- Department of Urology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
Background and objective: The treatment of impacted upper ureteral stones remains a significant challenge for urologists. Standard treatment protocols often favor Mini-Percutaneous Nephrolithotripsy (Mini-PCNL). It has been supposed to be associated with a higher stone clearance rate and a lower incidence of ureteral stricture compared to Flexible Ureteroscopy (FURS). Recently, FURS with flexible and navigable suction ureteral access sheath (FANS) has emerged as a promising alternative. The aim of this study was to compare the efficacy and safety of the FURS with FANS and Mini-PCNL for treating the impacted upper ureteral stones.
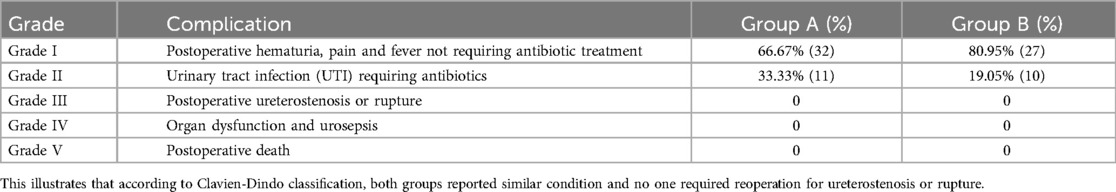
Method: A retrospective study of 80 patients treated with FURS with FANS (Group A, n = 43) or Mini-PCNL (Group B, n = 37) was conducted in our center (from June 2023 to August 2024). Primary outcomes included stone-free rate (SFR), hemoglobin drop, hospital stay, and complications (Clavien-Dindo classification) in 3 months.
Results: Both groups achieved comparable SFR (90.7% vs. 83.78%, P = 0.351). Group A had significantly lower hemoglobin drop (3.65 ± 8.39 vs. 7.89 ± 9.39 g/L, P = 0.036) and shorter hospital stays (1.79 ± 1.08 vs. 3.81 ± 1.37 days, P < 0.001). Complication rates were similar, but Group A had a higher rate of second-stage operation (18.6% vs. 8.1%, P = 0.174) and neither group required reoperation for ureteral stricture or rupture at 3 months post-surgery.
Conclusion: FURS with FANS is a safe and effective alternative to Mini-PCNL for impacted upper ureteral stones larger than 10 mm, offering shorter recovery times and lower bleeding. However, its higher second-stage operation rate necessitates further investigation.
1 Introduction
The optimal surgical management for impacted upper ureteral stones continues to represent a therapeutic dilemma in contemporary endourological practice. Currently, there is no universally accepted definition of impacted upper ureteral stones. Generally, they are defined as stones that cause hydronephrosis, remain stationary for more than 4–8 weeks, and cannot be bypassed with contrast medium or a guidewire at the initial attempt (1, 2). Chronic irritation of the ureteral wall by impacted stones induces inflammatory cell proliferation and polyp formation. This pathological process results in ureteral distortion, subsequently increasing the risk of surgical complications including residual stones, ureteral perforation, and postoperative iatrogenic ureteral stricture. These factors collectively contribute to enhanced surgical complexity and associated risks (3).
Mini-Percutaneous Nephrolithotripsy (Mini-PCNL) and Flexible Ureteroscopy (FURS) are currently the most common treatment options for upper ureteral stones, both demonstrating excellent stone clearance and low recurrence rates (4, 5). FURS offers advantages of minimal invasiveness through natural passages and shorter hospital stays. However, in cases of impacted stones, patients face increased risks of surgical failure, ureteral rupture, and urosepsis. More seriously, ureteral stricture is a common complication after FURS, particularly in cases of impacted stones, with studies reporting up to a 24% chance of postoperative ureteral stricture (6). Mini-PCNL is easier to achieve a high stone free rate (SFR), but it is associated with higher bleeding risks and longer recovery times (7).
The ureteral sheath is a crucial instrument in FURS which provides a smooth tube in order to reduce friction and damage during the insertion and withdrawal of the ureteroscope. Pushing the ureteral stone back to the kidney for lithotripsy can help minimize ureteral damage and avoid postoperative ureteral stricture. However, it is difficult to clear all the stone fragment by FURS with conventional sheath especially in cases of impacted stones (8).
