
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Toxicol., 09 April 2025
Sec. Clinical Toxicology
Volume 7 - 2025 | https://doi.org/10.3389/ftox.2025.1547535
 Meye Bloothooft1‡
Meye Bloothooft1‡ Pien Cremers2‡
Pien Cremers2‡ Sükriye Güven2‡
Sükriye Güven2‡ Stijn J. Stoutjesdijk2
Stijn J. Stoutjesdijk2 Mara Jiron2
Mara Jiron2 Mark Wessel2
Mark Wessel2 Marcel A. G. Van Der Heyden1*†
Marcel A. G. Van Der Heyden1*†Introduction: Lupin beans are the seeds of plants from the Fabaceae family. These beans are rich in protein and used for human consumption for several millennia. Their popularity is still increasing. Some species produce beans with high alkaloid contents, specifically of spartaine and lupanine. Without proper processing, consuming these beans can result in lupin poisoning that causes anticholinergic syndrome. We systematically analyzed all case reports describing lupin poisoning in humans in order to define most observed clinical findings, treatment options and outcome.
Methods: We screened Pubmed and Google scholar for human case reports on lupin poisoning. Obtained full-text papers in any language were screened for eligibility. Demographics, time-to-symptoms, treatment and outcome were analyzed. Symptoms were categorized using the ICD11 classification.
Results: Twenty-seven case reports describing 33 patients were obtained. Poisoning occurred in all age groups and sexes equally. Most frequent symptoms were bilateral mydriasis (n = 25), xerostomia (n = 25), blurred vision (n = 17), lightheadedness (n = 14), weakness (n = 11). Onset of symptoms was typically within 60 min. In most cases no treatment was required, and symptoms resolved within 24 h after which patients were discharged. Two of four children in the cohort required ICU admission and one died.
Discussion: Lupin poisoning is rare and requires most often a conservative clinical approach. However, in children the effects are more severe than in adults. Frequency of lupin poisoning may rise due to increased popularity of the beans as an alternative protein source.
Legumes, like lupin beans, are nutritious as well as affordable and are increasingly sold and consumed in today’s society. They are regarded as an addition to, or alternative for soybean protein, and are rich in protein and fibers. Also, they may offer positive effects on blood pressure, blood lipid levels and a person’s weight (Pereira et al., 2022). The consumption of lupin beans has increased over the last decades and is expected to increase even further. Since 2000 the production of lupin has increased from approximately 90,000 ton per year to 450,000 ton per year in Europe (Pereira et al., 2022; Lucas et al., 2015). Although the consumption of lupin beans has positive health benefits, it is less known that unprocessed lupin beans can have negative side effects by inhibiting the parasympathetic nervous system (Resta et al., 2008).
The genus of Lupins belongs to the family of Fabaceae, which comprises in total of approximately 280 species, of which 13 originate from the Old World (i.e., Europe and North Africa) (Eckstein et al., 2023). Domesticated lupin beans include four major species, namely, Lupinus albus, Lupinus angustifolius, Lupinus luteus, and Lupinus mutabilis. Two species, L. albus and L. mutabilis, have been used for consumption for many era (Figure 1) (Carvajal-Larenas et al., 2016). L. albus originates from the European Balkan region and is widespread in the Mediterranean region (Huyghe, 1997). L. mutabilis (or “Andean lupin,” also known as Tarwi) originates from the South American Andean highlands, where it was domesticated around 650 BC (Atchison et al., 2016). Archeological finds from the same region also strongly suggest the use of wild or other domesticated species in the sixth millennium BC (Atchison et al., 2016). Egyptian and Greek records indicate the use of lupin beans as a human food source in ancient times, as far back as 2000 BC [e.g., Zhukovsky (Zhukovsky, 1929); Gladstones (Gladstones, 1970)]. Furthermore, the medicinal use of lupin beans in various forms, including its so-called debittering water, was already apparent in ancient times as, for example, described by Pliny (AD 23/24 – AD 79) in his Naturalis Historia and shortly by Galenus (AD 129–199) in his De alimentorum facultatibus (Kurlovich, 2024).
