- 1Interventional Radiology Section, Department of Medical Imaging, University Hospital Timone, APHM, Marseille, France
- 2Aix Marseille Univ, LIIE, Marseille, France
- 3Aix Marseille Univ, CERIMED, Marseille, France
- 4Department of Visceral Surgery, Aix-Marseille University, Hôpital de la Timone, Marseille, France
- 5Department of Surgery, Sapienza University of Rome, Rome, Italy
Introduction: Hemorrhoidal artery embolization, also known as Emborrhoid, has emerged in recent years as a minimally invasive treatment option for patients with recurrent and unresponsive to medical therapies hemorrhoidal bleeding symptoms. We present here an overview of the profile of rectal artery embolization based on the most relevant and recent literature.
Methods: A comprehensive review of literature on Hemorrhoidal artery embolization, was conducted on PubMed–Medline. The most relevant literature was summarized narratively.
Results: Current literature confirms the feasibility, efficacy and safety of rectal artery embolization for bleeding hemorrhoids. To date, the results of nearly 250 patients who have undergone hemorrhoid embolization have been published in several studies. All these authors have reported high immediate technical success, with also high clinical success, ranging from 63% to 94%, without major complications. Because of its beneficial safety profile, rectal artery embolization represents an attractive option for selected patients. In case of recurrence of bleeding it is possible to consider repeating the embolization procedure. Treatment failure may be due to the presence of anatomical variants such as dominant middle rectal arteries, which can be investigated and treated in the second session if necessary.
Conclusion: Rectal artery embolization represents a valuable addition to the therapeutic armamentarium of bleeding hemorrhoidal disease, if patients are selected appropriately.
1 Background
The technique of rectal artery embolization has emerged as a new treatment option over the past decade for patients suffering from bleeding hemorrhoids. Hemorrhoidal disease is the most common anorectal disorder, affecting millions of people worldwide, with a prevalence ranging from 4.4% to 39% (1, 2) and predominant symptoms of bleeding and pain (3–5). The internal hemorrhoids are a physiological vascular structure composed of a richly anastomosing arteriovenous network that contributes to the continence of the anal canal, forming a circumferential submucosal bulge at the anorectal junction, known as the corpus cavernosum recti (CCR) (6–9). Although the pathophysiology remains controversial and multifactorial, internal hemorrhoidal pathology is thought to result from chronic hypertrophy of these vascular structures secondary to a chronic increase in flow through the CCR, ultimately leading to hyperplasia of the cushions responsible for congestive hypertension which can be considered as one of the main factor (10, 11).
Most patients are relieved by medical or minimally invasive treatments (injection sclerotherapy, rubber band ligation, infrared photocoagulation, bipolar diathermy), and surgical treatment is required in 10% of cases (12, 13). The gold-standard surgical procedure is the open hemorrhoidectomy of Milligan and Morgan (14–16). Today, however, there are less invasive techniques such as the Longo procedure. The hemorrhoidopexy with or without doppler-guided elective hemorrhoidal artery ligation (DG-HAL) (17–21) always in the context of a tailored approach. Following the principle of less invasivity emborrhoid introduced by vidal et al. in 2013 (22), is gaining a strong role in the surgical option panorama.
Here we discuss rectal artery embolization, its advantages and disadvantages, based on the most recent and relevant literature, and attempt to clarify its role in the treatment of hemorrhoidal disease.
