- Department of Vascular Surgery, Tianjin First Central Hospital, Tianjin, China
Persistent sciatic artery (PSA) is a rare anatomic variant disease with an incidence of approximately 0.025%–0.05% it is considered to be an axial congenital vascular malformation, which may be related to the failure of sciatic artery degeneration and iliofemoral artery dysplasia. Some patients may be asymptomatic, while others experience chronic pain, thrombosis, and aneurysm formation. We report the case of a 63-year-old female patient with a superficial femoralartery (SFA)-common femoral vein (CFV) arteriovenous fistula found on ultrasound of the lower extremities due to soreness and numbness of the lower limbs. Interventional surgery and computed tomography were performed to close the internal fistulas and detect the PSA. A coated stent graft was inserted to close the arteriovenous fistula. After 1-mongth follow-up, lower limb discomfort disappeared, and she was administered symptomatic treatment with anticoagulation and swelling reduction medication. Six months after surgery, computed tomography indicated the disappearance of internal fistula and good PSA progression. Lower extremity symptoms were considered to be related to the femoral arteriovenous fistula; therefore, no intervention was performed for the PSA, we only provided health education, such as reducing sedentary and right lying to prevent vascular lesions.
Introduction
The sciatic artery originates from the umbilical artery and is the main source of blood supply to the lower extremities during embryonic development. The sciatic arteries eventually recede, leaving behind remnants that persist as the popliteal and peroneal arteries. Prior to sciatic artery degeneration, the popliteal and peroneal arteries establish continuity with the superficial femoral artery (1, 2). If degeneration fails, it formed a persistent sciatic artery (PSA), which is a direct continuation of the internal iliac artery and may cause serious complications, such as chronic pain, thrombosis, and aneurysm formation. It is a rare anatomical variant with an incidence of approximately 0.025%–0.05% (3). Cases of PSA combined with arteriovenous fistula are very rare in the literature retrieved so far.
Case report
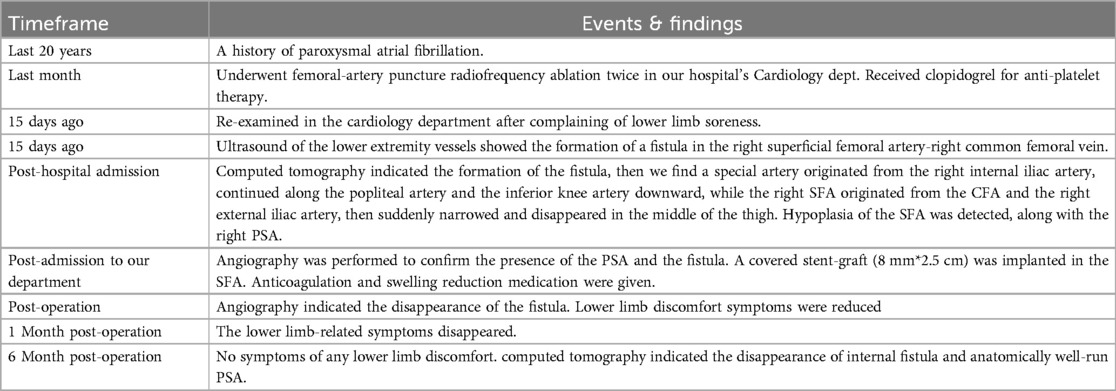
The patient was a 63-year-old woman with a history of paroxysmal atrial fibrillation for 20 years, who had undergone radiofrequency ablation surgery via femoral artery puncture twice in the Department of Cardiology of our hospital, and had been diagnosed with hypertension 1 month prior. Clopidogrel was administered for antiplatelet treatment. Fifteen days prior, she was re-examined in the cardiology department after complaining of a feeling of heaviness and soreness in the lower extremities with mild swelling. Ultrasound of the lower limb blood vessels revealed a femoral arteriovenous fistula, due to which she was admitted to our department (Table 1).
Physical examination revealed that the patient had a well-developed, symmetrical, and normal gait. The bilateral femoral, popliteal, dorsal, and posterior tibial artery pulses were palpable, and the right femoral artery showed a palpable bruit. The skin of both lower limbs was warm; the colour, muscle strength, sensation, and movement of both lower limbs were normal; there was no oedema; and no abnormalities were observed on neurological examination.
Laboratory tests after admission (routine blood tests, biochemistry, blood coagulation function) did not reveal any obvious abnormalities. Ultrasound of the lower extremity vessels showed the formation of a fistula in the right superficial femoral artery-right common femoral vein.
