- 1National Heart and Lung Institute, Faculty of Medicine, Imperial College London, London, United Kingdom
- 2Department of Thoracic Surgery, 424 General Military Hospital, Thessaloniki, Greece
- 3Department of Cardiothoracic Surgery, Hammersmith Hospital, London, United Kingdom
- 4Department of Cardiothoracic Surgery, New York University Langone Health, New York, NY, United States
Interprofessional education, an approach where healthcare professionals from various disciplines learn with, from, and about each other, is widely recognized as an important strategy for improving collaborative practice and patient outcomes. This narrative review explores the current state and future directions of interprofessional education in cardiothoracic surgery. We conducted a literature search using the PubMed, Scopus, and Web of Science databases, focusing on English-language articles published after 2000. Our qualitative synthesis identified key themes related to interprofessional education interventions, outcomes, and challenges. The integration of interprofessional education in cardiothoracic surgery training programs varies across regions, with a common focus on teamwork and interpersonal communication. Simulation-based training has emerged as a leading modality for cultivating these skills in multidisciplinary settings, with studies showing improvements in team performance, crisis management, and patient safety. However, significant hurdles remain, including professional socialization, hierarchies, stereotypes, resistance to role expansion, and logistical constraints. Future efforts in this field should prioritize deeper curricular integration, continuous faculty development, strong leadership support, robust outcome evaluation, and sustained political and financial commitment. The integration of interprofessional education in cardiothoracic surgery offers considerable potential for enhancing patient care quality, but realizing this vision requires a multifaceted approach. This approach must address individual, organizational, and systemic factors to build an evidence-based framework for implementation.
1 Introduction
Interprofessional education is widely acknowledged as a pivotal strategy for developing collaborative practice and improving health outcomes across several medical specialties (1–3). This educational approach, where healthcare professionals from diverse disciplines learn about, from, and with each other, prepares medical practitioners to deliver safe and patient-centered care (4, 5). At its core, interprofessional education aims to dissolve professional barriers, nurture mutual respect, and build cohesive healthcare teams through shared learning experiences (6, 7). Such a model is necessary in today's healthcare landscape, where complex patient needs demand a comprehensive and coordinated approach spanning various health disciplines (8, 9).
Interprofessional education gained momentum after the publication of multiple patient safety studies that highlighted the significance of collaborative practice (10–12). In recent years, policymakers and educational leaders have increasingly advocated for the widespread integration of interprofessional education into medical curricula, emphasizing its potential to improve patient outcomes and satisfaction (13). Prominent international organizations, including the World Health Organization, the World Federation of Medical Education, and the Organization for Economic Co-operation and Development, have proposed strategies to promote interprofessional education in healthcare (5, 14).
In cardiothoracic surgery, the need for interprofessional education is amplified due to the complicated nature of procedures and the multidisciplinary approach required for patient management. Over the past two decades, this specialty has witnessed significant technological advancements, such as robotic surgery and transcatheter techniques. These innovations require an educational framework that not only teaches technical expertise but also cultivates competencies in communication and teamwork (15–19). Furthermore, the rapid evolution of thoracic oncology, with its expanding array of anticancer treatments, necessitates close cooperation between thoracic surgeons and specialists from various disciplines (20–22). Moreover, collaborative competencies are needed to address challenges arising from perioperative care pathways for cardiothoracic surgery patients (23). Interprofessional education can improve professional interactions in these and many other settings involving cardiothoracic surgeons.
While the effectiveness of interprofessional education is well-established in general healthcare settings, its specific outcomes, benefits, and challenges in cardiothoracic surgery remain inadequately explored. This review aims to synthesize available evidence and outline strategies for integrating interprofessional collaboration in cardiothoracic surgery education.
2 Methods
We performed a literature search using the PubMed, Scopus, and Web of Science databases on April 1, 2024. To capture recently published material, we enabled auto-alerts through May 12, 2024. The search strategy included the following keywords: interprofessional education, cardiothoracic surgery, collaborative practice, multidisciplinary team, and surgical education. We limited the results to English-language articles published after 2000, without restrictions on study design. The initial screening process involved reviewing titles and abstracts to exclude articles clearly unrelated to our topic, such as those focusing solely on technical skills. We then obtained and evaluated the full-text versions of the remaining articles. Data from the selected studies were synthesized narratively, with a focus on interprofessional education interventions, outcomes, barriers, and facilitators. As this review did not involve the collection of primary patient data, ethical approval was not necessary. In conducting this literature review, we adhered to the guidelines outlined in the Scale for the Assessment of Narrative Review Articles (24).
3 Status of interprofessional education
Historically, cardiothoracic surgery training has primarily focused on developing the technical skills essential for performing a predefined scope of procedures (25–27). Mastering these skills is demanding given the high precision required for surgical interventions on vital intrathoracic organs. In recent years, the educational landscape of cardiothoracic surgery has undergone a substantial transformation, evolving in response to advances in medical knowledge, technological innovations, and changing societal needs (28, 29). This shift marks the beginning of an endeavor to define an educational framework that addresses not only the requisite technical proficiencies but also the behavioral skills necessary for team-based care.
The curriculum and structure of cardiothoracic surgery training vary widely across different regions and healthcare systems, each adapting to the unique needs of their medical and regulatory environments. As a common denominator, however, there has been a growing interest in non-technical skills. In the United States, the American Board of Medical Specialties and the Accreditation Council for Graduate Medical Education have jointly approved core competencies that provide a framework for important developmental areas. Among these, “interpersonal and communication skills” stands out as a core competency that contains the subcomponent of interprofessional and team communication (30, 31).
The United Kingdom has taken a similar approach to integrating interprofessional education in cardiothoracic surgery training. The country's training framework emphasizes capabilities in practice that are shared across all surgical specialties, with multidisciplinary team management as a key component (32). Moreover, the professional behaviors and competencies assessed during training are aligned with the General Medical Council's “Generic Professional Capabilities Framework” (33). This framework includes interpersonal and communication skills, ensuring that non-technical skills receive appropriate attention throughout the training program.
The European Board of Cardiothoracic Surgery is working towards standardizing training and promoting mutual recognition of qualifications across European Union member states. During assessment, candidates must demonstrate specific professional behaviors, including application of the principles of multidisciplinary and team-based care and selection of effective communication strategies to maintain patient safety and reduce the risk of medical errors (34). The thoracic oncology HERMES (Harmonizing Education in Respiratory Medicine for European Specialists) curriculum exemplifies the integration of interprofessional education in thoracic oncology training (35). This program advocates for the indispensable role of multidisciplinary teams in treating thoracic malignancies by promoting collaborative decision-making processes throughout all stages of cancer care. Various specialists, including thoracic surgeons, medical oncologists, radiation oncologists, and palliative care experts, are expected to seamlessly work together in order to achieve optimal patient outcomes. Interprofessional collaboration is promoted through structured educational activities and is a mandatory requirement for certification.
Numerous institutions worldwide have recognized the importance of early interprofessional education and have implemented programs at the undergraduate level. For instance, the University of British Columbia in Canada has been a pioneer in integrating interprofessional and interdisciplinary education into its health and human service programs over the past few decades (36). In the United Kingdom, interprofessional education is now a standard component in pre-qualifying health and social care courses in at least two-thirds of relevant universities (37). An increasing interest in the integration of interprofessional education in undergraduate medical curricula has also been documented in other countries within the European Higher Education Area, with Germany and Sweden as notable examples (38). These widespread initiatives demonstrate a growing global recognition of the value of early exposure to interprofessional collaboration in medical education. However, it is important to note that despite this progress, significant challenges and limitations continue to exist in the implementation and standardization of these programs across different educational systems and cultural contexts (38, 39).
4 Impact of interprofessional education
Interprofessional education has the potential to improve various aspects of cardiothoracic surgery, from patient care and safety to medical education and research (Table 1). Non-technical skills, such as communication, teamwork and collaboration, are important for the smooth functioning of multidisciplinary teams in complex surgical environments. Surgical teams that exhibit strong social skills have been associated with improved patient outcomes and lower mortality rates (47–49). Conversely, breakdowns in communication and teamwork have been linked to adverse events, preventable errors, and increased mortality rates (50, 51).
Simulation-based interprofessional education is an effective method for teaching these non-technical skills (52, 53). This approach provides a safe and controlled environment where healthcare professionals from different disciplines can collaboratively practice teamwork, communication, and crisis management, without putting patients at risk (54). Importantly, concomitant technical skills training, such as simulating operative procedures, has been shown to significantly improve the acquisition of non-technical competencies (55, 56). This finding supports the notion that technical and non-technical skills are intrinsically linked and should be learned together, reflecting the challenges of real-world clinical settings (57).
