
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Transplant. , 06 November 2024
Sec. Transplantation Immunology
Volume 3 - 2024 | https://doi.org/10.3389/frtra.2024.1500493
This article is part of the Research Topic Transplantation Pillars View all 10 articles
In the last five decades, remarkable surgical and medical advances ensued within the field of organ transplantation. These strides were marked by significant breakthroughs in transplant immunology, with Dr. Paul I. Terasaki standing as a true pillar of the field. This article highlights major milestones in Dr. Terasaki's life, his groundbreaking accomplishments in the field of transplant medicine, and his enduring philanthropic contributions to numerous medical and community organizations.
In the last five decades, remarkable surgical and medical advances ensued within the field of organ transplantation, supported by the revolutionary achievements of pioneers who helped turn what most considered “experimental” in the 1950s and 1960s into the gold-standard treatment option for patients with end-organ diseases (1). These strides were marked by significant breakthroughs in transplant immunology, with Dr. Paul I. Terasaki standing as a true pillar of the field (2). Dr. Terasaki pushed the boundaries of transplant immunology and histocompatibility science with his transformative contributions to our understanding of tissue typing and humoral rejection (3). In addition, Dr. Terasaki demonstrated an unwavering commitment to humanity through his philanthropic efforts. This commentary highlights major milestones in Dr. Terasaki's life, his groundbreaking accomplishments in the field of transplant medicine, and his enduring philanthropic contributions to numerous medical and community organizations.
Paul I. Terasaki, PhD, was born into a humble family in Los Angeles, California, on September 10th, 1929 (3). In 1942, during World War II, his family was forced to relocate to an internment camp in Arizona, where he lived in one modest room shared with his parents, his two brothers, and his aunt. Dr. Terasaki described their living conditions as poor, and the education he received during those three years of confinement as suboptimal (3). After World War II, his family hesitated to return to California and decided to move to Chicago, where Dr. Terasaki finished high school and then was enrolled as a pre-medicine student at the University of Illinois.
In 1948, feeling it was safe to return to Los Angeles, the Terasakis moved back, and Paul was transferred to the University of California Los Angeles (UCLA) to complete his degree in Zoology. He went on to earn three degrees at UCLA: a bachelor's degree in preventive medicine and public health, as well as a master's and a Ph.D in zoology (4). In 1954, he married Hisako Sumioka, a young artist, and the couple had four children (5).
After graduating, he joined the Department of Surgery at UCLA, where his research initially focused on chicken skin grafts. He developed an interest in transplant tolerance and eventually was awarded a postdoctoral fellowship to work in London for a year under future Nobel Prize laureate Peter Medawar. This experience shaped the rest of his career (3). Dr. Terasaki recalls that at that time, the debate about cellular vs. humoral contribution to graft rejection was ongoing, but he leaned mostly towards B-cells and focused on antibody involvement (3, 6).
Returning to UCLA as an “assistant research zoologist,” Dr.Terasaki worked tirelessly for the next five years, putting in 18-hour days (7, 8). In 1964, he made a major breakthrough by introducing the micro-cytotoxicity test. The test required only 1 microliter—one lambda—of serum to identify human leukocyte antigens (HLA) (Figure 1) (9). The “micro-test” was adopted as a standard in the United States in 1968, and two years later, in 1970, it was adopted as an international standard for genetically matching transplant candidates and recipients. In addition, the test was instrumental in resolving cases of disputed paternity and linking HLA to various diseases (10–12). At that time, Dr. Terasaki linked the presence of preformed antibodies against donor HLA antigens and hyperacute graft rejection (13). This finding set the ground for the need to test for these antibodies and to perform lymphocyte cross-match in patients awaiting transplantation.
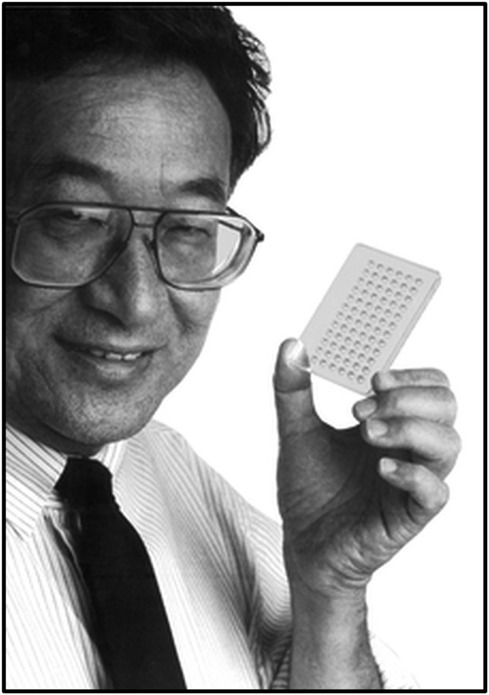
Figure 1. Dr.Paul I. Terasaki holding the Terasaki Plate. Source: https://terasaki.org.
