- 1Departamento de Clinica, Patologia y Tratamiento, Instituto Nacional de Parasitologia Dr M. Fatala Chaben, ANLIS CG Malbran, Buenos Aires, Argentina
- 2Departamento de Enfermedades Infecciosas, Hospital de Infecciosas FJ Muñiz, Buenos Aires, Argentina
- 3Departamento de Parasitologia, Instituto Nacional de Enfermedades Infecciosas, ANLIS CG Malbran, Buenos Aires, Argentina
- 4Departamento de Diagnóstico y Tratamiento, Hospital de Infecciosas FJ Muñiz, Buenos Aires, Argentina
- 5Department of Pediatrics, Schulich School of Medicine & Dentistry, Western University, London, ON, Canada
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2. COVID-19 leads, in most patients, to mild-to-moderate symptoms, but some develop severe disease and succumbed to death. People with medical conditions have a higher risk of death than those without them. Chagas disease (CD) can cause cardiac diseases in approximately one-third of affected people. The aim of this study is to find out if there is any clinical association between Chagas disease and COVID-19 severity. This is a cohort study of 29 patients who were hospitalized with COVID-19 and had a diagnosis of chronic Trypanosoma cruzi infection. This coinfected cohort was matched by sex, age, presence of comorbidities, and requirement of hospitalization on intensive care unit (ICU) at admission with a control cohort of patients hospitalized due to COVID-19 without CD in a 3:1 ratio (n = 87). The clinical outcomes evaluated were as follows: days of hospitalization, death, and requirement of ICU and mechanical respiratory assistance (MV). The study protocol was approved by the Institutional Ethics in Research Committee. The Chagas disease/COVID-19 coinfected cohort had a median age of 55 years old (49.0, 66.0); 17 (59%) were male. All patients survived the acute COVID-19. Three of them were admitted to the ICU, and two required MV. Twenty-two (75.8%) required supplemental oxygen. There were no statistical differences in any laboratory parameters between the groups except for lactic acid dehydrogenase, which showed higher levels in the coinfected cohort, with a median of 573 U/L (interquartile range: 486.00, 771.00) vs. 476 U/L (346.00, 641.00) in the control group (p = 0.007). There were no differences in clinical outcomes between both groups. On the cohort with Chagas disease, there were zero deaths, three (10.3%) were admitted in the ICU, and two (6.9%) required MV, while for the control group there were six deaths (6.6%), 13 required ICU (14.9%), and 11 required MV (12.6%), without a statistically significant difference. This small series of coinfected Chagas disease and COVID-19 does not suggest differences in clinical evolution compared to non-Chagas patients. This data is similar to a Brazilian cohort. More data of this population with and without cardiomyopathy is needed to optimize the follow-up and recommendation for the population affected by this neglected tropical disease about COVID-19.
Introduction
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2. The World Health Organization (WHO) declared COVID-19 a pandemic disease on February 11, 2020 (1). The first COVID-19 case of Argentina was diagnosed in a traveler patient on March 3, 2020, and at 1 year after, a total of 2.1 million people were affected, and 52,453 have died by COVID-19 in this country (2, 3). COVID-19 produces mild-to-moderate symptoms in most patients, but some develop severe disease, acute respiratory distress syndrome (ARDS), septic shock, and organ failure (including cardiac manifestations) and even succumbed to death (4, 5). In a North American cohort with more than 1.3 million laboratory-confirmed cases, 14% of patients required hospitalization and 5% died (6). It is also known that the probability of severe COVID-19 and death is higher in males, aged ≥60 years old, and those with chronic medical conditions. The most important comorbidities are arterial hypertension, diabetes mellitus, obesity, heart conditions (including cardiomyopathies), respiratory disease, chronic kidney disease, and cancer (7, 8). In people with these medical conditions, the risk of death is 12 times higher than those without them (6).
Trypanosomiasis americana, more commonly known as Chagas disease (CD), is an infection which, in its chronic phase, can cause cardiac diseases in approximately one-third of seroreactive people. The cardiac affliction is usually observed decades after Trypanosoma cruzi acquisition and is the most common cause of non-ischemic cardiomyopathy in Latin America. CD cardiomyopathy may develop typical conduction disturbances, heart failure, arrhythmias, thromboembolic disorders, and eventually sudden death (9, 10). In Argentina, the burden of this disease is a matter of public health as about 4% of the population has chronic CD, and it is the country with the most cases in the world (11).
