- 1National Institute for Medical Research, Tanga Centre, Tanga, Tanzania
- 2National Institute for Medical Research, Headquarters, Dar es Salaam, Tanzania
- 3Global Health Institute, University of Antwerp, Antwerp, Belgium
Introduction: Despite over 20 years of community-directed treatment with ivermectin (CDTI) in Mahenge area in Tanzania, the prevalence of onchocerciasis has remained high (over 40% in children 6-10 years using antibody testing and 49% using skinsnips in adults). The area has one of the highest prevalence of epilepsy, exceeding 3.5% in some of rural villages.
Methods: Between June and July 2019, in four rural villages using qualitative methods, we assessed factors potentially associated with the persistence of high Onchocerca volvulus transmission.
Results: Eleven focus group discussions were organized with persons with epilepsy and their caretakers, community resource persons, and community drug distributors (CDDs), and two in-depth interviews with district programme coordinators of neglected tropical diseases (NTD). Factors considered being responsible for the persistence of onchocerciasis transmission included not taking ivermectin during CDTI for fear of adverse reactions such as itching, swelling and misconception that the drug causes infertility. Challenges for high CDTI coverage included, long walking distance by CDDs to deliver drugs to households, persons being away for farming, low awareness of the disease including the association between onchocerciasis and epilepsy and limited supervision by the NTD coordinators.
Conclusion: Ivermectin uptake in Mahenge should be optimised by continuous advocacy about the importance of taking ivermectin to prevent onchocerciasisassociated morbidity and by improving supervision during CDTI.
1 Introduction
Onchocerciasis, commonly known as river blindness, is a neglected tropical disease (NTD) caused by the nematode worm Onchocerca volvulus transmitted through a bite of an infective blackfly of the genus Simulium (1–3). Onchocerciasis is known to affect the skin and to cause blindness if left untreated. An estimated 20.9 million people are infected globally, of whom 99% reside in sub-Saharan Africa (3, 4). The World Health Organization (WHO) targeted onchocerciasis for elimination by 2030 using a community-directed treatment with ivermectin (CDTI) strategy (5). For more than 20 years, CDTI has been the global cornerstone strategy for onchocerciasis control and elimination (2). Due to the former Onchocerciasis Control Programme in West Africa (OCP), the African Programme for Onchocerciasis Control (APOC), and the current Expanded Special Project for Elimination of NTD (ESPEN), onchocerciasis is no longer a public health problem in many onchocerciasis endemic areas in Africa (2, 5–7).
In Tanzania, the disease is endemic in Mahenge, in the Ulanga district of the Morogoro region, particularly in rural villages (1, 8–10) where a high prevalence of epilepsy, including nodding syndrome, has been reported (11–14). House-to-house surveys in these rural villages showed that 77.9% of persons with epilepsy met the criteria of onchocerciasis-associated epilepsy (13).
Growing epidemiological evidence suggests a strong association between onchocerciasis and epilepsy, including nodding syndrome (15–18). In January 2017, the prevalence of onchocerciasis antibodies among children aged 6-10 years in some remote rural villages in Mahenge was over 40%, despite more than 20 years of ivermectin distribution (12). Moreover, a study in 2019 among individuals aged six to 83 years in these rural villages documented a skin snip positivity rate of 49% before ivermectin distribution (19). Three months after ivermectin intake the skin snip positivity rate decreased to 17.8% (19).
Sub-optimal geographical and therapeutic coverage of CDTI could be among the factors contributing to the persistent high prevalence of onchocerciasis and epilepsy in Mahenge (12, 19). In order to reach the onchocerciasis elimination goal, it is important to identify factors that may negatively influence the performance of a CDTI programme. Therefore, we assessed factors associated with persistence of high transmission of onchocerciasis using qualitative methods in four rural villages in the Mahenge area.
2 Materials and methods
2.1 Study design and participants
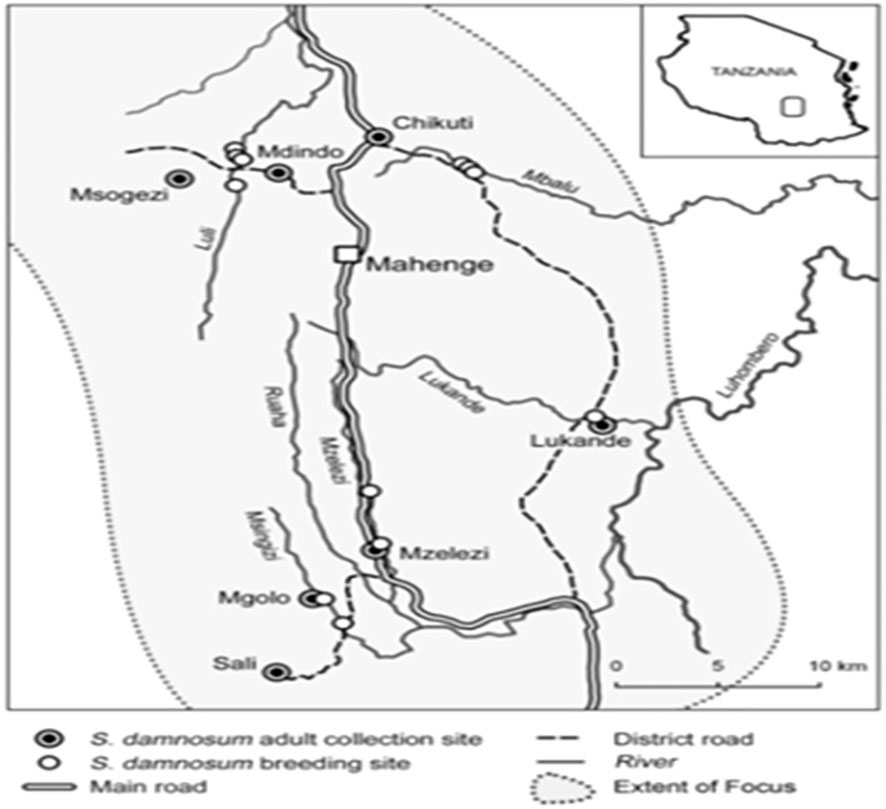
This qualitative study was conducted between June and July 2019 in four villages (Mdindo, Msogezi, Mzelezi and Sali) in Mahenge (Figure 1). Details of the study have been explained elsewhere (20) and this included 11 focus group discussions (FGDs) and two in-depth interviews (IDIs). We stopped including focus groups when no additional new data were being found. The purposeful sampling design was used to select persons with epilepsy (PWE) aged >18 years capable of giving informed consent, the parents/caretakers of PWE, community resource persons (CORPs) and community drug distributors (CDDs) to participate in FGDs. The two IDIs were carried out with the NTD programme coordinators, one been at the division and the other at the district level. Participants were excluded if they were away from the study area during the interview period or if they were sick or unwilling to participate in the study.
