
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
OPINION article
Front. Trop. Dis. , 20 September 2022
Sec. Tropical Disease Epidemiology and Ecology
Volume 3 - 2022 | https://doi.org/10.3389/fitd.2022.827102
Leprosy is an infectious disease caused by the bacillus Mycobacterium leprae (1). Leprosy patients can experience deformities that affect sight, touch, and manual dexterity. Macules, papules, and nodules are prevalent among other skin lesions (2). Along with these symptoms, leprosy patients experience immense stigma and discrimination, also called leprostigma.
Leprosy can be cured using a combination of three antibiotics - rifampicin, clofazimine, and dapsone - widely known as multidrug therapy (MDT). This treatment, found in 1970, was officially recommended by the World Health Organization (WHO) in 1981 (3, 4). As a result of this discovery, in the year 2000, the global prevalence rate of leprosy cases reduced to <1 case per 10,000 population (5). However, leprostigma is still active in society, and in some countries, discriminatory leprosy-related policies are yet to be amended (6). Negligence has brought even more leprostigma, misconceptions, and deterrence to patient management and life quality in both endemic and non-endemic countries (7), and due to the COVID-19 pandemic, leprosy management has been further harmed due to a decrease in diagnosis, treatment difficulties, increase in stigma, and increased susceptibility of leprosy patients to COVID-19 (8–23).
There are some published papers on leprosy and leprostigma, but reviews on the present-day situation, especially the impacts of COVID-19, are lacking. This paper aims to provide a thorough overview of past leprosy and leprostigma, as well as highlight the present-day situation regarding patient management, discriminatory governmental policies, and impacts of the COVID-19 pandemic. An updated overview will help ensure proper care of patients in light of the recent pandemic and underscore the continued need for interest in leprosy management despite its perceived unimportance.
Leprosy has existed for many centuries, but its origins are unknown (24). The disease has most likely spread around the world by human migrations such as relocation or colonization (25).
The origin of the term, leprosy, comes from biblical translations of Hebrew into Greek. The Hebrew word, “tsara’ath,” translated as “leprosy” in the authorized version of the Old Testament, is a non-scientific term that indicates ritualistic defilement instead of a specific skin disease (26). The Bible presents leprosy as a symbol that aggregates harmful consequences of impious behavior (27). Due to these presentations, leprosy was commonly misunderstood as hereditary and incurable and was considered as “a divine punishment or curse,” and this harmful image associated with the disease has resulted in inhumane treatments of patients such as leprosariums and mass executions (1, 24, 28, 29).
After the discovery of the bacillus M. Leprae as the cause of leprosy, countries set aims to eliminate leprosy. By providing MDT, an efficacious treatment based on the bacillus, to all government health facilities, the WHO successfully reduced the global prevalence of the disease (3, 4). However, complete elimination has yet to be reached as areas of high endemicity remain in many countries. For instance, in India, a country with more than 60% of the global burden of leprosy, the annual new case detection rate and prevalence rate per 10,000 people have remained nearly non-decreasing at 2.0 and 1.4, respectively, since 2007 (7).
One of the biggest obstacles in reaching the complete elimination of leprosy is universal leprostigma. The main sources of leprostigma are religious and linguistic stereotypes, misconceptions, and fear of people with deformities.
Religious and linguistic stereotypes come from many sources, one being the persistence of discriminatory language, as classified by the UN special rapporteur (30). Across diverse cultures, the word ‘leprosy’ was metaphorically associated with sins, curses or punishments, or evil spirits (26, 31). This association led to separate mass funerals for leprosy patients in Middle Age Europe and the mandatory attendance of exorcist performances for patients in South Korea (32, 33).
Other causes of the leprostigma are misconceptions that leprosy is hereditary and incurable and that deformities have infectivity. Research after the discovery of M. Leprae found that over 95% of the human population are naturally immune to leprosy, that over months of contact with an active leprosy patient is needed for a slim chance of infection, and that cured leprosy patients are no longer infectious (34). Yet, ignorance continued to associate deformity with infectivity, directly aiming leprostigma toward patients with irreversible deformities. Cured but deformed patients were found to often doubt their own infectivity, and some leprosy patients without deformities chose to dissociate themselves from those with deformities (35). Likewise, although leprosy was found to be nonhereditary and curable, children of leprosy patients were often denied admission to schools for being potential leprosy patients (7, 36).
Leprostigma led to the creation of thousands of leprosariums around the world. The treatment of patients in these leprosariums was extremely inhumane. Instead of treating the patients in a hospital-like setting, leprosariums considered the residents as criminals in prison (37).
In Japan, starting in the early 1900s, leprosarium doctors sterilized men and forced pregnant women to undergo abortions (38). Similarly, from the early 1900s, South Korean laws forced many leprosy patients to Sorok Island, the only leprosarium in South Korea. Surgeries and human experiments were performed on the patients without consent, and as Sorok Island was not a self-sufficient place, the increased inmates and lack of food led to a drastically increased death toll of the patients over the years (39).
