- 1Department of Surgery, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States
- 2Department of Surgery, Medical College of Wisconsin, Milwaukee, WI, United States
Objective: We investigated the impact of body mass index (BMI) on post-operative outcomes and survival of patients with interstitial pulmonary fibrosis (IPF) undergoing lung transplantation.
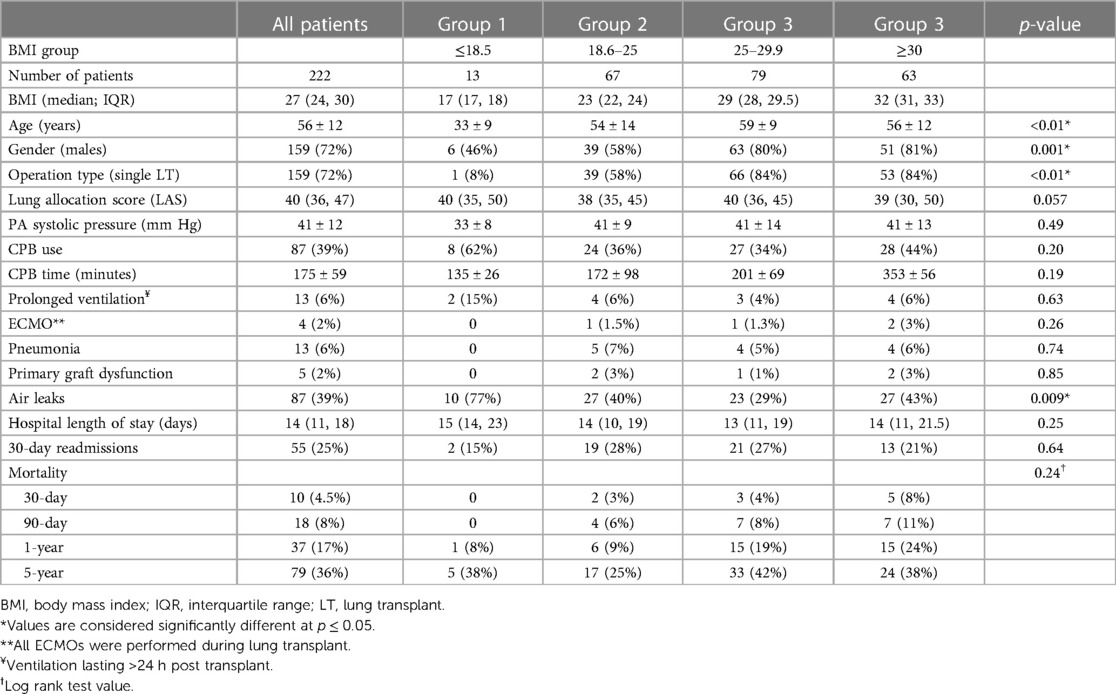
Methods: We retrospectively reviewed 222 patients with IPF that underwent lung transplant (LT) at our institution from 2005 to 2019. Recipients were divided in 4 groups: group-1 consisted of underweight patients (BMI ≤18.5 kg/m2), group-2 of normal weight patients (BMI 18.5–25 kg/m2), group-3 of over-weight patients (BMI 25–29.9 kg/m2) and group-4 of obese patients (BMI ≥30 kg/m2).
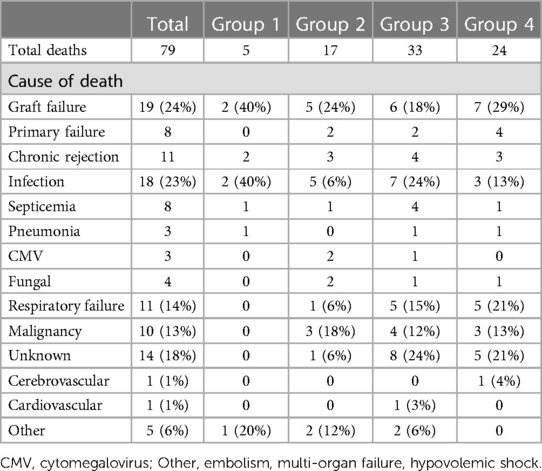
Results: Group-1 consisted of 13 (6%) patients, group-2 of 67 (30%) patients, group-3 of 79 (36%) patients, group-4 consisted of 63 (28%) patients. Median BMI for group-1 was 17 [interquartile range (IQR): 17, 18], for group-2 was 23 (22, 24), for group-3 was 29 (28, 29.5) and group-4 was 32 (31, 33). Patients in group-1 were significantly younger (p < 0.01). Single LT comprised the majority of operation type in group-2 to group-4 and it was significantly higher than group 1 (p < 0.01). Median follow-up time was 39 months (13–76). A total of 79 (35.5%) patients died by the end of study. Overall, five deaths occurred in group-1, 17 in group-2, 33 in group-3, and 24 in group-4. Kaplan–Meier analysis showed that mortality was not statistically significant between the groups (p = 0.24). Cox-regression analysis was used to assess other possible risk factors that could influence the effect of BMI on mortality, including transplant type (single, double), lung allocation score, and age, diabetes and creatinine levels at surgery. None of these factors were shown to affect patient mortality (p > 0.05). Overall reasons for death included graft failure (24%), infection (23%), respiratory failure (14%), and malignancy (13%).
