- 1Department of Orthopaedic Surgery, Guizhou Provincial People’s Hospital, Guiyang, China
- 2Department of Zunyi Medical University, Zunyi, China
Objective: To observe the clinical efficacy of prophylactic use of tibial extension stem in primary Total Knee Arthroplasty (TKA) in patients with severe knee varus deformity and tibial plateau bone defect, and its effect on reducing the rate of tibial prosthesis aseptic loosening.
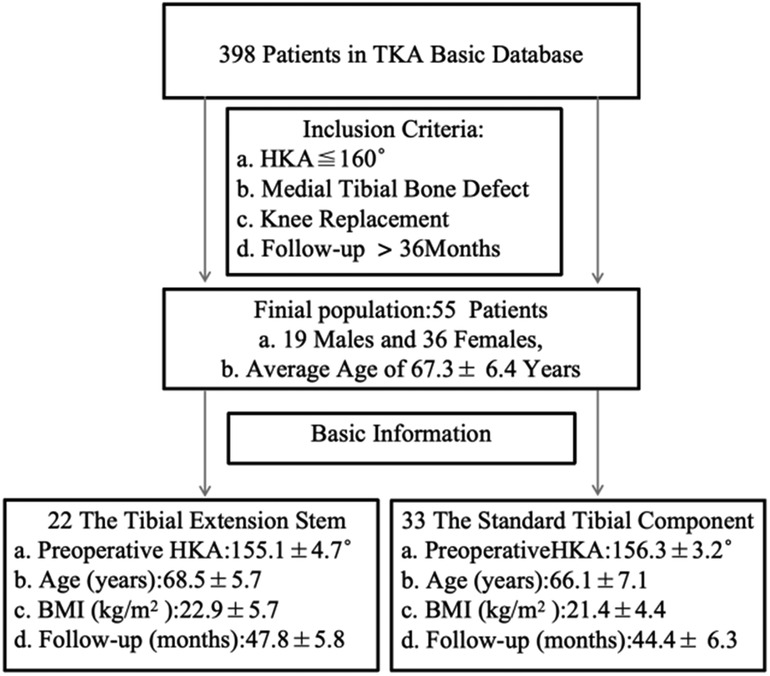
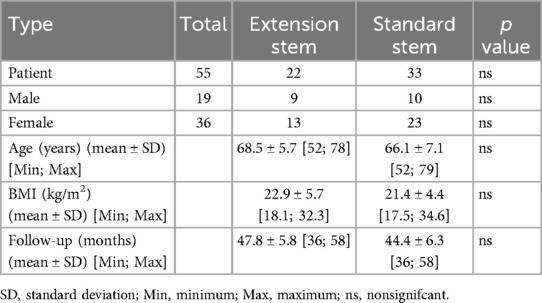
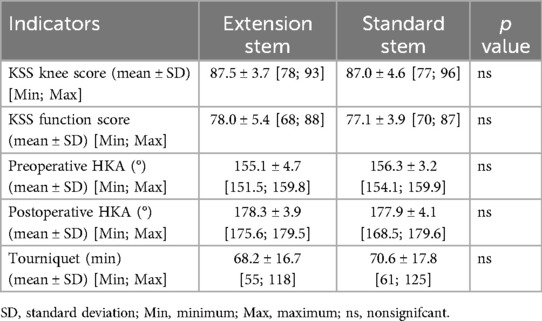
Methods: A total of 398 patients who underwent primary TKA in our hospital from August 2019 to June 2021 were collected. According to the strict inclusion/exclusion criteria, 55 patients with knee varus deformity (Hip-knee-ankle Angle, HKA ≤ 160°) and tibial bone defect were finally included. The tibial extension stem was used in 22 patients and standard tibial prosthesis was used in 33 patients. The general data, intraoperative parameters, preoperative and postoperative imaging parameters and knee function scores (KSS) were analyzed. The incidence of tibial prosthesis aseptic loosening, KSS score, radiological evaluation of the prosthesis and bone cement screws, and postoperative general complications were dynamically followed up and evaluated.