Publications described at least three immunopathologic processes for severe COVID-19: pulmonary macrophage activation syndrome, endothelialitis, and thrombotic microangiopathy (12). The cytokine storm in patients with COVID-19 resulted in severely damaged pulmonary tissues, leading to death (13). In chronic T. cruzi infection, parasitic cardiac tissular infiltration leads to permanent immune activation. This produces a chronic cycle of inflammation, fibrosis, and constant cardiac remodeling to develop in some patients with Chagas cardiomyopathy. Cardiomyopathy appears in patients with inflammatory immunologic reactions with a higher presence of interferon gamma and tumoral necrosis factor alfa. Conversely, patients with anti-inflammatory cytokine profiles and a higher production of interleukin 10 tend to remain in the chronic indeterminate phase (14). Besides cardiomyopathy, T. cruzi could produce hypercoagulability by thrombin activation, platelet hyperactivity, and endothelial damage (15). These inflammatory cytokine profiles and prothrombotic status could lead to a worse outcome of COVID-19 in Chagas disease patients.
Until now, there is very limited information available about this coinfection. The aim of this study was to describe the clinical evolution of a series of patients with chronic CD (with or without cardiomyopathy) hospitalized due to COVID-19 in an infectious diseases hospital in Buenos Aires, Argentina, during the first year of the COVID-19 pandemic.
Methods
This is a cohort study of patients hospitalized due to COVID-19, with and without CD (ratio 3:1), at Hospital de Infecciosas FJ Muñiz, Buenos Aires, Argentina, during the first pandemic year in Argentina, from March 1, 2020 to March 1, 2021. The inclusion criterion was all hospitalized patients due to COVID-19 with CD. CD diagnosis was made by two serological reactive tests detected during COVID-19 hospitalization or obtained from medical history charts. A COVID-19 diagnosis was made by SARS-CoV2 PCR on nasopharyngeal swabs.
The CD patients were matched with a control cohort of non-CD hospitalized patients at the same hospital with a confirmed diagnosis of COVID-19. The data from these patients was taken from the ECCOVID multicenter trial database. The last database was made by consecutive adult patients hospitalized due to COVID-19 in 19 hospitals in Argentina coordinated by the Infectious Disease Society of Argentina—SADI in Spanish (16).
Age, gender, comorbidities, laboratory and clinical parameters, clinical evolution, and length of hospitalization data were collected. The laboratory parameters were as follows: leukocytes, lymphocytes, neutrophils, lactic acid dehydrogenase (LDH), ferritin, and D dimer. Pulmonary computer tomography or a chest X-ray description was also recorded. Other relevant parameters, such as electrocardiogram, echocardiogram, and history of trypanocidal treatment in CD patients, when available, were registered, too.
Statistical Analysis
Nearest neighbor matching was applied, focusing on the propensity score for age, sex, presence of comorbidities, presence of multiple comorbidities, and need of intensive care unit (ICU) at admission. Categorical data is presented as absolute numbers and proportions, and continuous variables are expressed as means and standard deviation or as medians and interquartile ranges according to normality. Chi-square (χ2) or Fisher exact test was used to compare the distribution of categorical variables and Student’s t-test or Wilcoxon–Mann–Whitney test for continuous variables. The results were considered statistically significant if the two-tailed P-value was <0.05. All statistical analyses were performed with R software (version 4.0.1).
The study protocol was approved by the Institutional Ethics in Research Committee of the Hospital de Infecciosas FJ Muñiz, Buenos Aires, Argentina (DI-2021-21-GCABA-HIFJM). The ECCOVID Trial was approved by the same ethics committee (DI-2020-132-GCABA-HIFJM). Informed consent was waived owing to retrospective data collection in both protocols.
Results
COVID-19 and T. cruzi Coinfection Cohort
A total of 29 clinical charts of patients hospitalized for COVID-19 with a diagnosis of chronic T. cruzi infection (i.e., “coinfected cohort”) were eligible for this study. The coinfected cohort median age was 55 years old (interquartile range, IQR: 49.0, 66.0), 17 (59%) were male, 20 were born in Argentina and six in Bolivia, and three had missing data. There were eight patients with T. cruzi serologies during hospitalization, another eight have reactive serologies from other institution, and 13 patients had a diagnosis of CD reference on medical charts. The median time between the start of COVID-19 symptoms and hospitalization was 7 days (range, 2–24). The median length of hospitalization was 10 days (IQR: 7.0, 14.0). All patients survived acute COVID-19, but three of them were admitted to the ICU and two required mechanical respiratory assistance (MV). Twenty-two (75.8%) needed supplementary oxygen. The COVID-19 classification according WHO guidance (17) were as follows: 19 patients had moderate diseases as pneumonia, seven patients had severe diseases such as pneumonia with SpO2 <90% or respiratory rate >30 breaths/min at room air, and three had a critical disease, such as ARDS.