In recent years, the development of the flexible and navigable suction ureteral access sheath (FANS) has provided an effective solution to this problem. Compared to conventional sheaths, FANS demonstrates enhanced surgical efficacy through its flexible distal tip. It enables smoother navigation into steep infundibulum-pelvic angles (IPA) and facilitates effective stone fragment aspiration, although its effectiveness remains limited in certain lower calyces with steep IPA. It also simplifies and clarifies the assessment of the renal pelvis, ureter, and residual stone fragments after lithotripsy (9). The superiority of FURS with FANS surgery in the treatment of urinary stones has been consistently reported in the literature. Compared with the traditional sheath, FURS with FANS had a higher SFR and a lower risk of complications (10–14).
However, the comparative efficacy of Mini-PCNL and FURS with FANS in the treatment of impacted upper ureteral stones has not been adequately explored. In light of this, we compared retrospectively safety and efficiency of FURS with FANS and Mini-PCNL in treating impacted upper ureteral stones.
2 Patient and method
2.1 Inclusion criteria
This retrospective study included 80 patients with impacted upper ureteral stones diagnosed in the Urology Department of the First Affiliated Hospital of Chongqing Medical University between June 2023 and August 2024. All patients underwent treatment with either Mini-PCNL or FURS with FANS.
1. Patients aged ≥18 years with stones measuring 1.0–2.0 cm in maximum diameter.
2. Stones located below ureteropelvic junction (UPJ) and above the lower border of the fourth lumbar vertebra.
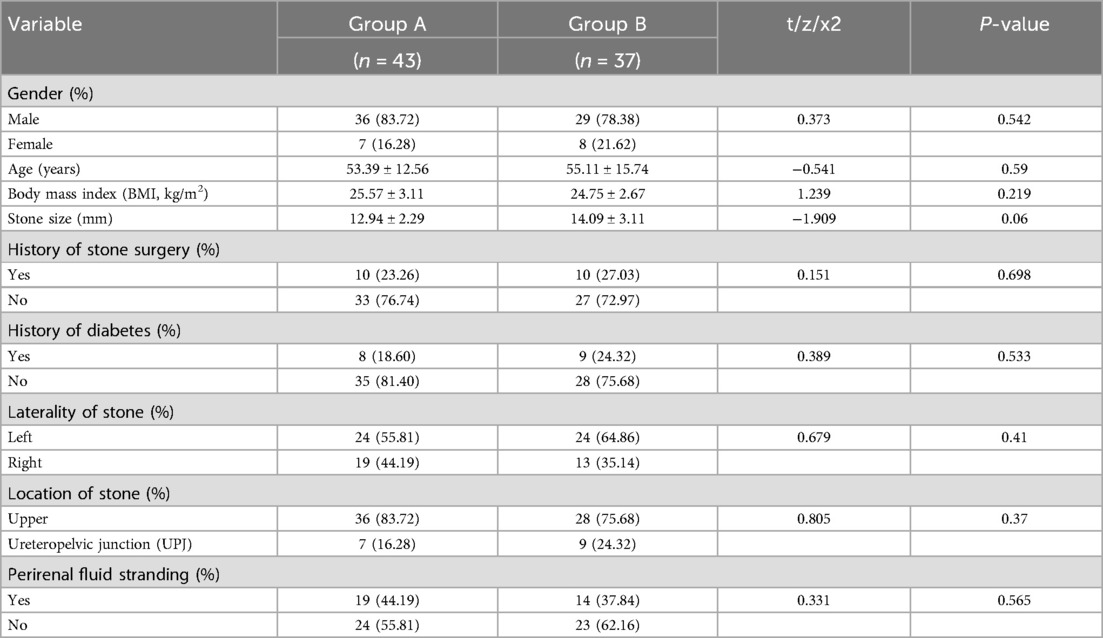
3. The diagnosis of impacted upper ureteral stones was confirmed intraoperatively (Figure 1).
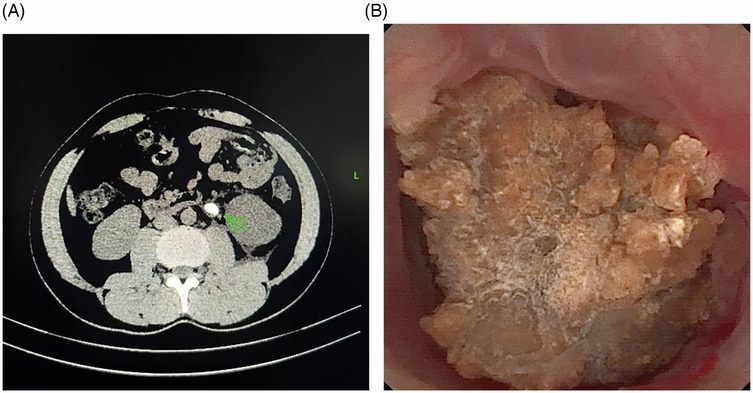
Figure 1. The impacted stone. (A) The stone impacted in the left ureter, ureteral wall thickening at the site of impaction and tissue edema surrounding the affected ureter. (B) The stone was observed to be tightly adherent to the ureteral wall in surgery. The mucosa at the site of impaction exhibited significant hyperemia and edema, with polyp formation noted.
