
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 11 February 2025
Sec. Orthopedic Surgery
Volume 12 - 2025 | https://doi.org/10.3389/fsurg.2025.1550166
This article is part of the Research Topic New Advances in Prosthetic Surgery of Large Joints View all articles
 Hongyu Jiang1,2,3
Hongyu Jiang1,2,3 Xueke Chang2,3
Xueke Chang2,3 Fubin Yu4
Fubin Yu4 Wei Li4
Wei Li4 Naihan Fang2,3
Naihan Fang2,3 Jianzhi Man2,3
Jianzhi Man2,3 Kangshu Guo2,3
Kangshu Guo2,3 Hongzheng Meng1,2*
Hongzheng Meng1,2* Wenqiang Zhang2*
Wenqiang Zhang2*
Aim: We aimed to explore the threshold of preoperative range of motion (ROM) and flxion contacture (FC) as a predictor of Poor knee function after TKA.
Method: A retrospective analysis was conducted on 84 Patients with haemophilia (PWH) (113 knees) who underwent knee arthroplasty in our hospital from January 2010 to December 2020 (mean follow-up 70.7 ± 22.4 months). General information, hemophilia information, surgical information, follow-up information were collected. Knees were divided into two groups: Group poor (41 knees) and Group excellent (72 knees). In the clinical evaluation, the FC, ROM and American Society Knee clinical Score (KSC), American Society Knee functional Score (KSF), Hospital for Special Surgery (HSS) scores were used preoperatively and at the final follow-up visit. Receiver operating characteristics (ROC) analysis was used to analyze the threshold of preoperative ROM and FC as a predictor of Poor knee function after TKA.
Result: Postoperative knee joint KSC, KSF, and HSS scores, as well as ROM and reduction in FC deformities at the last follow-up, improved significantly compared to preoperative levels. A notable correlation was observed between ROM and FC and the outcome of knee arthroplasty. The cutoff value of preoperative fexion contracture and ROM for poor knee function at last-follow up was 16.5° and 61.5°.
Conclusion: The study concludes that the efficacy of knee joint replacement surgery in hemophilia patients is influenced by the pre-ROM and Pre-FC. The better the pre- ROM, the better the knee efficacy. The greater the pre- flexion contracture degree, the worse the knee efficacy.
Hemophilia, a blood coagulation disorder caused by a deficiency of coagulation factors, predominantly manifests as bleeding of varying degrees and locations. The most common being sites are the limb joints, particularly the knee joints, which constitute about 45% of all joint bleeding incidents (1). Repeated intra-articular hemorrhage leads to articular cartilage destruction, joint space narrowing, reduced joint mobility, joint deformity, and ultimately, haemophilic arthropathy. The increased bleeding duration, continual iron deposition, and ongoing damage to synovial tissue and cartilage result in chronic proliferative synovial inflammation, exacerbating articular cartilage destruction (2, 3).
Because of postoperative pain and muscle atrophy, rehabilitation training is more arduous for patients with haemophilia (PWH), with recovery being inferior to that of osteoarthritis patients. Prosthesis survival post-surgery is lower in PWH compared to non- hemophiliac individuals, such as older patients with primary osteoarthritis (4, 5). Possible reasons include younger age at the time of surgery, higher activity, heavy wear of the prosthesis, and higher incidence of postoperative infection.
The average range of motion (ROM) of PWH after total knee replacement is less than that in cases of patients with osteoarthritis. Intra-capsular fibrotic changes and extracapsular muscle contractures are typical problems that affect the operative outcomes after TKA (6). The flexion contracture (FC) of the knee joint, especially its rapid progression, is one of the important indication criteria for TKA surgery. The level of postoperative contracture is important for successful outcomes of surgery as well.
Morphologically, these patients often exhibit developmental deformities of the tibial plateau, a reduced aspect ratio of the plateau, flattening of the intercondylar eminence, early formation of large osteophytes on the tibial plateau, altered positioning of the tibial tuberosity, and square patella cartilage formation, accompanied by extensive arthrofibrosis (7). Additionally, joint deformity often leads to a small fronto-occipital diameter and a larger right-left diameter of the femoral and tibial sides, complicating the prosthetic coverage of articular osteotomy surfaces and the intraoperative selection of femoral prosthesis size, as well as determining anatomical markers for the tibial component in tibial plateau replacement (8–10).
Considering the aforementioned studies, it is evident that PWH present greater surgical challenges and generally poorer postoperative outcomes, despite representing a small proportion of all knee replacement surgeries.
The objective of this study is to (1) compare the preoperative and postoperative knee function after total knee arthroplasty (TKA) in HA and, (2) determine the threshold of preoperative range of motion (ROM) and flexion contracture (FC) as a predictor of Poor knee function after TKA.