Not all of the patients resided in these leprosariums, but the lives of those living among the uninfected were not much better (40). In Korea, patients committed suicide and killed their children to prevent them from experiencing leprostigma. Community members murdered patients, associating the disease with sins and evil and fearing the possibility of infection. In some extreme cases, patients practiced cannibalism, believing it was a cure (39). Although South Korea had comparatively detailed written records of leprostigma, many other countries with endemic history may have experienced the same severity.
As patients became isolated, the lack of interaction between people with and without leprosy caused even more fear and misconceptions. A study done by Asampong et al. (41) found that in the beginning, caregivers of cured leprosy patients in health facilities feared eating near patients because of the false belief that patients remain infective even after treatment. Moreover, some caregivers admitted that the “scary deformities’’ made them feel uncomfortable eating near or being around the patients (41 p. 5). The initial apprehension dissipated as the patients and caregivers interacted, and the caregivers came to eat near and even share food with the patients (41). This change shows that leprostigma will decrease if the leprosy-affected are given the opportunity to interact more freely with the unaffected.
Surprisingly, public health interventions to aid leprosy elimination may have also contributed to the formulation of leprostigma and fear of leprosy in the present day. According to a literature review performed in 2014 by Sermrittirong and Van Brakel (42), a historical fear of leprosy instilled in the public mind by Information, Education, and Communication (IEC) campaigns through the use of frightening symptom images and propaganda to increase self-reports and diagnosis may have further stigmatized the leprosy-affected. Moreover, by implying the prevalence of leprosy only in areas of low socioeconomic status, health education systems of the United States and western Europe may have further categorized the disease while raising public awareness (43).
With the aim to reduce these misconceptions and leprostigma, Brazil and South Korea changed the terminology of the disease on national levels. In 1995, the federal law of Brazil officially prohibited the use of the word ‘leprosy’ in all documents and every institutional practice, and in 1999, the National Assembly of Korea enforced the change from ‘leprosy’ and ‘lepers’ to ‘Hansen’s disease’ and ‘patients with Hansen’s disease,’ respectively (32, 44). Worth noting, this review uses the medical term ‘leprosy’ instead of ‘Hansen’s disease’ for better understanding as only some countries recommend the terminology change.
Leprostigma reduction programs implemented in some countries include integrating leprosy-related services to general health education and care to reduce the isolation and differentiation of patients from society. By providing leprosy-related care close to patients’ homes, such programs hope to slowly connect and integrate leprosy patients to other patients with diseases (45).
Despite these attempts, misconceptions and leprostigma are still present. In 2003, a study was conducted in Delhi to measure public awareness and attitudes regarding the disease (46). Out of the 104 people interviewed, only 44.20% knew the cause of the disease and only 63.10% were aware that the disease is curable. Moreover, 54.80% felt reluctant to employ leprosy-affected people, and 61.50% favored patients to live within bounds (Table 1). Sermrittirong and Van Brakel (42) found that one possible reason for this continuation of leprostigma and misconceptions may be that most programs to resolve leprostigma are generalized, even though stigma differs for every society depending on the social history, cultural meaning, individuals involved, and prevalent conditions. In another review, Semrittirong et al. (47) recommended that such campaigns and interventions should be implemented only after a thorough study of the society.
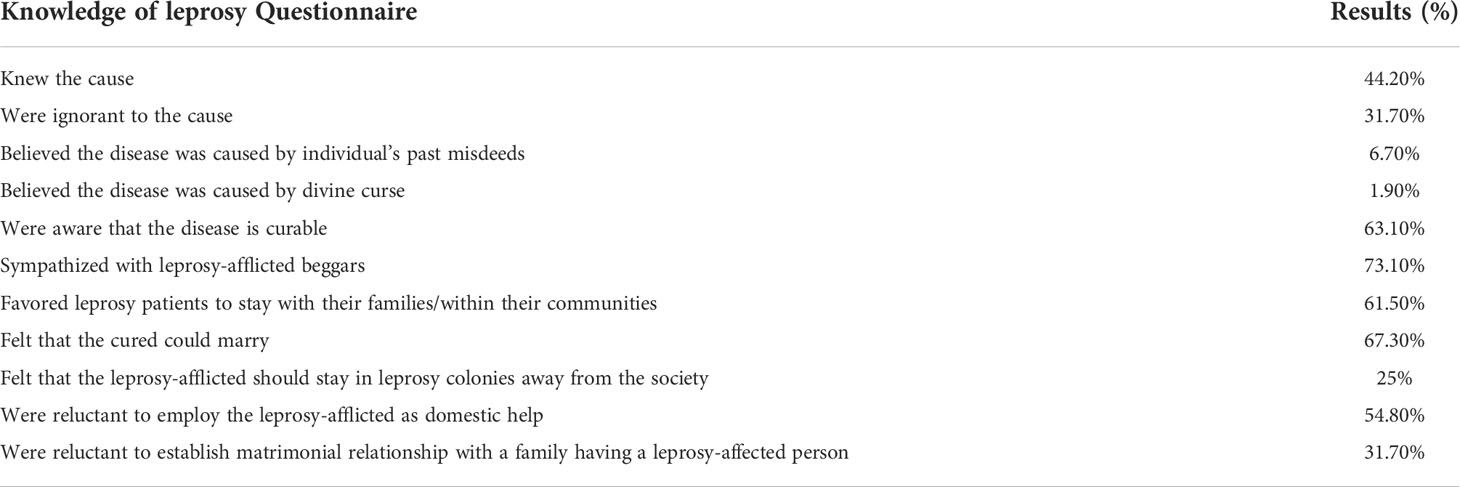
Table 1 People’s perception and knowledge of leprosy in Delhi in 2003 (46).