Most of the patients had comorbidities (69%) other than CD with or without myocardiopathy, and 65% of the patients with comorbidities had more than one. The comorbidities were as follows: 60% arterial hypertension, 40% overweight or obesity, 25% diabetes mellitus, 25% smoking (active or history of smoking), 10% had a history of tuberculosis, and 10% had others.
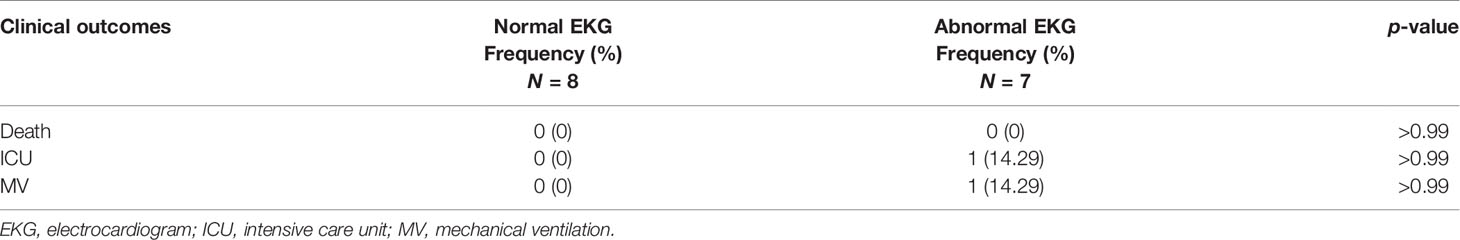
Only 15 (52%) patients had an electrocardiogram (EKG) done during hospitalization, of which eight (53%) were normal, and seven patients presented abnormalities associated with CD cardiomyopathy: two (29%) had a left anterior fascicular block, two (29%) had a right bundle branch block, one (14%) had a right bundle branch block with left anterior fascicular block, one (14%) had a right bundle branch block and ventricular premature beats, and one (14%) had sinus bradycardia. Two patients had an echocardiogram during hospitalization; one was normal and the other one had dilatation of left cardiac cavities, with an ejection fraction of 22%. It was possible to gather data on CD treatment in only one patient who had received benznidazole treatment 3 years earlier for 30 days.
During COVID-19 hospitalization, all 29 patients had a diagnosis of pneumonia. Twenty-seven (93%) received antibiotics, and the remaining two who did not receive antibiotics did not need supplementary oxygen either. Out of the 22 patients that required supplementary oxygen, 11 (50%) received systemic glucocorticoids. Out of the 11 patients that required supplementary oxygen and did not receive systemic glucocorticoids, one had severe pneumonia.
Out of the three patients who were admitted in ICU, two received convalescent human plasma and ivermectin. The other two patients in this cohort received ivermectin, too. Two patients were treated with oseltamivir, too, both aged over 60 years old and with comorbidities.