Results: All 55 patients completed long-term follow-up, with an average follow-up time of 46.1 ± 4.2 months. There was no significant difference in HKA Angle between the two groups before and after operation (p > 0.05). At least 36 months follow-up, The final Society Radiographic Evaluation System (KSRES) scores were significantly different in the range of 4–10 mm (p < 0.05), but no screw loosening, sinking, osteolysis, bone cement fracture and serious postoperative complications occurred in all patients. There was no significant difference in KSS scores between the two groups during the follow-up period (p > 0.05). At the end of follow-up, there was no aseptic loosening of tibial prosthesis and serious postoperative complications in both groups.
Conclusions: For patients with severe knee varus deformity and tibial plateau bone defect, the use of tibial extension stem in primary TKA may have a protective effect on the survival rate of prosthesis.
Introduction
Knee Osteoarthritis (OA), a common degenerative joint disease, is also one of the main causes of disability and chronic pain in patient's (1, 2). TKA is currently an effective and highly successful surgical method for treating primary Knee OA (3). In the past few decades, the number of total knee joint revisions after initial knee arthroplasty has rapidly increased worldwide. Although the clinical application of TKA has become quite mature in recent years, with the increase in the number of knee joint replacements, the incidence of postoperative complications has also increased, with the most common being aseptic loosening and infection. Research has confirmed that patients with severe inversion of the knee joint have a higher rate of loosening and revision after TKA surgery than do those with milder deformities (4–8). Previous studies have shown that improvements in tibial implants may effectively address this issue. The tibial extension stem are often used in complex initial and revision TKA, with the benefit of reducing tibial detachment and lateral shear stress (9, 10). In addition, the advantages of using a short the tibial extension stem include effectively dispersing stress at the prosthesis-bone interface, maintaining the stability of the prosthesis, reducing the probability of prosthesis loosening (11, 12), reducing micromovement, strengthening fixation, and potentially reducing the risk of pain (9, 13, 14).
Recently, an increasing number of researchers have been interested in the prophylactic use of the tibial extension stem in TKA surgery, as prophylactic use of the tibial extension stem has become a common surgical technique. This technology can effectively solve some problems that arise after TKA surgery and achieve better surgical results. However, there are currently few reports on whether prophylactic use of the tibial extension stem in TKA is more advantageous for reducing postoperative revision rates in patients with severe knee joint varus deformity combined with tibial plateau bone defects. Therefore, the purpose of this study was to observe whether prophylactic use of the tibial extension stem can reduce the incidence of early aseptic loosening of prostheses in patients with severe knee varus deformity combined with tibial plateau bone defects during initial TKA.
Materials and methods
The data for this retrospective study were based on a prospective collection of 398 TKA surgeries performed by the same team of joint surgeons at our institution from August 2019 to June 2021, with all surgical options selected for total knee arthroplasty. The inclusion criteria for this study included the following: (1) Knee joint HKA ≤ 160°; (2) Combined with tibial plateau bone defect (tibial plateau defect depth ≤10 mm, unilateral tibial plateau defect area <50%); (3) Perform primary TKA; (4) The follow-up time was at least 36 months. After screening, A total of 55 patients were enrolled, including 19 males and 36 females. All the patients were divided into two cohorts for observation, including 22 cases with 10mm × 40 mm the tibial extension stem and 33 cases with standard tibial prosthesis (Figure 1). For patients with tibial plateau bone defect depth <5 mm, autologous bone graft was used to fill the defect, and for patients with defect depth 5–10 mm, bone cement screw was used to support the defect.
The artificial joint implants used in both queues were sourced from Chunli Zhengda Medical Equipment Co., Ltd. (Beijing, China) (Figure 2). The average follow-up time after surgery was 46.1 ± 4.2 months. General information such as sex, age, and BMI was collected from all patients before surgery, and imaging data such as full-length films of both lower limbs and anterior posterior (AP) and lateral x-ray translucency lines were regularly obtained after surgery. Based on these findings, the hip knee ankle angle (HKA) and radiolucency line (RLL) were measured. Additionally, the American Knee Society Scale (KSS) is used for functional assessment.
