- 1Department of Research and Development, Mission to Save the Helpless, Jos, Nigeria
- 2Neglected Tropical Diseases Control Unit, Federal Ministry of Health, Abuja, Nigeria
- 3Parasitology and Epidemiology Unit, Department of Animal and Environmental Biology, Federal University Oye-Ekiti, Oye, Nigeria
- 4Disease Control and Epidemiology Unit, Lagos State Ministry of Health, Ikeja, Nigeria
- 5Sightsavers Country Office, Sightsavers, Kaduna, Nigeria
Background: In this study we summarized the lessons learnt during the first effective mass drug administration (MDA) campaign in one of the most urbanized states in Nigeria. We particularly discuss the implementation approach including associated challenges and future prospects.
Methods: We implemented schistosomiasis MDA with praziquantel in seven endemic districts of the state, using a sub-district/ward-level implementation approach. Upon completion, we conducted desk reviews of field reports and a high-level stakeholder meeting among 95 key personnel involved in the MDA. We reviewed excerpts from the meetings to highlight the strengths, weaknesses, threats and opportunities (SWOT) of the sub-district/ward-level implementation approach. Quantitative data were summarized using basic descriptive statistics, while qualitative data were analyzed to identify emerging themes.
Results: About 1.45 million children between age 5 and 15 were targeted for treatment, and a geographic (100%) and therapeutic coverage of 85.5% was achieved. Therapeutic coverage was optimal (>75%), across all the implementation districts (Range:76.2- 95.3%). Ifako-Ijaiye had the highest therapeutic coverage (95.3%), while Oshodi-Isolo as the least (76.2%). Strategies supporting high coverage includes; (1) adequate delineation of hard-to reach areas and allocation of commensurate resources, (2) improved consultation and microplanning among programmers, (3) addressing traffic congestion on transportation routes, (4) strengthened engagements and collaborations with community gatekeepers, (5) optimizing cash flow to mitigate financial risk, (6) capacity building of field stakeholders and, (7) regular advocacy and sensitization among stakeholders.
Conclusion: This study provides possible directions for implementation of schistosomiasis control by programs and agencies at sub-district/ward-level in a cosmopolitan and urbanized state, like that of Lagos, Nigeria.
1 Background
Schistosomiasis is one of the most common neglected tropical diseases (NTDs) in sub-Saharan Africa (1). The global burden is enormous across 78 countries, with about 206 million cases and 2.5 million disability adjusted life years (2). The most vulnerable population are the school-aged children (SAC) between ages 5-14 years. These children bear the brunt of these chronic infections which further increase their susceptibility to other infections and exacerbated health outcomes (3, 4). Control and elimination for schistosomiasis have been through mass administration (MDA) of praziquantel to SAC in endemic communities (5), with the requirement that endemic countries must consistently treat at least 75% of its at-risk population, to progress towards elimination (5).
Till date, the planning and implementation of MDA occur at implementation units (IUs), also known as the districts, province or local government areas (5). Disease prevalence and other population data generated at the community level are usually aggregated at the IUs, and used to determine the thresholds (cycles) of MDA to be implemented (5, 6). Before now, biannual (twice in a year) MDA is implemented to all SAC in IUs where schistosomiasis prevalence is above 50%, while annual (once in a year) MDA is recommended when prevalence is between 10 and 49.9%, and biennial (once in two years) MDA when prevalence is between 1 and 10% (5). However, recent WHO guidelines on schistosomiasis risk classification recommends annual MDA to all SAC when prevalence is above 50%, biennial MDA to 50% of SAC when the prevalence is between 10 and 49.9% and when the prevalence is between 1 and 10%, it is recommended that all SAC are treated twice during their years primary schooling age i.e., between 5 and 15 years of age (7).
Furthermore, the 2020-2030 NTD elimination road map highlights two major targets, (1) reducing the proportion of moderate and heavy intensity infections for schistosomiasis to <1% in 78 countries, and (2) reducing the number of tablets required during MDA by 50% while increasing domestic support (8; 9). Meeting these elimination targets require adaptation of approaches focused on increasing community participation in endemic settings to obtain consistent and absolute geographic and optimal therapeutic coverage rates (10–13). Moreso, the will to reduce number of tablets for MDA by 50%, requires more precise delineation of hotspots and estimation of treatment and resource needs (6, 14). The current approach of aggregating data at the IUs masks the disease patterns that exist at the community level, and also provide inaccurate estimation of treatment needs, challenges and progress (6, 14). The resultant over/under estimation of medicines, may lead to wastages and poor programme reach. In addition, there may be fatigue in MDA participation in areas that have been erroneously classified as endemic, resulting in increased cost of providing intervention at the expense of other unreached areas (15). The World Health Organization therefore advocates for data disaggregation at the IUs, to the sub-district or ward level during planning and implementation of MDA (16). It is believed that this approach will allow precise estimation of risk, better targeting and allocation of resources to transmission foci where it could be used efficiently and effectively (16).
In Nigeria, the NTD control unit in Lagos State in collaboration with Mission to Save the Helpless (MITOSATH), World Health Organization (WHO) and the Federal Ministry of Health (FMoH) conducted the first MDA for schistosomiasis in 2019 using the recommended sub-district approach, and achieved a therapeutic coverage of 85.8%. In this paper, we summarize the lessons learned during this process, and highlights the challenges and future prospects of implementing a sub-district approach. We believe our findings may be useful to disease control programs and other implementing agencies as they prepare to roll out the sub-district-based MDA strategy for schistosomiasis control, either in an urbanized state like that of Lagos, or elsewhere.