2 Patient selection
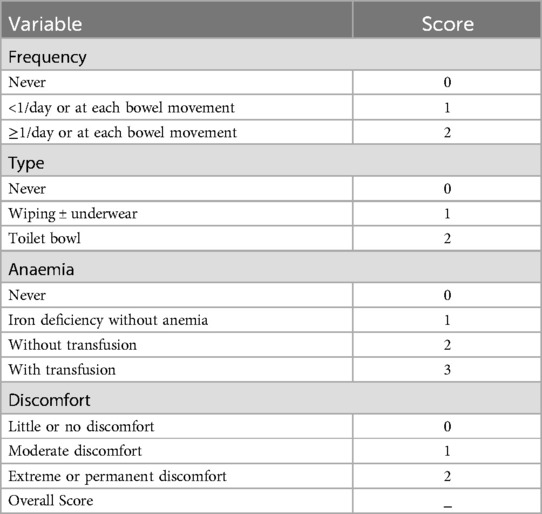
Selecting and monitoring patients who will benefit from an embolization procedure requires a multidisciplinary team of interventional radiologists and proctologists. An initial preoperative clinical examination by a proctologist or visceral surgeon is essential to assess the stage of hemorrhoidal disease and to verify the absence of anorectal cancer. At the initial consultation, the severity of hemorrhoidal symptoms is assessed using the Hemorrhoidal Bleeding Score (23), which ranges from 0, indicating that the severity of hemorrhoidal symptoms has not been assessed, to 9, indicating daily bleeding with anemia, requiring a blood transfusion (Table 1). The degree of internal prolapse is assessed using the Goligher classification (24, 25), ranging from 1 (no prolapse) to IV (irreducible prolapse) (Table 2). It is necessary to describe the number of pathological piles and the clinical characteristics of each of them. In particular the degree of Goligher but also which piles bleed and which ones do not bleed (20, 21).
The best candidates for rectal artery embolization are those with grade II-III prolapse and whose predominant symptoms are hemorrhagic in nature, as well as patients with grade IV prolapse in cases of surgical contraindication.
It is important to take a detailed history of the patient, which should include the extent, severity and duration of symptoms, daily eating habits, associated symptoms (e.g., fecal incontinence, constipation) and details of bowel movements. Rectal artery embolization is indicated for patients suffering from recurrent and unresponsive hemorrhoidal bleeding. This may be of interest in the case of patients on long-term anticoagulant or antiplatelet therapy, as well as patients with coagulation disorders (e.g., hemophilia). Chronic inflammatory bowel disease, on the other hand, is not a good indication, as these patients essentially suffer from anal fistulas or digestive tract lesions unrelated to hemorrhoidal lesions. However, embolization of the rectal arteries will not alleviate the normal ageing process or any positional pelvic disorders.
The preprocedural evaluation should rule out the presence of conditions that are general contraindications to hemorrhoid embolization, such as anorectal cancer, as well as those that are contraindications to conventional angiography, like renal failure and allergies to iodinated contrast media. Advanced atherosclerosis is a relative contraindication that could result in technical failure and should be assessed during preprocedural imaging.
3 Procedure
The patient is given detailed explanations about the procedure, its benefits, and risks. Written consent is obtained. The patient may receive light sedatives to reduce anxiety if it's necessary. No prophylactic antibiotics required. The puncture site (usually the groin area for access to the femoral artery) is shaved and disinfected.
Under local anaesthetic, the femoral artery is punctured and a valved introducer inserted. Transradial access can also be used, and can provide greater patient satisfaction and fewer complications than transfemoral access (26, 27). The radiologist uses real-time imaging (fluoroscopy) and cone-beam CT to guide the catheter through the arterial system to the inferior mesenteric artery and finally to the superior rectal arteries (28). Once the catheter is in place, a contrast agent is injected to visualize the rectal arteries and identify the branches supplying the hemorrhoids. The radiologist specifically targets the branches of the superior rectal arteries that supply the hemorrhoids. Microbeads or metal coils are injected through the catheter to occlude these arterial branches, thereby reducing blood flow to the hemorrhoids (29) (Figure 1).
