- 1Department of Sports Medicine Center, Nagasaki University Hospital, Nagasaki, Japan
- 2Department of Orthopaedic Surgery, Graduate School of Biomedical Sciences, Nagasaki University, Nagasaki, Japan
- 3Department of Orthopaedic Surgery, Jikei Hospital, Isahaya, Japan
- 4Clinical Research Center, Nagasaki University Hospital, Nagasaki, Japan
Background: Fatty infiltration (FI) of rotator cuff muscles in patients with rotator cuff tears is an important imaging factor for determining surgical indications. However, the associations between FI grade and the size or location of adjacent rotator cuff tears are not well-known. This study aimed to primarily determine whether tear size and location, especially for the SSc tendon, are associated with FI of adjacent rotator cuff muscles. The secondary aim was to clarify which patient factors are associated with rotator cuff muscle FI in rotator cuff tear cases.
Methods: This study examined 373 shoulders of 348 patients (264 males and 109 females; mean age of 62.8 years) who underwent arthroscopic rotator cuff surgery. The FI grades of the supraspinatus (SSP), infraspinatus (ISP), and subscapularis (SSc) muscles were assessed using preoperative magnetic resonance imaging (MRI) using the Goutallier classification modified by Fuchs. According to the preoperative MRI and intraoperative findings, the tear size of the posterior–superior rotator cuff (SSP–ISP) was classified using a modified six-grade scale of the Cofield classification, and that of the SSc tear was classified using a six-grade scale according to the Lafosse classification. Age at surgery, sex, body mass index (BMI), presence of diabetes mellitus (DM) or hyperlipidemia (HL), trauma history, and duration of symptoms were investigated.
Results: The FI grades of the SSP, ISP, and SSc were significantly associated with the size of the tears in those muscles (all P < 0.01). Furthermore, the FI grades of the SSP and the ISP were significantly associated with SSc tear size (P < 0.01), and the FI grade of the SSc was significantly associated with SSP–ISP tear size (P < 0.01). Patient age at surgery was significantly associated with FI grade (P < 0.01), with significant progression of the FI grade with advancing age. However, there were no significant associations between the FI grade and sex, BMI, presence of DM or HL, trauma history, and duration of symptoms.
Conclusions: The FI grade of each of the rotator cuff muscles is affected by not only the tear severity of the muscle concerned but also by the severity of any tear in the adjacent rotator cuff.
Background
The use of preoperative magnetic resonance imaging (MRI) to assess fatty infiltration (FI) and muscle atrophy of the rotator cuff muscles is important in surgical planning for rotator cuff tears, and the most widely used FI assessment method is the Goutallier classification modified by Fuchs using MRI (1–4). Progression is thought to be affected by several different factors, of which the relationship with rotator cuff tear size in particular has been widely reported (5–7). Supraspinatus (SSP) tendon injury is the most common form of rotator cuff tear, and it is thought that, as the tear widens, the damage extends to the infraspinatus (ISP) tendon and the subscapularis (SSc) tendon. FI of the rotator cuff muscles has been shown to progress as the tear enlarges (8).
In recent years, the attachments of the rotator cuff muscles have been the subject of in-depth anatomical studies (9, 10) that have identified the anatomical importance of the anterior–superior part. It is expected that disruption of the anterior–superior rotator cuff attachment affects muscle FI in both SSc and SSP over time. In clinical settings, there have been cases in which FI of the SSP and ISP muscles was more advanced than expected or cases in which it was better than expected, when compared with the status of the torn tendon based on the medical history and preoperative MRI (Figures 1A, 2A). The relationship between the FI of each muscle and anterior–superior tear size, especially in SSc tendon tears, has not yet been clarified. We hypothesized that in such cases, the progression of the SSc tear affects muscle FI of the adjacent rotator cuff.