2 Methods
2.1 Study area
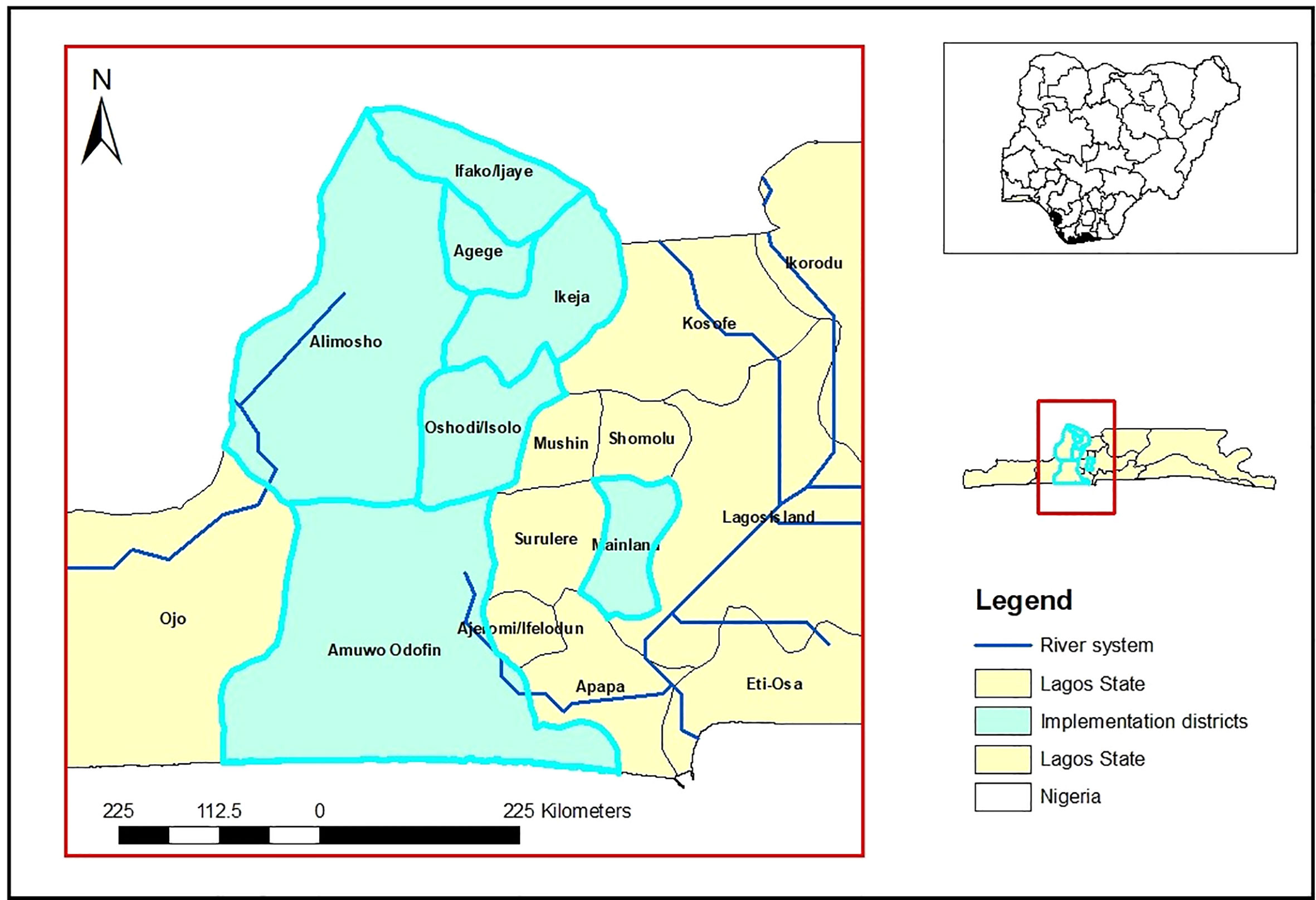
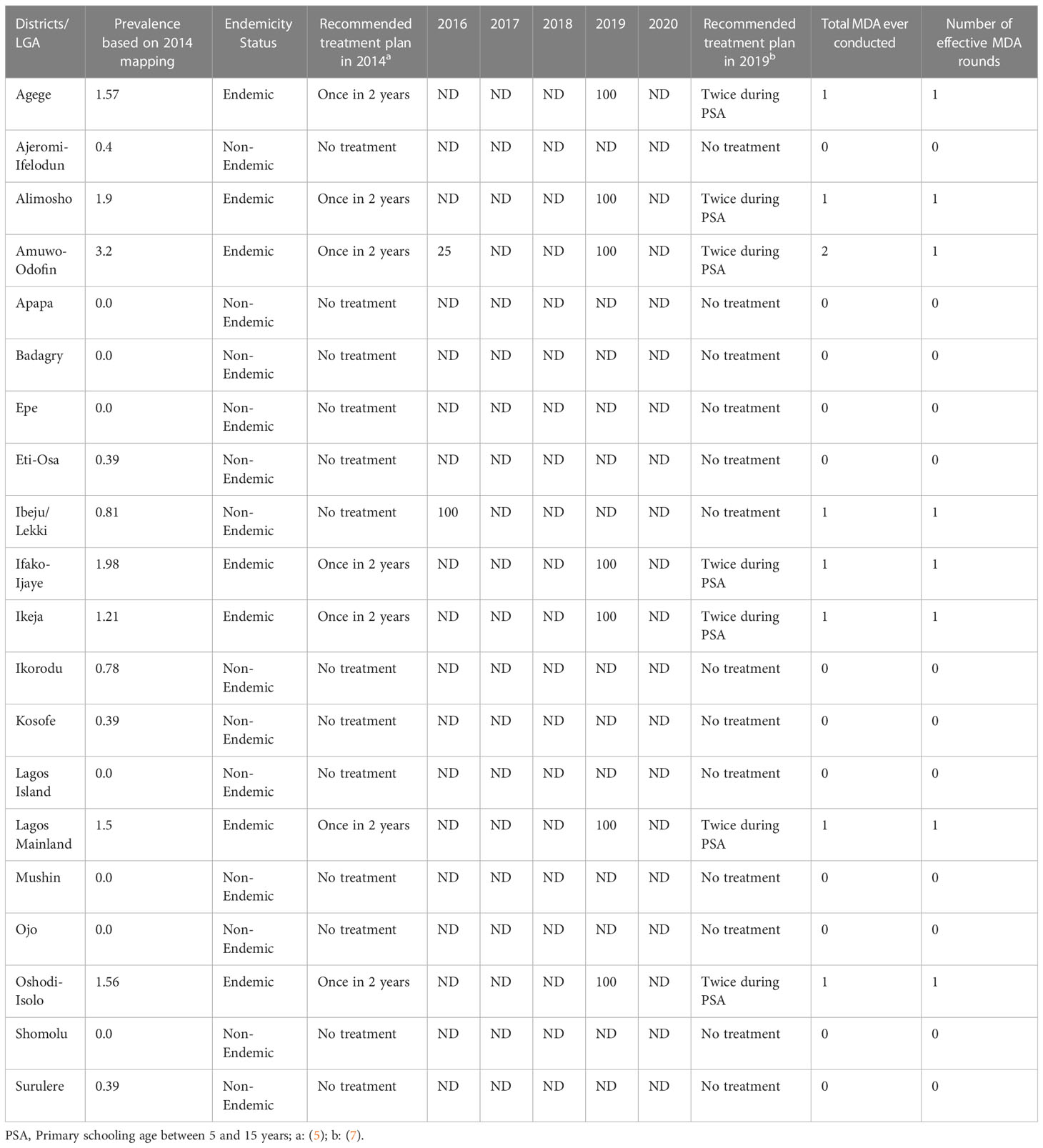
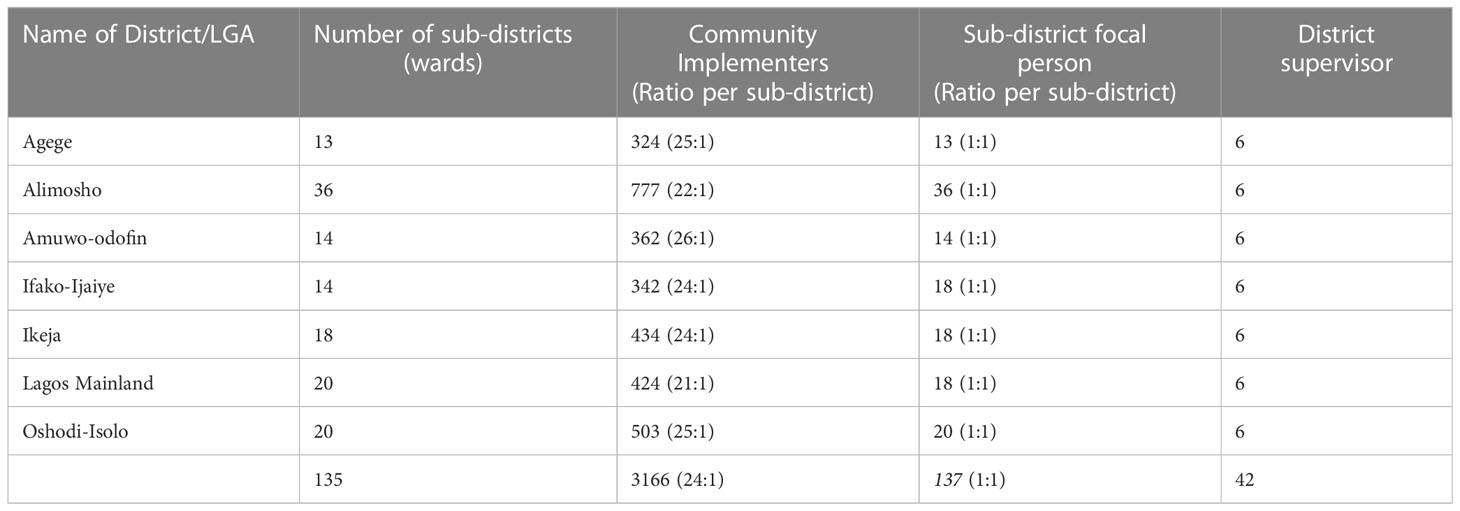
Lagos is the industrial hub and economic capital of Nigeria. It is located in the south western part of Nigeria and bordered to the south by the Atlantic Ocean and the west by the Republic of Benin. Lagos has 20 administrative units (districts) and 377 sub-districts (Figure 1). The city of Lagos covers an immense area, with a total of 1,171.28 square kilometers (452.23 square miles), and harbors a debatable population of over 20 million people (17, 18). It is a cosmopolitan state with a combination of both semi urban and urban settlements. Of the 20 districts in the state, a total of 13 were classified as non-endemic for schistosomiasis, with their prevalence ranging between 0.39% and 3.2% (19). Seven of the districts; Agege, Alimosho, Amuwo-Odofin, Ifako-Ijaye, Ikeja, Lagos Mainland and Oshodi-Isolo were endemic with prevalence values above 1%, and were the focus of the sub-district implementation strategy (Table 1). Until 2019, there was no history of MDA across the endemic districts, except in Amuwo-odofin, with a therapeutic coverage of 25% in 2016 (20).
2.2 Overview of the sub-district implementation strategy
This strategy was implemented across the seven schistosomiasis endemic districts in Lagos between November and December, 2019. Briefly, it involved dis-aggregation of IUs data into already established administrative sub-districts (i.e., ward). This was followed by community listing across the wards, identification of community stakeholders comprising of implementers and focal personnel, and training of stakeholders by experienced district health officers. Prior to implementation, sensitization and advocacy activities were conducted using radio jingles, town announcers and distribution of health educational materials in communities, markets and worship centers. Field implementation of MDA involved door to door administration of praziquantel in combination with some fixed distribution booths. Implementation was conducted over a period of 10 days, including weekends. Upon completion, treatment data were summarized by focal persons in each ward and submitted to district health officers.