2.2 Exclusion criteria
1. Stones located in the middle or lower segments of the ureter.
2. Patients with combined kidney stones or contralateral urinary stones.
3. Uncontrolled infection, other systemic diseases that cannot tolerate surgery, and abnormal urinary tract anatomy.
2.3 Study protocol
Patients were divided into two groups based on the surgical method.
Group A: included 43 patients treated with FURS with FANS.
Group B: included 37 patients treated with Mini-PCNL.
All patients underwent complete history taking and physical examinations. Preoperative laboratory investigations included urine analysis, urine culture and routine blood tests. Urinary Tract CT and Abdominal Ultrasound were used as a preoperative standard to evaluate the size of the stone. The primary outcome was SFR (defined as zero fragment or a single fragment ≤2 mm) assessed using Kidney, Ureter, and Bladder x-ray (KUB) immediately after operation, followed by the ultrasound examination or CT scan 3 months postoperatively. The hemoglobin drop and postoperative hospital stay were recorded as indicators to evaluate the short-term surgical outcomes. All patients were followed for 3 months and complications were classified by the Clavien-Dindo classification.
2.4 Operative technique
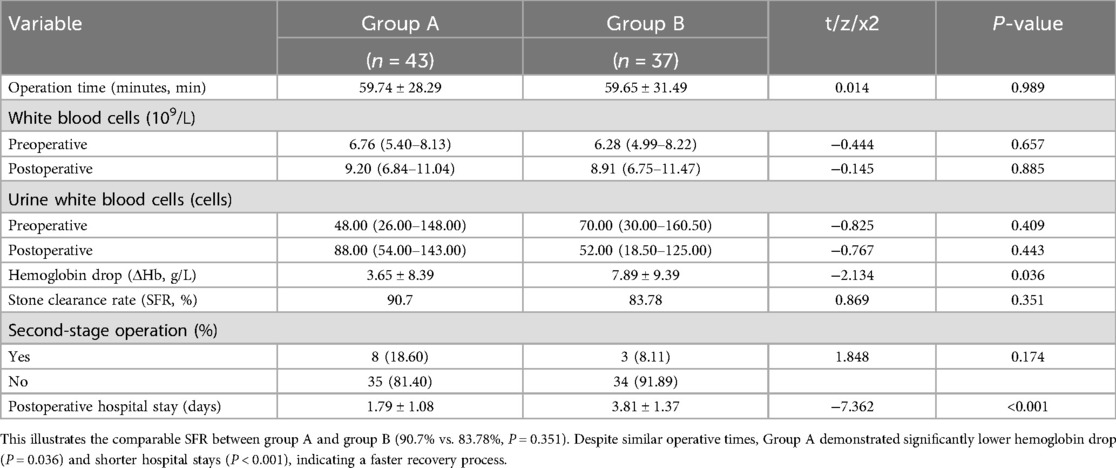
Group A (FURS with FANS): After general anesthesia, the patient was placed in the lithotomy position. A rigid ureteroscope was advanced into the ureter on the operative side to place a guidewire, and then a 11–13F FANS (Well Lead Medical, Guangzhou, China) was placed along the guidewire. A disposable flexible ureteroscope (Scivita Medical, Suzhou, China) was used to crush the stone with a holmium laser, attempting to return the stone to the kidney before or during lithotripsy to allow for further fragmentation and the sheath was used to suck the fragment under negative pressure. After the operation, a 5/6 F double-J stent (BOSTON TECH, USA) was inserted in the ureter on the operative side (Figure 2).