Leprostigma in society causes many patients with active leprosy to delay or avoid treatment (35). In Kaur and Ramesh’s research (48), nearly 77.4% of female leprosy patients in Delhi were afraid of receiving confronting questions about leprosy. Furthermore, Pelizzari et al. (49) found that some medical professionals even advised their patients to avoid discussing leprosy in public. These actions of avoiding mentioning or admitting leprosy is an obstacle to improving the public understanding of leprosy and may delay the identification of many leprosy patients (49, 50). This delay is especially harmful to the future of leprosy patients since a lack of treatment in the early stages may worsen symptoms, increase complications and transmissions to those in close contact, and increase the risk of deformities (50).
In General Health Questionnaire (GHQ)-based studies, leprosy patients scored highly (a higher score indicates worse mental health condition and quality of life), and hence were prone to experiencing psychiatric morbidity (51). Among the observed psychiatric conditions, depression (up to 71%), suicide (attempts) (around 33%), and anxiety disorders (10 to 20%) were the most frequently recorded. In addition to these diagnostic conditions, leprosy patients also had a higher identification of neuropsychiatric conditions and negative feelings such as sleep disorder and fear, respectively (51). Compared to other skin diseases, leprosy patients were more likely to suffer psychiatric disorders (52).
In a systematic review, Dijkstra et al. (53) evaluated the effect of gender on leprostigma and found significant gender inequality in leprostigma. Their results revealed that compared to males, leprostigma had a greater effect on female leprosy patients in health, psychological, and social domain; the lattermost was analyzed at family and community levels. Additionally, one study published after the previous systematic review evaluated the effect of gender on leprostigma in Korea (54). In this study, more women than men considered themselves disowned by and separated from their families. Regardless of the extent and subjectivity of the suffering, their findings indicate a greater frequency of discrimination among women solely due to their gender, similarly to the results of the previous systematic review.
The effect of leprostigma can extend to the families of the leprosy-affected. According to a recent systematic review that investigated the family members of leprosy patients regarding mental health, children of the leprosy-affected exhibit low self-esteem, worry about contracting the disease, higher depressive symptoms, and low health-related QoL (51). Another article evaluated the impact of leprosy, podoconiosis, and lymphatic filariasis on family quality of life in Northwest Ethiopia (55). This study found that both leprosy patients and their family members experienced frequent discrimination. Finding a partner and maintaining marriage proved especially difficult for leprosy-affected individuals, and this struggle even applied to their family members. Furthermore, the additional task of caring for the affected individual caused family members to experience stress, and at times, discontinue their education (55).
Compared to the past, the prevalence of leprosy has decreased prominently. Important research funding sources have stopped supporting leprosy research, perceiving it as eliminated (56). Because the disease now mainly affects only small populations in poor and developing countries, leprosy is categorized as a Neglected Tropical Disease, meaning it gains low interest in various medical industries (57). However, <1 case per 10,000 people, the threshold of elimination set by WHO, does not mean an absence of cases. Yet, the situations of those affected are often overlooked (56).
The prevalence of leprosy in India comes from the lack of health education and treatment delays (58). Patients are widely uninformed, and thus, prevented from reaching care at the appropriate times. Patients often ignore early symptoms of leprosy and visit healthcare facilities only when symptoms have lasted for months or years. The public health sector provides patients with free MDT and has been proven to give more accurate diagnoses than the private health sector (58). Nonetheless, most patients still visit the private health sector in their early stages of leprosy because government doctors are not easily accessible. This trend leads to more misdiagnoses and ineffective treatment, causing lasting complications for patients (58).
In India, the country with the most leprosy cases, patients still face leprostigma. According to the International Federation of Anti-Leprosy Associations (ILEP), as of June 2019, leprosy-affected people were denied their rights under 106 laws involving segregation, public transportation, marriage, and more (59). For example, under the Jammu and Kashmir Motor Vehicles Act, 1998, leprosy-affected people are “not eligible to obtain a driving license or drive a public service vehicle” (60). The unaltered discriminatory laws show that leprostigma remains to affect the lives of the patients.
