- Department of Orthopaedics, Xiantao First People’s Hospital, Xiantao, Hubei, China
Background: Peroneal artery injury following internal fixation of a calcaneal fracture is rare. The occurrence of a delayed pseudoaneurysm with an arteriovenous fistula after a peroneal artery injury is even rarer and has not been reported previously.
Case summary: Herein, we report the case of a 65-year-old female patient with a calcaneal fracture (Sanders Type ⅢAB) who underwent an open reduction and internal fixation surgery through the tarsal sinus approach. Two months postoperatively, she experienced left foot pain. Physical examination revealed pulsation at the surgical site and a positive Branham sign, which was suggestive of a delayed pseudoaneurysm. Emergency digital subtraction angiography (DSA) examination was performed, and this revealed a pseudoaneurysm and arteriovenous fistula at the distal end of the peroneal artery. Therefore, the patient underwent transcatheter coil embolization of the peroneal artery and had good postoperative outcomes.
Conclusion: Arterial injury should be suspected if massive hemorrhage occurs shortly after internal fixation for calcaneal fractures, and appropriate hemostatic measures should be promptly instituted. If unexplained pain and swelling develop along with a palpable pulse at the surgical site, a pseudoaneurysm should be suspected, and appropriate examinations should be promptly performed. Accurate diagnosis and prompt treatment are also crucial.
1 Introduction
Peroneal artery injury after internal fixation of a calcaneal fracture is an uncommon clinical entity. A delayed pseudoaneurysm with an arteriovenous fistula after a peroneal artery injury is even rarer (1).
The tarsal sinus incision for the treatment of calcaneal fractures is an important cause of peroneal artery end injury, the failure of hemostasis and the ongoing bleeding may lead to the formation of a pseudoaneurysm and an arteriovenous fistula (2).
Herein, we report the case of a patient who developed a pseudoaneurysm of the peroneal artery complicated by an arteriovenous fistula after surgical treatment of a calcaneal fracture through a tarsal sinus incision. In this report, we also discuss the causes and therapeutic options of this rare entity.
2 Case presentation
2.1 Clinical findings
A 65-year-old woman presented with a 3 h history of left foot pain due to a left calcaneal fracture secondary to a fall.
She had a history of hypertension that was diagnosed in February 2009 and was treated with nifedipine sustained-release tablets.
On physical examination, the patient's vital signs were as follows: Blood pressure, 185/110 mmHg. Furthermore, the patient had left foot swelling, tenderness, and heel varus deformity. She had no open wounds, no sensory or motor disorders, and good peripheral circulation.
Laboratory tests revealed the following: prothrombin activity, 59% (80%–100%); prothrombin time, 17.3 s(9.4–12.5 s); international normalized ratio, 1.40(0.85–1.15); partial thromboplastin time, 45.9 s(25.1–36.5 s), fibrinogen, 1.43 g/L(2–4 g/L); total bilirubin, 37.8 umol/L(0–24 umol/L); direct bilirubin, 15.9 umol/L(0–8 umol/L); albumin, 24.4 g/L(40–55 g/L); AST, 84 IU/L(15–40 IU/L); ALT, 75 IU/L(9–50 IU/L); and hepatitis C antibody, 682.07 s/co(0–1 s/co). No abnormalities were found on routine blood and urine tests. A radiograph of the patient's left foot revealed a clear fracture line on the left calcaneus with significant bone displacement of the posterior talocalcaneal joint (Figure 1).
2.2 Final diagnosis
After considering the patient's medical history and laboratory findings, the following diagnoses were made: left calcaneal fracture (Sanders type IIIAB), hepatitis C, abnormal coagulation function, impaired liver function, and third stage hypertension.
2.3 Treatment
As the calcaneal fracture classification was Sanders type IIIAB, we should restore the Böhler's angle (3). To get better outcoms, we prepared to treat it with ORIF (3). The patient underwent open reduction and internal fixation of the left calcaneal fracture through a tarsal sinus incision 11 days after being admitted when the foot swelling subsides. The fracture was adequately reduced and fixed, and a drainage tube was left in situ. The surgical incision was then sutured and dressed. One day postoperatively, the blood pressure was 170/105 mmHg, the drainage tube was removed, and pressure bandaging was continued. In the afternoon of the same day, the patient had a massive hemorrhage from the surgical site, which was controlled using pressure bandaging. The patient's hemoglobin level was decreased and her coagulation function was abnormal, as the hemorrhage had stopped, we didn't performed an additional investigation with echocolor Doppler or CT angiography, so that we failed to detect the injury of the peroneal artery in its early stage; therefore, she was transfused with packed red blood cells, fresh frozen plasma, and cryoprecipitate. Antiviral treatment for Hepatitis C was also administered. Although the surgical incision had healed 2 weeks postoperatively, a subcutaneous hematoma was still observed at the surgical site.