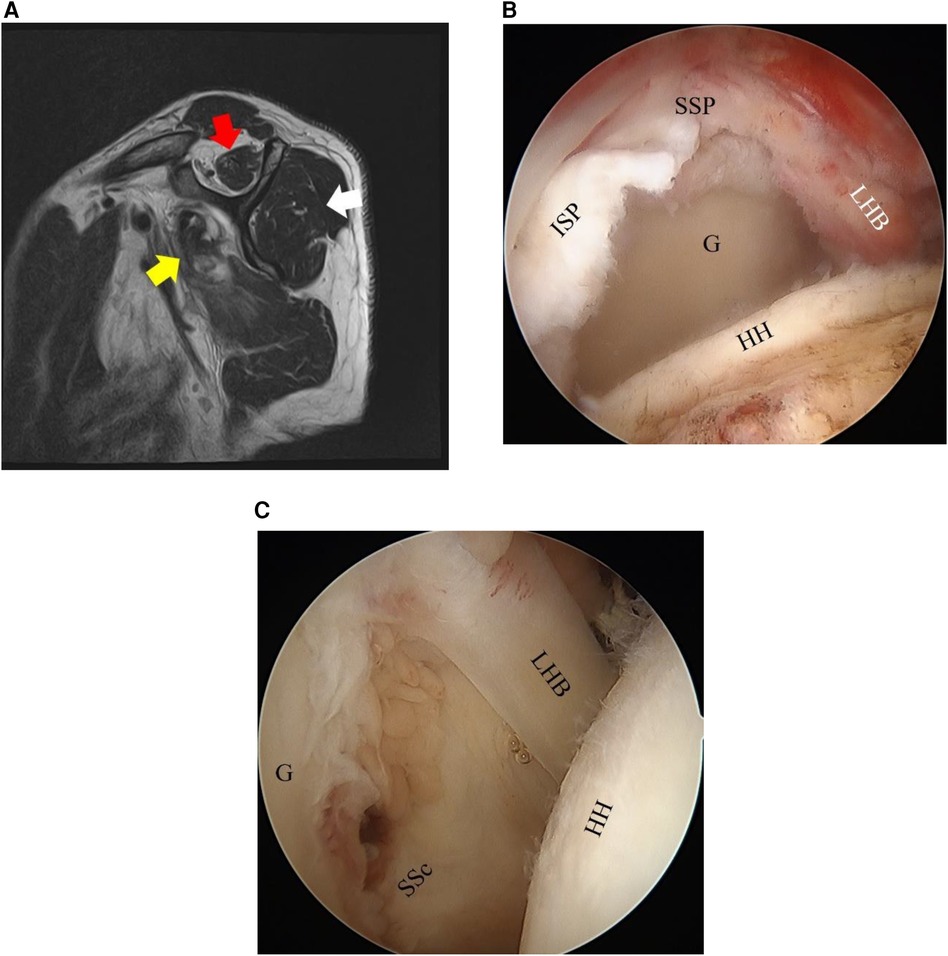
Figure 1. Fatty infiltration (FI) of the rotator cuff muscles on MRI sagittal images and arthroscopic findings of Case 1. (A) A 64-year-old man. Right rotator cuff tear. The FI grades of the SSP (red arrow), ISP (white arrow), and SSc (yellow arrow) are 2, 1, and 2, respectively. (B,C) Based on the arthroscopic findings, the SSP–ISP tear is graded as a massive tear and the SSc tear as Lafosse Type IV. SSP, supraspinatus tendon; ISP, infraspinatus tendon; SSc, subscapularis tendon; G, glenoid; LHB, long head of biceps; HH, humeral head.
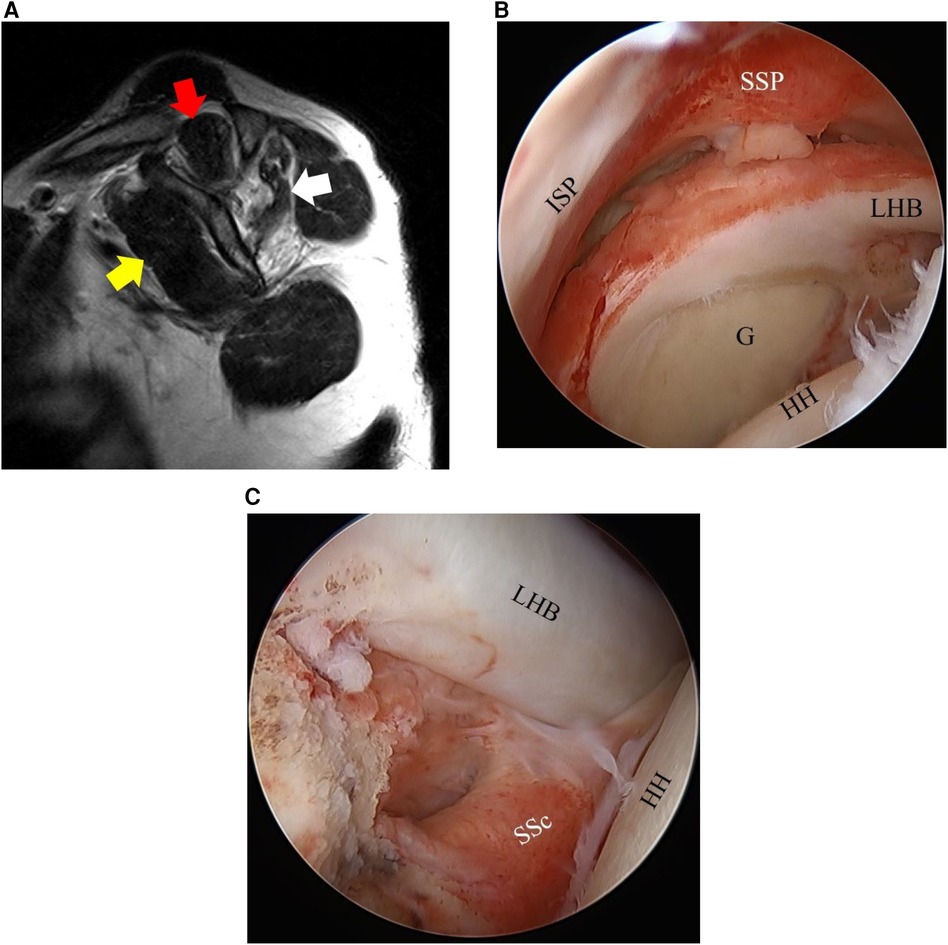
Figure 2. Fatty infiltration (FI) and arthroscopic findings of Case 2. (A) A 43-year-old man. The FI grades of the SSP (red arrow), ISP (white arrow), and SSc (yellow arrow) are 2, 3, and 0, respectively. (B,C) Based on the arthroscopic findings, the SSP–ISP tear is graded as a massive tear and the SSc tear as Lafosse Type I. SSP, supraspinatus tendon; ISP, infraspinatus tendon; SSc, subscapularis tendon; G, glenoid; LHB, long head of biceps tendon; HH, humeral head.
This study primarily aimed to determine whether tear size and location, especially in the SSc tendon, are associated with FI of adjacent rotator cuff muscles. The secondary aim was to clarify which patient factors, such as patient age, comorbidities, or trauma history, are associated with rotator cuff muscle FI.
Materials and methods
Study participants
The study examined 373 shoulders of 348 patients (mean age at surgery, 62.8 years; range, 31–80 years). Patients who underwent arthroscopic surgery (primary repair, fascia lata autograft, partial repair, or debridement only) for rotator cuff tears at our hospital between April 2013 and August 2022, in whom FI could be assessed on preoperative MRI in the