Figure 2. Treatment of impacted stones using FURS with FANS. (A) Pushing the stone back into the renal pelvis for lithotripsy due to protect ureter. (B) After pushing the stone back into the renal pelvis, ureteroscopic examination of the previous stone impaction site demonstrated no extensive iatrogenic ureteral trauma or structural disruption. (C) Utilizing FANS for fragment aspiration to prevent secondary ureteral impaction. (D) Placing stent under guidewire.
Group B (Mini-PCNL): Under general anesthesia, the patient was positioned in the prone position and the puncture needle was advanced into the pelvi-calyceal system under the guidance of ultrasound. A guidewire was placed through the inner stylet of the needle. Then, a 16/18F sheath (Well Lead Medical, Guangzhou, China) was placed along the guidewire at the puncture site to establish surgical access. After passing the access sheath with a nephroureteroscope, holmium laser was used for lithotripsy. Stone fragments were evacuated via a continuous irrigation system consisting of the 16/18F sheath and irrigation pump. After lithotripsy, a 5/6F double J stent (BOSTON TECH, USA) was inserted in the ureter on the operative side, and a percutaneous nephrostomy tube was placed.
2.5 Statistical analysis
The Statistical Package for the Social Sciences (SPSS, IBM, Chicago, IL, USA) was used for data analysis. p-value < 0.05 was considered statistically significant. The Student's t-test and the Mann–Whitney U test were used to assess the statistical significance of differences in parametric variables between the two study groups. Fisher's exact test and Pearson's Chi-squared Test were used to evaluate the association between two qualitative variables. Descriptive statistics were presented as mean ± standard deviation (SD) or numbers and percentages.
3 Ethical approval
This study was approved by the Ethics Committee of Chongqing Medical University. All patients' information was kept strictly confidential.
4 Result
The patient and stone characteristics are summarized in Table 1. The mean age of patients was 53.39 ± 12.56 years in Group A and 55.11 ± 15.74 years in Group B. In Group A, there were 36 male patients (83.72%) and 7 female patients (16.28%), while Group B included 29 male patients (78.38%) and 8 female patients (21.62%). The Body Mass Index (BMI) was 25.57 ± 3.11 kg/m² in Group A and 24.75 ± 2.67 kg/m² in Group B. There were no significant differences in sex, age and BMI between the two groups. The mean stone size was 12.94 ± 2.29 mm in Group A and 14.09 ± 3.11 mm in Group B. Similarly, no significant difference between two groups. Preoperative and postoperative data are presented in Table 2. Group A had comparable SFR with Group B (90.7% vs. 83.78%, P = 0.351). Group B had worse postoperative decreases in hemoglobin than Group A (7.89 ± 9.39 vs. 3.65 ± 8.39 g/L, P = 0.036) and the difference was statistically significant. Group A had a shorter postoperative hospital stay compared to Group B (1.79 ± 1.08 vs. 3.81 ± 1.37 days, P < 0.001). There was a higher rate of second-stage operation in Group A due to ureterostenosis and main reason for Group B was infection (18.60% vs. 8.11%, P = 0.174). In addition, there was no difference between the two groups in operative time, preoperative and postoperative inflammatory indicators. According to the Clavien-Dindo classification, 59 individuals were classified as grade Ⅰ (32 in Group A and 27 in Group B), while 21 cases at grade Ⅱ (11 in Group A and 10 in Group B). Neither group reported cases of postoperative ureteral stricture or rupture (Table 3).
5 Discussion
In this study, we retrospectively evaluated the safety and efficacy of FURS with FANS and Mini-PCNL in the management of impacted upper ureteral stones.
