
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Syst. Neurosci. , 12 February 2021
Volume 14 - 2020 | https://doi.org/10.3389/fnsys.2020.600582
Background: This comprehensive meta-analysis aimed to assess whether an increased homocysteine (Hcy) level is an independent predictor of unfavorable outcomes in acute ischemic stroke (AIS) patients.
Methods: A comprehensive literature search was conducted up to August 1, 2020 to collect studies reporting Hcy levels in AIS patients. We analyzed all the data using Review Manager 5.3 software.
Results: Seventeen studies with 15,636 AIS patients were selected for evaluation. A higher Hcy level was associated with a poorer survival outcome (OR 1.43, 95% CI: 1.25–1.63). Compared with the AIS group, Hcy levels were significantly lower in the healthy control patients, with an SMD of 5.11 and 95% CI (1.87–8.35). Analysis of the different subgroups of AIS demonstrated significant associations between high Hcy levels and survival outcomes only in Caucasian and Asian patients. Moreover, whereas high Hcy levels were closely associated with gender, B12 deficiency, smoking, and patients who received tissue plasminogen activator treatment, no significant difference was found between increased Hcy levels and age, drinking, hypertension, diabetes mellitus, and hyperlipidemia. In addition, the cut-off value (20.0 μmol/L) might be an optimum cut-off index for AIS patients in clinical practice.
Conclusion: This meta-analysis reveals that the Hcy level may serve as an independent predictor for unfavorable survival outcomes in AIS patients, particularly in Caucasian and Asian AIS patients. Further studies can be conducted to clarify this relationship.
Acute ischemic stroke (AIS) occurs primarily because of atherothrombotic or embolic vascular obstruction in vessels supplying blood to the brain, leading to the death of brain tissue and focal neurological deficits and is a serious public health concern (Smith et al., 2019; Jensen and Thomalla, 2020; Phipps and Cronin, 2020). It is the main cause of physical disability and the second leading cause of death worldwide, especially in developing countries (Feigin et al., 2015; Virani et al., 2020). Therefore, the identification of modifiable risk factors for the early screening, prognostic evaluation, and intensive treatment of AIS are in active demand.
In the past year, numerous epidemiological studies have supported that homocysteine (Hcy) is a non-traditional risk factor for ischemic stroke (Homocysteine Studies, 2002; Schwammenthal and Tanne, 2004). Elevated Hcy levels at AIS onset might also be related to increased hematoma volume, and increased Hcy levels may cause endothelial dysfunction, neurotoxicity, and the upregulation of thrombosis formation factors (Luo et al., 2019). For the past decade, numerous studies have also confirmed that elevated Hcy levels are associated with functional disability for AIS and recurrent strokes (He et al., 2014). A multicenter study performed by Kwon et al. revealed that high levels of serum HCY were independent predictors of early neurological deterioration in AIS patients (Kwon et al., 2014).
Nevertheless, it is unknown whether Hcy is an independent risk parameter for worse clinical outcome in AIS patients. Although the high expression of Hcy in AIS patients has been reported, its effectiveness in prognosis prediction is still under debate. Some results confirmed that Hcy in fact correlated with worse outcomes of AIS (Ling et al., 2018; Luo et al., 2019), whereas some other studies indicated that elevated Hcy levels are not significantly associated with or an independent predictor of AIS patients' clinical outcome (Bushnell and Goldstein, 2002; Ribo et al., 2004; Wang et al., 2017).
The best method to judge and evaluate Hcy in clinical practice remains under debate. Furthermore, the roles of Hcy levels in AIS patients' clinical outcomes have not been thoroughly explored. In this work, we aim to conduct a systematic evaluation of the prognostic value of Hcy levels in relation to AIS risk.
A comprehensive search was conducted in PubMed, Cochrane, Embase, and Web of Science for relevant articles published up to August 1, 2020. The search terms were (Hcy OR homocysteine OR tHcy OR total homocysteine OR hyperhomocysteimia OR HHcy) AND (“Acute ischaemic stroke” OR AIS OR ischaemic stroke OR IS OR stroke) and “outcome or clinical outcome or survival outcome or prognosis or prognostic.”
The following criteria were used to select eligible studies: (1) Hcy level evaluated in AIS patients, (2) assessment of the correlation between Hcy level and the pathogenesis of AIS, (3) sufficient and effective information to extract the OR of outcome and 95% CIs, and (4) published in English with peer review. We excluded the following studies: (1) duplicate data presented at conferences and in case reports; (2) reviews, invalid data, or abstracts only; (3) studies of animal models; and (4) studies with insufficient data to obtain ORs and no clear Hcy results. For duplicate publications, only the most recent comprehensive results with the highest-quality size were selected.
We extracted data on the study population (the first author's name, publication date, and country) and sample parameters [number of cases, median or mean of patient age, sex, tissue plasminogen activator (tPA) treatment, smoking, drinking, hypertension, diabetes mellitus, hyperlipidemia, cut-off value of Hcy levels]. If the results of multivariate analysis and univariate analysis were both provided, the former was selected. All data were obtained by two independent observers (SMH and YJT). Study quality was assessed according to the NOS criteria for retrospective studies (Stang, 2010). If data could not be extracted from the article, we considered the relevant data not available.