2.2 Study settings
The study was conducted in four rural villages in Mahenge: Mdindo Msogezi, Mzelezi and Sali (Figure 1).
Epidemiological surveys between 2017 and 2019 showed a high prevalence of epilepsy in these villages. The surveys also suggested a high level of ongoing onchocerciasis transmission based on a high O. volvulus IgG4 seroprevalence among children aged 6-10 years tested by the Ov16 rapid card test. In particular, 21.1% O. volvulus seroprevalence in Mzelezi, 35.8% in Sali, 38% in Mdindo and 42% in Msogezi village (12, 13). A recent skin snip survey in Mdindo and Msogezi villages found an alarming overall prevalence of microfilaria positivity of 49%, while that of children aged 6 to 10 years was 41.7% (19). In 2019 following our findings (10), the NTDC programme introduced biannual CDTI in the Mahenge area to accelerate the control of onchocerciasis transmission.
2.3 Data collection methods
Focus group discussions and IDIs were conducted to provide in-depth insights into the barriers to onchocerciasis elimination despite over 20 years of CDTI in the Mahenge area. Eleven FGDs were conducted in the four villages which involved the following groups: 1) PWE; 2) parents/guardians of PWE; 3) CDDs; and 4) CORPs (Table 1). As the villages Mdindo and Msogezi are located in the same geographical area, they were merged and one FGD was conducted by each of PWE, CDDs and CORPs. In Msogezi village, the PWE group had a mix of males and females. Each group comprised of 8 - 12 participants, with male and female participants in separate or mixed. The venues for the FGDs were chosen in consultation with the local village leaders in each village. Prior to the discussion, the importance of participating in the study was explained. The FGDs were conducted by experienced moderators in a ‘round table’ manner with numbering of participants in chronological order. The FGDs lasted for 45 to 60 minutes. Each IDI took 30 to 45 minutes and was conducted in a convenient setting for the NTD programme coordinators. Interview guides with open-ended questions were used to collect data. Interviews were conducted in Kiswahili language, the most widely spoken language in Tanzania and audio-recorded in addition to taking notes with permission from the participant(s).