The feasibility and effectiveness of interprofessional simulation-based training in the cardiothoracic operating room have been demonstrated by multiple studies. Bierer et al. (40) described the development and implementation of an inexpensive, in situ simulation model for training non-technical skills in managing an intraoperative airway crisis following pneumonectomy. This simulation scenario brought together participants from surgery, anesthesia, and nursing, creating an environment that closely resembled real-world operating room dynamics. Evaluations using validated instruments, such as Non-Technical Skills for Surgeons (58) and TeamSTEPPS2 (59), confirmed the model's construct validity by distinguishing non-technical skill levels between consultant surgeons and surgical trainees. Furthermore, the simulation revealed potential latent safety threats, including missing equipment and knowledge gaps regarding team members’ roles during a crisis. Participant feedback via the Method Material Member Overall questionnaire corroborated the high fidelity and educational value of the simulation experience. The success of this immersive, low-cost model shows its potential as a readily adoptable approach for institutions with limited simulation resources. It can empower thoracic surgery trainees to refine their non-technical skills while proactively identifying and addressing system vulnerabilities to improve patient safety practices.
In a similar study from the field of cardiac surgery, Merritt-Genore et al. (41) developed high-fidelity simulation events that replicated critical steps and potential crises during cardiopulmonary bypass. The study involved participants from various disciplines, including cardiothoracic surgeons, anesthesiologists, and perfusionists. These scenarios were designed to promote team communication, familiarize participants with uncommon but high-stakes events, and increase confidence in managing such situations. The results showed a significant improvement in participants’ self-confidence when handling scenarios of iatrogenic dissection and emergent return to cardiopulmonary bypass. Additionally, subjective observations and participant feedback indicated an overall positive impact on team dynamics, understanding of multidisciplinary perspectives, and performance during simulated crises. By exposing participants to realistic, high-risk scenarios and rotating them through unfamiliar roles, the simulation facilitated the development of non-technical skills necessary in the cardiac operating room. This approach addresses the need for effective teamwork in settings where lapses can rapidly lead to severe adverse events.
Simulation-based training can also serve as a tool to equip operating room teams with the required skills for navigating the challenges posed by the adoption of novel surgical technologies. Minimally invasive thoracic surgery has been shown to improve patient outcomes compared with open surgical approaches (60). However, these advancements introduce challenges in coordinating personnel and technology, alter situational awareness, and create potential pitfalls (61). A retrospective analysis of patient safety incidents in the French national thoracic surgery database from 2008 to 2019 revealed that 65.6% of 407 events related to minimally invasive surgery were attributed to human factors (62). These incidents originated from the interplay between individuals, their tasks, and the workplace environment. This statistic illustrates the urgent need for continuous professional development and error management training within interprofessional frameworks that improve team dynamics and operational safety (63, 64).
Baste et al. (42) developed a simulation-based crisis training program utilizing realistic models of catastrophic events specific to minimally invasive thoracic surgery. Their hybrid model, featuring medium-to-high fidelity, immersed participants in stressful scenarios encountered during robotic and video-assisted thoracic surgery, such as uncontrolled bleeding and contralateral tension pneumothorax. The simulation underwent rigorous evaluation through debriefing sessions and an independent audit focusing on human factors. Positive feedback from team members and the program's demonstrable impact on patient safety and team performance suggest its significant value. Consequently, the authors advocate for the integration of team simulation training and crisis resource management into a continuous educational program for professionals in minimally invasive thoracic surgery.
Interprofessional crisis simulations have also shown value as educational tools in critical care settings. Burkhart et al. (43) developed and evaluated a clinical simulation program that trained cardiothoracic surgery residents in the principles and practical application of post-cardiotomy extracorporeal membrane oxygenation (ECMO). The two-day course, designed and facilitated by a multidisciplinary faculty including surgeons, anesthesiologists, and perfusionists, combined didactic lectures with hands-on simulation. The results indicated significant improvements in residents’ confidence, knowledge, and crisis management skills related to ECMO. Specifically, the residents’ ability to accurately identify ECMO components increased from 40% before training to 69% after the course. Additionally, their proficiency in managing simulated crisis scenarios, such as arterial desaturation and hypertension, showed substantial improvement. Overall, this multidisciplinary approach addressed key cognitive and behavioral competencies for ECMO management among cardiothoracic surgery residents.
Kemper et al. (44) employed a modified Delphi method to identify and reach consensus on crisis scenarios suitable for simulation-based, nontechnical skills training in cardiac surgery teams. The researchers surveyed 114 experts from various disciplines, including cardiac surgeons, anesthesiologists, perfusionists, and operating room nurses, identifying 13 highly relevant crisis scenarios for interprofessional simulation training. These scenarios included a range of critical events, such as cardiopulmonary bypass failure, emergency sternotomy, cardiac resuscitation, and massive bleeding. The study's strength lies in its inclusive approach, incorporating insights from all cardiac surgery team members. Each profession contributes unique perspectives on crisis situations based on their specific roles. Thus, interprofessional consensus is imperative for developing valid and clinically applicable scenarios for simulation-based curricula in cardiac surgery.
Interprofessional education can play a significant role in the successful implementation of enhanced recovery after thoracic surgery (ERATS) pathways. ERATS protocols have been shown to reduce postoperative complications, shorten hospital stays, decrease costs, and improve patient-reported outcomes (65). Meyenfeldt et al. (45) investigated the determinants for an ERATS pathway for Dutch lung cancer patients by conducting semi-structured interviews with a wide range of stakeholders. These included general thoracic and cardiothoracic surgeons, anesthesiologists, pulmonary physicians, nurses, healthcare managers, patient representatives, an electronic medical record specialist, and a healthcare insurance company representative. The findings indicate the importance of a clear and concise multidisciplinary protocol in ensuring consistent care delivery across the involved specialties. Other key facilitators included leadership from a senior clinician and support from an ERATS coordinator. In contrast, inconsistent communication was found to have a negative impact. Interestingly, providing patients with consistent information and involving them in decision-making processes were also identified as important factors for the successful application of the ERATS protocol. Interprofessional education, by fostering clear communication among diverse healthcare professionals, promoting leadership and coordination skills, and prioritizing patient-centered care, can significantly contribute to the effective implementation and success of ERATS pathways (66–68).
Integrating interprofessional education in cardiothoracic surgery has yielded benefits not only in residency programs but also in preparing medical students for collaborative healthcare environments. Allen et al. (46) implemented a structured program to introduce first-year medical students to cardiothoracic surgery and laboratory research. This three-part, eight-week program comprised shadowing a cardiothoracic surgeon in the outpatient clinic and operating room, participating in large-animal operations in the laboratory, and completing a clinical research project under the guidance of a laboratory resident and faculty mentor. The program resulted in significant academic output, with 18 participants producing 39 peer-reviewed manuscripts. Furthermore, it influenced 80% of the eligible students to pursue surgical specialties, including cardiothoracic surgery, for their residency. This program's outcomes suggest the potential benefits of early interprofessional experiences in cardiothoracic surgery education, aligning with current trends that advocate for early exposure to multidisciplinary roles in preparing students for the collaborative nature of modern healthcare (69, 70).
5 Implementing interprofessional education: challenges and strategies
Despite the well-documented benefits of interprofessional education in cardiothoracic surgery, its implementation remains challenging. Most obstacles arise from the complex nature of the specialty, deeply ingrained professional norms, and unique dynamics within surgical teams. Successfully integrating interprofessional education in training programs requires a systematic approach to identifying and addressing these challenges (Table 2).
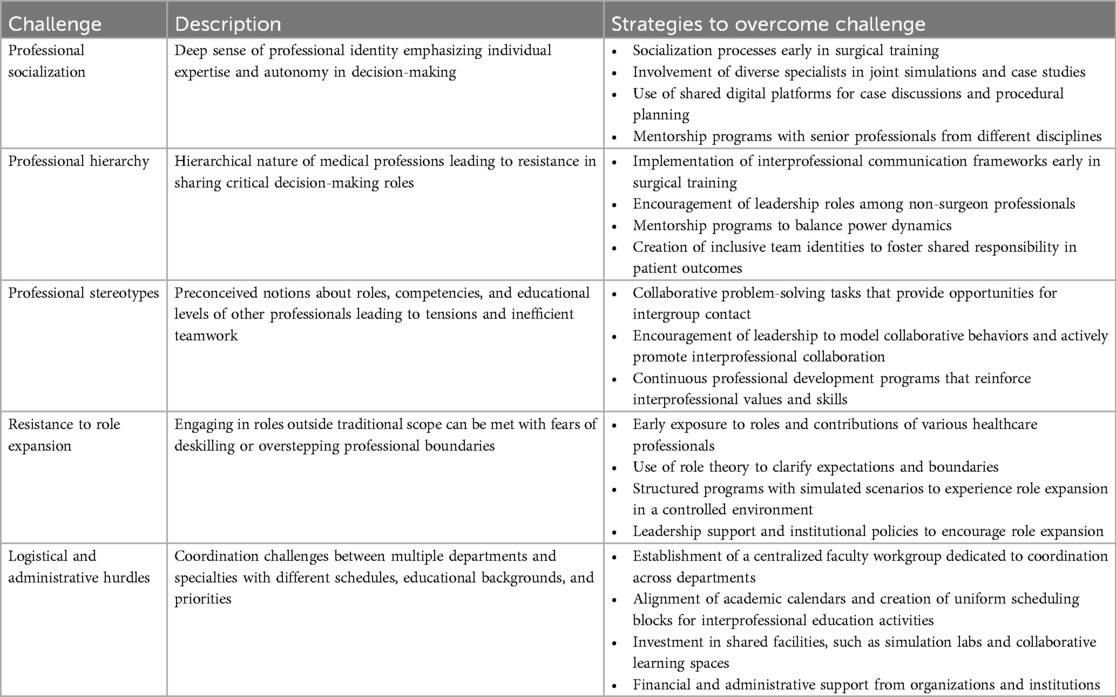
Table 2. Challenges and strategies in implementing interprofessional education in cardiothoracic surgery.
