
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 04 July 2024
Sec. Otorhinolaryngology - Head and Neck Surgery
Volume 11 - 2024 | https://doi.org/10.3389/fsurg.2024.1395936
 Luca Gazzini1
Luca Gazzini1 Arianna Caselli2
Arianna Caselli2 Virginia Dallari3*
Virginia Dallari3* Enrico Fazio1
Enrico Fazio1 Monir Abousiam1
Monir Abousiam1 Aurel Nebiaj1
Aurel Nebiaj1 Cecilia Albi4
Cecilia Albi4 Remo Accorona5
Remo Accorona5 Armando De Virgilio6
Armando De Virgilio6 Antonio Greco6
Antonio Greco6 Luca Calabrese1
Luca Calabrese1
Objective: The local spread of oral tongue squamous cell carcinoma (OTSCC) follows pathways of dissemination along areas of lesser resistance. In more advanced scenarios, the tumor can extend beyond the hemi-tongue of origin, by passing through the lingual septum and following the fibers of the transverse muscle. This can lead to the invasion of the contralateral extrinsic muscles, the first being the genioglossus and more laterally the hyoglossus. An anatomically guided surgical resection of the tumor can be planned to ensure both oncological safety and an acceptable functional outcome. This approach aims to preserve the hyo-styloglossus unit (HSU) whenever feasible.
Methods: Between January 2019 and November 2022, six patients received extended glossectomy Type B (EG Type B), with preservation of the HSU. Preliminary oncological results and functional results in terms of swallowing (FOIS score) and quality of life (MDADI) are presented.
Results: Five out of the six patients are alive and disease-free, while one patient died due to other causes. All patients who were candidates for an EG Type B underwent a swallowing assessment prior to surgery and followed daily postoperative swallowing training. At discharge, the patients continued swallowing training in an outpatient clinic. Five out of the six patients reached a full oral diet within 1 year of follow-up.
Conclusion: The oncological results confirm the safety of this technique. The importance of preserving the HSU, the minimal functional unit, shows very encouraging results in terms of swallowing rehabilitation.
Advanced oral tongue squamous cell carcinoma (OTSCC) represents a challenge for head and neck surgeons. The goal of surgery is to achieve oncological radicality while ensuring acceptable functional results in terms of speech and swallowing. In advanced tumors (cT3-T4a), the disease can spread through the lingual septum and along the intrinsic transverse muscle to involve the contralateral hemi-tongue (1). An anatomic-based approach, performed according to preoperative imaging and intraoperative findings, allows for complete and oncologically safe resection, preserving structures not involved in the disease.
In advanced OTSCC, one of the main adverse features in predicting postoperative swallowing impairment is the involvement of the base of the tongue (BOT). The key role of the BOT in maintaining an acceptable swallowing function was already demonstrated in the literature by the experience of Chen et al. in robotic surgery (2, 3). We postulated that to maintain an acceptable swallowing function, it is paramount to preserve a functional unit made by the hyoglossus and styloglossus muscles together with their innervation, for which the term hyo-styloglossus unit (HSU) was coined (Figure 1).
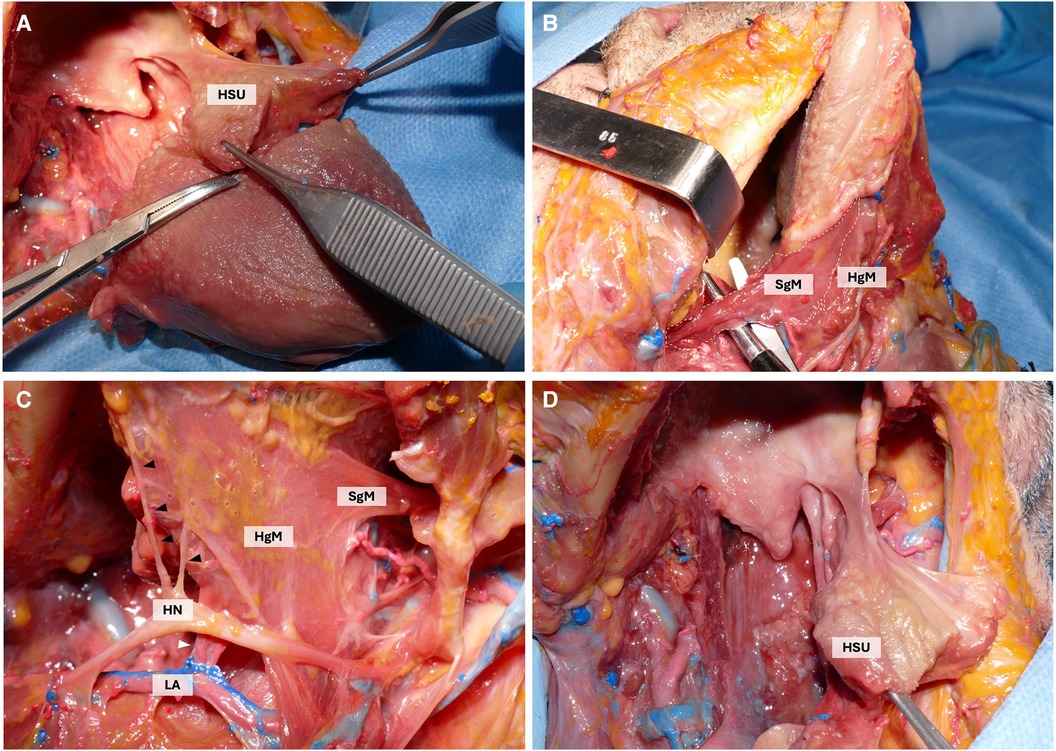
Figure 1 Cadaveric dissection highlighting the HSU. (A) Isolation of the intrinsic musculature of the HSU. (B) lateral view highlighting the course of the styloglossus muscle (SgM) whose fibers merge with those of the hyoglossus muscle (HgM). (C) Lateral view of the HSU highlighting the branches of the hypoglossal nerve (HN) (black arrowhead) and of the lingual artery (LA) (white arrowhead) supplying the HSU. Styloglossus muscle (SgM). (D) the HSU after the subtotal glossectomy.