2.3 Review of sub-district implementation approach
A 2-day consultation meeting was organized by MITOSATH, in collaboration with the Lagos State NTDs control unit and Federal Ministry of Health on 13th and 14th of September, 2021. A total of 95 delegates involved in the implementation approach participated in the meeting, from Federal Ministry of Health, Lagos State Ministry of Health, MITOSATH, Evidence Action, Sightsavers, Christian Blind Mission (CBM), RTI International and the Media. The meeting was designed to review the strength, weakness, opportunities and threats (SWOT) of the implementation approach, consolidate feedback from stakeholders and, highlight lessons learnt for future applications in other MDA programs. Participants were invited based on their involvements (field implementation, policy directions, funding, amongst others) in NTD control and elimination programme. The desired outcome from the meeting was identified as established evidences on, (1) factors that supported or hindered the sub-district implementation approach, (2) cost-effectiveness of the approach, and (3) possible pathways for future applications of the approach.
2.4 Data management and reporting
Foremost, desk review of technical reports and field notes were performed, and summarized into texts and charts as appropriate. Where applicable, additional data were sourced from the district/sub-district NTD focal persons to support emerging themes. Secondly, discussions during the consultation meetings were audio-recorded following the consents of the delegates. The daily rapporteur reports and communique of the meeting were harvested and summarized to highlight the opinions and agreements from the meeting. All quantitative data were summarized using basic descriptive statistics such as frequencies and percentages, while qualitative data were analyzed for themes and the most emerging theme was considered to be a more important variable.
3 Lessons learnt and recommendations
3.1 Coverage estimates
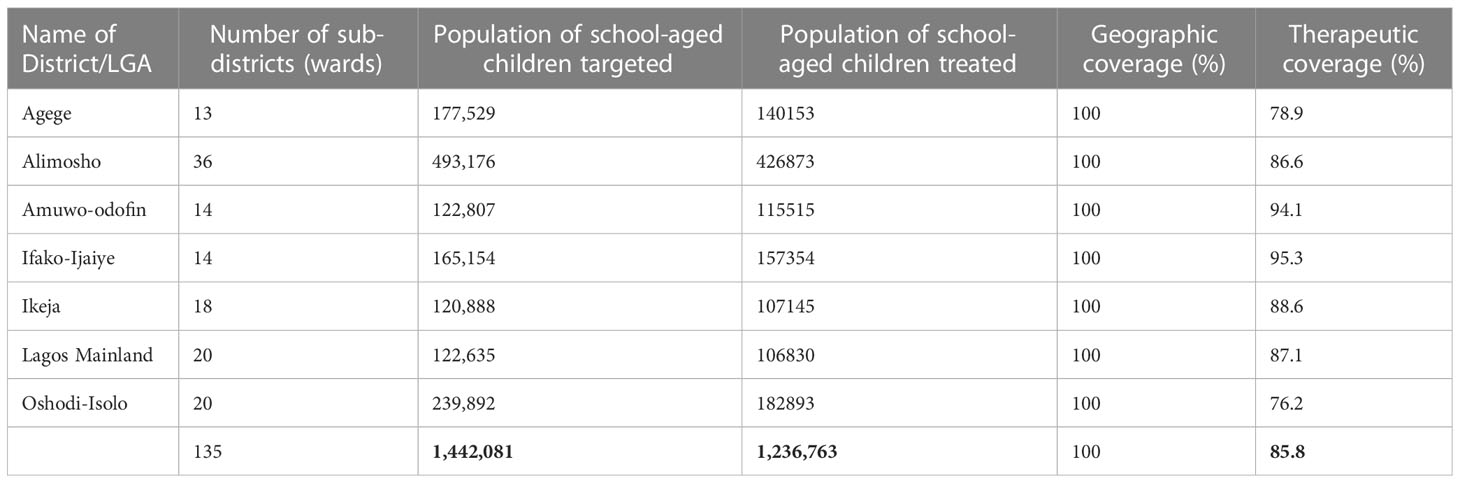
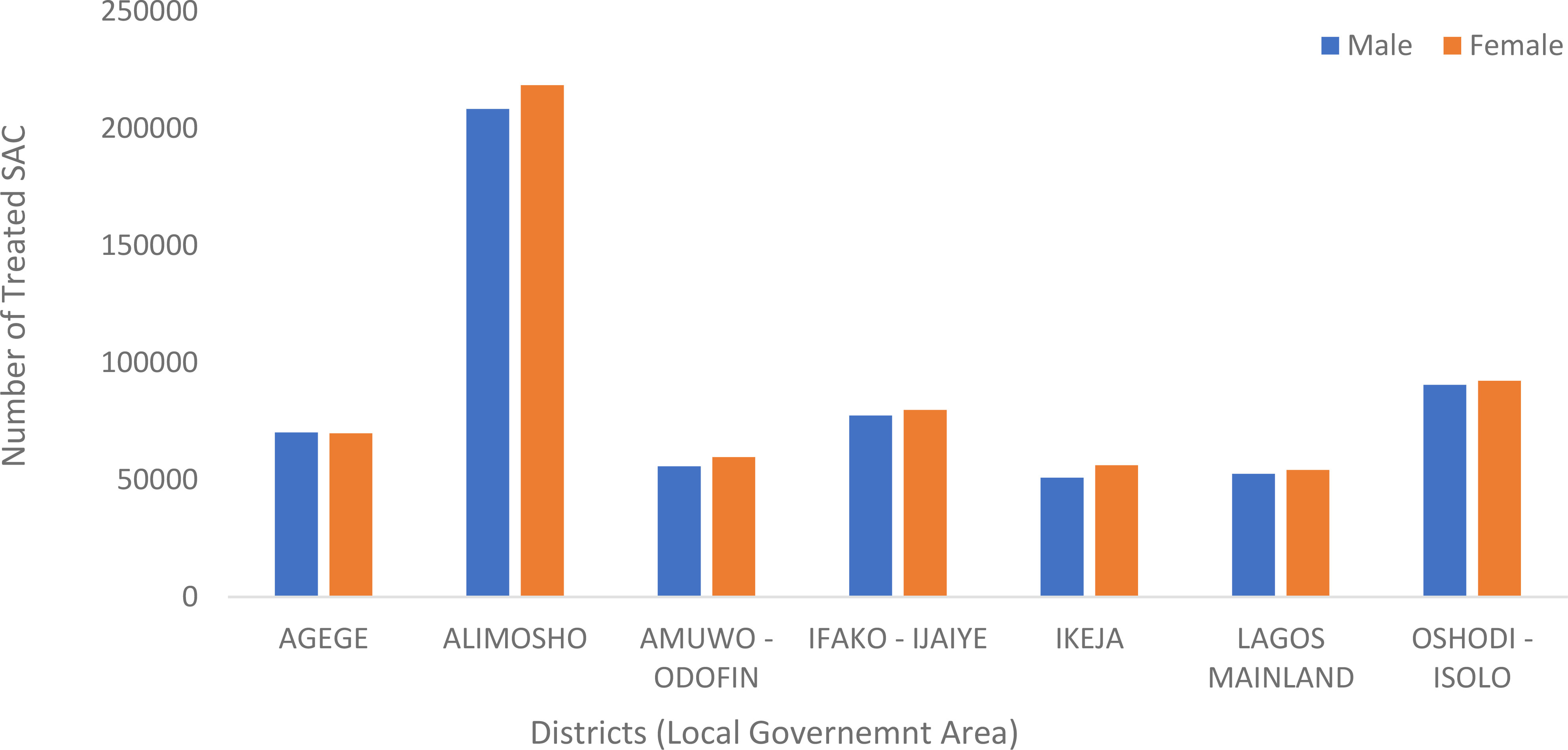
A total of 1.24 million (85.8%) children million were treated in the state. Therapeutic coverage was optimal across all the implementation districts (Range: 76.2% - 95.3%), and surpassed the 75% national threshold. Ifako-Ijaiye had the highest therapeutic coverage (95.3%), while Oshodi-Isolo as the least (76.2%). A geographic coverage of 100% was also recorded across the implementation districts (Table 2). By gender, 51% of those treated were females (Figure 2), however, there was no significant difference in the proportions of those treated by gender (p >0.05)
3.2 Microplanning
The heterogeneity of urban areas requires attention during MDA, and one major step is to establish smaller implementation units, a concept described as micro-targeting (21). The process of micro-targeting requires the establishment of who should deliver treatment, how many implementers would be required and how can these implementers be adequately motivated (21). Elsewhere, MDAs are usually planned using aggregated census data at the district level (22). However, during this activity, microplanning was done using disaggregated 2018 census data which allowed formation of smaller clusters of communities based on geographical proximities, and a more justified approach of allocating implementers. This strategy improved planning, and the estimation of medicines required for MDA (16).