Review Manager 5.3 (the Cochrane Collaboration) and STATA 16.0 (Stata Corporation) were used for the analysis. The pooled OR and its corresponding 95% CI were determined to assess the correlation between Hcy level and AIS patient outcome. ORs and 95% CIs were used to evaluate the relationships between Hcy level and clinical characteristics, including sex, smoking, drinking, tPA, hypertension, diabetes mellitus, and hyperlipidemia. Heterogeneity among these studies was assessed using the I2 statistic (Zintzaras and Ioannidis, 2005). A fixed-effects model (Mantel–Haenszel method) was used to calculate pooled ORs when there was no significant heterogeneity among studies (I2 > 50% suggested high heterogeneity); otherwise, the random-effects model was used. A p-value < 0.05 was considered to indicate significance. Publication bias was assessed using funnel plots and Egger's test (Peters et al., 2006).
The initial search identified 236 articles. Eventually, 17 articles published from 2001 to 2020 were included (Fallon et al., 2001; Sacco et al., 2004; Mizrahi et al., 2005; Perini et al., 2005; Yoldas et al., 2007; Okubadejo et al., 2008; Tu et al., 2013; Unal et al., 2013; Kwon et al., 2014; Shi et al., 2015; Forti et al., 2016; Tang et al., 2016; Yao et al., 2016; Markaki et al., 2017; Zhong et al., 2017; Alfieri et al., 2020; Li L. et al., 2020) (Figure 1). All studies reported follow-up time. Four of them were retrospective studies, and the remaining 13 were prospective studies. One prospective cohort included only men (Fallon et al., 2001), and one retrospective study cohort included only women (Markaki et al., 2017).
Of the 17 studies, six were conducted in China, two in Italy, two in Turkey, one in South Africa, one in Israel, one in the USA, one in Sweden, one in Brazil, one in Nigeria, and one in South Korea. The characteristics of these 17 studies and of a study of high methodological quality according to guidelines developed by the Newcastle–Ottawa Scale are shown in Table 1. Differences in the cut-off value for Hcy level were observed among the studies.
Of the 15 studies that evaluated the association between Hcy level and AIS survival outcome, six involved Caucasian patients (n = 4,981), seven involved Asian patients (n = 8254), and two involved African patients (n = 2,323).
The comprehensive OR for 13 prospective studies was 1.53 (95% CI 1.27–1.86, p < 0.0001, I2 = 85%, Figure 2A). The comprehensive OR for four retrospective studies was 2.49 (95% CI 1.04–5.96, p < 0.0001, I2 = 86%, Figure 2A). The comprehensive OR for all AIS patient outcomes was 1.43 (95% CI 1.25–1.63, p < 0.0001, I2 = 89%, Figure 2A and Table 2).
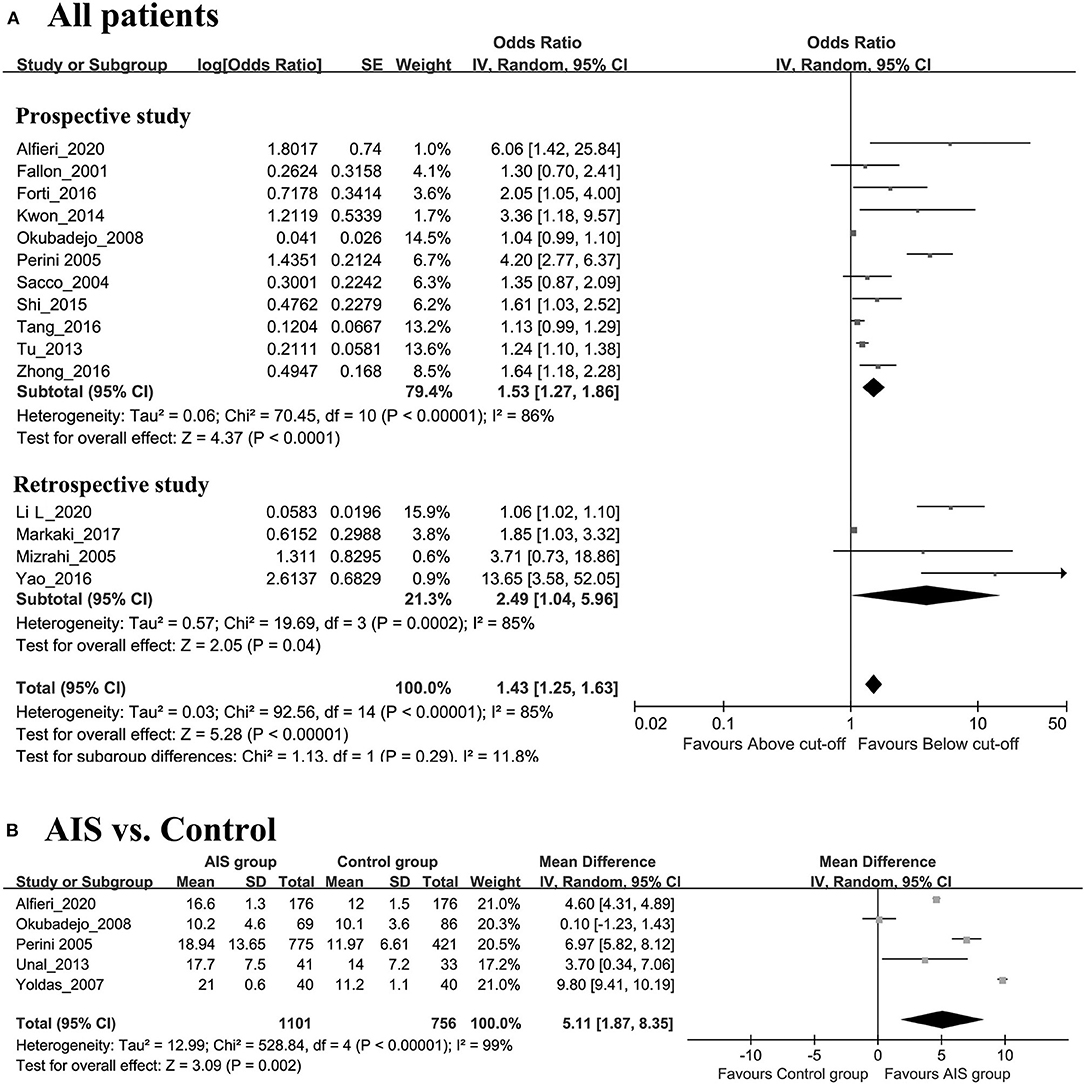
Figure 2. (A) Forest plot of study-specific relative risk statistics for AIS comparing the highest and lowest Hcy category group. (B) Forest plots of the subgroup analyses on sample size in relation to Hcy levels between AIS patients and healthy controls.