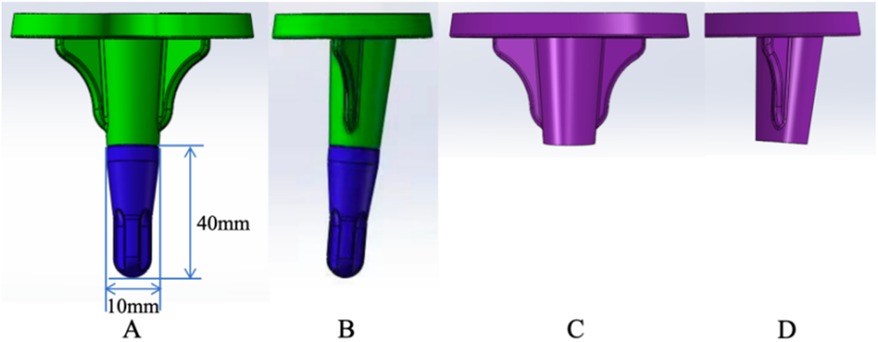
Figure 2. The tibial extension stem and standard tibial prosthesis implant; (A,B) the tibial extension stem tibial prosthesis anteroposterior and lateral position, (C,D) standard tibial prosthesis anteroposterior and lateral position.
Operative technique
A medial parapatellar approach was used in both groups, and the procedure was performed in the supine position with a balloon tourniquet applied at the root of the thigh on the affected side and pressure set at 280mmHg. After removing the distal femur and proximal tibia, the soft tissue around the knee joint was released to achieve the balance of tension between the medial and lateral soft tissue. Then the femoral prosthesis, tibial prosthesis and shim model were implanted (15). The lower limb alignment was normal, and the range of motion was from extension (0°) to flexion (120°). Autogenous bone or cement screws were implanted in the bone defect of tibial plateau, and the femoral and tibial prostheses and polyethylene pads were inserted to reduce the joint. After the bone cement was solidified, the stability of flexion and extension of the joint was good, and the position of the artificial joint prosthesis was confirmed by intraoperative x-ray film, and the operation was finished.
Follow-up and evaluation of tibial loosening
Radiological data were obtained before surgery and 36 months after surgery, including full-length radiographs of both lower limbs, anterior-posterior (AP) and lateral radiographs of the knee joint, and radiolucosal lines and HKA angles were measured (Figure 3). Follow-up and evaluation were performed by two specialists who were not involved in this operation to evaluate the results by radiographic measurements and the KSS scores at 36 months after surgery (16).
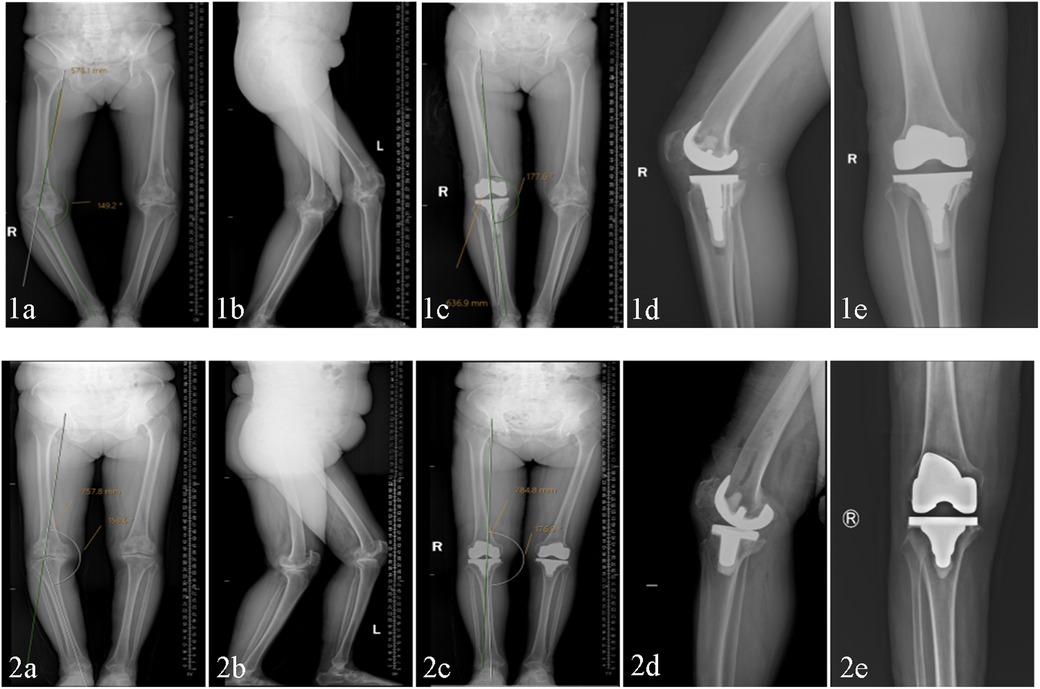