Data collected in FGDs and IDIs included the knowledge, perceptions and beliefs about: 1) onchocerciasis; 2) cause and prevention of the onchocerciasis; 3) association between onchocerciasis and epilepsy; 4) awareness about the role of CDTI for onchocerciasis elimination; and 5) challenges during the mass distribution of ivermectin.
2.4 Data processing and analysis
Interviews were conducted in Kiswahili language. The audio-recorded interviews, with permission from the participant(s), were verbatim transcribed by the research team and then translated into English for analysis. Data were analysed manually using content analysis. Classification and analysis of the data were independently done by the two moderators to enhance the credibility of the categorisation, deepen insights and ensure that findings reflected the research context. Coding was developed based on the predefined objectives of the study and elaborated by a preliminary review of the data to understand the narratives portrayed by participants. Inductive coding was used to identify sub-themes within each of the key themes.
3 Results
3.1 Demographic characteristics of FGDs and IDIs participants
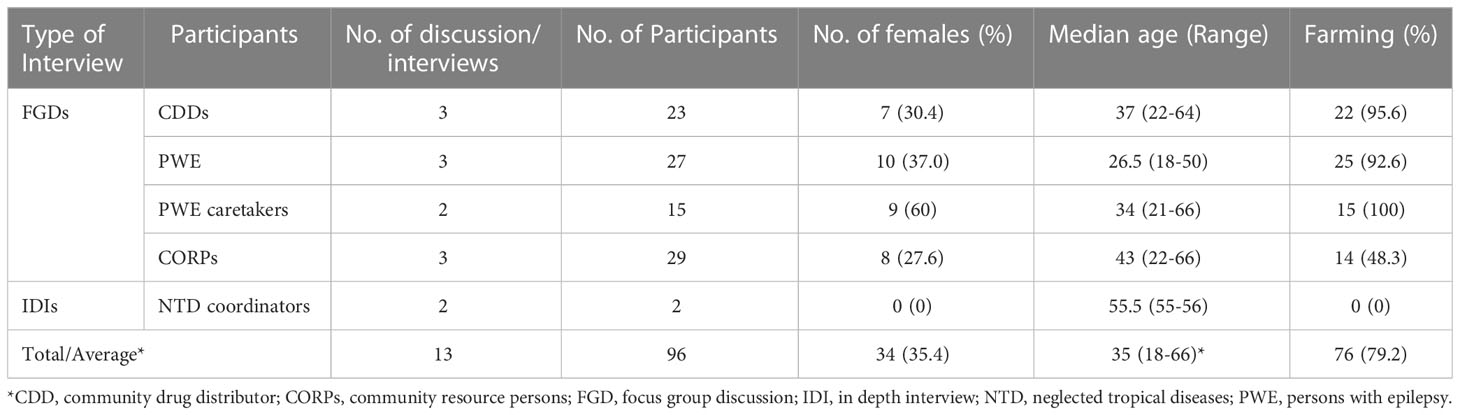
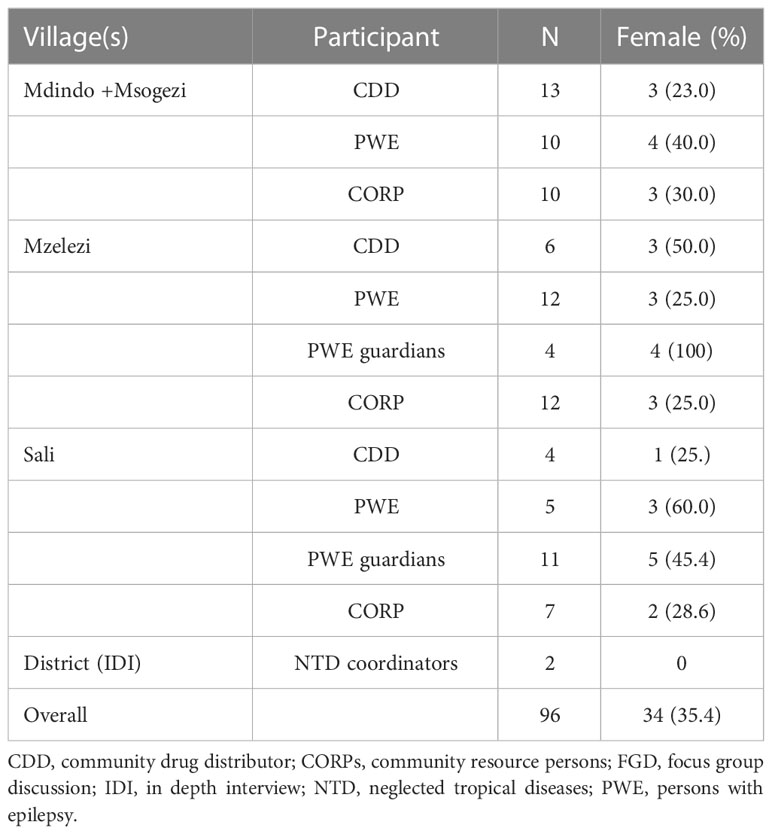
A total of 96 individuals (94 in FGDs) from four villages participated in this study, which involved 13 interviews: 11 FGDs and two IDIs (Tables 1A, 1B).
Most PWE were younger than participants of other groups, and their overall median age was 26.5 years (IQR: 18-50). The majority (79.2%) of study participants were involved in farming activities, with CORPs having the lowest proportion (48.3%) of individuals involved in farming. Other categories in the CORPs group included traditional healers (13.8%), public employees (13.8%) and religious leaders 10.3%. Females represented 35.4% of all discussants. Most PWE had schooling up to or below standard three, while other groups mainly had attained standard seven or above (Figure 2).
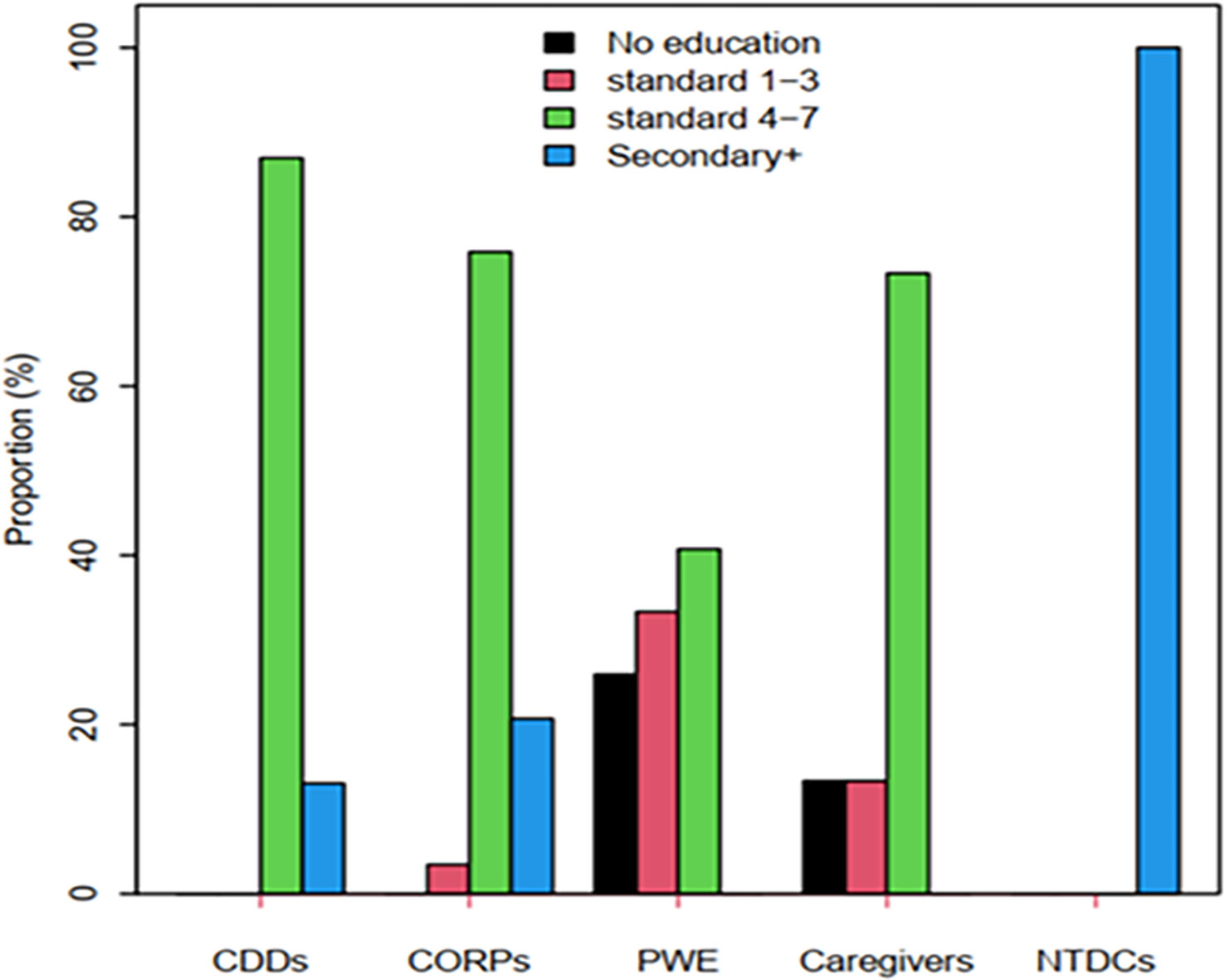
Figure 2 Education levels of different FGDs and IDIs participants. CDDs, community drug distributors; CORPs, community resource persons; NTDCs, NTD coordinators; PWE, persons with epilepsy.