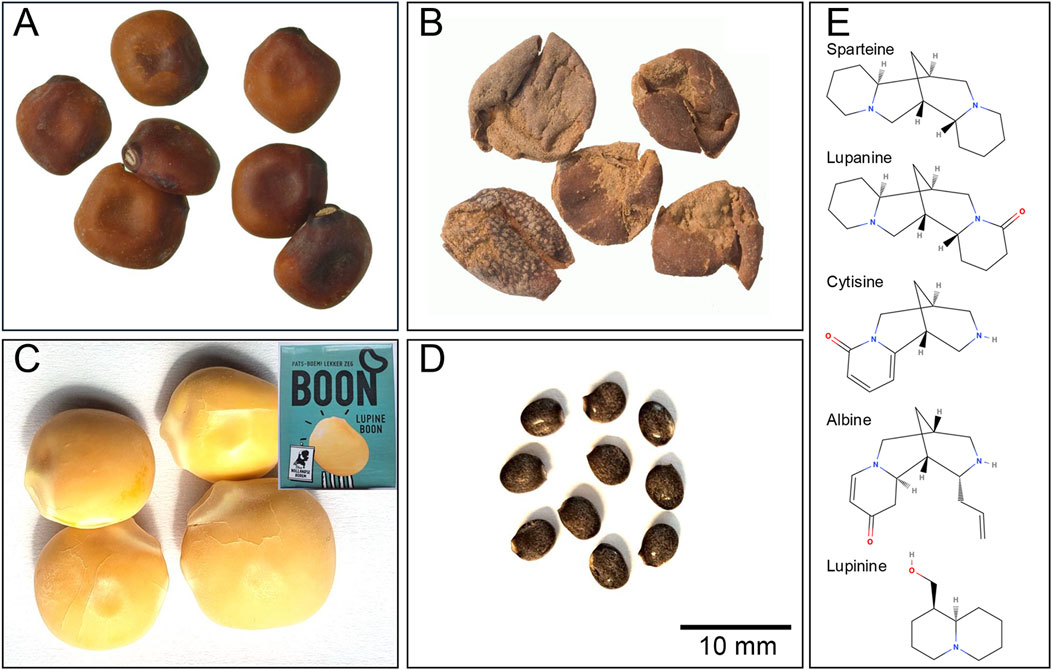
Figure 1. (A) Desiccated seeds and (B) discarded skins of white lupin or termis bean (Lupinus alba), from the Roman period (first to early second century AD) recovered from domestic refuse deposits at Quseir al-Qadim, Egypt (Van der Veen, 2011), Plate 13. Copyright M. Van der Veen, photos J. Morales (reproduced with approval of the original authors)). (C) Processed 21st century lupin seeds from the supermarket (inset container). (D) lupin seeds from the horticultural popular Washington lupin (Lupinus polyphyllus). Scale bar for panels (A–D). (E) Chemical structures of alkaloids present in lupin seeds (drawn using MolView).
Unprocessed lupin beans contain alkaloids, which are toxic and therefore unsuitable for consumption. These alkaloids bind to and block nicotinic and muscarinic cholinergic receptors, thereby (partially) inhibiting the parasympathetic nervous system. This is known as anticholinergic syndrome. Furthermore, the alkaloids sparteine and lupanine inhibit Na+ and K+ ion channels. L. mutabilis possesses high amounts of alkaloids, around 30 g/kg, with lupanine being the most prominent (±50%) alkaloid. L. albus contains around 10 g/kg alkaloids, with lupanine as the most prominent alkaloid (±70%). Other alkaloids present in lupin beans are, for example,: sparteine, lupinine, albine and cytisine (Figure 1E) (Schrenk et al., 2019).
Lupin beans that are available in supermarkets are processed and directly edible. To make unprocessed lupin beans suitable for consumption they need to be stripped of alkaloids by washing in a time demanding debittering process (Lowen et al., 1995). The beans should be soaked in a large amount of water, so-called debittering water, and cooked for 10 min each day for at least 5 days in a row before the beans are detoxified and safe for consumption, as described in a case report (Smith, 1987). The observed parasympathetic inhibition in patients after consumption of unwashed or insufficiently washed lupin beans or debittering water is known as lupin poisoning or intoxication (Ozkaya et al., 2021; Luque Marquez et al., 1991).
Since there is a shortfall in knowledge on the negative health outcomes of incorrectly processed lupin beans, we analyzed all existing case reports on lupin bean poisoning in humans, for demographics, symptoms and treatment. This review aims to increase awareness amongst healthcare workers and the general public of the symptoms, diagnosis and treatment of lupin bean poisoning.
A retrospective analysis of existing scientific literature on lupin poisoning was done. The review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines. Relevant papers were found via PubMed and Google Scholar using advanced search techniques with the following search terms: lupin AND toxicity, lupin AND poisoning, lupin toxicity OR lupin poisoning, and lupin bean intoxication. Articles in all languages (i.e., English, Spanish, Italian, French, German, Swedish, Hebrew), were assessed that came up with these search terms. Additional case reports were identified based on the reference lists of the articles found during the search in PubMed and Google Scholar. Since some case reports were written in Spanish, additional case reports were searched for in Spanish in Google, with search terms: lupinus intoxicacion or altramuz intoxicacion. Papers written in other languages than English were translated via Google Translate and subsequently reviewed by native speakers with a medical background.
