- Department of Plastic and Reconstructive Surgery, Nanfang Hospital, Southern Medical University, Guangzhou, China
Background: The application of autologous fat transplantation in facial lesions of patients with localized scleroderma (LoS) has been reported in recent years.
Objective: The authors report a case of worsening of active localized scleroderma after autologous fat transplantation.
Methods: A man presented with neck and facial skin atrophy and pigmentation with a history of LoS. Appearing 1.5 years ago, the lesion had progressively grown in size and shape. Consent was obtained after the patient was informed of the possible surgical risks during the active phase of the disease. He underwent autologous fat grafting into the right cheek with about 30 ml Coleman fat graft.
Results: Skin dyspigmentation and atrophy progressively deteriorated 1 month into therapy, with slightly increased erythema and enlargement of the lesion. Six months after the therapy, the localized scleroderma-related score worsened.
Limitations: There are different factors, such as that systemic medications could affect the treatment of localized scleroderma by autologous fat transplantation. Meanwhile, considering the limitation of the 6-month follow-up period, obtaining long-term follow-up data is necessary to evaluate sustained outcomes and potential complications.
Conclusion: More clinical research is needed to determine the time interval between disease inactivity and the application of any surgical procedures to avoid reactivation.
Introduction
Local scleroderma (LoS) is a rare disease of unknown etiology without satisfactory treatment for skin sclerosis and soft-tissue atrophy. Recent studies have shown the benefits of autologous fat grafting (AFG) in the treatment of skin fibrotic disorders and soft-tissue defects (1). However, the timing of fat grafting is still controversial. Development of scleroderma includes initial inflammatory (active) and late (inactive) stages. The typically active stage is characterized by recurring patches or plaques of extensive erythema and edema, while the inactive phase is characterized by hard plaques, resulting in dermal and subcutaneous soft-tissue atrophy and skin pigmentation (2). Early intervention during the active phase of the disease can control and delay the progression of the disease. The therapeutic goal at an early inflammatory stage is to suppress disease activity (3). Adipose-derived stem cells (ASCs) in the fat graft attenuate inflammation of sclerotic skin after transplantation (4). Our previous non-randomized controlled trial showed that sequential fat grafting is safe and effective in patients with stable LoS (5). However, according to European guidelines for LoS, trauma from surgery may serve as a triggering factor for the exacerbation or reactivation of LoS, and thus should be carefully considered (6).
Case report
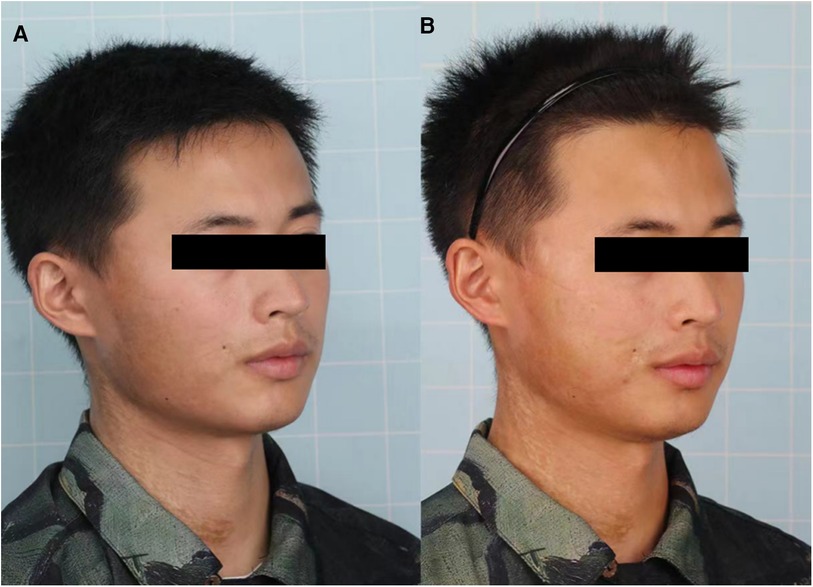
A 25-year-old man diagnosed with LoS presented to our department for the treatment of dyspigmentation and atrophy of the skin on the right side of his cheek and neck (Figures 1A, 2A). Appearing 1.5 years earlier, the lesion had progressively grown in size with dyspigmentation, accompanied by atrophy, erythema, and stiffening of the skin. Together, these results supported a diagnosis of the active stage of LoS. We obtained consent after informing the patient of the possible risks of surgery during the active phase of the disease. A total of 30 ml lipoaspirates was injected beneath the skin lesion. After fat grating, better facial symmetry was achieved since the volume loss was recovered by fat grafts. However, skin dyspigmentation and erythema progressively deteriorated 1 month after surgery, with enlargement of the lesion. Six months after surgery, his modified Localized Scleroderma Skin Severity Index (mLoSSI) score increased from 9 to 10, and the Localized Scleroderma Skin Damage Index (LoSDI) score increased from 7 to 12, compared with before surgery (Figures 1B, 2B), which indicated disease progression. The patient didn't receive any topical treatment or systemic medication throughout.
