- 1Technical Department, Unlimit Health, London, United Kingdom
- 2Research and Innovation Department, Unlimit Health, London, United Kingdom
- 3Programme National de Lutte Contre les Maladies Tropicales Négligées à Chimiothérapie Préventive, Ministry of Health of Côte d'Ivoire, Abidjan, Côte d’Ivoire
- 4Africa Open Lab, GlaxoSmithKline, Brentford, United Kingdom
- 5Sociology Department, Félix Houphouët-Boigny University, Abidjan, Côte d’Ivoire
- 6Monitoring, Evaluation and Research Department, Unlimit Health, London, United Kingdom
Introduction: Female genital schistosomiasis (FGS) is a neglected gynecological condition, putting women at-risk of poor sexual and reproductive health (SRH), including pregnancy complications or infertility. Early treatment of schistosomiasis with praziquantel is important to avoid disease progression to FGS as it is not always possible to reverse these symptoms. However, prevention programs with praziquantel have historically focused on school-aged children. Therefore, there is a gap to provide prevention services for young women in endemic areas, including Côte d’Ivoire.
Methods: We piloted integration of FGS prevention services into routine SRH care in seven health centers (Soubré district, Côte d’Ivoire, November 2020 to April 2021) and enrolled 56 health workers. We used mixed methods including key informant interviews, focus group discussions, and questionnaires to determine effectiveness, feasibility and acceptability of integration across health system decision makers, health workers and female patients (15 to 29 years old). For qualitative data, we used an inductive coding process to analyze themes. We used descriptive statistics to analyze quantitative data.
Results: Interviewed health workers perceived that the integrated services increased access and improved health outcomes for women (15 to 29 years old) due to the more comprehensive approach, although barriers to access included lack of transportation. Female patients surveyed at baseline (n=448) indicated there were no routine FGS prevention services. During the pilot, FGS prevention services were provided to >8500 women at-risk. Health workers interviewed at the end of the pilot indicated they could feasibly provide FGS prevention services as part of routine patient consultations, and they maintained knowledge from training on the key FGS health education points and the consultation processes to follow. The greatest challenge expressed by health workers was the high workload.
Discussion: Provision of integrated healthcare in the health center setting is an effective and acceptable way to increase access to prevention services and provide holistic care for women (15 to 29 years old) in this setting in Côte d’Ivoire. Future scale-up will require further streamlining of the strategy, building on existing platforms, whilst ensuring reduced impact on workload and consideration of how to overcome barriers to accessing health centers.
Introduction
Female genital schistosomiasis (FGS) is likely to be one of the most common gynecological conditions in places where prevalence of Schistosoma haematobium is elevated, yet it remains largely unknown and with almost no routinely available health services (1–3). It is estimated that 56 million women and girls across Africa are affected by FGS, given that up to 75% of women with S. haematobium infection will develop symptoms (1, 2, 4). Chronic infection leads to symptoms and complications including vaginal itching and discharge, post-coital bleeding, genital lesions, ectopic pregnancy, spontaneous abortion or infertility which are the consequence of schistosome eggs being deposited in the uterus, cervix, vagina, or vulva (2, 4, 5). The immunological reaction to the eggs has also been linked to prevalent human papillomavirus (HPV) and human immunodeficiency virus (HIV) (2, 6–9). Those at-risk of FGS are vulnerable population groups as transmission of schistosomiasis is caused by skin contact with freshwater sources, previously contaminated due to the lack of appropriate sanitation. Furthermore, the condition is significantly associated with young women (18 to 29 years old), who are more likely to be in contact with these water sources due to social and cultural activities such as collecting water, washing clothes or dishes, or bathing children, which can lead to greater risk of transmission (2, 10, 11).
Lack of awareness of FGS at all levels from the community upwards exacerbates the ability to address the condition. Stigma relating to the similarity of symptoms with sexually transmitted infections (STIs) is a significant issue for women suffering from FGS. A qualitative study in Ghana highlighted that stigma from health workers was a major barrier for women and girls seeking care because of the misunderstanding that FGS is linked to sexual promiscuity (11). In addition, qualitative research from Ghana and Tanzania has found that the complications associated with FGS can impact women’s mental wellbeing (2, 11). Given that FGS is not included in medical textbooks or trainings, lack of awareness amongst the medical profession can also lead to misdiagnosis and wasted time or negative outcomes for patients through ineffective treatments (1, 11–13).
The treatment used for schistosomiasis (praziquantel) kills the adult parasites, preventing further eggs being deposited. However, for women already suffering from FGS, praziquantel may only provide small improvements to existing symptoms and no current validated therapeutic options exist (4, 5). Prevention is therefore essential to avoid the development of more severe and potentially irreversible morbidity and is also recommended by the World Health Organization (WHO) (3, 14). There is increasing support for integration of FGS with existing HIV, HPV and other sexual and reproductive health (SRH) services, given that there are effective prevention interventions for all three diseases and pre-existing health platforms (3, 14, 15). Moreover, there is growing evidence that preventive chemotherapy with praziquantel could also be effective at averting new HIV infections, by reducing the prevalence of women with FGS-associated genital symptoms which put them at higher risk of transmission (8, 16, 17). Despite this there is very little research on how integration of prevention services should be conducted and what the consequences of integration are.
To provide evidence on the effectiveness, feasibility and acceptability of integration, this study piloted integration of FGS prevention services with routine SRH services in Côte d’Ivoire where the risk of S. haematobium infection remains high in certain districts (as defined by the 2022 WHO schistosomiasis guidelines) (18, 19). Furthermore, the ramifications of FGS are serious as the prevalence of HIV and rate of new infections is higher in women (≥15 years) than in men (20). Therefore, the focus of this study was to design and test processes and resources to support sustainable integration, allowing more women at-risk of FGS to have access to prevention services.
Methods
Study setting and population
The pilot study for integration of services was conducted in seven health centers in Soubré district, in Côte d’Ivoire, from November 2020 to April 2021 (Figure 1). The district was selected based on the high co-endemicity of HIV and S. haematobium. Prevalence of schistosomiasis was 41.9%, considered “moderate risk” according to WHO 2011 guidelines in use at the time of the study (21). Adults were therefore not targeted for preventive chemotherapy with praziquantel during annual mass drug administration (MDA) conducted by the Ministry of Health (MoH). Soubré district is known for agriculture and many fields have standing pools of water from the abundant river systems.
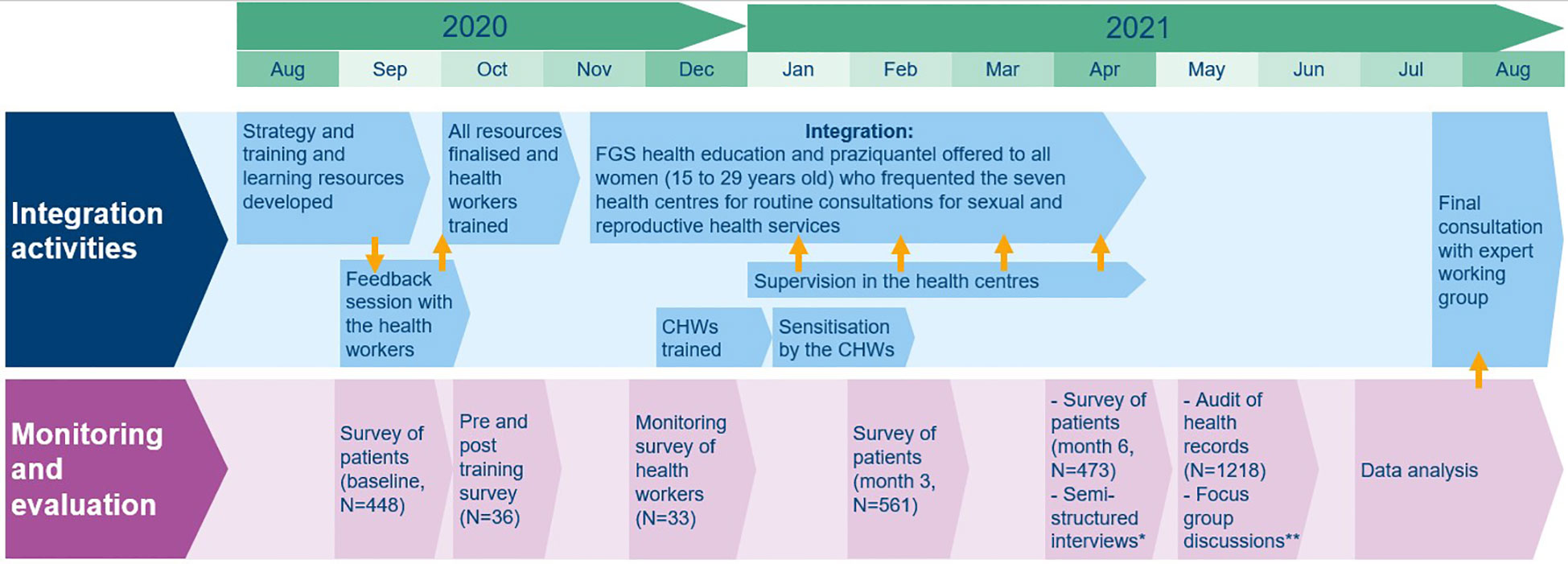
Figure 1 Overview of activities and timeline of the pilot study to integrate FGS prevention services into the national health system in Côte d’Ivoire. *Semi-structured interviews with decision makers (N=4), health workers (N=33), patients (N=40). **Focus group discussions with health workers (one group, N=10), CHWs (one group, N=9).
