- 1Department of Obstetrics and Gynaecology, School of Medical Sciences, College of Health and Allied Sciences, University of Cape Coast, Cape Coast, Ghana
- 2Department of Microbiology and Immunology, School of Medical Sciences, College of Health and Allied Sciences, University of Cape Coast, Cape Coast, Ghana
- 3Department of Community Medicine, School of Medical Sciences, College of Health and Allied Sciences, University of Cape Coast, Cape Coast, Ghana
- 4Department of Medical Laboratory Science, School of Allied Health Sciences, College of Health and Allied Sciences, University of Cape Coast, Cape Coast, Ghana
Cervical cancer (CC) continues to be a global burden, and a disease of public health interest, especially in low- and middle-income countries. This study explored the knowledge and awareness of human papillomavirus (HPV) infection and CC and the risk-behavioural characteristics of an adult female population in rural Ghana. A total of 274 women, aged 21 years and above were recruited through multi-stage sampling. A questionnaire was used to obtain data on their socio-demographic and socio-economic characteristics and assess their knowledge and awareness of HPV and CC through face-to-face interviews. In all, 187 (68.2%) participants had poor knowledge of HPV and CC with 87 (31.8%) having good knowledge. Only 18.2% and 48.9% of them had prior awareness of HPV infection and CC, respectively. Their primary source of information was the broadcast media (TV and Radio stations) (60.1%). Regarding risky lifestyle behaviours, the mean age at sexual debut was 18.52 ± 2.39 years, 82.8% have had more than one lifetime sexual partner, 81.0% were multiparous with 51.5% using oral contraceptives. Women with higher educational attainment (cOR = 0.41; 95%CI = 0.20-0.81), monthly income (cOR = 0.31; 95%CI = 0.10-1.02), and lifetime sexual partners (aOR = 0.46; 95%CI = 0.21-1.00) were less likely to have poor CC and HPV knowledge compared to their counterparts. In conclusion, adult females in the rural population have limited knowledge and awareness of HPV infection and CC with low CC screening. Intensive educational campaigns should be organised and spearheaded on multiple platforms by the Ghana Health Service and civil societies to sensitise and educate women, in the rural parts of the country, on CC and its related preventive measures.
Introduction
Cervical cancer (CC) continues to be of public health concern in Ghana, just like in most developing countries (1–4). Globally, it is rated among the top five most common cancers diagnosed among females, with a significant mortality rate (5, 6). CC is the fourth most common disease in women and the fourth greatest cause of cancer mortality, with a reported 604,000 new cases and 342,000 deaths globally in 2020 (7). In Ghana, CC continues to be the most predominant cancer diagnosed, with a mortality rate three times higher than the global rate (1, 2, 6, 8, 9). CC in Ghana has a high age-standardized incidence and death rate of 32.9 and 23.0 per 100,000 respectively (10).
Over 90% of CC cases are generally implicated with the acquisition and persistence of Human Papillomavirus (HPV) infection, more typically, the oncogenic types (11–13). As the most common sexually transmitted infection, it is considered that the risk of sexually active persons, especially women, getting infected with HPV within their lifetime is nearly 80% (11, 12, 14). However, other factors, coupled with HPV acquisition and persistence, increase the risk of developing precursor lesions and ultimately, CC. Agreeably, these factors can be broadly classified as; (1) those that increase the risk of acquiring infection and its persistence, such as multiple lifetime sexual partners, early age of sexual debut, co-infections and immune-related diseases; (2) those that increase the risk of carcinogenesis in the face of persistent HPV infection, such as smoking, multiparity, prolonged hormonal contraceptive usage and heavy alcohol consumption, and (3) those that combine both effects (15).
In Ghana, most patients with CC present with their condition to health facilities at advanced stages. This, ultimately, accounts for the high mortality rate in the country (1, 5). Several studies in Ghana (6, 16, 17) and other countries (18–22) have indicated low awareness and knowledge of CC and HPV infection to be major factors influencing the uptake of screening programmes.
To attain target 3.4 of the UN Sustainable Development Goal (SDG), the WHO projection of a 90-70-90 target by 2030 has been expanded to help with the ultimate goal of global elimination of CC (23, 24). Target 3.4 of the SDG aims to reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being. The WHO triple-intervention strategy aims to achieve 90% vaccination of all girls by age 15 years, 70% screening coverage of women twice between 35 to 45 years, and at least 90% treatment of all precancerous lesions detected (25, 26). To achieve this, public awareness of CC and HPV infection is recommended to enhance the development of appropriate attitudes toward CC prevention, diagnosis, and management (1, 17). However, since its discovery in the 4th century, knowledge and awareness of CC and its relationship with HPV infection, continue to stagnate, especially among rural populations (16, 27). The need to create public awareness, especially among the rural population is likely to enhance the development of a positive attitude towards the prevention, diagnosis and management of CC and ultimately attain the WHO 2030 triple projection strategy (28–30).
The impact of health education on CC knowledge and screening has earlier been reported (30). However, the level of CC and HPV knowledge among women in rural communities in Ghana has not been adequately explored. For instance, to the best of our knowledge of CC has not been assessed at the Akyemansa District. The objectives of this study were therefore to (1) assess the knowledge and awareness of HPV infection and CC among adult females, (2) determine the factors associated with knowledge and awareness of HPV infection and CC and (3) determine the risk-behavioural characteristics regarding HPV infection and CC among adult females in rural communities in the Akyemansa District of Ghana. The findings of this study would be important for implementation of interventions to increase cervical cancer awareness, screening and vaccination at the Akyemansa District and other rural communities.
Materials and methods
Study design and subjects
This cross-sectional study was conducted in five conveniently selected rural communities in the Akyemansa District of the Eastern Region of Ghana, from 1st May to 30th June 2019.
Study site and population
The Akyemansa District of the Eastern region of Ghana is a predominantly rural setting, which is endowed with several natural resources, including gold and diamond deposits. The population of women in the district was estimated as 49,371 representing 50.7% of the total population of the district based on the 2010 population and housing census (31). The prevalence of the human immunodeficiency virus (HIV) among adults in the district was 0.57% (32).
Sample size and sampling
The minimum sample size of 381 required for the study was determined using the StatCalc function of Epi Info software, Version 7.2.5.0 (Centre for Diseases Control, Atlanta, Georgia, USA, and World Health Organization, Geneva, Switzerland). The following assumptions were made: population size of women in the Akyemansa District of 49,371, a confidence level of 95%, expected proportion or knowledge prevalence of 50%, error margin of 5%, and design effect of 1.0. However, some participants invited were unwilling to participate because of the sensitive nature of some of the study questions therefore a total sample size of 274 was realised at the end of the study. Participants were required to be women who were (i) Ghanaians and residents of the district, (ii) 18 years and above, (iii) could express themselves in Twi or English languages and (iv) willing to participate in the study.