The present study demonstrated that FURS with FANS was an effective approach for the treatment of impacted upper ureteral stones. Mohey A et al. conducted a prospective study to evaluate the efficacy of conventional sheaths with FURS and PCNL for impacted ureteral stones (15). Their findings suggested that PCNL had superior SFR compared to FURS. However, our study found that FURS with FANS could achieve an equally effective SFR compared to Mini-PCNL. The impacted stone usually causes edema, erosion, and polyp growth of the ureteral mucosa, which will interfere with stone removal. To minimize this risk, stones were pushed back into the kidney before lithotripsy. However, due to the same pathological changes, the discharge of stone fragments postoperatively remains challenging. The flexible tip design of FANS enables access to renal calyces that conventional sheaths cannot reach, facilitating efficient stone fragment aspiration. This feature improves SFR and prevents fragment re-impaction in narrow anatomical segments (16, 17).
Similarly, the effectiveness of FANS is still limited by ureteral conditions. In cases of ureterostenosis or severe infection, a second-stage operation will be required, increasing hospitalization time and the risk of infection or thrombosis (18). In this study, eight cases in Group A underwent second-stage operation for stenosis, compared to only three cases in Group B, which were attributed to infection. This study found no difference in operative time between FURS with FANS and Mini-PCNL (59.74 ± 28.29 vs. 59.65 ± 31.49, P = 0.989). Previous studies on differences in operative time between FURS and PCNL had been inconclusive. On the one hand, Mini-PCNL may require a longer time due to the establishment of the PCNL tract. However, on the other hand, it is more effective than FURS in terms of stone fragmentation efficiency (19, 20). Zhu et al. reported that the operative time of PCNL was shorter than FURS with FANS for the treatment of renal or ureteral stones ≤30 mm (10). This difference may be attributed to the repeated insertion and withdrawal of the scope through FANS during stone suction (21).
Postoperative complications most commonly include bleeding and infection. Mini-PCNL, due to its invasive nature, carries a higher risk of intraoperative bleeding and blood transfusion compared to FURS, which is one of the reasons for selecting FURS (22). In this study, the extent of hemoglobin drop was employed as an indicator to evaluate intraoperative bleeding. Notably, there was significant difference in hemoglobin drop between the two groups. The Mini-PCNL group showed a higher mean value than the FURS group (7.89 ± 9.39 vs. 3.65 ± 8.39 g/L, P = 0.036), suggesting that FURS may offer a superior safety profile for patients with anemia or coagulation disorders. According to the Clavien-Dindo score, most complications in both groups were classified as Grade I or II. Furthermore, At 3 months follow-up, neither group required reoperation for ureterostenosis or rupture. It was suggested that pushing ureteral stones back into the kidney for lithotripsy under FURS with FANS and aspirating the fragments using negative pressure can avoid postoperative ureteral stricture while achieving a stone clearance rate comparable to Mini-PCNL.
A significant discrepancy was observed in the postoperative hospitalization duration between the two groups. Group A demonstrated shorter hospital stays compared to Group B (1.79 ± 1.08 vs. 3.81 ± 1.37 days, P < 0.001). Cheng et al. reported that FURS caused minimal postoperative pain or bleeding, had less impact on hemoglobin levels and coagulation, and offered advantages such as reduced bleeding, shorter hospital stays, and faster gastrointestinal recovery (23). Considering the invasive nature of Mini-PCNL and the potential of patients having a long-term indwelling nephrostomy tube after surgery, it can be argued that at the same SFR, FURS with FANS enhanced postoperative comfort, reduced nursing workload and delivered superior short-term surgical outcomes.
6 Conclusion
FURS with FANS for the management of impacted upper ureteral stones is a safe and feasible procedure, offering a high SFR, minimal bleeding, and shorter hospital stays, reducing the risk of postoperative ureteral stricture. However, compared to Mini-PCNL, it has a higher rate of second-stage operation due to ureteral conditions.