5.1 Professional socialization
Professional socialization may present a significant barrier to implementing interprofessional collaboration, particularly in specialized fields like cardiothoracic surgery. This process involves the induction of new members into the norms, values, behaviors, and social knowledge of a profession (71, 72). For cardiothoracic surgeons, this often translates into a deeply ingrained sense of professional identity shaped through many years of highly specialized training (73). The intense focus on technical proficiency, individual expertise, and independent decision-making instilled during training reinforces a culture where collaborative practice may be perceived as a challenge to the cardiothoracic surgeon's authority or an encroachment on their autonomy. Modifying this entrenched professional identity is a critical first step in developing an environment where interprofessional collaboration is normalized and valued.
Socialization processes should begin early in medical education and surgical training. Many cardiothoracic surgery training programs are characterized by isolation, as evidenced by the physical separation of educational spaces and minimal cross-professional engagements. Altering this segregated educational model would encourage early exposure to and appreciation of the roles of various healthcare professionals (74). Involving physicians, nurses, and allied health professionals in joint simulations and case studies can help cardiothoracic surgeons learn to communicate effectively across disciplines, understand the scope of each team member's knowledge, and apply this collaborative approach to clinical settings. Additionally, shared digital platforms that facilitate case discussions and procedural planning between different specialties could support such interprofessional education efforts (75). Mentorship programs pairing cardiothoracic surgery residents with senior healthcare professionals from different disciplines can further promote interprofessional socialization. These mentors can model collaborative behaviors and demonstrate the value of interdisciplinary input in clinical decision-making (76, 77). Moreover, continuous professional development opportunities focusing on interprofessional collaboration should be offered throughout residency programs. Workshops, seminars, and interprofessional rounds can reinforce the importance of teamwork and provide ongoing support for collaborative practice. Ideally, interprofessional education initiatives should be introduced as early as medical school, laying the foundation for effective teamwork and communication strategies throughout a physician's career.
5.2 Professional hierarchy
The hierarchical nature of healthcare professions, where certain disciplines and specialties are viewed as more prestigious than others, hinders collaborative practices (78, 79). Surgeons are traditionally positioned at the top of this hierarchy, potentially fostering a culture where the knowledge and skills of other team members are undervalued (80, 81). In cardiothoracic surgery, this dynamic can be pronounced due to the complex procedures and critical nature of the diseases involved, which often necessitate rapid, decisive actions that may reinforce hierarchical decision-making. This environment can create considerable barriers to integrating other healthcare and administrative team members in planning and execution phases.
Addressing these hierarchical disparities requires cultural shifts within teams to value equally each member's contributions and promote shared responsibility in patient outcomes. Interprofessional communication frameworks aimed at reducing socio-hierarchical gaps should be introduced early in the education and training process. For example, the “TRI-O” guide of interprofessional communication skills, which emphasizes openness for collaboration, information, and discussion, has been shown to help undergraduate medical, nursing, and health nutrition students initiate partnership-based communication and mutual collaboration (82). Encouraging leadership roles among non-surgeon healthcare professionals and implementing mentorship programs can further balance power dynamics (83). Moreover, creating inclusive identities within cardiothoracic surgery teams can help all members view themselves as part of a larger, cohesive unit rather than separate, hierarchical entities. This can be achieved by emphasizing the value of each profession's contribution to patient care and integrating this perspective in the training and daily operations of the clinical team (84). Institutions should support these initiatives by embedding interprofessional collaboration in their culture and mission statements.
5.3 Professional stereotypes
Professional stereotypes further complicate interactions among diverse healthcare teams. For instance, surgeons and nurses often hold preconceived notions about each other's roles, competencies, and educational levels, which can lead to tensions and inefficient teamwork (85, 86). These stereotypes are typically formed during early educational experiences and are reinforced throughout professional practice (72). In cardiothoracic surgery, where stakes and stress levels are exceptionally high, professional stereotypes can severely disrupt the collaborative atmosphere needed to ensure patient safety and optimal outcomes. Surgeons might view nurses and allied health professionals merely as assistants rather than as integral contributors who can offer valuable insights into patient care.
Interprofessional education can dismantle these stereotypes by encouraging shared experiences and mutual learning. Educational programs should provide cardiothoracic surgery trainees with opportunities for contact with other healthcare professionals to overcome prejudice, invalidate negative attitudes, and foster favorable opinions toward other professions (87, 88). Collaborative problem-solving tasks can promote such intergroup contact, thereby reducing professional stereotypes (84). Leadership support is also important in this context; leaders should actively promote interprofessional education to help shift cultural norms and reduce resistance to change (86). Continuous professional development programs that provide practical training in interprofessional skills are valuable tools to sustain these efforts.
5.4 Resistance to role expansion
Interprofessional education often requires professionals to engage in roles that may traditionally fall outside their scope. This approach may involve surgeons participating in nursing tasks and vice versa, to foster a better understanding of each other's roles and develop mutual respect (89). However, such role expansion can be met with resistance due to fears of deskilling or overstepping professional boundaries (86). In cardiothoracic surgery, where tasks demand precision and specialization, this blending of roles can be challenging. Cardiothoracic surgeons may fear that engaging in traditionally nursing-centric tasks could dilute their specialized skills or undermine their authority in the multidisciplinary team. Conversely, nurses might be reluctant to perform surgical tasks or make decisions typically reserved for surgeons, fearing errors and legal repercussions (90).
Overcoming resistance to role expansion requires addressing concerns about deskilling and overstepping professional boundaries. One effective method is the use of role theory to help professionals understand and negotiate their roles within a team (91, 92). By clarifying role expectations and boundaries, healthcare professionals can better appreciate their colleagues’ contributions without feeling that their own skills are being undermined (93). Interprofessional education programs that include simulated scenarios can help cardiothoracic surgery trainees experience role expansion in a controlled and supportive environment (94, 95). These programs should be structured to demonstrate how role flexibility can improve patient outcomes (96). Furthermore, cardiothoracic surgeons should be encouraged to view role expansion as an opportunity for professional growth rather than a threat. Leadership support and institutional policies can play a significant role in promoting this perspective.
5.5 Logistical and administrative hurdles
Organizing interprofessional education initiatives in cardiothoracic surgery presents significant logistical and administrative challenges. Successful implementation of joint educational sessions requires coordination between multiple departments that operate on varying schedules and have different educational backgrounds and priorities. Moreover, cardiothoracic surgery involves lengthy procedures that demand precise timing and availability of various specialists, complicating the integration of interprofessional education into routine training timelines. Beyond scheduling, logistical hurdles may include allocating spaces that can accommodate multidisciplinary teams and providing resources, such as appropriately equipped simulation labs (97).
Overcoming these logistical and administrative challenges requires strong institutional leadership, organizational support, and strategic planning. Coordination across departments can be facilitated by the establishment of a dedicated, adequately resourced, centralized faculty workgroup (98). This workgroup should include representatives from cardiothoracic surgery, anesthesia, nursing, and other relevant disciplines to ensure integration of all perspectives into the planning process. Furthermore, aligning academic calendars and creating uniform scheduling blocks specifically for interprofessional education activities can mitigate the difficulties posed by different schedules among disciplines (99). Investment in shared facilities, such as simulation labs and collaborative learning spaces, can address spatial challenges by providing dedicated venues for interprofessional education (98). To sustain these efforts, institutions should provide ongoing logistical, administrative, and financial support.