Two months after surgery, the patient still felt pain in her left foot and was admitted to the hospital. Physical examination revealed a palpable pulse at the surgical site and a positive Branham sign. Fresh blood was also aspirated through a puncture at the surgical site. Therefore, a pseudoaneurysm complicated by an arteriovenous fistula was suspected. Considering that DSA is the gold standard for the diagnosis of pseudoaneurysms, we performed the DSA examination directly. A Digital Subtraction Angiography (DSA) of the lower limb blood vessels revealed significant tortuosity at the distal end of the peroneal artery, rupture of the peroneal artery branches with a large amount of contrast agent spilling out and filling a sac-like structure on the lateral side of the left calcaneus, and numerous arteriovenous fistulas around it, with both ends of the carrying artery supplying blood. This confirmed the formation of a peroneal artery pseudoaneurysm complicated by an arteriovenous fistula. The patient underwent transcatheter coil embolization of the peroneal artery and had good postoperative outcomes. The patient was discharged the following day (Figure 2).
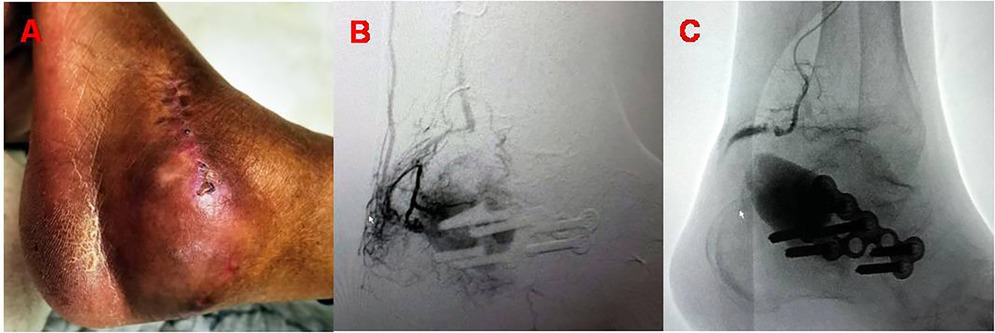
Figure 2. (A) Appearance of the left foot at the 2-month postoperative follow-up visit; (B) DSA imaging reveals features consistent with the formation of a peroneal artery pseudoaneurysm and arteriovenous fistula; (C) imaging after spring microcoil embolization of the peroneal artery pseudoaneurysm and arteriovenous fistula.
2.4 Outcome and follow-up
After 3 years of follow-up, the patient reported no pain, swelling, or subcutaneous pulsation in her left foot (Figure 3).
3 Discussion
Aneurysms are pathologically classified as real aneurysms, pseudoaneurysms, and dissecting aneurysms. Pseudoaneurysms are mostly caused by trauma, which can be iatrogenic or non-iatrogenic (4). When blood vessels are damaged, blood flows into the tissue spaces and forms a hematoma, which in turn develops a fibrous capsule wall and is formed into a pseudoaneurysm. Pseudoaneurysm accounts for approximately 1% of all aneurysms (5). Arteriovenous fistulas are abnormal rapid channels between arteries and veins, and can be caused by aneurysms, infections, and vascular injuries. Hence, arterial vessel injuries can lead to the formation of pseudoaneurysms and arteriovenous fistulas.