Inclusion criteria were: (1) Patients with a confirmed diagnosis of hemophilia who underwent knee replacement; (2) Patients receiving total knee replacement at the First Affiliated Hospital of Shandong First Medical University. Exclusion criteria included: (1) Patients lacking essential information such as demographics, laboratory, and surgical data; (2) Patients with concurrent conditions like tumors; (3) Patients without minimal 4-year follow-up.
All surgeries were conducted by the same department's physician team. PWH were classified into type A and B based onbased on coagulation factor deficiency. Patients were categorized into mild hemophilia (5%–40% coagulation factor activity), moderate (1%–5%), and severe (<1%) groups according to severity. Patients were categorized based on their coagulation factor usage into on-demand and prophylactic treatment groups. Postoperative knee joint outcomes were classified as excellent or poor. The excellent category was defined by scores of 70 or higher on the HSS, KSC, and KSF, a final follow-up ROM of at least 90°, FC under 15°, satisfactory incision healing, absence of infection, exudation, non-healing or delayed healing wounds, and no need for postoperative revision. Patients failing to meet these standards were placed in the poor category.
According to the Expert Consensus on Management Guide for Hemophilia (11), the FVIII level should be kept at 80%–100% on the operation day, 60%–80% on 1–3 days after the operation, 40%–60% on 4–6 days after the operation and 30%–50% on 7–14 days after the operation. All patients had no autologous blood transfusion. If the patient has HB <70 g/L or HCT <25%, it is considered as an indication that allogeneic blood transfusion is needed (12). Pain control was managed using intravenous narcotics by an intravenous patient controlled analgesia line and non-steroid anti-inflammatory drugs.
All PWH underwent a medial parapatellar approach, receiving intravenous tranexamic acid (TXA) (15 mg/kg) 10 min before skin incision and local application of TXA (1 g) in each joint post-joint capsule closure. Antibiotic prophylaxis was administered 30 min before and after surgery, using intravenous cefazolin (2.0 g) at regular intervals, or clindamycin for those allergic to cephalosporin. All operations are performed using mechanical alignment methods (Figure 1). To reduce postoperative bleeding and prevent infection, no drains were used. Pain management included intraoperative joint medication and postoperative oral tramadol (50 mg/bid). General anesthesia was employed, and the prosthesis was fixed with bone cement intraoperatively, akin to conventional total knee replacement procedures.
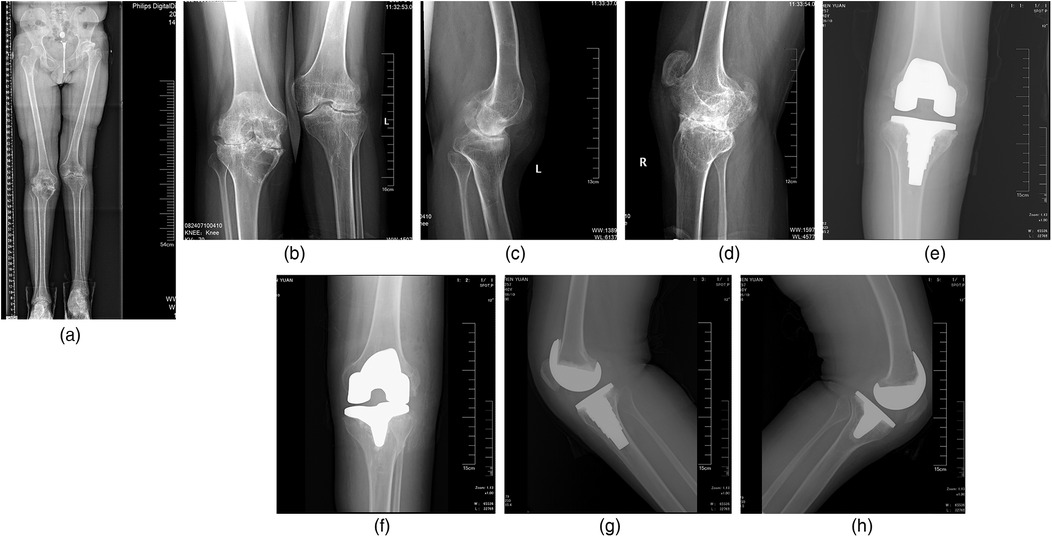
Figure 1. Radiographs of a 28-year-old male patient with severe haemophilic arthropathy. Preoperative x-rays showed extensive destruction of an articular surface, narrowing of the joint space, and a square patella. All operations are performed using mechanical alignment methods. (a) Preoperative anteroposterior radiographs of lower extremity length; (b) preoperative anteroposterior radiograph; (c,d) preoperative lateral radiograph of affected knee joint; (e,f) postoperative coronal knee radiographs; (g,h) postoperative sagittal knee radiographs.