Conclusions: Body mass index does not impact long-term survival of patients with IPF undergoing lung transplantation.
Introduction
Idiopathic pulmonary fibrosis (IPF) is the most common adult form of interstitial lung disease (ILD), characterized by a progressive deterioration of lung function leading to death (1). The disease progress could be slow and gradual over many years or accelerate to a rapid decline of respiratory function. Although, anti-fibrotic therapy has been shown to slow the lung function decline over time, IPF continues to be a progressive disease with poor prognosis, with a median survival time from diagnosis of 3–5 years (2–6). Although many obstacles to lung transplant (LT) remain, such as the shortage of donor lungs, opportunistic infections, and allograft rejection, LT is the ultimate treatment for patients with progressive loss of pulmonary function due to progressive pulmonary fibrosis. Due to the relative shortage of organs, the growing number of patients on the waiting list, and the increasing number of deaths during the wait for organs, the lung allocation score (LAS) was implemented in 2005 by the Organ Procurement and Transplantation Network (OPTN 7, 8). Studies have shown that LAS appears to be achieving its objectives by reducing waitlist time and altering the distribution of lung disease being transplanted on the basis of medical necessity (9). According to the data from the International Society for Heart and Lung Transplantation (ISHLT), IPF represents 40% of lung transplants. Of those 72% were bilateral lung transplantations and 28% were single lung transplants (10). Lung transplantation in itself is associated with disease-specific challenges and ISHLT has set a list of major and relative contraindications for listing patients for lung transplantation (11).
A few studies have found a correlation of BMI with patient outcomes and survival after LT and have indicated that preoperative BMI optimization is reflected in better outcomes (12–18). The purpose of our study was to investigate if pre-transplant BMI has any effect on post-operative outcomes and survival of patients in a selective group of patients with interstitial pulmonary fibrosis (IPF) undergoing lung transplantation.
Patients and methods
A total of 386 patients received lung transplants (LT) between November, 2007 and August, 2019 at the University of Wisconsin Hospital and Clinics. Of those, 222 (57.5%) patients had interstitial pulmonary fibrosis (IPF) as their indication for LT and were the subject population for our study.
This study was approved by our Institutional Review Board (IRB). A waiver of the need to obtain consent from patients was approved. All transplant were performed in strict compliance with the ISHLT ethics. Patient baseline characteristics and peri-operative data were prospectively acquired and maintained in our IRB approved database. Follow-up survival data were retrospectively collected from each patient's electronic medical record.
Patients were divided in 4 groups based on their body mass index (BMI): group 1 consisted of underweight patients with BMI ≤18.5 kg/m2, group 2 of normal weight patients with BMI 18.5–25 kg/m2, group 3 of overweight patients (BMI 25–29.9 kg/m2) and, group 4 of obese patients (BMI ≥30 kg/m2). Primary outcome was long-term patient survival. Secondary outcomes were post-operative complications including prolonged ventilation (ventilation lasting >24 h post-surgery), pneumonia, primary graft dysfunction, air leaks and unplanned hospital readmissions. Overall survival time was calculated from the date of transplant to the date of last follow-up visit or death.
Statistical analysis
Continuous variables are represented as mean ± standard deviation, and categorical variables are represented as number and percentage. Continuous variables were compared using one-way ANOVA. Categorical variables were compared using Kruskal–Wallis test to determine group differences. If the test showed there were differences between the 4 groups, the Mann–Whitney test was used for pairwise comparisons. Overall survival time was calculated from the date of transplantation to the date of last follow-up visit or death. Cumulative event rates were calculated by the method of Kaplan and Meier. p-values less than 0.05 (two-sided) were considered statistically significant. All analyses were performed using the IBM SPSS statistical software program (IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp).