The identified articles were screened and checked for inclusion (Figure 2). Papers were included in our analysis, if they were/had: human case-reports, accessible in full-text, no lupin poisoning with other diagnoses, cases with no medical history of other diseases that can cause anticholinergic symptoms, symptom description and background information, and cases without medication known to produce analogous symptoms. This resulted in 27 case reports that were used for further analysis.
To minimize interobserver variability, all case reports in this study were reviewed and interpreted by a minimum of two authors of the current paper. The following parameters, if available, were extracted from the case reports: patient characteristics; clinical symptoms; timeframe of the onset; symptoms; treatment; recovery time; type, dose and species of lupin.
We used the International Classification of Diseases (ICD) 11, the diagnostic classification system of the World Health Organization (WHO), to accurately categorize the symptoms of lupin poisoning. For analysis some data were categorized (e.g., age).
The search for lupin poisoning case reports resulted in 27 reports (Ozkaya et al., 2021; Pingault et al., 2009; Ortega Duarte et al., 2013; Luque Marquez et al., 1991; Malmgren et al., 2016; Litkey and Dailey, 2007; Li et al., 2017; Jamali, 2011; Gapany et al., 1983; Flores-Pamo et al., 2018; Di Grande et al., 2004; Daverio et al., 2014; Awada et al., 2011; Agid et al., 1988; Tsiodras et al., 1999; Smith, 1987; Schmidlin-Mészáros, 1973; Petraroia, 1926; Lowen et al., 1995; Lahoud et al., 2021; Alessandro et al., 2017; Camacho Saavedra and Uribe Uribe, 1995; Carazo Barrios and De la Fuente Cañete, 2022; Cidad et al., 2013; Lorente Esparza et al., 2021; Moreno González and Del Caño Garrido, 2021; Vivancos Gallego and Machín, 2014) describing 33 patients between 1926 and 2022 (Table 1). Patients that presented with lupin poisoning were of all ages (1–73 years old, Figure 3B) and occurred in both males and females, however slightly more females were poisoned (female n = 21, males n = 12, Figure 3A). Relatively often a female around 30–50 years old was described (n = 10). In some case reports patients stated that they had taken the beans/debittering water for health purposes: “because of healing properties,” “a suggestion of a friend against high cholesterol,” or “as diet, because of the diuretic effect” (Camacho Saavedra and Uribe Uribe, 1995; Cidad et al., 2013; Gapany et al., 1983; Ortega Duarte et al., 2013; Moreno González and Del Caño Garrido, 2021; Alessandro et al., 2017).
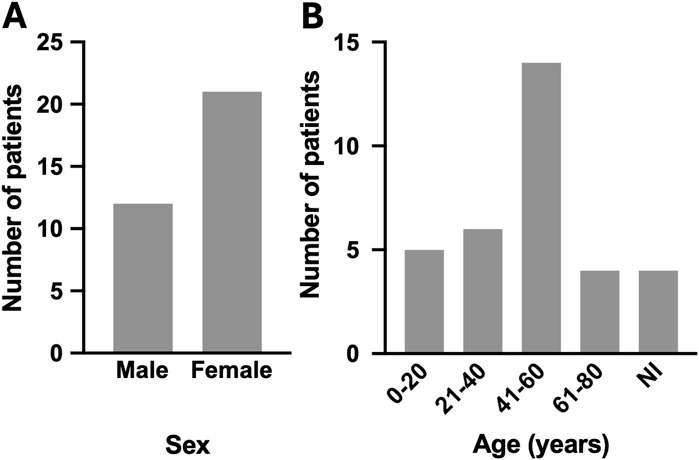
Figure 3. Sex (A) and age (B) distribution of lupin poisoning patients. NI = not included in the case report.
45% of the patients presented the first signs of poisoning within an hour after intake of lupin (n = 15). Although time to onset of symptoms varied between 15 min and 14 h (Figure 4A). Most patients ingested beans or debittering water, but also cases of lupin containing flour or homeopathics were mentioned, (Table 1). There was no clear correlation between type of beans [L. albus (n = 6) vs. L. mutabilis (n = 10)] or type of intake [beans (n = 17) vs. debittering water (n = 11)] and the severity of the symptoms. Since the dose of ingested beans is not described in most of the papers, it is hard to find causality between amount of beans/water ingested and the outcome.
