
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 10 April 2025
Sec. Orthopedic Surgery
Volume 12 - 2025 | https://doi.org/10.3389/fsurg.2025.1546873
This article is part of the Research TopicAdvances in Surgical and Basic Research in Hip Surgery: Complications, Artificial Intelligence and Surgery RoboticsView all 4 articles
 Xianglong Zhou
Xianglong Zhou Dongxuan Wei
Dongxuan Wei Jiheng Xiao
Jiheng Xiao Tianyi Xia
Tianyi Xia Haoran Zhou
Haoran Zhou Jianhui Xiang
Jianhui Xiang Hanhong Fang
Hanhong Fang Hui Song*
Hui Song* Liming Xiong*
Liming Xiong*
Objective: The objective of this study is to investigate the clinical efficacy of proximal femoral locking plates in comparison to cannulated compression screws for the treatment of femoral neck fractures.
Methods: A retrospective analysis of clinical data from 50 patients with femoral neck fractures treated at the Department of Orthopaedics, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology from September 2018 to June 2023. Patients were divided into 25 in the PFLP group and 25 in the CCS group. A comparison was made between the two groups in terms of the following variables: basic characteristics, perioperative information, and information during follow-up visits.
Results: The basic characteristics of the two groups were found to exhibit no statistically significant differences (P > 0.05). The PFLP group had significantly longer surgical times and greater Intraoperative hemorrhage loss compared to the CCS group (P < 0.05). The statistical analysis revealed that there were no significant differences in intraoperative fluoroscopy times and Garden index between the two groups (P > 0.05). The PFLP group exhibited a markedly superior fracture healing time, femoral neck shortening, and Harris hip scores in comparison to the CCS group (P < 0.05). The postoperative complication rates were 12% in the PFLP group and 20% in the CCS group, with no statistically significant difference (P > 0.05).
Conclusion: The results of this retrospective study suggest that the PFLP group demonstrated superior outcomes compared to the CCS group in several key areas, including fracture healing time, preservation of femoral neck length, recovery of hip function, and incidence of postoperative complications.
In recent years, the acceleration of global population aging and the frequent occurrence of traffic accidents have led to a significant increase in the incidence of hip fractures, placing a substantial burden on society and the healthcare system (1, 2). It is predicted that there will be 4.5 million hip fractures worldwide by 2050 (3). Among all types of hip fractures, those affecting the femoral neck are the most prevalent, accounting for 3.6% of all fractures and 50% of hip fractures (4). Femoral neck fractures present a substantial challenge in the field of Orthopaedics, exhibiting a high degree of severity and a multitude of complications. The implementation of conservative therapeutic modalities has been observed to frequently result in elevated rates of disability and mortality (5, 6). According to established principles of treatment for femoral neck fractures, early surgical intervention is recommended for the majority of patients who do not have contraindications to surgery (7–9).
The objective of surgical treatment is to restore stability and functionality to the hip joint, thereby reducing the incidence of complications associated with prolonged bed rest, including deep vein thrombosis, pneumonia, and pressure ulcers (10). Currently, the mainstay of surgical treatment for femoral neck fractures is internal fixation or hip arthroplasty. The specific approach is determined by the patient's age, physical condition and the anticipated functional requirements following the procedure (11). For middle-aged and young patients, as well as some elderly patients who are unable to tolerate arthroplasty and those with minor fracture displacement, internal fixation remains the primary choice and is a safe and effective treatment option (10, 12, 13). The primary advantages of internal fixation of femoral neck fractures include preservation of the femoral head, minimal trauma, and a simple surgical technique. The principal determinant of surgical success is the achievement of good anatomical reduction and stable internal fixation (14, 15). The use of stable internal fixation has been shown to facilitate postoperative recovery and reduce the prevalence of complications (16, 17). The most commonly employed internal fixation methods include the use of cannulated compression screws (CCS), femoral neck systems (FNS), proximal femoral locking plates (PFLP) and the combination of cannulated screws with medial support plates. The various methods have distinct advantages and limitations, and there is currently a debate among experts regarding the optimal internal fixation device for treatment (17, 18). The objective of this study is to investigate the clinical efficacy of internal fixation as a treatment for femoral neck fractures. To this end, a retrospective analysis has been conducted to compare the outcomes of proximal femoral locking plates and cannulated screws, with the objective of providing a reference for the treatment of these fractures.
The clinical data of 50 patients with femoral neck fractures admitted to the Department of Orthopaedics of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, China, from September 2018 to June 2023 were retrospectively analyzed. Informed consent was obtained from all participants, and ethical approval was granted by the Medical Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (Approval No. 20240652).
Inclusion criteria: (1) Age 18–65 years (2) Unilateral, closed, fresh femoral neck fracture (less than 3 weeks) (3) Diagnosis of femoral neck fracture based on history, physical examination, and imaging data (4) Normal function of the affected hip joint prior to injury (5) Absence of contraindications to surgery (6) Follow-up of at least 1 year with complete clinical data Exclusion criteria: (1) old, pathological or open femoral neck fractures (2) Serious dysfunction of vital organs such as the heart, lungs, brain and other vital organs, unable to tolerate surgery and anesthesia (3) combined with fracture and dysfunction of other parts of the lower limb (4) poor patient compliance and incomplete clinical data.