Results
Demographic profiles
Two hundred twenty two (222; 57.5%) of LT were due to IPF. When divided by their BMI at time of transplant, group 1 consisted of 13 (6%) patients, group 2 of 67 (30%) patients, group 3 of 79 (36%) patients and group 4 consisted of 63 (28%) patients (Table 1). Median BMI for g1 was 17 [interquartile range (IQR): 17, 18], for group 2 was 23 (IQR: 22, 24), for group 3 was 29 (28, 29.5) and for group 4 was 32 (31, 33). Patients in group 1 were significantly younger than patients in other groups (p < 0.01). Males comprised the majority of the patients in group 2, group 3 and group 4 (p = 0.01). Single LT comprised the majority of operation type in group 2, group 3 and group 4 and it was significantly higher than group 1 (p < 0.01; Table 1).
Clinical outcomes and post-operative survival
Patients were monitored for 5 years or until death. Median follow up time was 39 months (IQR: 13–76). There was no difference in prolonged ventilation, pneumonia and primary graft dysfunction between the groups (all p > 0.05). Significantly more air leaks occurred post-operatively in group 1 compared to other groups (p = 0.009). There was no statistically significant difference in hospital length of stay and 30-day readmissions between the four groups (p > 0.05; Table 1).
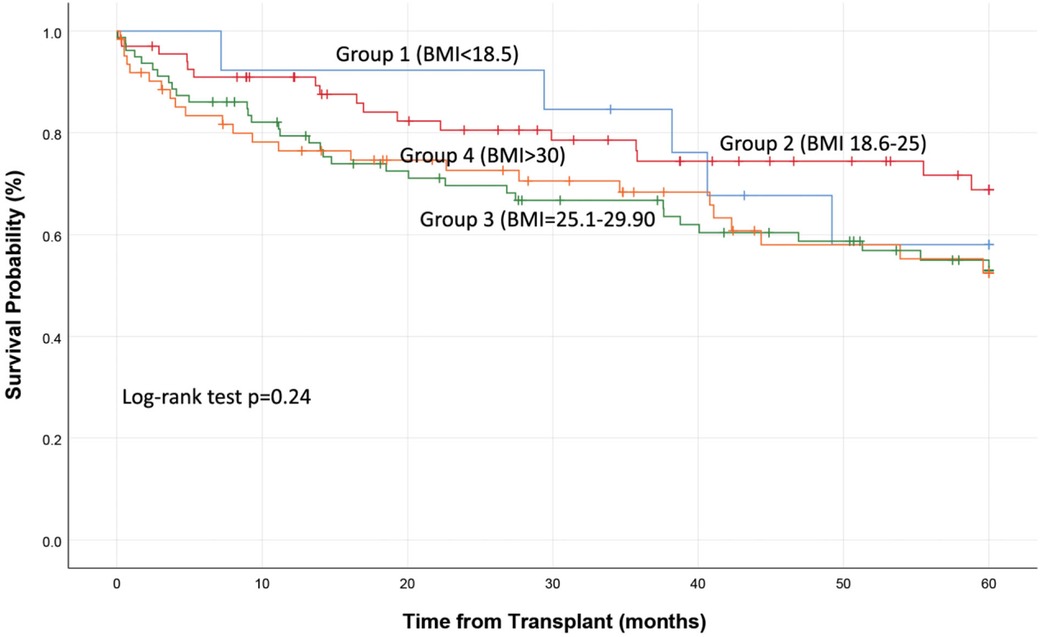
A total of 79 (35.5%) patients died by the end of study follow-up. Overall, 5 (6%) deaths occurred in group 1, 17 (21.5%) in group 2, 33 (42%) in group 3, and 24 (30%) in group 4. Mortality at 30- and 90-day, 1- and 5-year was similar between the groups (Log Rank test p = 0.24; Figure 1; Table 1). Cox-regression analysis was used to assess other possible risk factors that could influence the effect of BMI on mortality, including transplant type (single, double), lung allocation score, and age, diabetes and creatinine levels at surgery. None of these factors were shown to affect patient mortality (p > 0.05). Reasons for death included graft failure (24%), infection (23%), respiratory failure (14%), and malignancy (13%). Table 2 summarizes the breakdown of reasons for death for all four groups.