6 Discussion
Deep integration of interprofessional education in cardiothoracic surgery presents significant challenges but holds considerable potential to improve patient care, reshape professional relationships, and transform the overall culture of this specialty. Successful implementation, however, requires careful consideration of individual, organizational, and systemic factors. By examining the current landscape and emerging trends, we can better understand how the future of cardiothoracic surgery may be influenced by our ability to navigate this educational evolution.
Redesigning cardiothoracic surgery curricula with a greater emphasis on interprofessional education necessitates significant revisions to current training programs. These changes must extend beyond simply adding new content; they require a paradigm shift in how we conceptualize surgical education. Future programs must seamlessly integrate interprofessional competencies throughout, recognizing them as core components of professional certification rather than optional add-ons. This goal can be achieved through structured programs that combine various training and educational approaches, while offering diverse professional perspectives on patient care. It is paramount that these new pedagogical elements preserve the depth of specialized knowledge that cardiothoracic surgeons must possess.
This path to integration may require approval from multiple accreditation bodies and licensure organizations, especially in countries where a central regulatory authority is lacking or has diminished power (100, 101). The unique requirements and expectations of each profession's governing body can make alignment a delicate and time-consuming process (102). Success depends on close collaboration among these agencies to develop a harmonized framework that supports interprofessional education while maintaining the rigorous standards of each specialty.
Concrete and measurable interprofessional education outcomes will provide accreditation bodies with a strong mandate to endorse and sustain these programs. However, current metrics for interprofessional education often fall short, failing to capture subtle improvements in team dynamics and patient outcomes (103). In cardiothoracic surgery, where outcomes are closely linked to patient survival and quality of life, developing specific indicators that accurately reflect the effectiveness of interprofessional collaboration is crucial. These indicators should incorporate reliable and valid tools for measuring team functionality and performance. Furthermore, they must assess tangible impacts on patient care, such as recovery times, postoperative morbidity rates, and patient satisfaction. When selecting, developing, and validating evaluation tools for interprofessional education programs in cardiothoracic surgery, it is crucial to consider the specific learning objectives, the stage of learners’ professional development, and the contextual factors of the surgical environment.
Building on the need for robust evaluation of interprofessional collaboration initiatives, several validated tools have been developed and adapted for use in healthcare education settings. Among these, the Attitudes Toward Health Care Teams Scale (ATHCTS) has shown promise for evaluating interprofessional teamwork attitudes. Depending on the specific model, the ATHCTS may consist of various subscales, including quality of care (delivery), time constraints, physician centrality, team efficiency, and patient-centered care (104–106). It has shown acceptable to good internal consistency for its subscales and has been validated with both undergraduate and graduate healthcare students (107). Another widely used measure for assessing interprofessional education is the Readiness for Interprofessional Learning Scale (RIPLS) (108–111). However, recent critiques have highlighted psychometric concerns with the RIPLS, including issues with its factor structure and internal consistency, suggesting careful consideration of its use (112). The Interdisciplinary Education Perception Scale (IEPS) was identified as the most frequently used outcome measure in a systematic review assessing the efficacy of interprofessional education activities during student clinical placements (113). The IEPS assesses perceptions of interprofessional collaboration through four subscales: competency and autonomy, perceived need for cooperation, perception of actual cooperation, and understanding of others’ roles (114). This scale has demonstrated good psychometric properties, with Cronbach's alpha values generally exceeding 0.80 and test-retest weighted kappa values ranging from fair to moderate across its various subscales (115–119). This instrument could potentially be adapted to address the specific needs of cardiothoracic surgery. A validated, specialty-specific tool could enable precise and meaningful assessment of interprofessional education initiatives, thereby contributing to the development of evidence-based practices.
The success of interprofessional education in cardiothoracic surgery also hinges on the ability of clinical and educational supervisors to facilitate this new approach. Faculty development should aim to equip instructors with the skills necessary for interprofessional education, including conflict resolution and collaborative leadership (97, 120, 121). Additionally, educators must learn to create learning environments that authentically reflect the high-pressure and time-sensitive scenarios that are common in the field. By leveraging experiential learning and interactive teaching methods, interprofessional competencies can be readily integrated into the intensive technical training that characterizes cardiothoracic surgery (122, 123).
As faculty members advance to leadership roles, it is important that they actively promote interprofessional education practices as a priority within their institutions (89). This requires a proactive approach to overcome resistance stemming from traditional practices that favor professional boundaries in cardiothoracic surgery. Leaders should not only provide opportunities for interprofessional learning but also drive cultural shifts toward more collaborative practices. They must also engage influential stakeholders to secure the necessary resources for these initiatives (81). For example, administrators and managers who determine educational policies and control resources can implement changes in course structures, provide faculty support through academic incentives, and allocate funding to operate interprofessional education budgets (124–126).
Political and financial support at the government level can also create essential incentives for organizations to prioritize interprofessional education activities (127). Policies should encourage the adoption of interprofessional education by embedding it within accreditation standards and professional development requirements for cardiothoracic surgeons. Additionally, the procurement and maintenance of financial support for interprofessional education initiatives should be based on realistic budgets and detailed business plans (126, 128). For instance, funding could be allocated for developing interprofessional simulation centers that provide practical experience in a multiprofessional setting. Sharing these simulation centers and other resources, such as administrative support, can help reduce costs and ensure the long-term sustainability of interprofessional education initiatives.
Simulation centers undoubtedly offer valuable training opportunities; however, their effectiveness in interprofessional education depends on careful scenario design and facilitation. Scenarios that deliberately incorporate role ambiguity or conflicting priorities among team members can stimulate rich discussions about professional boundaries and collaborative decision-making. Additionally, involving patients or patient advocates in the design and execution of simulations can provide unique insights into team dynamics from the patient's perspective (129). This approach not only improves the realism of scenarios but also reinforces patient-centered care principles (130).
Complementing simulation-based approaches, artificial intelligence (AI) and machine learning are emerging as valuable tools in improving nontechnical skills and interprofessional education (131). AI-powered platforms can analyze team interactions during simulated scenarios, providing objective feedback on communication patterns, leadership dynamics, and decision-making processes (132). Machine learning algorithms can process complex team performance data to identify effective collaboration strategies and areas for improvement in interprofessional settings. These technologies may also facilitate adaptive learning experiences, automatically adjusting scenario difficulty based on team performance to optimize learning outcomes (133). However, integrating AI and machine learning into interprofessional education faces several challenges. These include ensuring that AI-based assessments capture the nuances of human interactions, avoiding the reinforcement of biases in team dynamics and maintaining the authenticity of interpersonal skill development. Additionally, the high cost and technical expertise required for implementation may limit widespread adoption, particularly in resource-constrained settings.
While the role of interprofessional education is usually discussed within the context of training and accreditation, it is worth considering its influence on the hiring process for cardiothoracic surgeons. Traditional job interviews often fall short in evaluating a candidate's ability to work effectively in interprofessional teams (134). In response, some institutions have implemented simulated interprofessional scenarios or team-based interviews into their recruitment process. These methods aim to gauge a candidate's collaborative competencies and their potential to contribute to a culture of interprofessional practice. However, it is important to recognize that these initial assessments are just a starting point. The complex and evolving nature of cardiothoracic surgery demands continuous interprofessional education throughout a surgeon's career to refine and adapt these essential collaborative skills.
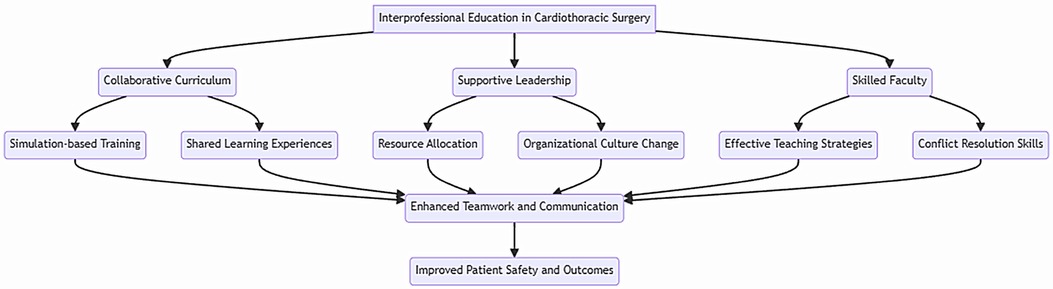
This narrative review possesses certain strengths. First, it is one of the first comprehensive examinations on interprofessional education in cardiothoracic surgery, providing an overview of existing practices, outcomes, and future directions. By synthesizing evidence from a wide range of sources, this review offers a broad perspective and a conceptual framework for interprofessional education in cardiothoracic surgery (Figure 1). Second, it provides practical insights into strategies for successful implementation, such as the use of high-fidelity simulation and the development of interprofessional outcome measures. Third, the review identifies key gaps in the literature and suggests directions for future research. This can guide the development of more rigorous and targeted studies to evaluate the effectiveness of interprofessional education interventions in cardiothoracic surgery. Finally, the timeliness and relevance of this review are significant. With an increasing emphasis on collaborative practice and patient-centered care, interprofessional education has become a critical component of modern surgical training. As such, this review is likely to be of interest to a wide range of stakeholders, including educators, clinicians, researchers, and policymakers.