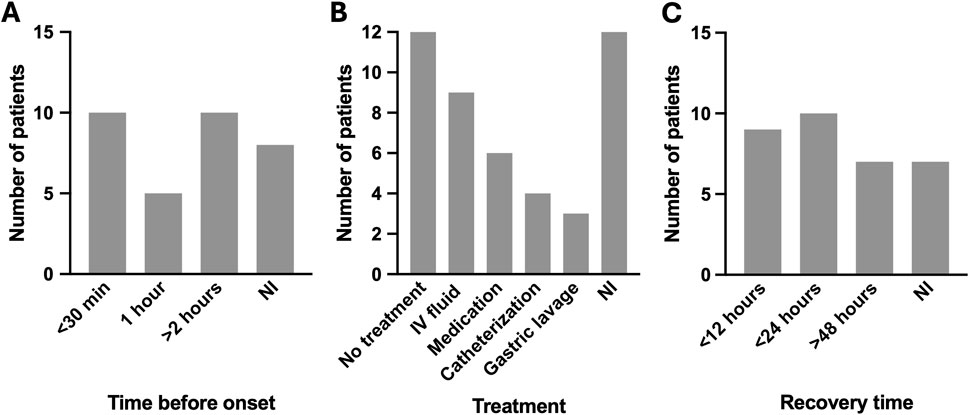
Figure 4. Time before onset symptoms (A), treatment (B) and recovery time (C) of lupin poisoning patients. NI = not included in the case report.
Sixty-nine different symptoms were described in the 33 different patients (Table 2 shows an overview of all symptoms reported n > 1; Supplementary Appendix 1 shows all symptoms per case), of which many occurred only once (n = 25). All symptoms (n = 262) were classified via the ICD11 system. Symptoms were mostly seen in the digestive system (n = 69), visual system (n = 63), nervous system (n = 29) and circulatory system (n = 23). Most common symptoms were mydriasis (n = 25), xerostomia (n = 25), blurred vision (n = 17), lightheadedness (n = 14) and weakness (n = 11). Symptoms seem to be progressing over time when patients present in the clinic quickly after the poisoning. For example, symptoms worsen or new symptoms appear.
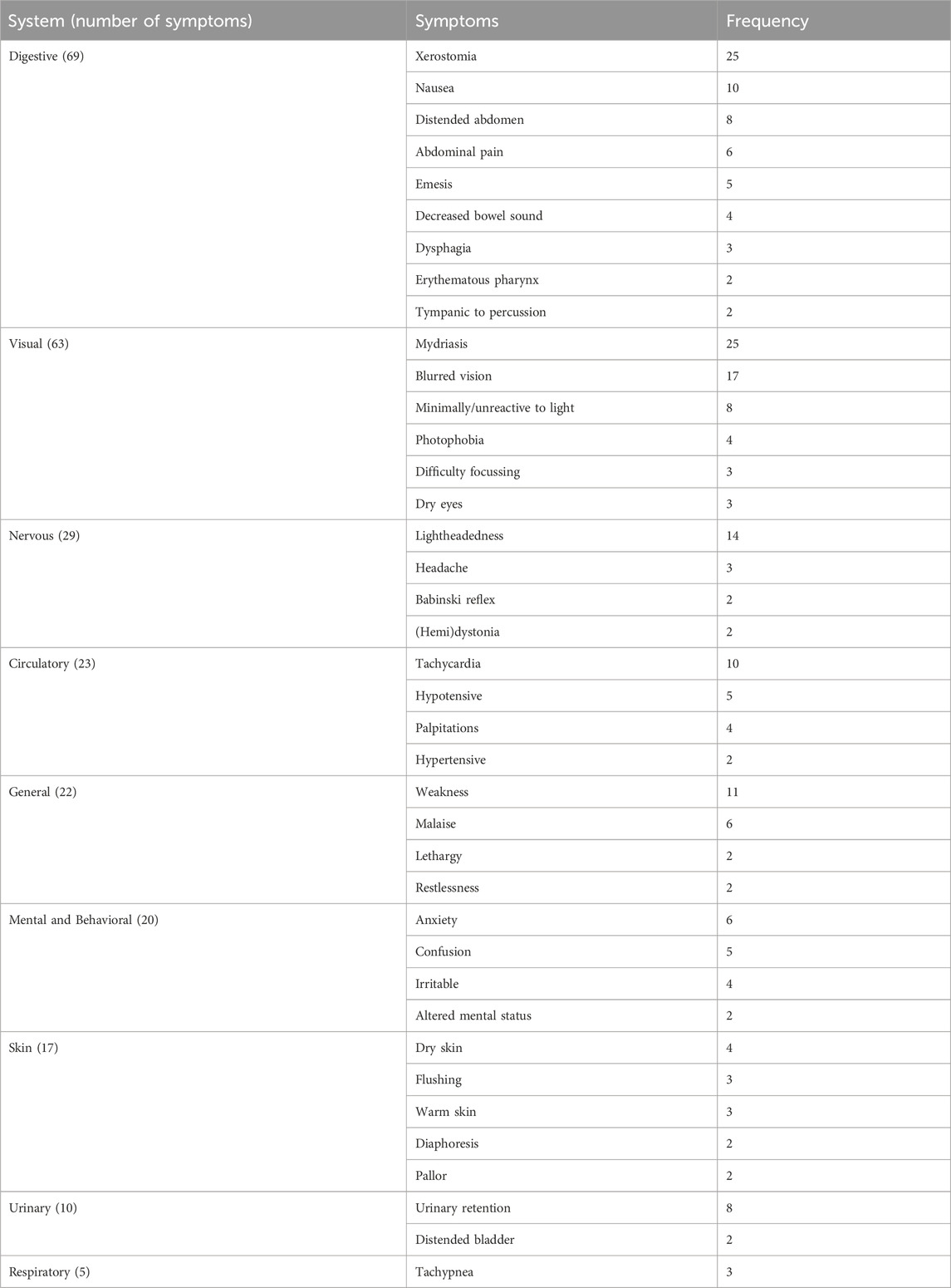
Table 2. Clinical symptoms associated with lupin poisoning. Only symptoms with n ≥ 2 are included in the table. All clinical symptoms per case are included in Supplementary Appendix 1. Symptoms are classified according to the ICD11 system.
58% of the patients recovered within 24 h (n = 19) after ingestion of lupin (Figure 4C), resulting in discharge from the hospital. Within these 24 h, most patients remained under observation but did not need any medical intervention. If any treatment was given, it was against one of the symptoms, like (urinary) catheterization (n = 4) for urinary retention and IV fluids (n = 9) to keep vitals stable (Table 1; Figure 4B). Gastric lavage or activated charcoal was mentioned a few times as an option to be used to prevent the alkaloids from absorbing. Gastric lavage was used twice and active charcoal once.