oblique sagittal image, were included. The exclusion criteria were cases of reoperation, cases of paralysis due to other diseases, cases of rotator cuff tear associated with shoulder dislocation, and cases of rotator cuff tear-related arthropathy for which reverse shoulder arthroplasty was indicated. There were 264 male shoulders and 109 female shoulders. The following patient factors were investigated for each participant: age at surgery, sex, body mass index (BMI), presence of diabetes mellitus (DM) or hyperlipidemia (HL), trauma history, and time from the appearance of symptoms to surgery (duration of symptoms). The time from trauma to MRI (in traumatic cases) was also investigated.
Evaluation of fatty infiltration (FI) and tear size
The FI grades of the SSP, ISP, and SSc were assessed on preoperative MRI according to the Goutallier classification modified by Fuchs (1–3). The assessment was conducted using the most lateral sagittal slice in which the scapular spine was continuous with the scapular body, the so-called Y-shaped view (1, 3) (Figures 1A, 2A). The field of view was 16 × 16 cm, and the thickness was 5 mm, for the sagittal sections. Grading of the fatty infiltration was as follows: Stage 0, no fatty infiltration; Stage 1, some fatty steaks; Stage 2, less fat than muscle; Stage 3, as much fat as muscle; and Stage 4, more fat than muscle (1, 3). Cysts around the rotator cuff muscle in continuity with the rotator cuff tear or glenohumeral joint were excluded from the assessment. All assessments were conducted by a single shoulder surgeon (lead author). To test reliability, 10 of the patients were randomly selected, and the Goutallier classifications of the SSP, ISP, and SSc muscles of these 10 patients were independently assessed twice by two experienced shoulder surgeons.