As shown in Figure 2B, the AIS group had significantly higher levels of Hcy than the control group (SMD = 5.11, 95% CI = 1.87–8.35, p = 0.002). The results of subgroup analyses on ethnicity showed that the associations were statistically significant in both Caucasian and Asian patients (Caucasian: OR 3.56, 95% CI 2.54–4.98, p < 0.00001, I2 = 20%, Figure 3A; Asian: HR 1.39, 95% CI 1.19–1.63, p < 0.00001, I2 = 86%, respectively, Figure 3B) but not in African patients (OR 1.04, 95% CI 0.99–1.10, p = 0.11) (Figure 3C).
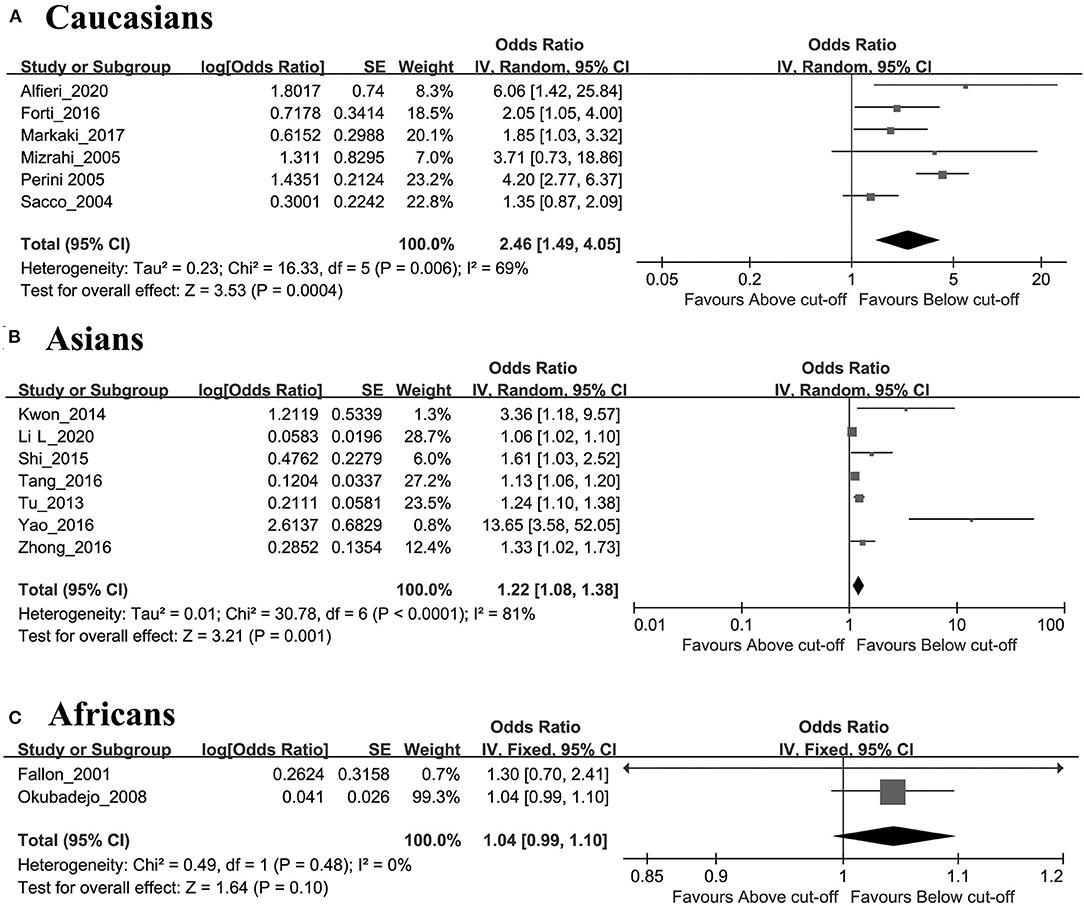
Figure 3. Forest plots of the subgroup analyses on ethnicity in relation to Hcy levels and risk of AIS patients: (A) Caucasians, (B) Asians, (C) Africans.
