
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 19 March 2025
Sec. Orthopedic Surgery
Volume 12 - 2025 | https://doi.org/10.3389/fsurg.2025.1521271
Background: Gas-containing pseudocyst is an uncommon cause of lumbar radiculopathy and most lumbar gas-containing pseudocysts locate in the spinal canal. While, extraforaminal gas-containing pseudocysts are very rare. Here, we reported a case of extraforaminal gas-containing pseudocyst, which compressed L4 exiting nerve root and caused lumbar radiculopathy.
Case presentation: A 62-year-old female presented with low back pain and radiation to anteromedial aspect of right thigh and anterior aspect of right calf. Computed tomography and magnetic resonance imaging of lumbar spine showed a gas-containing pseudocyst compressing in L4 exiting nerve root right extraforaminal area at L4–5 level. L4 exiting nerve root blocking was performed to confirm the responsible level. Then we performed BESS through a paraspinal approach to remove the gas-containing pseudocyst and release L4 exiting nerve root. Postoperatively, the patient achieved a good outcome and the pain was relieved.
Conclusions: Lumbar gas-containing pseudocyst in extraforaminal area is rare and can cause lumbar radiculopathy. Paraspinal approach BESS is an alternative method to treat extraforaminal gas-containing pseudocyst and can provide good outcome.
Epidural gas-containing pseudocysts (GCPs) are uncommon causes of lumbar radiculopathy and it has been reported that GCPs are often associated with the intervertebral vacuum phenomenon (1–3). Most lumbar GCPs locate in the spinal canal and coexist with a disk fragment (4, 5). While the extraforaminal GCPs causing nerve root compression are extremely rare (3–5).
The treatment of lumbar GCPs including conservative management, percutaneous needle aspiration, percutaneous endoscopy and open surgery (6, 7). As a new endoscopic technique, unilateral biportal endoscopic spinal surgery (BESS) increases surgical movement of instruments with the independent visualization and working portals, provides good and wide field of visualization to unrestricted access contralateral and foraminal and extraforaminal areas (3). BESS has been applied to treat lumbar disc herniation and lumbar spinal stenosis (4). In this report, we present a symptomatic extraforaminal GCP, which was removed by BESS.
A 62-year-old female presented with low back pain and radiation to anteromedial aspect of right thigh and anterior aspect of right calf. The VAS score was 6 and the pain had persisted for 3 months. Physical examination revealed a positive straight leg raising (SLR) sign and lasegue test on the right side. Magnetic resonance imaging (MRI) and computed tomography (CT) of lumbar spine showed a right extraforaminal GCP in L4–5 level, which compressing L4 exiting nerve root (Figure 1).

Figure 1. Right extraforaminal GCP of L4–5 was shown in MRI and CT. (A) MRI axial views of L4–5; (B) MRI sagittal view of L4–5; (C) CT axial views of L4–5; (D) CT sagittal view of L4–5. Red arrow indicated the extraforaminal GCP.
Before BESS, we performed L4 exiting nerve root blocking in the extraforaminal area. The patient reported obvious pain relief after this blocking, which indicated that the responsible level was L4/5, and the target was the right extraforaminal GCP in L4–5 level.
We performed BESS through a paraspinal approach. The patient was placed in prone position on a radiolucent table and under general anesthesia. After the target level was confirmed under fluoroscopic guidance, the skin entry point was 1.5 cm above and 1.5 cm below the inferior margin of L4 pedicle, and 2 cm lateral to external margin of L4 pedicle (Figure 2). Two portals (walking portal and viewing portal) were created according to the skin entry point.
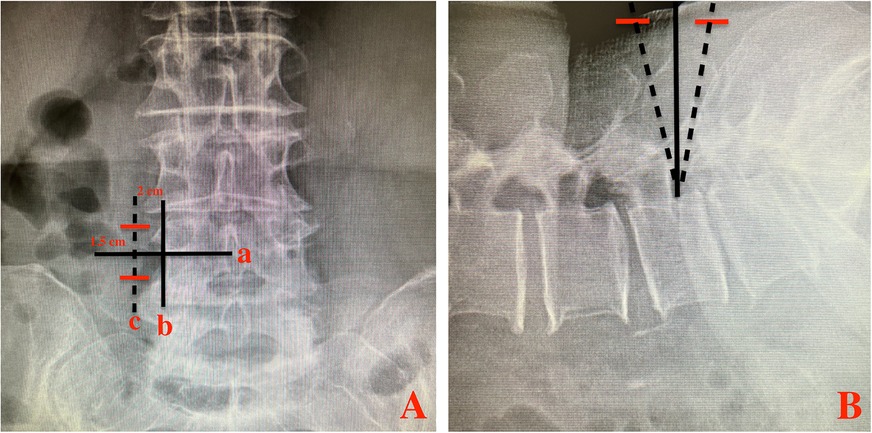
Figure 2. Two transverse skin incisions (red lines) made on the fluoroscopic AP (A) and lateral (B) views. line a: inferior margin of L4 pedicle; line b: external margin of L4 pedicle; line c: parallel line of b; Red line: skin incision.