In 1969, Dr. Terasaki became a professor of surgery at UCLA, and he founded the UCLA Tissue Typing Laboratory that year (14). In the 1970s and 80s, the Terasaki lab conducted most of the world's HLA-typing and donor-recipient matching (6). His team developed kits that allowed samples from across the globe to be shipped to Los Angeles with enough numbers of cells for cross-matching (6).
Dr. Terasaki was instrumental in establishing the UCLA kidney registry at UCLA in 1970, which eventually developed into an International Kidney Registry encompassing 52 transplant centers worldwide (15). Dr. Terasaki played a pivotal role in setting the first United Network for Organ Sharing (UNOS) kidney allocation system criteria, and the UCLA kidney transplant he championed served as a precursor for the national transplant database (16).
Additionally, in 1970, he developed, along with Geoffrey Collins, a simple cold storage method to keep donor kidneys viable for longer periods, making it possible to transport organs over long distances (11, 15, 17). In 1984, he founded One Lambda, Inc., a transplant diagnostic company with eight of his former students, to provide diagnostic tools for transplant centers to better match and monitor their patients pre/post-transplant (18).
In 1995, Dr.Terasaki reported that transplants between spouses who were unrelated and poorly HLA-matched had favorable outcomes (19). This led to a significant increase in transplants between spouses, friends, distant relatives, and even complete strangers, expanding the pool of available donors (15). In the late 1990s, One Lambda began to introduce a solid-phase system for identifying HLA antibodies using purified HLA and later recombinant techniques to identify HLA antibodies accurately and laid the groundwork for the creation of the “calculated” percent-reactive antibody, which provides a uniform estimate of how incompatible a transplant candidate is with potential donors (15). It also enabled laboratories to perform a virtual crossmatch, which streamlined organ allocation, significantly increasing the number of transplants among sensitized patients. One Lambda, Inc. was acquired by Thermo Fisher Scientific in 2012 and continues to play a central role in advancing tissue typing (20).
Following Dr.Terasaki's retirement from UCLA in 1999, he founded the Terasaki Foundation, a dedicated research center to study cancer immunotherapy and the role of humoral immunity in organ transplantation (14). Dr. Teraskai's recent contributions to the field transplant have demonstrated that HLA antibodies play a major role in late graft failure, reshaping the transplant community's understanding of chronic graft failure (21).
Dr.Terasaki held numerous leadership positions within the transplant community, including serving as president of the International Transplantation Society and the American Society of Histocompatibility and Immunogenetics, the OPTN/UNOS Board of Directors, and the Histocompatibility and Scientific Advisory Committees (6, 16). Throughout his career, he published over 900 scientific papers, authored more than 20 books, and mentored over 100 postdoctoral scholars (4, 6).
In addition to his groundbreaking scientific achievements, Dr.Terasaki is well-known for his philanthropic endeavors. Throughout his life, he donated $58 million to UCLA to support the Terasaki Life Sciences Building, the UCLA International Institute (later renamed the Paul I. and Hisako Terasaki Center for Japanese Studies), and endowed faculty chairs in that discipline and in U.S.–Japanese relations (4). The Terasakis also established the Nibei Foundation to facilitate fellowship opportunities and partnerships between Japanese and Japanese-American professors and doctors (4).
Paul and his wife, Hisako, were committed to preserving Japanese history in the US. Paul served on many committees, including the Japanese American National Museum in Los Angeles, the Memorial to Japanese American Patriotism in World War II in Washington D.C., and the US-Japan Council, and gave generously to these organizations. After the tsunami, he sponsored 20 Los Angeles college students to volunteer in Japan; the goal was to have the students understand the Tohoku disaster and learn about Japanese history and culture (22). Among many organizations supported by Paul & Hisako Terasaki (Table 1), notable contributions were made to Japanese American Citizens League, Keiro Senior Healthcare, Los Angeles Jewish Symphony, Los Angeles County Museum of Art, Little Tokyo Service Center-(Budukon), Manzanar Committee Smithsonian Institution, The Transplantation Society, the United States-Japan Bridging Foundation, UCLA-The Nikkei Student Union, University of Tokyo, Venice Japanese Community Center, and West LA United Methodist Church. Dr Terasaki also donated an endowed chair in the Department of Surgery at UCLA.
In recognition of his achievements, he received numerous prestigious awards, including the Medawar Prize in 1996—the world's highest honor for contributions to the field of transplantation—and the UCLA Medal in 2012, the university's highest distinction (20). In 2013, the American Society of Transplantation honored him as an Innovator in Transplantation (15). For his dedication to preserving the history of Japanese Americans, Terasaki was also awarded the U.S.-Japan Council Lifetime Achievement Award in 2014 (22).