A multi-stage sampling procedure was used to recruit the study participants. First, study communities were conveniently selected. Second, the probability proportionate to size approach was employed in selecting the households within each community. To select the study participants within the households in each community, house-to-house visits were employed. One female member of the selected households who met the inclusion criteria was selected upon consent to be interviewed.
Study instrument and data collection
A close-ended questionnaire, adopted from previous studies (33–35), with open-ended options to allow for additional information, was used to obtain information from the participants. The questionnaire consisted of twenty-one items and was administered by three trained female assistants, who could also translate the content of the questionnaire into the local languages through face-to-face interviews. The assistants had a two-day training on data gathering processes, community entry, and communication skills.
The questionnaire assessed sociodemographic information. Age was collected as a continuous data and categorised (21-30 years, 31-40 years, 41-50 years or 51 years or more). Participants’ gender (male or female), marital status (single, married, cohabiting, divorced, or widowed), and educational attainment (primary school, junior high school, senior high school, tertiary, or no formal education) were collected as categorical data. Open-ended questions were used to solicit information concerning participants’ religion and occupation. Respondents were also made to indicate their average monthly income (100-500, 600-1000, 1100-1500 or 1500 and more) in Ghana cedis.
Participants’ knowledge of HPV and CC was assessed using six items that assessed whether participants (i) have heard of HPV infection, (ii) have heard of cervical cancer, (iii) have ever been screened for HPV, (iv) could identify the screening tools for HPV, (v) knows HPV could be contracted through sexual contact and (vi) are aware of the availability of HPV vaccines. For each item, the participants were asked to choose one of the three options: “Yes,” “No,” or “Don’t know”. For the question (iv), participants were to choose between, “Pap smear”, “VIA” or “Don’t know”. A composite knowledge score was obtained by assigning a score of 1 to any positive response to the six (6) questions on knowledge of HPV infection, CC, and screening. A negative response was assigned a score of 0; thus, the score range was 0-6. Using their respective knowledge scores and a cut-off point based on the median score, the participants were categorised as having ‘poor’ or ‘good’ knowledge of HPV and CC.
The questionnaire finally assessed risky behavioural characteristics that are likely to expose respondents to CC. Information on participants’ frequency of alcohol intake, contraceptive use, and smoking habit were collected. Participants’ age at first sexual intercourse, number of lifetime sexual partners and parity were collected as continuous variables. These variables were categorised: age at first sexual intercourse (<18 years and ≥18 years), lifetime sexual partners (< 2 and ≥2) and parity (≤2 and >2).
Questionnaire validity and reliability were carried out before the commencement of the study by pretesting twenty adult females in Amamoma, a small community near the North Campus of the University of Cape Coast. The analysis showed that the questionnaire had good internal consistency with a Kuder-Richardson Reliability coefficient of 0.738. Again, we observed that some participants misconstrued HPV for HIV and so in the final study, we had to let participants know the two are different.
Data analysis
Data obtained was entered into Microsoft Excel (2016) and transferred into STATA Software version 14 (STATA Corp, Texas USA) for statistical analysis. Descriptive statistics such as frequencies, percentages, and means were used to summarize the background characteristics of participants.
A bivariate analysis using Pearson’s Chi-square, Fisher’s Exact tests, and a one-way analysis of variance was used to examine differences in knowledge of HPV and cervical cancer based on participants’ characteristics. Variables with P-value ≤ 0.25 in the bivariate analysis were included in a binary logistic regression analysis to identify possible determinants of knowledge of HPV and CC. The results of the regression analysis are reported as odd ratios (OR) with 95% confidence intervals (CI). A P-value less than 0.05 was considered statistically significant in all analyses.
Results
Socio-demographic and socio-economic characteristics of participants
Characteristics of the participants are detailed in Table 1. Of 381 participants required and invited to participate in the study, 274 females, representing a 72% response rate, participated in the study. The mean (SD) age of participants was 39.65 (13.63) years. The youngest was 21 years while the oldest was 80 years old. Most of the participants (91/274, 33.2%) were between 21 to 30 years of age. A little over half of them (168/274, 61.3%) had partners (married or cohabiting) and almost all (99.3%) were Christians. The highest educational attainment for majority of the participants (140/274, 51.1%) was junior high school (JHS), with majority being involved in trading (110/274, 40.1%). More than 80% of the participants (240/274, 87.6%) earned an average monthly income of Ghℂ600.00 (US$ 60.0) or lower.
Regarding the risk behaviours of the participants that may predispose them to the acquisition of HPV and the development of CC, more than half of them had their sexual debut after 18 years of age (191/274, 69.7%). Similarly, majority of participants have had more than one lifetime sexual partners (227/274, 82.8%), been taking hormonal contraceptives (141/274, 51.5%), and have had 2-4 pregnancies (122/274, 44.5%).