Serial dilators were used to dissect the back muscle and acquire operative space. The trocar of the scope was introduced into the viewing portal and a round, smooth periosteal elevator was inserted into the working portal. After triangulation occurs between scope and the periosteal elevator, minor bleeding was controlled and remnant soft tissues were removed by radiofrequency probe and shaver, to expose L5 superior articular process, L4 inferior articular process, L4 pedicle isthmus and the base of L4 transverse. Then, part of L4 transverse and pedicle isthmus, the tip of L5 superior articular process and the exterior part of L4 inferior articular process were removed with a 3 mm drill or arthroscopic burr and Kerrison punch (Figure 3). After that, the ligament flavum in foramen was exposed and flavectomy was performed. Maneuvering of the scope, extraforaminal GCP, exiting nerve root and foramen would be directly visualized (Figure 3). Through the working portal, pituitary forceps were used to remove the extraforaminal GCP, and the L4 exiting nerve root was successfully decompressed (Figure 3). The successful removal of extraforaminal GCP was confirmed on postoperative MRI and CT (Figure 4). A bone tunnel could be seen on a CT scan (Figure 4). The patient achieved a good outcome, VAS score improved to 3 on the first postoperative day, and improved to 1 on 7 days after operation.
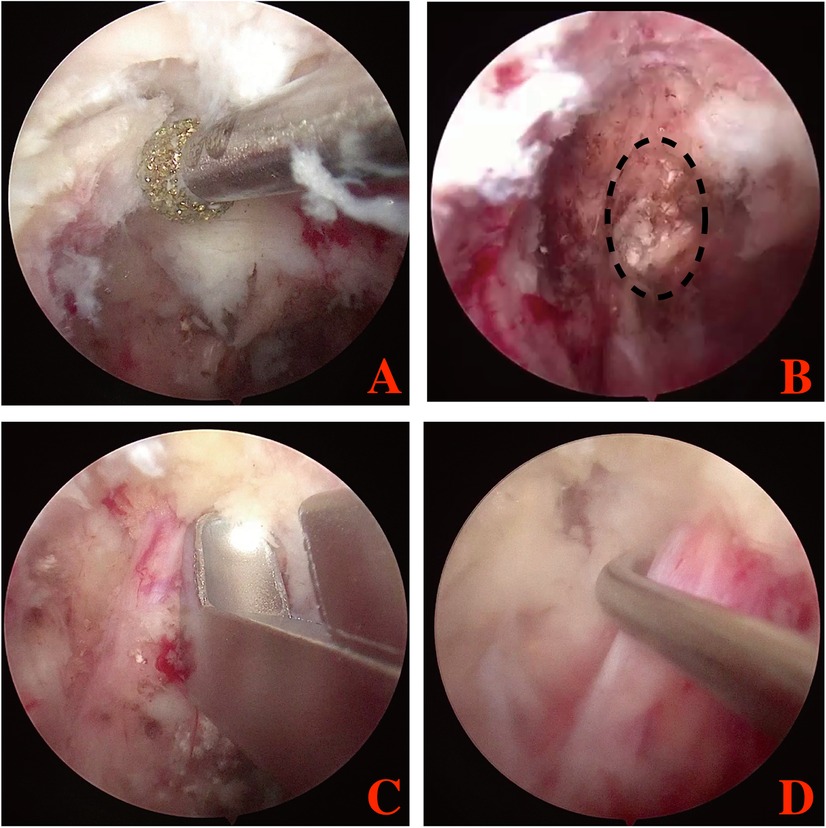
Figure 3. Endoscopic image during the BESS procedure. (A) the extraforaminal area was exposed; (B) extraforaminal GCP was exposed and removed; (C,D) L4 exiting nerve root were exposed and released. Black dotting circle: the extraforaminal GCP.

Figure 4. The extraforaminal area was shown in postoperative MRI and CT. (A) MRI axial views of L4–5; (B) MRI sagittal view of L4–5; (C) CT axial views of L4–5; (D) CT sagittal view of L4–5. Red arrow indicated the L4 exiting nerve root.
In the spine, the presence of gas or vacuum phenomenon is a relatively common radiological finding, and generally occurs in the intervertebral disc spaces (8). Compared with intervertebral gas, epidural GCP is much rare (7). Kuh et al. assessed the reported that 48.0% epidural GCP were found in the canal, 32.0% were found in the foramen, and 20.0% were found in extraforaminal area (9). We reviewed the articles about epidural GCPs, and found that 20 articles reported 43 cases of epidural GCPs (Table 1). Among them, only 9 cases (20.9%) of epidural GCPs located in extraforaminal area (4, 6, 9).
