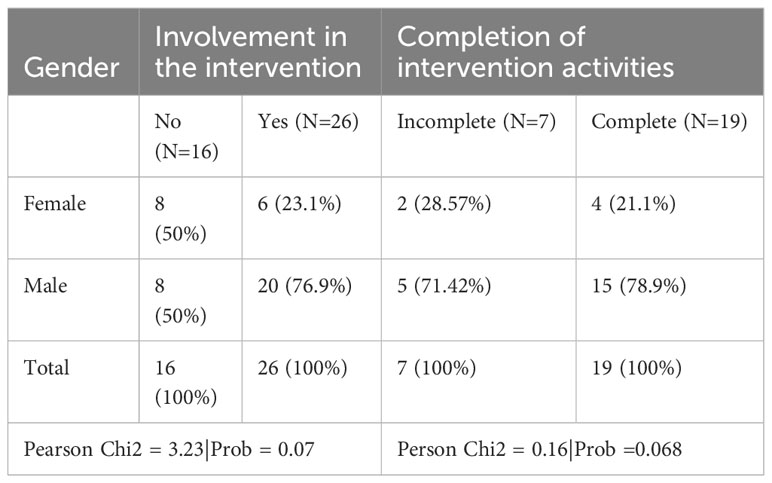
Table 4 Contingency Table showing the association between involvement in the intervention and gender.
Socioeconomic context
Considering health, education and living standards, UNDP (39) estimated that in 2020, about 69% of the population in Ethiopia was multidimensionally poor while 18.4% were vulnerable to multidimensional poverty (39). Poverty is much more prevalent in rural areas than urban areas in Ethiopia (40). High levels of poverty, civil war and dire economic situations mean that Ethiopia has had to rely heavily on foreign aid. In 2020, the total amount of development aid received by Ethiopia was $5.3 billion making the country among the top five recipients of foreign aid around the world (41).
The Ethiopian health care system is organized into three tiers: primary, secondary and tertiary levels (16). The primary level of care is comprised of primary hospitals (covering 60,000-100,000 people), health centers (covering 15,000-25,000) and satellite health posts (covering 3,000-5,000). In 2020, there were 3,777 functional health centers and 17,699 health posts in Ethiopia (42). The secondary level of care constitutes general hospitals (covering a population of 1-1.5 million), while the tertiary level of care comprises Specialized Hospitals (covering a population of 3.5-5 million) (42). Ethiopia suffers from an acute shortage of health facilities, and rural areas, in which about 80% of the population live, have been particularly under-served (43). In the Amhara region, where the evaluated intervention was implemented, health facilities remain scarce, at 2.54 health facilities (both governmental and private) per 10,000 population (43).
Public resources such as running water, electric power and paved roads were rarely available in the communities we studied. A local administrator said, “Only few individuals and small-scale millers have access to electricity” (KII, Local officials, Yilmana Densa District). Most of the residents rely on communal hand-dug wells for drinking water supply. The residents rely on small three-wheeler cars widely known as Bajaj for their transportation to nearby towns. Otherwise, they travel to markets, healthcare centers, farming lands, and churches on foot.
Only two healthcare centers serving up to 40,000 residents of the surrounding kebeles are found in the study areas. Each kebele has one health post accountable to the health center. HEWs operate at the health post level. The health centers consist of one physician, five health officers, five midwifes, two laboratory technicians, eight clinical nurses, three pharmacists, and three administrative staff. Most of the residents (nearly 90%) are enrolled in a community-based health insurance scheme and claimed that the scheme has improved access to treatments. A participant said. “I like the community-based health insurance introduced recently for farmers. It gave me the opportunity to receive medical treatment anytime we get sick” (IDI, affected female, age 38). Although most of the residents believed that the scheme improved utilization of healthcare services regardless of people’s economic status, local health professionals complained about the burden at healthcare facilities following the implementation of the program. A key informant remarked, “Now the farmers are coming to healthcare facilities even when they prick the tip of their fingers. They think they are entitled to get medical treatment even for minor injuries. This has created more burden on us” (KII, health professional, Yilmana Densa District).
Most affected individuals were poor and relied on subsistence agriculture. A key informant said, “As most of the podoconiosis patients are the poorest of the poor, they were unable to afford medical expenses” (KII, staff of an NGO). An affected farmer said, “As I am poor, I am not able to buy painkillers whenever I have acute attack” (IDI, male, age 50). Another affected person noted, “It is only my pain that held me back from improving my economic status. Had it not been for my pain, I would have become a rich farmer. I can’t work as I wish due to my leg. I found it difficult to buy some stuff including medicine” (a 39-year-old affected male). Some engage in farming activities barefoot, which increases their exposure to podoconiosis. In addition, as shown in Table 2, about three in four individuals in the communities had no formal education, limiting their future occupational opportunities and potential to make better earnings. Podoconiosis also limited affected individuals’ educational opportunities. Affected individuals quit schooling due to fear of stigma. One example includes: “I was enrolled to grade one, but soon quit school because of my sickness. I couldn’t bear the reaction of school children as everybody was pointing their fingers at me with insults” (IDI, male affected, 18 years old).