Five studies investigated the association of clinical characteristics such as sex and hypertension with elevated Hcy levels. Four studies investigated the relationship between smoking and Hcy levels. Three studies assessed the relationship between age and Hcy levels. Two studies assessed the association of clinical characteristics such as drinking, tPA, diabetes mellitus, and hyperlipidemia with elevated Hcy levels. One study assessed the relationship between B12 deficiency and Hcy levels (Table 3).
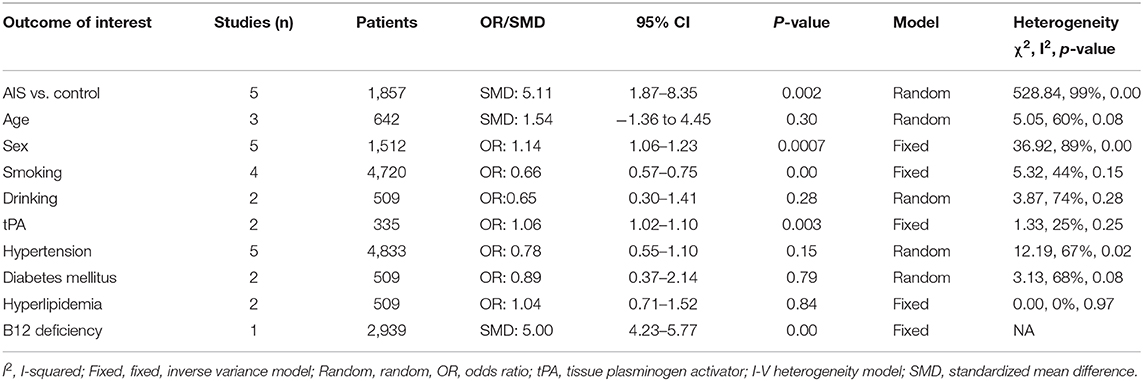
Table 3. Results of subgroup analysis of the association between Hcy level and clinic parameters in AIS.
There were statistically significant differences between Hcy levels in relation to sex, smoking, tPA, and B12 deficiency. The pooled ORs were as follows: OR 1.14, p = 0.0007; OR 0.66, p < 0.001; OR 1.06, p = 0.003; and SMD 5.0, p < 0.001, respectively. There were no significant differences in relation to the Hcy level and age, drinking, hypertension, diabetes mellitus, or hyperlipidemia in AIS patients. The pooled ORs were as follows: (SMD 1.54, p = 0.30; OR 0.65, p = 0.28; OR 0.78, p = 0.15; OR 0.89, p = 0.79; and OR 1.04, p = 0.84, respectively) (Table 3).
Analysis data for all cut-offs (including 13.0, 16.5, and 20.0 μmol/L) were used to elucidate the optimal cut-off of the Hcy level. The combined ORs and 95% CIs were as follows: 1.33 (95% CI 0.86–2.07) vs. 1.71 (95% CI 1.36–2.17) for a cut-off value of 13.0 μmol/L (Supplementary Figure 1), 1.29 (95% CI 1.13–1.49) vs. 2.62 (95% CI 0.74–9.33) for a cut-off value of 16.5 μmol/L (Supplementary Figure 2), and 1.96 (95% CI 1.39–2.75) vs. 1.59 (95% CI 1.16–2.19) for a cut-off value of 20.0 μmol/L (Supplementary Figure 3). In terms of both low and high cut-off values to assess high Hcy reactivity, subgroup analysis uncovered a significant correlation of high Hcy reactivity with worse survival outcome (p < 0.05, Supplementary Table 1).
The cut-off value (20.0 μmol/L) resulted in a significantly higher association with outcome than other values, indicating that the cut-off value (20.0 μmol/L) might be a superior cut-off index for clinical practice.
Publication bias was calculated by Begg's test and Egger's test for the outcome of AIS. Begg's test (p = 0.244) and Egger's test (p = 0.171) suggested that our results were stable (Figure 4).
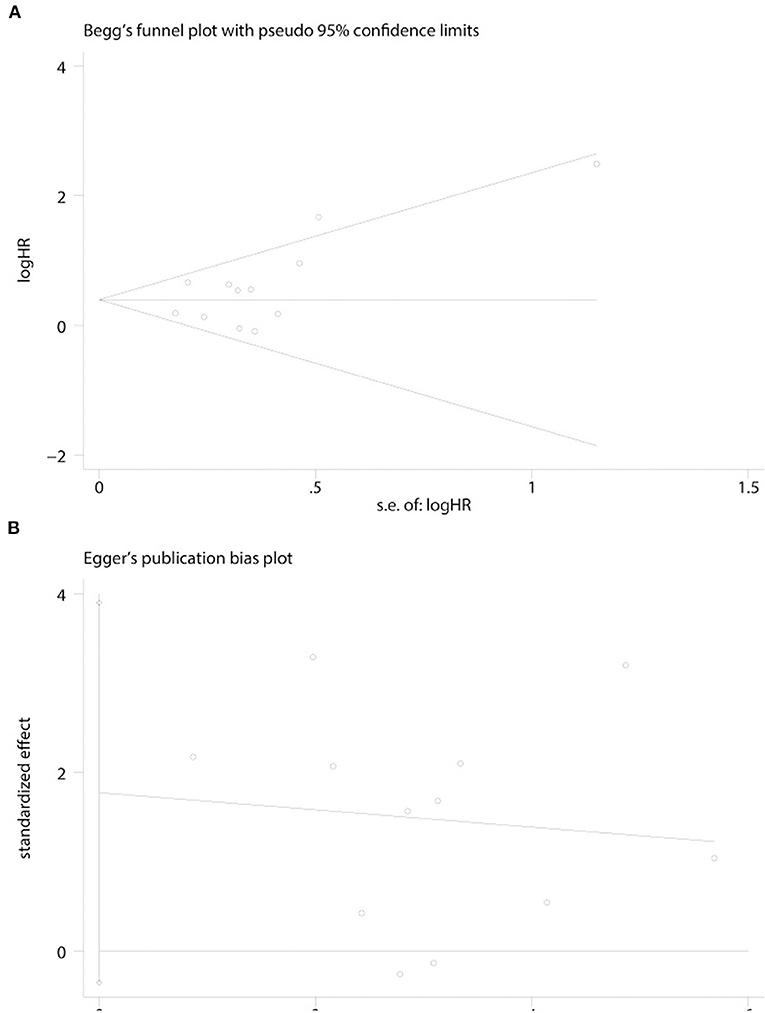
Figure 4. Funnel plots were used to evaluate publication bias on survival outcome. (A) Begg's test was not significant, intending no significant bias was observed on survival outcome. (B) Egger's test was not significant, intending no significant bias was observed on survival outcome.
