- 1Department of Neurosurgery, General Hospital of Xinjiang Military Command, Urumqi, China
- 2Department of Neurosurgery, Sir Run Run Shaw Hospital, College of Medical Sciences, Zhejiang University, Hangzhou, China
Background: Traumatic scalp arteriovenous fistula is a rare vascular abnormality. Open surgical removal and embolization have been employed to address this condition.
Methods: In this report, we present a case involving a 41-year-old man who exhibited a progressively enlarging pulsatile mass in his right occipital scalp. Computerized tomography angiography (CTA) and digital subtraction angiography (DSA) identified a complex scalp arteriovenous fistula (S-AVF). The combination of clinical symptoms and neuroimaging findings facilitated the diagnosis.
Results: Following a thorough discussion, we implemented a comprehensive strategy that included both endovascular embolization and surgical resection. The patient demonstrated an excellent prognosis with no reported discomfort.
Conclusions: A comprehensive surgical approach should be considered in the management of patients with complex scalp arteriovenous fistula.
Introduction
Traumatic scalp arteriovenous fistula (S-AVF) is a rare vascular abnormality (1, 2). Since the original report by Wardrop in 1827, only a limited number of cases have been documented (3). This condition is characterized by a direct connection between the arterial feeding vessels of the scalp and the draining veins, bypassing the intervening capillary beds (2). In contrast, arteriovenous malformation (AVM) is a congenital lesion that features a nidus between the arterial and venous systems (4–6). Due to abnormal hemodynamics, S-AVF can progress from a small swelling to a palpable subcutaneous mass, presenting various symptoms such as headache, bruits, tinnitus, epilepsy, hemorrhage, and scalp necrosis (7, 8). Several primary treatment methods, including open surgical removal and embolization, have been employed to address this condition (6, 9, 10). In this report, we present a distinct case of a ruptured Yokouchi type C S-AVF, which was successfully diagnosed through preoperative symptoms and neuroimaging studies, and resolved via a comprehensive treatment approach that included endovascular embolization and surgical resection. The patient exhibited an excellent response, suggesting that comprehensive treatment may be clinically beneficial for complex S-AVF.
Clinical report
History and examination
A 41-year-old man presented with a progressive, painless, pulsatile mass in his right occipital skull (Figure 1). He exhibited no neurological deficits. The patient reported having accidentally bumped his head against a corner of a window approximately 20 years prior. A general examination revealed a pulsating mass measuring 12 cm × 7 cm, accompanied by bilateral tortuous vessels. A loud bruit was detected upon auscultation. Computed tomography angiography (CTA) revealed a complex arteriovenous fistula located in the right occipital scalp and extending into part of the right temporoparietal region (Figure 1). Digital subtraction angiography (DSA) confirmed that the feeding arteries included the bilateral superficial temporal arteries (STA), bilateral occipital arteries (OA), and the right posterior auricular artery (PAA). The dominant draining vein was identified as the right superficial occipital vein. Furthermore, there was no connection observed between the intracranial and extracranial vessels (Figure 2A,B).

Figure 1. Scalp arteriovenous fistula (S-AVF). (A) 41-year-old man presented with a pulsating mass measuring 12 × 7 × 3 cm in size in his right occipital part. (B) CTA shows a complex multiple arteriovenous fistula located in the right occipital scalp and part of the right temporoparietal region, blood was supplied by branches of bilateral external carotid arteries and drained by the right superficial occipital vein.
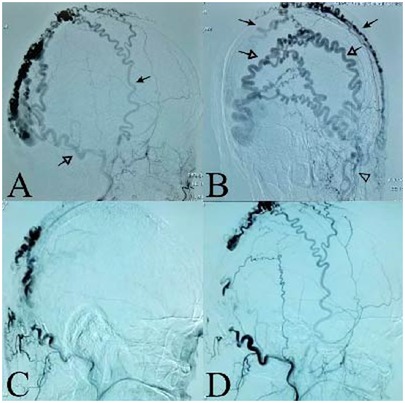
Figure 2. Interventional embolization of S-AVF. (A) Right external carotid artery angiography. Black arrow shows the right superficial temporal arteries (STA); white arrow shows the right occipital artery (OA). (B) Left external carotid artery angiography. The black arrow shows the bilateral superficial temporal arteries (STA); the white arrow shows the bilateral occipital arteries (OA). (C/D) DSA of right occipital artery embolization demonstrated the partial occlusion of the S-AVF.