Legal context
Ethiopia approved the International Covenant on Economic, Social and Cultural Rights in 1993, a treaty that has been ratified by more than 170 countries. Article 11 of the treaty reads “The States Parties to the present Covenant recognize the right of everyone to an adequate standard of living for himself and his family, including adequate food, clothing and housing, and to the continuous improvement of living conditions (44). In addition, Ethiopia accepts that all people have certain inalienable rights including a right to a standard of living adequate for the health and well-being as the UN General Assembly determined over 65 years ago, (45).
Healthcare professionals at the two healthcare facilities reported that they no longer provided supplies such as shoes or washing bowls for patients. Providing treatment supplies at healthcare facilities might have helped to integrate lymphedema management services into local healthcare structure. Expecting the regional health bureau would fulfil its responsibility and provide treatment supplies to patients, the intervention implementors planned to introduce the intervention activities to showcase and assist efforts of mainstreaming podoconiosis services. A key informant reported, “We requested the health centers to allocate budget to provide supplies for treatment. This could have helped to provide consistent services. But this did not happen” (KII, staff of IOCC). As the government fails to provide financial and related resources, podoconiosis continues to impact the lives of affected individuals.
Political context
Following studies on podoconiosis that showed the socioeconomic burden of the disease, the World Health Organization classified podoconiosis as a Neglected Tropical Condition in 2011 (46). A similar development convinced the Ethiopian Federal Ministry of Health to consider podoconiosis a priority issue (17). The government included podoconiosis in the National Master Plan for Neglected Tropical Diseases (NTDs) (16). These guidelines provide evidence-based practical guidance on patient management and disability prevention; and assisted the implementation of the intervention. The regional government also demonstrated its commitment in setting up NTD structures at zonal and district levels. A key informant said, “The NTD section has been established in the health sector structure at regional, zonal and district level to account for this neglected health problem.” (KII, NTD officer, Yilmana Densa district). Amhara region collaborates with intervention implementors. A staff of intervention implementors noted, “The Amhara Regional Health Bureau welcomed us when we inquired to recruit seconded staff and operate through integration approach along with the NTD team in the regional health office. This approach created advantages in sharing resources and experience, minimizing duplication of efforts and sharing knowledge among the NTD team” (KII, staff of intervention implementing organization).
We also noted that the attempt to have a dedicated budget line for podoconiosis from the government side has not been sufficient. A key informant said, “The Ministry has not allocated any budget for podoconiosis in the years 2022 and 2023” (KII, Podoconiosis focal person at Ministry of Health). Although the Ethiopian government has shown its commitment to podoconiosis by including it in national strategic plans, the government has shown little will to allocate budget to expand treatment services.
Lived experience
The lived experience of affected individuals influenced their willingness to become involved in intervention activities. Having experienced the chronic nature of podoconiosis as well as ineffective attempts to treat the disease, some affected individuals had a firm belief that nothing could be done to improve their condition and were not willing to adhere to treatment practices. Affected individuals who went to the healthcare facility did not get the treatment they were hoping for, as exemplified by the following statement from an affected person. “The health staff at the hospital informed me that they had no idea about the condition; whether it can be cured or not” (IDI, affected male, age 50).
Some affected individuals perceived their body to be unable to function. One account reads “Compared to healthy people, we are useless. My leg doesn’t take me forward. It holds me back. When we travel as a group to markets or other places, I can’t keep pace with the rest. When people reach to their destination, I could only reach halfway” (IDI, affected male, age 39).
Being unhappy with their physical condition and fearing public reactions, some patients preferred to stay at home. An affected person stated, “I feel ashamed of being with people in public gatherings fearing that I become the center of attention due to my abnormal feet. Some friends, priests and kind people invite me to sit next to them in church, but I do feel that my presence next to them may give discomfort to others. So, I don’t usually go out” (IDI, affected female, age 34 to 36). Another added “I sometimes feel that this condition might create discomfort among people. I would like to stay at home especially when the swelling creates wounds and bad odour” (IDI, affected female, age 65).
Discussion
Our study identified six of the seven contextual domains identified by Pfadenhauer et al. (21) as affecting the implementation of the selected intervention, and an additional lived experience domain. Some of these domains, such as the political and socio-economic domains, interacted across macro-, meso- and micro contextual levels and either facilitated or constrained involvement in the selected intervention while the ethical context had little impact of the evaluated intervention.
The effect of geographical factors
Soil minerals in red clay soil are among the causes of podoconiosis (47). Red clay soil covers most of the surface areas of the studied communities and increased individuals’ exposure to podoconiosis. However, individuals can take measures to reduce their contact with the soil. Most community members were not aware of the pathological effect of the red clay soil. Conducting health education campaigns to improve shoe wearing practices and reduce rural residents’ contact with the red clay soil may be helpful as long as health intervention implementors acknowledge accurate understandings may not alone bring desirable behavioral changes. While utilizing local health professionals was associated with better understanding of podoconiosis in rural Ethiopia (48), involving other local actors such as local administrators, schools, religious settings and agricultural extension workers could yield better outcomes. Agricultural extension workers, having a working relationship with farmers, are perceived as highly credible by rural residents in disseminating information about the impact of the soil on podoconiosis. A study by Elias et al. (49) found that agricultural extension workers play a significant role in training farmers to adopt new methods.
Confirming prior studies on the impact of distance on utilization of healthcare services in rural areas (50–53), our study found long distances between home and healthcare stations to be a structural barrier to participation in health interventions. Shifting the lymphoedema management and health education responsibility to HEWs at health posts may increase the outreach of intervention programs and improve health outcomes.