Hcy is a sulfur-containing amino acid that is widely known to be involved in the pathogenesis of multiple clinical conditions. Elevated Hcy levels have been shown to be related to cardiovascular disease, Alzheimer dementia, and cerebrovascular diseases, suggesting endothelial dysfunction as a major mechanism (Hooshmand et al., 2013; Chrysant and Chrysant, 2018). Moreover, reports have demonstrated the increased risk of stroke in individuals homozygous for the MTHFR T allele is close to the result predicted by the differences in homocysteine concentration given by this variant (Casas et al., 2005). In addition, the elevated level of Hcy promotes neural stem cell autophagy in both in vivo and in vitro models of AIS (Wang et al., 2019). However, the relationship between Hcy and prognosis remains unclear, and the roles and clinical implications of Hcy levels in AIS have not been thoroughly studied.
In our meta-analysis, the pooled data indicated the following: (1) AIS patients with a higher Hcy level had a worse survival outcome, and the Hcy level was higher in AIS patients than in healthy controls; (2) a high Hcy level was associated with sex and smoking and was not strongly associated with drinking, hypertension, diabetes mellitus, age, and hyperlipidemia in AIS patients; and (3) the cut-off value of 20.0 μmol/L might be superior to other cut-off values for clinical practice. (4) Hcy may serve as an independent risk factor influencing the survival outcome of AIS patients, particularly in Caucasians and Asians. Furthermore, our findings highlight that the Hcy level is a prognostic factor for AIS and suggest that thrombolytic therapy may be helpful in the high-risk subgroup of patients (Yao et al., 2016; Li L. et al., 2020).
In addition, we found a significant association between Hcy levels and vitamin B12 deficiency. In a subgroup analysis among 2,939 subjects, the effect of tHcy remained significant on conventional serum vitamin B12 levels. Several studies have shown that daily vitamin B supplementation has a significant protective effect on recent stroke or transient ischemic attack (Huang et al., 2012). One issue that needs to be addressed is to identify the impact of modifiable risk factors (i.e., hyperhomocysteinemia) on clinical practice, such as suggesting homocysteine-lowering interventions, like supplementation with B vitamins, to improve the prognosis of AIS patients or to reduce the risk of stroke in primary prevention in the high-risk subgroup of patients.
The biological role of Hcy explains its survival outcome and clinical role in AIS. Elevated Hcy levels suggest severe neuropathy and an increased volume of hemorrhage (Shandal and Luo, 2016; Zhou et al., 2018) because elevated plasma homocysteine can cause injury to vascular wall integrity and cerebrovascular permeability, which may result in endothelial dysfunction, elastic structure damage, and vascular endothelial damage and further damage the basic layer of cerebral arterioles and microvessels (Fan et al., 2017). Hyperhomocysteinemia has been widely regarded as an important risk factor in the formation of atherosclerosis, indicating that elevated Hcy levels are closely related to endothelial dysfunction (Lu et al., 2018; Borowczyk et al., 2019). Furthermore, high levels of Hcy also increase LDL oxidation, and the main mechanism of Hcy adverse effects on vascular endothelial function involves oxidative stress and the consumption of bioactive nitric oxide (Seo et al., 2010; AnandBabu et al., 2019).
Our results confirmed that high Hcy level was related to the gender of AIS patients. Moreover, gender has been shown to have an effect on the level of Hcy (Li J. et al., 2020), and recent studies have shown that there are significant gender differences in the relationship between Hcy and the risk of ischemic stroke disease (Zhong et al., 2017; Foscolou et al., 2019). Therefore, there may be a sex-specific correlation between Hcy and functional disability or cardiovascular events in patients with AIS.
The data demonstrated that the cut-off point of 20 μmol/L was superior to the cut-off points of 13.0 and 16.5 μmol/L in AIS patients. Several epidemiological studies have indicated that a wide range of cut-off points for Hcy is a modifiable risk factor. The present results indicated that the elevated Hcy levels to 18.6 μmol/L had a 1.61-fold increased risk of death compared with patients in the lowest quartile (10 μmol/L) (Shi et al., 2015). Based on the meta-analysis, we judged that the optimal cut-off value of Hcy was 20.0 μmol/L, and a similar cut-off point for Hcy (23.85 μmol/L) was shown by Yao et al. (2016). Thus, a cut-off point of 20.0 μmol/L Hcy is the most effective risk factor for AIS patients.