Despite its strengths, this literature review has several limitations that should be acknowledged. As a narrative review, it lacks the methodological rigor of a systematic review. The literature search was not exhaustive, and the selection of studies was not based on strict criteria. Consequently, relevant studies may have been overlooked, and the review may be subject to selection bias. Furthermore, the quality of the included studies was not formally assessed, limiting the ability to draw firm conclusions based on their findings. Another limitation is the paucity of high-quality studies investigating interprofessional education in cardiothoracic surgery. Most of the included studies were descriptive and had small sample sizes, reflecting the relative infancy of research in this area. Moreover, the included studies exhibited substantial heterogeneity in terms of intervention types, study populations, and outcome measures. This heterogeneity makes it challenging to compare results across studies and draw generalizable conclusions. Additionally, the included studies were conducted in high-income countries, particularly in North America and Europe. This geographical bias limits the applicability of the findings to other healthcare settings, especially in low- and middle-income countries, where the challenges to implementing interprofessional education may differ significantly. Finally, this review did not explore the cost-effectiveness of interprofessional education interventions. Given the resource-intensive nature of some of these interventions, such as high-fidelity simulation training, it is important to consider their financial implications and whether the benefits justify the costs. Future studies should include economic evaluations to guide decision-making about the allocation of resources for interprofessional education in cardiothoracic surgery.
7 Conclusions
Interprofessional education holds great promise for improving patient outcomes and professional satisfaction in cardiothoracic surgery. Realizing this potential necessitates extensive curricular reforms, faculty development initiatives, strong leadership support, and sustained political and financial commitment. Furthermore, ongoing research is warranted to develop validated assessment tools and standardized outcome measures that will enable the evaluation and continuous improvement of interprofessional education programs across different healthcare contexts. By addressing these key areas, the field of cardiothoracic surgery can make significant progress toward harnessing the full benefits of interprofessional education, ultimately improving patient care quality and outcomes.
Author contributions
SL: Conceptualization, Writing – original draft, Writing – review & editing. MS: Writing – original draft, Writing – review & editing. RC: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the review was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zechariah S, Ansa BE, Johnson SW, Gates AM, Leo GD. Interprofessional education and collaboration in healthcare: an exploratory study of the perspectives of medical students in the United States. Healthcare (Basel). (2019) 7:117. doi: 10.3390/healthcare7040117
2. Buring SM, Bhushan A, Broeseker A, Conway S, Duncan-Hewitt W, Hansen L, et al. Interprofessional education: definitions, student competencies, and guidelines for implementation. Am J Pharm Educ. (2009) 73:59. doi: 10.5688/aj730459
3. Barnsteiner JH, Disch JM, Hall L, Mayer D, Moore SM. Promoting interprofessional education. Nurs Outlook. (2007) 55:144–50. doi: 10.1016/j.outlook.2007.03.003
4. Iobst WF, Sherbino J, Cate OT, Richardson DL, Dath D, Swing SR, et al. Competency-based medical education in postgraduate medical education. Med Teach. (2010) 32:651–6. doi: 10.3109/0142159X.2010.500709
5. World Health Organization. Framework for action on interprofessional education and collaborative practice (2010). Available online at: https://iris.who.int/handle/10665/70185 (Accessed April 12, 2024).
6. Reeves S. Why we need interprofessional education to improve the delivery of safe and effective care. Interface—Comun Saúde Educ. (2016) 20:185–97. doi: 10.1590/1807-57622014.0092
7. Jackson A, Bluteau MP. Interprofessional education, collaborative practice and primary care. InnovAiT. (2011) 4:230–5. doi: 10.1093/innovait/inq166
8. Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update). Cochrane Database Syst Rev. (2013) 2013:CD002213. doi: 10.1002/14651858.CD002213.pub3
9. Thistlethwaite J. Interprofessional education: a review of context, learning and the research agenda. Med Educ. (2012) 46:58–70. doi: 10.1111/j.1365-2923.2011.04143.x
10. Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ. (2004) 170:1678–86. doi: 10.1503/cmaj.1040498
11. Institute of Medicine (US) Committee on Quality of Health Care in America. “Executive summary”. In: Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press (US) (2000). p. 17–25.
12. Wilson RM, Runciman WB, Gibberd RW, Harrison BT, Newby L, Hamilton JD. The quality in Australian health care study. Med J Aust. (1995) 163:458–71. doi: 10.5694/j.1326-5377.1995.tb124691.x
13. Committee on Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes; Board on Global Health; Institute of Medicine. Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes. Washington (DC): National Academies Press (US) (2015). p. 19–20.
14. Oandasan I, Reeves S. Key elements for interprofessional education. Part 1: the learner, the educator and the learning context. J Interprof Care. (2005) 19(Suppl 1):21–38. doi: 10.1080/13561820500083550
15. Servais EL, Blasberg JD, Brown LM, Towe CW, Seder CW, Onaitis MW, et al. The society of thoracic surgeons general thoracic surgery database: 2022 update on outcomes and research. Ann Thorac Surg. (2023) 115:43–9. doi: 10.1016/j.athoracsur.2022.10.025
16. Kalogeropoulos AS, Redwood SR, Allen CJ, Hurrell H, Chehab O, Rajani R, et al. A 20-year journey in transcatheter aortic valve implantation: evolution to current eminence. Front Cardiovasc Med. (2022) 9:971762. doi: 10.3389/fcvm.2022.971762 eCollection 2022.36479570
17. Coccia M. Evolution of technology in replacement of heart valves: transcatheter aortic valves, a revolution for management of valvular heart diseases. Health Policy Technol. (2021) 10:100512. doi: 10.1016/j.hlpt.2021.100512
18. Zirafa CC, Romano G, Key TH, Davini F, Melfi F. The evolution of robotic thoracic surgery. Ann Cardiothorac Surg. (2019) 8:210–7. doi: 10.21037/acs.2019.03.03
19. Wong MKH, Sit AKY, Au TWK. Minimally invasive thoracic surgery: beyond surgical access. J Thorac Dis. (2018) 10:S1884–91. doi: 10.21037/jtd.2018.05.196
20. Stinchcombe TE, Bradley JD. Thoracic oncology: current standard therapy and future developments. J Clin Oncol. (2022) 40:527–9. doi: 10.1200/JCO.21.02396
21. van Geffen WH, Blum TG, Aliberti S, Blyth KG, Bostantzoglou C, Farr A, et al. Continuous professional development: elevating thoracic oncology education in Europe. Breathe (Sheff). (2019) 15:279–85. doi: 10.1183/20734735.0296-2019
22. Soo RA, Stone ECA, Cummings KM, Jett JR, Field JK, Groen HJM, et al. Scientific advances in thoracic oncology 2016. J Thorac Oncol. (2017) 12:1183–209. doi: 10.1016/j.jtho.2017.05.019
23. Harrison TG, Ronksley PE, James MT, Brindle ME, Ruzycki SM, Graham MM, et al. The perioperative surgical home, enhanced recovery after surgery and how integration of these models may improve care for medically complex patients. Can J Surg. (2021) 64:E381–90. doi: 10.1503/cjs.002020
24. Baethge C, Goldbeck-Wood S, Mertens S. SANRA-a scale for the quality assessment of narrative review articles. Res Integr Peer Rev. (2019) 4:5. doi: 10.1186/s41073-019-0064-8
25. Crawford FA Jr. Thoracic surgery education–past, present, and future. Ann Thorac Surg. (2005) 79:S2232–2237. doi: 10.1016/j.athoracsur.2005.02.077
26. Crawford FA Jr. Thoracic surgery education. Ann Thorac Surg. (2000) 69:330–3. doi: 10.1016/s0003-4975(99)01473-3
27. Ellis FH. Education of the thoracic surgeon. Thorax. (1980) 35:405–14. doi: 10.1136/thx.35.6.405
28. Verrier ED. Joint council on thoracic surgical education: an investment in our future. J Thorac Cardiovasc Surg. (2011) 141:318–21. doi: 10.1016/j.jtcvs.2010.10.013
29. Chitwood WR, Spray TL, Feins RH, Mack MJ. Mission critical: thoracic surgery education reform. J Thorac Cardiovasc Surg. (2008) 136:812–3. doi: 10.1016/j.jtcvs.2008.08.012
30. Mitzman B, Beller JP, Edgar L. Thoracic surgery milestones 2.0: rationale and revision. J Thorac Cardiovasc Surg. (2020) 160:1399–404. doi: 10.1016/j.jtcvs.2019.12.132
31. Yang SC, Merrill W. Educational milestone development in phase II specialties: thoracic surgery. J Grad Med Educ. (2014) 6:329–31. doi: 10.4300/JGME-06-01s1-14
32. Shah R, Jahangiri M, Goodwin A, Barnard S, Moorjani N. Cardiothoracic Surgery Curriculum (2021). Available online at: https://www.iscp.ac.uk/media/1108/cardiothoracic-surgery-curriculum-aug-2021-approved-oct-20.pdf (Accessed April 14, 2024).