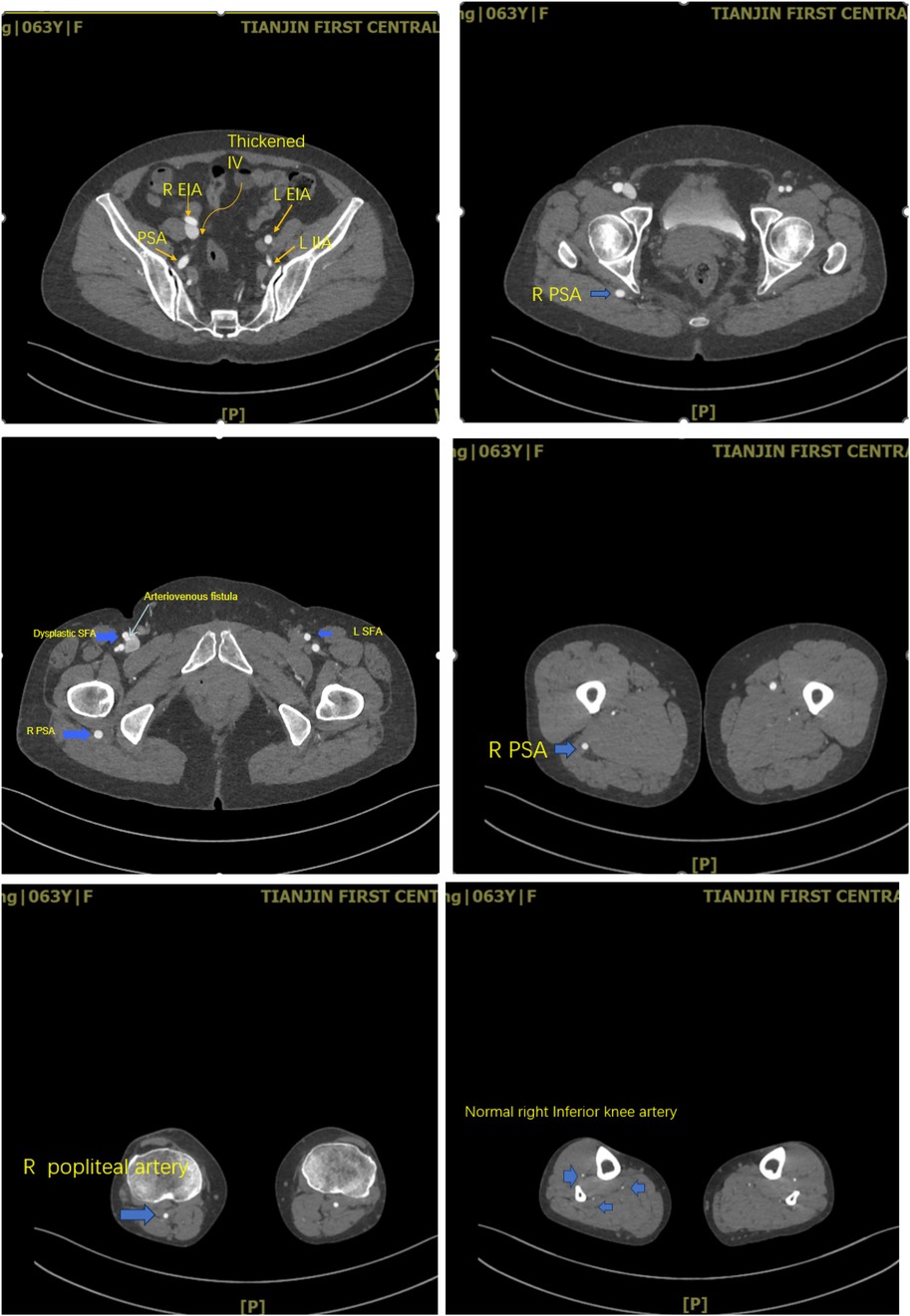
After being admitted to the hospital, Computed tomography angiography of the lower limbs confirmed the formation of the right superficial femoral artery-right common femoral venous fistula. Hypoplasia of the right SFA was detected, along with the right PSA (Figures 1, 2). The PSA originated from the right internal iliac artery, continued along the popliteal artery and the inferior knee artery downward, while the right SFA originated from the right CFA and external iliac artery, and suddenly narrowed and disappeared in the middle of the thigh.