In those reported cases, most epidural GCPs were found because of neurological symptoms, such as sciatica, lower extremity paresthesia and paralysis (6). The clinical features are very similar to common lumbar disc herniation. So CT and MRI are very helpful to diagnose and assess the epidural GCPs. Epidural GCPs can be identified with density from - 200 to - 900 Hounsfield units in CT scan (10), or with low signal on T1- and T2-weighted images of MRI (9). Sometimes, calcification has the same low signal intensity in MRI, making it difficult to distinguish between gas and calcification. So CT scan is the most useful radiological method for identifying epidural GCPs.
There are various therapeutic strategies to treat symptomatic epidural GCPs, including medications, percutaneous needle aspiration, surgical removal (endoscopic spinal surgery or open surgery) (5). The conservative management (such as medications and rest) and percutaneous needle aspiration are common treatments for epidural GCPs, especially for those patients with surgery contraindication. However, some authors reported that epidural GCPs recurred with a relapse of the radicular syndrome after conservative management or percutaneous needle aspiration (11, 12). Open surgery has good clinical outcomes by totally removing the epidural GCPs and herniated disk fragment. However, open surgery has large operative injury, as its protocol includes discectomy, decompressive laminectomy facetectomy and interbody fusion. So open surgery may be more suitable for those patients with concomitant spinal stenosis or segmental instability (9). Compared with open surgery, endoscopic spinal surgery has many surgical advantages, including less invasive procedure, faster postoperative recovery and lower cost (9). So for those patients without severe spinal stenosis or segmental instability, endoscopic spinal surgery may be a better choice. Percutaneous endoscopic surgery (interlaminar approach or transforaminal approach) is the most classical minimally invasive surgery for lumbar degenerative diseases. In classical percutaneous endoscopic surgery, a single portal was used, with multiple channels for irrigation, instrumentation, visualization, and a light source. So the single portal limited the motion of the instruments and obscures visualization of the operating field. Compared with classical percutaneous endoscopic surgery, BESS increases surgical movement of instruments with the independent visualization and working portals, provides good and wide field of visualization to unrestricted access contralateral and foraminal areas (13). So for those epidural GCPs located in lateral recess, foraminal or extraforaminal areas, BESS may be a better choice. In this case, we successfully removed extraforaminal gas-containing pseudocyst using BESS, and completely relieved the radiating pain.
Lumbar GCPs in extraforaminal area is rare and can cause lumbar radiculopathy. Paraspinal approach BESS is an alternative method to treat extraforaminal gas-containing pseudocyst and can provide good outcome.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by The study was approved by the Tongde Hospital of Zhejiang Province [Approval number: 2022-091(K)] and the study protocols followed the Ethical Guidelines of the Declaration of Helsinki. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Y-wZ: Writing – original draft, Data curation, Formal Analysis, Resources. BX: Conceptualization, Investigation, Methodology, Writing – original draft. X-kW: Funding acquisition, Resources, Writing – review & editing. A-tZ: Funding acquisition, Investigation, Writing – review & editing.
The author(s) declare that financial support was received for the research and/or publication of this article. This work is supported by The Zhejiang Provincial Natural Science Foundation (LQ22H060003) and Chinese Medicine Research Program of Zhejiang Province (CN) (2024ZF042).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declare that no Generative AI was used in the creation of this manuscript.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Krishnan P. Epidural gas pseudocyst: an uncommon cause of sciatica. Asian J Neurosurg. (2022) 17(2):396–8. doi: 10.1055/s-0042-1750809
2. Kim HS, Kim HS, Kim SW, Shin H. Sudden foot drop caused by foraminal gas pseudocyst. J Korean Neurosurg Soc. (2011) 49(6):384–6. doi: 10.3340/jkns.2011.49.6.384
