- 1Department of Spine Surgery, Liaocheng People’s Hospital, Liaocheng, Shandong, China
- 2Beijing Jishuitan Hospital Liaocheng Hospital, Liaocheng, Shandong, China
Purpose: This study aimed to describe a case of a patient with a lumbar ligamentum flavum cyst combined with spinal instability who underwent cyst resection and transforaminal lumbar interbody fusion (TLIF).
Methods: We present a rare case of a patient with a lumbar ligamentum flavum cyst combined with spinal instability causing radiculopathy. The patient underwent cyst resection and transforaminal lumbar interbody fusion.
Results: The patient underwent follow-up for 3 years postoperatively and remained asymptomatic, with favorable radiographic results.
Conclusions: Cysts resection and TLIF for ligamentum flavum cysts combined with spinal instability can achieve sufficient and effective decompression while simultaneously restoring spinal stability. Therefore, this approach is both an effective and safe treatment option.
Introduction
Ligamentum flavum cysts (LFCs) are rare space-occupying lesions in the spinal canal, which represent a unique entity being embedded in the inner surface of the ligamentum flavum with no epithelial lining and no association with spinal facets causing spinal canal compression and neurologic deficits (1–3). The symptoms are similar to those caused by lumbar disc herniation or lumbar spinal stenosis, such as lower back pain, numbness, pain, weakness, and cauda equina syndrome (4). Surgical intervention is recommended when patients exhibit acute neurological deterioration or when conservative treatment is ineffective. In this report, we present a case of a patient with a lumbar ligamentum flavum cyst combined with lumbar instability. The patient underwent cyst excision, spinal decompression, and interbody fusion, resulting in significant postoperative improvement in neurological symptoms and low back pain.
Case presentation
A 54-year-old woman presented with a 1-month history of low back pain accompanied by right leg radicular pain and numbness in the posterior lateral calf. The patient reported a pain score of 9 on the visual analog scale (VAS, 0 = no pain; 10 = extremely painful), and her Oswestry disability index (ODI) was 57.6%.
Physical examination revealed numbness in the skin of the posterolateral calf and weakness in both right ankle dorsiflexion and great toe extension (Grade 4). The Lasegue sign was negative on both limbs. Bilateral knee and Achilles tendon reflexes were decreased.
Before hospitalization, the patient received various conservative treatments, including non-steroidal anti-inflammatory drugs and acupuncture. However, her symptoms did not improve.
Laboratory tests showed that the white cell count (WCC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) of the patient were within normal limits. The dynamic lumbosacral radiographs showed obvious instability in the L4–L5 segment (Figure 1). The CT scan revealed a mass on the ventral side of the ligamentum flavum at the L4–L5 level (Figure 2). In addition, the enlarged L4–L5 facet joint space and the vacuum sign could be seen on the CT scan. Magnetic resonance imaging (MRI) scan showed a cystic lesion between the dural sac and ligamentum flavum at the L4–L5 level, compressing the cauda equina. The lesion was T1 hypointense and T2 hyperintense with significant rim enhancement after administration of gadolinium (Gd) (Figure 3).

Figure 1. Preoperative dynamic lumbosacral radiographs showing obvious instability in the L4–L5 segment.

Figure 2. Preoperative CT scan revealing a mass on the ventral side of the ligamentum flavum at the L4–L5 level. The enlarged facet space and the vacuum sign were observed.

Figure 3. Preoperative MRI of the cyst lesion showing T2 hyperintensity with significant rim enhancement after administration of gadolinium (Gd).
Surgical procedure and outcome
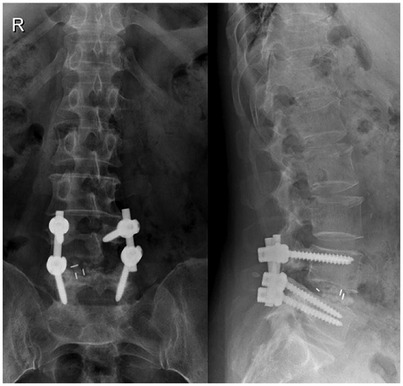
Under general anesthesia, the patient was positioned prone with the abdomen suspended in midair. The spinous process, lamina, and facet joint were exposed, and an effort was made to preserve the facet joint capsule at the L3–L4 level. Posterior decompression and transforaminal lumbar interbody fusion (TLIF) were performed (Figures 4, 5). Intraoperatively, the ligamentum flavum was removed en bloc, revealing a dark red isolated cyst noted on the ventral side of the ligamentum flavum, which was compressing the right L5 nerve root. Pathological examination confirmed the diagnosis of a ligamentum flavum cyst with hematoma. The patient presented with complete recovery of radiculopathy and low back pain. At 3 months postoperatively, her VAS score was 0 points, and her ODI was 7.2%. She was able to walk normally and remained relatively asymptomatic for 36 months after the operation at the last follow-up visit.