3.2 Knowledge, perceptions and beliefs about onchocerciasis
3.2.1 General knowledge and disease burden
Onchocerciasis was known by all participants of the FGDs but described using different local terminologies. The disease was referred to mainly by its skin manifestations. All the participants used the term “filaria”, the name used to describe the disease during CDTI campaigns. Other terminologies mentioned were itching skin, dry skin and spotted pigmentation of the skin, especially of the legs. Such terminologies were locally referred to as “ukurutu/mkita” (itching and dry skin) “lung’ang’a” (leopard skin, the chronic skin pigmentation caused by onchocerciasis). These conditions were mentioned by almost all groups in the discussions.
Participants had different views regarding onchocerciasis as a public health problem in their communities. Most participants considered onchocerciasis a serious health problem; however, epilepsy was perceived as the most afflicting disease. One CORP described epilepsy as the most burdensome condition in Msogezi village:
“In Msogezi, we are troubled with diseases like Malaria, onchocerciasis and other diseases, especially epilepsy which is the most devastating disease” [Msogezi, CORP].
Out of four CORPs from Sali village, two indicated epilepsy as the most important public health problem in their villages, while the other two considered malaria followed by epilepsy as the most important diseases. One ranked onchocerciasis in third position after epilepsy. Parent/caregivers from Sali and CORPs from Msogezi, mentioned epilepsy and malaria as the diseases most affecting their community.
Regarding onchocerciasis, a CDD from Sali village stated that some participants considered the disease a trivial treatable condition:
“This is just a normal disease, and we all use drugs (ivermectin) which are distributed every year” [Sali, CDD].
It was common understanding for most communities that ivermectin alleviate the clinical manifestations caused by onchocerciasis. However, this notion might have a negative impact on the uptake of ivermectin by people who do not feel sick. As a CDD exemplified:
“People who are supposed to swallow the drugs would ask you: Who told you that I am sick so that I swallow the drug?” [Sali, CDD].
A similar situation was portrayed by the NTD coordinators, in which some villagers stopped taking ivermectin once symptoms disappeared:
“As a result of long-term use ivermectin, some people do not swallow the drugs (ivermectin) because they no longer suffer from clinical conditions such as itching and rashes which were prevalent in previous years” [NTD Coordinator].
Most community members recognised that the burden of onchocerciasis decreased since the inception of CDTI over twenty years back. One of the IDIs explained that the prevalence of onchocerciasis dermatological manifestations decreased, but that it was still present in some people:
“A big problem was skin itching and hard, dry skin, which are less pronounced nowadays, although still few present skin itching” [NTD Coordinator].
3.2.2 Perceived causes and transmission of onchocerciasis
Study participants in all FGD knew that onchocerciasis is transmitted by a blackfly, locally known as “vifuna” (plural) and “kifuna” (singular). Most discussants understood that blackflies pick parasites from an infected person and inject it into another person, who can then acquire the disease as quoted in one of the groups:
“Many community members know that blackflies are the agent that transmits onchocerciasis in their area’’ [Mzelezi; CDD].
Another participant said:
“Not every blackfly carries the filarial parasite, only if the fly has bitten somebody with the infection, then the fly could transmit onchocerciasis to another person” [Mzelezi, CDDs], while a PWE caregiver said: “Blackflies bite people and leave them with this disease which causes rashes and itching” [Sali PWE Caretakers].
Some of participants were aware that blackflies breed in fast-flowing waters especially in the highlands, while others had different misconceptions that they breed in forests where thick foliage exists. Others, also associated fast flowing waters (spring) with no rapids as a breeding site for blackflies.
One of the NTD programme coordinators explained that some of the local communities relate blackflies breeding site with a well-known spring which is a major source of domestic water supply for cooking and drinking in Kitope a sub-village in Mzelezi. This sub-village has one of the highest number of people with epilepsy. He said:
“…, this community link the blackflies breeding sites to the ground/spring water flowing from the mountains in Kitope sub-village. This is the area with many people with epilepsy” [NTD coordinator].
A PWE caretaker stated that Mzelezi village had a high burden of onchocerciasis with intensive blackflies biting rates, which could be why many people are affected by epilepsy:
“The Kitope area is terribly affected, it has plenty of blackflies, there you may find two to three people in one household having epilepsy because of onchocerciasis” [Mzelezi, PWE caretaker].
3.2.3 Knowledge on the prevention of onchocerciasis
Participants had different views on the onchocerciasis prevention approaches. The majority believed the disease is preventable through taking ivermectin. One participant explained to have noticed that the burden of onchocerciasis decreased since ivermectin began to be distributed:
“Since we started taking the medicine (ivermectin), there have been big changes when it comes to (onchocerciasis) transmission where people are no longer presenting with symptoms as it used to be” [Mzelezi, CORP].
Another added to be aware that ivermectin prevented onchocerciasis:
“According to my understanding, filaria is caused by small flies, and its prevention is through taking (ivermectin) pills; apart from that, I know nothing else” [Sali, PWE caretaker].
Conversely, other participants did not believe onchocerciasis is preventable since bites from blackflies are unavoidable and abundant in their communities:
“Onchocerciasis cannot be prevented since blackflies are too many around here” [Sali, PWE and caretakers], while another participant said: “Eventually, we will all get onchocerciasis because, when we go outside to sweep or wash dishes, the flies bite us; now what are we preventing” [Sali, PWE and caretakers], a third person stated: “There is no prevention for onchocerciasis” [Mzelezi, CORP].