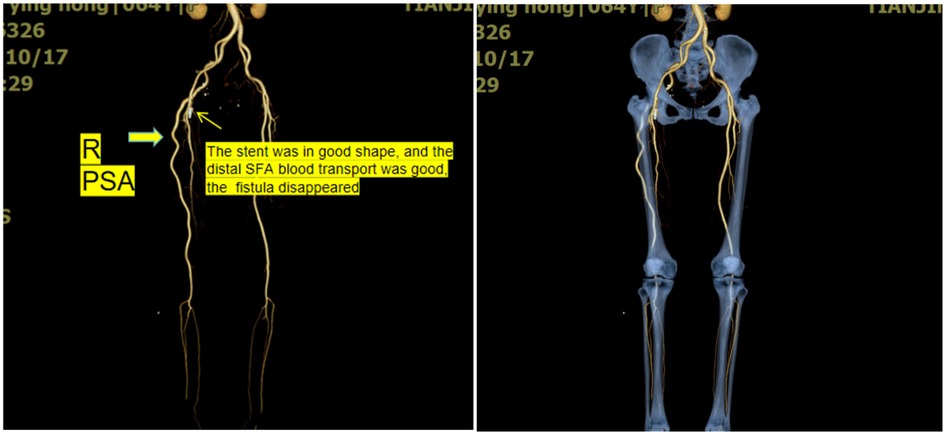
Figure 1. Three-dimensional reconstruction of the lower extremity arteries. The arrow in the diagram indicates the persistent sciatic artery.
Angiography was performed to confirm the presence of PSA (Figure 3). Due to the history of recent interventional surgery, the internal fistulae was considered iatrogenic. Considering that the patient's lower limb symptoms were related to arteriovenous fistula while not related to PSA, we closed the right arteriovenous fistula by implanting a covered stent-graft (8 mm*2.5 cm) in the superficial femora. Postoperative angiography revealed the disappearance of the arteriovenous fistula. The patient was advised to avoid sitting for a long time, and was administered symptomatic treatment with anticoagulation and swelling reduction medication. She was advised to follow up regularly in the vascular surgery clinic. The lower limb-related symptoms disappeared after 1 month. Six months after surgery, computed tomography indicated the disappearance of internal fistula and anatomically well-run PSA. The patient had normal cardiac function, normal dorsal foot/posterior tibial artery beats, warm skin, and no significant sensory and motor abnormalities (Figure 4). Quality of life was significantly improved compared to preoperative period.
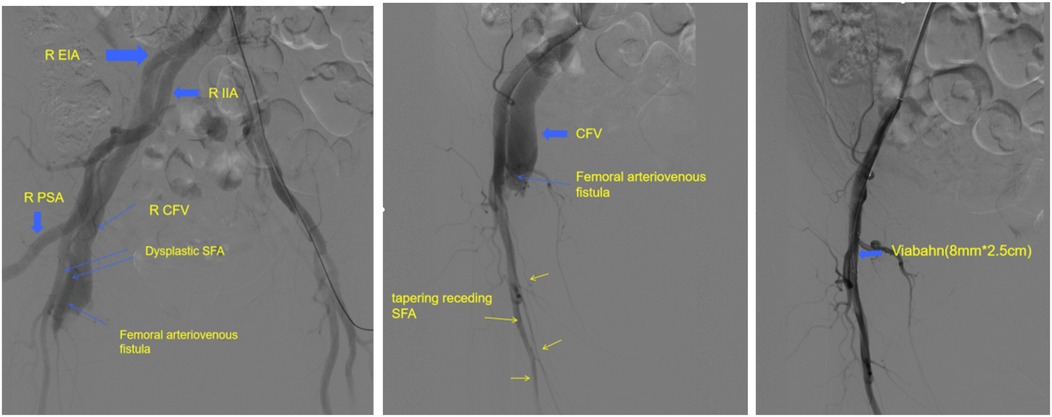
Figure 3. Arteriovenous fistula was seen on angiographic surgery. The PSA was confirmed intraoperatively. We placed a covered stent-graft to seal the internal fistula.
Discussion
In 1832, Green first reported the presence of a persistent sciatic artery in a postmortem case (4). PSA is a rare anatomical variant that persists in adulthood and predisposes patients to complications such as aneurysms and distal limb-threatening thromboembolism. PSA occurs bilaterally, with no significant differences according to sex or side of the body (5, 6). The incidence is approximately 0.025%–0.05 percent. Van Hooft et al. reported that the mean age at diagnosis of PSA was 57 years, with an almost equal sex distribution; according to a review of the literature, 56% of patients were female and 44% were male. Unilateral PSA accounts for 70% PSA cases (7). The rate of aneurysm formation in patients with PSA is approximately 44%.