In summary, a total of 135 wards were identified across the seven endemic districts during the microplanning exercise, and an average of 24 trained community implementers were allocated to represent each sub-district. (Table 3). The sub-district approach therefore allowed recruitment of more field implementers, in comparison with usual MDA programs in rural settings (23). For instance, MDA implemented in neighboring states (Ekiti and Ondo) engages one trained implementer per school to treat hundreds of children (24). Heavy workload on implementers have been reported to have negative influence on health worker’s motivation and performance, and should be addressed (25, 26). The increase in number of implementers during this activity therefore contributed positively to health workers motivation through reduce workload (27). Furthermore, in previous MDAs, allocation of supervisors to communities were done at the discretion of district supervisors (24). The allocation of one focal personnel per ward, and six supervisors per district, therefore allowed more precise pairing of proximal communities per ward focal person, thus ensuring more accountability and data management. Below are some of the excerpts from the stakeholders meeting;
“……. Ward focals were fully on ground to carry out their task in other to meet their targets…”- State NTD officer 1
“MAM for control schistosomiasis in Ifako-Ijaye LGA was a successful one, both the SNTD the focal persons in their various wards were active to make sure that the goals and objectives of the MAM were achieved-”- State NTD officer 2
3.3 Capacity building
One major challenge in the implementation of MDA in urbanized settings is the poor acceptance of non-health workers, or drug-distributors that were perceived to be less-qualified. This has been reported in Santo Domingo (28), and addressed by recruiting people with higher levels of education as drug distributors. In Nigeria, MDAs are largely implemented in rural areas, and the problems of poor acceptance of non-health workers are not common. However, considering the cosmopolitan nature of Lagos state, and its very low rurality index (29), a more refined strategy of recruiting and strengthening capacity of drug distributors became important.
To address this concern, we recruited implementers who are literate, had participated in other health programmes, and are familiar with the local context of the state. The recruitment process was easy considering that Lagos is the major economic hub of the country, and has a considerable high number of literate persons compared to other states in Nigeria (30, 31). The capacity building process of recruited volunteers were more intensive, with emphasis on MDA process, and other aspects of record keeping, medicine inventory and supervision. Implementers were also trained on how to report severe adverse events (SAEs), a major inclusion in the capacity development plan. The impact of real or rumored adverse event on urban MDA have been extensively describe by Adams and colleagues (2018), and needs to be controlled. The responsibilities of each implementer were then reinforced, with specific deliverables to monitor performance. During the stakeholders meeting, participants affirmed that the literacy status and competency of the implementers contributed to the success of the activity.