PWH did not receive anticoagulant therapy post-surgery. Physical methods, including ankle pumps and lower extremity elastic bandages, were employed to prevent deep venous thrombosis in the lower extremities. Patients engaged in exercises such as straight leg raises, ankle flexion, and extension. Continuous passive motion was used routinely, and an intensive rehabilitation protocol with active assisted range of motion exercises was encouraged on the first postoperative day and continued twice daily.
Data were analyzed using SPSS version 30.0. Preoperative and last follow-up values were compared using the t-test and chi-squared tests. In all analyses, p < 0.05 was considered statistically significant. The relationship between Preoperative values of FC, ROM and knee scores was investigated through the use of correlation analysis. Through receiver operating characteristics (ROC) analysis, we aimed to determine the threshold of preoperative ROM and FC as a predictor of Poor knee function after TKA.
A total of 84 (113 knees) PWH were included in this study. A total of 41 knees in the poor group and 72 knees in the excellent group were included according to the evaluation criteria. The follow-up ranged from 47 to 120 months (mean follow-up 70.7 ± 22.4 months). Table 1 showed a significant difference in the severity grading between the groups; a higher proportion of severe hemophilia was noted in the poor group. All eight patients undergoing quadriceps plasty belonged to the poor group (p < 0.001), and a higher proportion of patients in the poor group underwent bilateral knee replacements in a single anesthesia session (p = 0.037). The intraoperative bleeding was significantly higher in the poor group than in the excellent group. No significant differences were found in the Age, BMI, hemophilia type, Coagulation factor usage, Total Bleeding, Intraoperative blood transfusion or Length of hospital stay.
The FC decreased from 15.9° ± 9.5° to 7.9° ± 5.8°. The ROM increased from 60.2° ± 16.8° to 74.7° ± 9.7°. Similarly, the KSC, KSF and HSS greatly improved (P < 0.001). Thus, there were significant differences between the preoperative and final follow-up values of FC, ROM, KSC, KSF, and HSS, as shown in Table 2. Table 3 showed the degree of ROM at last follow-up was