COVID-19 Without Chagas Disease Cohort vs. COVID-19 With Chagas Disease Group
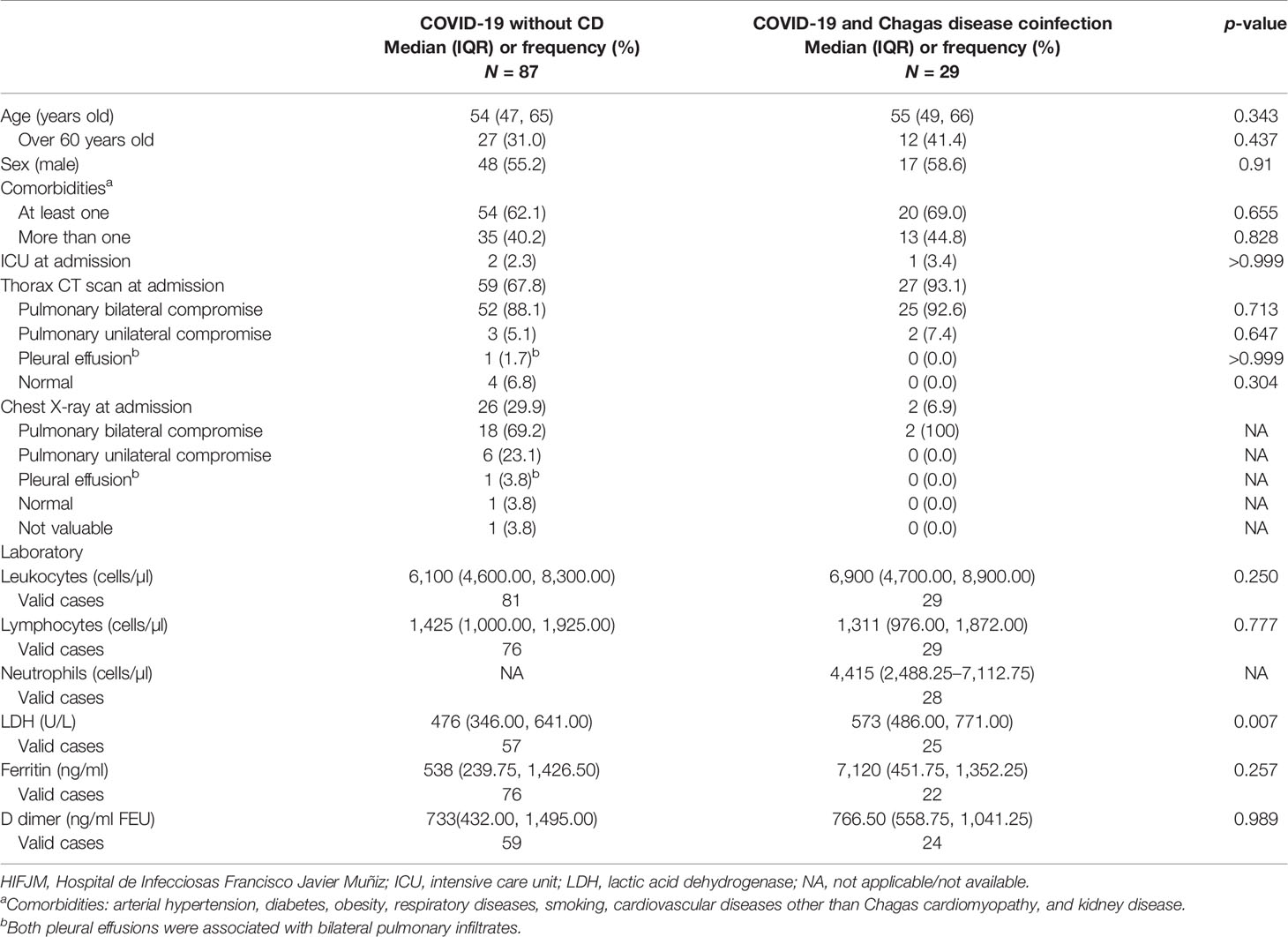
The total number of patients included for the cohort COVID-19 without CD was 87. There was no statistical difference in the laboratory parameters (leukocytes, lymphocytes, ferritin, and D dimer) between groups, except for LDH that showed higher levels on the coinfected cohort with a median of 573 U/L (IQR: 486.00, 771.00) vs. the control cohort with a median of 476 U/L (IQR: 346.0, 641.0; p = 0.007). This median LDH difference is not clinically relevant (Table 1).