Even in countries with a low prevalence of leprosy, leprosy patients are still neglected and stigmatized. According to research done in 2019, in South Korea, policies for leprosy patients fail to fully support those affected (39). The policies limit the subjects of protection to leprosy patients residing in facilities or settlements, even though the majority of the patients reside in open communities (Figure 1). Moreover, leprosy patients only receive 150,000 South Korean won (132.13 USD) per month from the government, which according to the patients, is not enough because the patients cannot support themselves due to age, discrimination, or disabilities (39). Furthermore, leprostigma is still evident in Korean society, just like in India. 37.05% of the interviewees answered that they experienced discrimination regarding their children’s marriage and a smaller percent answered that they recently experienced physical and verbal abuse (39). The comparison between countries with a high and low prevalence of leprosy suggests that the situation of leprosy patients and the extent of leprostigma is independent of the prevalence of the disease.
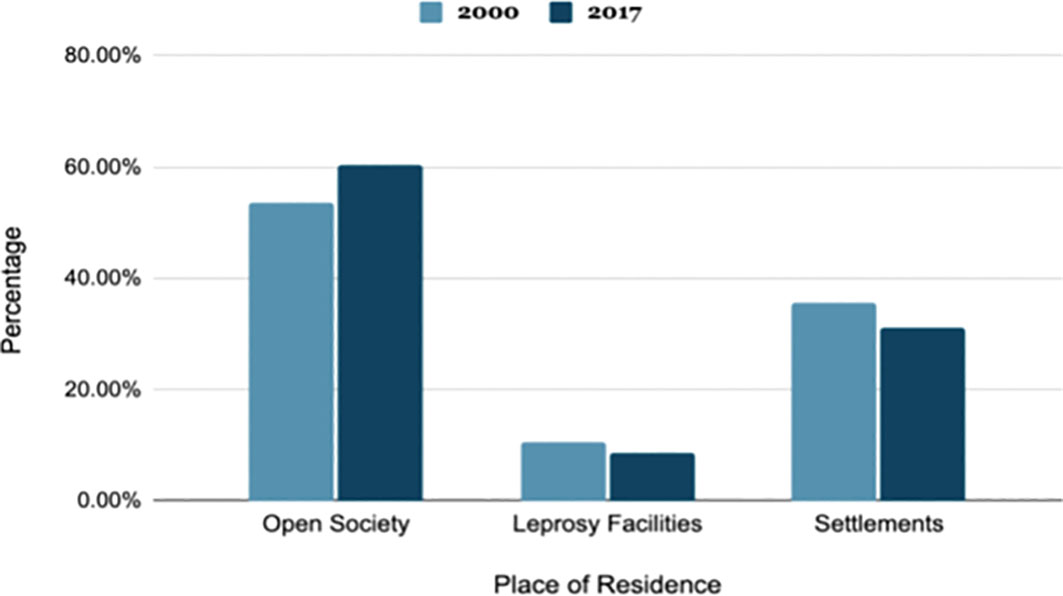
Figure 1 The residence of leprosy patients by percentage in South Korea in years 2000 and 2017 (39).
Recently, the COVID-19 pandemic has harmed the management of leprosy patients due to a decrease in diagnosis, treatment difficulties, increased susceptibility of leprosy patients to COVID-19 symptoms, and worsened leprostigma (8–23).
Numerous studies suggest a decreased diagnosis of leprosy after the emergence of COVID-19. Globally, WHO reports that the COVID-19 pandemic hindered the implementation of leprosy programs, causing a 37% reduction in new case detection between 2019 and 2020 (8). This reduction was especially significant in endemic countries. In a previous study by Da Paz et al. (9), the impact of the COVID-19 on the diagnosis of leprosy in Brazil was evaluated. They found a 41.4% reduction in the average number of leprosy cases from 2015 to 2019. Notably, this reduction was greater for patients below 15 years of age (-56.82%). Another study evaluating the impact of the COVID-19 on the diagnosis of leprosy in Brazil showed similar results (10). In this study, Matos et al. compared the new leprosy cases between January–September 2019 and January–September 2020. This comparison showed that leprosy diagnosis was reduced by 44.40% between these two durations. Especially when limiting the comparison period to April–September, the period after the emergence of COVID-19, the reduction was 51.10%, and a growing trend of COVID-19 cases and a downward trend of new leprosy cases were observed (10). In India, reports showed that there was a 13,730 decrease in newly reported cases of leprosy when comparing the periods between April-September of 2019 and 2022 (11). Compared to the previous year, this was a 63% drop in new diagnoses (11). Such a decrease in leprosy diagnosis may result in a hidden leprosy prevalence and continued transmission within the endemic community (10). Because late diagnosis causes severe and irreversible physical disabilities, the extent of leprostigma and psychosocial and physical hardships experienced by the leprosy-affected and their families are predicted to be worsened in the near future (10).