The health centers were selected based on the following criteria: provision of HIV/AIDS and SRH services, presence of ≥five health workers who provide first point of contact consultations and approximately 50 patients (women aged between 15 to 29 years old) visiting per week. Of the seven selected health centers, five were first-contact centers (primary healthcare), one was a medical facility focused on student care, and one was a general hospital.
There were three study populations selected for the following reasons:
1. All health workers (adults, male and female) providing first point of contact consultations for SRH at the selected health centers. This included doctors, nurses and midwives.
2. Female patients (women aged between 15 to 29 years old) who attended the selected health centers for routine HIV/AIDS and other SRH services. This age group is inclusive of those most significantly associated with having the condition and adolescents of ≥15 years old who fall outside the range of school-aged children (five to 14 years old) and therefore would not be included in the annual MDA programme. As the health centers were located in a district highly co-endemic for HIV and S. haematobium, female patients attending routine HIV/AIDS and other SRH services, who were within this age group, were assumed to be at-risk of developing FGS.
3. Community health workers (CHWs) (adults, male and female) who worked with the selected health centers and endemic communities in the catchment areas.
Intervention strategy development
A participatory design process was used to gather contextual and technical input to inform the development of the strategy and resources and to review and refine during planned phases of the pilot. Initial strategy development was conducted through consultations with the Neglected Tropical Disease (NTD) Programme [known as Programme National de Lutte Contre les Maladies Tropicales à Chimiothérapie Préventive (PNLMTN-CP)], MoH of Côte d’Ivoire and by health worker feedback (Figure 1). Feedback from the PNLMTN-CP and data collected from health workers and patients (described below) was used to make adjustments during implementation. The strategy was reviewed after implementation through the formation of an expert working group of national stakeholders (including members from the NTD, HIV and mother and child health programs of the MoH, from the governing body of the national health information system, and from research institutions). The purpose of which was to provide recommendations for future planning and to continue engaging on FGS beyond the scope of the pilot.
Intervention strategy
FGS prevention services were integrated into existing SRH health services (including for HIV/AIDS), targeting female patients aged 15 to 29 years old. The FGS prevention services were provided to each woman of the target population as part of the routine service and consisted of offering preventive chemotherapy (praziquantel) and FGS health education on prevention. Female patients in this target population were considered at-risk of schistosomiasis and therefore developing FGS since the services were located in an endemic district and considering the implications of being in this age group (highlighted in the Study Setting and Population section). For the purposes of this study, “integration” is defined as training existing health workers to provide praziquantel and FGS prevention messages during routine consultations, whilst also utilizing existing health reporting systems and existing drug-procurement systems for praziquantel delivery.
All health workers at the selected health centers (56 in total) were trained to follow three key steps during each consultation with female patients of 15 to 29 years old: Step one) Provide FGS prevention messages, including explaining what FGS is, the symptoms, risks, complications, the transmission cycle and preventive chemotherapy; Step two) Offer praziquantel, including confirming consent, offering a snack to prevent side effects from the drug and measuring dose accurately with dose pole or weighing scales; and Step three) Report the patient information and services provided using the FGS patient registration form. Training of 36 health workers took place in October 2020 prior to the start of the intervention (Figure 1) and training of the remaining 20 health workers took place in January 2021, upon further identification of their involvement in SRH services. All trained health workers provided FGS prevention services during implementation (Steps one, two and three).
CHWs (30 in total) were trained in December 2020 (Figure 1) to follow three key steps for women in the community: Step one) Provide FGS prevention messages; Step two) Refer women (15 to 29 years old) who present with FGS associated symptoms to one of the selected health centers; and Step three) Support the health workers to care for any women developing side effects in the community.
A training and learning resources package was developed to support integration:
● Training resources: all materials and messages for the training of health workers including presentation slides, resources for interactive activities and guide for the trainer. These resources were later adapted for CHWs.
● Information system integration resources: form to report patients with side effects from praziquantel (already in place in the health system), form to register information on FGS after each consultation (it had been planned to integrate the forms with official health registers, this was not possible within the timeframe of the study as the registers had already been printed for the year), mechanism to report any other problems.
● Awareness raising resources for health workers: aide-mémoire detailing key points from the training; it was used as a guide to follow during patient consultations and included a decision tree to support safe treatment of female patients. This was adapted for use by CHWs, including removing aspects on treatment.
● Awareness raising resources for female patients and women (15 to 29 years old) in the community: leaflet detailing key FGS prevention information. This was developed into a pictorial guide for use by CHWs during dissemination activities.
Data collection
Mixed methods were used in the monitoring and evaluation of the study, including the following qualitative and quantitative data collection activities: a survey of patients at baseline and months three and six of integration, a pre- and post-test during the training of health workers, a monitoring survey of the initial month of implementation by health workers, an audit of a selection of health records from the final month of implementation, semi-structured interviews with decision makers, health workers and patients (women 15 to 29 years old), and focus group discussions (FGDs) with health workers and CHWs (Figure 1).
Qualitative data collection
Participants were purposively selected based on their involvement in the pilot study. Semi-structured key informant interviews were conducted with 33 health workers and two FGDs (one with nine CHWs and one with ten health workers) were conducted to understand the perceived effectiveness, feasibility and acceptability of the processes and resources. The FGDs included a “force field” participatory exercise, in which participants jointly elucidated key facilitators and barriers for effective dissemination of health information. The exercise involved an interactive group work activity and was carried out in a series of steps: firstly, two sub-groups worked in parallel, one examining the “forces” (or factors) that support the achievement of the intervention and another examining the “forces” that acted as barriers; secondly, the sub-groups gathered again to present their work and collectively agree on a final list of positive and negative “forces”; and finally, these were scored and ranked according to their effect on outcomes. The aim of the activity was to ensure all members contributed and a consensus was reached on the “forces” which were most impactful (22).
Health workers were purposively selected if they had been trained as part of the study (out of the 56 in total) and had subsequently been involved in providing the FGS prevention services. They were selected evenly across the seven selected health centers, and representatives of each cadre (doctors, nurses, midwives) were asked to participate. CHWs were also purposively selected if they had been trained and were involved in community sensitization activities. They were selected evenly across the selected health center catchment areas.
Semi-structured key informant interviews with patients (40 women of 15 to 29 years old) were conducted to understand perceived acceptability and outcomes from the interactions with the services. Patients were selected evenly across four of the seven selected health centers (these were randomly selected and retained for quantitative data collection, described below). They were purposively selected if they were female, aged 15 to 29 years, and had attended the selected health centers for routine SRH services.
Semi-structured key informant interviews with four decision makers from the health center and district level who were involved in the pilot were conducted to understand acceptability, feasibility and capacity of the health workers. At the district level, all decision makers involved with the study were selected, at the health center level two heads of the centers were asked to participate based on their role leading health programs at this level. Data collection was conducted in French, recorded and transcribed. Interviews lasted between 30 minutes to one hour and the FGDs lasted three hours, on average.
Data collection was conducted by the Sociology Department of the University Félix Houphouët Boigny (UFHB), in collaboration with the PNLMTN-CP. Timelines for qualitative data collection can be seen in Figure 1 in the monitoring and evaluation section.
Quantitative data collection
All 36 health workers trained during the first training session were asked to participate in a pre- and post-training survey, conducted on papers forms, and all completed this as part of the training. Four were excluded due to participants only completing the post-training survey. 33 of the 36 initially trained health workers (three were not available) took part in a monitoring survey conducted one month after the start of integration, across all seven selected health centers. This prospectively determined any challenges with integration, logistics or resources. The monitoring survey was collected by two surveyors on survey phones using the application SurveyCTO (23).
Four health centers were selected randomly out of the seven at baseline and then retained for additional monitoring. Patients at the four health centers were surveyed at three timepoints during the pilot, once at baseline to assess knowledge of FGS and existing FGS services, and then repeated at month three and six of integration to assess knowledge of FGS after interaction with the services and acceptability and effectiveness of services. Data were collected by four surveyors, each based at one health center over two weeks, using phones with the application SurveyCTO (23). All female patients (15 to 29 years old) attending for routine SRH services were asked to participate in the survey.
An audit of the FGS patient registration forms was conducted for all forms completed during month six of integration, at the same four health centers. The verification was conducted by four auditors, using phones with the application SurveyCTO (23).
Surveyors and auditors were trained personnel from the Sociology Department of UFHB. Timelines for quantitative data collection can be seen in Figure 1 in the monitoring and evaluation section.