Ivermectin has been in use for so long in these communities that few people currently present clinical manifestations besides onchocerciasis-associated epilepsy. This changed the habits and perceptions of people towards using ivermectin. One of the NTD programme coordinators described that some community members were taking ivermectin intermittently, which can perpetuate transmission, as the adult worms do not die with ivermectin:
“Individuals presenting with clinical conditions of the disease are very few nowadays due to prolonged use of ivermectin, so people think (ivermectin) drugs are no longer required. But we provide education that if we take the drug annually, it will kill the microfilariae and adult worms, which are not killed by the drug and have a lifespan of about 15 years, will be sterilised from releasing microfilariae. This will stop transmission. Unfortunately, this misconception that people are no longer sick and that there is no need to take drugs has been why some people refused to take the drug” [IDI, NTD coordinator].
3.2.4 Knowledge of the association between onchocerciasis and epilepsy
Knowledge about the association between onchocerciasis and epilepsy was limited. Only a few participants were aware of this association, especially CDDs involved in the distribution of ivermectin or community health workers involved in the surveillance of epilepsy. As a CDD explained, the knowledge of onchocerciasis and epilepsy association was recently acquired following awareness sessions implemented in the study villages and facilitated the CDTI:
‘‘The community at some point did not understand that onchocerciasis can cause epilepsy, but after we (CDD) had been educated, we explained to the community that it could cause epilepsy. So, now over 70% of people understand it, which has made the distribution of ivermectin easy as most people are now coming for the drug instead of waiting at home” [Sali, CDD].
Another CDD from Sali village reiterated the awareness of the association that community health workers were communicating to the village:
‘‘… Community health workers were providing education that if you do not take ivermectin, you will get epilepsy. So now they (Sali community) know the association and understand why it is important to take the drug (ivermectin)” [Sali, CDD].
The community’s recent awareness of the association between onchocerciasis and epilepsy is also supported by one of the IDIs. The NTD programme coordinator confirmed that the local knowledge of the association was low since the training only recently included sessions on the association between epilepsy and onchocerciasis. He further described that the local belief that epilepsy is hereditary or the result of intermarriage had increased community resistance to changing perceptions of the cause of epilepsy, despite Mahenge being known to be endemic for both onchocerciasis and epilepsy:
“I can say, the knowledge on association is very limited (minimal), since there are so many thoughts, and everyone has their own knowledge and perceptions. Others think it is a hereditary disease, while others think it is due to intermarriage and be-witching, …., but due to recent training on the association between the two diseases, the knowledge seems to increase (on epilepsy being associated with onchocerciasis)” [IDI, NTD coordinator].
Nonetheless, groups not directly engaged in activities related to NTD or epilepsy control shared personal awareness of the association. A resource person admitted to being aware of the association and noticed a decrease in epilepsy incidence since CDTI was introduced:
‘‘To my knowledge, it is possible that onchocerciasis is a major cause of this disease (epilepsy); experience from the past when ivermectin was introduced shows that the epilepsy cases have been declining, and even the skin rashes have disappeared nowadays. My belief is that the parasite goes directly into the human brain and then causes epilepsy” [Sali, CORP].
Other participants refused to accept the association because they considered epilepsy a hereditary disease and onchocerciasis an infectious disease:
“What I know is that epilepsy is hereditary and not an infectious disease. So, I cannot say onchocerciasis can cause epilepsy” [Msogezi, CORP].
3.2.5 Community acceptance of the CDTI programme
Study participants were aware of the CDTI strategy. According to some participants, not everybody took ivermectin during the distribution period due to various claims, such as the drug causing itching and swelling of the body. One of the CORPs confessed never to have taken ivermectin since the CDTI started:
“I had never taken them since when the distribution started” [Mzelezi, CORP].
Another participant added the uncertainty that some people might receive the ivermectin tablet from the CDD but decide not to take it afterwards:
“There is a possibility that people receive the tablets and say that they will take them tomorrow/thereafter but end up throwing them away” [Mzelezi, PWE and caretakers].
3.2.6 Perceived individual reasons for not taking ivermectin
Different reasons for not to take ivermectin were reported. These included: not ready to forego alcohol for some days to avoid to take alcohol together with ivermectin, negligence, lack of knowledge why the drug should be swallowed for many years even when someone doesn’t show signs of the disease, adverse reactions (such as swelling), pretending to be pregnant or underage, elderly people and infertility. The latter reasons seemed to raise concern to many participants as quoted by men who were afraid that the drug could cause infertility or the inability to participate fully in sexual intercourse:
“The drug (ivermectin) causes infertility and reduces sexual drive (loss of libido) in men” [Msogezi, CDD].
Another participant said:
“Men do not want to take the medicine (ivermectin) because they do not want to reduce their libido” [Sali, female PWE caretaker].
Another portrayed the perceptions referred by some community members as follows:
“We cannot swallow these medications since they reduce sexual drive in men and at the end we will not be able to reproduce, …, You cannot find these medications in town even white people do not use them” [Sali, CORP].
However, an NTD coordinator stated that now people understood the benefits of taking ivermectin, while in the past, they confused the symptoms of onchocerciasis with the side effects of the treatment:
“Such misconceptions of ivermectin causing sexual performance existed in the past, but nowadays, people understand the benefits and need of the medicine (ivermectin). In the past, people were so affected with oncho; that is why they had less libido. They used to scratch themselves so much that they could not sleep or perform any economic activities, but after using these medicines, they sleep and work peacefully” [IDI, NTD coordinator].