Surgeries were performed by four shoulder surgeons, with one senior surgeon (lead author) supervising the surgeries of the three other surgeons. Surgery was conducted under general anesthesia with the patient in the beach chair position. The size of the posterior–superior (SSP–ISP) tear was classified on a six-grade scale according to the modified Cofield classification (11) based on preoperative MRI evaluation and intraoperative arthroscopic findings. If only the SSc was torn, this was classified as no tear, and the tears were classified as a partial tear (bursal side or joint side), small tear (<1 cm), medium tear (<1–3 cm), large tear (3–5 cm), or massive tear (>5 cm). The SSc tear was classified on a six-grade scale according to the Lafosse classification (12) with arthroscopic findings, with the humerus in slight flexion and neutral rotation in the beach chair position, and preoperative imaging analysis (Type 0, no tear; Type I, partial superior third lesion; Type II, complete superior third lesion; Type III, complete superior two-thirds lesion; Type IV, complete tendon lesion with well-centered humeral head and FI graded ≤3; Type V, complete tendon lesion with subluxated humeral head, coracoid conflict, and FI graded ≥3) (Figures 1B,C, 2B,C).
Statistical analysis
Cohen's κ statistics were calculated for both intraobserver and interobserver reliabilities of the Goutallier classification. To investigate the associations between the FI grades of each rotator cuff muscle and SSP–ISP and SSc tear size, we performed a linear-by-linear association test (13) to assess whether SSP–ISP and SSc tear severities tended to be higher when the FI grade for each rotator cuff muscle was higher. The associations between FI grade and sex, the presence of DM or HL, and trauma were investigated by the Mann–Whitney U-test, and the associations between FI grade and age, BMI, duration of symptoms, and trauma–MRI duration were investigated by Spearman's rank correlation coefficient. Age, BMI, period since symptom onset to surgery, and trauma–MRI duration were stratified by 10-year, 5 kg/m2, 6-month, and 3–6-month intervals, respectively, and the relationships with muscle FI were examined. Two-sided P-values are reported. Significance was determined at a P-value of <0.05. Statistical analyses were performed using Statcel 3 (OMS Publications, Tokyo, Japan) and R4.2.1 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
The mean age of the study participants was 62.8 years, with 46.6% in the 60–69-year age group, and 70.8% were men. The mean BMI was 24.0 kg/m2, and 68% of participants had a BMI ≤25.0 kg/m2. Approximately 12% of cases had DM and HL (statins were administered at the time of surgery in 70% of HL cases). A trauma history was reported in 39.4% of the participants. The mean duration of symptoms was 7.9 months, and this duration was ≤6 months in 63.8% of participants (Table 1). In terms of SSP–ISP tear size, the medium tear group was the largest, with 158 shoulders (42.4%), followed by the large tear group, with 105 (28.1%). SSc tear size according to the Lafosse classification was “no tear” in 119 shoulders (31.9%), and the largest group among those shoulders for which a tear was observed was Type II, in 101 shoulders (27.1%) (Table 1).
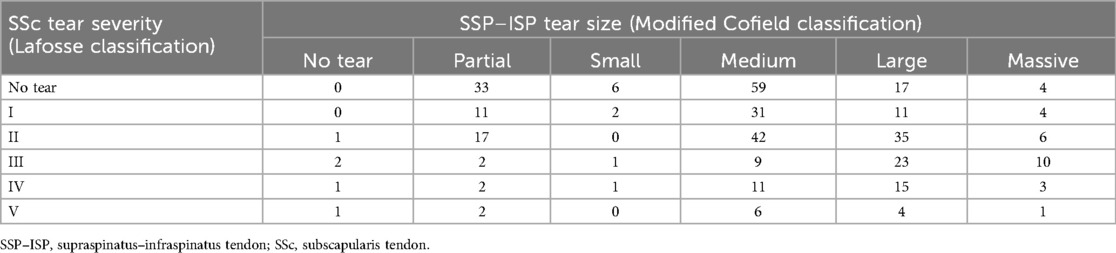
Table 2 shows the combined status of SSP–ISP tears and SSc tears. The most common combinations were SSP–ISP medium tear only or SSP–ISP medium/large tears with Lafosse Type II SSc tears (Table 2).
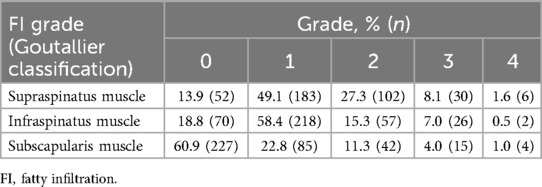
The average time from MRI to surgery was 2.2 months. Regarding the FI grades by the Goutallier classification, Stage 1 was the most common in SSP with 183 cases and 218 cases in ISP, and Grade 0 was the most common in SSc with 227 cases (Table 3). The Cohen κ statistics for intraobserver and interobserver reliabilities of the Goutallier classification were 0.81 and 0.71, respectively.