Qualitative data analysis
Transcribed interviews for health workers and decision makers were translated from French to English by professional translators, all other transcripts were analyzed in French. A data-driven inductive process was used to code. Codes were then grouped into overarching themes, informed by the objectives of each activity to develop an analytical framework for each study population. Data were interpreted by consolidating the themes across all coded transcripts. Coding and analysis were conducted using the MAXQDA 11 Qualitative Analysis Software (24).
Quantitative data analysis
Survey and audit data were analyzed using descriptive statistics through the software R (2022) or Microsoft Excel (2022) (25, 26). Survey variables analyzed included demographic information, FGS knowledge, FGS services provided and perceptions of these. Audit variables analyzed included patient information, FGS services provided and health worker adherence to service processes. Data collected through the different methods, across the same time points, were triangulated.
Service coverage was calculated during the audit based on the following: total number of FGS patient registration forms completed in April 2021 where at least one category of information provided and praziquantel taken/total number of female patients of the target population as registered through the routinely collected health records.
Ethical considerations
Ethical approval was obtained from the Comité National d’Ethique des Sciences de la vie et de la Santé, in Côte d’Ivoire (reference number: 120-20/MSHP/CNESVS-km). Written informed consent for those ≥18 years of age was obtained prior to any data collection or provision of FGS prevention services. For those between 15 to 17 years, written assent was obtained in addition to informed consent from a parent or guardian. All relevant information was provided in French and health workers and data collection teams were able to provide additional explanation in the main local languages of Dioula and Baoulé as required.
Praziquantel was administered under supervision by trained health workers, and any side effects were dealt with in accordance with the health center and MoH procedures. Any female patient who could not be treated for her SRH needs at the selected health centers were referred for more specialized care in line with MoH guidelines.
Results
Sociodemographic characteristics of participants
Female patients (15 to 29 years old)
Table 1 shows a summary of the sociodemographic characteristics of the female patients (15 to 29 years old) who were selected across the three timepoints of the surveys of patients. The numbers of participants vary across the three timepoints according to the number of patients visiting the selected health centers during the two-week data collection period.
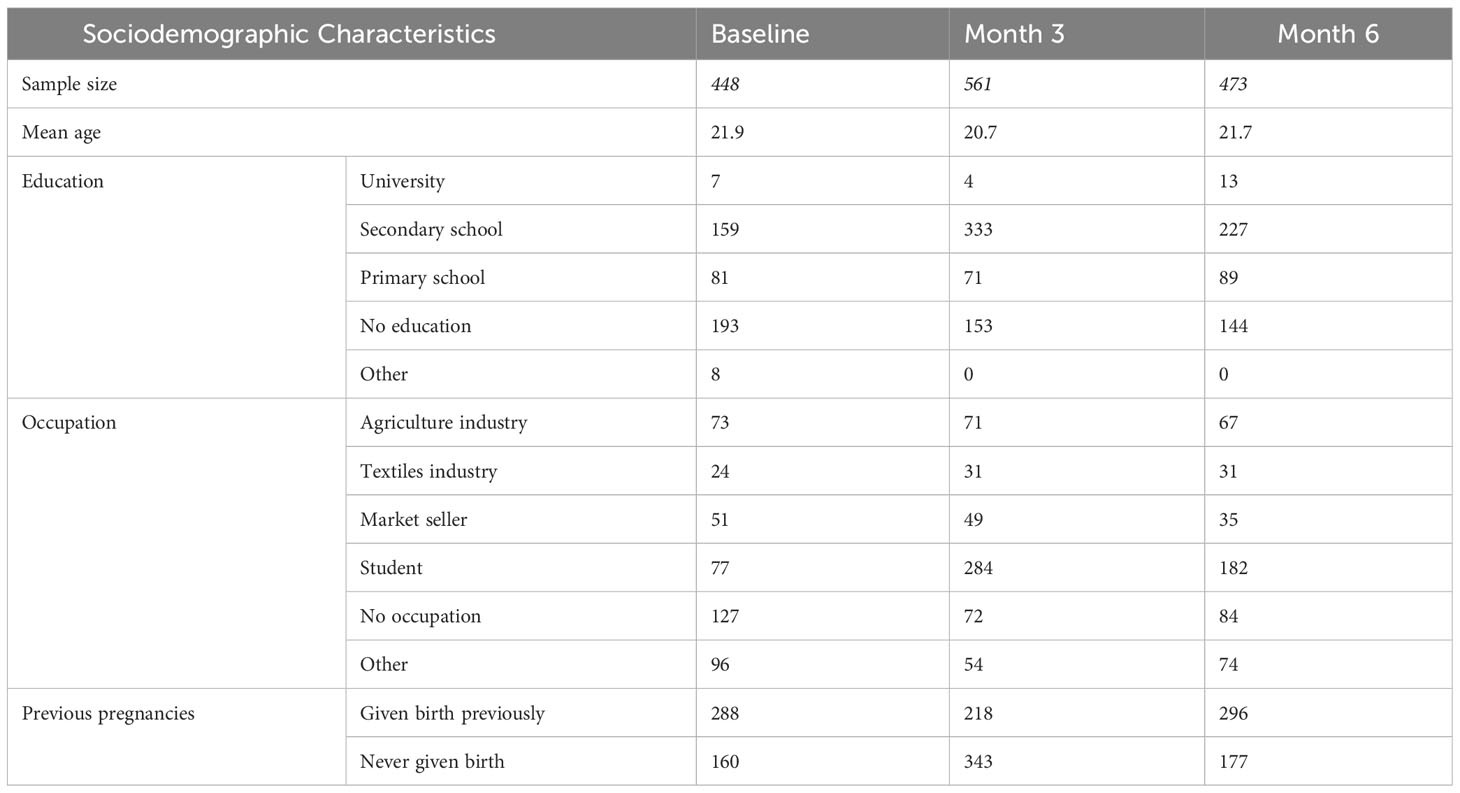
Table 1 Sociodemographic characteristics of selected female patients (15 to 29 years old) according to the surveys of patients.
Of the 40 female patients interviewed, they had a mean age of 19.7 years (ranging from 15 to 29 years old). Most were students (57.5%, n=23); the majority had also been educated to secondary school level (77.5%, n=31), none had been educated to a higher level than this, two had no formal education and five did not respond.
Health workers
Of the 33 health workers who were interviewed, this included both 15 males and 17 females (one not recorded) and from a range of medical professions including midwives, nurses and doctors across all seven selected health centers. They had been working in their current role for an average of 6.8 years (ranging from five months to 20 years). The FGD included five males and five females, across the medical professions mentioned and from all seven selected health centers.
CHWs
The FGD included six males and three females, representing five of the seven selected health centers, and had been in their roles as CHWs for an average of 7.9 years (ranging from one to 15 years); their work included activities for HIV/AIDS, neglected tropical diseases, malaria, tuberculosis and immunization programs.
Decision makers
Four decision makers were interviewed, all were males. Two of the decision makers were at the district level and had been in the role for seven and 16 years, and two decision makers were the heads of their health centers and had been in the role for one year each.