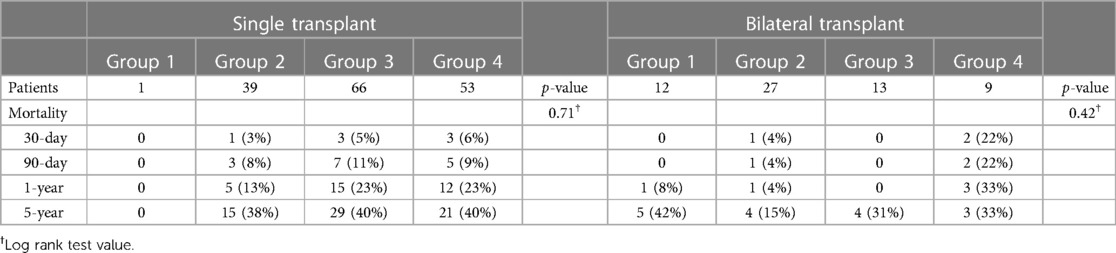
Of the 79 total deaths, 37 of them occurred within 1 year post transplant. When divided by BMI groups 1 death occurred in group 1, 6 in group 2, 15 in group 3, and 15 in group 4 (Log Rank test p = 0.086). Reasons for death in the first year post-transplant included, graft failure (n = 8; 22%), infections (17%) and respiratory failure (25%). Overall, a majority of the deaths occurred in patients undergoing single lung transplant. Thirty-two of 36 (89%) deaths that occurred the first year were in patients receiving single LT (Table 3) We did not find a a statistically significant difference in mortality between different BMI groups in single or bilateral lung transplant patients (Table 3; Figure 2).
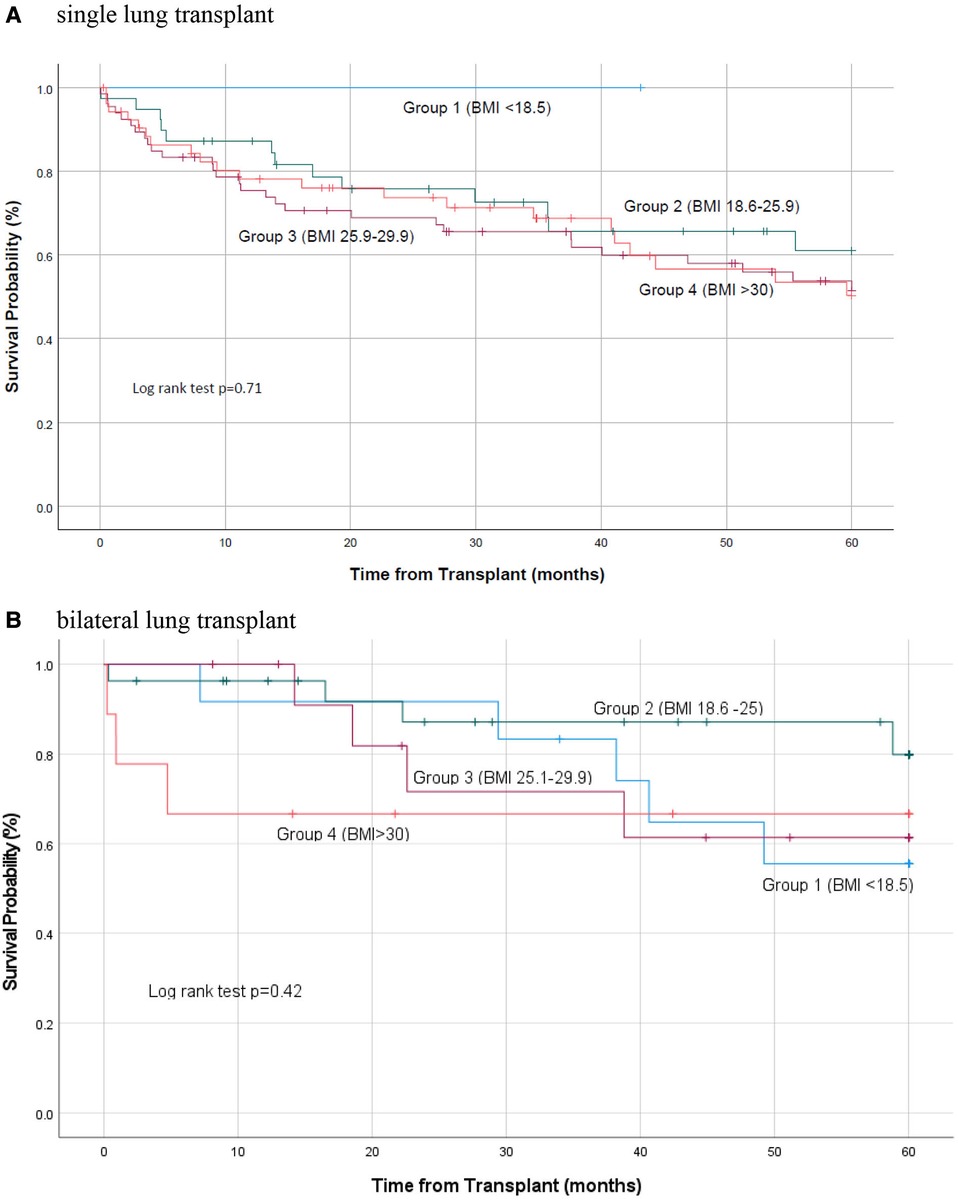
Figure 2. Kaplan Meier survival curve based on transplant type. (A) Single lung transplant; (B) Bilateral lung transplant.