The associations of the sizes of SSc and SSP–ISP tears with the degree of FI in each rotator cuff muscle were investigated. SSP–ISP tear size was significantly associated not only with the FI grades of the SSP and ISP but also with that of the SSc (Table 4) (P < 0.01). SSc tear severity was also significantly associated not only with the FI grade of the SSc but also with those of the SSP and ISP (Table 5) (P < 0.01).
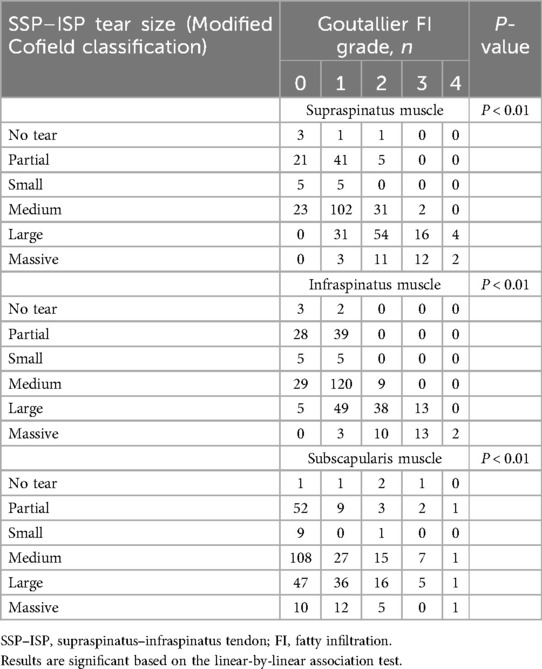
Table 4. Associations between SSP–ISP tear severity (modified Cofield classification) and fatty infiltration of each rotator cuff muscle.
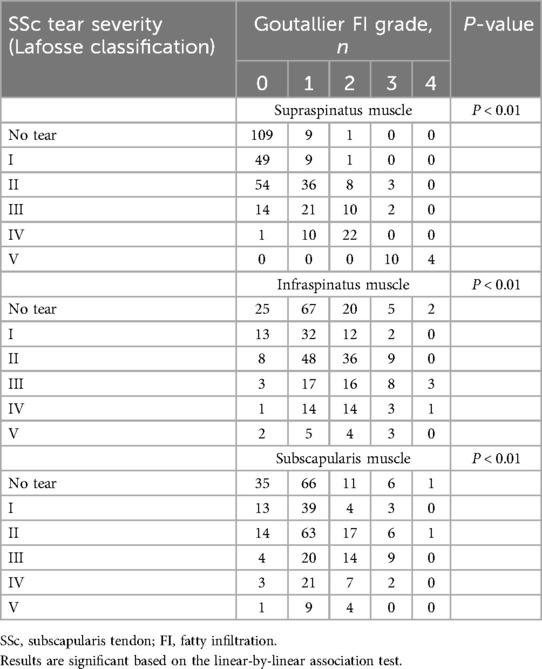
Table 5. Associations between SSc tear severity (Lafosse classification) and fatty infiltration of the rotator cuff muscles.
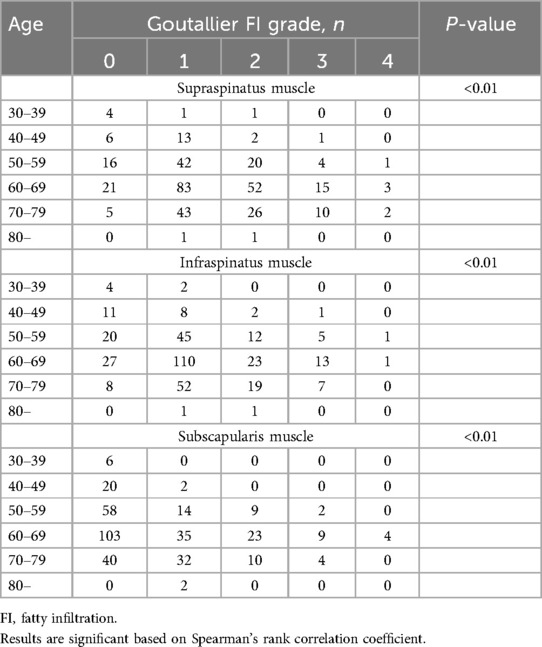
The associations between the FI grade according to the Goutallier classification and the different patient factors were investigated. Patient age at surgery was significantly associated with the FI grades of the SSP, ISP, and SSc, with the FI grade progressing significantly with advancing age (Table 6). However, there were no significant associations of the FI grade with sex, BMI, presence of DM or HL, and duration of symptoms (Table 7).