The effect of epidemiological factors
The prevalence and burden of podoconiosis also have implications for health interventions. The high prevalence of the disease at national and regional levels encouraged collaboration between government offices and intervention implementors. It also encouraged local health professionals. On the other hand, unaffected members of the communities did not consider podoconiosis to be an important condition. Members of the community may show reluctance to participate in health interventions if they do not consider podoconiosis to be a serious concern. The debilitating physical condition and frequent occurrence of acute attacks increased demand for health interventions. However, due to their physical pain and social burden, affected individuals could not fully participate in the intervention activities. Inclusion of home-based intervention for individuals with mobility problems or severe illness could increase the accessibility of health interventions.
The effect of socio-cultural factors
Our study showed that endorsement of inaccurate beliefs about podoconiosis is pervasive in the two communities. This finding is broadly in line with earlier studies (13, 48, 54, 55) that reported high prevalence of misconceptions in rural Ethiopia. These studies indicated the implications of wrong beliefs on adoption of preventive behaviour and stigmatizing attitudes. To date, the impact of widely regarded beliefs on acceptability of accurate understanding about NTDs has not been sufficiently discussed. Our study implies that health interventions aiming to help people reach accurate and nuanced understanding of conditions could be challenged by existing misunderstanding as rural residents might resist accurate information. Existing beliefs, whether accurate or otherwise, cannot be simply disregarded as they have been created and maintained through lived experience. As noted by Curtis (56), community beliefs are stable over time and cannot be easily discarded. Even after receiving health information from intervention implementors, community members may hold accurate and inaccurate assumptions simultaneously. Consequently, various and even conflicting explanations about conditions may be pervasive and reduce the impact of health interventions (57, 58). Going forward, the challenge for health interventions will be not only expanding accurate understanding but also dispelling established misconceptions.
A key to podoconiosis prevention is regular footwear practice (7). Individuals need to wear footwear in a range of conditions and settings to avoid prolonged contact with red clay soil. Several individuals, particularly the elderly, still walk barefoot in the two communities. This study noted that there is no consistent use of footwear across settings and situations. This was a result of multiple factors including lack of awareness about the causes of podoconiosis, shoe wearing norms, unsuitability of footwear for agricultural activities and inability to buy shoes, as found by a prior study (59). Existing practices could affect the acceptability of health interventions that aim to improve shoe wearing practices in rural areas. Thus, interventions should come up with a multistage intervention to change people’s understanding about the causes of podoconiosis and practice of shoe wearing through health education and economic empowerment activities. In addition, they should intervene at community level to change existing attitudes and norms about footwear practices. Collaborating with shoe producers to increase the availability of comfortable, practical, and affordable shoes and boots in podoconiosis endemic areas could also encourage shoe wearing practices.
We further found that gender inequalities can affect the outreach of health interventions. Other studies on NTDs have indicated that gender-related factors affect healthcare access (53, 60–63). A study by Negussie et al. (64) also underscored the effect of gender on uptake and effect of lymphedema management services. Our findings indicate that health interventions should be aware of gender-specific disadvantages and design a gender-sensitive strategy to reach affected patients who were previously excluded from health care services. If intervention implementors fail to consider gender differences, they contribute to perpetuating gender inequalities by widening heath inequalities between affected men and women.
The effect of socioeconomic factors
Much has been written about the effect of socioeconomic status on individuals’ health (65, 66). However, despite recent calls for the inclusion of socioeconomic factors within health intervention evaluations (21, 28), little has been said about how health interventions operate within a given socioeconomic context. Our study indicates that socioeconomic factors interacted at macro, meso and micro levels to affect health interventions.
At macro level, the poor socio-economic status of the country limited the government’s ability to provide health services for affected individuals. High levels of poverty, civil war and the dire economic situation mean that Ethiopia has had to rely heavily on foreign aid. Foreign aid has been the major source of government revenue and is reported to have positive role in the country’s infrastructure development and economic growth (67, 68). On the other hand, experts argue that foreign aid may erode domestic authority (69–71) and aid-receiving countries may easily be pressured only to perform donor-driven programs (72, 73). Scholars assert that western aid policies towards Africa have been dominated by liberal economic and political conditionalities, respect for human rights and governance; and ‘partnership’ policies involving intensive and extensive redesigning of policy formation (69, 71). This may force the government to formulate policies and strategies in line with the donor’s policy at the expense of local realties and needs. As there has been little interest to intervene on podoconiosis by global actors, Ethiopian governments may have limited capacity to promulgate strategies and implement interventions to control and prevent podoconiosis.
Provision of health services via government healthcare facilities was also challenging. The implementation and outcome of the intervention should then be seen in the light of available health services and staffing patterns in a given context if interventions are delivered in government healthcare centers. Infrastructure including transportation services and existing healthcare structures like CBHI can influence utilization, accessibility, and outreach. Being aware of existing socioeconomic conditions and designing a strategy that considers existing resources will be important to boost community empowerment and the health status of affected individuals. In addition, diseases like podoconiosis require long-term self-care and an ability to purchase treatment materials on a regular basis. The poor economic status of affected individuals challenges this practice. Lack of education could also limit individuals’ access to health information and their ability to understand intervention messages. Lack of schooling was associated with lower knowledge about podoconiosis in earlier studies among rural residents in Ethiopia (13, 47, 48). The study also found that rural residents had limited access to water which is consistent with a prior study in Northern Ethiopia that found lack of water contributed to poor foot hygiene practices (54). This could further affect individuals’ acceptability and adoption of the intervention’ guideline about personal hygiene. In the absence of adequate supplies of health resources, interventions against podoconiosis will be less effective in improving the lives of affected individuals.