All patients were provided with pre-operative symptomatic treatment, including pain relief, edema reduction, and thrombosis prophylaxis. Patients underwent a series of diagnostic imaging procedures, including positive and lateral x-rays, CT scans with three-dimensional reconstruction of the affected hip joint, and ultrasound examinations of the deep and superficial veins of both lower limbs. Pre-operative examinations were performed to exclude contraindications to anesthesia and surgery, and if necessary, cardiovascular medicine, respiratory and critical care medicine, anesthesiology and other related departments were invited to consult with patients to assess their tolerance to surgery.
All patients were administered general anesthesia with tracheal intubation. The patients were positioned in the supine position on an orthopedic lower extremity traction bed. Following the satisfactory completion of closed reduction, the traction bed was secured, and the standard disinfection and draping procedures were conducted. PFLP group (Figure 1): A straight lateral incision of approximately 5 cm was made distally, starting from the highest point of the greater trochanter of the femur. The tissue was then dissected layer by layer until the lateral cortex of the femur was exposed. A proximal femoral locking plate (PFLP) of appropriate length (Tianjin Weiman Biomaterials Company) was placed on the proximal femur. A guide pin was inserted, the depth of the guide pin was measured with a reamer, cannulated locking screws were sequentially inserted, and the position and depth of the cannulated screws were verified with C-arm fluoroscopy. Subsequently, the guide pin was extracted. The screws were positioned within the distal femoral shaft region of the proximal femoral locking plate for fixation. A typical case is shown in Figure 2. CCS group: An inverted triangular configuration was utilized to insert guide pins percutaneously. Subsequent adjustments were made to the position and depth of the guide pins under C-arm fluoroscopy in both anteroposterior and lateral views. The depth of the guide pins was determined by means of a reamer, and cannulated screws (Wuhan Mindray Company) were then inserted in a sequential manner. In patients with relatively weak lateral femoral cortices, the addition of supplementary washers may be considered. Subsequently, the guide pin was extracted. A typical case is shown in Figure 3. The incision was irrigated with saline solution, then sutured in layers and covered with a sterile dressing.

Figure 1. A schematic diagram of a proximal femoral locking plate (A,B) and the treatment of a femoral neck fracture (C).
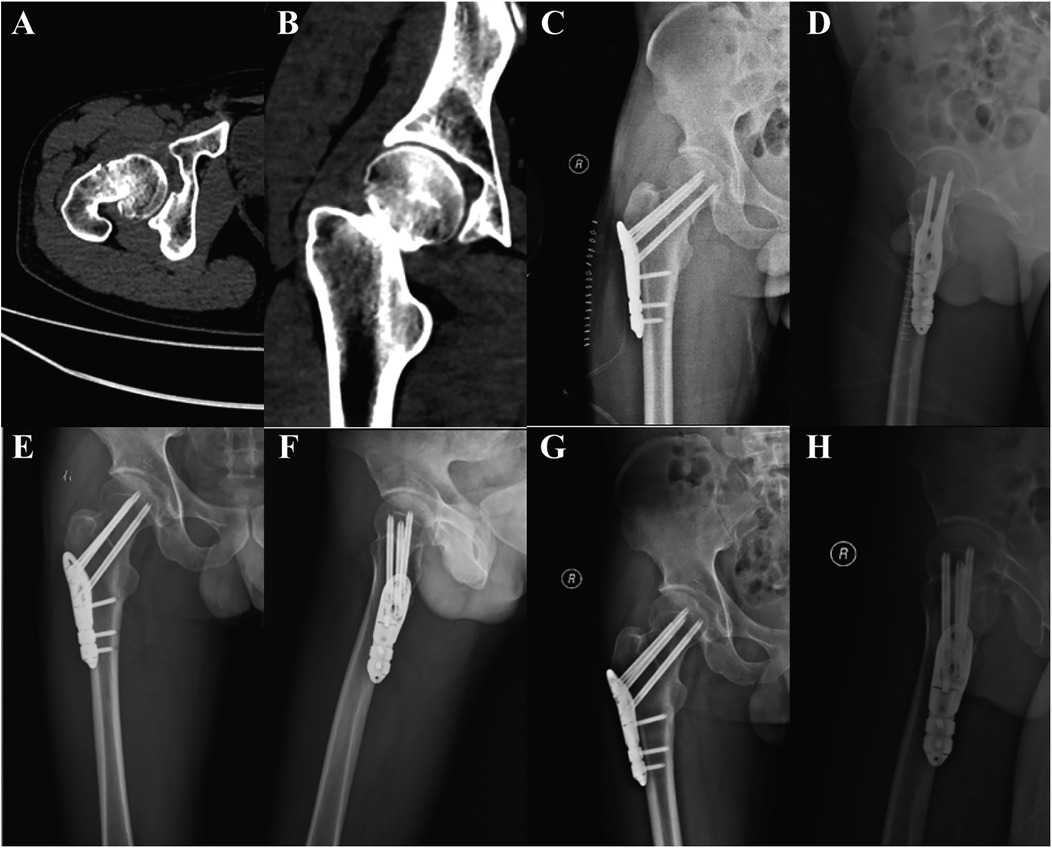
Figure 2. A 40-year-old male patient was admitted to the hospital due to pain and restricted range of motion in the right hip following a traffic injury, and he underwent PFLP treatment. (A,B) Pre-operative CT images of the patient showed a right femoral neck fracture, Garden type IV. (C,D) Review radiographs 1 day post-operatively in the anteroposterior and lateral positions showed good reduction. (E,F) Review radiographs 4 months post-operatively. (G,H) Review radiographs 12 months post-operatively.