greater in excellent group (79.4° vs. 66.5°, p < 0.001). The degree of flexion contracture at last follow-up was greater in the poor group (11.9° vs. 5.6°, p < 0.001). The degree of ROM change and FC change was greater in poor group (ROM change 19.4° vs. 11.1°, p < 0.001; FC change 11.2° vs. 6.4°). The degree of preoperative ROM and FC was greater in excellent group (Pre-ROM 68.2° vs. 46.2°, p < 0.001; Pre-FC 12° vs. 23°). The preoperative and the last follow-up KSC, KSF and HSS scores were greater in the excellent group in comparison to the poor group. KSC, KSF, HSS was positively correlated with preoperative ROM (P < 0.001); KSC, KSF, HSS was negatively correlated with preoperative FC(P < 0.001) (Figure 2). When evaluating the cutoff point of preoperative FC and ROM for Poor knee function after TKA at last follow-up on ROC analysis, the cutoff value was 61.5° in the ROM and 16.5° in FC (Figure 3).
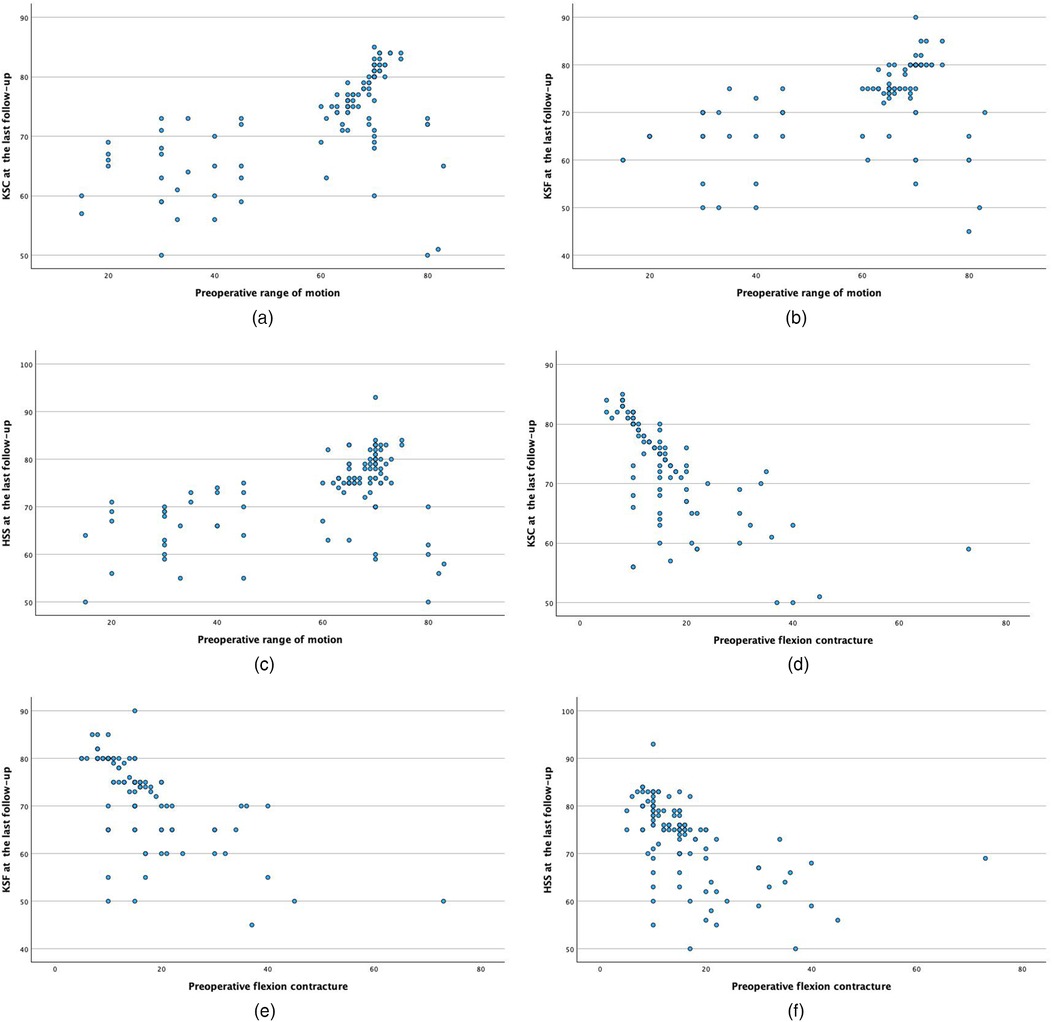
Figure 2. Correlation analysis between preoperative FC, ROM and last follow-up KSC, KSF, HSS. (a) Correlation analysis between pre-ROM and last follow-up KSC(P < 0.001); (b) correlation analysis between pre-ROM and last follow-up KSF(P < 0.001); (c) correlation analysis between pre-ROM and last follow-up HSS(P < 0.001); (d) correlation analysis between pre-FC and last follow-up KSC(P < 0.001); (e) correlation analysis between pre-FC and last follow-up KSF(P < 0.001); (f) correlation analysis between pre-FC and last follow-up HSS(P < 0.001).
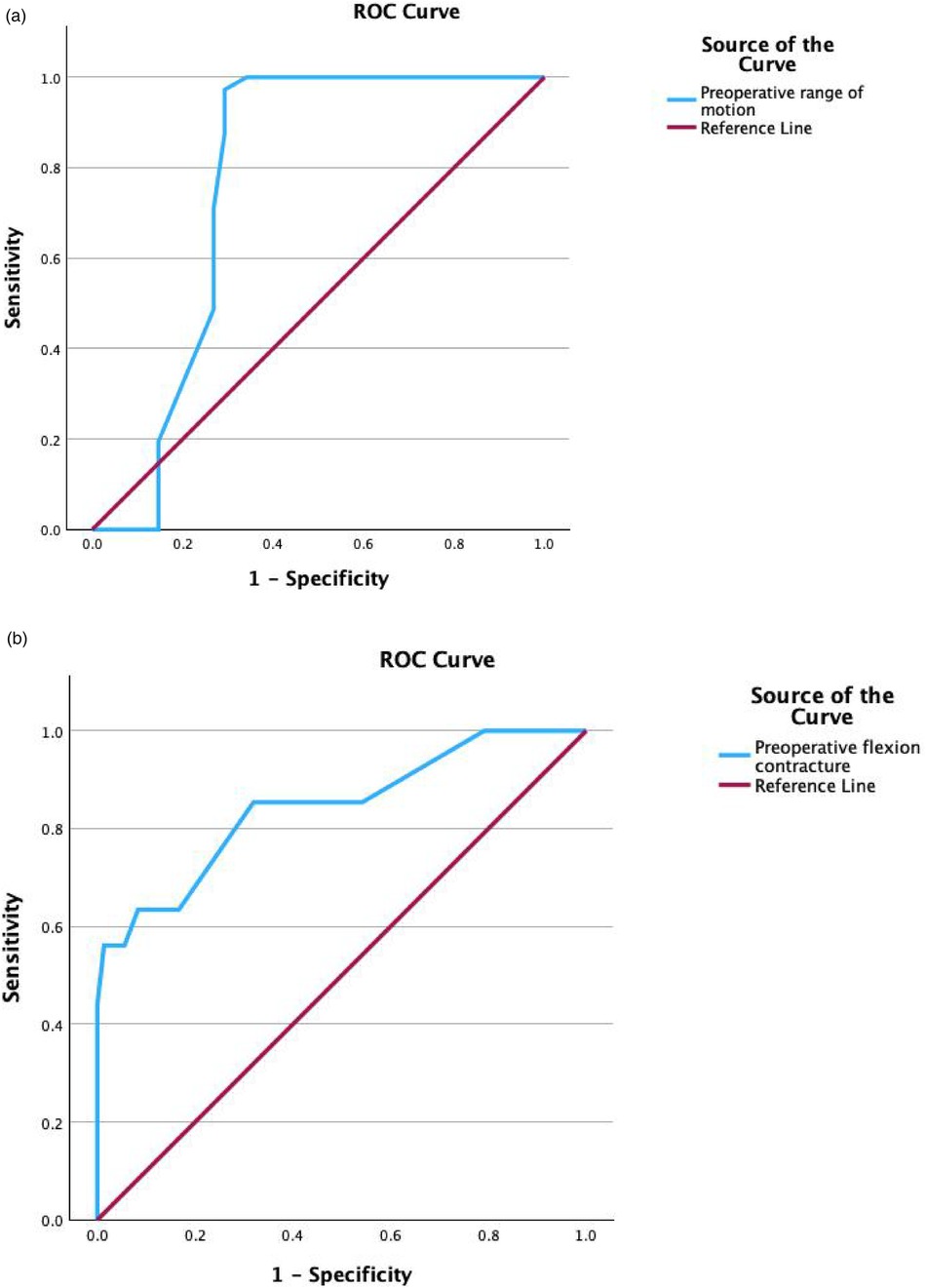
Figure 3. ROC curve to determine the threshold of preoperative ROM and FC as a predictor of poor knee function after TKA. (a) The threshold of preoperative ROM as a predictor of Poor knee function after TKA [Area Under the ROC Curve (AUC) = 0.767 Cutoff = 61.5°]. (b) The threshold of preoperative FC as a predictor of Poor knee function after TKA [Area Under the ROC Curve (AUC) = 0.843 Cutoff = 16.5°].
Knee replacement has been demonstrated to be an effective intervention for improving knee function, knee scores, and knee mobility. Atilla et al. followed 21 patients, utilizing the Knee Society Score (KSS) to evaluate functional and pain levels, noting an increase in ROM from 26.7° preoperatively to 73.0° postoperatively and a decrease in flexion contractures from 21.7° to 8.3°, with the KSS improving from 22.9 to 72.9 points. Pain assessments indicated a significant decrease from 8.4 preoperatively to 2.1 postoperatively, highlighting the procedure's efficacy in enhancing function and alleviating pain in hemophilia patients.