The effect of legal factors
Little research has been conducted on the impact of the legal context on interventions against NTDs. This study showed that the Ethiopian government’s failure to provide health services to affected individuals has hampered implementation of the intervention. For a long period, advocates have considered human rights-based approach to achieve better health outcomes (74). Protecting the health of citizens is primarily a responsibility of governments. Making the Ethiopian government accountable for the rights of citizens to health, adequate clothing, and healthy working conditions, could help expand preventive health services (75). Thus, implementors should advance the idea of employing human rights-based approaches to address the needs of affected and at-risk populations, synchronizing with social justice interventions and the legal duties of governments. However, in settings like Ethiopia where financial resources are limited and the provision of healthcare services are highly influenced by political and economic factors, this should not constitute a shift away from other interventions, but rather be one of many approaches to tackle the problem.
The effect of political factors
The political context operated at national and regional levels to positively influence the implementation of the intervention. The Ethiopian government’s commitment to control podoconiosis resulted in the development of national programs and treatment guidelines that facilitated the implementation of activities using government resources and structures at lower levels. Regional government offices also collaborated with the intervention implementors during the implementation of the intervention. On the other hand, the government’s failure to allocate budget to podoconiosis negatively affected the integration of the intervention activities into local healthcare structures. Such effects of the political context should be recognized by health intervention implementors as this could help them conduct more realistic interventions anticipating possible opportunities, constraints and impacts (76, 77).
The effect of lived experience
Although it was not included in the CICI framework (21), the lived experience of affected individuals has the potential to influence participation in intervention activities. Lived experience incorporates the actual experience itself along with the meanings attributed to the experience by affected individuals (78). Despite acknowledging the knowledge, skills and attributes of affected individuals as agents that can influence the implementation of a given intervention (21), exponents of the CICI framework tended to give little emphasis to the lived experiences that might have shaped knowledge and attitudes. Experiencing the chronic nature of disease, some affected individuals had a strong belief that their condition could not be improved at all. Affected individuals’ lives and their meaning have been severely affected by the condition. Some had very low self-esteem and experienced self-stigma.
Interventions have the potential to improve the self-concept and living conditions of affected individuals if they consider their lived experience. However, few studies exist to explain how these experiences might be considered as evidence along with impact evaluation and economic analysis of interventions (79). An earlier study argued that affected individuals’ experience is essential to understand the nature of a condition as well the needs of affected individuals. Understanding this would be important to learn about the lives of affected individuals, their values and the deficiencies in their lives (79). This will help to identify important skills for the adoption of preventive behaviors to deal with the challenges of everyday life (80). Listening to the lived experience of affected individuals gives intervention implementors an opportunity to craft contextualized intervention to meet those deficiencies (79).
The study has several strengths such as a very high participation rate. We evaluated a health intervention using the CICI evaluation framework with a clear conceptualization of different contextual domains. The comprehensive analysis of the contextual domains across different levels (for instance, political and socio-economic domains at macro, meso and micro levels) resulted in identifying factors that facilitated and constrained health intervention in rural settings. We employed reliable measures to assess individuals’ knowledge about podoconiosis and shoe wearing practices across settings and situations. The qualitative data also provided rich information about affected individuals’ experiences and contextual factors. Employing both qualitative and quantitative methods, we were able to enhance the accuracy and validity of the findings. On the other hand, the study had some limitations. The study did not include data on the outcome of the intervention as we focused on the implementation process. In addition, staff of NGOs and health professionals may have provided socially desirable answers about the implementation process of the intervention.
Conclusion
Viewing public health interventions as sets of events within a complex context helps us understand the effects of the context on these interventions. Guided by the CICI framework, our study showed in what contexts podoconiosis interventions may operate. On top of the CICI’s domains, our study showed that additional domains such as lived experience could affect health intervention, indicating evaluation theories should be modified in line with local realties.
The study showed that interventions cannot be wholly understood by simply looking at intervention delivery points and the changes brought about by interventions. Interventions are context-specific and may not always effectively deal with challenges posed by socio-cultural, economic, political, ethical, legal, epidemiological, and geographic contexts. Identifying the deterrent effects of these factors will help implementors to design programs that can withstand these challenges. The programs in the long run could help alter the contextual factors. The study also showed that contextual factors do not only present challenges but opportunities that can facilitate the implementation of intervention programs. Utilizing these facilitators saves resources and increases the efficiency and effectiveness of interventions. Taken together, this information will underpin the development of complex health interventions that can successfully reduce the impact of podoconiosis and similar NTDs in endemic areas.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study obtained ethical clearance from the Research Governance and Ethics Committee (RGEC) of Brighton and Sussex Medical School (BSMS) (Reference: ER/BSMS9E3G/8) and the Ethiopian Society of Sociologists, Social Workers and Anthropologists (ESSSWA) (Reference: ESSSWA 019/21). The Amhara Public Health Institute, regional and zonal health bureaus granted permission to conduct the study in the selected areas. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. GT: Conceptualization, Funding acquisition, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. PN: Conceptualization, Funding acquisition, Resources, Supervision, Visualization, Writing – review & editing. GD: Conceptualization, Funding acquisition, Investigation, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. SZ: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study is part of a large project known as Social Sciences for Severely Stigmatizing Skin Conditions (5S-Foundation) that aims to end the neglect of three NTDs, namely, podoconiosis, scabies and mycetoma in Ethiopia, Rwanda and Sudan using a social science perspective. This research was funded by the NIHR (200140) using UK international development funding from the UK Government to support global health research.