Figure 3. A 50-year-old female patient was admitted to the hospital for treatment of right hip pain and limited range of motion following a fall and underwent CCS treatment. (A,B) Pre-operative CT images of the patient showed a right femoral neck fracture, Garden type IV. (C,D) Review radiographs 1 day post-operatively in the anteroposterior and lateral positions showed good reduction. (E,F) Review radiographs 4 months post-operatively. (G,H) Review radiographs 13 months post-operatively.
In the postoperative period, the patient's vital signs were monitored, and pain relief and prophylactic antibiotic therapy were administered in accordance with standard practice. A postoperative review of the hip positive and lateral radiographs was conducted. Following surgery, patients were instructed to perform passive flexion and extension of the hip and knee joints of the affected limb, as well as muscle function exercises. The sutures were removed 10–12 days following the surgical procedure. Patients were monitored via outpatient visits and telephone calls.
The study included 50 patients with femoral neck fractures, divided into two groups: the PFLP group (n = 25) and the CCS group (n = 25). The baseline characteristics included patient age, sex, body mass index (BMI), side of fracture, cause of injury, Garden classification, time from injury to surgery, and duration of follow-up. Perioperative information included Surgical time, intraoperative hemorrhage, intraoperative fluoroscopy times. Subsequent data included a postoperative reassessment of reduction quality (Garden index), fracture healing time, femoral neck shortening at 1 year postoperatively or at the final follow-up, and hip Harris (19) score. The postoperative complications observed included osteonecrosis of the femoral head, bone nonunion, screw withdrawal, and screw breakage.
All data analyses were conducted using IBM SPSS Statistics 29.0 software, as specified in the study methodology. The normality of the distribution of the quantitative data was assessed using the Shapiro–Wilk test, while the equality of variances was evaluated through Levene's test. The quantitative results were expressed as mean ± standard deviation. The data indicated that the variable in question exhibited a mean value of . The differences between the two groups were then compared using a two-independent-samples t-test. Comparisons between groups of qualitative data were analyzed using the chi-squared test or Fisher's exact probability method. All statistical tests were conducted with a significance level of P < 0.05 to ascertain the statistical significance of observed differences.
The differences in age, gender, BMI, fracture side, cause of injury, fracture type, time from injury to surgery, and follow-up time between the two groups were not statistically significant (P > 0.05, Table 1), and were comparable.
Patients treated with PFLP exhibited longer surgical times (81.01 ± 6.43 min vs. 69.28 ± 15.93 min) and increased intraoperative hemorrhage (85.47 ± 18.85 ml vs. 36.76 ± 6.64 ml), with a statistically significant difference (P < 0.05, Table 2). No statistically significant difference was observed in the number of intraoperative fluoroscopies and fracture reduction Garden index between the two groups (P > 0.05, Table 2).
The mean fracture healing time for patients in the PFLP group was 4.85 ± 1.10 months, which was significantly shorter than that of the CCS group (5.66 ± 0.71 months; P < 0.05, Table 3). Both groups exhibited femoral neck shortening following surgery; however, this was significantly less pronounced in the PFLP group compared to the CCS group (1.09 ± 0.99 mm vs. 4.26 ± 4.49 mm, P < 0.05, Table 3). The postoperative Haaris scores for the two groups exhibited a notable disparity (P < 0.05, Table 3), with a mean of 89.12 ± 2.13 for the PFLP cohort and a mean of 84.52 ± 8.43 for the CCS group. With regard to postoperative complications, the incidence rates in the two groups were 12% in the PFLP group and 20% in the CCS group, with no statistically significant difference (P > 0.05, Table 3).
Surgical treatment is the primary intervention for most patients with femoral neck fractures, with the specific surgical approach often contingent on the patient's age. Currently, arthroplasty is the preferred surgical option for elderly patients, particularly those aged 75 and above (20, 21). Although arthroplasty is a more invasive procedure and is associated with complications such as periprosthetic infection and loosening, it has a shorter treatment period and can rapidly reduce pain, restore hip function, and achieve early weight bearing (22). For patients in the younger and middle-aged demographic, internal fixation remains the primary treatment option (23). Nevertheless, a paucity of evidence-based medical literature exists to define the optimal internal fixation treatment. In the present study, we present the clinical results of treating femoral neck fractures with PFLP and CCS. The results showed that the fracture healing time, degree of femoral neck shortening, and Harris score of patients in the PFLP group were significantly superior to those in the CCS group; however, operative time and intraoperative bleeding were longer in the PFLP group compared to the CCS group. These results indicate that PFLP has the potential to accelerate fracture healing, reduce the extent of postoperative femoral neck shortening, and improve hip functionality, but is associated with increased operative time and intraoperative bleeding, and its efficacy in the remaining observed indicators is comparable to that of CCS.