We also investigated whether there was a relationship between BMI and survival when BMI was considered a continuous variable. We found that BMI did not affect patient survival at 1- and 5-year post-transplant, even when considered as a continuous variable (p = 0.36; HR: 0.931, CI [0.79–1.08] and p = 0.59; HR: 0.97, CI [0.89–1.06] at 1-year and 5-year post-transplant respectively.
Median survival time of patients undergoing single LT was 37 (IQR: 11, 73) months and median survival time of patients undergoing double LT was 43 (IQR: 18, 82) months (p = 0.52). Forty percent (n = 63) of the patients undergoing single LT died during the study follow-up and 25% (n = 16) patients undergoing double LT died during the study follow-up (p = 0.037). There was not a significant relationship between BMI, operation type (single vs. double LT) and survival at 5-year post transplant (p = 0.08; HR: 0.30, CI [0.29–1.01].
Discussion
The question whether BMI affects surgical outcomes and patient survival after LT has been the focus of several investigations. Although ISHLT guidelines recommend that BMI of 30 kg/m2 or greater, be considered a relative contraindication to lung transplantation, in practice, BMI thresholds for candidacy vary across centers. Conflicting results in the literature may drive these decisions. A large study using UNOS data found that both pre-transplant underweight and obesity contributed to up to 12% of deaths in the first year after transplantation and concluded that BMI is an independent risk factor for death after LT (19). Looking at a similar population another group found that overweight and class I obesity were not associated with early mortality (13). A study using the Scientific Registry of Transplant Recipients (SRTR) database, focused on individual BMI units and found that BMI is an independent predictor of mortality in lung transplant recipients at both 90 days and 1 year post-transplantation (12). They concluded that the patterns of BMI effect on patient survival do not fit into the predefined BMI categories.
In this study, we evaluated the impact of BMI on a select group of patients undergoing LT, patients with IPF. We used two approaches in our analysis. In the first approach, our study population was divided in groups based on their BMI. The relationship between BMI and both short- and long-term patient survival was not statistically meaningful. To avoid the bias of BMI grouping the second approach looked at BMI as a continuous variable. This approach resulted in similar findings that BMI did not affect short- and long-term patient survival in the select group of recipients with ILD.
A few studies have investigated BMI and survival in IPF patients. Alakhras and colleagues, examined 197 patients with a BMI <25, BMI 25–30 and BMI >30 (20). They found that there was an association between survival and BMI, and that increased BMI was associated with better survival. Of note, these patients did not undergo lung transplantation. Another study found that obese patients who receive bilateral LT might be at higher risk of 90-day mortality compared with patients of normal weight (21). Bilateral lung transplantation is the preferred option compared to single lung transplantation. Single lung transplantation is associated with poorer long-term outcomes (22). If we look at the latest SRTR annual report, even in 2010 bilateral lung transplant rates were significantly higher than single lung transplantation in USA (unlike the study cohort). If BMI really influences outcomes, the higher mortality rates seen in this cohort of patients may have confounded BMI effect on outcomes.