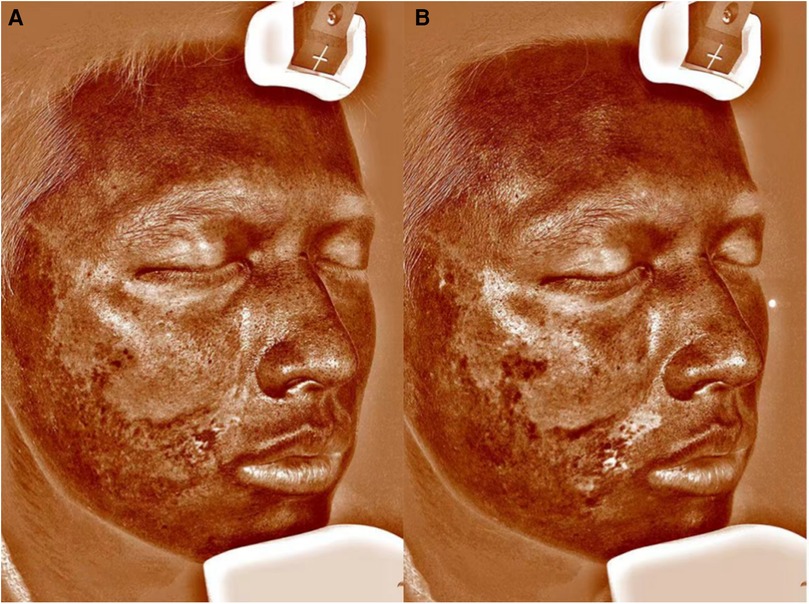
Figure 2. VISIA images before (A) and 6 months after autologous fat grafting (B). VISIA skin analyzer is a facial skin analysis system.
Discussion
Short-term hyperpigmentation is one of the few adverse events we observed in patients with active LoS receiving AFG, which spontaneously remits within 2 months. However, persisting dyspigmentation and enlarged lesion size 6 months after surgery suggest disease progression. Although LoS is usually self-limited, with frequent spontaneous regressions within 3–5 years, recurrence rates are high, even after many years of inactivity (3). In 2023, Wang and Long (7) reported a case suggesting that AFG in patients with stable scleroderma may lead to disease reignition. Disease reignition or progression could prolong the resolution time of disease activity signs and may affect the final effect of disease treatment.
In the latest European guidelines for LoS (S2k guideline) (8), it is suggested considering autologous fat stem cell transplantation for correcting soft-tissue defects in the head area in cases of linear LoS, which could be performed during the inactive or active phases of LoS and under systemic therapy (>75% consensus). It is worth noting that in the practice guidelines of diagnosis and treatment in China (9), surgery is not considered to be a cure for the disease, nor the primary method of treating the inflammatory aspects. Nevertheless surgical interventions such as fat transfer and flap reconstruction are best suited to ameliorating the sequelae of maculopathy, including visual impairment, and dysfunction in patients with inactive stage.
Moreover, topical or systemic medications may be required for the active stage of morphea. For example, the literature acknowledges PDRN could reduce disease activity and damage in quiescent localized scleroderma (10). In fact, we found no consensus on the optimal timing of intervention and/or accompanying systemic medications for AFG. Thus, after the disease has been stabilized through medication, fat grafting may offer a more effective treatment approach.