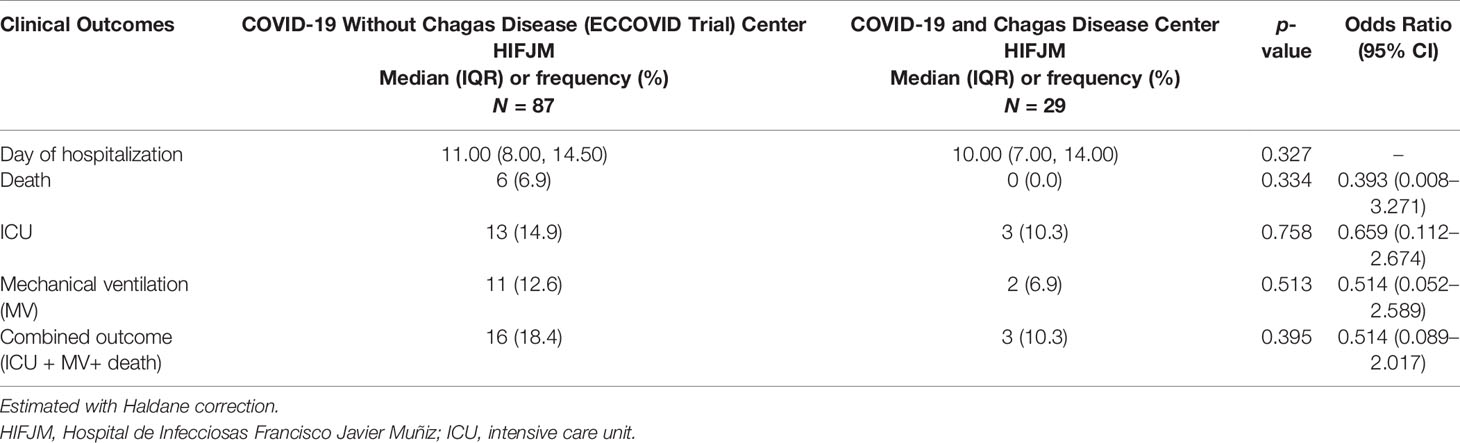
There were no differences in length of hospitalization, death, requirement of ICU and MV, and a combined outcome made of the following parameters: requirement of ICU and/or MV and or death between both groups (Table 2). In the coinfection cohort, there were zero deaths, three (10.3%) were admitted in the ICU, and two (6.9%) required MV, while in the control group, there were six deaths (6.6%), 13 required ICU (14.9%), and 11 required MV (12.6%). The analysis of the clinical outcomes did not show any statistical difference between groups. There were no differences on clinical COVID-19 evolution between CD patients with abnormal EKG (n = 7) vs. those with normal EKG (n = 8) (Table 3).
Discussion
In this study, we describe the evolution of patients with chronic CD—with and without myocardiopathy—hospitalized due to COVID-19. Reassuringly, we did not observe any statistically significant difference in clinical outcomes for coinfected patients compared to controls. These data are consistent with a Brazilian series recently published (18). Molina et al. have shown minor differences in C-reactive protein (CRP) in the group coinfected with CD. Unfortunately, we do not have data of the CRP levels for most patients, but other acute-phase reactants such as ferritin and D dimer were similar between groups; LDH had a higher median in the CD group, which seemed clinically insignificant (19). Another laboratory subrogate marker described in patients with severe and critical COVID‐19 is lymphopenia, but we could not find any differences in lymphocyte count between the groups. With this limited data, mostly concordant with the Brazilian series, we cannot assume that there is any difference in the immune, laboratory, and clinical response in hospitalized patients due to COVID-19 with a history of T. cruzi chronic infection.
Myocardial acute COVID-19 involvement in both groups cannot be ruled out as it was not routine to perform troponin measurements and EKG to all hospitalized patients due to COVID-19 in our center. The coinfected cohort had 46% of EKG abnormalities typical of CD cardiomyopathy. These data are similar to the Brazilian series with 60% EKG alterations (18). In both studies, Brazilian and ours, patients classified as CD with or without cardiomyopathy are limited mostly for missing data such as EKG and echocardiogram. This missing data makes it not possible to estimate a confident difference about the coinfection between patients with CD cardiomyopathy and without it, an important knowledge that is still missing.
In our study, we did not observe any deaths from acute COVID-19 in the coinfected cohort, while the mortality rate in the non-CD control group was 6.9%, without statistical difference. In the Brazilian series, mortality was 32.3 and 30.6% in each group—CD and non-CD, again without any significant difference. There is an important difference in the global mortality rate between the Brazilian series and our study. This difference in the global mortality rate can be because of the circulation of deadly variants, such as the Gamma variant, the collapse of the Brazilian health system during outbreak waves, and public misinformation (20, 21). However, both studies, one with high mortality rate and the other with a low rate, still show no mortality difference due to COVID-19 between CD and control groups. In the 75.8% of the coinfected group that required supplementary oxygen, only about 50% of them received systemic corticoids; some cases were because they were hospitalized before this treatment indication was supported by the recovery trial data (22). Another treatment issue to note is the high use of antibiotics, which were prescribed to 22 of 29 hospitalized confirmed COVID-19 patients; this high rate of antibiotic prescribing is quite concordant with publications from the United States of America, where 83% and at least 71% of the hospitalized COVID-19 patients received antibiotics without a microbiologically confirmed infection (23, 24). Two patients of the coinfected cohort in the ICU received convalescent human plasma and ivermectin as compassionate treatment; these treatments are not currently indicated, but compassionate treatments are expected to change dynamically during any new and severe disease, such as the COVID-19 pandemic, before evidence support them or not (25–27).