Our study has a few limitations, including its retrospective nature and the small sample size from a single institution. In addition, this observational study did not account for all other elements related to BMI that we could not capture such as frailty, change in weight over time, muscle mass, distribution of adipose tissue, targeted pre-transplant treatment, weight loss after surgery, rehabilitation characteristics for each group, etc. However, despite these limitations, this is the first study of ILD patients to analyze the effect of BMI on survival where BMI was also considered a continuous variable. This approach removes the bias on designation of BMI groups being somewhat arbitrary and may or may not reflect the actual effect on survival. The fact that both approaches gave similar results is reassuring.
Further exploration with a larger patient population may lead to additional insights into the association of BMI and patient survival and may help with management of patients afflicted with this disease.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by University of Wisconsin Internal Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
EL contributed to the study design, data collection, statistical analysis, data interpretation, and manuscript composition and revision. MD contributed to the study design, data collection, statistical analysis, data interpretation, and manuscript composition and revision. JM: contributed to the study design, data collection, statistical analysis, data interpretation, and manuscript composition and revision. GL contributed to statistical analysis and data interpretation. ND contributed to the study design, data collection, statistical analysis, data interpretation, and manuscript composition and revision. DM contributed to the study design, data collection, statistical analysis, data interpretation, and manuscript composition and revision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kim R, Meyer KC. Therapies for interstitial lung disease: past, present and future. Ther Adv Respir Dis. (2008) 2(5):319–38. doi: 10.1177/1753465808096948
2. Raghu G, Collard HR, Egan JJ, Martinez FJ, Behr J, Brown KK, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. (2011) 183(6):788–824. doi: 10.1164/rccm.2009-040GL
3. Raghu G, Amatto VC, Behr J, Stowasser S. Comorbidities in idiopathic pulmonary fibrosis patients: a systematic literature review. Eur Respir J. (2015) 46(4):1113–30. doi: 10.1183/13993003.02316-2014
4. Raghu G, Remy-Jardin M, Myers JL, Richeldi L, Ryerson CJ, Lederer DJ, et al. Diagnosis of idiopathic pulmonary fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. (2018) 198(5):e44–68. doi: 10.1164/rccm.201807-1255ST
5. Olson AL, Swigris JJ, Lezotte DC, Norris JM, Wilson CG, Brown KK. Mortality from pulmonary fibrosis increased in the United States from 1992 to 2003. Am J Respir Crit Care Med. (2007) 176(3):277–84. doi: 10.1164/rccm.200701-044OC
6. Travis WD, Costabel U, Hansell DM, King TE Jr, Lynch DA, Nicholson AG, et al. An official American thoracic society/European respiratory society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. (2013) 188(6):733–48. doi: 10.1164/rccm.201308-1483ST
7. Egan TM, Kotloff RM. Pro/con debate: lung allocation should be based on medical urgency and transplant survival and not on waiting time. Chest. (2005) 128:407–15. doi: 10.1378/chest.128.1.407
8. Egan TM, Murray S, Bustami RT, Shearon TH, McCullough KP, Edwards LB, et al. Development of the new lung allocation system in the United States. Am J Transplant. (2006) 6(5 Pt 2):1212–27. doi: 10.1111/j.1600-6143.2006.01276.x
9. Osaki S, Edwards NM, Johnson MR, Velez M, Munoz A, Lozonschi L, et al. Improved survival after heart transplantation in patients with bridge to transplant in the recent era: a 17-year single-center experience. J Heart Lung Transplant. (2009) 28(6):591–7. doi: 10.1016/j.healun.2009.03.008
10. Khush KK, Cherikh WS, Chambers DC, Harhay MO, Hayes D Jr, Hsich E, et al. The international thoracic organ transplant registry of the international society for heart and lung transplantation: thirty-sixth adult heart transplantation report—2019; focus theme: donor and recipient size match. J Heart Lung Transplant. (2019) 38(10):1056–66. doi: 10.1016/j.healun.2019.08.004