In addition, subgroup analysis by ethnicity revealed that in both Caucasians and Asians, the level of serum Hcy was significantly related to the survival time of AIS patients but not in African ASI patients. The inconsistency may be related to factors such as environment, lifestyles, and living conditions.
Our study also has some limitations. First, the employed methods for detecting serum Hcy levels and cut-off values differed, which may result in sensitivity and reliability issues. Second, clinical factors including blood pressure, blood glucose, smoking, drinking, diabetes mellitus, hypertension, and hyperlipidemia in each study may lead to bias. These variances may have produced heterogeneity in this study. Third, there was a small study impact due to the limited sample size of our study. There is thus certainly a need for large-scale trials to investigate the roles of other factors that are likely to cause AIS.
This meta-analysis is the first study to systematically assess the correlation of the Hcy level with clinical characteristics and its prognostic role in AIS. Elevated Hcy levels may contribute to disease progression and are a significant risk factor affecting survival outcome, and the reliable convenience and low cost of Hcy measurement should further facilitate its wider application in patients with AIS. The evaluation of the Hcy level should raise the possibility of employing an aggressive treatment strategy.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
SH, JC, and YT wrote the main manuscript text and approved it. All authors contributed to the article and approved the submitted version.
This study was supported by Luohe youth top notch talent plan (grant no. LBJZ201601), Key R & D and promotion projects of Henan science and technology department in 2018 (grant no. 182102310229), and Medical science and technology research plan of Henan Province (grant no. LHGJ20191412).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnsys.2020.600582/full#supplementary-material
Alfieri, D. F., Lehmann, M. F., Flauzino, T., de Araujo, M. C. M., Pivoto, N., Tirolla, R. M., et al. (2020). Immune-inflammatory, metabolic, oxidative, and nitrosative stress biomarkers predict acute ischemic stroke and short-term outcome. Neurotox. Res. 38, 330–343. doi: 10.1007/s12640-020-00221-0
AnandBabu, K., Sen, P., and Angayarkanni, N. (2019). Oxidized ldl, homocysteine, homocysteine thiolactone, and advanced glycation end products act as pro-oxidant metabolites inducing cytokine release, macrophage infiltration, and pro-angiogenic effect in arpe-19 cells. PLoS ONE 14:e0216899. doi: 10.1371/journal.pone.0216899
Borowczyk, K., Piechocka, J., Glowacki, R., Dhar, I., Midtun, O., Tell, G. S., et al. (2019). Urinary excretion of homocysteine thiolactone and the risk of acute myocardial infarction in coronary artery disease patients: the wenbit trial. J. Intern. Med. 285, 232–244. doi: 10.1111/joim.12834
Bushnell, C. D., and Goldstein, L. B. (2002). Homocysteine testing in patients with acute ischemic stroke. Neurology 59, 1541–1546. doi: 10.1212/01.WNL.0000034173.19459.D0
Casas, J. P., Bautista, L. E., Smeeth, L., Sharma, P., and Hingorani, A. D. (2005). Homocysteine and stroke: evidence on a causal link from mendelian randomisation. Lancet 365, 224–232. doi: 10.1016/S0140-6736(05)70152-5
Chrysant, S. G., and Chrysant, G. S. (2018). The current status of homocysteine as a risk factor for cardiovascular disease: a mini review. Expert. Rev. Cardiovasc. Ther. 16, 559–565. doi: 10.1080/14779072.2018.1497974
Fallon, U. B., Elwood, P., Ben-Shlomo, Y., Ubbink, J. B., Greenwood, R., and Smith, G. D. (2001). Homocysteine and ischaemic stroke in men: the caerphilly study. J. Epidemiol. Community Health. 55, 91–96. doi: 10.1136/jech.55.2.91
Fan, C. D., Sun, J. Y., Fu, X. T., Hou, Y. J., Li, Y., Yang, M. F., et al. (2017). Astaxanthin attenuates homocysteine-induced cardiotoxicity in vitro and in vivo by inhibiting mitochondrial dysfunction and oxidative damage. Front. Physiol. 8:1041. doi: 10.3389/fphys.2017.01041
Feigin, V. L., Mensah, G. A., Norrving, B., Murray, C. J., Roth, G. A., and Group G. B. D. Stroke Panel Experts (2015). Atlas of the global burden of stroke (1990–2013): the gbd 2013 study. Neuroepidemiology 45, 230–236. doi: 10.1159/000441106
Forti, P., Maioli, F., Arnone, G., Coveri, M., Pirazzoli, G. L., Zoli, M., et al. (2016). Homocysteinemia and early outcome of acute ischemic stroke in elderly patients. Brain Behav. 6:e00460. doi: 10.1002/brb3.460