Figure 3. The tibial extension stem group (1) and standard tibial prosthesis group (2) were compared in terms of preoperative and postoperative DR and HKA angles; (a,b) preoperative full-length anteroposterior lateral (DR) and preoperative HKA angle of both lower limbs. (c) Postoperative 36-month HKA angle. (d,e) Postoperative 36-month knee joint AP and lateral positions.
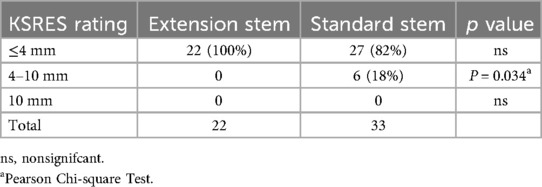
All patients had Anterior Posterior (AP) and lateral x-ray images of the knee joint taken during follow-up at least 36 months after surgery, and the preoperative and postoperative HKA angles were measured using our institution's image storage system (Figure 3). Radiographic transparency was also measured by two professional orthopedic physicians who did not participate in the surgery (Figure 4). According to Meneghini et al. (17) and Chalmers et al. (18), the KSRES scoring system for total knee arthroplasty in the United States is allocated based on the cumulative number of radiolucent lines on knee AP and lateral x-rays. The scoring of AP and lateral x-rays was determined by measuring the width of the radial translucency line in millimeters for each area of the AP and lateral x-rays. The sum of the widths of each area was the total score. The KSRES score was less than or equal to 4 millimeters, 4–10 mm, or greater than or equal to 10 mm. To evaluate whether there was aseptic loosening of the tibial prosthesis, the score was evaluated as follows: 4 points or lower, indicating no progression or possible insignificance; a score of 4–10 indicated that looseness did not occur but may have had a tendency to occur. Regular reexamination and close monitoring of progress was conducted; a score of 10 or higher indicated possible or imminent loosening regardless of symptoms. A preliminary diagnosis of implant loosening was made by combining clinical and imaging techniques. Patients suspected of implant loosening underwent blood tests (C-reactive protein concentration, white blood cell count, and erythrocyte sedimentation rate), CT scans, and other techniques to confirm the occurrence of aseptic loosening.