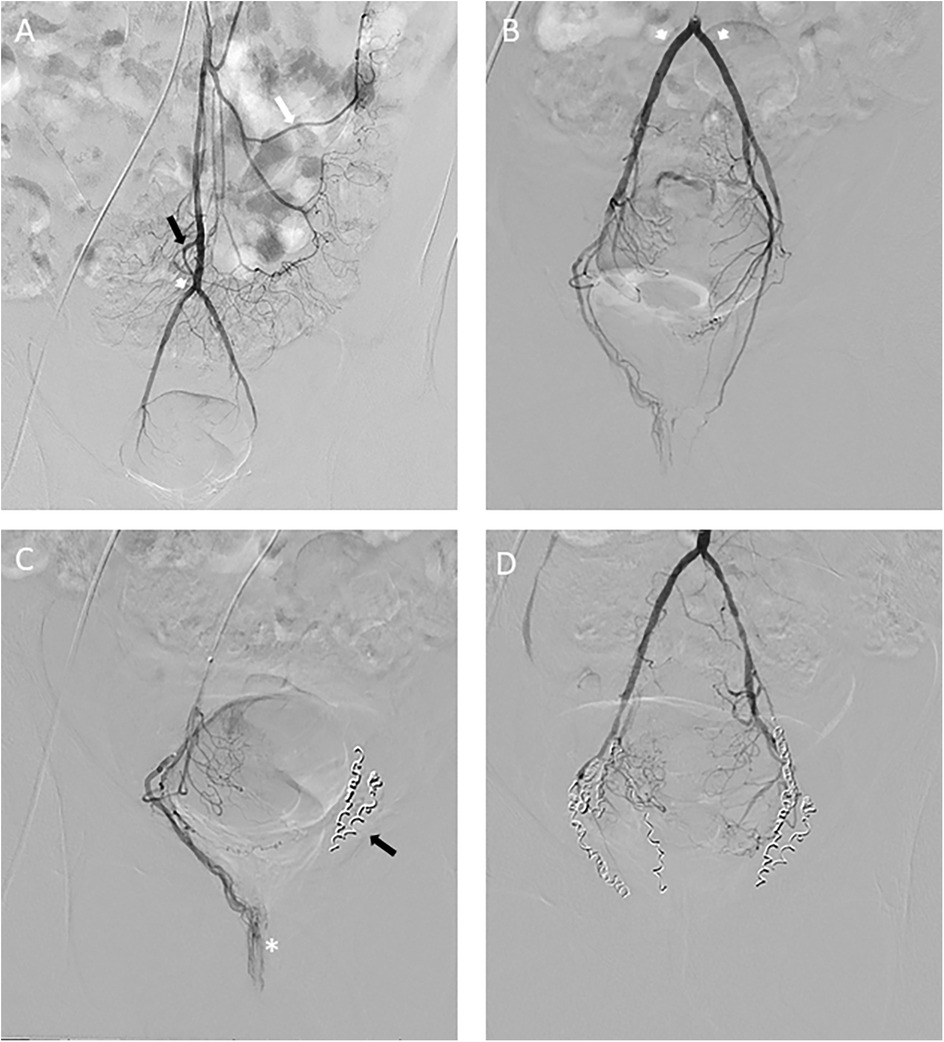
Figure 1. (A) Frontal digital subtraction angiography showing a modal anatomy of the inferior mesenteric artery, in order, the left colonic artery (white arrows) and then the sigmoid artery (black arrows). Then comes the SRA (arrowheads) terminal branch of the IMA that ends in projection from the pubic bone. (B) Frontal DSA showing codominant right and left SRA anterior branches (arrowheads). (C) Progression of the microcatheter to the tortuous right anterior branch, projecting opposite the pubic bone (asterisk) and embolization of the left SRA artery (black arrow) (D) At the end of the procedure, no residual branch is opacified under the pubic symphysis.
After embolization, the catheter is carefully removed. Pressure is applied to the insertion site to stop any bleeding. Sometimes, a vascular closure device is used to seal the incision (30). A compression dressing. The patient is monitored for a few hours to observe any signs of immediate complications, such as bleeding or an allergic reaction to the contrast agent (31). Instructions are provided on caring for the insertion site, managing pain, and recognizing signs of potential complications.
The patient can return home the same day after the interventional radiologist's visit if except in cases where the patient prefers to stay overnight in hospital under supervision.
4 Efficacy
Studies show that rectal artery embolization can significantly reduce symptoms. The technical success rate of rectal artery embolization is high, indicating that radiologists can usually successfully occlude the targeted arteries without major complications. Patients treated with rectal artery embolization often report high levels of satisfaction due to the minimally invasive nature of the procedure and rapid symptom relief (32–40).