Knowledge and awareness of cervical cancer and HPV infection
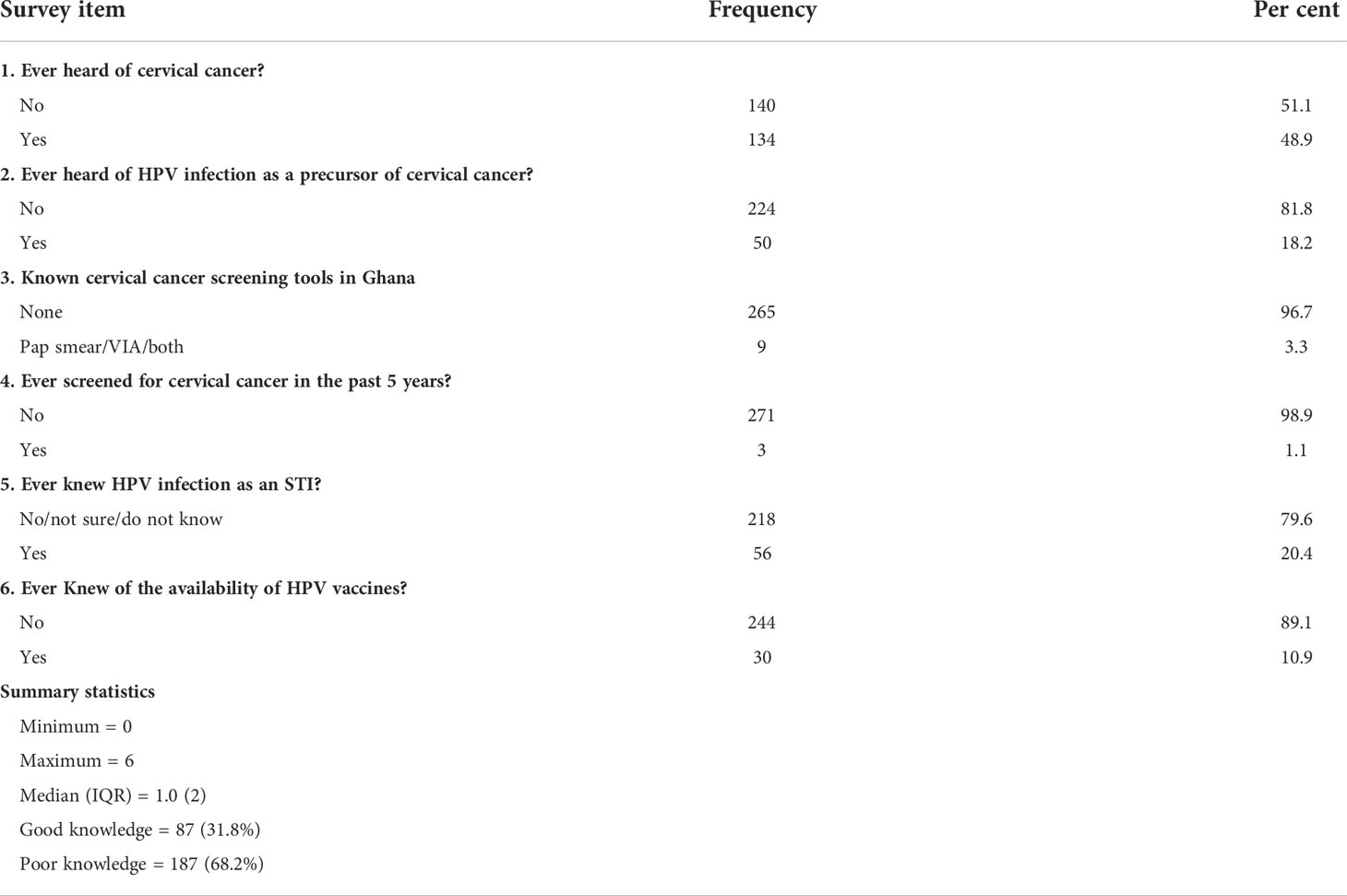
With regards to knowledge and awareness of CC and HPV infection (Table 2), only 134 (48.9%) and 50 (18.2%) of the participants had previously heard of CC and HPV infection, respectively. Only 9 (3.3%) of the participants were aware of either the conventional Pap smear test and/or Visual Inspection with Acetic acid (VIA) being the common screening tools in Ghana, and only 3 (1.1%) had ever been screened in the past 5 years. In addition, only 56 (20.4%) and 30 (10.9%) knew that HPV infection is sexually transmitted and that vaccines are available for HPV, respectively.
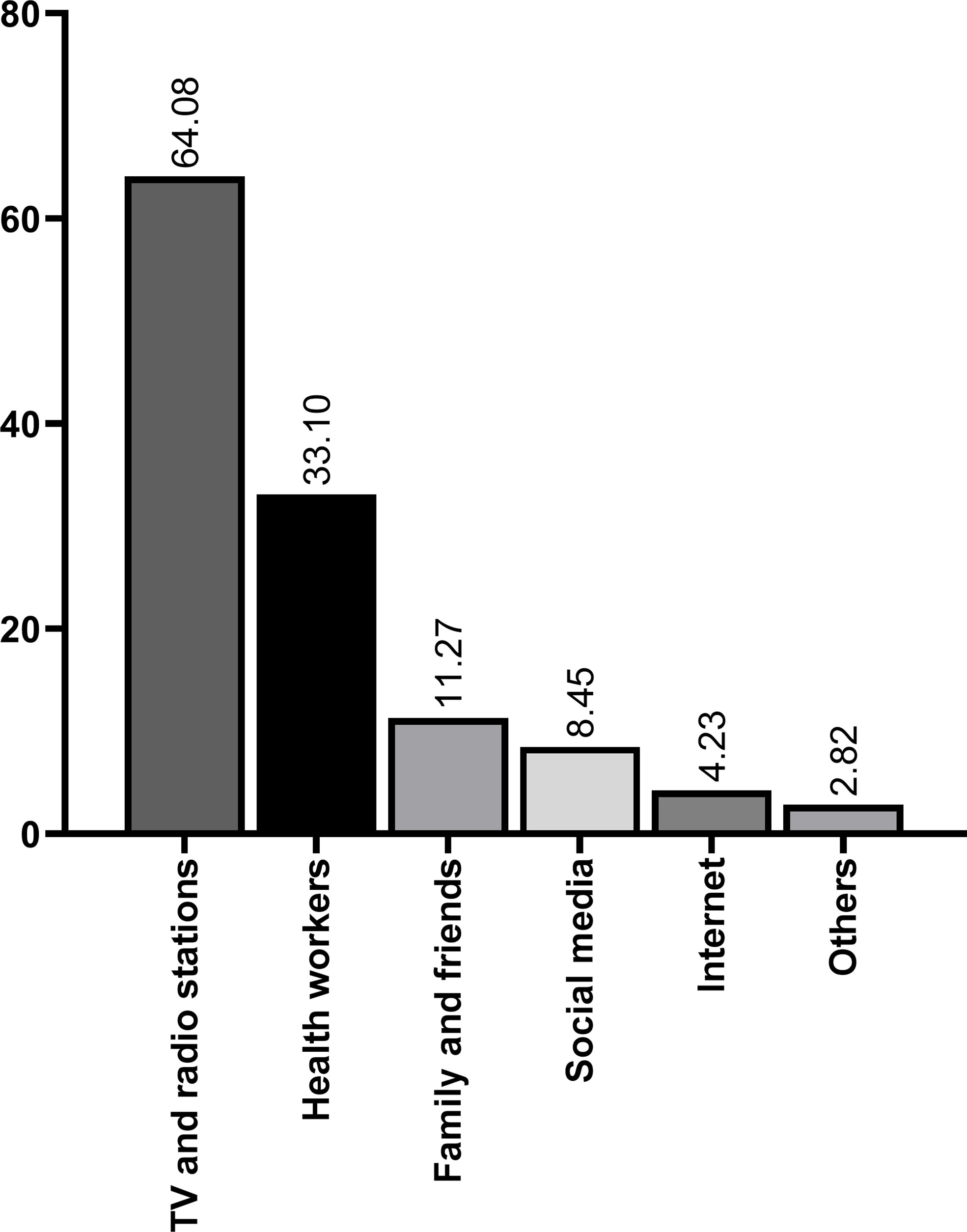
The median (interquartile range [IQR]) knowledge score of respondents was 1.0 (2) out of a maximum score of 6.0: 47.8% (n = 131) provided no positive response, whereas only 0.4% (n =1) provided positive responses to all 6 questions. Among the participants who provided any positive response, the majority (n=58, 21.2%) answered so with only 2 questions. Overall, only 87 (31.8%) had good knowledge with 187 (68.2%) demonstrating a poor knowledge score. When asked to provide their sources of information about HPV and CC, the primary sources of information cited by most of the participants were the broadcast media (64.1%) and education by community health workers and facilities (33.1%) (Figure 1).