33. General Medical Council. Generic professional capabilities framework (2017). Available online at: https://www.gmc-uk.org/-/media/documents/generic-professional-capabilities-framework–2109_pdf-70417127.pdf (Accessed April 14, 2024).
34. European Board of Cardiothoracic Surgery. European Board of Cardiothoracic Surgery Syllabus (2017). Available online at: https://www.ebcts.org/syllabus (Accessed April 14, 2024).
35. Gamarra F, Noël JL, Brunelli A, Dingemans AC, Felip E, Gaga M, et al. Thoracic oncology HERMES: european curriculum recommendations for training in thoracic oncology. Breathe (Sheff). (2016) 12:249–55. doi: 10.1183/20734735.009116
36. Charles G, Bainbridge L, Gilbert J. The university of British Columbia model of interprofessional education. J Interprof Care. (2010) 24:9–18. doi: 10.3109/13561820903294549
37. Cornes M. Review of interprofessional education in the United Kingdom (1997–2013). J Interprof Care. (2015) 29:85. doi: 10.3109/13561820.2014.981479
38. Colonnello V, Kinoshita Y, Yoshida N, Bustos Villalobos I. Undergraduate interprofessional education in the European higher education area: a systematic review. Int Med Educ. (2023) 2:100–12. doi: 10.3390/ime2020010
39. Lash DB, Barnett MJ, Parekh N, Shieh A, Louie MC, Tang TT. Perceived benefits and challenges of interprofessional education based on a multidisciplinary faculty member survey. Am J Pharm Educ. (2014) 78:180. doi: 10.5688/ajpe7810180
40. Bierer J, Memu E, Leeper WR, Fortin D, Fréchette E, Inculet R, et al. Development of an in situ thoracic surgery crisis simulation focused on nontechnical skill training. Ann Thorac Surg. (2018) 106:287–92. doi: 10.1016/j.athoracsur.2018.01.058
41. Merritt-Genore H, Adams A, Zavala R, Brakke T. Interprofessional simulation in cardiothoracic surgery improves team confidence. J Extra Corpor Technol. (2022) 54:250–4. doi: 10.1182/ject-250-254
42. Baste JM, Bottet B, Selim J, Sarsam M, Lefevre-Scelles A, Dusseaux MM, et al. Implementation of simulation-based crisis training in robotic thoracic surgery: how to improve safety and performance? J Thorac Dis. (2021) 13:S26–34. doi: 10.21037/jtd-2020-epts-03
43. Burkhart HM, Riley JB, Lynch JJ, Suri RM, Greason KL, Joyce LD, et al. Simulation-based postcardiotomy extracorporeal membrane oxygenation crisis training for thoracic surgery residents. Ann Thorac Surg. (2013) 95:901–6. doi: 10.1016/j.athoracsur.2012.12.015
44. Kemper T, van Haperen M, Eberl S, Winkelman T, van Deventer SM, Waller E, et al. Crisis scenarios for simulation-based nontechnical skills training for cardiac surgery teams: a national survey among cardiac anesthesiologists, cardiac surgeons, clinical perfusionists, and cardiac operating room nurses. Simul Healthc. (2023) 18:367–74. doi: 10.1097/SIH.0000000000000715
45. Meyenfeldt EMV, van Nassau F, de Betue CTI, Barberio L, Schreurs WH, Marres GMH, et al. Implementing an enhanced recovery after thoracic surgery programme in The Netherlands: a qualitative study investigating facilitators and barriers for implementation. BMJ Open. (2022) 12:e051513. doi: 10.1136/bmjopen-2021-051513
46. Allen JG, Weiss ES, Patel ND, Alejo DE, Fitton TP, Williams JA, et al. Inspiring medical students to pursue surgical careers: outcomes from our cardiothoracic surgery research program. Ann Thorac Surg. (2009) 87:1816–9. doi: 10.1016/j.athoracsur.2009.03.007
47. Neily J, Mills PD, Young-Xu Y, Carney BT, West P, Berger DH, et al. Association between implementation of a medical team training program and surgical mortality. JAMA. (2010) 304:1693–700. doi: 10.1001/jama.2010.1506
48. Catchpole K, Mishra A, Handa A, McCulloch P. Teamwork and error in the operating room: analysis of skills and roles. Ann Surg. (2008) 247:699–706. doi: 10.1097/SLA.0b013e3181642ec8
49. Young GJ, Charns MP, Daley J, Forbes MG, Henderson W, Khuri SF. Best practices for managing surgical services: the role of coordination. Health Care Manage Rev. (1997) 22:72–81. doi: 10.1097/00004010-199710000-00010
50. Christian CK, Gustafson ML, Roth EM, Sheridan TB, Gandhi TK, Dwyer K, et al. A prospective study of patient safety in the operating room. Surgery. (2006) 139:159–73. doi: 10.1016/j.surg.2005.07.037
51. Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. (2004) 13(Suppl 1):i85–90. doi: 10.1136/qhc.13.suppl_1.i85
52. Arriaga AF, Gawande AA, Raemer DB, Jones DB, Smink DS, Weinstock P, et al. Pilot testing of a model for insurer-driven, large-scale multicenter simulation training for operating room teams. Ann Surg. (2014) 259:403–10. doi: 10.1097/SLA.0000000000000342
53. Paige JT, Kozmenko V, Yang T, Gururaja RP, Hilton CW, Cohn I, et al. Attitudinal changes resulting from repetitive training of operating room personnel using of high-fidelity simulation at the point of care. Am Surg. (2009) 75:584–90. doi: 10.1177/000313480907500709
54. Knudson MM, Khaw L, Bullard MK, Dicker R, Cohen MJ, Staudenmayer K, et al. Trauma training in simulation: translating skills from SIM time to real time. J Trauma. (2008) 64:255–63. doi: 10.1097/TA.0b013e31816275b0
55. Sparks JL, Crouch DL, Sobba K, Evans D, Zhang J, Johnson JE, et al. Association of a surgical task during training with team skill acquisition among surgical residents: the missing piece in multidisciplinary team training. JAMA Surg. (2017) 152:818–25. doi: 10.1001/jamasurg.2017.1085
56. Black SA, Nestel DF, Kneebone RL, Wolfe JHN. Assessment of surgical competence at carotid endarterectomy under local anaesthesia in a simulated operating theatre. Br J Surg. (2010) 97:511–6. doi: 10.1002/bjs.6938
57. Steinemann S, Berg B, Skinner A, DiTulio A, Anzelon K, Terada K, et al. In situ, multidisciplinary, simulation-based teamwork training improves early trauma care. J Surg Educ. (2011) 68:472–7. doi: 10.1016/j.jsurg.2011.05.009
58. Yule S, Flin R, Paterson-Brown S, Maran N, Rowley D. Development of a rating system for surgeons’ non-technical skills. Med Educ. (2006) 40:1098–104. doi: 10.1111/j.1365-2929.2006.02610.x
59. Parker AL, Forsythe LL, Kohlmorgen IK. TeamSTEPPS®: an evidence-based approach to reduce clinical errors threatening safety in outpatient settings: an integrative review. J Healthc Risk Manag. (2019) 38:19–31. doi: 10.1002/jhrm.21352
60. Baiu I. Video- vs robotic-assisted thoracic surgery-the race for resource utilization. JAMA Netw Open. (2024) 7:e248854. doi: 10.1001/jamanetworkopen.2024.8854
61. Catchpole K, Bisantz A, Hallbeck MS, Weigl M, Randell R, Kossack M, et al. Human factors in robotic assisted surgery: lessons from studies ‘in the wild.’. Appl Ergon. (2019) 78:270–6. doi: 10.1016/j.apergo.2018.02.011
62. Bottet B, Rivera C, Dahan M, Falcoz PE, Jaillard S, Baste JM, et al. Reporting of patient safety incidents in minimally invasive thoracic surgery: a national registered thoracic surgeons experience for improvement of patient safety. Interact Cardiovasc Thorac Surg. (2022) 35:ivac129. doi: 10.1093/icvts/ivac129
63. Buljac-Samardzic M, Doekhie KD, Van Wijngaarden JDH. Interventions to improve team effectiveness within health care: a systematic review of the past decade. Hum Resour Health. (2020) 18:2. doi: 10.1186/s12960-019-0411-3
64. Lown BA, Kryworuchko J, Bieber C, Lillie DM, Kelly C, Berger B, et al. Continuing professional development for interprofessional teams supporting patients in healthcare decision making. J Interprof Care. (2011) 25:401–8. doi: 10.3109/13561820.2011.583563
65. Medbery RL, Fernandez FG, Khullar OV. ERAS And patient reported outcomes in thoracic surgery: a review of current data. J Thorac Dis. (2019) 11:S976–86. doi: 10.21037/jtd.2019.04.08