Baseline knowledge of FGS and provision of FGS services
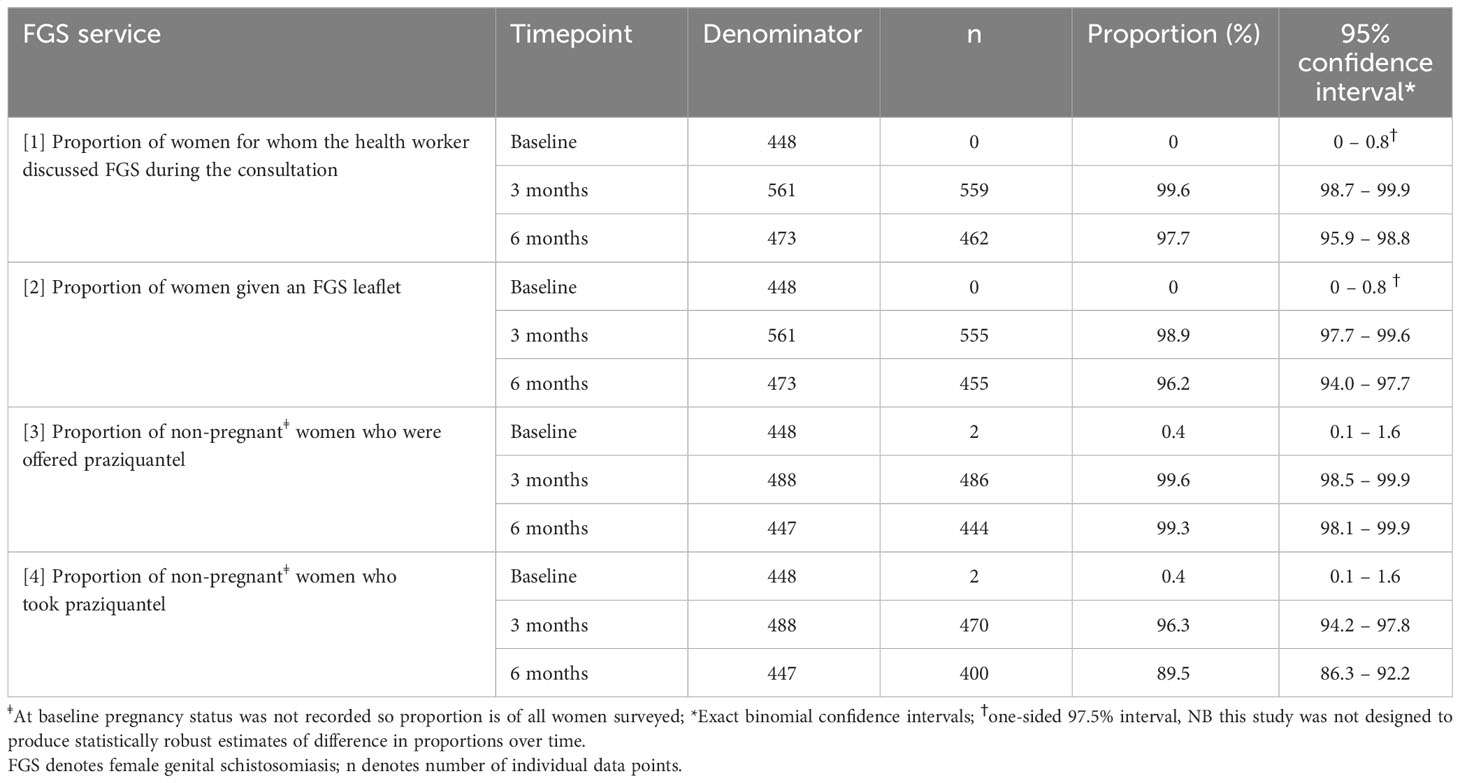
Of the 448 female patients surveyed at baseline, only 2.5% had heard of FGS previously (n=11). The majority of these participants were unaware of the symptoms, and none could describe how the disease is contracted or prevented in the community, nor could they name the medicine used to prevent it. Results from the survey showed that no routine services for FGS were available at baseline: the proportion of female patients with whom the health worker discussed FGS was zero at baseline and only two patients reported being offered praziquantel (Table 2).
The pre-training survey indicated that 37.5% (n=12) of surveyed health workers had heard of FGS. Of these, only 41.6% (n=5) recognized all the common symptoms associated with FGS and 16.6% (n=2) knew how it could be contracted. Most health workers (71.9%, n=23) had heard of praziquantel with only 37.5% (n=12) knowing that praziquantel is used to prevent or treat schistosomiasis. Any information provided to patients at the time only referred to schistosomiasis, not FGS. Only five health workers indicated that praziquantel was routinely available in their health center.
Provision of FGS prevention services during the study
At the health center level, there was a good level of adherence by health workers to the intervention processes of providing FGS prevention messages, offering praziquantel and then reporting. According to the patient surveys at months three and six, FGS services were provided in the majority of routine consultations (Table 2).
The audit of records conducted during the final month of implementation showed coverage of services amongst the target population which was lower than reported in the patient surveys. Coverage was only possible to calculate from two of the four audited health centers, due to incomplete health registers. For the two health centers, 45.3% (n=191) and 64.3% (n=218) of eligible patients received at least one of the key FGS prevention messages and took praziquantel.
At the community level, results from the CHW FGD indicated that they were able to follow the intervention processes. The CHWs indicated that they disseminated health information and that they understood how to report any instances of side effects to the health center for proper management, although no such instances occurred. The CHWs were trained to refer women in the community, only if they presented with symptoms associated with FGS to one of the seven selected health centers. In practice, the CHWs indicated that they referred all women who were between the ages of 15 to 29 years old.
Effectiveness and feasibility of FGS prevention service integration
Benefits of service integration
Most interviewed decision makers and health workers perceived that integration improved health outcomes by preventing FGS and infertility, and some also highlighted that HIV infections may be prevented. Other benefits identified by health workers included that they could meet the needs of the patients more holistically and that they were better able to recognize (“diagnose”) female patients who may be suffering from FGS. This had the additional benefits of improving treatment accuracy. For example:
“This is good, it allows us to avoid false diagnoses. When a person comes in with pelvic pain, we always miss it. But since we are told about FGS, we avoid unnecessary trips for this person. It is welcome because we now know what FGS is.” Male nurse
FGS health education
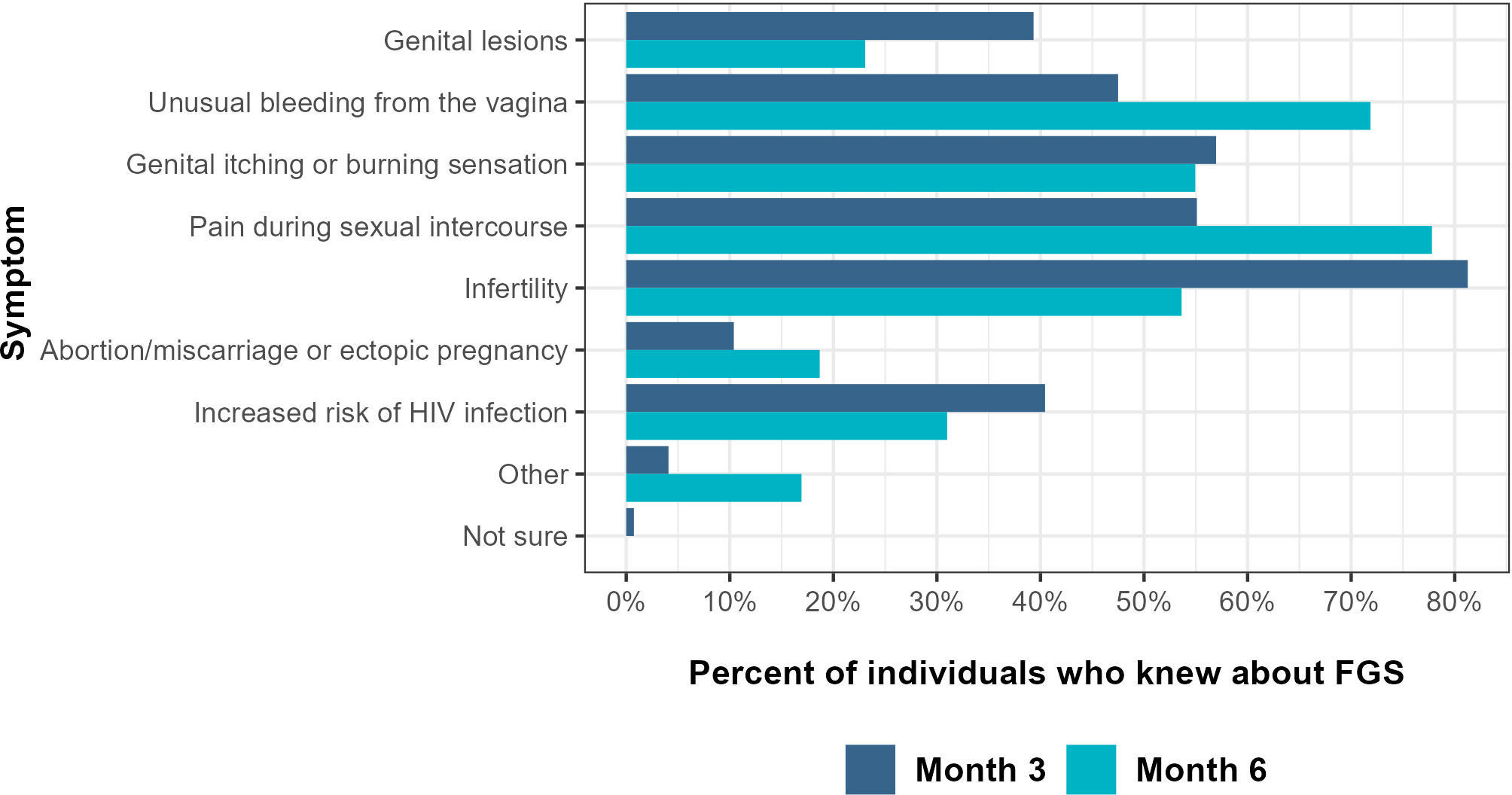
Patient interviews and the survey of patients at months three and six indicated that health workers effectively explained key FGS prevention information to female patients. After the consultation, all patients were aware of at least one symptom (Figure 2) and at month three and six 88% (n=472 and n=398 respectively) of patients mentioned bathing and washing clothes in open sources of water as a possible risk factor for transmission and 98% (n=527 and n=447 respectively) knew of the preventive treatment for FGS.