7 Limitation
Further studies are required to validate the findings comparing FURS with FANS and Mini-PCNL. The long-term efficacy and safety of these two surgical approaches require further investigation to better inform clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Association of Chongqing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
HT: Methodology, Software, Writing – original draft, Writing – review & editing. YC: Data curation, Validation, Writing – original draft, Writing – review & editing. ZW: Investigation, Writing – review & editing. FY: Supervision, Writing – review & editing. JL: Methodology, Writing – review & editing. JL: Supervision, Writing – original draft, Writing – review & editing, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Chongqing Young and Middle-aged High-end Medical Talents Project (2022) and Chongqing Health Appropriate Technology Promotion Project (2024jstg033).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chandhoke R, Bamberger JN, Gallante B, Atallah W, Gupta M. Peri-calculus ureteral thickness on computed tomography predicts stone impaction at time of surgery: a prospective study. J Endourol. (2020) 34(1):107–11. doi: 10.1089/end.2019.0449
2. Mugiya S, Ito T, Maruyama S, Hadano S, Nagae H. Endoscopic features of impacted ureteral stones. J Urol. (2004) 171(1):89–91. doi: 10.1097/01.ju.0000100960.08768.81
3. Haitao L, Ben C, Xin C, Long Y, Xu Z, Junnan X, et al. Comparison of Moses laser and Raykeen laser in patients with impacted upper ureteral stone undergoing flexible ureteroscopic holmium laser lithotripsy. BMC Urol. (2024) 24(1):190. doi: 10.1186/s12894-024-01576-8
4. Albala DM, Assimos DG, Clayman RV, Denstedt JD, Grasso M, Gutierrez-Aceves J. Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J Urol. (2001) 166(6):2072–80. doi: 10.1016/s0022-5347(05)65508-5
5. Kim CH, Chung DY, Rha KH, Lee JY, Lee SH. Effectiveness of percutaneous nephrolithotomy, retrograde intrarenal surgery, and extracorporeal shock wave lithotripsy for treatment of renal stones: a systematic review and meta-analysis. Medicina (Kaunas). (2020) 57(1):26. doi: 10.3390/medicina57010026
6. Darwish AE, Gadelmoula MM, Abdelkawi IF, Abdellatif AM, Abdel-Moneim AM, Hammouda HM. Ureteral stricture after ureteroscopy for stones: a prospective study for the incidence and risk factors. Urol Ann. (2019) 11(3):276–81. doi: 10.4103/UA.UA_110_18
7. Wang F, Hong Y, Yang Z, Ye L. Comparison of retrograde intrarenal surgery and standard percutaneous nephrolithotomy for management of stones at ureteropelvic junction with high-grade hydronephrosis. Sci Rep. (2021) 11(1):14050. doi: 10.1038/s41598-021-93551-8
8. Breda A, Territo A, López-Martínez JM. Benefits and risks of ureteral access sheaths for retrograde renal access. Curr Opin Urol. (2016) 26(1):70–5. doi: 10.1097/MOU.0000000000000233
9. Chen Y, Zheng L, Lin L, Li C, Gao L, Ke L, et al. A novel flexible vacuum-assisted ureteric access sheath in retrograde intrarenal surgery. BJU Int. (2022) 130(5):586–8. doi: 10.1111/bju.15873
10. Zhu W, Liu S, Cao J, Wang H, Liang H, Jiang K, et al. Tip bendable suction ureteral access sheath versus traditional sheath in retrograde intrarenal stone surgery: an international multicentre, randomized, parallel group, superiority study. EClinicalMedicine. (2024) 74:102724. doi: 10.1016/j.eclinm.2024.102724
11. Zhu Z, Cui Y, Zeng F, Li Y, Chen Z, Hequn C. Comparison of suctioning and traditional ureteral access sheath during flexible ureteroscopy in the treatment of renal stones. World J Urol. (2019) 37(5):921–9. doi: 10.1007/s00345-018-2455-8
12. Xiao J, Chen H, Liu T. Retrograde intrarenal surgery combined with flexible terminal suction ureteral access sheath in treating bilateral urinary system stones. Asian J Surg. (2024) 47(6):2921–2. doi: 10.1016/j.asjsur.2024.02.038