Makris et al. provide an extensive review of multiple studies assessing the efficacy and outcomes of rectal artery embolization in treating hemorrhoidal disease (41). Fourteen studies involving a total of 362 patients were analyzed. The mean maximum follow-up duration was 12.1 months, and the average hospital stay was 1.5 days. The mean technical success rate was 97.8% (SD 3.5). A significant reduction in the French bleeding score was observed before and after embolization (P = 0.004). The effect on pain was reported in 6 of 14 studies, and all of them reported significant relief; however, this finding was quantified with various questionnaires. Bleeding recurrence during the follow-up period was reported in 11 of the 14 studies, with an average occurrence in 22.5% of patients (range, 5.4%–44%). Among this subgroup, 5%–43% of patients required embolization of additional vessels, such as the inferior rectal artery (IRA) or middle rectal artery (MRA). No cases of bowel ischemia, necrosis, or anorectal complications were reported.
Another meta-analysis published by Nguyenhuy looked at 14 different studies involving some 400 patients (42). This study confirms a success rate of rectal embolization between 73% and 89% with no major complication.
Compared to traditional surgical treatments such as hemorrhoidectomy, rectal artery embolization offers several advantages (even if a comparison with transanal desarterialization without pexia or sclerotherapy seems more appropriate):
- Less Postoperative Pain: Patients generally experience less pain after embolization compared to hemorrhoidectomy.
- Quicker Recovery: The procedure is less invasive, allowing for a quicker return to normal activities.
- Fewer Complications: The complication rate is generally lower compared to traditional surgical interventions.
5 Complications and follow-up
Rectal artery embolization is generally accepted to have a very beneficial side effect profile. Complications at the puncture site, such as hematoma, infection, and pseudoaneurysm, may occur but are rare, particularly when using ultrasound-guided vascular access and a closure device. There have been no reported anal complications associated with nonterminal occlusion using microcoils, and no cases of sphincteric dysfunction have been reported to date.
Anal discomfort, such as tenesmus, may occur during the procedure but typically resolves spontaneously. It is crucial to exercise caution when using microspheres in hemorrhoid embolization to prevent any ischemic complications while treating a benign condition like hemorrhoids.
After embolization, each patient is monitored by the interventional radiologist, proctologist, or surgeon to evaluate changes in symptoms using the hemorrhoidal bleeding score, Goligher classification, and a quality of life score. Any complications approximately three months after the procedure are recorded using the Clavien–Dindo grading system (grades I–IV) for surgical complications (43, 44). During the 3-month follow-up visit, patients are reassessed using the 36-item short-form health survey and the hemorrhoidal bleeding score. If there are improvements and the patient is satisfied, the procedure is deemed successful. In cases of procedural failure, a new embolization may be proposed to identify any residual artery.
6 Conclusion
Rectal artery embolization is a minimally invasive treatment option for patients with bleeding hemorrhoidal disease. Safety and efficacy have been adequately proven in the short and medium term. Because its therapeutic approach is completely different from other techniques, rectal artery embolization also has some unique features.
Hemorrhoidal artery embolization should target patients with recurrent bleeding as their main symptom. This technique has some limitations, as it does not improve the prolapse itself, and should only be used in cases where painful symptoms are at the forefront, when all other pathologies have been eliminated and usual treatments ineffective. Collaboration with proctologists and visceral surgeons is crucial. The aim is not to replace existing surgical therapies but to provide an additional treatment option for patients.
The most important advantages are the absence of post-operative complications, particularly post-operative pain, the ambulatory nature of the management and the high efficacy. If patients are selected appropriately, hemorrhoidal artery embolization represents a step towards more patient-oriented treatment, and a valuable addition to the therapeutic arsenal in the treatment of chronic hemorrhoidal disease. Randomized controlled trials with longer follow-up are needed to determine the optimal role of this emerging and minimally invasive technique. In addition, the place of different embolization materials needs to be assessed in a comparative study. The latest studies show superior clinical success rates when using microparticles, with lower re-intervention rates compared with coils.