Besides the two series, ours and the Brazilian one, there are other few case reports published which described CD and COVID-19 clinical evolution. Two cases that died due to COVID-19 were both patients who were over 60 years old and had other comorbidities (28). Then, two other fatal cases were reported in cardiac transplant patients because of CD myocardiopathy; the two of them died due to respiratory insufficiency caused by COVID-19 and CMV reactivation (29). Finally, another case reports a Brazilian woman with COVID-19 who survived; she had Chagas cardiomyopathy (congestive cardiac failure and arrhythmia right bundle branch block treated with a pacemaker, propranolol, and an anticoagulant) and dimorphic leprosy (30). The scarce information about this coinfection, after more than 18 months of the COVID-19 pandemic, shows again that CD is a neglected disease, as there is almost no information for this population.
There are some limitations in our study, such as the fact that there are some missing data (i.e., CD serologies and EKG for all the patients) because during the outbreak the health system almost collapsed and resources (including human resources) had to be used with priority criteria, and not all complementary studies could be easily done on isolated patients. Another limitation is that the number of patients in the coinfected cohort, which was 29, is not substantial, but as far as we know, there is only one study with this coinfection clinical approach with a similar number of included patients carried out in Brazil (18), so we hoped to elucidate some unknown gaps with our information, thus making a contribution to the other series.
Conclusion
In this small series of CD and COVID-19 hospitalized patients, we did not observe any differences in their clinical evolution compared to CD uninfected controls. CD does not seem to be a significant comorbidity for severe COVID-19, besides the risks associated to CD cardiomyopathy. More data of this CD population, with and without cardiomyopathy, is needed to optimize the follow-up and recommendations for the population affected by this neglected tropical disease about COVID-19.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Comité de Ética en Investigación del Hospital de Infecciosas F.J. Muñiz. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
MF and GG conceptualized and directed the project. MF, OA, AG, and LV contributed to resources and data curation. AB took charge of the methodology. MF, AB, FG, SL, and TO wrote the article. All authors contributed to the article and approved the submitted version.
Funding
The authors of this study declare that they received an unrestricted grant from Fundacion Mundo Sano (bXVuZG9zYW5vQG11bmRvc2Fuby5vcmc=) to support the publication costs of this article.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We want to thank Grupo ECCOVID, SADI (Sociedad Argentina de Infectología) for provide the controls database and to all the health care workers that deal with COVID-19 pandemia, especially the ones from Hospital de Infecciosas FJ Muñiz, Buenos Aires, Argentina.
References
1. World Health Organization. WHO Characterizes COVID-19 as an Pandemic. Available at: https://www.paho.org/en/news/11-3-2020-who-characterizes-covid-19-pandemic (Accessed September 12, 2021).
2. Ministerio de Salud de la Nación Argentina. Salud Confirma El Primer Caso De Coronavirus En El País. Available at: https://www.argentina.gob.ar/noticias/salud-confirma-el-primer-caso-de-coronavirus-en-el-pais (Accessed September 12, 2021).
3. Ministerio de Salud de la Nación Argentina. Nuevos Coronavirus COVID 19. Informes Diarios. Reportes. Available at: https://www.argentina.gob.ar/coronavirus/informes-diarios/reportes/marzo2021 (Accessed September 12, 2021).
4. Zheng Z, Peng F, Xu B, Zhao J, Liu H, Peng J, et al. Risk Factors of Critical & Mortal COVID-19 Cases: A Systematic Literature Review and Meta-Analysis. J Infect (2020) 81:e16–25. doi: 10.1016/j.jinf.2020.04.021
5. Zhou Y, Yang Q, Chi J, Dong B, Lv W, Shen L, et al. Comorbidities and the Risk of Severe or Fatal Outcomes Associated With Coronavirus Disease 2019: A Systematic Review and Meta-Analysis. Int J Infect Dis (2020) 99:47–56. doi: 10.1016/j.ijid.2020.07.029
6. Centre for Disease Control and Prevention. Coronavirus Disease 2019 Case Surveillance—United States, January 22–May 30, 2020. Available at: https://www.cdc.gov/mmwr/volumes/69/wr/pdfs/mm6924e2-H.pdf (Accessed September 12, 2021).