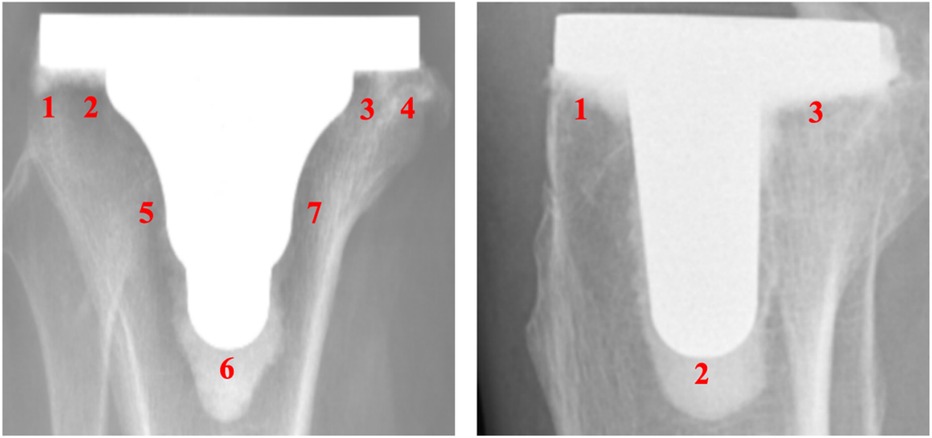
Figure 4. Knee joint AP and lateral x-ray images, divided according to the American knee association TKA postoperative x-ray evaluation system (KSRES score).
Statistical analysis
The measured parameters between the two groups were expressed as mean ± standard deviation (x ± s). The preoperative and postoperative HKA, KSS scores and implant loosening were analyzed by one-way ANOVA and t test, respectively. P < 0.05 was considered statistically significant, and all statistical analyses were performed using the Statistical Product and Service Solutions (SPSS) version 23.0 (SPSS Inc., Chicago, Illinois, USA).
Results
General information
There were no differences in age, sex, BMI, follow-up time, or surgical time between the tibial extension stem group and the standard tibial prosthesis group based on comparisons of the preoperative general information (Table 1).
Surgical outcomes
The preoperative HKA Angle of the tibial extension stem group was smaller than that of the standard tibial prosthesis group according to the evaluation of 2 orthopedic surgeons who were not involved in the operation (155.1° ± 4.7° vs. 156.3° ± 3.2°, P > 0.05). However, no statistically significant difference was found between the tibial extension stem group and the standard tibial prosthesis group in terms of postoperative HKA. (178.3° ± 3.9° vs. 177.9° ± 4.1°, P > 0.05) (Table 2).
Postoperative complications
The mean follow-up time was 46.1 ± 4.2 months. There were no serious postoperative complications of tibial prosthesis aseptic loosening, screw loosening, sinking, osteolysis, bone cement fracture and infection in the the tibial extension stem group and the standard tibial prosthesis group.
KSS and KSS functional scores
The KSS (87.5 ± 3.7 points vs. 87.0 ± 4.6 points, P > 0.05) and KSS (78.0 ± 5.4 points vs. 77.1 ± 3.9 points, P > 0.05) indicated that there was no significant difference between the short tibial extension rod group and the standard tibial prosthesis group (Table 2).
Radiological measurements
Radiological parameters were measured at least 36 months after surgery in all patients. There was no significant difference in the occurrence of aseptic loosening between the tibial extension stem group and standard tibial prosthesis group in AP and lateral positions (P > 0.05).There was no significant difference in KSRES score between the tibial extension stem group and the standard tibial prosthesis group in the range of ≤4 mm and ≥10 mm. However, in the standard tibial prosthesis group, there were 6 patients (18%) with KSRES score between 4 and 10 mm. Pearson's chi-square test showed that there was a significant difference between the two groups (p < 0.05). The results showed that the risk of aseptic loosening in the standard tibial prosthesis group was higher than that in the short tibial prosthesis group, and regular review and close attention should be paid to its progress (Table 3).