The PFLP treatment of femoral neck fractures necessitates an incisional approach, which entails a larger incision, augmented exposure, and a longer surgical time frame. The advantages of the PFLP include its conformity to the anatomical design of the proximal femur and its preset collo-diaphyseal angle and angle of inclination (24). The design in question has been demonstrated to reduce the damage to the blood supply of the femoral head that is caused by periosteal stripping and repeated adjustments of the guide pins. It is therefore still in the category of minimally invasive surgery. The PFLP demonstrates notable biomechanical advantages, with the threads of its hollow screw tail locking into the plate as a whole. This transfers the bending force borne by the head-neck screws to the femoral diaphysis cortex, providing favorable angular stability and anti-rotation capability. Furthermore, it allows patients to bear weight and undergo rehabilitation training at an early postoperative stage (25–27). This approach better preserves the length of the femoral neck and reduces the incidence of complications such as screw loosening, screw withdrawal, and screw breakage. As a result, the likelihood of requiring a revision procedure is decreased (28). Although the number of studies on PFLP for femoral neck fractures is limited, the results of the available studies corroborate some of the findings of this study (29–31). Although CCS for femoral neck fractures offers several advantages, including a short operative time, minimal surgical trauma, ease of use, and a high healing rate, its three-screw fixation has insufficient resistance to inversion and shear. This can result in fracture end loosening, which may lead to complications such as screw withdrawal, screw breakage, femoral neck shortening, and secondary subrotator fracture (32, 33).
One of the keys to the treatment of femoral neck fractures is quality control of the reduction, and poor reduction is an important factor leading to healing complications and reoperation (34). It is also imperative to give due attention to the correct choice of internal fixation and precise screw placement. Adequate reduction facilitates accurate nailing, while stable internal fixation ensures reduction efficiency and motion stability. In order to ensure optimal outcomes, fluoroscopy of the frontal and lateral views is essential during surgery. This allows for a comprehensive assessment of the fracture site, including the line of force, the cervical shaft angle, the anterior tilt angle, the alignment of the cortex, and the position of the screw. The use of hollow screw fixation in the treatment of femoral neck fractures has been shown to result in dynamic compression of the fracture end during weight bearing. However, this approach has also been associated with an increased risk of shortening the femoral neck (Figure 4).
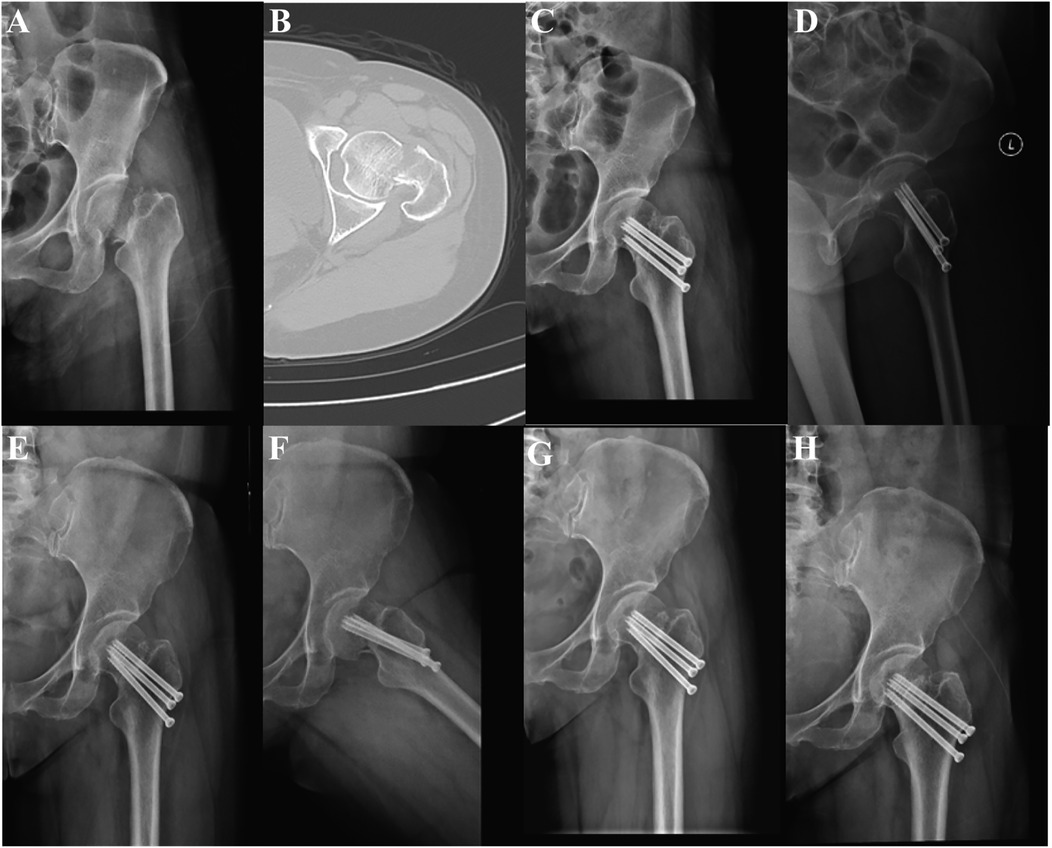
Figure 4. A 50-year-old female patient was admitted to the hospital for treatment of left hip pain and limited range of motion following a fall and underwent CCS treatment. (A,B) Pre-operative CT images of the patient showed a left femoral neck fracture, Garden type IV. (C,D) Review radiographs 1 day post-operatively in the anteroposterior and lateral positions showed good reduction. (E–H) Review radiographs at 12 and 18 months postoperatively showed femoral neck shortening.