Discussion
Extradural cysts are classified anatomically or pathologically, according to their anatomical structure of origin, namely, herniated disc cyst, facet joint cyst, ligamentum flavum cyst, and posterior longitudinal ligament cyst (5, 6). LFCs were first described by Moiel et al. (7), and they arise from the ligamentum flavum with no connections to spinal facets. The pathogenesis of ligamentum flavum cysts remains unclear. According to previous research, hypertrophy of the ligamentum flavum and ligamentous degeneration and fibrosis are frequently present and likely to be sequelae of localized spinal trauma (8). Microtrauma caused by increased motion at a particular motion segment, segmental instability, and local stress associated with degeneration at the level of occurrence are considered risk factors for ligamentum flavum cysts (9, 10). Other studies indicated that the LFCs were closely related to aging or aging-related structural changes in ligamentum flavum, such as amyloid accumulation and calcification (2).
The most commonly reported location of LFCs is the L4–L5 level, which is the most mobile segment of the lumbar spine, followed by the L5–S1 and L3–L4 levels (11). In the present case, spondylolisthesis and instability can be observed at the L4–L5 level. The vacuum sign can be observed in the right facet of L4–L5, and effusion can be observed in the left facet. These signs suggest segmental instability and facet degeneration.
MRI is the gold standard for LFC diagnosis, allowing for high-resolution imaging of spinal cord tissue, edema, and ligaments (4, 12). The ligamentum flavum cyst appears typically as an epidural cystic mass located on one side of the ligamentum flavum with a clear boundary. It shows a low signal on T1-weighted images and a high signal on T2-weighted images, similar to the density of cerebrospinal fluid, and slight enhancement can be observed on a contrast-enhanced scan (4).
The majority of symptomatic cysts usually presents with radiculopathy, such as sciatica in the case of lumbar cysts, and can mimic symptoms related to intervertebral disc herniation, synovial cysts, ganglion cysts, and schwannomas (2). Peripheral plexopathies also need to be distinguished. The most common presenting symptoms of lumbosacral plexopathy include low back pain with unilateral radiation and possible association with positionality. MR neurography and electromyography are useful methods for differential diagnosis (13).
Conservative treatment such as steroid injection or CT-guided puncture is feasible when symptoms are mild. Surgical intervention should be considered in patients who have failed conservative treatment or in those with progressive and severe neurological deficits. Various surgical treatment strategies for ligamentum flavum cysts have been reported, such as microscopic fenestration and cystectomy, endoscopic cystectomy, and lumbar interbody fusion, among others (8, 14). The goal of surgical excision is decompression and complete removal of cysts along with ligamentum flavum (15). In our case, due to significant lumbar instability, we performed en bloc resection of the ligamentum flavum and TLIF. In this study, the surgical results were satisfactory during the follow-up.
Conclusion
Ligamentum flavum cysts are rare conditions that can cause sciatica. Currently, there is no uniform consensus on the surgical treatment of symptomatic lumbar ligamentum flavum cysts, and the surgical approach depends on the specific situation of the patient. Cyst resection and TLIF for ligamentum flavum cysts combined with spinal instability can achieve a sufficient and effective decompression, while simultaneously restoring spinal stability. Therefore, this approach is both an effective and safe treatment option.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Liaocheng People's Hospital Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
KY: Writing – original draft. CJ: Conceptualization, Writing – original draft. DL: Methodology, Writing – review & editing. JY: Formal Analysis, Investigation, Writing – review & editing. XW: Data curation, Investigation, Writing – review & editing. HX: Supervision, Writing – review & editing.