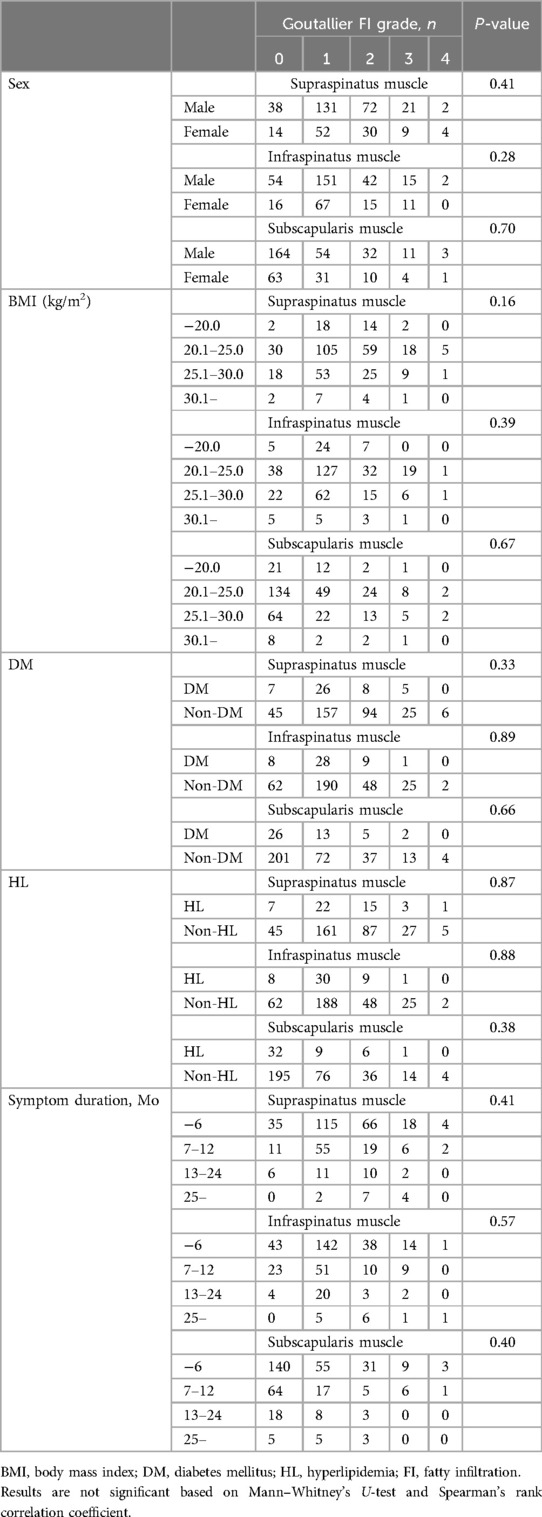
Table 7. Associations between fatty infiltration of each rotator cuff muscle and sex, BMI, patient comorbidities, and duration of symptoms.
There was no significant difference in FI of each rotator cuff muscle between traumatic and non-traumatic cases. In addition, there was no significant correlation between the time from injury to MRI and FI of the muscle in traumatic cases (Table 8).
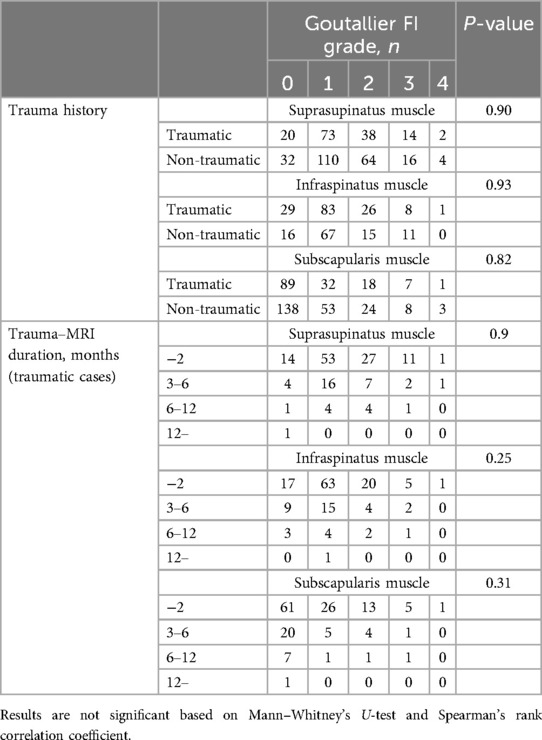
Table 8. Comparison between traumatic and non-traumatic cases with the Goutallier classification, and associations between fatty infiltration of each rotator cuff muscle and trauma–MRI duration (traumatic cases).