Foscolou, A., Rallidis, L. S., Tsirebolos, G., Critselis, E., Katsimardos, A., Drosatos, A., et al. (2019). The association between homocysteine levels, mediterranean diet, and cardiovascular disease: a case-control study. Int. J. Food. Sci. Nutr. 70, 603–611. doi: 10.1080/09637486.2018.1547688
He, Y., Li, Y., Chen, Y., Feng, L., and Nie, Z. (2014). Homocysteine level and risk of different stroke types: a meta-analysis of prospective observational studies. Nutr. Metab. Cardiovasc. Dis. 24, 1158–1165. doi: 10.1016/j.numecd.2014.05.011
Homocysteine Studies, Collaboration (2002). Homocysteine and risk of ischemic heart disease and stroke: a meta-analysis. JAMA 288, 2015–2022. doi: 10.1001/jama.288.16.2015
Hooshmand, B., Polvikoski, T., Kivipelto, M., Tanskanen, M., Myllykangas, L., Erkinjuntti, T., et al. (2013). Plasma homocysteine, alzheimer, and cerebrovascular pathology: a population-based autopsy study. Brain 136, 2707–2716. doi: 10.1093/brain/awt206
Huang, T., Chen, Y., Yang, B., Yang, J., Wahlqvist, M. L., and Li, D. (2012). Meta-analysis of b vitamin supplementation on plasma homocysteine, cardiovascular, and all-cause mortality. Clin. Nutr. 31, 448–454. doi: 10.1016/j.clnu.2011.01.003
Jensen, M., and Thomalla, G. (2020). Causes and secondary prevention of acute ischemic stroke in adults. Hamostaseologie 40, 22–30. doi: 10.1055/s-0039-1700502
Kwon, H. M., Lee, Y. S., Bae, H. J., and Kang, D. W. (2014). Homocysteine as a predictor of early neurological deterioration in acute ischemic stroke. Stroke 45, 871–873. doi: 10.1161/STROKEAHA.113.004099
Li, J., Wang, Y., Li, H., Zuo, Z., Lin, J., Wang, A., et al. (2020). Homocysteine level predicts response to dual antiplatelet in women with minor stroke or transient ischemic attack: subanalysis of the chance trial. Arterioscler. Thromb. Vasc. Biol. 40, 839–846. doi: 10.1161/ATVBAHA.119.313741
Li, L., Ma, X., Zeng, L., Pandey, S., Wan, R., Shen, R., et al. (2020). Impact of homocysteine levels on clinical outcome in patients with acute ischemic stroke receiving intravenous thrombolysis therapy. PeerJ 8:e9474. doi: 10.7717/peerj.9474
Ling, C., Hong, Z., Yu, W., Yu, L., and Xin, S. (2018). The serum homocysteine level in patients with acute ischemic stroke (ais) after thrombolysis and its relationship with clinical outcomes. Rev. Assoc. Med. Bras. (1992) 64, 438–442. doi: 10.1590/1806-9282.64.05.438
Lu, S., Deng, J., Liu, H., Liu, B., Yang, J., Miao, Y., et al. (2018). Pkm2-dependent metabolic reprogramming in cd4(+) t cells is crucial for hyperhomocysteinemia-accelerated atherosclerosis. J. Mol. Med. (Berl.) 96, 585–600. doi: 10.1007/s00109-018-1645-6
Luo, Y., Jin, H., Guo, Z. N., Zhang, P., Zhang, L. Y., Chen, J., et al. (2019). Effect of hyperhomocysteinemia on clinical outcome and hemorrhagic transformation after thrombolysis in ischemic stroke patients. Front. Neurol. 10:592. doi: 10.3389/fneur.2019.00592
Markaki, I., Klironomos, S., Kostulas, K., and Sjostrand, C. (2017). Elevated plasma homocysteine upon ischemic stroke is associated with increased long-term mortality in women. PLoS ONE. 12:e0183571. doi: 10.1371/journal.pone.0183571
Mizrahi, E. H., Fleissig, Y., Arad, M., and Adunsky, A. (2005). Plasma homocysteine level and functional outcome of patients with ischemic stroke. Arch. Phys. Med. Rehabil. 86, 60–63. doi: 10.1016/j.apmr.2004.01.031
Okubadejo, N. U., Oladipo, O. O., Adeyomoye, A. A., Awosanya, G. O., and Danesi, M. A. (2008). Exploratory study of plasma total homocysteine and its relationship to short-term outcome in acute ischaemic stroke in nigerians. BMC Neurol. 8:26. doi: 10.1186/1471-2377-8-26
Perini, F., Galloni, E., Bolgan, I., Bader, G., Ruffini, R., Arzenton, E., et al. (2005). Elevated plasma homocysteine in acute stroke was not associated with severity and outcome: stronger association with small artery disease. Neurol. Sci. 26, 310–318. doi: 10.1007/s10072-005-0505-7
Peters, J. L., Sutton, A. J., Jones, D. R., Abrams, K. R., and Rushton, L. (2006). Comparison of two methods to detect publication bias in meta-analysis. JAMA 295, 676–680. doi: 10.1001/jama.295.6.676
Phipps, M. S., and Cronin, C. A. (2020). Management of acute ischemic stroke. BMJ 368:l6983. doi: 10.1136/bmj.l6983
Ribo, M., Montaner, J., Molina, C. A., Arenillas, J. F., Santamarina, E., Quintana, M., et al. (2004). Admission fibrinolytic profile is associated with symptomatic hemorrhagic transformation in stroke patients treated with tissue plasminogen activator. Stroke 35, 2123–2127. doi: 10.1161/01.STR.0000137608.73660.4c
Sacco, R. L., Anand, K., Lee, H. S., Boden-Albala, B., Stabler, S., Allen, R., et al. (2004). Homocysteine and the risk of ischemic stroke in a triethnic cohort: the northern manhattan study. Stroke 35, 2263–2269. doi: 10.1161/01.STR.0000142374.33919.92