Along with the delay in diagnosis, COVID-19 has created difficulties in leprosy treatment. In countries with relatively weak health systems, hospital admissions and consultations are discouraged for most health conditions, including leprosy, due to their focus on responding to COVID-19 cases (12, 13). Such prioritization has prevented leprosy patients from easily accessing treatment, leaving them with severe physical disabilities (13). Moreover, due to the effectiveness of systemic corticosteroids in the treatment of COVID-19 complications, there has been a decreased availability of oral corticosteroids, which is used to treat those suffering from leprosy-associated reactions (14). Additionally, though related data is limited, COVID-19 and leprosy co-infection may increase the severity and frequency of leprosy-related complications (15).
Furthermore, leprosy patients may be more susceptible to COVID-19. Previous use of steroids and immunosuppressant therapy for leprosy-reaction management makes leprosy patients more susceptible to COVID-19 and vulnerable to its symptoms (14, 16). Moreover, physical disabilities and deformities like dry skin, as well as poverty resulting from social difficulties, prevents leprosy patients from maintaining the personal hygiene necessary to prevent COVID-19 infection and thus increase their chance of contracting COVID-19 (17). From a more organizational perspective, many parts of leprosy communities have been turned into field hospitals for COVID-19 patients and some of these communities do not have appropriate access to COVID-19 prevention information due to institutional neglect, thus increasing their susceptibility and vulnerability to COVID-19, especially due to their high population of elderly people who are more vulnerable to COVID-19 symptoms (17).
In a more societal context, COVID-19-related stigma and regulations may contribute to an increase in leprostigma and marginalizations. Numerous studies found that COVID-19 survivors, their families, and healthcare workers during the pandemic experienced heightened overall stigma and scrutiny due to public fear of possible infections due to encouragement of social isolation and improper understanding of the disease (18–20). Such COVID-19 stigmatizations, as proposed by Chopra and Arora (21), may further stigmatize and delay the diagnosis of other airborne diseases, suggesting a potential detriment to leprosy and the leprosy-affected. For patients co-infected with leprosy and COVID-19, the prevalent stigma for both diseases is thought to bring increased stigma (12). Moreover, studies suggest that public health interventions for COVID-19 like social distancing disproportionately marginalize already-stigmatized minorities like leprosy-affected communities and harm the psychological well-being of the leprosy-affected by further restricting their already-limited social lives, providing additional fear of infection (16), and increasing stigma (22, 23).
Leprosy has been ignored in many institutions due to its reduced global prevalence, especially in developed countries. However, patients and their families experience even more leprostigma and misconceptions due to this negligence (7). The present-day leprosy situation shows that regardless of the leprosy prevalence, affected individuals and their families in numerous countries suffer leprostigma, and that the COVID-19 pandemic has further worsened patient management and leprostigma. Therefore, more attention to leprosy management is needed to better support the patients.
In order to improve the present situation of leprosy and create a safe and supportive environment for those affected, the following endeavors can be taken:
First, governments in both endemic and non-endemic countries must review their health system to implement necessary alterations in light of the present-day situation. Specifically, countries with weak health systems like India must provide more health education and easier access to medical facilities to prevent the current diagnosis and treatment delays. Even in countries with effective health systems, COVID-19 prioritization has brought difficulties in diagnosis and treatment of leprosy patients. Accordingly, health-related agencies must construct a medical system to allocate sufficient treatment and provide easier access to medical facilities to current and prospective leprosy patients even during pandemics. This process will help identify and improve weaknesses in health systems and prepare for future health crises.
Second, research funding must continue. More research can be conducted to further identify the causes behind leprosy and leprostigma continuation, and how psychological and physical well-beings of patients can be improved to support their rehabilitation. Moreover, research on the relationship between COVID-19 and leprosy is needed. This research should identify methods to improve personal hygiene of leprosy patients to decrease susceptibility to infections, impacts of leprosy and COVID-19 co-infections, and how to treat co-infections like COVID-19 where treatment method(steroids) overlap. Furthermore, although WHO reports a decrease in leprosy diagnosis due to hinderance of leprosy program implementations, more research may be needed to determine if COVID-19 prevention policies like social distancing and mask mandates contributed by decreasing the leprosy infection incidence rate itself.
Third, to prevent leprostigma, leprosy interventions must be reviewed and specialized, leprosy-related policies must be removed, altered, or added, and COVID-19 stigma must be actively repressed. By reviewing leprosy interventions, previous unintentional instillation of fear, leprostigma, and categorizations of the disease in the public mind will be reduced. To continue, specializing stigma reduction programs for different areas with careful consideration of their culture, prevalent leprosy symptoms, and affected populations will increase its effectiveness. Furthermore, changing leprosy-related policies that discriminate against or neglect the leprosy-affected will help prevent leprostigma, and adding new, supportive policies will help protect the leprosy-affected in various circumstances. Likewise, COVID-19 stigma must be repressed as it may help decrease stigma and diseases of other airborne diseases, including leprostigma.