According to the findings of previous studies, femoral neck shortening has been demonstrated to result in diminished gait velocity and to manifest as an impairment in gait symmetry and physical functioning (35). A multicenter cohort study by Zlowodzki et al. (36) further revealed the impact of femoral neck shortening on patients' postoperative quality of life. The study identified significant variations in EuroQol questionnaire scores and SF-36 physical function scores between patients with femoral neck shortening greater than 5 mm and those with shortening less than 5 mm. In a prospective multicenter study of hip fracture prognosis in China, researchers found that femoral neck shortening was significantly associated with poorer hip function in patients under 55 years of age (37). Notably, in that study, 35.7% of patients with femoral neck fractures treated with hollow nails experienced more than 5 mm of femoral neck shortening. A recent study found that the modified Harris Hip Score (mHHS) and Visual Analogue Score (VAS) were significantly lower in the femoral neck shortening group (≥5 mm) than in the no shortening group (38). Finite element analysis revealed that the stress distribution in the hip joint changed after the shortening of the femoral neck, and the stress distribution in the femoral head was not uniform (39, 40). When there is severe shortening of the femoral neck, the unevenness of load distribution is further exacerbated and hip mobility is significantly reduced, which may also lead to an increased probability of femoral head necrosis. The femoral neck is susceptible to postoperative shortening due to its anatomical and biomechanical characteristics. A correlation has been observed between shortening of the femoral neck and the onset of pain and decreased hip function, and this shortening may increase the long-term risk of osteonecrosis of the femoral head. In general, the femoral neck is prone to postoperative neck shortening due to its special anatomical structure and biomechanical properties, and there is a correlation between shortening of the femoral neck and the development of pain and decline in hip function. They may also increase the long-term risk of femoral head necrosis. The findings of our study demonstrated that the PFLP group exhibited a notable advantage over the CCS group with respect to the preservation of femoral neck length and postoperative Harris scores. This may be attributed to the enhanced mechanical stability and shear resistance of the PFLP plate screw locking structure (41). Furthermore, in our case, we found that although PFLP did not have the effect of CCS sliding compression, fracture healing could still be achieved with good repositioning and strong internal fixation, even if there was a gap at the fracture break (Figure 5).
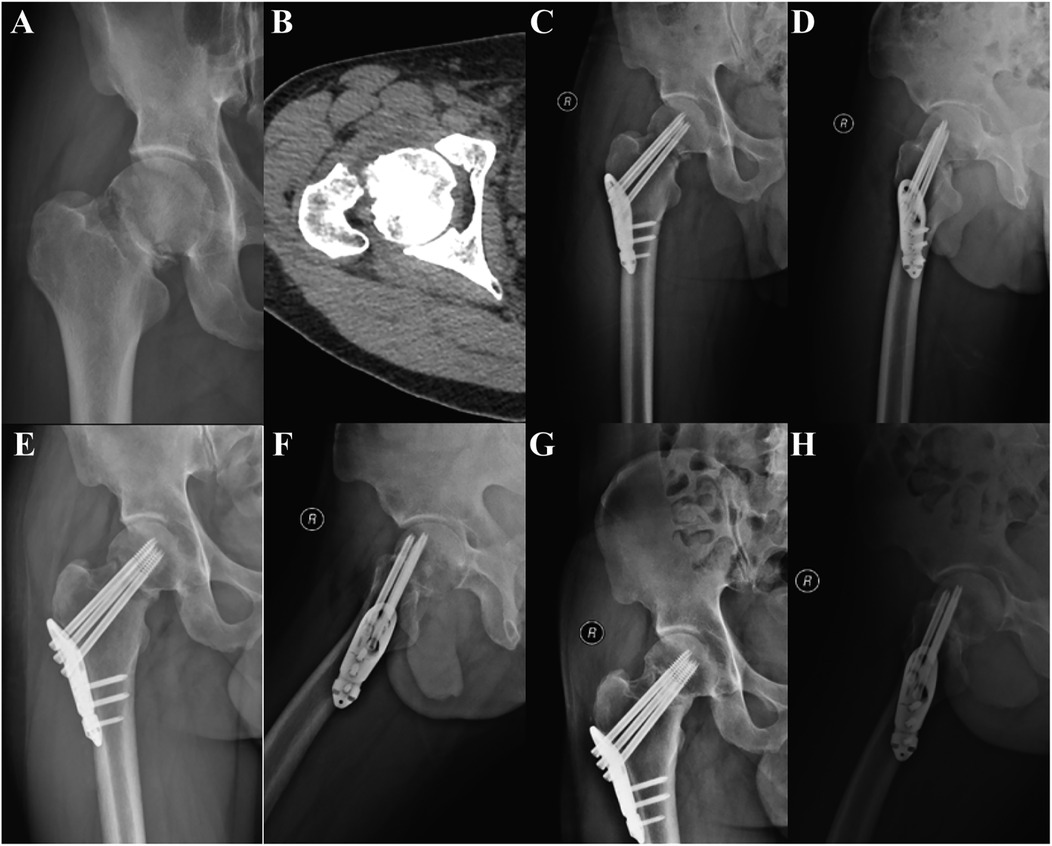
Figure 5. A 52-year-old male patient was admitted to the hospital for treatment of right hip pain and limited range of motion following a fall and underwent PFLP treatment. (A,B) Pre-operative CT images of the patient showed a right femoral neck fracture, Garden type IV. (C,D) Review radiographs 1 day post-operatively in the anteroposterior and lateral positions showed good reduction, but a gap was present at the fractured end. (E,F) Review radiographs 3 months post-operatively showed gradual fracture healing and a reduction in the fracture gap. (G,H) Review radiographs 6 months post-operatively showed disappearance of the gap and good fracture healing.