Discussion
In this clinical study, 55 patients with severe knee varus deformity combined with tibial bone defect were divided into two cohorts for observation. Through at least 36 months of follow-up, radiographic data showed that there were no serious postoperative complications of tibial prosthesis aseptic loosening, screw loosening, subsidence, osteolysis, bone cement fracture and infection in the tibial extension stem group and the standard tibial prosthesis group.All radiolucent line measurement (RLL) KSRES scores were less than 10 in both groups. No direct evidence of imminent or possible failure was found. Although there was no significant difference in the survival rate of prosthesis between the two groups in this study, the KSRES score in the 4–10 mm range was 6 cases (18%) in the standard tibial prosthesis group, and 0 case in the tibial extension stem group, there was a significant difference between the two groups (p < 0.05). The results indicate that these 6 patients may have a tendency and progression of loosening. The risk of aseptic loosening in the standard tibial component group is higher than that in the tibial extension stem group. The risk of implant stability reduction is higher, suggesting that the prophylactic use of the tibial extension stem in primary TKA may protect the survival rate of prosthesis in patients with severe knee varus deformity and tibial bone defect.
The inclusion of a the tibial extension stem at the lower end of the tibial prosthesis platform is a common practice aimed at enhancing the stability of the tibial plateau prosthesis and distributing the body's weight evenly. Previous studies have shown that prophylactic use of the tibial extension stem can reduce the risk of postoperative complications and improve the treatment outcome of patients. the tibial extension stem can improve the clinical efficacy of patients and improve the survival rate of prostheses by increasing the contact area of the tibial implant-bone interface, thereby improving the stability of tibial prosthesis and reducing a certain amount of tibial pressure. At the same time, Glenn et al. (14) and Hegde et al. (19) showed that prophylactic use of a short tibial extension resulted in a lower incidence of aseptic loosening in patients with preoperative genu varum deformity, because the short tibial extension could reduce compression stress by 136% and shear stress at the bone-cement interface by 92%. Moreover, a study conducted by Fournier (20) et al. demonstrated that the proactive adoption of the tibial extension stem during primary total knee arthroplasty may effectively mitigate the aforementioned issues. In this rigorously conducted study comprising 180 patients, the rate of tibial implant loosening was 3% in the cohort lacking the tibial extension stem, while the corresponding rate was 0% in the cohort equipped with such stem. It is widely acknowledged that obesity is linked to heightened postoperative complications and diminished prognosis scores subsequent to total knee arthroplasty (TKA). In a study conducted by Steere et al. with an average follow-up duration of 34 months, neither group experienced any instances of aseptic loosening failure, irrespective of the use of prophylactic the tibial extension stem (21). Furthermore, quantitative analysis revealed no significant difference in the percentage of RLL between the two groups. Research conducted by Abdel MP (22) et al. revealed that the use of abbreviated extension stem in TKA procedures for obese individuals can effectively diminish the occurrence of tibial loosening, as observed during a minimum two-year postoperative monitoring period.
The novelty of this study lies in the fact that it is the first comparison between patients with preoperative HKA ≤ 160° and combined tibial plateau bone defects in TKA surgery and whether prophylactic use of the tibial extension stem is used. Preventive use of the tibial extension stem can effectively repair tibial varus deformities in patients with tibial bone defects, restore good lower limb force lines, improve gait and pain symptoms, restore motor function, and improve quality of life. This brings good news to patients with primary knee osteoarthritis with severe genu varum deformity and tibial plateau bone defect, and has very important guiding significance for their clinical diagnosis and treatment. Moreover, during postoperative follow-up observation, if the KSRES score is found to be within the 4–10 mm range, patients should receive more regular follow-up and close monitoring of their progression. At the same time, patients should be educated regarding safety measures, such as reducing high-intensity activities and avoiding falls and collisions. However, there are still many shortcomings in this study, such as the small sample size, short follow-up period, and the possibility of some patients missing serious complications and experiencing aseptic loosening due to being lost to follow-up. It is necessary to include more patients and extend the follow-up time in future studies to further verify the long-term efficacy of these regimens. In summary, the preventive use of the tibial extension stem has been widely used in TKA surgery, but its effectiveness still needs further research. At present, the use of a the tibial extension stem may be an effective treatment for patients with severe knee varus deformity combined with tibial bone defects, but sufficient preoperative planning and risk assessment should be conducted before surgery to ensure its safety and effectiveness, and correct surgical decisions should be made. Personalized treatment should be conducted with an approach clinically based on the specific circumstances.