Anatomically, the PSA is the continuation of the internal iliac artery. It accompanies the sciatic nerve, passes through the ischial foramen, and follows the back of the leg all the way to the ankle. Gauffre classifies the PSA into 5 categories. In types 1 and 2, PSA is fully present (8). The difference between types 1 and 2 is that in type 1, there is a fully developed SFA, whereas in type 2, the SFA is partially (type 2a, which is the most common type) or completely absent (type 2b). This case we introduced belongs to type 2a PSA. In types 3 and 4, the SFA are fully developed (1, 2). Type 3 is a partially proximal PSA with a distal deletion, and type 4 is a partially distal PSA with proximal artery absence (3). Gaufre et al. described type 5 PSA, in which the PSA originates from the middle sacral artery; in type 5a, the SFA is complete, and in type 5b, the SFA is absent (8).
While according to the anatomic status and the presence of aneurysm, Ahn et al. proposed a new classification system and treatment option (9). Class I from Ahn-Min's classification includes types 1 and 5a from the Pillet-Gauffre classification, class II includes types 3 and 4, and class III includes types 2a, 2b, and 5b. Class IV is a new class that is not classifiable by the previous Pillet-Gauffre classification. Ahn et al. insist that the risk of embolism from the presence of aneurysm is an important factor for treatment and bypass surgery is mostly required in classes III and IV (9). This case belongs to type 2a according to the Pillet-Gauffre classification, or class III the Ahn-Min's classification, PSA. As PSA was fully present, resulting in adequate distal blood supply and no ischemia or embolism occurred, therefore, conservative treatment was chosen.
PSA can be detected incidentally or confirmed through examinations such as arterial Doppler ultrasound, CT angiography, MRI angiography, or general angiography (10). Colour Doppler ultrasound can reveal gluteal artery aneurysm and determine the presence of a mural thrombus. CT angiography and MRI angiography confirmed the diagnosis and determined its relationship with adjacent anatomical structures, such as the sciatic nerve. Besides, most cases reported in the literature have generally used angiography (11). That's what we did.
The differentiating considerations for pulsatile PSA aneurysms include enlarged bursa, abscess, sciatic nerve hernia, granulomatous disease, tumours, and congenital or acquired arteriovenous fistulas (12).
Treatment depends on the patient's symptoms and relevant anatomical findings, as well as the physiological function and status of the SFA (13, 14). However, femoropopliteal artery bypass grafting is considered inadequate if the common femoral artery is underdeveloped. Therefore, grafting from the PSA (excluding aneurysms) is recommended to avoid persistent exposure of the graft to the hip region due to the potential risk of new aneurysms or pseudoaneurysms in the future, or arterial or graft occlusion (15). When PSA is entangled with the sciatic nerve, endovascular treatment (including a coil or stent graft) can be considered. Future complications such as thromboembolism or rupture of the lower limb should be avoided (4, 8). Asymptomatic, incidentally diagnosed PSA should be treated with medication and regular follow-up, as we have done in the case presented here (16). The patient's lower limb symptoms were attributed to the arteriovenous fistula rather than the persistent sciatic artery, which justified the decision to treat the fistula alone. About the 1-month postoperative drug treatment, we used rivaroxaban 20 mg qd to prevent stent and venous thrombosis, and diosamine 0.9 g bid to improve blood circulation. 1 month after the surgery till now, we administered clopidogrel 75 mg qd as antiplatelet therapy to prevent stent restenosis and thrombotic events in the systemic circulation.