11. Weill D, Benden C, Corris PA, Dark JH, Davis RD, Keshavjee S, et al. A consensus document for the selection of lung transplant candidates: 2014–an update from the pulmonary transplantation council of the international society for heart and lung transplantation. J Heart Lung Transplant. (2015) 34(1):1–15. doi: 10.1016/j.healun.2014.06.014
12. Fernandez R, Safaeinili N, Kurihara C, Odell DD, Jain M, DeCamp MM, et al. Association of body mass index with lung transplantation survival in the United States following implementation of the lung allocation score. J Thorac Cardiovasc Surg. (2018) 155(4):1871–9. doi: 10.1016/j.jtcvs.2017.11.031
13. Singer JP, Peterson ER, Snyder ME, Katz PP, Golden JA, D'Ovidio F, et al. Body composition and mortality after adult lung transplantation in the United States. Am J Respir Crit Care Med. (2014) 190(9):1012–21. doi: 10.1164/rccm.201405-0973OC
14. Chandrashekaran S, Keller CA, Kremers WK, Peters SG, Hathcock MA, Kennedy CC. Weight loss prior to lung transplantation is associated with improved survival. J Heart Lung Transplant. (2015) 34(5):651–7. doi: 10.1016/j.healun.2014.11.018
15. Komatsu T, Chen-Yoshikaw TF, Oshima A, Harashima SI, Aoyama A, Inagaki N, et al. Severe underweight decreases the survival rate in adult lung transplantation. Surg Today. (2017) 47(10):1243–8. doi: 10.1007/s00595-017-1508-8
16. Upala S, Panichsillapakit T, Wijarnpreecha K, Jaruvongvanich V, Sanguankeo A. Underweight and obesity increase the risk of mortality after lung transplantation: a systematic review and meta-analysis. Transpl Int. (2016) 29(3):285–96. doi: 10.1111/tri.12721
17. De la Torre MM, Delgado M, Paradela M, González D, Fernández R, García JA, et al. Influence of body mass Index in the postoperative evolution after lung transplantation. Transplant Proc. (2010) 42(8):3026–8. doi: 10.1016/j.transproceed.2010.07.078
18. Buchko MT, Nagendran J. Body mass index in lung transplantation: every unit counts. J Thorac Cardiovasc Surg. (2018) 155(4):1869–70. doi: 10.1016/j.jtcvs.2017.12.089
19. Lederer DJ, Wilt JS, D'Ovidio F, Bacchetta MD, Shah L, Ravichandran S, et al. Obesity and underweight are associated with an increased risk of death after lung transplantation. Am J Respir Crit Care Med. (2009) 180(9):887–95. doi: 10.1164/rccm.200903-0425OC
20. Alakhras M, Decker PA, Nadrous HF, Collazo-Clavell M, Ryu JH. Body mass index and mortality in patients with idiopathic pulmonary fibrosis. Chest. (2007) 131(5):1448–53. doi: 10.1378/chest.06-2784
21. Gries CJ, Bhadriraju S, Edelman JD, Goss CH, Raghu G, Mulligan MS. Obese patients with idiopathic pulmonary fibrosis have a higher 90-day mortality risk with bilateral lung transplantation. J Heart Lung Transplant. (2015) 34(2):24. doi: 10.1016/j.healun.2014.09.031
22. Organ Procurement and Transplantation Network (OPTN) and Scientific Registry of Transplant Recipients (SRTR). OPTN/SRTR 2021 Annual Data Report. U.S. Department of Health and Human Services, Health Resources and Services Administration (2023). Available at: http://srtr.transplant.hrsa.gov/annual_reports/Default.aspx (Accessed July, 2023).
Keywords: lung transplant, outcomes, body mass index, pulmonary fibrosis, survival
Citation: Lushaj EB, DeCamp MM, Maloney J, Leverson G, De Oliveira N and McCarthy D (2023) Body mass Index does not impact long-term survival of patients with idiopathic pulmonary fibrosis undergoing lung transplantation. Front. Transplant. 2:1146779. doi: 10.3389/frtra.2023.1146779
Received: 17 January 2023; Accepted: 1 August 2023;
Published: 23 August 2023.
Edited by:
Varun Puri, Washington University in St. Louis, United StatesReviewed by:
Soma Jyothula, Heart and Lung Institute, Methodist Hospital, United StatesLetizia Corinna Morlacchi, Fondazione IRCCS Ca' Granda Ospedale Maggiore Policlinico di Milano, Italy
© 2023 Lushaj, DeCamp, Maloney, Leverson, De Oliveira and McCarthy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Entela B. Lushaj bHVzaGFqQHN1cmdlcnkud2lzYy5lZHU=
 Entela B. Lushaj
Entela B. Lushaj Malcolm M. DeCamp
Malcolm M. DeCamp James Maloney1
James Maloney1 Glen Leverson
Glen Leverson Nilto De Oliveira
Nilto De Oliveira Daniel McCarthy
Daniel McCarthy