Correlates of knowledge and awareness of cervical cancer and HPV infection among women in the Akyemansa District
The factors which were significantly associated with knowledge and awareness of HPV infection and CC were educational attainment (χ2 = 6.780, p = 0.009) and monthly income (χ2 = 4.092, p = 0.048) based on bivariate analysis (Table 3). Women with a higher educational attainment (Senior high school and above) were less likely to have poor knowledge of HPV and CC than those with lower education (Junior high school and lower). Likewise, women with higher monthly income (> GHℂ1,000) were less likely to have poor knowledge of HPV and CC than those with lesser monthly income (≤ GHℂ1,000).
Multivariate analysis showed that women with higher educational attainment (cOR = 0.41; 95%CI = 0.20-0.81), monthly income (cOR = 0.31; 95%CI = 0.10-1.02), and lifetime sexual partners (aOR = 0.46; 95%CI = 0.21-1.00), are less likely to have poor CC and HPV knowledge compared to their counterparts (Table 4).
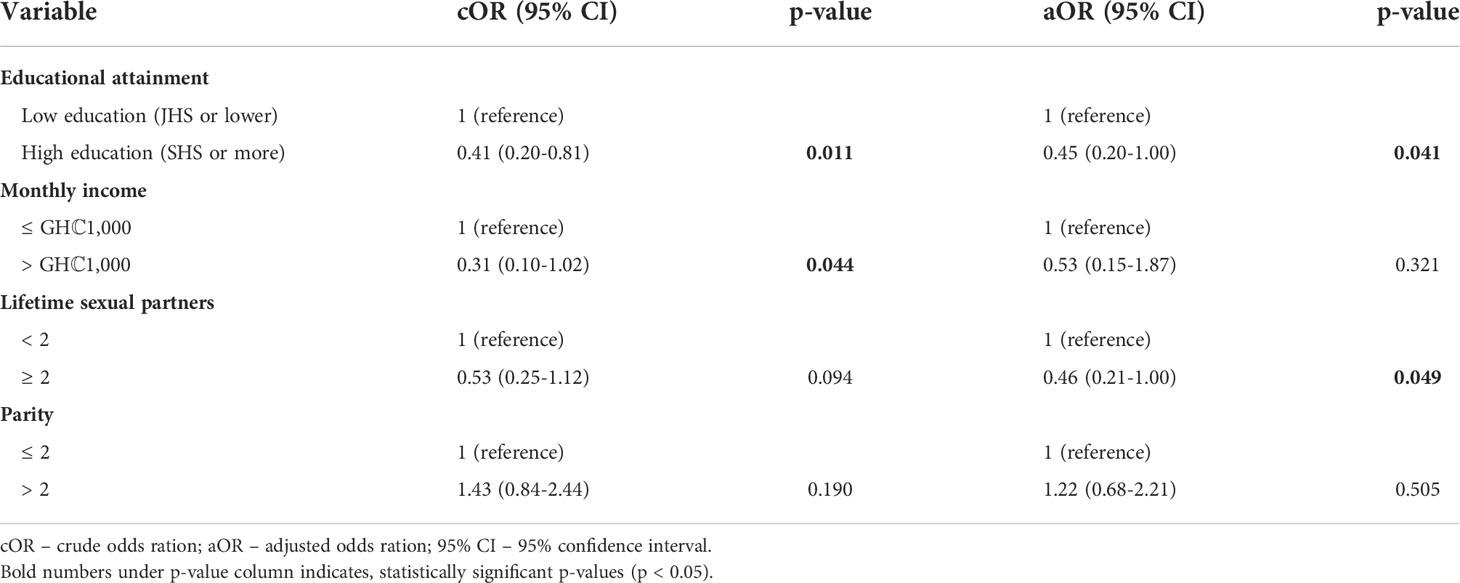
Table 4 Factors independently associated with poor knowledge of HPV and CC based on univariate and multivariate analysis.
Discussion
The need to create public awareness, especially among rural populations, is likely to enhance the development of a positive attitude towards the prevention, diagnosis and management of CC and ultimately attain the WHO 2030 triple projection strategy. This study highlights a gap in CC and HPV knowledge and awareness among rural women in the Akyemansa District of Ghana. The broadcast media (TV and radio stations) and health workers are reported to be the main source of information on CC and HPV. The major factors associated with a good knowledge and awareness were higher education, higher income and surprisingly having higher lifetime sexual partners. The study also reports a relatively high involvement in risky lifestyles which are likely to expose women in the selected communities to CC and HPV infection.
The WHO recommends that CC screening should begin at the age of 30 years, for the general population and 25 years, for women living with HIV. Subsequently, regular screening should be performed every 3-5 years, depending on the screening method used (23, 24, 36). In this study, the mean age of the participants (39.7 ± 13.6 years) shows that most of the women (64.6%, n=177) were within the recommended age range for CC screening which is stipulated at 25-65 years of age (37). Given this, it was expected that most of the participants would have had at least one CC screening at the time of the study. Also, similar to earlier studies, this study found most of the participants to be 21-30 years (90, 32.8%) (22, 38, 39). This signifies that over 30% of the participants should have had their initial CC screening at the time of the study.