Operation and postoperative course
After analyzing the angio-architecture and size of the S-AVF, we decided to proceed with a comprehensive treatment involving endovascular embolization and surgical removal. Onyx liquid embolic material was successfully injected into the branches of the right occipital arteries supplying the S-AVF. Post-embolization digital subtraction angiography (DSA) revealed partial occlusion of the S-AVF, with the bilateral superficial temporal arteries only faintly contributing to its perfusion (Figure 2C,D). To prevent scalp necrosis, we ceased endovascular treatment at this point. Notably, the mass size was significantly reduced compared to pre-embolization measurements. Following several days of observation, both the temperature and color of the skin returned to normal. Surgical resection was then performed in a prone position under general anesthesia. A semicircular scalp incision was made along the mass, and to minimize bleeding, we initially ligated the tortuous vessels surrounding the mass. Upon incising the scalp, we observed an abundance of large, tortuous, dilated venous plexuses situated beneath the galea aponeurotica. We ligated and completely excised the feeding arteries and draining veins. Finally, we removed the mass and sutures, closed the flap in a standard manner (Figure 3, Figure 4A).
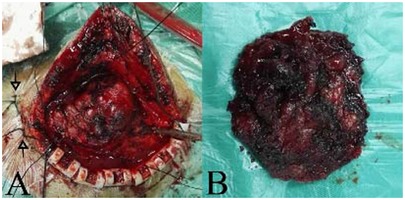
Figure 3. The mass of surgical resection. (A) The white arrows show suture lines ligating the feeding arteries near the mass. (B) The mass was totally removed.

Figure 4. The scalp after surgical resection. (A) The surgical incision was dry and clean, and the raised mass disappeared on the third day. (B) After the 12-month follow-up, no recurrence and nothing abnormal was observed, except for lack of hair in part of surgical incision.
Histopathological examination confirmed the presence of an arteriovenous fistula. Postoperatively, all symptoms resolved, and no complications arose. At the 12-month follow-up, no recurrence was found (Figure 4B).
Discussion
The diagnosis of S-AVF
Traumatic S-AVF is an uncommon vascular disease, reported infrequently in the literature (11–13). This condition is characterized by a direct connection between the arterial feeding vessels and the draining veins of the scalp, bypassing the intervening capillary beds (2). The superficial temporal artery (STA) is most commonly involved due to its long and relatively superficial course in the scalp (2, 14). Treatment is challenging due to the complex pathogenesis and heterogeneous angio-architecture associated with the disease.
The main symptoms of traumatic S-AVF can vary and may include a pulsatile mass, bruits, tinnitus, headaches, epilepsy, hemorrhage, and scalp necrosis (7, 8). Sofela et al. reported that congestive heart failure may even occur in severe cases (8).
The pathophysiology of traumatic S-AVF remains not fully understood. The laceration theory posits that simultaneous laceration of both the artery and the adjacent vein leads to the formation of the fistula (15). An alternative mechanism, known as the disruption theory, suggests that the rupture of the vasa vasorum in the artery wall initiates the process. This rupture leads to the proliferation of endothelial cells from the damaged vasa vasorum, facilitating the formation of numerous small vessels and resulting in vascular communication channels between the artery and vein (1).
Yokouchi classified S-AVF into three types: Type A, a single fistula fed by a single proximal feeding artery; Type B, a single fistula fed by multiple feeding arteries; and Type C, multiple fistulas with plexiform feeding arteries and a main dilated draining vein (16). Our case falls under Type C, which is considered to require a comprehensive treatment approach that combines embolization with surgical removal (16, 17).