The most important finding of this study is determine the threshold of preoperative ROM and FC as a predictor of Poor knee function after TKA. We strongly advise individuals with hemophilia to prioritize the strengthening of their knee joints by maintaining ROM above 61.5° and FC levels below 16.5°.
Preoperative range of motion (ROM) is usually considered to be the most important predictor of functional outcome after TKA. Atilla et al. also observed that replacements in knees with poor mobility had inferior outcomes compared to those with more flexible joints (13). In a study of 20 patients with haemophilia, the mean ROM at last follow-up was 92° and the mean preoperative flexion contracture was 3° (14). In a cohort of 116 haemophilic procedures at a single institution, a 5° improvement in flexion contracture and a 15° improvement in ROM were reported (15). In our cohort, the average ROM change of the knee joint at the last follow-up was 14.5° and the average FC change was 8°. Compared with the above literature, Our study yielded similar results. This study confirms that knee replacement is effective in managing hemophilic arthropathy.
A study by Noble et al. showed that patients' expectations were highly correlated with their satisfaction after total knee replacement (16). With their serious functional impairment and extreme pain preoperatively, the daily needs of our patients were unfulfilled before TKA. For activities of daily living, 65°–70° of knee flexion are necessary for the swing phase of normal gait, whereas at least 90° are needed to descend stairs and 105° to rise from a low chair (5).
Yi Liu et al. analyzed 71 hemophilia patients (78 knee joints), finding that severely rigid knees (preoperative ROM ≤50°) experienced poorer outcomes and more complications than moderately stiff knees (ROM 50°–90°) (17). These findings are consistent with ours. Other studies have shown a negative correlation between preoperative flexion contracture degrees and postoperative knee function.