“The NTD activity was a huge success in Agege. Good understanding and team work was created among the ward focal persons. Through the intensive supervision and tutoring of the FMoH person [Name withheld], we were able to build the best team of ward focal persons, implementers, and LGA team” - State NTD officer 3
“Availability of trainable and ready to learn team from State level to community level…”- Participant 1, Stakeholder Meeting
3.4 Community sensitization and advocacy
Communication is one of the most important tools in MDA implementation. Messages about NTDs, associated morbidities, how NTDs can be prevented, why an MDA is being undertaken, information on drug safety and possible adverse effects, timing and location of MDA and overall benefits of the MDA needs to be communicated during sensitization and advocacy visits (21, 32). Communication becomes particularly important in urban areas as NTDs are perceived to be uncommon and not easily recognized as threats (21). There are reports from Nigeria about the poor penetration of NTD promotional activities particularly among elitist populations (12, 13). More than 80% attendees in an NTD programme do not know anyone who has benefitted from MDA and about 70% have not received any NTD health educational messages before (13). This situation particularly makes acceptance of MDA difficult in urban areas.
These experiences shaped the sensitization and advocacy plans during the sub-district implementation approach in Lagos State. Foremost, the Lagos State Scientific Advisory Committee on NTDs (LA-SACON) was inaugurated, and this allowed seamless sensitization of high-level policy makers and stakeholders in government. Prior to community sensitization, pre-activity enquiries were made on the list of effective community networks in the implementation areas. This was followed by series of dialogues with traditional leaders, community-based organization and religious societies in front-line communities across all the districts. Sensitization were made using educational materials designed in different languages on schistosomiasis. These actions were reinforced with community-wide campaigns leveraging on the resources of other health programme in the district, for example the Maternal Health and Child (MNCH) week programme. Furthermore, flag-off activities were carried out in some districts to support community dialogues. However, engagements with critical stakeholders happened shortly before and after implementation. It is therefore important to activate consistent engagement and communication with stakeholders throughout the year and not only during MDA (13). In addition, high powered advocacy visits to stakeholders at the ministries of health and education are needed to create ownership and strengthened partnership for MDA in the state.
3.5 Logistics
Accurate projections of material and human resources are essential when planning urban MDAs considering the high population density and diverse demography. As such, the need to achieve absolute geographic coverage across the implementation districts was prioritized. One major perceived challenge was traffic congestion, which consumes about 3 billion working hours annually in Lagos, with a very high risk of negatively impacting MDA coverage (33). Hence, we optimized our transportation strategy by allocating more budgetary costs, which allowed implementers to utilize alternative transport medium such as private bike and taxis within the cities whose roads are always congested. In some hard-to-reach riverine areas, the team travelled on boats. Some of the participants commented on the tedious nature of implementation of MDA in the state.
“Amuwo-odofin has 14 wards spread across the Riverine areas. Simultaneously treatment commenced and ended successfully without any loss of life or pronounced casualties.” - Participant 2 Stakeholder Meeting
Within the complex city of Lagos, there are a number of hard-to-reach areas, and other residential areas with restricted access. We therefore employed a mix of strategies to optimize coverage. Foremost, we approached and requested support from education unions regulating the activities of privately-owned schools located in areas with restricted areas such as military zones, para-military and top-class residential estates. Following this, we reinforced our visibility, by investing in the production and use of identity badges, official letter of intent, and customized aprons for non-health workers. This increased the acceptance of implementers in the communities. This strategy has also been used to support urban MDA implementation in Santa Domingo (28).
Furthermore, in these restricted areas, there are lower chances of performing repeated visits during MDA, as such we instituted a centralized mode of treatment using a fixed booth. Medicines were properly managed to avoid wastages and returns were tracked using an inventory form. We also created a daily feedback reporting loop via WhatsApp messenger platform across all levels of implementation. The mix of distribution strategies is not uncommon during urban MDA implementation, and has been reported in Mali (34) and Samoa (35). Across these settings, implementers employed a mix of door-door approach, with distributions at private and public schools, fixed post such as markets, major intersections, in front of chief of residence, government offices, and churches.
3.6 Budget management
Given that the sub-district implementation strategy was being piloted in Nigeria for the first time, there was uncertainty regarding the specific costs associated with its implementation. The budgeting approach differed significantly from previous MDAs due to factors such as a larger number of implementers, the urbanized nature of the state, and its extensive geographical area. In previous MDAs, allowances were disbursed through cash transfers, where the recipient would confirm the receipt of funds by signing a payment voucher. However, considering the risk associated with travelling around with funds in Lagos, the strategy was optimized to a cashless mode using online transfers. As a result, a total of 5,182 electronic transactions were made during this activity. This project therefore stands out as the first MDA in Nigeria to expand the use of electronic payments to community health implementers. Detailed feedback mechanism including daily reporting channels and mid-activity review meeting were instituted. This allowed identification of challenges encountered during the payment process. In cases where implementers did not meet performance expectations, they were closely monitored, and if necessary, replaced with another participant, resulting in discontinued payments.
4 Challenges and recommendations
The sub-district MDA implementation strategy faced a couple of challenges which should be carefully considered when future programmes are planned in Lagos. Firstly, due to the urbanized nature of the state, there were significant disturbances which ranged from traffic congestion to security threats from the activities of street thugs known as “Area Boys”. In addition, poor access and coverage were also experienced in military zones and classified estates. There were also concerns regarding the logistics for treatment in hard-to-reach communities. Clashes with other health programme within the district also hindered continuous implementation, as MDA was completely new to the health workers.