In this study, the PFLP group achieved relatively satisfactory treatment results. For middle-aged patients younger than 60 years and stable fracture patients between 60 and 75 years, PFLP can be an effective treatment for femoral neck fractures if they are in good physical condition, have a high activity level and a strong will to preserve the hip (9). Nevertheless, the practice of internal fixation of femoral neck fractures continues to present a number of significant challenges. First, internal fixation requires a long recovery period, and fracture nonunion and femoral head necrosis are always insurmountable obstacles. In addition, repeated nailing adjustments during surgery may exacerbate bone loss, especially in osteoporotic patients. Therefore, it is imperative that the treatment cycle and risk of secondary revision surgery be adequately considered when performing internal fixation of femoral neck fractures. When formulating an individualized treatment strategy, it is important to consider the patient's age, general condition, current mobility, and anticipated functional needs, as well as the indications for surgery. It is imperative to assess the immediate and long-term consequences of disparate treatment modalities on the patient in order to select the most suitable treatment approach and achieve the optimal outcome.
This study is a single-center retrospective cohort study with a low level of evidence in evidence-based medicine. As a result, there is a possibility of selection bias during the study. Furthermore, the sample size of this study is relatively small, the follow-up period is relatively brief, and the postoperative follow-up period may be insufficient to fully observe the occurrence of femoral head necrosis and other complications. It would be beneficial for future research to focus on conducting large prospective multicenter randomized controlled trials, which would allow for a more comprehensive and detailed evaluation of the efficacy of treatment modalities for femoral neck fractures.
In conclusion, both the PFLP and CCS groups achieved satisfactory efficacy in the treatment of femoral neck fractures. Compared with the CCS group, the PFLP group showed more significant advantages in fracture healing time, preservation of femoral neck length and restoration of hip function. Therefore, PFLP achieved satisfactory results in the treatment of femoral neck fractures and can be used as an effective internal fixation method for the treatment of femoral neck fractures.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Medical Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
XZ: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. DW: Data curation, Investigation, Writing – review & editing. JihX: Data curation, Investigation, Writing – review & editing. TX: Formal analysis, Writing – review & editing. HZ: Formal analysis, Writing – review & editing. JiaX: Project administration, Writing – review & editing. HF: Methodology, Writing – review & editing. HS: Methodology, Supervision, Writing – original draft, Writing – review & editing. LX: Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the National Natural Science Foundation of China (No. 82472437) and the Xianning City Science and Technology Program (No. 2023GCYF102).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
PFLP, proximal femoral locking plate; CCS, cannulated compression screws.