Lastly, more social interactions between the leprosy-affected and unaffected should be encouraged. As disease awareness increases and more patients become exposed in society, the prevalence of misconceptions and leprostigma will decrease and patients will experience smoother rehabilitation processes.
Leprosy and leprostigma is commonly believed as severe phenomena of the past, but they are still prevalent around the globe and have been worsened due to the recent COVID-19 pandemic. To improve the present situation and prevent its repetition, leprosy-related health systems, interventions, and policies must be reviewed and altered, research funding must continue, and social participation of the leprosy-affected must be encouraged.
The first author, HS, contributed to the study design, data collection, analysis, and writing. The corresponding author, YO, contributed to the writing. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Couto Dal Secco RG, França K, Castillo D, AlHarbi M, Lotti T, Fioranelli M, et al. A synopsis of the history of hansen’s disease. Wien Med Wochenschr (2017) 167(Suppl 1):27–30. doi: 10.1007/s10354-017-0590-2
2. Singh GP. Psychosocial aspects of hansen’s disease (leprosy). Indian Dermatol Online J (2012) 3(3):166–70. doi: 10.4103/2229-5178.101811
4. Smith CS, Aerts A, Saunderson P, Kawuma J, Kita E, Virmond M. Multidrug therapy for leprosy: A game changer on the path to elimination. Lancet Infect Dis (2017) 17(9):e293–7. doi: 10.1016/S1473-3099(17)30418-8
5. Reibel F, Cambau E, Aubry A. Update on the epidemiology, diagnosis, and treatment of leprosy. Med Mal Infect (2015) 45(9):383–93. doi: 10.1016/j.medmal.2015.09.002
6. Maymone MBC, Venkatesh S, Laughter M, Abdat R, Hugh J, Dacso MM, et al. Leprosy: Treatment and management of complications. J Am Acad Dermatol (2020) 83(1):17–30. doi: 10.1016/j.jaad.2019.10.138
7. Mohanty P, Naaz F, Bansal A, Kumar D, Gupta U. Challenges beyond elimination in leprosy. Int J Mycobacteriol (2017) 6(3):222. doi: 10.4103/ijmy.ijmy_70_17
8. Leprosy. In: World health organization. (2022) Geneva, Switzerland::World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/leprosy.
9. Da Paz WS, Souza M, Tavares D, Jesus AR, Santos AD, Carmo RF, et al. Impact of the COVID-19 pandemic on the diagnosis of leprosy in Brazil: an ecological and population-based study. Lancet Regional Health - Americas (2022) 9:100181. doi: 10.1016/j.lana.2021.100181
10. Matos TS, do Nascimento VA, do Carmo RF, Moreno de Oliveira Fernandes TR, de Souza CDF, da Silva TFA. Impact of the COVID-19 pandemic on the diagnosis of new leprosy cases in Northeastern Brazil, 2020. Int J Dermatol (2021) 60(8):1003–6. doi: 10.1111/ijd.15705
11. de Arquer GR, Kumar A, Singh RK, Satle N, Mamidi R, Biswas P. COVID-19 and leprosy new case detection in India. In: Leprosy review, vol. 92 1. (2021). p. 88–91 (Colchester, UK:Lepra). doi: 10.47276/lr.92.1.88
12. Fauziyah S, Putri S, Salma Z, Wardhani H, Hakim F, Sucipto T, et al. How should Indonesia consider its neglected tropical diseases in the COVID-19 ERA? hopes and challenges (review). Biomed Rep (2021) 14(6):1–10. doi: 10.3892/br.2021.1429
13. Covid-19: India’s most vulnerable battle two infectious diseases at once as total countrywide lockdown continues. Available at: https://www.lepra.org.uk/pr/COVID19_India%E2%80%99s_most_vulnerable_battle_two_infectious_diseases_at_once_as_total_countrywide_lockdown_continues.pdf.
14. Narang T, Bhardwaj A, Gupta SK, Suneetha S, Pradhan S, Agarwal P, et al. Updates on management of leprosy in the context of covid-19 pandemic: Recommendations by IADVL sig leprosy. Indian Dermatol Online J (2021) 12(7):24. doi: 10.1371/journal.pntd.0008460
15. Antunes DE, Goulart IM, Goulart LR. Will cases of leprosy reaction increase with COVID-19 infection? PloS Negl Trop Diseases (2020) 14(7):1–4. doi: 10.1371/journal.pntd.0008460
16. Mahato S, Bhattarai S, Singh R. Inequities towards leprosy-affected people: A challenge during COVID-19 pandemic. PloS Negl Trop Diseases (2020) 14(7):1–4. doi: 10.1371/journal.pntd.0008537
17. United Nations Human Rights- Special Procedures. Mandate of the special rapporteur on the elimination of discrimination against persons affected by leprosy and their family members- open letter on COVID-19 and leprosy to the UN member states (2020). Available at: https://www.ohchr.org/Documents/Issues/Leprosy/SR_leprosy_Open_letter_22May2020.pdf.
18. Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Diseases (2020) 20(7):782. doi: 10.1016/S1473-3099(20)30498-9
19. Economou M. Social distance in covid-19: Drawing the line between protective behavior and stigma manifestation. Psychiatriki (2021) 32(3):183–6. doi: 10.22365/jpsych.2021.025
20. Yuan Y, Zhao Y-J, Zhang Q-E, Zhang L, Cheung T, Jackson T, et al. Covid-19-related stigma and its sociodemographic correlates: A comparative study. Globalization Health (2021) 17(1):1–9. doi: 10.1186/s12992-021-00705-4
21. Chopra KK, Arora VK. Covid-19 and social stigma: Role of scientific community. Indian J Tuberculosis (2020) 67(3):284–5. doi: 10.1016/j.ijtb.2020.07.012
22. Smith RA, Hughes D. Infectious disease stigmas: Maladaptive in modern society. Communication Stud (2014) 65(2):132–8. doi: 10.1080/10510974.2013.851096
23. van Daalen KR, Cobain M, Franco OH, Chowdhury R. Stigma: The social virus spreading faster than covid-19. J Epidemiol Community Health (2021) 75(4):313–4. doi: 10.1136/jech-2020-214436
25. Monot M, Honoré N, Garnier T, Araoz R, Coppée J-Y, Lacroix C, et al. On the origin of leprosy. Science (2005) 308(5724):1040–2. doi: 10.1126/science/1109759
26. Browne SG. Some aspects of the history of leprosy: the leprosie of yesterday. Proc R Soc Med (1975) 68(8):485–93. doi: 10.1177/003591577506800809
28. Grzybowski A, Sak J, Pawlikowski J, Nita M. Leprosy: Social implications from antiquity to the present. Clin Dermatol (2016) 34(1):8–10. doi: 10.1016/j.clindermatol.2015.10.009
29. Robertson J. The leprosy asylum in India: 1886-1947. J Hist Med Allied Sci (2009) 64(4):474–517. doi: 10.1093/jhmas/jrp014
30. Cruz A.. United nations, general assembly, special rapporteur on leprosy. In: Stigmatization as dehumanization: Wrongful stereotyping and structural violence against women and children affected by leprosy (New York, United States of America:United Nations General Assembly) (2019). Available at: https://www.undocs.org/A/HRC/41/47.
31. Jacob JT, Franco-Paredes C. The stigmatization of leprosy in India and its impact on future approaches to elimination and control. PloS Negl Trop Dis (2008) 2(1):e113. doi: 10.1371/journal.pntd.0000113
32. Chae GT. Modern history of hansen’s disease in Korea. Infect Chemother (2020) 52(4):647–53. doi: 10.3947/ic.2020.52.4.647
33. Miller T, Smith-Savage R. Medieval leprosy reconsidered (2006). Available at: https://www.semanticscholar.org/paper/51a1db6b47bdad5c05fe1d55aa11759cfcc60151.
34. Transmission (2021). Available at: https://www.cdc.gov/leprosy/transmission/index.html.
35. Background – the stigma of leprosy – Nepal leprosy trust (2021). Available at: https://www.nlt.org.uk/about/background/.
36. Navon L. Beggars, metaphors, and stigma: a missing link in the social history of leprosy. Soc Hist Med (1998) 11(1):89–105. doi: 10.1093/shm/11.1.89
37. Baumann SL, Lee OJ, Im S-B. Stories of suffering with leprosy and cancer in Korea. Nurs Sci Q (2013) 26(3):274–9. doi: 10.1177/0894318413489171
38. McCurry J. Japanese Leprosy patients continue to fight social stigma. Lancet (2004) 363(9408):544. doi: 10.1016/s0140-6736(04)15586-4
39. National Human Rights Commissions of Korea. Hansen’s disease patients human rights factual survey outcome report on the perspective of the aging society (2019). Available at: https://library.humanrights.go.kr/search/media/img/CAT000000048628?metsno=000000001369&fileid=M000000001369_FILE000001.
40. Kim J-H. Death and survival of patients with hansen’s disease in colonial Korea. Korean J Med Hist (2019) 28(2):469–508. doi: 10.13081/kjmh.2019.28.469
41. Asampong E, Dako-Gyeke M, Oduro R. Caregivers’ views on stigmatization and discrimination of people affected by leprosy in Ghana. PloS Negl Trop Dis (2018) 12(1):e0006219. doi: 10.1371/journal.pntd.0006219
42. Sermrittirong S, Van Brakel WH. Stigma in leprosy: concepts, causes and determinants. Lepr Rev (2014) 85(1):36–47. doi: 10.47276/lr.85.1.36
43. Gussow Z, Tracy G. Stigma and the leprosy phenomenon: The social history of a disease in the nineteenth and twentieth centuries. Bull History Med (1970) 44:425–49.