Health seeking behavior
Health workers considered that health seeking behavior improved through the involvement of CHWs, and health workers also highlighted that more women from the community were encouraged to come to the health center due to word of mouth from other patients, for example:
“…I gave two leaflets to two sisters who came. And then they left. I was visited by two other girls who came with the leaflets. I didn’t know them. They had the leaflets and they arrived. But they said … it was these leaflets that made them come. Because when the girls … the patients sent them the leaflets … they were neighbors, they understood that they had to come, because … they had been in contact with the water for a long time. So when they saw the pictures, they understood.” Female midwife
Access to FGS services
Access to FGS services improved during the pilot. At baseline routine FGS services were not available, during the intervention 8526 patients received praziquantel across all seven health centers from November 2020 to April 2021. Through the consultations, the medicine was provided for free. The survey of patients at months three and six indicated that the health center was considered the most convenient source to access praziquantel (74%, n=408, and 94%, n=433 respectively), compared to CHWs or pharmacies, with the latter being perceived as an expensive option due to the need to pay for the drug. However, health workers and CHWs identified several challenges for patient access to health centers including lack of transportation options for women in the community and not perceiving the need to attend if they considered themselves healthy or were too busy working. Health workers also reported that they could not always provide FGS services during routine consultations, due to challenges of workload or conflicting priorities in the cases of emergencies or patients going into labor.
Health worker capacity
Three areas were identified by the decision makers and health workers which influenced health worker capacity. Firstly, the effectiveness of the training; secondly, the workload of the health workers; and thirdly, the availability of resources, support and effective processes.
Firstly, health workers reported that the training was sufficient to conduct the FGS services and provided a sense of commitment to continued practice (mentioned in varying degrees by at least 24 health workers interviewed). For example:
“Well, with the arrival of FGS in our [health center], we have as an activity, it is the activity itself that has arrived, the FGS has entered into our habits, into the habits of the providers…” Male nurse
Knowledge of FGS and praziquantel was improved by the training and largely maintained by the health workers, according to the pre- and post-training survey and interviews conducted at the end of the integration period. Although, evidence from the audit observed that health workers had challenges measuring dose using weight. Comparing dose given to dose recommended by the WHO (40mg/kg) (27), based on the weight of the patient (for the patients where weight and dose was recorded, n=390), 79 patients were provided the correct dose while 258 were under dosed and 53 patients were provided a larger than recommended dose. The mean difference was 0.5 tablets less than required.
Secondly, the burden of the additional workload and the time constraints were a significant challenge, with one or both being mentioned by most health workers (n=29) and all decision makers. For example:
“There’s too much work and the ladies wait a long time, that’s the problem. When we finish the routine consultation, by the time she sits down to eat, it’s true that eating is good for her, but she sits down to eat and waits for it to happen, it’s a bit complicated. While there are other people still waiting. It is not easy.” Female nurse
Thirdly, overall, health workers affirmed that the required resources were available and that the support provided was sufficient at all levels of the system. However, health workers from all but one of the seven health centers reported challenges maintaining adequate food supplies (for patients to avoid praziquantel side effects) given fluctuations in patient numbers. Many health workers indicated that CHWs sensitizing women in the community supported them to provide FGS prevention messages during consultations. Health workers also reported that sharing tasks between colleagues supported them to overcome the challenges of workload, as explained:
“If you are alone in the facility, it is not easy. Why, because with FGS, it is necessary to take the time to explain there are several questions. Women often do not understand quickly … Here in [the health centre], there are three of us. This is the programme we have made. If one is doing the consultation, the others are doing the awareness-raising on FGS.” Female nurse
Health workers stated challenges with the reporting process which was considered time consuming as the form was not integrated with the routine health registers.
Acceptability of FGS prevention service integration
Decision makers
All decision makers cited advantages of integration, such as improving the ability to meet the needs of the patients, more efficient use of limited resources and more effective problem solving. Decision makers indicated the need for FGS services across Côte d’Ivoire, which was considered a gap prior to the intervention, as explained below:
“In terms of complete care, …the pregnant woman, I say the woman and especially those who have HIV are taken into account in a complete way by sculpting all the horizons, to be able to screen or prevent all the pathologies, and I think that it is very good.” Decision maker at district level
Acceptance was reduced in areas where decision makers reported the needs of the patients were not met. These included that the target population was deemed too narrow to reach all women of child-bearing age who might be at-risk and that due to the workload of the health workers, FGS and other routine services were sometimes conflicting rather than balanced. This is explained below:
“Especially since in the [health center] here you have seen for yourself that there are too many tasks. So there are sacrifices. They are even forced to conduct the activity. So this is a difficulty. That’s it! If you have to carry out the daily activities and then you have to do the activity at the same time, it’s very difficult.” Decision maker at health center level
Health workers
For health workers, the most significant factor positively influencing acceptance was the value that they accorded to preventing FGS and the associated morbidity of infertility (mentioned by 22 health workers interviewed). For example:
“So prevention of FGS is very important for woman because it saves her home in a way. During relations with her husband, there will hardly be any problems. And the little problems with the pill and all that can help her. It can help with the problems of delays in giving birth and so on. Well, the female reproductive system is very sensitive. We can make them aware of this and it’s especially when we talk about this that it encourages women to come to us.” Male nurse
In general, the health workers felt comfortable providing the services for FGS as they considered praziquantel safe and felt “comfortable in [their] method”.
However, health workers reported concerns with the ability of the intervention to reach all women at-risk due to challenges with patient access to the health centers. Furthermore, nine health workers also mentioned the concern that the target population was too narrow to reach all women at-risk.
Female patients