3. Seo HY, Yim JH, Chung JY. Severe radiating pain caused by extraforaminal gas-containing pseudocyst. J Orthop Sci. (2014) 19(3):507–10. doi: 10.1007/s00776-012-0313-x
4. Pak KI, Hoffman DC, Lutz HGE. Percutaneous intradiscal aspiration of a lumbar vacuum disc herniation: a case report. HSS J. (2011) 7(1):89–93. doi: 10.1007/s11420-010-9168-x
5. An JW, Lee CW. Surgical treatment of extra-foraminal gas containing pseudocyst compressing L5 nerve root by using unilateral biportal endosopy: a case report. World Neurosurg. (2019) 124:145–50. doi: 10.1016/j.wneu.2018.12.186
6. Lassoued Ferjani H, Ben Ammar L, Kaffel D, Maatallah K, Triki W, Ben Nessib D, et al. Radiculopathies caused by spontaneous pneumorrachis: two case reports and review of literature. Clin Case Rep. (2021) 9(11):e05061. doi: 10.1002/ccr3.5061
7. Zhu B, Jiang L, Liu XG. Transforaminal endoscopic decompression for a giant epidural gas-containing pseudocyst: a case report and literature review. Pain Physician. (2017) 20(3):E445–9.28339445
8. Kang SS, Kim MS, Ko KM, Park JC, Hong SJ, Yoon YJ, et al. Symptomatic epidural gas cyst treated with epidural block and percutaneous needle aspiration-a case report. Korean J Anesthesiol. (2012) 62(4):379–81. doi: 10.4097/kjae.2012.62.4.379
9. Kuh SU, Heo DH, Kim KS, Cho YJ. Lumbar epidural gas-containing pseudocysts as a cause of severe radicular pain. Joint Bone Spine Rev Rhumatisme. (2011) 78(4):398–401. doi: 10.1016/j.jbspin.2010.10.006
10. Belfquih H, El Mostarchid B, Akhaddar A, gazzaz M, Boucetta M. Sciatica caused by lumbar epidural gas. Pan African Medical Journal. (2014) 18:162. doi: 10.11604/pamj.2014.18.162.1354
11. Bosser V, Dietemann JL, Warter JM, Granel de, Solignac M, Beaujeux R, Buchheit F. L5 radicular pain related to lumbar extradural gas-containing pseudocyst. Role of CT-guided aspiration. Neuroradiology. (1990) 31(6):552–3. doi: 10.1007/bf00340142
12. Hu D, Xu K, Xiao S. Lumbar radiculopathy caused by epidural gas collection. Case Rep Orthop. (2022) 2022:8338131. doi: 10.1155/2022/8338131
13. Choi KC, Shim HK, Hwang JS, Shin SH, Lee DC, Jung HH, et al. Comparison of surgical invasiveness between microdiscectomy and 3 different endoscopic discectomy techniques for lumbar disc herniation. World Neurosurg. (2018) 116:e750–8. doi: 10.1016/j.wneu.2018.05.085
14. Lin RM, Wey KL, Tzeng CC. Gas-containing “ganglion” cyst of lumbar posterior longitudinal ligament at L3. Spine. (1994) 18(16):2528–32. doi: 10.1097/00007632-199312000-00026
15. Rajhi H, Morvan G, Hmaied E, Heissler P. Traitement percutané d'un pseudo-kyste gazeux épidural: cause rare de sciatique. J Radiol. (2005) 86(2):164–6. doi: 10.1016/S0221-0363(05)81337-X
16. Lee DY, Lee SH. L2 radicular compression caused by a foraminal extradural gas pseudocyst. J Korean Neurosurg Soc. (2010) 47(3):232–4. doi: 10.3340/jkns.2010.47.3.232
17. Yasuoka H, Nemoto O, Kawaguti M, Naitou S, Yamamoto K, Ukegawa Y. An unusual case of nerve root compression by intradiscal gas pseudocyst of the lumbar spine. J R Army Med Corps. (2010) 156(1):47–8. doi: 10.1136/jramc-156-01-11
18. Vaquero J, Parajon A. Lumbar radiculopathy due to gas-containing pseudocyst. J Rheumatol. (2011) 38(10):2264. doi: 10.3899/jrheum.110564
19. Yun SM, Suh BS, Park JS. Symptomatic epidural gas-containing cyst from intervertebral vacuum phenomenon. Korean J Spine. (2012) 9(4):365–8. doi: 10.14245/kjs.2012.9.4.365
20. Beltagi AHE, Swamy N, Dashti F. Vacuum epidural cyst with acute neurological presentation. A case report. Neuroradiol J. (2013) 26(2):213–7. doi: 10.1177/197140091302600212
Keywords: gas-containing pseudocys, extraforaminal area, unilateral biportal endoscopic spinal surgery, case report, literature review
Citation: Zhang Y-w, Xu B, Wang X-k and Zheng A-t (2025) Symptomatic extraforaminal gas-containing pseudocyst treated with unilateral biportal endoscopic spinal surgery: a case report and literature review. Front. Surg. 12:1521271. doi: 10.3389/fsurg.2025.1521271
Received: 1 November 2024; Accepted: 25 February 2025;
Published: 19 March 2025.
Edited by:
Nikolaos CH. Syrmos, Aristotle University of Thessaloniki, GreeceReviewed by:
Sherwan Hamawandi, Hawler Medical University, IraqCopyright: © 2025 Zhang, Xu, Wang and Zheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xu-ke Wang, d2FuZ3h1a2UyMDAyQDE2My5jb20=; Ao-te Zheng, YW90ZTE5OTJAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.