Acknowledgments
We would like to thank study participants, local officials in Amhara region of Ethiopia. We would also like to acknowledge the support and cooperation of intervention funders (IZUMI Foundation) and the intervention implementers (IOCC and NaPAN).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the UK government.
References
1. World Health Organization. Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021–2030. Geneva, Switzerland: World Health Organization (2020).
2. Hastings J. Rumours, riots and the rejection of mass drug administration for the treatment of schistosomiasis in morogoro, tanzania. J biosocial Sci (2016) 48 Suppl 1:S16–39. doi: 10.1017/S0021932016000018
3. Parker M, Allen T, Hastings J. Resisting control of neglected tropical diseases: dilemmas in the mass treatment of schistosomiasis and soil-transmitted helminths in north-west Uganda. J Biol Sci. (2008) 40(2):161–81. doi: 10.1017/S0021932007002301
4. Celone M, Person B, Ali SM, Lyimo JH, Mohammed UA, Khamis AN, et al. Increasing the reach: Involving local Muslim religious teachers in a behavioral intervention to eliminate urogenital schistosomiasis in Zanzibar. Acta Tropica. (2016) 163:142–8. doi: 10.1016/j.actatropica.2016.08.004
5. Burnim M, Ivy JA, King CH. Systematic review of community-based, school-based, and combined delivery modes for reaching school-aged children in mass drug administration programs for schistosomiasis. PloS Negl Trop Dis. (2017) 11:e0006043. doi: 10.1371/journal.pntd.0006043
6. Silumbwe A, Halwindi H, Zulu JM. How community engagement strategies shape participation in mass drug administration programmes for lymphatic filariasis: The case of Luangwa District, Zambia. PloS Negl Trop Dis. (2019) 13:e0007861. doi: 10.1371/journal.pntd.0007861
7. Price EW, Plant D. The significance of particle size of soils as a risk factor in the etiology of podoconiosis. Trans Royals Soc Trop Med Hyg. (1990) 8:885–6. doi: 10.1016/0035-9203(90)90115-U.
8. Deribe K, Brooker SJ, Pullan RL, Sime H, Gebretsadik A, Assefa A, et al. Epidemiology and individual, household and geographical risk factors of podoconiosis in Ethiopia: results from the first nationwide mapping. Am J Trop Med Hyg. (2015) 92:148–58. doi: 10.4269/ajtmh.14-0446.
9. Phillips C, Samuel A, Tiruneh G, Deribe K, Davey G. The impact of acute adenolymphangitis in podoconiosis on caregivers: A case study in Wayu Tuka woreda, Oromia, Western Ethiopia. ‘If she was healthy, I would be free.’. PloS Negl Trop Dis. (2019) 13:e0007487. doi: 10.1371/journal.pntd.0007487
10. Tekola AF, Mariam DH, Davey G. Economic costs of endemic non-filarial elephantiasis in Wolaita Zone, Ethiopia. Trop Med Int Health. (2006) 11:1136–44. doi: 10.1111/j.1365-3156.2006.01658.x.
11. Deribe K, Negussu N, Newport MJ, Davey G, Turner HC. The health and economic burden of podoconiosis in Ethiopia. Trans R Soc Trop Med Hyg. (2020) 114:284–92. doi: 10.1093/trstmh/traa003
12. Ali O, Deribe K, Semrau M, Mengiste A, Kinfe M, Tesfaye A, et al. A cross-sectional study to evaluate depression and quality of life among patients with lymphoedema due to podoconiosis, lymphatic filariasis and leprosy. Trans R Soc Trop Med Hyg. (2020) 114:983–94. doi: 10.1093/trstmh/traa130
13. Ayode D, McBride CM, de Heer H, Watanabe E, Gebreyesus T, Tadele G, et al. The association of beliefs about heredity with preventive and interpersonal behaviors in communities affected by podoconiosis in rural Ethiopia. Am J Trop Med Hyg. (2012) 87:623–30. doi: 10.4269/ajtmh.2012.12-0204
14. Molla YB, Tomczyk S, Amberbir T, Tamiru A, Davey G. Patients’ perceptions of podoconiosis causes, prevention and consequences in East and West Gojam, Northern Ethiopia. BMC Public Health. (2012a) 12:828. doi: 10.1186/1471-2458-12-828
15. Tora A, Franklin H, Deribe K, Reda AA, Davey G. Extent of podoconiosis-related stigma in Wolaita Zone, Southern Ethiopia: a cross-sectional study. Springer Plus. (2014) 3:647. doi: 10.1186/2193-1801-3-647
16. FDRE Ministry of Health. Second edition of National Neglected Tropical Disease (NTDs). Addis Ababa: Ethiopian, Ministry of Health (2016).