Discussion
In the present study, the associations between FI grades and SSc or SSP–ISP tear size, as well as the various patient factors, were investigated. It was found that there were significant associations between SSc tear size and the FI grade of the SSc itself and between SSP–ISP tear size and the FI grade of the SSP–ISP itself. Furthermore, it was shown that SSc tear size was associated with the FI grades of the SSP and the ISP and that SSP–ISP tear size was associated with the FI grade of the SSc. There were some patients in the present study in whom the FI grade of the ISP was comparatively mild, but the FI grades of the SSP and the SSc were more advanced (Figure 1A), and others in whom the FI grade of the ISP was advanced, but the FI grades of the SSP and the SSc were comparatively mild (Figure 2A). Based on the results of the present study, the severity of adjacent rotator cuff tears including the SSc may affect the FI grade of the SSP and ISP in these cases. In clinical settings, we should consider the effect of any tear in the adjacent rotator cuff when assessing the FI grade of the rotator cuff muscles.
The reason for the associations between the size of the tear in each rotator cuff and the FI of the adjacent rotator cuff found in this study is thought to be its anatomical structure. Because the attachments of the SSc and the SSP are close to each other, their disruption may affect the FI of each of these muscles. In recent years, the anatomical structure of the anterior–superior part of the rotator cuff has been clarified, and many studies have testified to its clinical importance. Mochizuki et al. (10) found that the insertion area of the SSP is located at the anteromedial region of the highest impression on the greater tuberosity and is sometimes located at the superior-most area on the lesser tuberosity. Arai et al. (9) conducted a detailed investigation of the insertion of the tendinous portion of the SSc into the lesser tuberosity and reported that, in most cases, the superior-most insertion was located on the superior margin of the lesser tuberosity and that a “thin tendinous slip” extended further upward. These results indicate a close relationship between the SSc and the SSP attachment around the bicipital groove (upper side of the lesser tuberosity and anterior portion of the greater tuberosity). In terms of clinical studies, a prospective study of non-traumatic rotator cuff tears conducted by Hebert-Davies et al. (8) reported that FI was three times more likely to be advanced when damage extended into the anterior portion of the SSP than in cases when the anterior part was preserved. The results of these studies are indicative of both the importance of the anterior fibers of the SSP tendon and its close relationship with the superior part of the SSc tendon, and their anterior and superior insertions may play important roles in the proper functioning of these muscles. The present study demonstrated significant associations between the FI grades in the SSP and the ISP with SSc tear size, results that are not inconsistent with the anatomical and clinical findings described above. These results suggest that the FI grades of the SSP and the ISP may be affected not only by the size of tears in these muscles themselves but also by whether there is any collapse in the anterior–superior part, including the lesser tuberosity into which the SSc inserts. It is difficult to explain the relationship between SSc and ISP tear size and FI, which are not adjacent to each other. This may be due to the fact that SSP and ISP form a layered structure and are connected to each other (10).
The limitations of this study include its nature as a retrospective study that only investigated patients who underwent a variety of arthroscopic surgeries and excluded severe FI cases for which reverse shoulder arthroplasty was indicated. For these reasons, it was not possible to examine the relationship between FI and postoperative cuff integrity of the adjacent rotator cuff. Similarly, although this retrospective study showed an indirect association between adjacent rotator cuff tears and rotator cuff muscle FI, prospective longitudinal studies are needed to directly demonstrate their relationship. Another limitation of the statistical analysis is that some cells in the table had a small sample size, making multivariate analysis difficult. In the present study, SSc and SSP–ISP tears were classified and investigated based on preoperative MRI and arthroscopic findings, but in the case of large or massive tears, the size of the tear may have affected the FI of the entire rotator cuff muscles.