Two out of the four children described in the case reports ended up in the intensive care unit (Flores-Pamo et al., 2018; Ozkaya et al., 2021), but also recovered after a few days and were discharged eventually (Daverio et al., 2014) (Table 1). One of the children, a 1-year-old boy, died (Petraroia, 1926). All but one patient recovered completely. This case presented with an intake of lupin beans over the time course of 8 years (Agid et al., 1988). She gradually recovered in the 20 months after quitting eating the beans. She remained with some complaints after that. Given the relatively low intake compared to the other cases and the long time frame before the onset of symptoms, there might have been confounding etiologies. However, such were not described in the case report and symptoms disappeared after ending the intake of lupin beans.
Lupin beans are consumed more and more in today’s society. They are considered healthy and a substitute for soybeans (Pereira et al., 2022). However, when beans are not correctly stripped of the toxic alkaloids the beans can be toxic or even lethal (Lowen et al., 1995; Schmidlin-Mészáros, 1973; Petraroia, 1926). The high amount of alkaloids in the beans affect the parasympathetic nervous system and cause anticholinergic syndrome (Ozkaya et al., 2021; Luque Marquez et al., 1991). In this review the human case reports on lupin bean poisoning have been collected and data regarding the poisoning, symptoms and treatment were extracted.
The beans that were consumed that led to poisoning were L. albus and L. mutabilis. The poisoning symptoms generally occurred within 1 h after consumption of the beans, or the debittering water of the processing of the beans. Most common symptoms of poisoning were with dryness (mouth, eyes, skin), sight problems, abdominal problems, muscle (tension, contractions) and urinary retention. In most cases a wait and see policy was sufficient and patients recovered mostly within 24 h and were discharged. When treated, some patients got gastric lavage or activated charcoal as treatment to remove the beans from the stomach. To maintain stable vitals, some patients received IV fluids. In case of urinary retention patients received catheterization. Extra care should be taken with children, since a few cases described ICU admission or lethal outcome (Flores-Pamo et al., 2018; Ozkaya et al., 2021; Petraroia, 1926; Daverio et al., 2014).