66. Gantayet-Mathur A, Chan K, Kalluri M. Patient-centered care and interprofessional collaboration in medical resident education: where we stand and where we need to go. Humanit Soc Sci Commun. (2022) 9:1–24. doi: 10.1057/s41599-022-01221-5
67. Mohammed CA, Anand R, Saleena Ummer V. Interprofessional education (IPE): a framework for introducing teamwork and collaboration in health professions curriculum. Med J Armed Forces India. (2021) 77:S16–21. doi: 10.1016/j.mjafi.2021.01.012
68. van Diggele C, Roberts C, Burgess A, Mellis C. Interprofessional education: tips for design and implementation. BMC Med Educ. (2020) 20:455. doi: 10.1186/s12909-020-02286-z
69. Caverzagie KJ, Nousiainen MT, Ferguson PC, Ten Cate O, Ross S, Harris KA, et al. Overarching challenges to the implementation of competency-based medical education. Med Teach. (2017) 39:588–93. doi: 10.1080/0142159X.2017.1315075
70. Thibault GE. Reforming health professions education will require culture change and closer ties between classroom and practice. Health Aff Proj Hope. (2013) 32:1928–32. doi: 10.1377/hlthaff.2013.0827
71. Mandy A, Milton C, Mandy P. Professional stereotyping and interprofessional education. Learn Health Soc Care. (2004) 3:154–70. doi: 10.1111/j.1473-6861.2004.00072.x
72. Carpenter J. Doctors and nurses: stereotypes and stereotype change in interprofessional education. J Interprof Care. (1995) 9:151–61. doi: 10.3109/13561829509047849
73. Salvatore D, Numerato D, Fattore G. Physicians’ professional autonomy and their organizational identification with their hospital. BMC Health Serv Res. (2018) 18:775. doi: 10.1186/s12913-018-3582-z
74. Joynes VCT. Defining and understanding the relationship between professional identity and interprofessional responsibility: implications for educating health and social care students. Adv Health Sci Educ Theory Pract. (2018) 23:133–49. doi: 10.1007/s10459-017-9778-x
75. Grosser J, Bientzle M, Kimmerle J. A literature review on the foundations and potentials of digital teaching scenarios for interprofessional health care education. Int J Environ Res Public Health. (2020) 17:3410. doi: 10.3390/ijerph17103410
76. Mandane B, Nakum S, Thandi J, Jasina J. 17 Interprofessional mentoring: the key towards a better multidisciplinary team working model? BMJ Lead. (2020) 4:A6–7. doi: 10.1136/leader-2020-FMLM.17
77. Lait J, Suter E, Arthur N, Deutschlander S. Interprofessional mentoring: enhancing students’ clinical learning. Nurse Educ Pract. (2011) 11:211–5. doi: 10.1016/j.nepr.2010.10.005
78. Braam A, Buljac-Samardzic M, Hilders CGJM, van Wijngaarden JDH. Collaboration between physicians from different medical specialties in hospital settings: a systematic review. J Multidiscip Healthc. (2022) 15:2277–300. doi: 10.2147/JMDH.S376927
79. Hindhede AL, Larsen K. Prestige hierarchies and relations of dominance among health professionals. Prof Prof. (2020) 10:e3447. doi: 10.7577/pp.3447
80. Essex R, Kennedy J, Miller D, Jameson J. A scoping review exploring the impact and negotiation of hierarchy in healthcare organisations. Nurs Inq. (2023) 30:e12571. doi: 10.1111/nin.12571
81. Hammick M, Freeth D, Koppel I, Reeves S, Barr H. A best evidence systematic review of interprofessional education: BEME guide no. 9. Med Teach. (2007) 29:735–51. doi: 10.1080/01421590701682576
82. Claramita M, Riskiyana R, Susilo AP, Huriyati E, Wahyuningsih MSH, Norcini JJ. Interprofessional communication in a socio-hierarchical culture: development of the TRI-O guide. J Multidiscip Healthc. (2019) 12:191–204. doi: 10.2147/JMDH.S196873
83. Bornman J, Louw B. Leadership development strategies in interprofessional healthcare collaboration: a rapid review. J Healthc Leadersh. (2023) 15:175–92. doi: 10.2147/JHL.S405983
84. Kauff M, Bührmann T, Gölz F, Simon L, Lüers G, van Kampen S, et al. Teaching interprofessional collaboration among future healthcare professionals. Front Psychol. (2023) 14:1185730. doi: 10.3389/fpsyg.2023.1185730
85. Kvarnström S. Difficulties in collaboration: a critical incident study of interprofessional healthcare teamwork. J Interprof Care. (2008) 22:191–203. doi: 10.1080/13561820701760600
86. Hall P. Interprofessional teamwork: professional cultures as barriers. J Interprof Care. (2005) 19:188–96. doi: 10.1080/13561820500081745
87. Carpenter J, Dickinson C. Understanding interprofessional education as an intergroup encounter: the use of contact theory in programme planning. J Interprof Care. (2016) 30:103–8. doi: 10.3109/13561820.2015
88. Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. J Pers Soc Psychol. (2006) 90:751–83. doi: 10.1037/0022-3514.90.5.751
89. D'Amour D, Oandasan I. Interprofessionality as the field of interprofessional practice and interprofessional education: an emerging concept. J Interprof Care. (2005) 19(Suppl 1):8–20. doi: 10.1080/13561820500081604
90. DeKeyser Ganz F, Berkovitz K. Surgical nurses’ perceptions of ethical dilemmas, moral distress and quality of care. J Adv Nurs. (2012) 68:1516–25. doi: 10.1111/j.1365-2648.2011.05897.x
91. Michalec B, Hafferty FW. Role theory and the practice of interprofessional education: a critical appraisal and a call to sociologists. Soc Theory Health. (2015) 13:180–201. doi: 10.1057/sth.2015.2
92. Walker PH, Baldwin D, Fitzpatrick JJ, Ryan S, Bulger R, DeBasio N, et al. Building community: developing skills for interprofessional health professions education and relationship-centered care. J Am Acad Nurse Pract. (1997) 9:413–8. doi: 10.1111/j.1745-7599.1997.tb01027.x
93. Rodrigues da Silva Noll Gonçalves J, Gonçalves R N, da Rosa SV, Schaia Rocha Orsi J, Santos de Paula KM, Moysés SJ, et al. Potentialities and limitations of interprofessional education during graduation: a systematic review and thematic synthesis of qualitative studies. BMC Med Educ. (2023) 23:236. doi: 10.1186/s12909-023-04211-6
94. Vatn L, Dahl BM. Interprofessional collaboration between nurses and doctors for treating patients in surgical wards. J Interprof Care. (2022) 36:186–94. doi: 10.1080/13561820.2021.1890703
95. Verd-Aulí X, Maqueda-Palau M, Miró-Bonet M. Interprofessional collaboration in joint clinical sessions in an intensive care unit: perceptions of nurses and physicians. Enferm Intensiva (Engl Ed. (2021) 32:3–10. doi: 10.1016/j.enfi.2020.02.004
96. Collette AE, Wann K, Nevin ML, Rique K, Tarrant G, Hickey LA, et al. An exploration of nurse-physician perceptions of collaborative behaviour. J Interprof Care. (2017) 31:470–8. doi: 10.1080/13561820.2017
97. Brandt B, Lutfiyya MN, King JA, Chioreso C. A scoping review of interprofessional collaborative practice and education using the lens of the triple aim. J Interprof Care. (2014) 28:393–9. doi: 10.3109/13561820.2014.906391
98. Mladenovic J, Tilden VP. Strategies for overcoming barriers to IPE at a health sciences university. J Interprofessional Educ Pract. (2017) 8:10–3. doi: 10.1016/j.xjep.2017.05.002
99. Li JTS, Chau JPC, Wong SYS, Lau ASN, Chan WCH, Yip PPS, et al. Interprofessional education—situations of a university in Hong Kong and major hurdles to teachers and students. Front Educ. (2022) 7:653738. doi: 10.3389/feduc.2022.653738
100. Akdemir N, Peterson LN, Campbell CM, Scheele F. Evaluation of continuous quality improvement in accreditation for medical education. BMC Med Educ. (2020) 20:308. doi: 10.1186/s12909-020-02124-2
101. Nicklin W, Fortune T, van Ostenberg P, O'Connor E, McCauley N. Leveraging the full value and impact of accreditation. Int J Qual Health Care. (2017) 29:310–2. doi: 10.1093/intqhc/mzx010