In general, majority of the study population (68.2%, n=187) demonstrated poor knowledge of CC and HPV infection with over 70% of participants provided no positive response to any of the survey questions. The proportions of participants who were aware of HPV infection and CC were 18.2% (50/274) and 48.9% (134/274) respectively. Earlier studies at Elmina, a town along the coastal belt of Ghana, South Africa and Northeast China (16, 21, 40, 41) reported similarly reduced awareness of HPV and CC. On the contrary, previous studies in Southwest China, Ethiopia, North Korea, Qatar and Nigeria reported greater proportions of awareness of CC and HPV infection among the studied populations (3, 42–45). The differences in awareness could be explained by differences in the study population as the earlier studies involved participants from peri-urban and urban communities where adequate information on the disease may be available.
In this study, poor knowledge of HPV infection and CC was significantly associated with lower education, and lower income. A study in Ethiopia similarly identified 80% of the study population to have poor knowledge of CC and HPV infection (3) and this observation was associated with the socio-economic characteristics of the studied population. Lower education has, in several studies, been attributed to a poor knowledge of CC and HPV in the continent (46–48). This is an issue of concern requiring attention. It has been reported in China that women who are well educated are more willing to undergo CC screening (49). Just as reported in Ghana (30) and other African countries (48, 50, 51), an increased health literacy could have a significant effect on CC awareness and screening. The association of income with CC and HPV knowledge corroborates earlier reports from Kenya and Botswana (46, 52). Poor knowledge of CC and HPV among women with low income could be explained by inability to assess healthcare and the media which are the main sources of health information in the communities.
The study highlights some specific gaps in knowledge and awareness for consideration. For instance, with regards to knowledge of the common screening methods for cervical cancer used in Ghana, only 9 (3.3%) of the participants knew of the Pap test and Visual Inspection with Acetic Acid (VIA). This finding contradicted those of Heena etal. (33) and Owoeye and Ibrahim (45) who reported over 50% awareness of cervical cancer screening methods in Saudi Arabia and Nigeria, respectively. The later studies involved a population of health workers in an urban area in Saudi Arabia (33) and students and staff of a tertiary institution in an urban area in Nigeria (45). This suggests that peer-led enhanced health education in schools, working areas and the community at large helps create adequate awareness among populations in different geographical locations (30, 53, 54).
In the preceding 5 years, only 3 (1.09%) of the participants have had cervical cancer screening. This finding could be attributed to the absence of screening centres in the communities and difficulty in accessing those outside the communities because of distance and limited financial resources to cater for the cost of screening and management. In Ghana, there are a few public and private healthcare facilities that actively provide CC screening services and these are done at a cost to patients because this service is not covered by the National Health Insurance Scheme (1). Low patronage of the screening services among women in Ghana has been attributed to low financial resources, low education, lack of national CC screening programmes and low levels of satisfaction and involvement in the health system (6). Contrary to our study, a relatively increased rate of screening was reported in Gabon and Nigeria (22, 55) and this was attributed to recommendations by physicians. To improve the patronage of CC screening among women, there should be the provision of adequate infrastructure and resources, trained health personnel, the inclusion of CC screening on the NHIS, provision of adequate education and well-laid policies on regular CC screening nationwide, especially in the rural communities (17, 41, 56).
In our study, the primary sources of knowledge of CC and HPV were the broadcasting media (TV and radio stations), health workers, family and friends, social media, the internet and others such as schools and churches. This finding was similar to that of an earlier study in Uganda (57) and it could be due to the similarity in the mode of dissemination of information in our areas of study. Integration of related health awareness themes into television and radio programmes, especially in the local dialects, may widely contribute to the awareness of CC in rural communities. It has been reported that talks at organised places and platforms improve the awareness of the infection and disease (58, 59); however, an increased screening rate could be achieved with the broadcasting of educational movies related to the disease (59).
Concerning lifestyles which may predispose participants to infection, we observed that, the mean age of the women at sexual debut was 18.5 ± 2.39 years with almost one-third having their sexual debut before 18 years. This finding was similar to that of other studies in Ghana and Nigeria (60, 61). Again, over 60% of the participants (180/274, 65.7%) have had either two or three-lifetime sexual partners. Sexual intercourse is important for HPV transmission (62, 63). HPV infection and its persistence have been linked with an early age of sexual debut and multiple sexual partners (64–67). It was observed that having a higher number of lifetime sexual partners was associated with a good knowledge of CC. It is possible that these women have experienced CC or HPV symptoms and had sought for medical attention in the past. It has earlier been reported in Tanzania that women with increased number of lifetime sexual partners are more likely to take CC screening services (68). We also observed increased use of hormonal contraceptives among participants, as well as multiparity among a larger portion of the studied population. Contraceptive utilisation and parity have earlier been linked with HPV and CC (66, 67, 69). Educational campaigns should focus on educating women on how these risky behaviours puts them at risk of having CC.
Strengths and limitations of the study
This study is the first to highlight a gap in knowledge of CC and HPV with consequently reduced screening among rural populations in the Akyemansa District of Ghana. However, the study is not without limitations and therefore the findings should be interpreted considering these limitations. First, the sampling technique was likely to introduce some level of sampling bias. Some communities were not selected because of the convenient nature in which communities were selected for the study. The findings of this study may not represent that of communities which were not included in the study. Secondly, the small sample size limits the representativeness, generalizability and validity of the findings. Prospective follow-up research with a larger sample size would be more useful in determining the level of knowledge of HPV and cervical cancer in the district. By interviewing participants, social desirability bias is possible, particularly in answering questions on sexual history, use of contraceptives, alcohol intake and smoking history. Because of the sensitive nature of some of the questions it is possible that some information provided was under or over reported due to personal reasons.
Conclusion
We report that adult women in the rural parts of the Eastern Region of Ghana have limited knowledge and awareness of HPV infection and cervical cancer, as well as the screening and preventive tools available. Consequently, most of the women have certain lifestyle behaviours that predispose them to the risk of acquiring HPV infection and the subsequent development of cervical cancer. It is recommended that extensive educational campaigns on cervical cancer and its prevention be organised to increase knowledge and awareness in the rural communities of the country. Finally, the government should adopt and implement policies that would ensure increased patronage and availability of cervical cancer screening services in the area.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board, University of Cape Coast (UCCIRB/CHAS/2019/30). The patients/participants provided their written informed consent to participate in this study.
Author contributions
SE-B, LM, SK-A and SE developed the concept and design of the study. LM, BA-F and EA engaged in participants’ recruitment, and data collection. LM and ME engaged in data entry and analysis, and initial manuscript writing. SE-B, ME, SK-A and SE were involved with the review of data and interpretation of research findings, and review of the manuscript. All authors reviewed the manuscript and accepted the final version for submission.
Funding
This study was mainly supported by personal funds from the authors.