Funding
The authors declare financial support was received for the research, authorship, and/or publication of this article. Shandong Medicine and Health Technology Program (202404071052).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gazzeri R, Canova A, Fiore C, Galarza M, Neroni M, Giordano M. Acute hemorrhagic cyst of the ligamentum flavum. J Spinal Disord Tech. (2007) 20(7):536–8. doi: 10.1097/BSD.0b013e31804b4605
2. Taha H, Bareksei Y, Albanna W, Schirmer M. Ligamentum flavum cyst in the lumbar spine: a case report and review of the literature. J Orthop Traumatol. (2010) 11:117–22. doi: 10.1007/s10195-010-0094-y
3. Shah K, Segui D, Gonzalez-Arias S. Midline ligamentum flavum cyst of lumbar spine. World Neurosurg. (2018) 110:284–7. doi: 10.1016/j.wneu.2017.11.075
4. Tang J, Liu K, Xie W, Li X, Gan X, Li Y, et al. Endoscopic treatment of lumbar ligamentum flavum cyst by interlaminar approach: a minimally invasive and effective alternative to open surgery. J Orthop Surg Res. (2023) 18(1):344. doi: 10.1186/s13018-023-03824-3
5. Beltagi AH E, Swamy N, Dashti F. Vacuum epidural cyst with acute neurological presentation. A case report. Neuroradiol J. (2013) 26:213–7. doi: 10.1177/197140091302600212
6. Khalatbari K, Ansari H. MRI of degenerative cysts of the lumbar spine. Clin Radiol. (2008) 63:322–8. doi: 10.1016/j.crad.2007.05.020
7. Moiel RH, Ehni G, Anderson MS. Nodule of the ligamentum flavum as a cause of nerve root compression: a case report. J Neurosurg. (1967) 27(5):456–8. doi: 10.3171/jns.1967.27.5.0456
8. Chan AP, Wong TC, Sieh KM, Leung SS, Cheung KY, Fung KY. Rare ligamentum flavum cyst causing incapacitating lumbar spinal stenosis: experience with 3 Chinese patients. J Orthop Surg Res. (2010) 5:81. doi: 10.1186/1749-799X-5-81
9. Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: clinical presentation, the role of spinal instability, and treatment. J Neurosurg. (1996) 85(4):560–5. doi: 10.3171/jns.1996.85.4.0560
10. Kao CC, Uihlein A, Bickel WH, Soule EH. Lumbar intraspinal extradural ganglion cyst. J Neurosurg. (1968) 29(2):168–72. doi: 10.3171/jns.1968.29.2.0168
11. Seo DH, Park HR, Oh JS, Doh JW. Ligamentum flavum cyst of lumbar spine: a case report and literature review. Korean J Spine. (2014) 11:18–21. doi: 10.14245/kjs.2014.11.1.18
12. Rainone GJ, Zelmanovich R, Laurent D, Lucke-Wold B. How war has shaped neurosurgery. World Neurosurg. (2023) 178:136–44. doi: 10.1016/j.wneu.2023.07.100
13. Foreman M, Maddy K, Patel A, Reddy A, Costello M, Lucke-Wold B. Differentiating lumbar spinal etiology from peripheral plexopathies. Biomedicines. (2023) 11(3):756. doi: 10.3390/biomedicines11030756
14. Sharma SB, Lin GX, Kim JS. Full-endoscopic resection of ligamentum flavum cyst in lumbar spine. World Neurosurg. (2019) 130:427–31. doi: 10.1016/j.wneu.2019.07.120
Keywords: surgical decompression, spinal instability, lumbar interbody fusion, ligamentum flavum (LF), cyst
Citation: Yang K, Ji C, Luo D, Yin J, Wu X and Xu H (2025) Case Report: Surgical treatment of lumbar ligamentum flavum cysts combined with spinal instability causing radiculopathy. Front. Surg. 12:1481216. doi: 10.3389/fsurg.2025.1481216
Received: 19 August 2024; Accepted: 23 January 2025;
Published: 10 February 2025.
Edited by:
Altay Sencer, Istanbul University, TurkeyReviewed by:
Brandon Peter Lucke-Wold, University of Florida, United StatesFeyza Karagöz Güzey, Bagcilar Training and Research Hospital, Türkey
Copyright: © 2025 Yang, Ji, Luo, Yin, Wu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Xu, eHVoc3BpbmVAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Keshi Yang1,2,†
Keshi Yang1,2,† Hui Xu
Hui Xu