Conclusions
At the time of the final follow-up(6-month), there was no recurrence of the lower limb discomfort symptoms. The treatment, conservative approach to PSA in this case with iatrogenic femoral arteriovenous fistula, was considered successful in the long term. When choosing the optimal treatment, consideration should be given to whether there is a relationship between lower extremity symptoms and the presence of PSA. Multiple individualised approaches should be considered in future studies. We expect longer follow-up results and more case data.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the studies involving humans because The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This research involving human participants conformed to the guidelines of the Declaration of Helsinki (2013). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LW: Writing – original draft, Writing – review & editing. YG: Writing – original draft, Writing – review & editing. SY: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We thank all study participants for participating in this study, and agreeing to use and publication of their data, as well as all the editors who reviewed this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cvetic V, Miletic M, Lukic B, Nestorovic D, Kostic O, Sladojevic M, et al. Successful hybrid approach treatment of a large persistent sciatic artery aneurysm-a case report. Medicina. (2023) 59(7):1328. doi: 10.3390/medicina59071328
2. Meghpara MK, Alaoudi M, Mutyala M. Persistent sciatic artery in a patient with unilateral acute lower extremity ischemia. J Vasc Surg Cases Innov Tech. (2021) 7(1):89–92. doi: 10.1016/j.jvscit.2020.08.034
3. Vadvala HV, Fishman EK. Bilateral persistent sciatic arteries. Radiology. (2023) 306(3):e221563. doi: 10.1148/radiol.221563
4. Green PH. On a new variety of the femoral artery.: with observations. Lancet. (1832) 17:730–1. doi: 10.1016/S0140-6736(02)83351-7
5. Nunes C, Sousa J, O'Neill Pedrosa J, Oliveira V, Silva E, Baldaia L, et al. An incidental finding of a persistent sciatic artery—case report and literature review. Port J Card Thorac Vasc Surg. (2023) 30(3):67–70. doi: 10.48729/pjctvs.370
6. Sinha M, Pandey NN, Rajagopal R, Jagia P. Bilateral persistent sciatic arteries: a rare anatomical variant. BMJ Case Rep. (2020) 13(2):e233742. doi: 10.1136/bcr-2019-233742
7. Yun WS, Kim HJ, Hwang D, Kim HK. Significance of collateral circulation in managing persistent sciatic artery: two case reports. Front Surg. (2023) 10:1159463. doi: 10.3389/fsurg.2023.1159463
8. Gauffre S, Lasjaunias P, Zerah M. Sciatic artery: a case, review of literature and attempt of systemization. Surg Radiol Anat. (1994) 16(1):105–9. doi: 10.1007/BF01627932
9. Ahn S, Min S-K, Min S-I, Ha J, Jung IM, Kim SJ, et al. Treatment strategy for persistent sciatic artery and novel classification reflecting anatomic status. Eur J Vasc Endovasc Surg. (2016) 52(3):360–9. doi: 10.1016/j.ejvs.2016.05.007
10. Cacioppa LM, Rosati M, Macchini M, Rossini N, Boscarato P, Vento V, et al. Different manifestations of persistent sciatic artery and possible treatment options: a series of four cases. Diagnostics (Basel). (2024) 14(21):2383. doi: 10.3390/diagnostics14212383
11. Sainz González F, Sánchez Galán Á, Lorente A, Palacios P. Persistent sciatic artery: a case report and literature review. Neurocirugia. (2022) 33(5):254–7. doi: 10.1016/j.neucie.2022.02.001
12. Liu Y, Yue W, Huang D. Bilateral persistent sciatic arteries with right sciatic artery aneurysm thrombosis and distal embolization: A case report. Ultraschall Med. (2025). doi: 10.1055/a-2444-2843
13. D'Adamo A, Sirignano P, Fanelli F, Mansour W, Montelione N, Cirelli C, et al. Endovascular solution of acute limb ischemia engendered by persistent sciatic artery pseudoaneurysm due to stent fracture. Ann Vasc Surg. (2017) 43:310.e9–e12. doi: 10.1016/j.avsg.2017.01.016
14. Nistor V, Billong A, Pirvu A, Feugier P. Endovascular treatment of persistent sciatic artery stenoses responsible for critical ischemia. J Med Vasc. (2024) 49(5-6):219–21. doi: 10.1016/j.jdmv.2024.09.002
15. Mariani E, Andreone A, Perini P, Azzarone M, Ucci A, Freyrie A. Endovascular treatment of persistent sciatic artery occlusion: case report and literature review. Ann Vasc Surg. (2021) 74:526.e13–e23. doi: 10.1016/j.avsg.2021.03.022
Keywords: persistent sciatic artery, dysplasia, iatrogenic arteriovenous fistula, common femoral vein, superficial femoral artery
Citation: Wang L, Gu Y and Yang S (2025) Conservative approach to a rare case of persistent sciatic artery with iatrogenic femoral arteriovenous fistula: a case report. Front. Surg. 12:1498368. doi: 10.3389/fsurg.2025.1498368
Received: 18 September 2024; Accepted: 10 February 2025;
Published: 26 February 2025.
Edited by:
Saroj Das, Imperial Consultants, United KingdomReviewed by:
Mojahid Najem, Bedford Hospital NHS Trust, United KingdomPasqualino Sirignano, Sapienza University of Rome, Italy
Natália Polidorio, Memorial Sloan Kettering Cancer Center, United States
Copyright: © 2025 Wang, Gu and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sen Yang, MTMxMzIxNTU3NTZAMTYzLmNvbQ==
 Lizhao Wang
Lizhao Wang Yan Gu
Yan Gu Sen Yang*
Sen Yang*