In other cases, which we were not able to access the full-text paper, also pediatric death was described. The citation of these cases by Schmidlin-Mészáros (1973) describes a 10-year-old child that died after 3 h, with similar symptoms as described in our cases, e.g., mydriasis and convulsions. And a 1.5-year-old child that also died after eating 5–10 g of lupin beans. So, of all the reported poisoning in children (n = 6) three died, two were admitted to the ICU and one had toxication symptoms, but recovered on its own (Ozkaya et al., 2021; Flores-Pamo et al., 2018; Petraroia, 1926; Daverio et al., 2014; Schmidlin-Mészáros, 1973). While for all the adult cases reports, this has not occurred. Only one other case cited by Schmidlin-Mészáros (1973) describes an adult that got into a coma, but recovered. Obviously, case reports are only written on the out of the ordinary cases and possible confounding etiologies are not always described and some cases are from almost a century ago. But it is striking that children are more severely affected after poisoning than adults. Therefore, it might potentially be beneficial to treat children with gastric lavage soon after consumption to reduce the amount of alkaloids absorbed in the body and worsen the poisoning. Also, monitoring of vital signs is important, since for most cases the symptoms worsen over time.
Most alkaloids have a half-life within 12 h in humans, which aligns with the recovery of patients within 12–24 h in general. The alkaloids are partially metabolized via the liver and CYP2D6 (Schrenk et al., 2019). This enzyme is known to have polymorphisms, which can lead to a different rate in metabolism of the alkaloids. This might explain why some patients take more time to recover than others. Alkaloid concentrations between 10–50 mg/kg are estimated to cause poisoning, which might be even lower for children. It is not known how frequent lupin poisoning occurs, but probably not often, given that most consumed lupin beans are from the supermarket, and those are already debittered (Schrenk et al., 2019).
Besides lupin poisoning, lupin allergy also exists. An allergic reaction is not caused by alkaloids, but by conglutin proteins that result mainly in anaphylaxis, asthmatic or urticaria. Cross reactivity with peanut allergy is often seen. Lupin allergy is expected to affect a few percent of the population, although studies on lupin allergies are limited (Sanz et al., 2010; Villa et al., 2020). So, lupin allergy has a different clinical representation, and therefore also different treatment compared to poisoning.
A narrative review like this gives much insight in lupin poisoning by comparing the different case reports. However, we rely on the available information in the case reports. The reports often provide an elaborate description of the cases, but sometimes the description is limited. For example, the amount or type of lupin beans is not always described but would give valuable insight in lupin poisoning. So, the largest limitation in this study remains the availability of data.
Although lupin poisoning prevalence is low and outcomes are usually good, proper treatment can avoid symptoms going from bad to worse, definitely in children. With this review we aimed to describe the symptoms and treatment of lupin poisoning by extracting data of existing lupin poisoning case reports. Therewith we hope that healthcare professionals can diagnose and treat those patients as best as possible. And since it is expected more lupin will be consumed it is important to increase awareness and knowledge on lupin intoxication.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
MB: Supervision, Writing – original draft, Writing – review and editing, Data curation, Formal Analysis, Visualization. PC: Data curation, Formal Analysis, Visualization, Writing – original draft, Writing – review and editing. SG: Data curation, Formal Analysis, Writing – original draft, Writing – review and editing. SS: Data curation, Formal Analysis, Writing – original draft, Writing – review and editing. MJ: Data curation, Writing – original draft, Writing – review and editing. MW: Data curation, Writing – original draft, Writing – review and editing. MH: Writing – review and editing, Conceptualization, Methodology, Supervision, Writing – original draft.
The author(s) declare that no financial support was received for the research and/or publication of this article.
We want to thank M. Van der Veen for providing the photos of lupin for Figure 1.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/ftox.2025.1547535/full#supplementary-material
Agid, Y., Pertuiset, B., and Dubois, B. (1988). Motoneuron disease as manifestation of lupin seed toxicity. Lancet 1, 1347. doi:10.1016/s0140-6736(88)92169-1
Alessandro, L., Wibecan, L., Cammarota, A., and Varela, F. (2017). Pupillary disorders in the emergency room: lupinus mutabilis intoxication. J. Clin. Toxicol. 7, 360. doi:10.4172/2161-0495.1000360
Atchison, G. W., Nevado, B., Eastwood, R. J., Contreras-Ortiz, N., Reynel, C., Madriñán, S., et al. (2016). Lost crops of the Incas: origins of domestication of the Andean pulse crop tarwi, Lupinus mutabilis. Am. J. Bot. 103, 1592–1606. doi:10.3732/ajb.1600171
Awada, A., Atallah, D., and Zoghbi, A. (2011). Anticholinergic syndrome after intoxication by lupine seeds (Tourmos). J. Med. Liban. 59, 233–234.
Camacho Saavedra, L., and Uribe Uribe, L. (1995). Intoxicación por agua de Lupinus mutabilis (“Chocho”). Bol. Soc. Peru. Med. Interna 8, 35–37.