7. Centers for Disease Control and Prevention. People With Certain Medical Conditions. Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html (Accessed September 12, 2021).
8. Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA (2020) 323(13):1239–42. doi: 10.1001/jama.2020.264832091533
9. Ribeiro AL, Nunes MP, Teixeira MM, Rocha MO. Diagnosis and Management of Chagas Disease and Cardiomyopathy. Nat Rev Cardiol (2012) 9:576–89. doi: 10.1038/nrcardio.2012.109
10. Prata A. Clinical and Epidemiological Aspects of Chagas Disease. Lancet Infect Dis (2001) 1:92–100. doi: 10.1016/S1473-3099(01)00065-2
11. WHO - World Health Organization Chagas Disease in Latin America: An Epidemiological Update Based on 2010 Estimates. Wkly Epidemiol Rec (2015) 6:33–44.
12. Marik PE, Iglesias J, Varon J, Kory P. A Scoping Review of the Pathophysiology of COVID-19. Int J Immunopathol Pharmacol (2021) 35:20587384211048026. doi: 10.1177/20587384211048026
13. Dhama K, Patel SK, Pathak M, Yatoo MI, Tiwari R, Malik YS, et al. An Update on SARS-CoV-2/COVID-19 With Particular Reference to Its Clinical Pathology, Pathogenesis, Immunopathology and Mitigation Strategies. Travel Med Infect Dis (2020) 37:101755. doi: 10.1016/j.tmaid.2020.101755
14. Dutra WO, Menezes CA, Magalhaes LM, Gollob KJ. Immunoregulatory Networks in Human Chagas Disease. Parasite Immunol (2014) 36(8):377e87. doi: 10.1111/pim.12107
15. Pérez-Campos, Mayoral L, Hernández-Huerta MT, Papy-García D, Barritault D, Zenteno E, et al. Immunothrombotic Dysregulation in Chagas Disease and COVID-19: A Comparative Study of Anticoagulation. Mol Cell Biochem (2021) 476:3815–25. doi: 10.1007/s11010-021-04204-3
16. Cordova E, Mykietiuk A, Sued O, De Vedia L, Pacifico N, Garcia Hernandez MH, et al. Clinical Characteristics and Outcomes of Hospitalized Patients With SARS-CoV-2 Infection in a Latin American Country: Results From the ECCOVID Multicenter Prospective Study. PloS One (2021) 16(10):e0258260. doi: 10.1371/journal.pone.0258260
17. World Health Organization. Clinical Management of COVID-19: Interim Guidance, 27 May 2020. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1 (Accessed September 12, 2021).
18. Molina I, Marcolino M, Pires M, Ramos L, Silva R, Guimarães M, et al. Chagas Disease and SARS-CoV-2 Coinfection Does Not Lead to Worse in-Hospital Outcomes. Sci Rep (2021) 11:20289. doi: 10.1038/s41598-021-96825-3
19. Iwamura A, Tavares da Silva M, Hümmelgen A, Pereira P, Falcai A, Grumach A, et al. Immunity and Inflammatory Biomarkers in COVID-19: A Systematic Review. Rev Med Virol (2021) 31:e2199. doi: 10.1002/rmv.2199
20. Knaul FM, Touchton M, Arreola-Ornelas H, Atun R, Anyosa RJC, Frenk J, et al. Punt Politics as Failure of Health System Stewardship: Evidence From the COVID-19 Pandemic Response in Brazil and Mexico. Lancet Reg Health Am (2021) 4:100086. doi: 10.1016/j.lana.2021.100086
21. Vijaykumar S, Rogerson D, Jin Y, de Oliveira Costa MS. Dynamics of Feedback Behaviours to Social Peers Sharing COVID-19 Misinformation on WhatsApp in Brazil. J Am Med Inform Assoc (2021) 21:ocab219. doi: 10.1093/jamia/ocab219
22. RECOVERY Collaborative Group, Horby P, Lim W, Emberson J, Mafham M, Bell J, et al. Dexamethasone in Hospitalized Patients With Covid-19. N Engl J Med (2021) 384:693–704. doi: 10.1056/NEJMoa2021436
23. Martin A, Shulder S, Dobrzynski D, Quartuccio K, Pillinger K. Antibiotic Use and Associated Risk Factors for Antibiotic Prescribing in COVID-19 Hospitalized Patients. J Pharm Pract (2021) 22:8971900211030248. doi: 10.1177/08971900211030248
24. Chopra V, Flanders S, Vaughn V, Petty L, Gandhi T, McSparron J, et al. Variation in COVID-19 Characteristics, Treatment and Outcomes in Michigan: An Observational Study in 32 Hospitals. BMJ Open (2021) 11(7):e044921. doi: 10.1136/bmjopen-2020-044921. 23.