Acknowledgments
Special appreciation goes to the traditional leaders in the Akyemansa District for their invaluable support. Many thanks also, to the trained female assistants- Josephine Nketsiah, Alberta Kwatsikor and Archleana Odofley Nortey – for their effortless assistance with the data collection.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Stuart A, Obiri-Yeboah D, Adu-Sarkodie Y, Hayfron-Benjamin A, Akorsu AD, Mayaud P. Knowledge and experience of a cohort of HIV-positive and HIV-negative ghanaian women after undergoing human papillomavirus and cervical cancer screening. BMC Womens Health (2019) 19:123. doi: 10.1186/s12905-019-0818-y
2. Handlogten KS, Molitor RJ, Roeker LE, Narla NP, Bachman MJ, Quayson S, et al. Cervical cancer screening in Ghana, west Africa: prevalence of abnormal cytology and challenges for expanding screening. Int J Gynecol Pathol (2014) 33:197–202. doi: 10.1097/PGP.0b013e318298a9e6
3. Mengesha A, Messele A, Beletew B. Knowledge and attitude towards cervical cancer among reproductive age group women in gondar town, north West Ethiopia. BMC Public Health (2020) 20:209. doi: 10.1186/s12889-020-8229-4
4. Song D, Li H, Li H, Dai J. Effect of human papillomavirus infection on the immune system and its role in the course of cervical cancer. Oncol Lett (2015) 10:600–6. doi: 10.3892/ol.2015.3295
5. Binka C, Doku DT, Awusabo-Asare K. Experiences of cervical cancer patients in rural Ghana: An exploratory study. PloS One (2017) 12:e0185829. doi: 10.1371/journal.pone.0185829
6. Calys-Tagoe BN, Aheto JM, Mensah G, Biritwum RB, Yawson AE. Cervical cancer screening practices among women in Ghana: evidence from wave 2 of the WHO study on global AGEing and adult health. BMC Women's Health (2020) 20:1–9. doi: 10.1186/s12905-020-00915-9
7. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin (2021) 71:209–49. doi: 10.3322/caac.21660
8. Awua A, Sackey S, Osei Y, Asmah R, Wiredu EJIA. Prevalence of human papillomavirus genotypes among women with cervical cancer in Ghana. Cancer (2016) 11:4. doi: 10.1186/s13027-016-0050-4
9. Nartey Y, Hill PC, Amo-Antwi K, Nyarko KM, Yarney J, Cox B. Cervical cancer in the greater Accra and Ashanti regions of Ghana. J Global Oncol (2017) 3:782–90. doi: 10.1200/JGO.2016.005744
10. Ampofo AG, Adumatta AD, Owusu E, Awuviry-Newton K. A cross-sectional study of barriers to cervical cancer screening uptake in Ghana: An application of the health belief model. PloS One (2020) 15:e0231459. doi: 10.1371/journal.pone.0231459
11. Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol (1999) 189:12–9. doi: 10.1002/(SICI)1096-9896(199909)189:1%3C12::AID-PATH431%3E3.0.CO;2-F
12. Schiffman M, Castle PE, Jeronimo J, Rodriguez AC, Wacholder S. Human papillomavirus and cervical cancer. Lancet (2007) 370:890–907. doi: 10.1016/S0140-6736(07)61416-0
13. Traore IMA, Zohoncon TM, Dembele A, Djigma FW, Obiri-Yeboah D, Traore G, et al. Molecular characterization of high-risk human papillomavirus in women in bobo-dioulasso, Burkina Faso. BioMed Res Int (2016) 2016:1–6. doi: 10.1155/2016/7092583
14. Palefsky JM. Human papillomavirus-related disease in men: Not just a women's issue. J Adolesc Health (2010) 46:S12–9. doi: 10.1016/j.jadohealth.2010.01.010
15. Deligeoroglou E, Giannouli A, Athanasopoulos N, Karountzos V, Vatopoulou A, Dimopoulos K, et al. HPV infection: Immunological aspects and their utility in future therapy %. J Infect Dis Obstetrics Gynecology (2013) 2013:9. doi: 10.1155/2013/540850
16. Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in elmina, southern Ghana. Int J women's Health (2015) 7:31. doi: 10.2147/IJWH.S71797
17. Binka C, Nyarko SH, Awusabo-Asare K, Doku DT. Barriers to the uptake of cervical cancer screening and treatment among rural women in Ghana. BioMed Res Int (2019) 2019:6320938. doi: 10.1155/2019/6320938
18. Reichheld A, Mukherjee PK, Rahman SM, David KV, Pricilla RA. Prevalence of cervical cancer screening and awareness among women in an urban community in south India–a cross sectional study. J A. O. G. H. (2020) 86:1–7. doi: 10.5334/aogh.2735
19. Mohammed KA, Subramaniam DS, Geneus CJ, Henderson ER, Dean CA, Subramaniam DP, et al. Rural-urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med (2018) 109:39–43. doi: 10.1016/j.ypmed.2018.01.016
20. Zahnd WE, James AS, Jenkins WD, Izadi SR, Fogleman AJ, Steward DE, et al. Rural–urban differences in cancer incidence and trends in the united states. Cancer Epidemiol Biomarkers Prev (2018) 27:1265–74. doi: 10.1158/1055-9965.EPI-17-0430
21. Shabani LW, Moodley M, Naidoo TD. Knowledge, awareness and attitude towards human papilloma virus vaccine in a resource-constrained setting: a comparison between an urban and rural population in south Africa. South Afr J Gynaecological Oncol (2019) 11:1–6. doi: 10.1080/20742835.2019.1589183
22. Assoumou SZ, Mabika BM, Mbiguino AN, Mouallif M, Khattabi A, Ennaji MM. Awareness and knowledge regarding of cervical cancer, pap smear screening and human papillomavirus infection in gabonese women. BMC Women’s Health (2015) 15:1–7. doi: 10.1186/s12905-015-0193-2
23. Gultekin M, Ramirez PT, Broutet N, Hutubessy R. World health organisation call for action to eliminate cervical cancer globally. Int J Gynaecol Cancer-BMJ (2020) 0:2. doi: 10.1136/ijgc-2020-001285
24. GAP. Stronger collaboration, better health: 2020 progress report on the global action plan for healthy lives and well-being for all. Geneva: WHO (2020).
25. Canfell K, Kim JJ, Brisson M, Keane A, Simms KT, Caruana M, et al. Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet (2020) 395:591–603. doi: 10.1016/S0140-6736(20)30157-4
26. World Health Organization. Draft global strategy towards the elimination of cervical cancer as a public health problem (2019). Available at: https://www.who.int/docs/default-source/cervical-cancer/cerv-cancer-elimn-strategy-16dec-12pm.pdf (Accessed Dec 16, 2019).