Female patients interviewed were positive about the health education aspects of the intervention. During month three and six of the patient survey, most female patients felt at ease discussing FGS with the health worker. Only two and four patients respectively reported feeling uncomfortable, for reasons including they did not think it was necessary or that it conflicted with their religious beliefs. In relation to using the recommended prevention measures, only a minority of patients who were interviewed (n=9) indicated that they could fully implement all recommendations in their daily routines and lifestyle. They reported that the main challenge was the lack of alternatives for interacting with open water sources, particularly when they visited rural settings, or activities which demanded constant water contact.
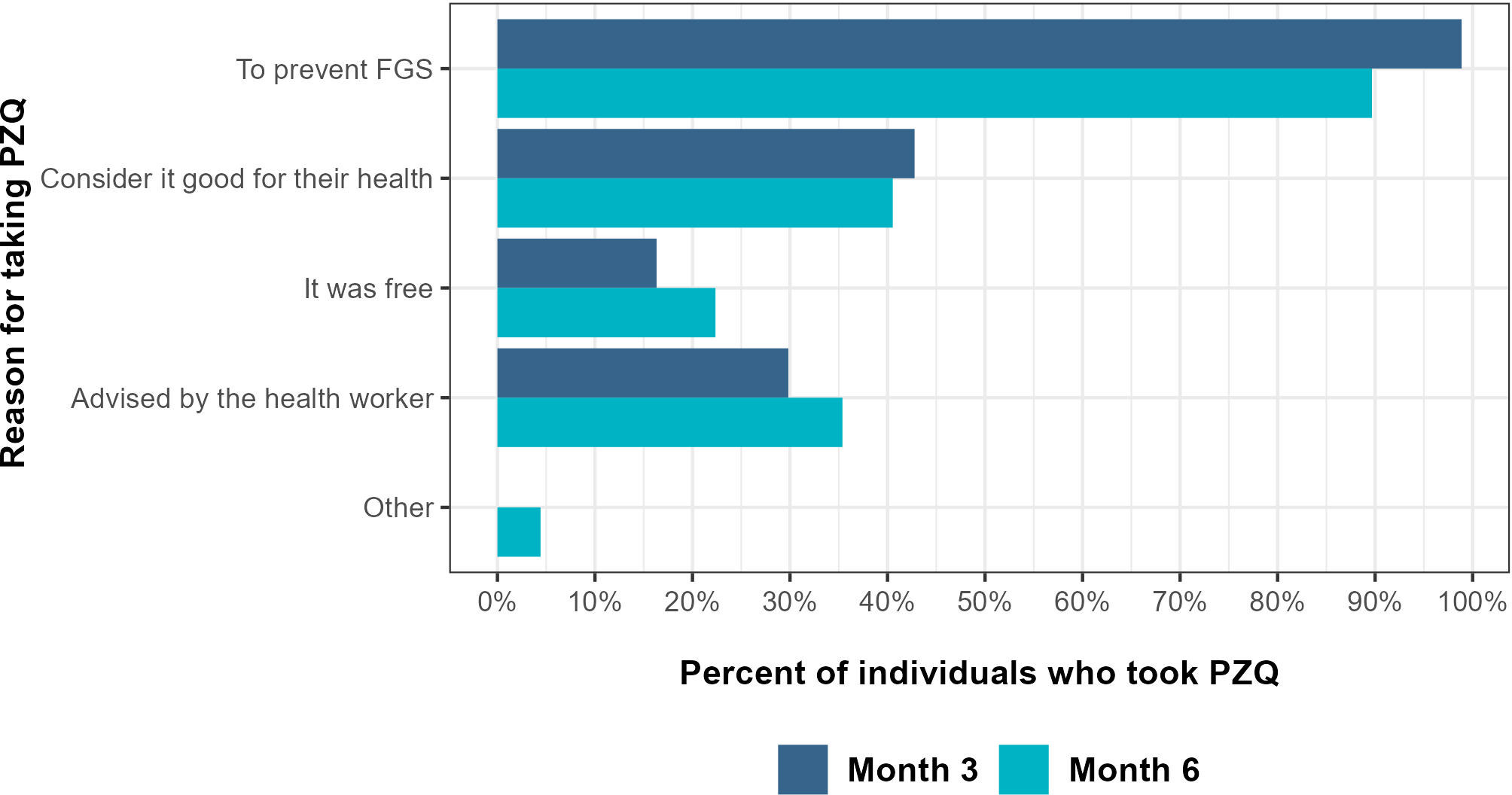
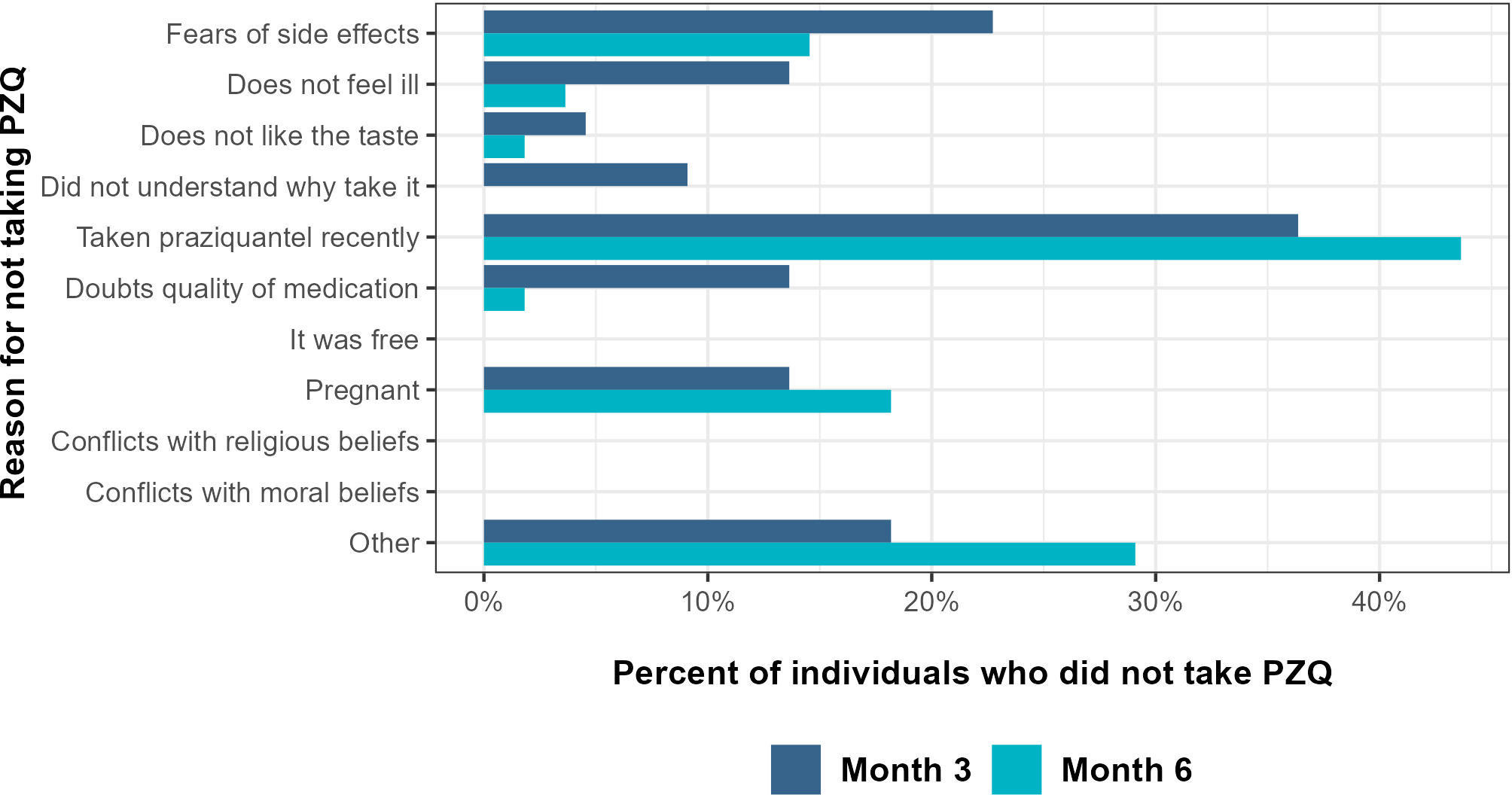
Treatment acceptance was high: most surveyed patients agreed to take praziquantel (96%, n=470, and 90%, n=400, at months three and six respectively). The reasons the patients decided to take praziquantel were largely related to the health benefits (Figure 3). Among the patients who did not take praziquantel, the key reasons that they stated were they had taken praziquantel recently, fear of side effects or “other”, including that they were too ill or for religious reasons (Figure 4). Health workers also raised some concerns around treatment acceptance, with a total of 19 health workers interviewed reporting at least one reason why patients may be reluctant to take praziquantel. Key motives identified included the size or bitter taste of the tablet, fear of side effects, or because they did not think it was necessary as they did not feel ill or were not in contact with water sources.
Discussion
Evidence from this pilot study indicates that integration of FGS prevention services into routine HIV/AIDS and SRH services has the potential to increase access, in a way that is considered acceptable and convenient, and provide more holistic care for women at-risk of FGS in Côte d’Ivoire. The study results address the gap to understand how women at-risk can be reached effectively. Furthermore, the positive impacts of this integration strategy were particularly stark given the lack of existing or routine services or training for health workers available. Research indicates that lack of awareness of health issues amongst health workers is a common factor leading to provision of inappropriate services or information and puts unnecessary strain on resources due to repeat patient visits (11, 15, 28, 29). This study highlighted how integration has the potential to improve health outcomes with health workers self-reporting their improved ability to recognize FGS symptoms and provide appropriate treatment. A comprehensive training package on FGS was a fundamental factor influencing the ability of health workers to provide effective services during this intervention. As found in many settings, as well as other health projects in Côte d’Ivoire, health workers are also a trusted source of information and if effectively trained they can improve awareness amongst patients (30–34). A true acceptance of the health messages provided through the intervention was highlighted by women sharing the information through word of mouth, demonstrating the importance of effective communication strategies to have wider reaching impacts on health and improving health seeking behavior (30, 35, 36).
Feasibility of implementation of the FGS services with routine SRH services was linked to the extent of integration with existing systems; for example, challenges arose due to lack of efficiency where the health record reporting was not fully integrated. This and the increased workload associated with the pilot strategy was a significant challenge for health workers in providing sustainable and consistent services. Overburdened workload has been consistently shown to be a challenge for successful integration, leading health workers to become stressed and demotivated (33, 37, 38). In addition to avoiding these outcomes, it is also important for this to be addressed to achieve the full benefits of integration of health services found in other settings, including improved efficiency of processes, resource and time management, and cost reductions (16, 39, 40). Based on evidence from the health workers, a potential solution to this would be to fully integrate all reporting processes to streamline the amount of work required by new services. Other solutions could come from considering all the interacting aspects and levels of the health system, by using a systems thinking approach (41, 42). For example, whilst the support provided by CHWs in sensitizing the community was greatly valued, they also increased demand on the services by raising awareness and referring women in the community. This impacted health worker workload and made the number of patients frequenting the health center harder to predict. With the introduction of new health services, changes in demand need to be monitored to ensure effective supply chain management and prevent human resources being overloaded. This demonstrates the importance of health system strengthening (HSS) to be considered alongside implementation of new services, to ensure there is sufficient capacity in the system (43). An important aspect of HSS is health worker capacity, which in this study was increased with training and the introduction of support systems. The ability of the health workers to retain the information provided during the training and maintain motivation meant that the services were still being provided to a high standard, with minimal adaptions, by the end of a six-month period. This indicates how, with appropriate support, the strategy implemented could lead to sustained impact on health outcomes for women at-risk of FGS.
A strong facilitator for the acceptability of the pilot by health workers and decision makers was that they perceived that the FGS services were important to provide for female patients. This was in terms of acknowledging the gap in existing services and the perceived importance of preventing women from developing FGS, particularly in relation to preventing the morbidity associated with infertility. The strong cultural importance surrounding fertility was something which resonated with stakeholders and women at-risk, highlighting how crucial context-specific messaging is to facilitate acceptance and uptake at all levels (44–46). Despite this, there was concern that the health center platform was not optimal for reaching all women in the catchment area who were likely to be at-risk. Challenges of access in more rural settings, as well as factors relating to characteristics and behaviors of the target age group (for example, that they would be busy working or not have perceived need to use health center services) posed a challenge. In this study, social mobilization by the CHWs was seen as essential to augment the positive outcomes of the integrated services, by raising awareness of the new services and of FGS. However, novel approaches are still required to overcome the barriers to coverage when using the health center as a platform for prevention, which could include elements of campaign-like approaches, as has been used in similar settings. Often, involvement of the health system structures at the community level, for example CHWs or trained traditional midwives, is crucial to the success of these approaches, and being members of the communities that they serve improves access (28, 33, 47). Exploring how these players could implement FGS prevention services, including praziquantel administration, in their communities, could be a feasible way to improve service reach, especially given their involvement in similar MDA campaigns for school-aged children. Alternatively, mobile clinics have also been an effective tool to reach more remote populations, for example for FGS screening (28, 30, 35).