17. Deribe K, Kebede B, Mengistu B, Negussie H, Sileshi M, Tamiru M, et al. Podoconiosis in Ethiopia: from neglect to priority public health problem. Ethiopian Med J. (2017) 55:65–74.
18. Nucleus Health and Social Affairs Consultancy Firm. End-term evaluation report for “Preventing podoconiosis project (PPP): expanding podoconiosis interventions in Ethiopia” project. In: Evaluation report. Addis Ababa, Ethiopia: National Podoconiosis Action Network (NaPAN) (2017).
19. Hounsome N, Kinfe M, Semrau M, Ali O, Tesfaye A, Mengiste A, et al. Economic assessment of a community-based care package for people with lower limb disorder caused by lymphatic filariasis, podoconiosis and leprosy in Ethiopia. Trans R Soc Trop Med Hyg. (2020) 114:1021–34. doi: 10.1093/trstmh/traa111.
20. Dellar R, Ali O, Kinfe M, Mengiste A, Davey G, Bremner S, et al. Effect of a community-based holistic care package on physical and psychosocial outcomes in people with lower limb disorder caused by lymphatic filariasis, podoconiosis, and leprosy in Ethiopia: results from the EnDPoINT pilot cohort study. Am J Trop Med Hyg. (2022) 107:624–31. doi: 10.4269/ajtmh.21-1180
21. Pfadenhauer LM, Gerhardus A, Mozygemba K, Lysdahl KB, Booth A, Hofmann B, et al. Making sense of complexity in context and implementation: the Context and Implementation of Complex Interventions (CICI) framework. Implement Sci: IS. (2017) 12:21. doi: 10.1186/s13012-017-0552-5
22. Moore GF, Evans RE, Hawkins J, Littlecott H, Melendez-Torres GJ, Bonell C, et al. From complex social interventions to interventions in complex social systems: Future directions and unresolved questions for intervention development and evaluation. Eval (Lond). (2019) 25:23–45. doi: 10.1177/1356389018803219
23. Ziemann A, Brown L, Sadler E, Ocloo J, Boaz A, Sandall J. Influence of external contextual factors on the implementation of health and social care interventions into practice within or across countries-a protocol for a ‘best fit’ framework synthesis. System Rev. (2019) 8:258. doi: 10.1186/s13643-019-1180-8
24. Blacklock C, Gonçalves Bradley DC, Mickan S, Willcox M, Roberts N, Bergström A, et al. Impact of Contextual Factors on the Effect of Interventions to Improve Health Worker Performance in Sub-Saharan Africa: Review of Randomised Clinical Trials. PloS One (2016) 11(1):e0145206. doi: 10.1371/journal.pone.0145206
25. Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health (2002) 56(2):119–27. doi: 10.1136/jech.56.2.119
26. Mozygemba K, Hofmann B, Lysdahl KB, Pfadenhauer L, van der Wilt GJ, Gerhardus A. Guidance to assess socio-cultural aspects. In: Lysdahl KB, Mozygemba K, Burns J, Chilcott JB, Brönneke JB, Hofmann B, editors. (European Union) Guidance for assessing effectiveness, economic aspects, ethical aspects, socio-cultural aspects and legal aspects in complex technologies (2015).
28. Victora CG, Schellenberg JA, Huicho L, Amaral J, El Arifeen S, Pariyo G, et al. Context matters: interpreting impact findings in child survival evaluations. Health Policy Plann. (2005) 20 Suppl 1:i18–31. doi: 10.1093/heapol/czi050
29. European Network for Health Technology Assessment (EUnetHTA). HTA Core Model for screening technologies. Work Package 4 Core HTA EUnetHTA Joint Action 2010 - 2012 (EUnetHTA). (2011).
30. Guidance for assessing effectiveness, economic aspects, ethical aspects, socio-cultural aspects and legal aspects. 2016 (2016). Available online at: http://www.integrate-hta.eu/downloads/ (Accessed January 20, 2023).
31. Nash R, Hudson A, Luttrell C. Mapping political context: A toolkit for Civil Society Organisations Overseas Development Institute—Research and Policy in Development Programme. Retrieved August 1, 2023 from Mapping Political Context: A Toolkit for Civil Society Organisations - ODI Toolkits - Toolkits (London: Overseas Development Institute (odi)). (2006).
32. CSA. Population Projections for Ethiopia 2007-2037. Addis Ababa, Ethiopia: Central Statistcis Authority (2013).
33. Mekonnen G. Characterization of agricultural soils in CASCAPE intervention woredas of Amhara region. Ethiopia: CASCAPE report. Bahir Dar University (2015).
34. Mesfin S, Adem AA, Mullu A, Melesse AM. Historical trend analysis of rainfall in amhara national regional state. In: Melesse AM, Abtew W, Moges SA, editors. Nile and Grand Ethiopian Renaissance Dam. Springer Geography. Springer, Cham (2021). doi: 10.1007/978-3-030-76437-1_25
35. Deribe K, Cano J, Newport MJ, Golding N, Pullan RL, Sime H, et al. Mapping and modelling the geographical distribution and environmental limits of podoconiosis in Ethiopia. PloS Negl Trop Dis. (2015) 9:e0003946. doi: 10.1371/journal.pntd.0003946
36. Creswell J, Clark P. Designing and Conducting Mixed Methods Research. Thousand Oaks CA: Sage (2007).
37. MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. In: Krippendorff K, Bock MA, editors. The content analysis reader. Sage, Thousand Oaks, CA (2009). p. 211–19.