Flexion contracture in hemophilic arthropathy is caused from fibrosis of the surrounding soft tissue, combined with periarticular osteopenia (18). Fernandez A et al. reviewed 2,634 knee replacements, finding that contractures over 10° were associated with significantly lower international knee scores and ROM compared to those under 10° (19). Kagaya et al. reported that joint contractures of the lower extremity affect the gait pattern and decrease the patients' ability to walk. They concluded that hip or knee flexion contracture of <15° and absence of ankle equinus is required to maintain positive step length and forward movement of the centre of gravity (20). In the case of flexion contracture following TKA, there are many methods to correct this deformity; such as, manipulation under anesthesia (21), dynamic splinting (22) or revision TKA (23). Our study not only compares the knee function of the excellent group with that of the poor group, but also calculates the exact values of Preoperative ROM and Pre-FC using the ROC analysis.
In summary, ROM and FC are closely related to postoperative knee outcomes, and corresponding functional knee exercises are extremely important. For PWH with a flexion contracture deformity of the knee joint, it is recommended that they apply pressure to the knee joint with a 5-kilogram weight for 10 min, three times a day. In addition, patients should be encouraged to walk more every day, ensuring that they take in more than 5,000 steps. For PWH with severe knee flexion and extension deficits, it is recommended Manipulation under anesthesia.
Concerning knee mobility, Baumgardner et al. (24) identified age as a factor, with mobility decreasing as patients age, possibly due to reduced joint use or immobilization, which leads to quadriceps atrophy and restricts mobility or causes stiffness. Effective postoperative rehabilitation, especially quadriceps training, is crucial as most patients suffer muscle atrophy from inadequate dynamic joint stability, creating a cycle of joint bleeding and exacerbating hemophilic arthropathy. Annual bleeding frequency also impacts mobility, with higher frequencies limiting mobility. Soucie and others have shown that knee function significantly improves when annual bleeding episodes are fewer than 3 (25). Pabinger I advocates for regular administration of concentrated coagulation factors to hemophilia patients (26), while Schramm recommends starting prophylactic treatment for those with 2–3 bleeds per month (27). Prophylactic transfusions and strengthening quadriceps exercises are advised to enhance mobility and improve outcomes following knee replacement surgery.
Obesity is a major health concern not only in the general population but also in patients with haemophilia (28). Body adiposity and disease severity in haemophilia have been found in cross-sectional studies to be negatively associated with joint mobility. Compared with haemophilia males with normal BMI, those who were obese had lower ROM at initial visit and a faster rate of joint mobility loss in the lower limbs (29). We suggest that body weight control and effective treatment of bleeds should be implemented together to achieve better joint ROM outcomes in males with haemophilia.
Research indicates that severity grading is also a significant factor. The age of first bleeding in patients with severe grading hemophilia was significantly younger than that of mild grading patients (p < 0.05), and the rate of joint deformity in patients with severe grading hemophilia was statistically different compared to that of mild to moderate grading hemophilia (p < 0.05). Severe grading hemophilia patients have a high frequency of bleeding, and the frequency of joint bleeding is an important influencing factor in the formation of hemophilic arthritis. The number of annual bleeds also affects joint mobility, and the degree of restriction of joint mobility is more severe in patients with a high frequency of bleeding (25).
This study had certain limitations. First, this is a retrospective study, with non-flexible knees constituting the control group. Considering the rare incidence of hemophilia, it is difficult to conduct such a prospective study in a single institution. Second, the 5-year follow-up time for some patients was relatively short. Hence, we could not determine the occurrence of late complications, such as aseptic loosening of the prosthesis or late prosthetic joint infection, which potentially develops over a long period after surgery. And the scores used to assess efficacy are subjective. Although the sample size is large for a single institution, including samples from multi-center institutions and expanding the sample size to encompass more influencing factors could provide more definitive results. Despite some limitations, data from the present study can be used to inform PWH about the threshold of poor knee function after TKA.
The study concludes that TKA can improve knee function in PWH, and the efficacy of knee joint replacement surgery in PWH is influenced by the preoperative ROM and Preoperative FC. The better the preoperative ROM, the better the knee efficacy. The greater the preoperative flexion contracture degree, the worse the knee efficacy. Statistical analysis revealed that preoperative FC of 16.5° and Preoperative ROM of 61.5° is an important threshold. The authors recommend that hemophilia patients actively exercise their quadriceps to enhance knee mobility.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Ethics Committee of the First Affiliated Hospital of Shandong First Medical University. This study was retrospective and did not require patients to sign informed consent. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this study was retrospective and did not require patients to sign informed consent.