Strengths and limitations
Triangulation of the results across the mixed methods approach is a key strength of this study methodology which facilitated the consolidation of evidence on the effectiveness, feasibility and acceptability of the integration of FGS prevention services. One limitation of the study was that the results on the coverage of services appeared to be lower according to the audit compared to the surveys of patients. During the surveys of patients, after the routine consultations, the health workers would direct the patients to the survey team. It is therefore possible that selection bias occurred either from the health workers or because female patients who had accepted the new services would also be more likely to accept to participate in the survey. Nevertheless, the results from the patient surveys remain an important indication that health workers were feasibly able to provide all the FGS services, even at six months after training, and providing key evidence on how the selected patients interacted with these services.
Conclusion
This pilot study provides evidence that FGS prevention services can be feasibly integrated with routine HIV/AIDS and SRH services, which is perceived as an important and necessary intervention for women at-risk, particularly given the challenges treating the long-term morbidity associated with the condition. The implementation of the integrated services in the selected health centers provided an effective platform to increase access to preventive chemotherapy for FGS and health education, with the training and health education aspects effectively improving awareness of FGS and key prevention measures. Following the pilot for integration, the expert working group (formed during the study) will consider how to overcome the challenges identified, to refine the strategy in preparation for scale up. This will be supported by the high level of buy-in shown by the MoH. Two key areas of focus include firstly the streamlining of processes to support the workload of health workers and secondly to identify the optimal strategy to combine the health center platform with community outreach to further improve the reach of prevention services. As endemic countries like Côte d’Ivoire continue increasing country ownership in line with the WHO NTD Roadmap to 2030, discussions around the sustainability of funding for integrated services and the availability of key resources such as praziquantel will need to continue. Integration at large scale has the propensity to effectively reach women at-risk, in accordance with the new WHO schistosomiasis guidelines to target all adults at-risk (19, 43), and to be a sustainable prevention measure that is resource- and cost-effective, with health impacts beyond just FGS prevention but also the possible prevention of suspected co-morbidities such as HIV and HPV.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Ethical approval was obtained from the Comité National d’Ethique des Sciences de la vie et de la Santé, in Côte d’Ivoire (reference number: 120-20/MSHP/CNESVS-km). Written informed consent for those ≥18 years of age was obtained prior to any data collection or provision of FGS prevention services. For those between 15 to 17 years, written assent was obtained in addition to informed consent from a parent or guardian.
Author contributions
AP: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. CV: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Resources, Validation, Writing – review & editing. AK: Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing. JN: Conceptualization, Funding acquisition, Methodology, Resources, Validation, Writing – review & editing. SL: Data curation, Investigation, Writing – review & editing. NDh: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – review & editing. NDj: Writing – review & editing. AT: Data curation, Investigation, Writing – review & editing. FF: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Validation, Visualization, Writing – review & editing. AM: Conceptualization, Methodology, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This pilot study was funded by UK AID via the Coalition for Operational Research on Neglected Tropical Diseases (COR-NTD), which is a Georgia nonprofit organization, with its principal place of business at 330 W. Ponce de Leon Ave, Decatur, Georgia 30030, USA. Grant number: NTD-SC_212D.
Acknowledgments
Thank you to all the women (15 to 29 years old) who attended the selected health centers during the study and agreed to participate or were involved at the community level. Thank you to the decision makers, health workers and community health workers who were involved in the study, who agreed to participate and committed their time and efforts to providing FGS prevention services. Thank you to all personnel (named as authors and other members of the team) from the Programme National de Lutte Contre les Maladies Tropicales à Chimiothérapie Préventive of the Ministry of Health in Côte d’Ivoire who led the implementation of the pilot study, provided technical input and leadership for strategy development and for their continued dedication to the fight against schistosomiasis and female genital schistosomiasis. Thanks also to the leaders within the Ministry of Health of Côte d’Ivoire who approved and supported this work. Thank you to the members of the Sociology Department of the University of Félix Houphouët Boigny (named as authors and other members of the team) who led the high-quality data collection of all monitoring and evaluation activities. Thank you to all colleagues within Unlimit Health (formerly SCI Foundation) (named as authors and other members of the team) who supported these activities, provided technical input and were dedicated to the success of the pilot and steps beyond. Thank you to Merck KGaA, the pharmaceutical company which donated praziquantel through the World Health Organization donation program, for the purposes of this pilot study. And finally, thank you to our funder UK AID via the Coalition for Operational Research on Neglected Tropical Diseases who provided the resources to allow the project to take place.
Conflict of interest
Author JN is currently employed by GlaxoSmithKline United Kingdom, during the time of study implementation and data collection she was employed by Unlimit Health. AP, CV, ND and FF was employed by Unlimit Health.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hotez PJ, Harrison W, Fenwick A, Bustinduy AL, Ducker C, Mbabazi PS, et al. Female genital schistosomiasis and HIV/AIDS: Reversing the neglect of girls and women. PloS Negl Trop Dis (2019) 13(4):e0007025. doi: 10.1371/journal.pntd.0007025
2. Downs JA, Mguta C, Kaatano GM, Mitchell KB, Bang H, Simplice H, et al. Urogenital schistosomiasis in women of reproductive age in Tanzania’s lake Victoria region. Am J Trop Med Hyg (2011) 84(3):364. doi: 10.4269/AJTMH.2011.10-0585
3. UNAIDS. No more neglect: female genital schistosomiasis and HIV (2019). Available at: https://www.unaids.org/en/resources/documents/2019/female_genital_schistosomiasis_and_hiv.
4. Christinet V, Lazdins-Helds JK, Stothard JR, Reinhard-Rupp J. Female genital schistosomiasis (FGS): from case reports to a call for concerted action against this neglected gynaecological disease. Int J Parasitol (2016) 46(7):395–404. doi: 10.1016/j.ijpara.2016.02.006
5. Hotez PJ, Fenwick A, Kjetland EF. Africa’s 32 cents solution for HIV/AIDS. PloS Negl Trop Dis (2009) 3(5):e430. doi: 10.1371/journal.pntd.0000430
6. Brodish PH, Singh K. Association between Schistosoma haematobium Exposure and Human Immunodeficiency Virus Infection among Females in Mozambique. Am J Trop Med Hyg (2016) 94(5):1040. doi: 10.4269/ajtmh.15-0652
7. Kjetland EF, Ndhlovu PD, Gomo E, Mduluza T, Midzi N, Gwanzura L, et al. Association between genital schistosomiasis and HIV in rural Zimbabwean women. AIDS (2006) 20(4):593–600. doi: 10.1097/01.aids.0000210614.45212.0a
8. Livingston M, Pillay P, Zulu SG, Sandvik L, Kvalsvig JD, Gagai S, et al. Mapping Schistosoma haematobium for Novel Interventions against Female Genital Schistosomiasis and Associated HIV Risk in KwaZulu-Natal, South Africa. Am J Trop Med Hyg (2021) 104(6):2055. doi: 10.4269/ajtmh.20-0679
9. Shukla JD, Kleppa E, Holmen S, Ndhlovu PD, Mtshali A, Sebitloane M, et al. The association between female genital schistosomiasis and other infections of the lower genital tract in adolescent girls and young women: A cross-sectional study in South Africa. J Low Genit Tract Dis (2023) 27(3):291–6. doi: 10.1097/LGT.0000000000000756
10. WHO. Schistosomiasis Fact Sheet (2022). Available at: https://www.who.int/news-room/fact-sheets/detail/schistosomiasis.
11. Kukula VA, MacPherson EE, Tsey IH, Stothard JR, Theobald S, Gyapong M. A major hurdle in the elimination of urogenital schistosomiasis revealed: Identifying key gaps in knowledge and understanding of female genital schistosomiasis within communities and local health workers. PloS Negl Trop Dis (2019) 13(3):e0007207. doi: 10.1371/journal.pntd.0007207
12. Leutscher PDC, Ramarokoto C, Hoffmann S, Jensen JS, Ramaniraka V, Randrianasolo B, et al. Coexistence of urogenital schistosomiasis and sexually transmitted infection in women and men living in an area where Schistosoma haematobium is endemic. Clin Infect Dis (2008) 47(6):775–82. doi: 10.1086/591127
13. Jacobson J, Pantelias A, Williamson M, Kjetland EF, Krentel A, Gyapong M, et al. Addressing a silent and neglected scourge in sexual and reproductive health in Sub-Saharan Africa by development of training competencies to improve prevention, diagnosis, and treatment of female genital schistosomiasis (FGS) for health workers. Reprod Health (2022) 19(1):20. doi: 10.1186/s12978-021-01252-2
14. WHO. Deworming adolescent girls and women of reproductive age. Policy brief (2022). Available at: https://www.who.int/publications/i/item/9789240037670.