3.2.7 Perceived challenges during mass drug administration
Reported challenges by FGDs participants included poor geographical coverage, lack of incentives, absence of prophylactic medications for ivermectin side effects and transport, refusal of the community members to take the drug, and negligence by CDDs and village leaders to adhere to the stipulated guidelines such as not distributing ivermectin “directly observed”. A community health worker mentioned the latter problem:
“Collection of ivermectin by family members to use them later is a big problem. Large percentage of these people they end-up not swallowing the drug” [Mdindo and Msogezi, CDD]
Some areas are hard to reach due to the topographical layout of Mahenge terrain. Therefore, a CDD acknowledged that some CDDs could not reach all households in the hard-to-reach and large areas due to the limited number of days (two weeks) to carry out the CDTI:
“Some households are located too far from the village, and it is difficult to reach them repeatedly, especially when distributing ivermectin; you can go around even three times without finding residents” [Mzelezi, CDD].
Low compensations for CDDs participating in distribution of ivermectin was also pointed as another challenge that affects the distribution. The CDDs suggested increasing the allowance to improve CDDs productivity:
“The allowance we receive is too low. In order to reduce complaints from the CDDs and improve efficiency, we suggest increasing the allowance’’ [Mzelezi, CDD].
Supervision during CDTI is very important to ensure that CDDs are performing their work according to the guidelines which include how to dispense the drug according to height and directly observed. The supervision should involve programme coordinators, persons in charge of health facilities and community leaders.
One the CDD pointed out how some of the villages leaders fails to play their supervision role:
“Village chairpersons consider themselves as bosses, therefore, do not supervise drug distribution activity, they only concentrate on other business, and during the day they send false information to the authority although they did not follow up” [Msogezi, CDD].
Wrong timing for distribution was also another challenge that was affecting the CDTI programme. To increase the CDTI coverage, participants suggested not to distribute ivermectin during the farming season when the majority of people relocate for farming but distribute ivermectin in months that people are back in the villages:
“Distribution of drugs (ivermectin) should be carried out in the months of June or July, which is not the farming season in this area” [Mzelezi, CORP].
4 Discussion
Our study aimed to assess factors associated with persistence of high transmission of onchocerciasis using qualitative methods in four rural villages in the Mahenge area despite more than 20 years of CDTI. In 2018, a research project was initiated in the area to reduce the incidence of onchocerciasis-associated epilepsy. Within this project, a biannual CDTI programme was initiated in 2019 based on the successful impact of such intervention in Northern Uganda on reducing the incidence of epilepsy and nodding syndrome (21).
All study participants had a basic knowledge about onchocerciasis and used local names to describe the clinical manifestations of the disease. Similar to observations in 2018 in Mahenge, in the villages of Isongo and Uponera, most participants associated the transmission of onchocerciasis with blackflies (“vifuna”) (22). Some participants further described that blackflies carrying larvae obtained during a blood meal infect other humans during a subsequent bite. Furthermore, there was a consensus among the NTD programme coordinators and some FGD participants that the burden of skin itching caused by onchocerciasis had decreased due to CDTI.
Similar to previous studies in Mahenge (22), Nigeria (23) and Ethiopia (24, 25), witchcraft, and supernatural powers were not mentioned as causes of onchocerciasis. This is in contrast with persistent misconceptions about epilepsy in the Mahenge area (20). The fact that there were no misconceptions about onchocerciasis most likely is the consequence of the over 20 years of CDTI. Before each CDTI round, training sessions are organised by the NTD programme to orient the CDDs on how to approach the communities and raise community awareness on why ivermectin is important. However, such programmes were rarely implemented. National campaigns through radio and other media have been the cornerstone to educate communities. However, only a small proportion of people in rural areas listen to the radio and watch TV. A nationwide media survey in Pakistan indicated that in rural settings only 18% watched TV regularly and only 14% listened to the radio (26). This indicates that community meetings should be used to complement radio and TV programmes.
The knowledge about the association between onchocerciasis and epilepsy was recently acquired as a consequence of the ongoing research project in the area (11–13, 20, 27). The fact that onchocerciasis is associated with epilepsy has shown to increase the adherence to CDTI and coverage in areas with high epilepsy and onchocerciasis prevalence (20).
Most study participants were aware of the CDTI strategy. This awareness is crucial for attaining high geographical coverage and reaching the last miles of onchocerciasis elimination. However, some community members refused to take ivermectin due to fear of adverse events. Particularly men were afraid of reduced libido. This was also reported in another study in Tanzania (28). Such fear is not justified as there is no evidence that ivermectin at the therapeutic dose given during CDTI will affect the persons libido (29). Similarly to a previous study, the acceptability of the CDTI was high among the respondents (22) and the onchocerciasis disease burden was described to have decreased in Mahenge since the implementation of CDTI.
Reported challenges for the CDTI programme included poor geographical CDTI coverage, lack of incentives for CDDs, lack of prophylactic medications for ivermectin side effects, refusal of the community members to take the drug and negligence of CDDs and village leaders to adhere to WHO stipulated guidelines to administer the ivermectin dose to children based on height. Similar challenges were reported in other studies (30, 31). Poor programme management with lack of supervision and monitoring of CDDs were also reported. Because of long-distance walking without transport in a mountainous area, CDDs often failed to distribute the ivermectin in a directly observed way. Moreover, in Mahenge, one CDD per 250 people was considered to be insufficient for distributing ivermectin within the two allocated weeks. Advocacy from the CDTI programme leadership was mentioned to be important to increase the uptake of ivermectin; however, such support was reported to be lacking. Respondents felt that there is a need to assign more and better salaries for CDDs to engage more people. Timing for distribution of ivermectin was also important since majority of people relocates to farming areas between February and May. So, it was advised to distribute ivermectin during months outside the faming period to find most of people in their homes.
A limitation of our study is that the villages included in our study were villages with a high prevalence of onchocerciasis-associated epilepsy that had been targeted with interventions to increase the CDTI coverage. As such, misconception about onchocerciasis and ivermectin may have been even more prominent in other endemic villages of Mahenge without awareness programmes, similar to what has been shown in hard-to-reach, resource-limited villages in South West Ethiopia (32).