HJ: Conceptualization, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. XC: Formal Analysis, Conceptualization, Writing – review & editing. FY: Formal Analysis, Writing – original draft. WL: Writing – original draft, Conceptualization, Formal Analysis. NF: Writing – review & editing, Formal Analysis. JM: Writing – review & editing, Conceptualization, Formal Analysis. KG: Writing – review & editing, Formal Analysis. WZ: Writing – original draft, Writing – review & editing, Funding acquisition, Project administration, Resources, Supervision. HM: Writing – original draft, Writing – review & editing, Funding acquisition, Project administration, Resources.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Natural Science Foundation of Shandong Province (No. ZR2022MH299) and Natural Science Foundation of Shandong Province (No. ZR2021MH166).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Onwuzurike N, Warrier I, Lusher JM. Types of bleeding seen during the first 30 months of life in children with severe haemophilia A and B. Haemophilia. (1996) 2:137–40. doi: 10.1111/j.1365-2516.1996.tb00156.x
2. Zhu H, Meng Y, Tong P, Zhang S. Pathological mechanism of joint destruction in haemophilic arthropathy. Mol Biol Rep. (2021) 48:969–74. doi: 10.1007/s11033-020-06052-8
3. Pasta G, Annunziata S, Polizzi A, Caliogna L, Jannelli E, Minen A, et al. The progression of hemophilic arthropathy: the role of biomarkers. Int J Mol Sci. (2020) 21:7292. doi: 10.3390/ijms21197292
4. Ernstbrunner L, Hingsammer A, Catanzaro S, Sutter R, Brand B, Wieser K, et al. Long-term results of total knee arthroplasty in haemophilic patients: an 18-year follow-up. Knee Surg Sports Traumatol Arthrosc. (2017) 25:3431–8. doi: 10.1007/s00167-016-4340-6
5. Strauss AC, Schmolders J, Friedrich MJ, Pflugmacher R, Müller MC, Goldmann G, et al. Outcome after total knee arthroplasty in haemophilic patients with stiff knees. Haemophilia. (2015) 21:e300–5. doi: 10.1111/hae.12698
6. Goddard NJ, Rodriguez-Merchan EC, Wiedel JD. Total knee replacement in haemophilia. Haemophilia. (2002) 8:382–6. doi: 10.1046/j.1365-2516.2002.00604.x
7. Kang DG, Khurana S, Baek JH, Park YS, Lee SH, Kim KI. Efficacy and safety using autotransfusion system with postoperative shed blood following total knee arthroplasty in haemophilia. Haemophilia. (2014) 20:129–32. doi: 10.1111/hae.12244
8. Ma Y, Mizu-Uchi H, Ushio T, Hamai S, Akasaki Y, Murakami K, et al. Bony landmarks with tibial cutting surface are useful to avoid rotational mismatch in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2019) 27:1570–9. doi: 10.1007/s00167-018-5052-x
9. Kawahara S, Okazaki K, Matsuda S, Mitsuyasu H, Nakahara H, Okamoto S, et al. Medial sixth of the patellar tendon at the tibial attachment is useful for the anterior reference in rotational alignment of the tibial component. Knee Surg Sports Traumatol Arthrosc. (2014) 22:1070–5. doi: 10.1007/s00167-013-2468-1
10. Hirakawa M, Miyazaki M, Ikeda S, Matsumoto Y, Kondo M, Tsumura H. Evaluation of the rotational alignment of the tibial component in total knee arthroplasty: position prioritizing maximum coverage. Eur J Orthop Surg Traumatol. (2017) 27:119–24. doi: 10.1007/s00590-016-1850-3
11. Srivastava A, Brewer AK, Mauser-Bunschoten EP, Key NS, Kitchen S, Llinas A, et al. Guidelines for the management of hemophilia. Haemophilia. (2013) 19(1):e1–47. doi: 10.1111/j.1365-2516.2012.02909.x
12. Murphy MF, Wallington TB, Kelsey P, Boulton F, Bruce M, Cohen H, et al. Guidelines for the clinical use of red cell transfusions. Br J Haematol. (2001) 113(1):24–31. doi: 10.1046/j.1365-2141.2001.02701.x
13. Atilla B, Caglar O, Pekmezci M, Buyukasik Y, Tokgozoglu AM, Alpaslan M. Pre-operative flexion contracture determines the functional outcome of haemophilic arthropathy treated with total knee arthroplasty. Haemophilia. (2012) 18(3):358–63. doi: 10.1111/j.1365-2516.2011.02695.x
14. Innocenti M, Civinini R, Carulli C, Villano M, Linari S, Morfini M. A modular total knee arthroplasty in haemophilic arthropathy. Knee. (2007) 14(4):264–8. doi: 10.1016/j.knee.2007.05.001