Carazo Barrios, L., and De La Fuente Cañete, C. (2022). Intoxicación por harina de altramuz: nuevas perspectivas a través de un caso clínico. Rev. Toxicol. 39, 33–35.
Carvajal-Larenas, F. E., Linnemann, A. R., Nout, M. J. R., Koziol, M., and Van Boekel, M. A. J. S. (2016). Lupinus mutabilis: composition, uses, toxicology, and debittering. Crit. Rev. Food Sci. Nutr. 56, 1454–1487. doi:10.1080/10408398.2013.772089
Cidad, P., D’Anna, O., Noval, S., Henríquez, M., and Armadá, F. (2013). Midriasis arreactiva bilateral tras intoxicación por Lupinus Mutabilis. Bol. Soc Oftalmo Madr., 53.
Daverio, M., Cavicchiolo, M. E., Grotto, P., Lonati, D., Cananzi, M., and Da Dalt, L. (2014). Bitter lupine beans ingestion in a child: a disregarded cause of acute anticholinergic toxicity. Eur. J. Pediatr. 173, 1549–1551. doi:10.1007/s00431-013-2088-2
Di Grande, A., Paradiso, R., Amico, S., Fulco, G., Fantauzza, B., and Noto, P. (2004). Anticholinergic toxicity associated with lupin seed ingestion: case report. Eur. J. Emerg. Med. 11, 119–120. doi:10.1097/00063110-200404000-00014
Eckstein, R. L., Welk, E., Klinger, Y. P., Lennartsson, T., Wissman, J., Ludewig, K., et al. (2023). Biological flora of central Europe – lupinus polyphyllus lindley. Perspect. Plant Ecol. Evol. Syst. 58, 125715. doi:10.1016/j.ppees.2022.125715
Flores-Pamo, A. E., Pisano, E., and Carreazo, N. Y. (2018). Anticholinergic toxicity in a one-year-old male following ingestion of Lupinus mutabilis seeds: case report. Sao Paulo Med. J. 136, 591–593. doi:10.1590/1516-3180.2016.0157220517
Huyghe, C. (1997). White lupin (Lupinus albus L.). Field Crops Res. 53, 147–160. doi:10.1016/S0378-4290(97)00028-2
Jamali, S. (2011). Dilated pupils, dry mouth and dizziness - a case study. Aust. Fam. Phys. 40 (10), 789–790.
Kurlovich, B. (2024). The history of Lupins domestication. Available online at: https://sites.google.com/site/biodiversityoflupins/16-the-history-of-lupins-domestication (Accessed July 15, 2024).
Lahoud, C., Hanna, N. G., Jalkh, A., and Azar, G. (2021). Acute bilateral fixed mydriasis caused by lupini bean intoxication. Wilderness Environ. Med. 32, 217–220. doi:10.1016/j.wem.2021.01.003
Li, K., Van Wijk, X. M. R., Hayashi, S., Lynch, K. L., Wu, A. H. B., and Smollin, C. G. (2017). Anticholinergic toxicity associated with ingestion of water containing lupini bean extract. Clin. Toxicol. 55, 687–688. doi:10.1080/15563650.2017.1315821
Litkey, J., and Dailey, M. W. (2007). Anticholinergic toxicity associated with the ingestion of lupini beans. Am. J. Emerg. Med. 25, 215–217. doi:10.1016/j.ajem.2006.08.004
Lorente Esparza, C., Pérez Laencina, L., Ballarín Naya, L., Real Torrijos, M., Oliveira Brito, M., and Vera Colás, M. (2021). Intoxicación por agua de cocción de “chochos” o altramuces. Rev. Sanit. Investig. 5.
Lowen, R. J., Alam, F. K., and Edgar, J. A. (1995). Lupin bean toxicity. Med. J. Aust. 162, 256–257. doi:10.5694/j.1326-5377.1995.tb139879.x
Lucas, M. M., Stoddard, F. L., Annicchiarico, P., Frias, J., Martinez-Villaluenga, C., Sussmann, D., et al. (2015). The future of lupin as a protein crop in Europe. Front. Plant Sci. 6, 705–706. doi:10.3389/fpls.2015.00705
Luque Marquez, R., Gutierrez-Rave, M., and Infante Miranda, F. (1991). Acute poisoning by lupine seed debittering water. Vet. Hum. Toxicol. 33, 265–267.
Malmgren, L., RoséN, J., Dahlman, D., and Von Wowern, F. (2016). Leguminous plant causes poisoning with anticholinergic syndrome. Lakartidningen 113:DY6T.
Moreno GonzáLEZ, M., and Del CañO Garrido, A. (2021). Intoxicación tras ingesta de sopa de altramuces. Valoración en el servicio de urgencias. Caso clínico. Rev. Electrónica PortalesMedicos.com 16, 963.