The diagnosis of S-AVF is based on local symptoms and characteristic AVF manifestations observed through imaging techniques such as magnetic resonance imaging/angiography (MRI/MRA), computed tomography angiography (CTA), and digital subtraction angiography (DSA). Notably, DSA is regarded as the gold standard for imaging S-AVF, as it allows for dynamic observation of both the feeding arteries and the draining veins.
The management of S-AVF
The goal of treating S-AVF is to prevent hemorrhage and scalp necrosis, as well as to alleviate the pulsatile mass. Traditionally, open surgery has been the standard treatment, offering clear removal of lesions with a low incidence of complications (18). However, with the advent of micro-catheters and enhanced embolization materials, endovascular therapy has emerged as a significant therapeutic option for S-AVF. Nonetheless, endovascular treatment for complex multiple S-AVF can be challenging, as it carries a risk of recurrence post-embolization and may not adequately address all abnormal vessels, thus failing to achieve a radical cure for the mass (19). Additionally, complications following embolization can include tenderness, hyperemia, scalp necrosis, and the potential escape of embolic materials into the circulatory system (2, 20), as well as thrombosis formation or vessel dissection (21).
In our current case study, we present a comprehensive approach to managing complex multiple S-AVF (Yokouchi Type C) through a combination of endovascular embolization and surgical removal. Given the definitive preoperative diagnosis and the tailored therapeutic plan for S-AVF, embolization was frequently employed as an initial strategy to mitigate the risks associated with surgical resection. We emphasize the importance of monitoring the skin's temperature and color post-embolization to detect signs of ischemia or necrosis, which may necessitate flap transfer during open surgery, alongside the administration of drugs to enhance microcirculation. Following embolization, the mass size significantly decreases, and substantial blood loss is reduced during surgical resection. Clinical practice has demonstrated that ligating the feeding arteries adjacent to the mass should be prioritized to minimize bleeding during surgery.
This case contributes to our understanding of this rare condition. The combination of clinical symptoms and neuroimaging studies plays a crucial role in diagnosis. The prognosis for complex multiple S-AVF is excellent following a comprehensive surgical approach.
Conclusions
Traumatic scalp arteriovenous fistula (S-AVF) is a rare vascular abnormality characterized by a direct connection between the arterial feeding vessels and the draining veins of the scalp, effectively bypassing the intervening capillary beds. Comprehensive treatment methods, including open surgical removal and endovascular embolization, have been employed to address this condition. Overall, the prognosis is generally favorable following comprehensive treatment.
Data availability statement
The data presented in this article is available upon request from the corresponding author.
Ethics statement
The studies involving human participant was reviewed and approved by the Institutional Review Board of the Hospital. The patient/participant provided their written informed consent to participate in this study.
Author contributions
ZM: Writing – original draft, Conceptualization, Data curation. ZZ: Writing – original draft. DX: Writing – review & editing. LQ: Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Badejo L, Rockwood P. Traumatic arteriovenous fistula of the scalp. J Neurosurg. (1987) 66:773–4. doi: 10.3171/jns.1987.66.5.0773
2. Li F, Zhu S, Liu Y, Chen Y, Chi L, Chen G, et al. Traumatic arteriovenous fistula of the superficial temporal artery. J Clin Neurosci. (2007) 14:595–600. doi: 10.1016/j.jocn.2006.04.011
3. Wardrop J. Case of carotid aneurism, successfully treated by tying the artery above the aneurismal tumour. Med Chir Trans. (1827) 13:217–74. doi: 10.1177/09595287270130P120
4. Smith AB. Vascular malformations of the brain: radiologic and pathologic correlation. J Am Osteopath Coll Radiol. (2012) 1:10–22.