15. Solimeno LP, Mancuso ME, Pasta G, Santagostino E, Perfetto S, Mannucci PM. Factors influencing the long-term outcome of primary total knee replacement in haemophiliacs: a review of 116 procedures at a single institution. Br J Haematol. (2009) 145(2):227–34. doi: 10.1111/j.1365-2141.2009.07613.x
16. Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. (2006) 452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e
17. Liu Y, Liu YF, Meng HZ, Sun T, Gao P, Li ZZ, et al. Total knee arthroplasty exhibits satisfactory long-term clinical efficacy in the treatment of patients with haemophilia with stiff knees. Front Surg. (2023) 9:1014844. doi: 10.3389/fsurg.2022.1014844
18. Atilla B, Caglar O, Pekmezci M, Buyukasik Y, Tokgozoglu AM, Alpaslan M. Pre operative flexion contracture determines the functional outcome of haemophilic arthropathy treated with total knee arthroplasty, haemoph. Off J World Fed Hemoph. (2012) 18(3):358–63. doi: 10.1111/j.1365-2516.2011.02695.x
19. Fernandez A, Sappey-Marinier E, Shatrov J, Batailler C, Neyret P, Huten D, et al. Preoperative flexion contracture does not affect outcome in total knee arthroplasty: a case-control study of 2,634 TKAs. Orthop Traumatol Surg Res. (2023) 109(5):103592. doi: 10.1016/j.otsr.2023.103592
20. Kagaya H, Ito S, Iwami T, Obinata G, Shimada Y. A computer simulation of human walking in persons with joint contractures. Tohoku J Exp Med. (2003) 200(1):31–7. doi: 10.1620/tjem.200.31
21. Li Z, Lan F, Shen Y, An S, Xu N, Yin C, et al. Prediction of the need for manipulation under anesthesia for flexion contracture after total knee arthroplasty in patients of advanced age. J Int Med Res. (2019) 47(7):3061–9. doi: 10.1177/0300060519851328
22. Finger E, Willis FB. Dynamic splinting for knee flexion contracture following total knee arthroplasty: a case report. Cases J. (2008) 1 (1):421. doi: 10.1186/1757-1626-1-421
23. Fehring TK, Odum SM, Griffin WL, McCoy TH, Masonis JL. Surgical treatment of flexion contractures after total knee arthroplasty. J Arthroplast. (2007) 22(6 Suppl 2):62–6. doi: 10.1016/j.arth.2007.03.037
24. Baumgardner J, Elon L, Antun A, Stein S, Ribeiro M, Slovensky L, et al. Physical activity and functional abilities in adult males with haemophilia: a cross-sectional survey from a single US haemophilia treatment centre. Haemophilia. (2013) 19(4):551–7. doi: 10.1111/hae.12134
25. Soucie JM, Cianfrini C, Janco RL, Kulkarni R, Hambleton J, Evatt B, et al. Joint range-of-motion limitations among young males with hemophilia: prevalence and risk factors. Blood. (2004) 103(7):2467–73. doi: 10.1182/blood-2003-05-1457
26. Pabinger I, Heistinger M, Muntean W, Reitter-Pfoertner SE, Rosenlechner S, Schindl T, et al. Hämophiliebehandlung in Österreich [treatment of haemophilia in Austria]. Wien Klin Wochenschr. (2015) 127(Suppl 3):115–30. doi: 10.1007/s00508-015-0872-x
27. Schramm W. Experience with prophylaxis in Germany. Semin Hematol. (1993) 30(3 Suppl 2):12–5.8367737
28. Biere-Rafi S, Haak BW, Peters M, Gerdes VE, Büller HR, Kamphuisen PW. The impairment in daily life of obese haemophiliacs. Haemophilia. (2011) 17(2):204–8. doi: 10.1111/j.1365-2516.2010.02417.x
Keywords: patients with haemophilia, range of motion, flexion contracture, total knee arthroplasty, knee function
Citation: Jiang H, Chang X, Yu F, Li W, Fang N, Man J, Guo K, Meng H and Zhang W (2025) How much preoperative ROM and FC is a predictor for poor result after total knee arthroplasty in hemophilic arthropathy?. Front. Surg. 12:1550166. doi: 10.3389/fsurg.2025.1550166
Received: 23 December 2024; Accepted: 21 January 2025;
Published: 11 February 2025.
Edited by:
Michela Saracco, University of Naples Federico II, ItalyReviewed by:
Arcangelo Russo, Kore University of Enna, ItalyCopyright: © 2025 Jiang, Chang, Yu, Li, Fang, Man, Guo, Meng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenqiang Zhang, cWZzendxQHNpbmEuY29t; Hongzheng Meng, bWh6X2h5QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.