44. Opromolla PA, Martelli ACC. A terminologia relativa à hanseníase. Bras Dermatol (2005) 80(3):293–4. doi: 10.1590/S0365-05962005000300011
45. Marcela Castro C, Erazo L, Gunturiz ML. Strategies for reducing leprosy stigma. Mycobacterial Diseases (2018) 08(01):1–4. doi: 10.4172/2161-1068.1000253
46. Kaur H, Gandhi A. People’s perception of leprosy–a study in Delhi. Indian J Lepr (2003) 75(1):37–46.
47. Sermrittirong S, Van Brakel WH, Bunbers-Aelen JF. How to reduce stigma in leprosy–a systematic literature review. Lepr Rev (2014) 85(3):149–57. doi: 10.47276/lr.85.3.149
48. Kaur H, Ramesh V. Social problems of women leprosy patients–a study conducted at 2 urban leprosy centres in Delhi. Lepr Rev (1994) 65(4):361–75. doi: 10.5935/0305-7518.19940037
49. Pelizzari VD, Arruda GO, Marcon SS, Fernandes CA. Perceptions of people with leprosy about disease and treatment. Rev Rene (2016) 17(4):466. doi: 10.15253/2175-6783.2016000400005
50. WHO. Global strategy for further reducing the leprosy burden and sustaining leprosy control activities (2006–2010), operational guidelines (2006). Available at: https://www.who.int/lep/resources/SEAGLP20062.pdf?ua=1.
51. Somar P, Waltz MM, van Brakel WH. The impact of leprosy on the mental wellbeing of leprosy-affected persons and their family members - a systematic review. Glob Ment Health (Camb) (2020) 7(e15):e15. doi: 10.1017/gmh.2020.3
52. Erinfolami AR, Adeyemi JD. A case control study of psychiatric morbidities among subjects with leprosy in Lagos, Nigeria. Int J Psychiatry Med (2009) 39(1):89–99. doi: 10.2190/PM.39.1.g
53. Dijkstra JIR, Van brakel WH, van Elteren M. Gender and leprosy-related stigma in endemic areas: A systematic review; leprosy review;, Vol. 88 (Colchester, UK:Lepra) (2017). pp. 419–40. doi: 10.47276/lr.88.3.419.
54. Joo Y, Yang J. The relation between disease stigma and gender: societal and familial discrimination experiences of hansenians. Family culture [Internet] (2020) 32(1):: 193–222. doi: 10.21478/family.32.1.202003.007
55. Van ‘t Noordende AT, Aycheh MW, Schippers A. The impact of leprosy, podoconiosis and lymphatic filariasis on family quality of life: A qualitative study in Northwest Ethiopia. PloS Negl Trop Dis (2020) 14(3):e0008173. doi: 10.1371/journal.pntd.0008173
56. Lockwood DNJ, Suneetha S. Leprosy: too complex a disease for a simple elimination paradigm. Bull World Health Organ (2005) 83(3):230–5.
57. Centers for Disease Control and Prevention. Neglected tropical diseases (2022). Available at: https://www.cdc.gov/globalhealth/ntd/diseases/index.html (Accessed March 30, 2022).
58. Muthuvel T, Govindarajulu S, Isaakidis P, Shewade HD, Rokade V, Singh R, et al. “I wasted 3 years, thinking it’s not a problem”: Patient and health system delays in diagnosis of leprosy in India: A mixed-methods study. PloS Negl Trop Dis (2017) 11(1):e0005192. doi: 10.1371/journal.pntd.0005192
59. International Federation of Anti Leprosy Associations (ILEP). Ending discrimination against persons affected by leprosy in India. In: Office of the united nations high commissioner for human rights (2019) (Geneva, Switzerland:Office of the United Nations High Commissioner for Human Rights(OHCHR). Available at: https://tbinternet.ohchr.org/Treaties/CRPD/Shared%20Documents/Ind/INT_CRPD_CSS_Ind_35564_E.docx.
60. Discriminatory Laws. International federation of anti-leprosy associations. Available at: https://ilepfederation.org/discriminatory-laws/.
Keywords: COVID-19, discrimination, epidemiology, leprostigma, leprosy, public health
Citation: Shin H and Oh Y (2022) Leprosy and leprostigma: A review from the past through COVID-19. Front. Trop. Dis 3:827102. doi: 10.3389/fitd.2022.827102
Received: 01 December 2021; Accepted: 22 July 2022;
Published: 20 September 2022.
Edited by:
James Rudge, University of London, United KingdomReviewed by:
Swetalina Pradhan, AIIMS Patna, IndiaCopyright © 2022 Shin and Oh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yul Oh, ZGhkYmZAaGFubWFpbC5uZXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.