25. Simonovich VA, Burgos Pratx LD, Scibona P, Beruto MV, Vallone MG, Vázquez C, et al. A Randomized Trial of Convalescent Plasma in Covid-19 Severe Pneumonia; PlasmAr Study Group. N Engl J Med (2021) 384:619–29. doi: 10.1056/NEJMoa2031304
26. Libster R, Pérez Marc G, Wappner D, Coviello S, Bianchi A, Braem V, et al. Early High-Titer Plasma Therapy to Prevent Severe Covid-19 in Older Adults. N Engl J Med (2021) 384:610–8. doi: 10.1056/NEJMoa2033700
27. Krolewiecki A, Lifschitz A, Moragas M, Travacio M, Valentini R, Alonso DF, et al. Antiviral Effect of High-Dose Ivermectin in Adults With COVID-19: A Proof-of-Concept Randomizedtrial. EClinicalMedicine (2021) 37:100959. doi: 10.1016/j.eclinm.2021.100959
28. Alberca R, Yendo T, Ramos Y, Fernandes L, Mendonça Oliveira L, Teixeira F, et al. Case Report: COVID-19 and Chagas Disease in Two Coinfected Patients. Am J Trop Med Hyg (2020) 103:2353–6. doi: 10.4269/ajtmh.20-1185
29. Gozzi-Silva SC, Benard G, Alberca RW, Yendo TM, Teixeira FME, Oliveira LM, et al. SARS-CoV-2 Infection and CMV Dissemination in Transplant Recipients as a Treatment for Chagas Cardiomyopathy: A Case Report. Trop Med Infect Dis (2021) 6(1):22. doi: 10.3390/tropicalmed6010022
30. Kurizky PS, Cerqueira SRPS, Cunha DV, Albuquerque CP, Aires RB, Mota LMHD, et al. The Challenge of Concomitant Infections in the Coronavirus Disease 2019 Pandemic Era: Severe Acute Respiratory Syndrome Coronavirus 2 Infection in a Patient With Chronic Chagas Disease and Dimorphic Leprosy. Rev Soc Bras Med Trop (2020) 53:e20200504. doi: 10.1590/0037-8682-0504-2020
Keywords: COVID-19, Chagas disease, Argentina, coinfection—disease, clinical evolution, Trypanosoma cruzi
Citation: Fernandez ML, Benchetrit A, Astudillo OG, Garay AM, De Vedia L, Garcia Bournissen F, Lloveras SC, Orduna TA and Gonzalez GD (2022) COVID-19 and Chagas Disease in Buenos Aires, Argentina. Front. Trop. Dis 2:779428. doi: 10.3389/fitd.2021.779428
Received: 18 September 2021; Accepted: 08 November 2021;
Published: 15 February 2022.
Edited by:
Alfonso J. Rodriguez-Morales, Fundacion Universitaria Autónoma de las Américas, ColombiaReviewed by:
Wilmer Villamil Gómez, University of Sucre, ColombiaMaría Fernanda García-Bustos, Universidad Nacional de Salta, Argentina
D. Katterine Bonilla-Aldana, Fundacion Universitaria Autónoma de las Américas, Colombia
Copyright © 2022 Fernandez, Benchetrit, Astudillo, Garay, De Vedia, Garcia Bournissen, Lloveras, Orduna and Gonzalez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marisa Liliana Fernandez, bWFyaXNhLmZlcm5hbmRlekBnbWFpbC5jb20=
 Marisa Liliana Fernandez
Marisa Liliana Fernandez Andres Benchetrit
Andres Benchetrit Osvaldo German Astudillo3,4
Osvaldo German Astudillo3,4 Tomas Agustín Orduna
Tomas Agustín Orduna