Based on this study and on the fact that despite 25 years of annual CDTI, the prevalence of onchocerciasis and epilepsy remained high in certain rural villages in Mahenge, in 2019, bi-annual CDTI was introduced. However, in 2020 there was only one distribution of ivermectin due to the COVID-19 pandemic. In 2021, in a house-to-house 82.3% of the population in the four rural study villages took at least once ivermectin (D Bhwana, personal communication).
5 Conclusions
Continuous advocacy about the importance of taking ivermectin biannually and regular supervision during CDTI by district and national coordinators are crucial to attain the onchocerciasis elimination goal. District coordinators and CDDs must ensure drugs are available at the health facility before the distribution days, and advocacy campaigns should associate ivermectin uptake as prophylactic treatment for onchocerciasis and associated epilepsy. There is also the need to motivate CDDs with more incentives and increase the number of days assigned to CDTI. Additionally, it was suggested to distribute ivermectin during the months that farming is not taking place to maximise CDTI coverage.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Ethical approval was obtained from the Ethics committee of the National Institute for Medical Research, Tanzania (NIMR/HQ/R.8a/Vol.IX/227) and the ethics committee of the University of Antwerp, Belgium. Informed consent was obtained from all subjects involved in the study.
Author contributions
Conceptualization, DB, BM, and RC; Methodology, DB, BM, AM, IM, and RC; Software, BM; Validation, BM and RC; Formal analysis, DB, BM, IM, AM; Investigation, DB, BM, IM, AM, PM, WM; Resources, RC; Data curation, BM; Writing—original draft preparation, DB, BM; Writing—review and editing. DB, BM, L-JA, IM, AM, PM, WM and RC; Visualization, DB, BM; Supervision, BM and RC; Project administration, BM; Funding acquisition, RC; All authors have read and agreed to the published version of the manuscript
Funding
The study was funded by VLIRUOS (Flemish Interuniversity Council for University Development Cooperation). The study sponsors, had no role in the design, execution, interpretation, or writing of the study
Acknowledgments
Deogratius Raphael, Gisela Ligazio, Exavery Kazingoma, Christopher Katyawa and Jackson Magogo are acknowledged for organising community meetings. Study participants, community members and leaders for acceptance to participate in the study. Health authorities in Morogoro Region and Ulanga District for their cooperation and support provided to the study teams. The Director General of the National Institute for Medical Research provided the permission to publish this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Häusermann W, Hausermann W. On the biology of simulium damnosum theobald, 1903, the main vector of onchocerciasis in the mahenge mountains, ulanga, Tanzania. Acta Trop (1969) 26(1):29–69.
2. Brattig NW, Cheke RA, Garms R. Onchocerciasis (river blindness) - more than a century of research and control. Acta Trop (2021) 218:105677. doi: 10.1016/j.actatropica.2020.105677
3. World Health Organization (WHO). Onchocerciasis, in: Ey facts (2019). Available at: https://www.who.int/news-room/fact-sheets/detail/onchocerciasis (Accessed 30.01.2023).
4. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet (London England) (2018) 392(10159):1789–858. doi: 10.1016/S0140-6736(18)32279-7
5. Hopkins AD. Neglected tropical diseases in Africa: a new paradigm. Int Health (2016) 8 Suppl 1:i28–33. doi: 10.1093/inthealth/ihv077
6. Tekle AH, Zouré HGM, Noma M, Boussinesq M, Coffeng LE, Stolk WA, et al. Progress towards onchocerciasis elimination in the participating countries of the African programme for onchocerciasis control: epidemiological evaluation results. Infect Dis Poverty. (2016) 5(1):1–25. doi: 10.1186/s40249-016-0160-7
7. World Health Organization (WHO). Ending the neglect to attain the sustainable development goals: A road map for neglected tropical diseases 2021–2030: overview. World Health Organization (2020).
8. Colas JL. Geographical distribution of onchocerciasis in the ulanga area, Tanzania. East Afr Med J (1966) 43(10):426–9.
9. Colas JL. Onchocerciasis survey in kisawasawa. (Ulanga district, Tanzania). East Afr Med J (1966) 43(1):19–20.
10. Geigy R, Colas J, Fernex M. Endemic onchocerciasis in the ulanga area, Tanzania. Acta Trop (1965).
11. Greter H, Mmbando B, Makunde W, Mnacho M, Matuja W, Kakorozya A, et al. Evolution of epilepsy prevalence and incidence in a Tanzanian area endemic for onchocerciasis and the potential impact of community-directed treatment with ivermectin: a cross-sectional study and comparison over 28 years. BMJ Open (2018) 8(3):e017188. doi: 10.1136/bmjopen-2017-017188
12. Mmbando BP, Suykerbuyk P, Mnacho M, Kakorozya A, Matuja W, Hendy A, et al. High prevalence of epilepsy in two rural onchocerciasis endemic villages in the mahenge area, Tanzania, after 20 years of community directed treatment with ivermectin. Infect Dis Poverty. (2018) 7(1):64. doi: 10.1186/s40249-018-0450-3
13. Bhwana D, Mmbando BP, Dekker MC, Mnacho M, Kakorozya A, Matuja W, et al. Clinical presentation of epilepsy in six villages in an onchocerciasis endemic area in mahenge, Tanzania. Epileptic Disord (2019) 21(5):425–35. doi: 10.1684/epd.2019.1093
14. Hendy A, Krüger A, Pfarr K, De Witte J, Kibweja A, Mwingira U, et al. The blackfly vectors and transmission of onchocerca volvulus in mahenge, south eastern Tanzania. Acta Trop (2018) 181:50–9. doi: 10.1016/j.actatropica.2018.01.009