27. Pierz AJ, Randall TC, Castle PE, Adedimeji A, Ingabire C, Kubwimana G, et al. A scoping review: Facilitators and barriers of cervical cancer screening and early diagnosis of breast cancer in Sub-Saharan African health settings. Gynecologic Oncol Rep (2020) 33:100605. doi: 10.1016/j.gore.2020.100605
28. Abiodun OA, Olu-Abiodun OO, Sotunsa JO, Oluwole FA. Impact of health education intervention on knowledge and perception of cervical cancer and cervical screening uptake among adult women in rural communities in Nigeria. BMC Public Health (2014) 14:1–9. doi: 10.1186/1471-2458-14-814
29. Koç Z, Özdes EK, Topatan S, Çinarli T, Sener A, Danaci E, et al. The impact of education about cervical cancer and human papillomavirus on women's healthy lifestyle behaviors and beliefs: using the PRECEDE educational model. Cancer Nurs (2019) 42:106–18. doi: 10.1097/NCC.0000000000000570
30. Ebu NI, Amissah-Essel S, Asiedu C, Akaba S, Pereko KA. Impact of health education intervention on knowledge and perception of cervical cancer and screening for women in Ghana. BMC Public Health (2019) 19:1505. doi: 10.1186/s12889-019-7867-x
31. Ghana Statistical Service. 2010 population and housing census: District analytical report - akyemansa district. Accra, Ghana: Ghana Statistical Service (2014).
33. Heena H, Durrani S, Alfayyad I, Riaz M, Tabasim R, Parvez G, et al. Knowledge, attitudes, and practices towards cervical cancer and screening amongst female healthcare professionals: A cross-sectional study. J Oncol (2019) 2019:5423130. doi: 10.1155/2019/5423130
34. Jassim G, Obeid A, Al Nasheet HA. Knowledge, attitudes, and practices regarding cervical cancer and screening among women visiting primary health care centres in Bahrain. BMC Public Health (2018) 18:128. doi: 10.1186/s12889-018-5023-7
35. Yu C, Rymer J. Women's attitudes to and awareness of smear testing and cervical cancer. Br J Family Plann (1998) 23:127–33.
36. WHO. WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention, second edition. Geneva: WHO (2021).
37. Wang W, Arcà E, Sinha A, Hartl K, Houwing N, Kothari S. Cervical cancer screening guidelines and screening practices in 11 countries: A systematic literature review. Prev Med Rep (2022) 28:101813. doi: 10.1016/j.pmedr.2022.101813
38. Kadian L, Gulshan G, Sharma S, Kumari I, Yadav C, Nanda S, et al. A study on knowledge and awareness of cervical cancer among females of rural and urban areas of haryana, north India. J Cancer Education. (2020) 36:844–9. doi: 10.1007/s13187-020-01712-6
39. Ebu NI, Mupepi SC, Siakwa MP, Sampselle CM. Knowledge, practice, and barriers toward cervical cancer screening in elmina, southern Ghana. Int J women's Health (2014) 7:31–9. doi: 10.2147/IJWH.S71797
40. Hoque E, Hoque M. Knowledge of and attitude towards cervical cancer among female university students in south Africa. South Afr J Epidemiol Infection (2009) 24:21–4. doi: 10.1080/10158782.2009.11441335
41. Ning Y-E, Liu Y, Xu X-Y, Zhang X-Y, Wang N, Zheng L-Q. Knowledge of cervical cancer, human papilloma virus (HPV) and HPV vaccination among women in northeast China. J Cancer Education. (2019) 35:1197–205. doi: 10.1007/s13187-019-01582-7
42. Al Meer F, Aseel M, Al Khalaf J, Al Kuwari M, Ismail M. Knowledge, attitude and practices regarding cervical cancer and screening among women visiting primary health care in Qatar. J E.-E. M. H. J (2011) 17:855–61. doi: 10.26719/2011.17.11.856
43. Tran NT, Choe SI, Taylor R, Ko WS, Pyo HS, So HC. Knowledge, attitude and practice (KAP) concerning cervical cancer and screening among rural and urban women in six provinces of the democratic people's republic of Korea. J A. P. J C. P (2011) 12:3029–33.
44. Baloch Z, Yasmeen N, Li Y, Zhang W, Lu H, Wu X, et al. Knowledge and awareness of cervical cancer, human papillomavirus (HPV), and HPV vaccine among HPV-infected Chinese women. Med Sci Monit (2017) 23:4269–77. doi: 10.12659/MSM.903370
45. Owoeye I, Ibrahim I. Knowledge and attitude towards cervical cancer screening among female students and staff in a tertiary institution in the Niger delta. Int J Med Biomed Res (2013) 2:48–56. doi: 10.14194/ijmbr.219
46. Ngune I, Kalembo F, Loessl B, Kivuti-Bitok LW. Biopsychosocial risk factors and knowledge of cervical cancer among young women: A case study from Kenya to inform HPV prevention in Sub-Saharan Africa. PloS One (2020) 15:e0237745. doi: 10.1371/journal.pone.0237745
47. Ali F, Kuelker R, Wassie B. Understanding cervical cancer in the context of developing countries. Ann Trop Med Public Health (2012) 5:3–15. doi: 10.4103/1755-6783.92871
48. Strohl AE, Mendoza G, Ghant MS, Cameron KA, Simon MA, Schink JC, et al. Barriers to prevention: knowledge of HPV, cervical cancer, and HPV vaccinations among African American women. Am J Obstetrics Gynecology (2015) 212:65.e1–5. doi: 10.1016/j.ajog.2014.06.059
49. Jia Y, Li S, Yang R, Zhou H, Xiang Q, Hu T, et al. Knowledge about cervical cancer and barriers of screening program among women in wufeng county, a high-incidence region of cervical cancer in China. PloS One (2013) 8:e67005. doi: 10.1371/journal.pone.0067005
50. Kangmennaang J, Onyango EO, Luginaah I, Elliott SJ. The next Sub Saharan African epidemic? a case study of the determinants of cervical cancer knowledge and screening in Kenya. Soc Sci Med (2018) 197:203–12. doi: 10.1016/j.socscimed.2017.12.013
51. Tsegay A, Araya T, Amare K, G Tsadik F. Knowledge, attitude, and practice on cervical cancer screening and associated factors among women aged 15-49 years in adigrat town, northern ethiopi: A community-based cross-sectional study. Int J Womens Health (2020) 12:1283–98. doi: 10.2147/IJWH.S261204