Despite his inauspicious childhood, Dr. Terasaki went on to achieve enormous success as a pioneer in transplant medicine, a mentor to countless health professionals, and a dedicated benefactor to numerous academic, social service, and community organizations. Dr. Terasaki passed away on January 25, 2016, at the age of 86. His legacy will continue to inspire generations to come, and he will be remembered with deep respect and admiration for his groundbreaking contributions and the lives he touched.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
JK: Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Pilch NA, Bowman LJ, Taber DJ. Immunosuppression trends in solid organ transplantation: the future of individualization, monitoring, and management. Pharmacotherapy. (2021) 41:119–31. doi: 10.1002/phar.2481
2. Terasaki PI. A brief history of HLA. Immunol Res. (2007) 38:139–48. doi: 10.1007/s12026-007-0020-4
3. Terasaki PI. Courage and character, leaders and legends: an interview with Paul I. Terasaki, PhD. Interview by Linda Ohler. Prog Transplant. (2012) 22:4–5. doi: 10.7182/pit2012275
4. Paul Terasaki, 86, transplant medicine pioneer, philanthropist, UCLA faculty member and alumnus | UCLA. Available online at: https://newsroom.ucla.edu/releases/paul-terasaki-86-transplant-medicine-pioneer-philanthropist-ucla-faculty-member-and-alumnus (accessed September 10, 2024).
5. Niiya B. Paul Terasaki | Densho Encyclopedia. (2023) Available online at: https://encyclopedia.densho.org/Paul_Terasaki/#cite_note-ftnt_ref4-4 (accessed September 7, 2024).
6. Gale RP, Opelz G. Paul I Terasaki (10 September, 1929–25 January, 2016). Bone Marrow Transplant. (2016) 51:621–2. doi: 10.1038/bmt.2016.70
8. Terasaki Institute—Our Legacy. Available online at: https://terasaki.org/institute/about-us/legacy.html (accessed September 7, 2024).
9. Terasaki PI, McClelland JD. Microdroplet assay of human serum cytotoxins. Nature. (1964) 204:998–1000. doi: 10.1038/204998b0
10. Schlosstein L, Terasaki PI, Bluestone R, Pearson CM. High association of an HL-A antigen, W27, with ankylosing spondylitis. N Engl J Med. (1973) 288:704–6. doi: 10.1056/NEJM197304052881403
11. Cecka JM. Interview with Dr Paul Terasaki. Am J Transplant. (2003) 3:1047–51. doi: 10.1034/j.1600-6143.2003.00194.x
12. Terasaki PI. Resolution by HLA testing of 1000 paternity cases not excluded by ABO testing. J Fam L. (1977) 16:543.
13. Terasaki PI, Marchioro TL, Starzl TE. Sero-typing of human lymphocyte antigens: preliminary trials on long-term kidney homograft survivors. (1965)
14. Dr. Paul I. Terasaki. Available online at: https://international.ucla.edu/japan/article/180854 (accessed September 10, 2024).
15. Cecka JM, Gjertson DW, Reed EF. Paul I. Terasaki, PhD, 1929–2016. Am J Transplant. (2016) 16:1365–6. doi: 10.1111/ajt.13747
16. In Memoriam: Paul Terasaki, Ph.D.—UNOS. Available online at: https://unos.org/news/in-memoriam-paul-terasaki-ph-d/ (accessed September 10, 2024).
17. Collins GM, Bravo-Shugarman M, Terasaki PI. Kidney preservation for transportation: initial perfusion and 30 h’ ice storage. Lancet. (1969) 294:1219–22. doi: 10.1016/S0140-6736(69)90753-3
18. Paul Terasaki Obituary (1929–2016). Los Angeles, CA—Los Angeles Times. Available online at: https://www.legacy.com/us/obituaries/latimes/name/paul-terasaki-obituary?id=16378170 (accessed September 10, 2024).
19. Terasaki PI, Cecka JM, Gjertson DW, Takemoto S. High survival rates of kidney transplants from spousal and living unrelated donors. N Engl J Med. (1995) 333:333–6. doi: 10.1056/NEJM199508103330601
20. The Lifesaving Work of Paul Terasaki | National Inventors Hall of Fame®. Available online at: https://www.invent.org/blog/inventors/paul-terasaki-tissue-typing (accessed September 10, 2024).
21. Kaneku H, O’leary JG, Banuelos N, Jennings LW, Susskind BM, Klintmalm GB, et al. de novo donor-specific HLA antibodies decrease patient and graft survival in liver transplant recipients. Am J Transplant. (2013) 13:1541–8. doi: 10.1111/ajt.12212
22. 2014 USJC Annual Conference—U.S.-Japan Council. Available online at: https://www.usjapancouncil.org/2014-usjc-annual-conference/ (accessed September 10, 2024).
Keywords: transplantation, histocompatibility, micro-cytotoxicity, philanthropy, humoral immunity
Citation: Kobashigawa J (2024) Paul I. Terasaki, Ph.D: a pioneer in transplant medicine and a dedicated philanthropist. Front. Transplant. 3:1500493. doi: 10.3389/frtra.2024.1500493
Received: 23 September 2024; Accepted: 23 October 2024;
Published: 6 November 2024.
Edited by:
Jerzy Kupiec-Weglinski, University of California, Los Angeles, United StatesReviewed by:
David W. Gjertson, University of California, Los Angeles, United StatesCopyright: © 2024 Kobashigawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jon Kobashigawa, am9uLmtvYmFzaGlnYXdhQGNzaHMub3Jn
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.