1. Zhang C, Feng J, Wang S, Gao P, Xu L, Zhu J, et al. Incidence of and trends in hip fracture among adults in urban China: a nationwide retrospective cohort study. PLoS Med. (2020) 17:e1003180. doi: 10.1371/journal.pmed.1003180
2. Walter N, Szymski D, Kurtz SM, Lowenberg DW, Alt V, Lau EC, et al. Epidemiology and treatment of proximal femoral fractures in the elderly U.S. population. Sci Rep. (2023) 13:12734. doi: 10.1038/s41598-023-40087-8
3. Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. (2018) 49:1458–60. doi: 10.1016/j.injury.2018.04.015
4. Thorngren K-G, Hommel A, Norrman PO, Thorngren J, Wingstrand H. Epidemiology of femoral neck fractures. Injury. (2002) 33(Suppl 3):C1–7. doi: 10.1016/S0020-1383(02)00324-8
5. Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. (2004) 15:897–902. doi: 10.1007/s00198-004-1627-0
6. Nijdam T, Schiepers T, Laane D, Schuijt HJ, van der Velde D, Smeeing D. The impact of implementation of palliative, non-operative management on mortality of operatively treated geriatric hip fracture patients: a retrospective cohort study. J Clin Med. (2024) 13:2012. doi: 10.3390/jcm13072012
7. Fernandez MA, Griffin XL, Costa ML. Management of hip fracture. Br Med Bull. (2015) 115:165–72. doi: 10.1093/bmb/ldv036
8. Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. (2017) 377:2053–62. doi: 10.1056/NEJMcp1611090
9. Xu D-F, Bi F-G, Ma C-Y, Wen Z-F, Cai X-Z. A systematic review of undisplaced femoral neck fracture treatments for patients over 65 years of age, with a focus on union rates and avascular necrosis. J Orthop Surg Res. (2017) 12:28. doi: 10.1186/s13018-017-0528-9
10. McDonough CM, Harris-Hayes M, Kristensen MT, Overgaard JA, Herring TB, Kenny AM, et al. Physical therapy management of older adults with hip fracture. J Orthop Sports Phys Ther. (2021) 51(2):CPG1–81. doi: 10.2519/jospt.2021.0301
11. Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management. J Orthop Trauma. (2015) 29:121–9. doi: 10.1097/BOT.0000000000000291
12. Overmann AL, Richards JT, O’Hara NN, D’Alleyrand JC, Slobogean GP. Outcomes of elderly patients with nondisplaced or minimally displaced femoral neck fractures treated with internal fixation: a systematic review and meta-analysis. Injury. (2019) 50:2158–66. doi: 10.1016/j.injury.2019.09.039
13. Rivera F, Comba LC, Colombo M, Benazzo F, Cavaliere P, Solarino G. Management of intracapsular hip fracture: current trends from a national survey. Injury. (2024) 55(Suppl 4):111539. doi: 10.1016/j.injury.2024.111539
14. Augat P, Bliven E, Hackl S. Biomechanics of femoral neck fractures and implications for fixation. J Orthop Trauma. (2019) 33(Suppl 1):S27–32. doi: 10.1097/BOT.0000000000001365
15. Zhang X, Zhang Y, Huang S, Qi X, Li W, Lv Y, et al. Biomechanical effects of FNS on femoral neck fractures based on different reduction quality: finite element analysis. BMC Musculoskelet Disord. (2024) 25:914. doi: 10.1186/s12891-024-08041-5
16. Samsami S, Augat P, Rouhi G. Stability of femoral neck fracture fixation: a finite element analysis. Proc Inst Mech Eng H. (2019) 233:892–900. doi: 10.1177/0954411919856138
17. Yuan D, Zhang Z, Wang X, Chang W, Xie W, Zhang Y. Efficacy of four internal fixation devices on femoral neck fractures in young adults: a systematic review and network meta-analysis. Medicine. (2024) 103:e40265. doi: 10.1097/MD.0000000000040265
18. Fan X, Zhou Y, Dai S, Lao K, Zhang Q, Yu T. Bio-mechanical effects of femoral neck system versus cannulated screws on treating young patients with Pauwels type III femoral neck fractures: a finite element analysis. BMC Musculoskelet Disord. (2024) 25:83. doi: 10.1186/s12891-023-07110-5
19. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. (1969) 51:737–55. doi: 10.2106/00004623-196951040-00012
20. Ye C-Y, Liu A, Xu M-Y, Nonso NS, He R-X. Arthroplasty versus internal fixation for displaced intracapsular femoral neck fracture in the elderly: systematic review and meta-analysis of short- and long-term effectiveness. Chin Med J (2016) 129:2630–8. doi: 10.4103/0366-6999.192788
21. Ramadanov N, Jóźwiak K, Hauptmann M, Lazaru P, Marinova-Kichikova P, Dimitrov D, et al. Cannulated screws versus dynamic hip screw versus hemiarthroplasty versus total hip arthroplasty in patients with displaced and non-displaced femoral neck fractures: a systematic review and frequentist network meta-analysis of 5703 patients. J Orthop Surg Res. (2023) 18:625. doi: 10.1186/s13018-023-04114-8
22. Liu Y, Chen X, Zhang P, Jiang B. Comparing total hip arthroplasty and hemiarthroplasty for the treatment of displaced femoral neck fracture in the active elderly over 75 years old: a systematic review and meta-analysis of randomized control trials. J Orthop Surg Res. (2020) 15:215. doi: 10.1186/s13018-020-01725-3
23. Lewis SR, Macey R, Stokes J, Cook JA, Eardley WG, Griffin XL. Surgical interventions for treating intracapsular hip fractures in older adults: a network meta-analysis. Cochrane Database Syst Rev. (2022) 2:CD013404. doi: 10.1002/14651858.CD013404.pub2