Conclusions
The results of the present study not only confirmed the previously reported association between rotator cuff tear size and FI grade but also identified associations between SSc tear size and the FI grades of the SSP and ISP and between SSP–ISP tear size and the FI grade of the SSc. The FI grade of each rotator cuff muscle depended not only on the size of the tear in the tendon itself but also on whether there was a tear in the adjacent part of the rotator cuff including the SSc. In light of this finding, the effect of any tear in the adjacent rotator cuff must be considered when assessing the FI grade of the rotator cuff muscles in clinical settings.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Clinical Research Ethics Committee at Nagasaki University Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SK: Investigation, Methodology, Writing – original draft, Writing – review & editing. KC: Writing – original draft, Writing – review & editing. TA: Investigation, Writing – review & editing. KS: Investigation, Writing – review & editing. SS: Data curation, Formal Analysis, Writing – original draft. MO: Supervision, Writing – original draft, Writing – review & editing.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg. (1999) 8:599–605. doi: 10.1016/s1058-2746(99)90097-6
2. Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. (1994) 304:78–83. doi: 10.1097/00003086-199407000-00014
3. Kuzel BR, Grindel S, Papandrea R, Ziegler D. Fatty infiltration and rotator cuff atrophy. J Am Acad Orthop Surg. (2013) 21:613–23. doi: 10.5435/JAAOS-21-10-613
4. Somerson JS, Hsu JE, Gorbaty JD, Gee AO. Classifications in brief: Goutallier classification of fatty infiltration of the rotator cuff musculature. Clin Orthop Relat Res. (2016) 474:1328–32. doi: 10.1007/s11999-015-4630-1
5. Giri A, Freeman TH, Kim P, Kuhn JE, Garriga GA, Khazzam M, et al. Obesity and sex influence fatty infiltration of the rotator cuff: the Rotator Cuff Outcomes Workgroup (ROW) and multicenter Orthopaedic Outcomes Network (MOON) cohorts. J Shoulder Elbow Surg. (2022) 31:726–35. doi: 10.1016/j.jse.2021.12.011
6. Kim HM, Dahiya N, Teefey SA, Keener JD, Galatz LM, Yamaguchi K. Relationship of tear size and location to fatty degeneration of the rotator cuff. J Bone Joint Surg Am. (2010) 92:829–39. doi: 10.2106/JBJS.H.01746
7. Melis B, Wall B, Walch G. Natural history of infraspinatus fatty infiltration in rotator cuff tears. J Shoulder Elbow Surg. (2010) 19:757–63. doi: 10.1007/s11999-009-1207-x
8. Hebert-Davies J, Teefey SA, Steger-May K, Chamberlain AM, Middleton W, Robinson K, et al. Progression of fatty muscle degeneration in atraumatic rotator cuff tears. J Bone Joint Surg Am. (2017) 99:832–39. doi: 10.2106/JBJS.16.00030
9. Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: an anatomic and clinical investigation. Arthroscopy. (2008) 24:997–1004. doi: 10.1016/j.arthro.2008.04.076
10. Mochizuki T, Sugaya H, Uomizu M, Maeda K, Matsuki K, Sekiya I, et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. (2008) 90:962–9. doi: 10.2106/JBJS.G.00427
11. Cofield RH, Parvizi J, Hoffmeyer PJ, Lanzer WL, Ilstrup DM, Rowland CM. Surgical repair of chronic rotator cuff tears. A prospective long-term study. J Bone Joint Surg Am. (2001) 83:71–7. doi: 10.2106/00004623-200101000-00010
12. Lafosse L, Lanz U, Saintmard B, Campens C. Arthroscopic repair of subscapularis tear: surgical technique and results. Orthop Traumatol Surg Res. (2010) 96:S99–108. doi: 10.1016/j.otsr.2010.09.009
Keywords: rotator cuff tear, fatty infiltration, Goutallier classification, Lafosse classification, Cofield classification, tear size, tear location
Citation: Kajiyama S, Chiba K, Aoki T, Sada K, Sato S and Osaki M (2024) Associations between fatty infiltration of rotator cuff muscles and tear size or location of rotator cuff tendon. Front. Surg. 11:1416921. doi: 10.3389/fsurg.2024.1416921
Received: 13 April 2024; Accepted: 6 August 2024;
Published: 22 August 2024.
Edited by:
Chi-Ming Wong, Hong Kong Polytechnic University, Hong Kong SAR, ChinaReviewed by:
Mattia Alessio-Mazzola, San Raffaele Hospital (IRCCS), ItalyGregory Alexander Hoy, Monash University, Australia
Copyright: © 2024 Kajiyama, Chiba, Aoki, Sada, Sato and Osaki. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shiro Kajiyama, a2F6aWNvQG5hZ2FzYWtpLXUuYWMuanA=
 Shiro Kajiyama
Shiro Kajiyama Ko Chiba2
Ko Chiba2 Shuntaro Sato
Shuntaro Sato