5. Khera D, Khera PS, Sinha A. A case of pulsatile scalp swelling in a child. BMJ Case Rep. (2017) 2:218214. doi: 10.1136/bcr-2016-218214
6. Zheng F, Augustus Pitts H, Goldbrunner R. Traumatic arteriovenous fistula of the scalp in the left temporoparietal region with intra- and extracranial blood supply. Case Rep Vasc Med. (2016) 2:8671472. doi: 10.1155/2016/8671472
7. Dabus G, Pizzolato R, Lin E, Kreusch A, Linfante I. Endovascular treatment for traumatic scalp arteriovenous fistulas: results with onyx embolization. J Neuro Interv Surg. (2014) 6:405–8. doi: 10.1136/neurintsurg-2013-010724
8. Sofela A, Osunronbi T, Hettige S. Scalp cirsoid aneurysms: case illustration and systematic review of literature. Neurosurgery. (2020) 86(2):E98–E107. doi: 10.1093/neuros/nyz303
9. Albuquerque Sousa LH, Maranha Gatto LA, Demartini Junior Z, Koppe GL. Scalp cirsoid aneurysm: an updated systematic literature review and an illustrative case report. World Neurosurg. (2018) 119:416–27. doi: 10.1016/j.wneu.2018.08.098
10. Gurkanlar D, Gonul M, Solmaz I, Gonul E. Cirsoid aneurysms of the scalp. Neurosurg Rev. (2006) 29(03):208–12. doi: 10.1007/s10143-006-0023-y
12. Fisher-Jeffes ND, Domingo Z, Madden M, de Villiers JC. Arteriovenous malformations of the scalp. Neurosurgery. (1995) 36:656–60. doi: 10.1227/00006123-199504000-00003
13. Nishijima I, Ikemura R, Gushiken M, Miyagi K, Iha K. Nonsurgical treatment of scalp arteriovenous malformation using a combination of ultrasound-guided thrombin injection and trans- arterial coil embolization. J Vasc Surg. (2012) 55:833–6. doi: 10.1016/j.jvs.2011.08.013
14. Hyshaw C, Di Tullio M, Renaudin J. Superficial temporal arteriovenous Fistula. Surg Neurol. (1979) 12:46–8.451861
15. Stasik JF, Engelcke BR, Zwemer F. False aneurysm of the external maxillary artery: report of case. J Oral Surg Anesth Hosp Dent Serv. (1964) 22:441–5.14178807
16. Yokouchi T, Iwabuchi S, Tomiyama A, Samejima H, Ogata N, Goto K. Embolization of scalp AVF. Interv Neuroradiol. (1999) 1:121–6. doi: 10.1177/15910199990050S122
17. Komiyama M, Nishikawa M. Non-traumatic arteriovenous fistulas of the scalp treated by a combination of embolization and surgical removal. Neuro Med Chir (Tokyo). (1996) 36:162–5. doi: 10.2176/nmc.36.162
18. El Shazly AA, Saoud KM. Results of surgical excision of cirsoid aneurysm of the scalp without preoperative interventions. Asian J Neurosurg. (2012) 7:191–6. doi: 10.4103/1793-5482.106651
19. Xue B, Yi L, Chao Y. Surgical resection of a complex multiple scalp AVF without preoperative embolization: a case report. Turk Neurosurg. (2015) 25(4):638–42. doi: 10.5137/1019-5149.JTN.8707-13.2
20. Amlashi SF, Riffaud L, Morandi X. Arteriovenous fistula of the superficial temporal artery: an exceptional complication of the pterional approach. J Neurol Neurosurg Psychiatry. (2004) 75:1077–8. doi: 10.1136/jnnp.2003.019489
Keywords: scalp arteriovenous fistula (S-AVF), comprehensive approach, endovascular embolization, surgical resection, trauma
Citation: Ma Z, Zou Z, Xie D and Qian L (2025) Comprehensive surgery of complex scalp arteriovenous fistula: a successful trial. Front. Surg. 11:1492616. doi: 10.3389/fsurg.2024.1492616
Received: 7 September 2024; Accepted: 17 December 2024;
Published: 13 January 2025.
Edited by:
Stefano Cianci, University of Messina, ItalyReviewed by:
Majed Katati, University of Granada, SpainEgan Kalmykov, Brandenburg Medical School Theodor Fontane, Germany
Copyright: © 2025 Ma, Zou, Xie and Qian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dajiang Xie, eWFuZ3NodXh1QDI5ODAuY29t
†These authors share first authorship
 Zhiming Ma1,†
Zhiming Ma1,† Dajiang Xie
Dajiang Xie