24. Jia X, Zhang K, Qiang M, Han Q, Zhao G, Wu Y, et al. Design of well-matched end-structure of anatomical proximal femoral locking plate based on computer-assisted imaging combined with 3D printing technology: a quality improvement study. Int J Surg. (2023) 109:1169–79. doi: 10.1097/JS9.0000000000000300
25. Saß M, Mittlmeier T. Joint-preserving treatment of medial femoral neck fractures with an angular stable implant. Oper Orthop Traumato. (2016) 28:291–308. doi: 10.1007/s00064-016-0443-y
26. Yin H, Pan Z, Jiang H. Is dynamic locking plate(targon FN) a better choice for treating of intracapsular hip fracture? A meta-analysis. Int J Surg. (2018) 52:30–4. doi: 10.1016/j.ijsu.2018.01.044
27. Yu X, Li Y-Z, Lu H-J, Liu B-L. Treatment of a femoral neck fracture combined with ipsilateral femoral head and intertrochanteric fractures: a case report. World J Orthop. (2024) 15:973. doi: 10.5312/wjo.v15.i10.973
28. Shu DP, Xiao YP, Bei MJ, Ji T, Peng YJ, Ma B, et al. Dynamic compression locking system versus multiple cannulated compression screw for the treatment of femoral neck fractures: a comparative study. BMC Musculoskelet Disord. (2020) 21:230. doi: 10.1186/s12891-020-03259-5
29. Lin D, Lian K, Ding Z, Zhai W, Hong J. Proximal femoral locking plate with cannulated screws for the treatment of femoral neck fractures. Orthopedics. (2012) 35:e1–5. doi: 10.3928/01477447-20111122-38
30. Alshameeri Z, Elbashir M, Parker MJ. The outcome of intracapsular hip fracture fixation using the Targon femoral neck (TFN) locking plate system or cannulated cancellous screws: a comparative study involving 2004 patients. Injury. (2017) 48:2555–62. doi: 10.1016/j.injury.2017.08.063
31. Haider S, Harris TJ, Turner AC, Podeszwa DA, Hartman CA, Morris WZ. Treatment of Delbet II/III pediatric femoral neck fractures with proximal femoral locking plate versus cannulated screws. J Pediatr Orthop. (2024) 44:213–20. doi: 10.1097/BPO.0000000000002625
32. Crump EK, Quacinella M, Deafenbaugh BK. Does screw location affect the risk of subtrochanteric femur fracture after femoral neck fixation? A biomechanical study. Clin Orthop. (2020) 478:770–6. doi: 10.1097/CORR.0000000000000945
33. Zhu X-Z, Wang W, Wu S-H, Mei J. Reoperation rate and implants’ position variation features of displaced femoral neck fractures with sliding compression or length-stable fixation in young and middle-aged population. BMC Musculoskelet Disord. (2022) 23:993. doi: 10.1186/s12891-022-05956-9
34. Krischak G, Beck A, Wachter N, Jakob R, Kinzl L, Suger G. Relevance of primary reduction for the clinical outcome of femoral neck fractures treated with cancellous screws. Arch Orthop Trauma Surg. (2003) 123:404–9. doi: 10.1007/s00402-003-0571-3
35. Zielinski SM, Keijsers NL, Praet SF, Heetveld MJ, Bhandari M, Wilssens JP, et al. Femoral neck shortening after internal fixation of a femoral neck fracture. Orthopedics. (2013) 36:e849–58. doi: 10.3928/01477447-20130624-13
36. Zlowodzki M, Brink O, Switzer J, Wingerter S, Woodall J Jr, Petrisor BA, et al. The effect of shortening and varus collapse of the femoral neck on function after fixation of intracapsular fracture of the hip: a multi-centre cohort study. J Bone Joint Surg Br. (2008) 90:1487–94. doi: 10.1302/0301-620X.90B11.20582
37. Slobogean GP, Stockton DJ, Zeng BF, Wang D, Ma B, Pollak AN. Femoral neck shortening in adult patients under the age of 55 years is associated with worse functional outcomes: analysis of the prospective multi-center study of hip fracture outcomes in China (SHOC). Injury. (2017) 48:1837–42. doi: 10.1016/j.injury.2017.06.013
38. Lee DH, Kwon JH, Kim K-C. The effects and risk factors of femoral neck shortening after internal fixation of femoral neck fractures. Clin Orthop Surg. (2024) 16:718–23. doi: 10.4055/cios24089
39. Li W-L, Yu X, Pang Q-J. The biomechanical effects of femoral neck shortening on femoral head and neck. Chin J Exp Surg. (2016) 36:378–84. doi: 10.3760/cma.j.issn.0253-2352.2016.06.008
40. Yu X, Zhang DF, Song MS, Chen ZM, Yang K, Pang QJ. Finite element analysis of evaluating the change of the hip joint biomechanics following femoral neck shortening after cannulated screw fixation for osteoporotic femoral neck fracture. Zhonghua Yi Xue Za Zhi. (2020) 100:2628–32. doi: 10.3760/cma.j.cn112137-20200219-00364
Keywords: hip fracture, femoral neck fracture, internal fixation, proximal femoral locking plate, cannulated compression screws
Citation: Zhou X, Wei D, Xiao J, Xia T, Zhou H, Xiang J, Fang H, Song H and Xiong L (2025) Comparison of clinical efficacy between proximal femoral locking plate and cannulated compression screws for femoral neck fracture. Front. Surg. 12:1546873. doi: 10.3389/fsurg.2025.1546873
Received: 17 December 2024; Accepted: 20 March 2025;
Published: 10 April 2025.
Edited by:
Wanbo Zhu, University of Wisconsin-Madison, United StatesReviewed by:
Domenico Fenga, University of Messina, ItalyCopyright: © 2025 Zhou, Wei, Xiao, Xia, Zhou, Xiang, Fang, Song and Xiong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Song, ZHJfc29uZ2hAMTYzLmNvbQ==; Liming Xiong, eGlvbmdsaW1pbmdAaHVzdC5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.