15. Engels D, Hotez PJ, Ducker C, Gyapong M, Bustinduy AL, Secor WE, et al. Integration of prevention and control measures for female genital schistosomiasis, HIV and cervical cancer. Bull World Health Organ (2020) 98(9):615. doi: 10.2471/BLT.20.252270
16. Ndeffo Mbah ML, Poolman EM, Atkins KE, Orenstein EW, Meyers LA, Townsend JP, et al. Potential cost-effectiveness of schistosomiasis treatment for reducing HIV transmission in Africa – the case of Zimbabwean women. PloS Negl Trop Dis (2013) 7(8):e2346. doi: 10.1371/journal.pntd.0002346
17. Ndeffo Mbah ML, Kjetland EF, Atkins KE, Poolman EM, Orenstein EW, Meyers LA, et al. Cost-effectiveness of a community-based intervention for reducing the transmission of Schistosoma haematobium and HIV in Africa. Proc Natl Acad Sci U S A (2013) 110(19):7952–7. doi: 10.1073/pnas.1221396110
18. ESPEN, WHO. Cote d’Ivoire Schistosomiasis Profile (2022). Available at: https://espen.afro.who.int/diseases/schistosomiasis#&gid=201&pid=1.
19. WHO. WHO guideline on control and elimination of human schistosomiasis (2022). Available at: https://www.who.int/publications/i/item/9789240041608.
20. UNAIDS. Côte d’Ivoire. UNAIDS (2022). Available at: https://www.unaids.org/en/regionscountries/countries/ctedivoire.
21. WHO. Helminth control in school-age children: a guide for managers of control programmes, 2nd ed. World, Geneva: WHO Press. Vol. 78. (2011).
22. Narayanasamy N. Participatory Rural Appraisal: Principles, Methods and Application. India: SAGE Publications India Pvt Ltd. (2009).
23. Dobility Inc. SurveyCTO. Cambridge MA: Dobility Inc., (2017). Available at: http://www.surveycto.com/.
24. VERBI Software. MAXQDA. Berlin, Germany: VERBI Software (2021). Available at: https://www.maxqda.com/.
25. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing (2021). Available at: https://www.r-project.org/.
26. Microsoft Corporation. Microsoft Excel. Microsoft Corportation (2021). Available at: https://office.microsoft.com/excel.
27. WHO. Praziquantel: Getting the dosage right. Geneva: TDR. (2008). Available at: https://www.who.int/tdr/news/2008/praziquantel-dosing/en/.
28. Nemungadi TG, Furumele TE, Gugerty MK, Djirmay AG, Naidoo S, Kjetland EF. Establishing and integrating a female genital schistosomiasis control programme into the existing health care system. Trop Med Infect Dis (2022) 7(11):382. doi: 10.3390/tropicalmed7110382
29. Gyapong JO, Gyapong M, Yellu N, Anakwah K, Amofah G, Bockarie M, et al. Integration of control of neglected tropical diseases into health-care systems: challenges and opportunities. Lancet (2010) 375(9709):160–5. doi: 10.1016/S0140-6736(09)61249-6
30. Torres-Vitolas CA, Trienekens SCM, Zaadnoordijk W, Gouvras AN. Behaviour change interventions for the control and elimination of schistosomiasis: A systematic review of evidence from low- and middle-income countries. PloS Negl Trop Dis (2023) 17(5):e0011315. doi: 10.1371/journal.pntd.0011315
31. Rowe R, Calnan M. Trust relations in health care–the new agenda. Eur J Public Health (2006) 16(1):4–6. doi: 10.1093/eurpub/ckl004
32. Grant M, Wilford A, Haskins L, Phakathi S, Mntambo N, Horwood CM. Trust of community health workers influences the acceptance of community-based maternal and child health services. Afr J Prim Heal Care Fam Med (2017) 9(1):a1281. doi: 10.4102/phcfm.v9i1.1281
33. Piotrowski H, Oluwole A, Fapohunda VO, Adejobi JB, Nebe OJ, Soneye I, et al. Mixed-methods evaluation of integrating female genital schistosomiasis management within primary healthcare: a pilot intervention in Ogun State, Nigeria. Int Health (2023) 15:18–29. doi: 10.1093/inthealth/ihac073
34. Coulibaly M, Kouamé J, Kadjo F, Koumi-Mélèdje MD, Hounsa A, Sackoukouakou J, et al. Determinants of contraceptive use in Abidjan (Côte d’Ivoire). J Public Health Afr (2022) 13(2):2204. doi: 10.4081/jphia.2022.2204
35. Torres-Vitolas CA, Dhanani N, Fleming FM. Factors affecting the uptake of preventive chemotherapy treatment for schistosomiasis in Sub-Saharan Africa: A systematic review. PloS Negl Trop Dis (2021) 15(1):1–33. doi: 10.1371/journal.pntd.0009017
36. Inghels M, Coffie PA, Larmarange J. Recours aux soins de santé globale et de santé sexuelle et reproductive, chez les étudiants de l’université Houphouët-Boigny, Abidjan, Côte d’Ivoire. Rev Epidemiol Sante Publique (2017) 65(5):369–79. doi: 10.1016/j.respe.2017.04.059
37. Mutisya R, Wambua J, Nyachae P, Kamau M, Karnad SR, Kabue M. Strengthening integration of family planning with HIV/AIDS and other services: experience from three Kenyan cities. Reprod Health (2019) 16(Suppl 1):16. doi: 10.1186/s12978-019-0715-8
38. Amponsah-Dacosta E, Blose N, Nkwinika VV, Chepkurui V. Human papillomavirus vaccination in South Africa: programmatic challenges and opportunities for integration with other adolescent health services? Front Public Heal (2022) 10:799984. doi: 10.3389/fpubh.2022.799984
39. Sweeney S, Obure C, Maier C, Greener R, Dehne K, Vassall A. Costs and efficiency of integrating HIV/AIDS services with other health services: a systematic review of evidence and experience. Sex Transm Infect (2012) 88(2):85–99. doi: 10.1136/sextrans-2011-050199
40. Warren CE, Mayhew SH, Hopkins J. The current status of research on the integration of sexual and reproductive health and HIV services. Stud Fam Plann (2017) 48(2):91. doi: 10.1111/sifp.12024
41. Swanson RC, Cattaneo A, Bradley E, Chunharas S, Atun R, Abbas KM, et al. Rethinking health systems strengthening: key systems thinking tools and strategies for transformational change. Health Policy Plan (2012) 27(Suppl 4):iv54. doi: 10.1093/heapol/czs090
42. de Savigny D, Adam T. Systems thinking for Health Systems Strengthening (2009). Available at: http://apps.who.int/iris/bitstream/handle/10665/44204/9789241563895_eng.pdf;jsessionid=14193F87E7A02F4ABF7F525AB3065FB5?sequence=1.
43. WHO. Ending the neglect to attain the Sustainable Development Goals: a road map for neglected tropical diseases 2021–2030. Geneva (2020). Available at: https://www.who.int/publications/i/item/9789240010352.
44. Arikawa S, Dumazert P, Messou E, Burgos-Soto J, Tiendrebeogo T, Zahui A, et al. Childbearing desire and reproductive behaviors among women living with HIV: A cross-sectional study in Abidjan, Côte d’Ivoire. PloS One (2020) 15(10):e0239859. doi: 10.1371/journal.pone.0239859
45. Nattabi B, Li J, Thompson SC, Orach CG, Earnest J. A systematic review of factors influencing fertility desires and intentions among people living with HIV/AIDS: Implications for policy and service delivery. AIDS Behav (2009) 13(5):949–68. doi: 10.1007/s10461-009-9537-y
46. Burgess S, Kra KW, Allen M, Vandermark J, Turke S. Aspiring to establish a family: Reproductive health among young unmarried women in Abidjan, Côte d’Ivoire. Cult Health Sex (2020) 24(2):210–25. doi: 10.1080/13691058.2020.1826580
Keywords: female genital schistosomiasis, sexual and reproductive health, integration, health system, HIV, health worker capacity, training, health education
Citation: Preston A, Vitolas CT, Kouamin AC, Nadri J, Lavry SL, Dhanani N, Dje N, Toh A, Fleming FM and Meite A (2023) Improved prevention of female genital schistosomiasis: piloting integration of services into the national health system in Côte d’Ivoire. Front. Trop. Dis 4:1308660. doi: 10.3389/fitd.2023.1308660
Received: 06 October 2023; Accepted: 01 December 2023;
Published: 22 December 2023.
Edited by:
Amy S. Sturt, University of London, United KingdomReviewed by:
Laura Dean, Liverpool School of Tropical Medicine, United KingdomMoudachirou Ibikounle, University of Abomey-Calavi, Benin
Copyright © 2023 Preston, Vitolas, Kouamin, Nadri, Lavry, Dhanani, Dje, Toh, Fleming and Meite. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ashley Preston, YS5wcmVzdG9uQHVubGltaXRoZWFsdGgub3Jn
 Ashley Preston
Ashley Preston Carlos Torres Vitolas2
Carlos Torres Vitolas2