Conclusion
For patients with severe knee varus deformity and tibial plateau bone defect, the use of tibial extension stem in primary TKA may have a protective effect on the survival rate of prosthesis.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
Ethics statement
The studies involving humans were approved by Ethical Review Committee of Guizhou Provincial People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
FY: Writing – original draft, Writing – review & editing. YL: Investigation, Writing – original draft. XS: Software, Writing – original draft. XZ: Data curation, Writing – original draft. LS: Methodology, Writing – original draft. TG: Writing – review & editing, Funding acquisition. YR: Writing – review & editing. BL: Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research and/or publication of this article. Regional fund of national nature science foundation of China: 822604312. Guizhou Provincial Science and Technology Project [ZK(2022) 252]. Support plan project of Guizhou provincial science and technology department: [2023] Normal 196.
Acknowledgements
Thanks to the National Natural Science Foundation of China (82260431) and the Science and Technology Support Plan of Guizhou Province [2023]. General 196 and the Guizhou Provincial Science and Technology Foundation (ZK[2022] 252) supported this study, and we also thank Guizhou Provincial People's Hospital for allowing retrospective access to the data and assisting us with statistical analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TKA, total knee arthroplasty; HKA, hip-knee-ankle angle; AP, anterior-posterior radiographs; RLL, incidence of radiolucency; KSS score, American knee society score; BMI, body mass index; KSRES, radiographic evaluation scoring system for total knee arthroplasty; SPSSS, statistical package for social sciences.
References
1. Alenazi AM, Alqahtani BA, Vennu V, Alshehri MM, Alanazi AD, Alrawaili SM, et al. Gait speed as a predictor for diabetes incidence in people with or at risk of knee osteoarthritis: a longitudinal analysis from the osteoarthritis initiative. Int J Environ Res Public Health. (2021) 18:20210421. doi: 10.3390/ijerph18094414
2. Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. Oarsi guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. (2019) 27:1578–89. doi: 10.1016/j.joca.2019.06.011
3. Memtsoudis SG, Della Valle AG, Besculides MC, Gaber L, Laskin R. Trends in demographics, comorbidity profiles, in-hospital complications and mortality associated with primary knee arthroplasty. J Arthroplasty. (2009) 24:518–27. doi: 10.1016/j.arth.2008.01.307
4. Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME, et al. Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am. (2013) 95:126–31. doi: 10.2106/JBJS.K.00607
5. Marcovigi A, Zambianchi F, Giorgini A, Digennaro V, Catani F. The impact of bone deformity on osteoarthritic varus knee correctability. J Arthroplasty. (2016) 31:2677–84. doi: 10.1016/j.arth.2016.07.007
6. Fehring TK, Fehring KA, Anderson LA, Otero JE, Springer BD. Catastrophic varus collapse of the tibia in obese total knee arthroplasty. J Arthroplasty. (2017) 32:1625–9. doi: 10.1016/j.arth.2016.12.001
7. Keating EM, Meding JB, Faris PM, Ritter MA. Long-term followup of nonmodular total knee replacements. Clin Orthop Relat Res. (2002) 404:34–9. doi: 10.1097/00003086-200211000-00007
8. Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, et al. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. (2004) 428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e
9. Scott CE, Biant LC. The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br. (2012) 94:1009–15. doi: 10.1302/0301-620X.94B8.28289
10. Lonner JH, Klotz M, Levitz C, Lotke PA. Changes in bone density after cemented total knee arthroplasty: influence of stem design. J Arthroplasty. (2001) 16:107–11. doi: 10.1054/arth.2001.16486