Author contributions
JP: Writing – original draft, Writing – review & editing. DM: Writing – review & editing. MD: Writing – review & editing. JD: Writing – review & editing. IK: Writing – review & editing. VV: Writing – review & editing. GG: Writing – review & editing. FT: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Riss S, Weiser FA, Schwameis K, Riss T, Mittlböck M, Steiner G, et al. The prevalence of hemorrhoids in adults. Int J Colorectal Dis. (2012) 27(2):215–20. doi: 10.1007/s00384-011-1316-3
2. Ganz RA. The evaluation and treatment of hemorrhoids: a guide for the gastroenterologist. Clin Gastroenterol Hepatol. (2013) 11(6):593–603. doi: 10.1016/j.cgh.2012.12.020
3. Lee EW, Laberge JM. Differential diagnosis of gastrointestinal bleeding. Tech Vasc Interv Radiol. (2004) 7:112–22. doi: 10.1053/j.tvir.2004.12.001
4. Longstreth GF. Epidemiology and outcome of patients hospitalized with acute lower gastrointestinal hemorrhage: a population-based study. Am J Gastroenterol. (1997) 92:419–24.9068461
5. Kluiber RM, Wolff BG. Evaluation of anemia caused by hemorrhoidal bleeding. Dis Colon Rectum. (1994) 37(10):1006–7. doi: 10.1007/BF02049313
6. Aigner F, Bodner G, Gruber H, Conrad F, Fritsch H, Margreiter R, et al. The vascular nature of hemorrhoids. J Gastrointest Surg. (2006) 10(7):1044–50. doi: 10.1016/j.gassur.2005.12.004
7. Aigner F, Bodner G, Conrad F, Mbaka G, Kreczy A, Fritsch H. The superior rectal artery and its branching pattern with regard to its clinical influence on ligation techniques for internal hemorrhoids. Am J Surg. (2004) 187:102–8. doi: 10.1016/j.amjsurg.2002.11.003
8. Thomson WH. The nature of haemorrhoids. Br J Surg. (1975) 62(7):542–52. doi: 10.1002/bjs.1800620710
9. Stelzner F. The corpus cavernosum recti. Dis Colon Rectum. (1964) 7:398–9. doi: 10.1007/BF02616852
10. Miller R, Bartolo DC, Roe A, Cervero F, Mortensen NJ. Anal sensation and the continence mechanism. Dis Colon Rectum. (1988) 31(6):433–8. doi: 10.1007/BF02552612
11. Lestar B, Penninckx F, Kerremans R. The composition of anal basal pressure. An in vivo and in vitro study in man. Int J Colorectal Dis. (1989) 4(2):118–22. doi: 10.1007/BF01646870
12. Cengiz TB, Gorgun E. Hemorrhoids: a range of treatments. Cleve Clin J Med. (2019) 86(9):612–20. doi: 10.3949/ccjm.86a.18079
13. Altomare DF, Giuratrabocchetta S. Conservative and surgical treatment of haemorrhoids. Nat Rev Gastroenterol Hepatol. (2013) 10(9):513–21. doi: 10.1038/nrgastro.2013.91
14. Arezzo A, Podzemny V, Pescatori M. Surgical management of hemorrhoids. State of the art. Ann Ital Chir. (2011) 82(2):163–72.21682110
15. Simillis C, Thoukididou SN, Slesser AA, Rasheed S, Tan E, Tekkis PP. Systematic review and network meta-analysis comparing clinical outcomes and effectiveness of surgical treatments for haemorrhoids. Br J Surg. (2015) 102(13):1603–18. doi: 10.1002/bjs.9913
16. Zhang G, Liang R, Wang J, Ke M, Chen Z, Huang J, et al. Network meta-analysis of randomized controlled trials comparing the procedure for prolapse and hemorrhoids, Milligan-Morgan hemorrhoidectomy and tissue-selecting therapy stapler in the treatment of grade III and IV internal hemorrhoids(meta-analysis). Int J Surg. (2020) 74:53–60. doi: 10.1016/j.ijsu.2019.12.027
17. Scheyer M, Antonietti E, Rollinger G, Mall H, Arnold S. Doppler-guided hemorrhoidal artery ligation. Am J Surg. (2006) 191(1):89–93. doi: 10.1016/j.amjsurg.2005.10.007