13. Geavlete P, Mulţescu R, Geavlete B. Re: application of suctioning ureteral access sheath during flexible ureteroscopy for renal stones decreases the risk of postoperative systemic inflammatory response syndrome. Eur Urol. (2024) 85(1):94. doi: 10.1016/j.eururo.2023.08.020
14. Zhang Z, Xie T, Li F, Wang X, Liu F, Jiang B, et al. Comparison of traditional and novel tip-flexible suctioning ureteral access sheath combined with flexible ureteroscope to treat unilateral renal calculi. World J Urol. (2023) 41(12):3619–27. doi: 10.1007/s00345-023-04648-w
15. Mohey A, Abdelfattah AA, Mohammed AE, Marzouk A, El-Dakhakhny AS. Comparative study between antegrade flexible ureteroscopy and reterograde intrarenal surgery in the management of impacted upper ureteric stones 1.5 cm or larger. World J Urol. (2023) 41(12):3731–6. doi: 10.1007/s00345-023-04672-w
16. Wang DJ, Liang P, Yang TX, Liu YQ, Tang QL, Zhou XZ, et al. RIRS With FV-UAS vs. MPCNL for 2–3-cm upper urinary tract stones: a prospective study. Urolithiasis. (2024) 52(1):31. doi: 10.1007/s00240-024-01539-6
17. Gauhar V, Traxer O, Castellani D, Sietz C, Chew BH, Fong KY, et al. Could use of a flexible and navigable suction ureteral access sheath be a potential game-changer in retrograde intrarenal surgery? Outcomes at 30 days from a large, prospective, multicenter, real-world study by the European association of urology urolithiasis section. Eur Urol. (2024) 10(6):975–82. doi: 10.1016/j.euf.2024.05.010
18. Xu X, Liao S, Wei G, Xu F, Jiang Y, Lu Z, et al. A comparative study of retrograde intrarenal surgery versus percutaneous nephrolithotomy for the management of staghorn renal calculi. Ann Ital Chir. (2024) 95(4):568–74. doi: 10.62713/aic.3474
19. Liu Y, Zhang H, Wen Z, Jiang Y, Huang J, Wang C, et al. Efficacy and safety of minimally invasive percutaneous nephrolithotomy versus retrograde intrarenal surgery in the treatment of upper urinary tract stones (>1 cm): a systematic review and meta-analysis of 18 randomized controlled trials. BMC Urol. (2023) 23(1):171. doi: 10.1186/s12894-023-01341-3
20. Erkoc M, Bozkurt M. Comparison of Mini-percutaneous nephrolithotomy and retrograde intrarenal surgery for renal pelvic stones of 2–3 cm. J Laparoendosc Adv Surg Tech. (2021) 31(6):605–9. doi: 10.1089/lap.2020.0860
21. Constantinou BT, Benedicto BC, Porto BC, Belkovsky M, Passerotti CC, Artifon EL, et al. PCNL vs. two staged RIRS for kidney stones greater than 20 mm: systematic review, meta-analysis, and trial sequential analysis. Minerva Urol Nephrol. (2024) 76(1):31–41. doi: 10.23736/S2724-6051.23.05577-5
22. Li Z, Lai C, Shah AK, Xie W, Liu C, Huang L, et al. Comparative analysis of retrograde intrarenal surgery and modified ultra-mini percutaneous nephrolithotomy in management of lower pole renal stones (1.5–3.5 cm). BMC Urol. (2020) 20(1):27. doi: 10.1186/s12894-020-00586-6
Keywords: flexible and navigable suction ureteral access sheath, flexible ureteroscopy, mini-percutaneous nephrolithotripsy, impacted stone, stone-free rate
Citation: Tang H, Che Y, Wu Z, Yuan F, Liu J and Li J (2025) Comparison of flexible ureteroscopy with flexible and navigable suction ureteral access sheath and mini-percutaneous nephrolithotripsy for the treatment of impacted upper ureteral stones: a retrospective study. Front. Surg. 12:1562428. doi: 10.3389/fsurg.2025.1562428
Received: 17 January 2025; Accepted: 17 March 2025;
Published: 27 March 2025.
Edited by:
Bo Xiao, Tsinghua University, ChinaCopyright: © 2025 Tang, Che, Wu, Yuan, Liu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie Li, bGlqaWV1cm9AMTYzLmNvbQ==
†These authors have contributed equally to this work
 Haiyang Tang
Haiyang Tang Yulong Che†
Yulong Che† Fangchao Yuan
Fangchao Yuan Jiayu Liu
Jiayu Liu Jie Li
Jie Li