It is therefore important to implement strategies to address these challenges when future sub-district implementation programme is been planned, especially in an urbanized areas such as that of Lagos State. Some of the strategies employed in the present activity include; (1) prior delineation of hard to reach areas and appropriate allocation of commensurate resources, (2) improved consultation and microplanning to prevent undue clash of MDA programme with other programmes and also promote co-implementation where applicable, (3) increasing transportation budget to allow other flexible means of transportation that beats traffic congestion, (4) strengthened engagements and collaborations with authorities of areas identified to be with restricted access, (5) deploying cashless mode of payment of implements to mitigate financial risk, (6) capacity building of health workers on SAEs and management strategies and, (7) deployment of regular advocacy and sensitization to stakeholders across all implementation levels to further promote ownership, resource drive motivation, funding and awareness.
5 Conclusion
In this paper, we summarized the lessons learnt during the implementation of MDA for schistosomiasis control using sub-district implementation approach. We highlighted the perceptions of high-level NTD stakeholders on the challenges encountered and future prospects of such implementation approach. We believe that this report would provide guidance to disease control programs and other implementing agencies as they prepare to roll out the sub-district MDA approach for schistosomiasis control.
Author contributions
FO conceptualized the study. ON, HM, IA, LJ, AJM, OJO, SI, PA, IN, IJ, EA participated in deliberation and implementation activities. HM and AJM collected all data. HM performed all statistical analysis and data summaries. HM prepared the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The implementation of these activities was funded by ASCEND/Sightsavers through Mission to Save the Helpless. The funding did not cover this publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hotez PJ, Kamath A. Neglected tropical diseases in sub-saharan Africa: review of their prevalence, distribution, and disease burden. PloS Negl Trop Dis (2009) 3(8):e412. doi: 10.1371/journal.pntd.0000412
2. World Health Organization (WHO). Schistosomiasis. fact sheet (2022). Available at: https://www.who.int/news-room/fact-sheets/detail/schistosomiasis (Accessed 3 February 2022).
3. Grantham-McGregor S, Ani C. A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr (2001) 131:649S–68S. doi: 10.1093/jn/131.2.649S
4. Ezeamama AE, Friedman JF, Acosta LP, Bellinger DC, Langdon GC, Manalo DL, et al. Helminth infection and cognitive impairment among Filipino children. Am J Trop Med Hygiene. (2005) 72:540–8. doi: 10.4269/ajtmh.2005.72.540
5. World Health Organization (WHO). Helminth control in school-age children: a guide for managers of control programmes (2011). Available at: https://www.who.int/neglected_diseases/resources/9789241548267/en/ (Accessed 15 April 2021).
6. Mogaji HO, Dedeke GA, Bada BS, Bankole S, Adeniji A, Fagbenro MT, et al. Distribution of ascariasis, trichuriasis and hookworm infections in ogun state, southwestern Nigeria. PloS One (2020) 15(6):e0233423. doi: 10.1371/journal.pone.0233423
7. ESPEN. (2022). Available at: https://espen.afro.who.int/.
8. Montresor A, Mupfasoni D, Mikhailov A, Mwinzi P, Lucianez A, Jamsheed M D, Mikhailov A, Mwinzi P, Lucianez A, Jamsheed M, et al. The global progress of soil-transmitted helminthiases control in 2020 and world health organization targets for 2030. PloS Negl Trop Dis (2020) 14(8):e0008505. doi: 10.1371/journal.pntd.0008505
9. World Health Organization. Ending the neglect to attain the sustainable development goals: a road map for neglected tropical diseases 2021–2030 Vol. 2020. . Geneva: World Health Organization (2020).
10. Mathieu E, Direny AN, de RMB, Streit TG, Addiss DG, Lammie PJ. Participation in three consecutive mass drug administrations in leogane, Haiti. Trop Med Int Health (2006) 11:862–8. doi: 10.1111/j.1365-3156.2006.01626.x
11. El-Setouhy M, Abd Elaziz KM, Helmy H, Farid HA, Kamal HA, Ramzy RM, et al. The effect of compliance on the impact of mass drug administration for elimination of lymphatic filariasis in Egypt. Am J Trop Med Hyg (2007) 77:1069–73. doi: 10.4269/ajtmh.2007.77.1069
12. Olamiju OJ, Olamiju FO, Adeniran AA, Mba IC, Ukwunna CC, Okoronkwo C, et al. Public awareness and knowledge of neglected tropical diseases (NTDs) control activities in Abuja, Nigeria. PloS Negl Trop Dis (2014) 8(9):e3209. doi: 10.1371/journal.pntd.0003209
13. Mogaji HO, Odoh IM, Iyeh CI, Adeniran AA, Oyedeji SI, Okoh HI, et al. Attendee awareness about preventive chemotheraphy neglected tropical diseases (PC-NTD) control during the first world neglected tropical diseases day in ekiti state, Nigeria. PloS Negl Trop Dis (2021) 15(3):e0009315. doi: 10.1371/journal.pntd.0009315
14. Hürlimann E, Schur N, Boutsika K, Stensgaard A-S, Laserna de Himpsl M, Ziegelbauer K, et al. Toward an open-access global database for mapping, control, and surveillance of neglected tropical diseases. PloS Negl Trop Dis (2011) 5(12):e1404. doi: 10.1371/journal.pntd.0001404
15. Ross AGP, Chau TN, Inobaya MT, Olveda RM, Li Y, Harn DA. A new global strategy for the elimination of schistosomiasis. Int J Infect Dis. (2017) 54:130–7. doi: 10.1016/j.ijid.2016.09.023
16. Global Schistosomiasis Alliance (GSA). Accelerating progress for schistosomiasis conttrol and elimination post-2020 (2019). Available at: https://www.eliminateschisto.org/sites/gsa/files/content/attachments/2019-06-26/Final_GSA_Accelerating%20Progress%20For%20Schistosomiasis%20Control%20and%20Elimination%20Post%202020%20Meeting%20Report_0.pdf.