102. Al-Eyd G, Achike F, Agarwal M, Atamna H, Atapattu DN, Castro L, et al. Curriculum mapping as a tool to facilitate curriculum development: a new school of medicine experience. BMC Med Educ. (2018) 18:185. doi: 10.1186/s12909-018-1289-9
103. Gilbert JH, Yan J, Hoffman SJ. A WHO report: framework for action on interprofessional education and collaborative practice. J Allied Health. (2010) 39(Suppl 1):196–7.21174039
104. Hayashi T, Shinozaki H, Makino T, Ogawara H, Asakawa Y, Iwasaki K, et al. Changes in attitudes toward interprofessional health care teams and education in the first- and third-year undergraduate students. J Interprof Care. (2012) 26:100–7. doi: 10.3109/13561820.2011.644355
105. Curran VR, Sharpe D, Forristall J, Flynn K. Attitudes of health sciences students towards interprofessional teamwork and education. Learn Health Soc Care. (2008) 7:146–56. doi: 10.1111/j.1473-6861.2008.00184.x
106. Heinemann GD, Schmitt MH, Farrell MP, Brallier SA. Development of an attitudes toward health care teams scale. Eval Health Prof. (1999) 22:123–42. doi: 10.1177/01632789922034202
107. Kim K, Ko J. Attitudes toward interprofessional health care teams scale: a confirmatory factor analysis. J Interprof Care. (2014) 28:149–54. doi: 10.3109/13561820.2013.857645
108. Baxter SK. Perspectives and practice: speech and language therapy student views of an interprofessional learning experience. Learn Health Soc Care. (2004) 3:102–10. doi: 10.1111/j.1473-6861.2004.00065.x
109. Hind M, Norman I, Cooper S, Gill E, Hilton R, Judd P, et al. Interprofessional perceptions of health care students. J Interprof Care. (2003) 17:21–34. doi: 10.1080/1356182021000044120
110. Horsburgh M, Lamdin R, Williamson E. Multiprofessional learning: the attitudes of medical, nursing and pharmacy students to shared learning. Med Educ. (2001) 35:876–83. doi: 10.1046/j.1365-2923.2001.00959.x
111. Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med Educ. (1999) 33:95–100. doi: 10.1046/j.1365-2923.1999.00298.x
112. Mahler C, Berger S, Reeves S. The readiness for interprofessional learning scale (RIPLS): a problematic evaluative scale for the interprofessional field. J Interprof Care. (2015) 29:289–91. doi: 10.3109/13561820.2015.1059652
113. Guitar NA, Connelly DM. A systematic review of the outcome measures used to evaluate interprofessional learning by health care professional students during clinical experiences. Eval Health Prof. (2021) 44:293–311. doi: 10.1177/0163278720978814
114. Luecht RM, Madsen MK, Taugher MP, Petterson BJ. Assessing professional perceptions: design and validation of an interdisciplinary education perception scale. J Allied Health. (1990) 19:181–91.2365636
115. McFadyen AK, Maclaren WM, Webster VS. The interdisciplinary education perception scale (IEPS): an alternative remodelled sub-scale structure and its reliability. J Interprof Care. (2007) 21:433–43. doi: 10.1080/13561820701352531
116. Mu K, Chao CC, Jensen GM, Royeen CB. Effects of interprofessional rural training on students’ perceptions of interprofessional health care services. J Allied Health. (2004) 33:125–31.15239410
117. Hawk C, Buckwalter K, Byrd L, Cigelman S, Dorfman L, Ferguson K. Health professions students’ perceptions of interprofessional relationships. Acad Med. (2002) 77:354–7. doi: 10.1097/00001888-200204000-00020
118. Hawk C, Byrd L, Killinger LZ. Evaluation of a geriatrics course emphasizing interdisciplinary issues for chiropractic students. J Gerontol Nurs. (2001) 27:6–12. doi: 10.3928/0098-9134-20010701-07
119. Hayward KS, Powell LT, McRoberts J. Changes in student perceptions of interdisciplinary practice in the rural setting. J Allied Health. (1996) 25:315–27.9119733
120. Ratka A, Zorek JA, Meyer SM. Overview of faculty development programs for interprofessional education. Am J Pharm Educ. (2017) 81:96. doi: 10.5688/ajpe81596
121. Anderson L, Hean S, O’Halloran C, Pitt R, Hammick M. Faculty development for interprofessional education and practice. In: Steinert Y, editor. Faculty Development in the Health Professions. Dordrecht: Springer (2014). p. 287–310.
122. Babin C, Salem Y, Quiben M, Davis B. Interprofessional education (IPE) faculty development—a scoping review. Health Interprof. Pract. Educ. (2023) 5:1–26. doi: 10.61406/hipe.269
123. Silver IL, Leslie K. Faculty development for continuing interprofessional education and collaborative practice. J Contin Educ Health Prof. (2017) 37:262–7. doi: 10.1097/CEH.0000000000000178
124. Folkman AK, Tveit B, Sverdrup S. Leadership in interprofessional collaboration in health care. J Multidiscip Healthc. (2019) 12:97–107. doi: 10.2147/JMDH.S189199
125. Alghamdi H, Breitbach A. Governance of interprofessional education and collaborative practice. In: Alnaami MY, Alqahtani DA, Alfaris EA, Abdulghani HM, Mohammed CA, editors. Novel Health Interprofessional Education and Collaborative Practice Program: Strategy and Implementation. Singapore: Springer (2023). p. 125–44.
126. Girard MA. Interprofessional education and collaborative practice policies and law: an international review and reflective questions. Hum Resour Health. (2021) 19:9. doi: 10.1186/s12960-020-00549-w
127. Oandasan I, Reeves S. Key elements of interprofessional education. Part 2: factors, processes and outcomes. J Interprof Care. (2005) 19:39–48. doi: 10.1080/13561820500081703
128. Fahs DB, Honan L, Gonzalez-Colaso R, Colson ER. Interprofessional education development: not for the faint of heart. Adv Med Educ Pract. (2017) 8:329–36. doi: 10.2147/AMEP.S133426
129. Kneebone R, Weldon SM, Bello F. Engaging patients and clinicians through simulation: rebalancing the dynamics of care. Adv Simul (Lond). (2016) 1:19. doi: 10.1186/s41077-016-0019-9
130. Snow R. “Real patient participation in simulation”. In: Nestel D, Bearman M, editors. Simulated Patient Methodology: Theory, Evidence and Practice. Chichester, UK: John Wiley & Sons (2014). p. 103–9.
131. Lomis K, Jeffries P, Palatta A, Sage M, Sheikh J, Sheperis C, et al. Artificial intelligence for health professions educators. NAM Perspect. (2021) 2021:10.31478/202109a. doi: 10.31478/202109a
132. Connolly C, Hernon O, Carr P, Worlikar H, McCabe I, Doran J, et al. Artificial intelligence in interprofessional healthcare practice education—insights from the home health project, an exemplar for change. Comput Sch. (2023) 40:412–29. doi: 10.1080/07380569.2023.2247393
133. Liaw SY, Tan JZ, Lim S, Zhou W, Yap J, Ratan R, et al. Artificial intelligence in virtual reality simulation for interprofessional communication training: mixed method study. Nurse Educ Today. (2023) 122:105718. doi: 10.1016/j.nedt.2023.105718
Keywords: cardiothoracic surgery, curriculum, interprofessional collaboration, interprofessional education, multidisciplinary team, simulation, surgical education
Citation: Lampridis S, Scarci M and Cerfolio RJ (2024) Interprofessional education in cardiothoracic surgery: a narrative review. Front. Surg. 11:1467940. doi: 10.3389/fsurg.2024.1467940
Received: 21 July 2024; Accepted: 21 August 2024;
Published: 4 September 2024.
Edited by:
Luca Bertolaccini, European Institute of Oncology (IEO), ItalyReviewed by:
Mohamed Rahouma, NewYork-Presbyterian, United StatesMehmet Oğuzhan Özyurtkan, Medicana International İstanbul Hospital, Türkiye
Ahmed G. Elkhouly, Tanta University, Egypt
Filipe Azenha, University of Lucerne, Switzerland
Alessio Campisi, Integrated University Hospital Verona, Italy
Copyright: © 2024 Lampridis, Scarci and Cerfolio. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Savvas Lampridis, c2F2dmFzLmxhbXByaWRpc0Bkb2N0b3JzLm9yZy51aw==
 Savvas Lampridis
Savvas Lampridis Marco Scarci
Marco Scarci Robert J. Cerfolio
Robert J. Cerfolio