39. UNDP. Multidimensional Poverty Index 2022. Unpacking deprivation bundles to reduce multidimensional poverty. Briefing note for countries note 2022 Multidimensional poverty index. Ethiopia: ETH.pdf (undp.org (2022).
40. Forum for Social Studies. Environment, poverty and conflict. Addis Ababa Ethiopia: Forum for Social Studies (FSS) (2004).
41. World Bank. International Debt Statistics 2022. Retrieved February 2, 2023 from International Debt Statistics. The World Bank (2022).
42. FDRE Ministry of Health. Health and Health-Related Indictors. Addis Ababa: Health and health related indicators _2013 EFY.pdf (moh.gov.et (2021).
43. FDRE Ministry of Health. Essential Health Package Services for Ethiopia. Addis Ababa: Ethiopian, Ministry of Health (2019).
44. United Nations Treaty Collections. Nd. International Covenant on Economic, Social and Cultural Rights. G.A. Res. 2200A/21(1966). Available online at: https://treaties.un.org/Pages/ViewDetails.aspx?src=IND&mtdsg_no=IV-3&chapter=4.
45. UN General Assembly. Universal declaration of human rights (217 [III] A). Paris: United Nations (1948).
46. World Health Organization. Podoconiosis: endemic non-filarial elephantiasis (2011). Available at: http://www.who.int/neglected_diseases/diseases/podoconiosis/en/.
47. Molla YB, Le Blond JS, Wardrop N, Baxter P, Atkinson PM, Newport MJ, et al. Individual correlates of podoconiosis in areas of varying endemicity: a case-control study. PloS Negl Trop Dis. (2013) 7:e2554. doi: 10.1371/journal.pntd.0002554
48. Engdawork K, McBride CM, Ayode D, Allen CG, Davey G, Tadele G. Rural youths’ understanding of gene x environmental contributors to heritable health conditions: The case of podoconiosis in Ethiopia. PloS Negl Trop Dis. (2018) 12:e0006763. doi: 10.1371/journal.pntd.0006763
49. Elias A, Nohmi M, Yasunobu K, Ishida A. Effect of agricultural extension program on smallholders’ farm productivity: Evidence from three p. The Journal of Agricultural Science (2013) 5, 163. doi: 10.5539/jas.v5n8p163.
50. Bautista-Gomez MM, Doerfler J, Del Mar Castro M. Barriers to cutaneous leishmaniasis care faced by indigenous communities of rural areas in Colombia: a qualitative study. BMC Infect Dis. (2022) 22:302. doi: 10.1186/s12879-022-07204-w
51. Oldenburg CE, Sié A, Ouattara M, Bountogo M, Boudo V, Kouanda I, et al. Distance to primary care facilities and healthcare utilization for preschool children in rural northwestern Burkina Faso: results from a surveillance cohort. BMC Health Serv Res (2021) 21(1):212. doi: 10.1186/s12913-021-06226-5
52. Hodge A, Byrne A, Morgan A, Jimenez-Soto E. Utilisation of health services and geography: deconstructing regional differences in barriers to facility-based delivery in Nepal. Maternal Child Health J. (2015) 19:566–77. doi: 10.1007/s10995-014-1540-x
53. Garapati P, Pal B, Siddiqui NA, Bimal S, Das P, Murti K, et al. Knowledge, stigma, health seeking behaviour and its determinants among patients with post kalaazar dermal leishmaniasis, Bihar, India. PloS One. (2018) 13:e0203407. doi: 10.1371/journal.pone.0203407
54. Molla YB, Tomczyk S, Amberbir T, Tamiru A, Davey G. Podoconiosis in east and west Gojam zones, northern Ethiopia. PloS Negl Trop Dis. (2012b) 6:e1744. doi: 10.1371/journal.pntd.0001744
55. Tekola F, Bull S, Farsides B, Newport MJ, Adeyemo A, Rotimi CN, et al. Impact of social stigma on the process of obtaining informed consent for genetic research on podoconiosis: a qualitative study. BMC Med ethics (2009) 10:13. doi: 10.1186/1472-6939-10-13
56. Curtis V. Why disgust matters. Philos Trans R Soc B: Biol Sci. (2011) 366:3478–90. doi: 10.1098/rstb.2011.0165.
57. Subbotsky EV. Causal explanations of events by children and adults: Can alternative causal models coexist in one mind? Br J Dev Psychol. (2001) 19:23–46. doi: 10.1348/026151001165949.
58. Legare CH, Rosengren K, Evans M, Harris P. The coexistence of natural and supernatural explanations across cultures and development. Soc Res Child Dev. (2012) 83:779–93. doi: 10.1111/j.1467-8624.2012.01743.x.