52. Mcfarland DM. Cervical cancer and pap smear screening in Botswana: knowledge and perceptions. Int Nurs Rev (2003) 50:167–75. doi: 10.1046/j.1466-7657.2003.00195.x
53. Poudel K, Sumi N, Yano R. Impact of peer-led cancer education program on knowledge, health beliefs, practice, and self-esteem among pairs of Nepalese high-school students and their knowledge-sharing partners. Healthcare (2021) 9:1–16. doi: 10.3390/healthcare9010064
54. Mbachu C, Dim C, Ezeoke U. Effects of peer health education on perception and practice of screening for cervical cancer among urban residential women in south-east Nigeria: a before and after study. BMC Women's Health (2017) 17:41. doi: 10.1186/s12905-017-0399-6
55. Okunowo AA, Daramola ES, Soibi-Harry AP, Ezenwankwo FC, Kuku JO, Okunade KS, et al. Women's knowledge of cervical cancer and uptake of pap smear testing and the factors influencing it in a Nigerian tertiary hospital. J Cancer Res Pract (2018) 5:105–11. doi: 10.1016/j.jcrpr.2018.02.001
56. Nartey Y, Hill P, Amo-Antwi K, Asmah R, Nyarko K, Yarney J, et al. Recommendations for cervical cancer prevention and control in Ghana: public education and human papillomavirus vaccination. Ghana Med J (2018) 52:94–102. doi: 10.4314/gmj.v52i2.6
57. Mukama T, Ndejjo R, Musabyimana A, Halage AA, Musoke D. Women’s knowledge and attitudes towards cervical cancer prevention: a cross sectional study in Eastern Uganda. BMC Women's Health (2017) 17:9. doi: 10.1186/s12905-017-0365-3
58. Rosser J, Njoroge B, Huchko M. Changing knowledge, attitudes, and behaviors regarding cervical cancer screening: The effects of an educational intervention in rural Kenya. Patient Educ Couns (2015) 98:884–9. doi: 10.1016/j.pec.2015.03.017
59. Gatumo M, Gacheri S, Sayed A-R, Scheibe A. Women’s knowledge and attitudes related to cervical cancer and cervical cancer screening in isiolo and tharaka nithi counties, Kenya: a cross-sectional study. BMC Cancer (2018) 18:745. doi: 10.1186/s12885-018-4642-9
60. Obiri-Yeboah D, Akakpo PK, Mutocheluh M, Adjei-Danso E, Allornuvor G, Amoako-Sakyi D, et al. Epidemiology of cervical human papillomavirus (HPV) infection and squamous intraepithelial lesions (SIL) among a cohort of HIV-infected and uninfected ghanaian women. BMC Cancer (2017) 17:688. doi: 10.1186/s12885-017-3682-x
61. Durowade K, Osagbemi G, Salaudeen A, Musa O, Akande T, Babatunde O, et al. Prevalence and risk factors of cervical cancer among women in an urban community of kwara state, north central Nigeria. J Prev Med hyg (2012) 53:213–9.
62. KrüGer Kjaer S, Chackerian B, Van Den Brule AJ, Svare EI, Paull G, Walbomers JM, et al. High-risk human papillomavirus is sexually transmitted: evidence from a follow-up study of virgins starting sexual activity (intercourse). Cancer Epidemiol Biomarkers Prev (2001) 10:101–6.
63. Houlihan CF, Baisley K, Bravo IG, Kapiga S, De Sanjosé S, Changalucha J, et al. Rapid acquisition of HPV around the time of sexual debut in adolescent girls in Tanzania. Int J Epidemiol (2016) 45:762–73. doi: 10.1093/ije/dyv367
64. De Sanjose S, Cortés X, Méndez C, Puig-Tintore L, Torné A, Roura E, et al. Age at sexual initiation and number of sexual partners in the female Spanish population: Results from the AFRODITA survey. Eur J Obstetrics Gynecology Reprod Biol (2008) 140:234–40. doi: 10.1016/j.ejogrb.2008.04.005
65. Antonsson A, De Souza MM, Panizza BJ, Whiteman DC. Sexual debut and association with oral human papillomavirus infection, persistence and oropharyngeal cancer–an analysis of two Australian cohorts. Int J Cancer. (2022) 151(5):764–9. doi: 10.1002/ijc.33986
66. Lukac A, Sulovic N, Smiljic S, Ilic AN, Saban O. The prevalence of the most important risk factors associated with cervical cancer. Materia socio-medica (2018) 30:131. doi: 10.5455/msm.2018.30.131-135
67. Liu Z-C, Liu W-D, Liu Y-H, Ye X-H, Chen S-D. Multiple sexual partners as a potential independent risk factor for cervical cancer: a meta-analysis of epidemiological studies. Asian Pacific J Cancer Prev (2015) 16:3893–900. doi: 10.7314/APJCP.2015.16.9.3893
68. Kileo NM, Michael D, Neke NM, Moshiro C. Utilization of cervical cancer screening services and its associated factors among primary school teachers in ilala municipality, dar es salaam, Tanzania. BMC Health Serv Res (2015) 15:552. doi: 10.1186/s12913-015-1206-4
Keywords: cervical cancer, human papillomavirus (HPV), rural, knowledge, awareness, infection
Citation: Ken-Amoah S, Blay Mensah LB, Eliason S, Anane-Fenin B, Agbeno EK, Essuman MA and Essien-Baidoo S (2022) Poor knowledge and awareness of human papillomavirus and cervical cancer among adult females in rural Ghana. Front. Trop. Dis 3:971266. doi: 10.3389/fitd.2022.971266
Received: 16 June 2022; Accepted: 17 October 2022;
Published: 03 November 2022.
Edited by:
Deepa Dongarwar, Baylor College of Medicine, United StatesReviewed by:
Surajudeen Abdulrahman, Health Education England East Midlands, United KingdomKorede Yusuf, Adelphi University, United States
Copyright © 2022 Ken-Amoah, Blay Mensah, Eliason, Anane-Fenin, Agbeno, Essuman and Essien-Baidoo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Samuel Essien-Baidoo, c2Vzc2llbi1iYWlkb29AdWNjLmVkdS5naA==
 Sebastian Ken-Amoah
Sebastian Ken-Amoah Loretta Betty Blay Mensah
Loretta Betty Blay Mensah Sebastian Eliason3
Sebastian Eliason3 Mainprice Akuoko Essuman
Mainprice Akuoko Essuman