11. Gonzalez FJ Q, Meyers KN, Schraut N, Mehrotra KG, Lipman JD, Wright TM, et al. Do metaphyseal cones and stems provide any biomechanical advantage for moderate contained tibial defects in revision TKA? A finite-element analysis based on a cadaver model. Clin Orthop Relat Res. (2021) 479:2534–46. doi: 10.1097/CORR.0000000000001912
12. Gopalakrishnan A, Hedley AK, Kester MA. Magnitude of cement-device interfacial stresses with and without tibial stemming: impact of BMI. J Knee Surg. (2011) 24:3–8. doi: 10.1055/s-0031-1275388
13. Barrack RL, Stanley T, Burt M, Hopkins S. The effect of stem design on end-of-stem pain in revision total knee arthroplasty. J Arthroplasty. (2004) 19:119–24. doi: 10.1016/j.arth.2004.06.009
14. Glenn JC, Sokoloski SN, Damer BM, Tabit JM. Tibia pain at end of stem with stemmed revision total knee arthroplasty: treatment with cortical strut graft technique. J Arthroplasty. (2010) 25:497.e1–5. doi: 10.1016/j.arth.2009.02.020
15. Goudarz Mehdikhani K, Morales Moreno B, Reid JJ, de Paz Nieves A, Lee YY, Gonzalez Della Valle A. An algorithmic, pie-crusting medial soft tissue release reduces the need for constrained inserts patients with severe varus deformity undergoing total knee arthroplasty. J Arthroplasty. (2016) 31:1465–9. doi: 10.1016/j.arth.2016.01.006
16. Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB, Kinemax Outcomes G. Validity and responsiveness of the knee society clinical rating system in comparison with the sf-36 and WOMAC. J Bone Joint Surg Am. (2001) 83:1856–64. doi: 10.2106/00004623-200112000-00014
17. Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR. Development of a modern knee society radiographic evaluation system and methodology for total knee arthroplasty. J Arthroplasty. (2015) 30:2311–4. doi: 10.1016/j.arth.2015.05.049
18. Chalmers BP, Sculco PK, Fehring KA, Trousdale RT, Taunton MJ. A novel percentage-based system for determining aseptic loosening of total knee arthroplasty tibial components. J Arthroplasty. (2017) 32:2274–8. doi: 10.1016/j.arth.2017.02.020
19. Hegde V, Bracey DN, Brady AC, Kleeman-Forsthuber LT, Dennis DA, Jennings JM. A prophylactic tibial stem reduces rates of early aseptic loosening in patients with severe preoperative varus deformity in primary total knee arthroplasty. J Arthroplasty. (2021) 36:2319–24. doi: 10.1016/j.arth.2021.01.049
20. Fournier G, Muller B, Gaillard R, Batailler C, Lustig S, Servien E. Increased survival rate for primary TKA with tibial short extension stems for severe varus deformities at a minimum of 2 years follow-up. Knee Surg Sports Traumatol Arthrosc. (2020) 28:3780–6. doi: 10.1007/s00167-020-05848-2
21. Steere JT, Sobieraj MC, DeFrancesco CJ, Israelite CL, Nelson CL, Kamath AF. Prophylactic tibial stem fixation in the obese: comparative early results in primary total knee arthroplasty. Knee Surg RelatRes. (2018) 30:227–33. doi: 10.5792/ksrr.18.022
Keywords: total knee arthroplasty, knee varus deformity, tibial bone defect, the tibial extension stem, surgery
Citation: Yuan F, Li Y, Shen X, Zhu X, Sun L, Ren Y, Guo T and Li B (2025) Clinical application of the tibial extension stem in primary TKA for knee varus deformity combined with tibial bone defect. Front. Surg. 12:1558338. doi: 10.3389/fsurg.2025.1558338
Received: 10 January 2025; Accepted: 26 February 2025;
Published: 18 March 2025.
Edited by:
Hongzhi Hu, Huazhong University of Science and Technology, ChinaReviewed by:
Yusong Yuan, China-Japan Friendship Hospital, ChinaZhipeng Dai, People’s Hospital of Zhengzhou University, China
Copyright: © 2025 Yuan, Li, Shen, Zhu, Sun, Ren, Guo and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bo Li, bXlyb25sZWVAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Fei Yuan
Fei Yuan Yankun Li1,†
Yankun Li1,†