18. Brown SR, Tiernan JP, Watson AJM, Biggs K, Shephard N, Wailoo AJ, et al. Haemorrhoidal artery ligation versus rubber band ligation for the management of symptomatic second-degree and third-degree haemorrhoids (HubBLe): a multicentre, open-label, randomised controlled trial. Lancet. (2016) 388(10042):356–64. doi: 10.1016/S0140-6736(16)30584-0
19. Giordano P, Tomasi I, Pascariello A, Mills E, Elahi S. Transanal dearterialization with targeted mucopexy is effective for advanced haemorrhoids. Colorectal Dis. (2014) 16(5):373–6. doi: 10.1111/codi.12574
20. Elbetti C, Giani I, Novelli E, Fucini C. Martellucci the single pile classification: a new tool for the classification of haemorrhoidal disease and the comparison of treatment results. J Updates Surg. (2015) 67(4):421–6. doi: 10.1007/s13304-015-0333-0
21. Elbetti C, Giani I, Consiglio FM, Novelli E, Santini A. Martellucci tailored excisional treatment for high-grade haemorrhoidal disease. J Updates Surg. (2014) 66(4):283–7. doi: 10.1007/s13304-014-0269-9
22. Vidal V, Louis G, Bartoli JM, Sielezneff I. Embolization of the hemorrhoidal arteries (the emborrhoid technique): a new concept and challenge for interventional radiology. Diagn Interv Imaging. (2014) 95(3):307–15. doi: 10.1016/j.diii.2014.01.016
23. Fathallah N, Beaussier H, Chatellier G, Meyer J, Sapoval M, Moussa N, et al. Proposal for a new score: hemorrhoidal bleeding score. Ann Coloproctol. (2021) 37(5):311–7. doi: 10.3393/ac.2020.08.19
25. Romano FM, Sciaudone G, Canonico S, Selvaggi F, Pellino G. Scoring system for haemorrhoidal disease. Rev Recent Clin Trials. (2021) 16(1):96–100. doi: 10.2174/1574887115666200319162033
26. Caputo RP, Tremmel JA, Rao S, Gilchrist IC, Pyne C, Pancholy S, et al. Transradial arterial access for coronary and peripheral procedures: executive summary by the transradial committee of the SCAI. Catheter Cardiovasc Interv. (2011) 78(6):823–39. doi: 10.1002/ccd.23052
27. Iezzi R, Campenni P, Posa A, Parello A, Rodolfino E, Marra AA, et al. Outpatient transradial emborrhoid technique: a pilot study. Cardiovasc Intervent Radiol. (2021) 44(8):1300–6. doi: 10.1007/s00270-021-02856-8
28. Orth RC, Wallace MJ, Kuo MD, Technology Assessment Committee of the Society of Interventional Radiology. C-arm cone-beam CT: general principles and technical considerations for use in interventional radiology. J Vasc Interv Radiol. (2008) 19(6):814–20. doi: 10.1016/j.jvir.2008.02.002
29. Tradi F, Panneau J, Brige P, Mege D, Habert P, Hak JF, et al. Evaluation of multiple embolic agents for embolization of the superior rectal artery in an animal model. Cardiovasc Intervent Radiol. (2022) 45(4):510–9. doi: 10.1007/s00270-021-03041-7
30. Noori VJ, Eldrup-Jørgensen J. A systematic review of vascular closure devices for femoral artery puncture sites. J Vasc Surg. (2018) 68(3):887–99. doi: 10.1016/j.jvs.2018.05.019
31. Hessel SJ, Adams DF, Abrams HL. Complications of angiography. Radiology. (1981) 138(2):273–81. doi: 10.1148/radiology.138.2.7455105
32. Sun X, Xu J, Zhang J, Jin Y, Chen Q. Management of rectal bleeding due to internal haemorrhoids with arterial embolisation: a single-centre experience and protocol. Clin Radiol. (2018) 73:985.e1–e6. doi: 10.1016/j.crad.2018.07.105
33. Vidal V, Sapoval M, Sielezneff Y, De Parades V, Tradi F, Louis G, et al. Emborrhoid: a new concept for the treatment of hemorrhoids with arterial embolization: the first 14 cases. Cardiovasc Intervent Radiol. (2015) 38(1):72–8. doi: 10.1007/s00270-014-1017-8