15. Colebunders R, Basáñez MG, Siling K, Post RJ, Rotsaert A, Mmbando B, et al. From river blindness control to elimination: Bridge over troubled water. Infect Dis Poverty. (2018) 7(1):1–15. doi: 10.1186/s40249-018-0406-7
16. Colebunders R, Njamnshi AK, Menon S, Newton CR, Hotterbeekx A, Preux PM, et al. Onchocerca volvulus and epilepsy: A comprehensive review using the Bradford hill criteria for causation. PLoS Negl Trop Dis (2021) 15(1):e0008965. doi: 10.1371/journal.pntd.0008965
17. Chesnais CB, Nana-djeunga HC, Njamnshi AK, Lenou-nanga CG, Boullé C, Bissek AZ, et al. The temporal relationship between onchocerciasis and epilepsy: A population-based cohort study. Lancet Infect Dis (2018) 18(11):1278–86. doi: 10.1016/S1473-3099(18)30425-0
18. Chesnais CB, Bizet C, Campillo JT, Njamnshi WY, Bopda J, Nwane P, et al. A second population-based cohort study in Cameroon confirms the temporal relationship between onchocerciasis and epilepsy. Open Forum Infect Dis (2020) 7(6):ofaa206. doi: 10.1093/ofid/ofaa206
19. Bhwana D, Dusabimana A. Ivermectin treatment response in two rural villages with a high prevalence of onchocerciasis and epilepsy , mahenge Tanzania. Afr Health Sci (2019) 22(3):607–16. doi: 10.4314/ahs.v22i3.65
20. Mmbando BP, Bhwana DK, Massawe IS, Magili P, Mahone S, Makunde W, et al. Community knowledge, attitudes, and practices regarding epilepsy in mahenge, Tanzania: A socio-anthropological study in an onchocerciasis-endemic area with a high prevalence of epilepsy. Epilepsy Behav (2022) 128(July):6–8. doi: 10.1016/j.yebeh.2022.108568
21. Gumisiriza N, Mubiru F, Siewe Fodjo JN, et al. Prevalence and incidence of nodding syndrome and other forms of epilepsy in onchocerciasis-endemic areas in northern Uganda after the implementation of onchocerciasis control measures. Infect Dis Poverty (2020) 9(1):12.doi: 10.1186/s40249-020-0628-3
22. Mushi V. Implementation Challenges of Community Directed Treatment with Ivermectin Program for Control of Onchocerciasis in Ulanga, Tanzania. East Afr Health Res J (2021) 5(2):123–8.doi: 10.24248/eahrj.v5i2.661
23. Adeoye AO, Ashaye AO, Onakpoya OH. Perception and attitude of people toward onchocerciasis (river blindness) in south Western Nigeria. Middle East Afr J Ophthalmol (2010) 17(4):310–4. doi: 10.4103/0974-9233.71594
24. Yirga D, Deribe K, Woldemichael K, Wondafrash M, Kassahun W. Factors associated with compliance with community directed treatment with ivermectin for onchocerciasis control in southwestern Ethiopia. Parasit Vectors (2010) 3(1):48. doi: 10.1186/1756-3305-3-48
25. Shuford KV, Turner HC, Anderson RM. Compliance with anthelmintic treatment in the neglected tropical diseases control programmes: a systematic review. Parasit Vectors (2016) 9(1):29. doi: 10.1186/s13071-016-1311-1
26. Stiles M. Imran khan and EPI: challenging conventional approaches to health promotion in Pakistan. Health Millions. (1995) 21(4):16–9.
27. Bhwana D, Das L, Siewe Fodjo JN, Francis F, Challe DP, Makunde HW, et al. A peer support group intervention to decrease epilepsy-related stigma in an onchocerciasis-endemic area in mahenge, Tanzania: A pilot study. Epilepsy Behav (2021) 124:108372. doi: 10.1016/j.yebeh.2021.108372
28. Mushi V. Implementation challenges of community directed treatment with ivermectin program for control of onchocerciasis in ulanga, Tanzania. East Afr Heal Res J (2021) 5(2):123–8. doi: 10.24248/eahrj.v5i2.661
29. York KJ, Kabole I, Mrisho M, Berry DM, Schmidt E. Factors affecting community participation in the CDTI program in morogoro, Tanzania. J Nurs Scholarsh an Off Publ Sigma Theta Tau Int Honor Soc Nurs. (2015) 47(1):96–104. doi: 10.1111/jnu.12121
30. Brieger WR, Okeibunor JC, Abiose AO, Wanji S, Elhassan E, Ndyomugyenyi R, et al. Compliance with eight years of annual ivermectin treatment of onchocerciasis in Cameroon and Nigeria. Parasit Vectors. (2011) 4:152. doi: 10.1186/1756-3305-4-152
31. Amazigo UV, Leak SGA, Zoure HGM, Okoronkwo C, Diop Ly M, Isiyaku S, et al. Community-directed distributors-the “foot soldiers” in the fight to control and eliminate neglected tropical diseases. PLoS Negl Trop Dis (2021) 15(3):e0009088. doi: 10.1371/journal.pntd.0009088
Keywords: onchocerciasis, community directed treatment with ivermectin, elimination, epilepsy, focus group discussions, misconceptions
Citation: Bhwana D, Massawe IS, Mushi AK, Magili P, Amaral L-J, Makunde W, Mmbando BP and Colebunders R (2023) Factors associated with low-uptake of ivermectin in Mahenge, an area with high prevalence of onchocerciasis and epilepsy in Tanzania: A qualitative perspective. Front. Trop. Dis 4:1079012. doi: 10.3389/fitd.2023.1079012
Received: 24 October 2022; Accepted: 13 March 2023;
Published: 03 April 2023.
Edited by:
Catherine A Gordon, QIMR Berghofer Medical Research Institute, The University of Queensland, AustraliaReviewed by:
Mike Yaw Osei-Atweneboana, Council for Scientific and Industrial Research-Water Research Institute (CSIR-WRI), GhanaVerner Orish, University of Health and Allied Sciences, Ghana
Copyright © 2023 Bhwana, Massawe, Mushi, Magili, Amaral, Makunde, Mmbando and Colebunders. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Bhwana, ZGFuYmh3YW5hQHlhaG9vLmNvbQ==
 Dan Bhwana
Dan Bhwana Isolide S. Massawe
Isolide S. Massawe Adiel K. Mushi2
Adiel K. Mushi2 Luís-Jorge Amaral
Luís-Jorge Amaral Robert Colebunders
Robert Colebunders