Ortega Duarte, A., Martin-Sanchez, F. J., Gonzalez-Castillo, J., and Ruiz-Artacho, P. (2013). Intoxicación por «agua de chocho. Med. Clínica 140, 43–44. doi:10.1016/j.medcli.2012.05.023
Ozkaya, P., Ari, H., Turanli, E., Koc, G., and Karapinar, B. (2021). Severe lupin bean intoxication: an anticholinergic toxidrome. Pediatr. Emerg. Med. J. 8, 108–111. doi:10.22470/pemj.2021.00262
Pereira, A., Ramos, F., and Sanches Silva, A. (2022). Lupin (Lupinus albus L.) seeds: balancing the good and the bad and addressing future challenges. Molecules 27, 8557. doi:10.3390/molecules27238557
Petraroia, M. (1926). Su di un caso letale ci lupinosi nell’uomo (avvelenamento per ingestione di semi secchi di lupino). Il Policlin. Sezione Prat. Period. Med. Chir. Ig. 33, 1356–1366.
Pingault, N. M., Gibbs, R. A., Barclay, A. M., and Monaghan, M. (2009). Two cases of anticholinergic syndrome associated with consumption of bitter lupin flour. Med. J. Aust. 191, 173–174. doi:10.5694/j.1326-5377.2009.tb02732.x
Resta, D., Boschin, G., D’Agostina, A., and Arnoldi, A. (2008). Evaluation of total quinolizidine alkaloids content in lupin flours, lupin-based ingredients, and foods. Mol. Nutr. Food Res. 52, 490–495. doi:10.1002/mnfr.200700206
Sanz, M. L., De Las Marinas, M. D., Fernández, J., and Gamboa, P. M. (2010). Lupin allergy: a hidden killer in the home. Clin. Exp. Allergy 40, 1461–1466. doi:10.1111/j.1365-2222.2010.03590.x
Schmidlin-Mészáros, J. (1973). Eine Nahrungsmittelvergiftung mit Lupinenbohnen. Mittl. aus dem Geb. Leb. Hyg. 64, 194–205.
Schrenk, D., Bodin, L., Chipman, J. K., Del Mazo, J., Grasl-Kraupp, B., Hogstrand, C., et al. (2019). Scientific opinion on the risks for animal and human health related to the presence of quinolizidine alkaloids in feed and food, in particular in lupins and lupin-derived products. Efsa J. 17, e05860. doi:10.2903/j.efsa.2019.5860
Tsiodras, S., Shin, R. K., Christian, M., Shaw, L. M., and Sass, D. A. (1999). Anticholinergic toxicity associated with lupine seeds as a home remedy for diabetes mellitus. Ann. Emerg. Med. 33, 715–717. doi:10.1016/S0196-0644(99)80012-2
Van Der Veen, M. (2011). Consumption, trade and innovation: exploring the botanical remains from the Roman and Islamic ports at Quseir al-Qadim. Frankfurt, Egypt: Africa Magna Verlag.
Villa, C., Costa, J., and Mafra, I. (2020). Lupine allergens: clinical relevance, molecular characterization, cross-reactivity, and detection strategies. Compr. Rev. Food Sci. Food Saf. 19, 3886–3915. doi:10.1111/1541-4337.12646
Vivancos Gallego, M. J., and Machín, E. (2014). Intoxicación por “agua de cocción de chochos”. Rev. Esp. Nutr. Comunitaria 20, 35–36. doi:10.7400/RENC.2014.01.1.5007
Keywords: lupin, alkaloid, L. albus, L. mutabilis, anticholinergic syndrome, ACS, poisoning, intoxication
Citation: Bloothooft M, Cremers P, Güven S, Stoutjesdijk SJ, Jiron M, Wessel M and Van Der Heyden MAG (2025) Lupin poisoning: a review. Front. Toxicol. 7:1547535. doi: 10.3389/ftox.2025.1547535
Received: 18 December 2024; Accepted: 24 March 2025;
Published: 09 April 2025.
Edited by:
Sascha Rohn, Technical University of Berlin, GermanyReviewed by:
Claude Lambre, Institut National de la Santé et de la Recherche Médicale (INSERM), FranceCopyright © 2025 Bloothooft, Cremers, Güven, Stoutjesdijk, Jiron, Wessel and Van Der Heyden. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marcel A. G. Van Der Heyden, bS5hLmcudmFuZGVyaGV5ZGVuQHVtY3V0cmVjaHQubmw=
†ORCID: Marcel A. G. Van Der Heyden, orcid.org/0000-0002-4225-7942
‡These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.