Conclusion
The authors believe that more clinical research is needed to determine the time interval between disease inactivity and the application of any surgical procedures to avoid reactivation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SH: Writing – original draft, Writing – review & editing. JL: Writing – original draft, Writing – review & editing. FL: Project administration, Writing – review & editing. JC: Methodology, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
The authors certify that written consent has been obtained from the patient for publication of identifiable patient photographs with the understanding that this information may be publicly available. We thank the patient for granting permission to publish this information.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AFG, autologous fat grafting; ASCs, adipose-derived stem cells; mLoSSI, modified Localized Scleroderma Skin Severity Index; LoSDI, Localized Scleroderma Skin Damage Index.
References
1. Creadore A, Watchmaker J, Maymone MBC, Pappas L, Lam C, Vashi NA. Cosmetic treatment in patients with autoimmune connective tissue diseases: best practices for patients with morphea/systemic sclerosis. J Am Acad Dermatol. (2020) 83:315–41. doi: 10.1016/j.jaad.2019.12.081
2. Abbas L, Joseph A, Kunzler E, Jacobe HT. Morphea: progress to date and the road ahead. Ann Transl Med. (2021) 9:437. doi: 10.21037/atm-20-6222
3. Albuquerque JV, Andriolo BN, Vasconcellos MR, Civile VT, Lyddiatt A, Trevisani VF. Interventions for morphea. Cochrane Database Syst Rev. (2019) 7:CD005027. doi: 10.1002/14651858.CD005027.pub5
4. Jiang W, Wang J, Lin J, Jiang S, Quan Y, Liao Y, et al. Adipose-derived stem cell-enriched lipotransfer reverses skin sclerosis by suppressing dermal inflammation. Plast Reconstr Surg. (2022) 150:578–87. doi: 10.1097/prs.0000000000009435
5. Liu J, Wang J, Zhang Q, Lu F, Cai J. Clinical, histologic, and transcriptomic evaluation of sequential fat grafting for morphea: a nonrandomized controlled trial. JAMA Dermatol. (2024) 160:425–33. doi: 10.1001/jamadermatol.2023.5908
6. Knobler R, Moinzadeh P, Hunzelmann N, Kreuter A, Cozzio A, Mouthon L, et al. European dermatology forum S1-guideline on the diagnosis and treatment of sclerosing diseases of the skin, part 1: localized scleroderma, systemic sclerosis and overlap syndromes. J Eur Acad Dermatol Venereol. (2017) 31:1401–24. doi: 10.1111/jdv.14458
7. Wang HC, Long X. The reactivation of scleroderma after autologous fat grafting. J Craniofac Surg. (2023) 34:e708–10. doi: 10.1097/scs.0000000000009614
8. Kreuter A, Moinzadeh P, Kinberger M, Horneff G, Worm M, Werner RN, et al. S2k guideline: diagnosis and therapy of localized scleroderma. J Dtsch Dermatol Ges. (2024) 22:605–20. doi: 10.1111/ddg.15328
9. Jacobe H. [Morphea (localized scleroderma) in adults: management]. (2024). Available online at: https://www.uptodate.cn/contents/zh-Hans/morphea-localized-scleroderma-in-adults-management (Accessed March 5, 2024).
Keywords: autologous fat grafting, morphea, localized scleroderma, active stage, pigmentary
Citation: Han S, Liu J, Lu F and Cai J (2024) Case Report: Exacerbation after fat grafting in patients with active localized scleroderma. Front. Surg. 11:1457593. doi: 10.3389/fsurg.2024.1457593
Received: 1 July 2024; Accepted: 8 August 2024;
Published: 23 August 2024.
Edited by:
Biao Cheng, General Hospital of Southern Theater Command of PLA, ChinaReviewed by:
Maurizio Romagnuolo, IRCCS Ca’ Granda Foundation Maggiore Policlinico Hospital, ItalyXiao Long, Peking Union Medical College Hospital (CAMS), China
Copyright: © 2024 Han, Liu, Lu and Cai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Lu, NDA2NjA0MjkzQHFxLmNvbQ==; Junrong Cai, ZHJqdW5yb25nY2FpQG91dGxvb2suY29t
†These authors have contributed equally to this work and share first authorship
 Shunxin Han
Shunxin Han Juzi Liu†
Juzi Liu† Junrong Cai
Junrong Cai