Several factors can lead to arterial injuries in orthopedic surgery, including direct puncture of the fracture block, intraoperative injury, puncture injury of the drainage tube, and improper placement of screws and other internal fixation devices. The peroneal artery is a branch of the posterior tibial artery that runs obliquely behind theupper part of the flexor hallucis longus muscle, descends between the posterior part of thefibula and the tibialis posterior muscle, and distally accompanies the sural nerve. The tarsal sinus approach is used for the management of calcaneal fractures. During the procedure, the surgical incision is extended from 1 cm below the tip of the lateral malleolus to the distal 4th metatarsal, which is not generally associated with damage to the peroneal artery. However, because the steel plate is placed at the distal end, the incision needs to be extended to the Achilles tendon, which increases the risk of peroneal artery injury. Additionally, during the operation, the surface of the calcaneus needs to be sharply separated using a surgical blade; however, it cannot be separated under direct vision, which increases the possibility of peroneal artery injury. Based on the above factors, the treatment of calcaneal fractures using a tarsal sinus incision is an important cause of peroneal artery end injury. The peroneal artery thins into an arteriole, especially at its terminal part; hence, the blood pressure at this part is not high. After injury, a thrombus forms in the blood vessel to stop bleeding through local compression (6, 7). On the first day after the operation, the patient had a massive hemorrhage from the surgical site, which was controlled using pressure bandaging. The surgical incision healed at a later time. However, the peroneal artery did not thrombose and continued to bleed, resulting in a pseudoaneurysm. This was likely caused by the patient's poor coagulation function and high blood pressure. Due to our failure to detect the pseudoaneurysm in a timely manner, it led to the formation of an arteriovenous fistula.
After an arterial wall injury, a pseudoaneurysm can develop within hours to months (6, 8). The clinical manifestations of delayed pseudoaneurysms are limb pain, swelling, and progressive anemia (6, 7, 9). Physical examination can reveal a local mass, tenderness, and pulsation under the skin. When an arteriovenous fistula is formed, local tremor can be palpated at the site, and a rough, persistent, vascular murmur can be heard on auscultation along with a positive Branham sign. Imaging examinations should be performed when a pseudoaneurysm is suspected (10, 11). DSA is the gold standard for the diagnosis of pseudoaneurysms, as it can clarify the relationship between an artery and an aneurysm, and also reveal the hemodynamic features of the pathologies, while providing the basis for making appropriate treatment plans. Currently, the commonly used treatment methods for arteriovenous fistulas are thrombin injection under ultrasound guidance, transcatheter coil embolization under DSA, catheter embolization and surgical treatment (12–14). The patient in this report was treated with transcatheter coil embolization under DSA, as it was considered that DSA is more minimally invasive. and it had satisfactory postoperative outcomes.
4 Conclusion
The findings of this case report and a brief literature review suggest that a delayed pseudoaneurysm of the peroneal artery complicated by an arteriovenous fistula after calcaneal fracture is a very rare surgical complication that can be caused by iatrogenic injury and other comorbidities such as hypertension and coagulopathies. Therefore, adequate preparations should be made preoperatively, while identifying and promptly managing the patient's comorbidities. Surgeons should also be familiar with the relevant anatomy of the foot and operate carefully to avoid damaging the peroneal artery. And we can look for less traumatic techniques, including closed reduction, external fixation, and percutaneous surgery (PS), in order to reduce complication rate (15). If a vascular injury occurs postoperatively, it should be examined and treated promptly. Using these measures, the incidence of iatrogenic pseudoaneurysms complicated by arteriovenous fistulas can be reduced, and additional injury to patients can be avoided.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