59. Ayode D, McBride CM, de Heer HD, Watanabe E, Gebreyesus T, Tora A, et al. A qualitative study exploring barriers related to use of footwear in rural highland Ethiopia: implications for neglected tropical disease control. PloS Negl Trop Dis. (2013) 7:e2199. doi: 10.1371/journal.pntd.0002199
60. Rao S, Garole V, Walawalkar S, Khot S, Karandikar N. Gender differentials in the social impact of leprosy. Leprosy Rev. (1996) 67:190–9. doi: 10.5935/0305-7518.19960019
61. Wharton-Smith A, Rassi C, Batisso E, Ortu G, King R, Endriyas M, et al. Gender-related factors affecting health seeking for neglected tropical diseases: findings from a qualitative study in Ethiopia. PloS Negl Trop Dis. (2019) 13:e0007840. doi: 10.1371/journal.pntd.0007840
62. Dijkstra JIR, Van Brakel WH, Van Elteren M. Gender and leprosy-related stigma in endemic areas: A systematic review. Leprosy Rev. (2017) 88:419. doi: 10.47276/lr.88.3.419.
63. Courtright P, West SK. Contribution of sex-linked biology and gender roles to disparities with trachoma. Emerg Infect Dis. (2004) 10:2012–6. doi: 10.3201/eid1011.040353
64. Negussie H, Molla M, Ngari M, Berkley JA, Kivaya E, Njuguna P, et al. Lymphoedema management to prevent acute dermatolymphangioadenitis in podoconiosis in northern Ethiopia (GoLBeT): a pragmatic randomised controlled trial. Lancet Global Health. (2018) 6:e795–803. doi: 10.1016/S2214-109X(18)30124-4
65. Wang J, Geng L. Effects of socioeconomic status on physical and psychological health: lifestyle as a mediator. Int J Environ Res Public Health. (2019) 16:281. doi: 10.3390/ijerph16020281
66. Lutfey K, Freese J. Toward some fundamentals of fundamental causality: Socioeconomic status and health in the routine clinic visit for diabetes. Am J Sociol. (2005) 110:1326–72. doi: 10.1086/428914
67. Setargie F. The impact of foreign aid on economic growth of Ethiopia. J Econ Sustain Dev. (2015) 6:122–31.
68. Tewodros G, Solomon T. Predictability of foreign aid and economic growth in Ethiopia Vol. 10. United KIngdom: Cogent Economics & Finance (2022). p. 2098606. doi: 10.1080/23322039.2022.2098606
69. Brown W. SOVEREIGNTY MATTERS: AFRICA, DONORS, AND THE AID RELATIONSHIP. Afr Affairs (2013) 112:262–82.
70. David W. The World Bank and Social Transformation in International Politics. London: Routledge (2008).
71. Plank DN. Aid, Debt, and the End of Sovereignty: Mozambique and Its Donors. J Modern Afr Stud (1993) 31(03):407. http://www.jstor.org/stable/41413028.
72. Wright G. NGOs and Western hegemony: causes for concern and ideas for change. Dev Pract. (2012) 22:123–34.
73. Hellström L, Beckman L. Life challenges and barriers to help seeking: adolescents’ and young adults’ Voices of mental health. Int J Environ Res Public Health. (2021) 18:13101. doi: 10.3390/ijerph182413101
74. Parks T. The Rise and Fall of Donor Funding for Advocacy NGOs: Understanding the Impact. Dev Pract (2008) 18(2):213–22. http://www.jstor.org/stable/27751904.
75. Mahomed F, Bhabha J, Stein MA, Pūras D. Establishing good practice for human rights-based approaches to mental health care and psychosocial support in Kenya. Health Hum Rights. (2020) 22:139–53.
76. Shahvisi A, Meskele E, Davey G. A human right to shoes? Establishing rights and duties in the prevention and treatment of podoconiosis. Health Hum Rights. (2018) 20:53–65.
77. Edwards N, Di Ruggiero E. Exploring which context matters in the study of health inequities and their mitigation. Scand J Public Health. (2011) 39:43–9. doi: 10.1177/1403494810393558
78. Craig P, Di Ruggiero E, Frohlich KL, Mykhalovskiy E, White M, behalf of the Canadian Institutes of Health Research (CIHR)–National Institute for Health Research (NIHR) Context Guidance Authors Group. Taking account of context in population health intervention research: guidance for producers, users and funders of research. Southampton: NIHR Evaluation, Trials and Studies Coordinating Centre (2018).
79. Lisa G ed. Lived experience. In: The SAGE Encyclopaedia of Qualitative Research Methods. SAGE Publications.
Keywords: contextual factors, neglected tropical diseases, podoconiosis, Ethiopia, intervention, evaluation
Citation: Engdawork K, Tadele G, Nahar P, Davey G and Zaman S (2024) The effect of contextual factors on a health intervention against podoconiosis in Ethiopia. Front. Trop. Dis 5:1346368. doi: 10.3389/fitd.2024.1346368
Received: 29 November 2023; Accepted: 07 February 2024;
Published: 06 March 2024.
Edited by:
Joseph Daniel Turner, Liverpool School of Tropical Medicine, United KingdomReviewed by:
Manuel Ritter, University Hospital Bonn, GermanyJan Douglass, James Cook University, Australia
Copyright © 2024 Engdawork, Tadele, Nahar, Davey and Zaman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kibur Engdawork, S2lidXIuZW5nYXdvcmtAYWF1LmVkdS5ldA==
 Kibur Engdawork
Kibur Engdawork Getnet Tadele
Getnet Tadele Papreen Nahar
Papreen Nahar Gail Davey
Gail Davey Shahaduz Zaman
Shahaduz Zaman