34. Tradi F, Louis G, Giorgi R, Mege D, Bartoli JM, Sielezneff I, et al. Embolization of the superior rectal arteries for hemorrhoidal disease: prospective results in 25 patients. J Vasc Interv Radiol. (2018) 29:884–892.e1. doi: 10.1016/j.jvir.2018.01.778
35. Moussa N, Bonnet B, Pereira H, Pechmajou L, Pellerin O, Abed A, et al. Mid-term results of superior rectal artery and coils for hemorrhoidal embolization with particles bleeding. Cardiovasc Intervent Radiol. (2020) 43:1062–9. doi: 10.1007/s00270-020-02441-5
36. Moggia E, Talamo G, Gallo G, Bianco A, Barattini M, Salsano G, et al. Do we have another option to treat bleeding hemorrhoids? The emborrhoid technique: experience in 16 patients. Rev Recent Clin Trials. (2021) 16:81–6. doi: 10.2174/18761038MTA13MjA5x
37. Zakharchenko A, Kaitoukov Y, Vinnik Y, Tradi F, Sapoval M, Sielezneff I, et al. Safety and efficacy of superior rectal artery embolization with particles and metallic coils for the treatment of hemorrhoids (emborrhoid technique). Diagn Interv Imaging. (2016) 97:1079–84. doi: 10.1016/j.diii.2016.08.002
38. Moussa N, Sielezneff I, Sapoval M, Tradi F, Del Giudice C, Fathallah N, et al. Embolization of the superior rectal arteries for chronic bleeding due to haemorrhoidal disease. Colorectal Dis. (2017) 19:194–9. doi: 10.1111/codi.13430
39. Sirakaya M, O’Balogun A, Kassamali RH. Superior rectal artery embolisation for haemorrhoids: what do we know so far? Cardiovasc Intervent Radiol. (2021) 44(5):675–85. doi: 10.1007/s00270-020-02733-w
40. Talaie R, Torkian P, Moghadam AD, Tradi F, Vidal V, Sapoval M, et al. Hemorrhoid embolization: a review of current evidences. Diagn Interv Imaging. (2022) 103(1):3–11. doi: 10.1016/j.diii.2021.07.001
41. Makris GC, Thulasidasan N, Malietzis G, Kontovounisios C, Saibudeen A, Uberoi R, et al. Catheter-directed hemorrhoidal dearterialization technique for the management of hemorrhoids: a meta-analysis of the clinical evidence. J Vasc Interv Radiol. (2021) 32(8):1119–27. doi: 10.1016/j.jvir.2021.03.548
42. Nguyenhuy M, Xu Y, Kok HK, Maingard J, Joglekar S, Jhamb A, et al. Clinical outcomes following rectal artery embolisation for the treatment of internal haemorrhoids: a systematic review and meta-analysis. Cardiovasc Intervent Radiol. (2022) 45(9):1351–61. doi: 10.1007/s00270-022-03154-7
43. Angle JF, Siddiqi NH, Wallace MJ, Kundu S, Stokes L, Wojak JC, et al. Society of interventional radiology standards of practice committee. Quality improvement guidelines for percutaneous transcatheter embolization: society of interventional radiology standards of practice committee. J Vasc Interv Radiol. (2010) 21(10):1479–86. doi: 10.1016/j.jvir.2010.06.014
Keywords: hemorrhoids, embolization, emborrhoid, hemorrhage, radiology, interventional
Citation: Panneau J, Mege D, Di Bisceglie M, Duclos J, Khati I, Vidal V, Gallo G and Tradi F (2025) Hemorrhoidal disease: what role can rectal artery embolization play? Front. Surg. 11:1474799. doi: 10.3389/fsurg.2024.1474799
Received: 2 August 2024; Accepted: 18 December 2024;
Published: 7 January 2025.
Edited by:
Vincent de Parades, Hôpital Saint-Joseph, FranceReviewed by:
Iacopo Giani, Azienda USL Toscana Centro, ItalyZi Qin Ng, Royal Perth Hospital, Australia
Copyright: © 2025 Panneau, Mege, Di Bisceglie, Duclos, Khati, Vidal, Gallo and Tradi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julien Panneau, anVsaWVuLnBhbm5lYXVAYXAtaG0uZnI=
 Julien Panneau
Julien Panneau Diane Mege
Diane Mege Mathieu Di Bisceglie1,2,3
Mathieu Di Bisceglie1,2,3