Y-LL: Writing – original draft. SC: Supervision, Writing – original draft. YA: Formal Analysis, Validation, Writing – review & editing. WZ: Investigation, Writing – original draft. J-CL: Conceptualization, Data curation, Supervision, Writing – review & editing, Formal Analysis. Y-FY: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors wish to thank the patient and the hospital.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ching KC, McCluskey KM, Srinivasan A. Peroneal arteriovenous fistula and pseudoaneurysm: an unusual presentation. Case Rep Vasc Med. (2014) 2014:506067. doi: 10.1155/2014/506067
2. Femino JE, Vaseenon T, Levin DA, Yian EH. Modification of the sinus tarsi approach for open reduction and plate fixation of intra-articular calcaneus fractures: the limits of proximal extension based upon the vascular anatomy of the lateral calcaneal artery. Iowa Orthop J. (2010) 30:161–7.21045990
3. Biz C, Refolo M, Zinnarello FD, Crimì A, Dante F, Ruggieri P. A historical review of calcaneal fractures: from the crucifixion of Jesus Christ and Don Juan injuries to the current plate osteosynthesis. Int Orthop. (2022) 46(6):1413–22. doi: 10.1007/s00264-022-05384-3
4. Punnam SR, Hadid T, Franklin PB, Gandhi DB, Abela GS, Shah DO, et al. Shaft aneurysm of femoropopliteal expanded polytetrafluoroethylene graft treated with a covered stent. Vasc Endovasc Surg. (2008) 42(4):386–90. doi: 10.1177/1538574408315207
5. Naser ZJ, Aukerman W, Tretter J, Morrissey S. Traumatic superficial temporal artery pseudoaneurysm & management following mandible fracture. Trauma Case Rep. (2023) 43:100753. doi: 10.1016/j.tcr.2023.100753
6. Sharma G, Singh R, Kumar A, Sharma V, Farooque K. Acute femoral artery pseudoaneurysm due to lesser trochanter fragment: an unusual complication of an intertrochanteric fracture. Chin J Traumatol. (2013) 16(5):301–3. doi: 10.3760/cma.j.issn.1008-1275.2013.05.011
7. Murphy PG, Geoghegan JG, Austin O, More-O'Ferrall R, Quinlan WR, Keaveny TV. Pseudoaneurysm of the profunda femoris artery due to intertrochanteric fracture of the hip. Arch Orthop Trauma Surg. (1999) 119(1–2):117–8. doi: 10.1007/s004020050372
8. Butterworth JW, Butterworth WA, Wu R. Three-year delayed presentation of femoral pseudoaneurysm after penetrating limb trauma. Ann Vasc Surg. (2015) 29(2):362.e11–5. doi: 10.1016/j.avsg.2014.09.019
9. Ryzewicz M, Robinson M, McConnell J, Lindeque B. Vascular injury during fixation of an intertrochanteric hip fracture in a patient with severe atherosclerosis: acase report. J Bone Joint Surg Am. (2006) 88(11):2483–6. doi: 10.2106/JBJS.F.00389
10. Singh S, Arora S, Thora A, Mohan R, Sural S, Dhal A. Pseudoaneurysm of profunda femoris artery following dynamic hip screw fixation for intertrochanteric femoral fracture. Chin J Traumatol. (2013) 16(4):233–6. doi: 10.3760/cma.j.issn.1008-1275.2013.04.010
11. Kim JW, Lee JI, Park KC. Pseudoaneurysm of the deep femoral artery caused by a guide wire following femur intertrochanteric fracture with a hip nail: acase report. Acta Orthop Traumatol Turc. (2017) 51(3):266–9. doi: 10.1016/j.aott.2017.03.011
12. Behera C, Naagar S, Krishna K, Taraporewalla DR, Garudadhri GV, Prasad K. Sudden death due to ruptured pseudoaneurysm of femoral artery in injected drug abusers - report of four cases at autopsy and review of literature. J Forensic Leg Med. (2014) 22:107–11. doi: 10.1016/j.jflm.2013.12.010
13. Craviari C, Taggart NW, Cetta F, Hagler DJ, Bower TC, Mauriello DA, et al. Percutaneous treatment of a complex saccular aortic pseudoaneurysm with covered stenting after subclavian artery translocation. JACC Cardiovasc Interv. (2014) 7(3):e23–4. doi: 10.1016/j.jcin.2013.07.017
14. Barquet A, Gelink A, Giannoudis PV. Proximal femoral fractures and vascular injuries in adults: incidence, aetiology and outcomes. Injury. (2015) 46(12):2297–313. doi: 10.1016/j.injury.2015.10.021
15. Biz C, Barison E, Ruggieri P, Iacobellis C. Radiographic and functional outcomes after displaced intra-articular calcaneal fractures: a comparative cohort study among the traditional open technique (ORIF) and percutaneous surgical procedures (PS). J Orthop Surg Res. (2016) 11(1):92. doi: 10.1186/s13018-016-0426-6
Keywords: peroneal artery, delayed pseudoaneurysm, arteriovenous fistula, calcaneal fracture, arterial injury, case report, tarsal sinus incision
Citation: Li Y-L, Chen S, Ai Y, Zhang W, Liu J-C and Yang Y-F (2025) Peroneal artery pseudoaneurysm with arteriovenous fistula after calcaneal fracture surgery: a case report. Front. Surg. 12:1527992. doi: 10.3389/fsurg.2025.1527992
Received: 14 November 2024; Accepted: 3 February 2025;
Published: 17 February 2025.
Edited by:
Pasqualino Sirignano, Sapienza University of Rome, ItalyReviewed by:
Carlo Biz, University of Padua, ItalyFederica Ruggiero, Sapienza University of Rome, Italy
Copyright: © 2025 Li, Chen, Ai, Zhang, Liu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ya-Fan Yang, NDkyNTIwMDkyQHFxLmNvbQ==
 Yu-Long Li
Yu-Long Li Sheng Chen
Sheng Chen