Schwammenthal, Y., and Tanne, D. (2004). Homocysteine, b-vitamin supplementation, and stroke prevention: from observational to interventional trials. Lancet Neurol. 3, 493–495. doi: 10.1016/S1474-4422(04)00826-9
Seo, H., Oh, H., Park, H., Park, M., Jang, Y., and Lee, M. (2010). Contribution of dietary intakes of antioxidants to homocysteine-induced low density lipoprotein (ldl) oxidation in atherosclerotic patients. Yonsei. Med. J. 51, 526–533. doi: 10.3349/ymj.2010.51.4.526
Shandal, V., and Luo, J. J. (2016). Clinical manifestations of isolated elevated homocysteine-induced peripheral neuropathy in adults. J. Clin. Neuromuscul. Dis. 17, 106–109. doi: 10.1097/CND.0000000000000108
Shi, Z., Guan, Y., Huo, Y. R., Liu, S., Zhang, M., Lu, H., et al. (2015). Elevated total homocysteine levels in acute ischemic stroke are associated with long-term mortality. Stroke 46, 2419–2425. doi: 10.1161/STROKEAHA.115.009136
Smith, M., Reddy, U., Robba, C., Sharma, D., and Citerio, G. (2019). Acute ischaemic stroke: challenges for the intensivist. Intensive Care. Med. 45, 1177–1189. doi: 10.1007/s00134-019-05705-y
Stang, A. (2010). Critical evaluation of the newcastle-ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25, 603–605. doi: 10.1007/s10654-010-9491-z
Tang, C. Z., Zhang, Y. L., Wang, W. S., Li, W. G., and Shi, J. P. (2016). Serum levels of high-sensitivity c-reactive protein at admission are more strongly associated with poststroke depression in acute ischemic stroke than homocysteine levels. Mol. Neurobiol. 53, 2152–2160. doi: 10.1007/s12035-015-9186-2
Tu, W. J., Zhao, S. J., Liu, T. G., Yang, D. G., and Chen, H. (2013). Combination of high-sensitivity c-reactive protein and homocysteine predicts the short-term outcomes of chinese patients with acute ischemic stroke. Neurol. Res. 35, 912–921. doi: 10.1179/1743132813Y.0000000228
Unal, E., Mungan, S., Bilen, S., Karadag, Y., Oztekin, N., Bakir, F., et al. (2013). The effects of lipoprotein(a) and homocysteine on prognosis and risk factors in acute ischemic stroke. Int. J. Neurosci. 123, 532–536. doi: 10.3109/00207454.2013.772609
Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., et al. (2020). Heart disease and stroke statistics-2020 update: a report from the american heart association. Circulation 141, e139–e596. doi: 10.1161/CIR.0000000000000757
Wang, M., Liang, X., Cheng, M., Yang, L., Liu, H., Wang, X., et al. (2019). Homocysteine enhances neural stem cell autophagy in in vivo and in vitro model of ischemic stroke. Cell Death Dis. 10:561. doi: 10.1038/s41419-019-1798-4
Wang, W., Gao, C., Yu, C., Liu, S., Hou, D., Wang, Y., et al. (2017). No association between elevated total homocysteine levels and functional outcome in elderly patients with acute cerebral infarction. Front. Aging. Neurosci. 9:70. doi: 10.3389/fnagi.2017.00070
Yao, E. S., Tang, Y., Xie, M. J., Wang, M. H., Wang, H., and Luo, X. (2016). Elevated homocysteine level related to poor outcome after thrombolysis in acute ischemic stroke. Med. Sci. Monit. 22, 3268–3273. doi: 10.12659/MSM.900010
Yoldas, T., Gonen, M., Godekmerdan, A., Ilhan, F., and Bayram, E. (2007). The serum high-sensitive c reactive protein and homocysteine levels to evaluate the prognosis of acute ischemic stroke. Mediators Inflamm. 2007:15929. doi: 10.1155/2007/15929
Zhong, C., Xu, T., Xu, T., Peng, Y., Wang, A., Wang, J., et al. (2017). Plasma homocysteine and prognosis of acute ischemic stroke: a gender-specific analysis from catis randomized clinical trial. Mol. Neurobiol. 54, 2022–2030. doi: 10.1007/s12035-016-9799-0
Zhou, Z., Liang, Y., Qu, H., Zhao, M., Guo, F., Zhao, C., et al. (2018). Plasma homocysteine concentrations and risk of intracerebral hemorrhage: a systematic review and meta-analysis. Sci. Rep. 8:2568. doi: 10.1038/s41598-018-21019-3
Keywords: homocysteine, acute ischaemic stroke, outcome, meta-analysis, systematic review
Citation: Huang S, Cai J and Tian Y (2021) The Prognostic Value of Homocysteine in Acute Ischemic Stroke Patients: A Systematic Review and Meta-Analysis. Front. Syst. Neurosci. 14:600582. doi: 10.3389/fnsys.2020.600582
Received: 30 August 2020; Accepted: 21 December 2020;
Published: 12 February 2021.
Edited by:
Paola Bonsi, Santa Lucia Foundation (IRCCS), ItalyReviewed by:
Cinzia Costa, University of Perugia, ItalyCopyright © 2021 Huang, Cai and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuejun Tian, dGlhbnl1ZWp1bmx6dUAxNjMuY29t; dGlhbnlqMTRAbHp1LmVkdS5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.