17. Lagos State Government (LASG). About Lagos (2020). Available at: https://lagosstate.gov.ng/about-lagos/.
18. Wikipedia. Lagos State (2020). Available at: https://en.wikipedia.org/wiki/Lagos_State.
19. Federal Ministry of Health (FMoH). Epidemiological mapping survey report in Lagos state. Nigeria: Federal Ministry of Health (2014).
20. Federal Ministry of Health (FMoH). Mass drug administration campaign report in amuwo-odofin. Nigeria: Lagos State (2016).
21. Adams AM, Vuckovic M, Birch E, Brant TA, Bialek S, Yoon D, et al. Eliminating neglected tropical diseases in urban areas: a review of challenges, strategies and research directions for successful mass drug administration. Trop Med Infect Dis (2018) 3(4):122. doi: 10.3390/tropicalmed3040122
22. Kamara W, Zoerhoff KL, Toubali EH, Hodges MH, Bisanzio D, Chowdhury D, et al. Are census data accurate for estimating coverage of a lymphatic filariasis MDA campaign? results of a survey in Sierra Leone. PloS One (2019) 14(12):e0224422. doi: 10.1371/journal.pone.0224422
23. Macfarlane CL, Dean L, Thomson R, Garner P. Community drug distributors for mass drug administration in neglected tropical disease programmes: systematic review and analysis of policy documents. J Global Health (2019) 9(2):20414. doi: 10.7189/jogh.09.020414
24. Mission to Save the Helpless (MITOSATH). Mass drug administration campaign report in ekiti and ondo states. Nigeria: Mission To Save The Helpless (2019).
25. Njomo DW, Amuyunzu-nyamongo M, Magambo JK, Njenga SM. The role of personal opinions and experiences in compliance with mass drug administration for lymphatic filariasis elimination in Kenya. PloS One (2012) 7(11):1–7. doi: 10.1371/journal.pone.0048395
26. Rilkoff H, Tukahebwa EM, Fleming FM, Leslie J, Cole DC. Exploring gender dimensions of treatment programmes for neglected tropical diseases in Uganda. PloS Negl Trop Dis (2013) 7(7):1–9. doi: 10.1371/journal.pntd.0002312
27. Inegbedion H, Inegbedion E, Peter A, Harry L. Perception of workload balance and employee job satisfaction in work organisations. Heliyon (2020) 6(1):e03160. doi: 10.1016/j.heliyon.2020.e03160
28. Gonzales M, Baker MC, Celestino A, Santa Morillo D, Chambliss A, Adams S, et al. How lymphatic filariasis was eliminated from an urban poor setting in Santo Domingo, Dominican republic. Int Health (2019) 11(2):108–18. doi: 10.1093/inthealth/ihy059
29. Madu IA. The structure and pattern of rurality in Nigeria. GeoJournal (2010) 75:175–84. doi: 10.1007/s10708-009-9282-9
30. UNESCO. (2012). Available at: http://www.unesco.org/new/fileadmin/MULTIMEDIA/HQ/ED/pdf/Nigeria.pdf.
31. Kuyinu YA, Femi-Adebayo TT, Adebayo BI, Abdurraheem-Salami I, Odusanya OO. Health literacy: prevalence and determinants in Lagos state, Nigeria. PloS One (2020) 15(8):e0237813. doi: 10.1371/journal.pone.0237813
32. Krentel A, Fischer PU, Weil GJA. Review of factors that influence individual compliance with mass drug administration for elimination of lymphatic filariasis. PloS Negl Trop Dis (2013) 7:e2447. doi: 10.1371/journal.pntd.0002447
33. Economic Intelligence Unit (EIU). Ministry of economic planning & budget working paper series no 2 – July 2013 the socio-economic costs of traffic congestion in Lagos (2013). Available at: http://mepb.lagosstate.gov.ng/wp-content/uploads/sites/29/2017/01/EIU-Working-Paper-2-Draft-2-Traffic-Congestion.pdf.
34. Dembele M. The ingredients of a successful MDA approach in Bamako, Mali. In: Proceedings of the 2017 COR-NTD meeting, vol. 4. Baltimore, MD, USA: Coalition for Operational Research on Neglected Tropical Diseases (COR-NTDs) (2017).
Keywords: schistosomiasis, praziquantel, urban, elimination, Lagos, Nigeria, sub-district level implementation
Citation: Olamiju FO, Nebe O, Mogaji H, Abdus-Salam I, Jenrola L, Marcus AJ, Olamiju OJ, Isiyaku S, Amodu-Agbi P, Nwoye I, Achu I and Abah E (2023) The first mass drug administration campaign for schistosomiasis control in Lagos, Nigeria: lessons for future control programs. Front. Trop. Dis 4:1094320. doi: 10.3389/fitd.2023.1094320
Received: 10 November 2022; Accepted: 01 June 2023;
Published: 29 June 2023.
Edited by:
Yaobi Zhang, Helen Keller International, United StatesReviewed by:
Emmanuel Abraham Mpolya, Nelson Mandela African Institution of Science and Technology, TanzaniaClement Ameh Yaro, University of Uyo, Nigeria
Copyright © 2023 Olamiju, Nebe, Mogaji, Abdus-Salam, Jenrola, Marcus, Olamiju, Isiyaku, Amodu-Agbi, Nwoye, Achu and Abah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hammed Mogaji, bW9nYWppaGFtbWVkQGdtYWlsLmNvbQ==
 Francisca O. Olamiju1
Francisca O. Olamiju1 Hammed Mogaji
Hammed Mogaji Ijeoma Achu
Ijeoma Achu