The study aims to describe the surgical approach to advanced cT4a tumors that extend beyond the lingual septum to the contralateral hemi-tongue involving the genioglossus muscle while sparing the hyoglossus and styloglossus muscle of the contralateral side. The procedure of the subtotal glossectomy sparing the HSU (EG Type B) is described step by step, focusing on the surgical anatomy. In addition, preliminary functional results in terms of swallowing and quality of life (QoL) are presented.
A retrospective review of patients who underwent EG Type B for advanced OTSCC between January 2019 and November 2022 was conducted in the Department of Otolaryngology-Head and Neck Surgery in “Ospedale Centrale” of Bolzano (4).
All patients underwent preoperative MRI with gadolinium, which is a fundamental decision-making tool to depict the invasion of key anatomical structures.
Based on the clinical presentation and MRI, the indications for subtotal glossectomy with preservation of the HSU are as follows:
○ advanced cT3-cT4a OTSCC extended beyond the lingual septum and involving the contralateral hemi-tongue (Figure 2);
○ bilateral involvement of the genioglossus muscle, with sparing of the contralateral hyoglossus, styloglossus muscle, and hypoglossal nerve; and
○ general patient conditions permitting major surgery and reconstruction with a microvascular free flap.
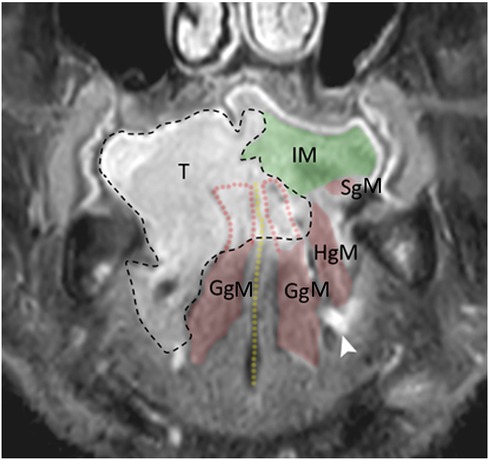
Figure 2 MRI sagittal view: tumor enveloping the genioglossus muscle on both sides. T, tumor; IM, intrinsic musculature; SgM, styloglossus muscle; GgM, genioglossus muscle; HgM, hyoglossus muscle. Yellow dotted line, lingual septum; black dotted line, tumor border.
An ipsilateral CTS is performed, following the surgical steps of the standard technique already described in the literature (5, 6). The only difference is that in this case the dissection of the lingual septum must be avoided. At this point, the macroscopic invasion of the contralateral genioglossus muscle can be assessed under direct vision. We describe thereby the surgical approach to the contralateral compartment of the tongue (7):
○ The first step is the detachment of the insertion of the contralateral genioglossus muscle from the mental symphysis.
○ The contralateral lingual artery is identified by using the genioglossus muscle surface as the dissection plane to locate it. The lingual artery runs between the lateral aspect of the genioglossus muscle and the medial aspect of the hyoglossus and styloglossus muscles.
○ Taking the lingual artery as a landmark, the hyoglossus and styloglossus muscles are identified superficially in relation to the vascular space. The hyoglossus muscle is located in an anterior position, while the styloglossus muscle is located posteriorly and its distal fibers merge anteriorly with the lateral fibers of the hyoglossus muscle. These two muscle structures, together with the terminal branches of the hypoglossal nerve directed to them, represent the HSU. During the surgical dissection, care has to be taken to preserve the HSU in order to maintain its anatomical integrity and thus the functionality of the BOT.
○ The sublingual region is dissected, identifying the sublingual gland, which is cleared of surrounding stromal tissue. Moreover, lingual and hypoglossal nerves are identified and their terminal branches directed to the genioglossus muscle are sectioned. Care must necessarily be taken to preserve the branches for the hyoglossal and styloglossal muscles in order to maintain motor innervation to the HSU.
○ The last step is the detachment of the genioglossus from the hyoid bone. Finally, the resection of the dorsal aspect of the tongue with the mucosa and intrinsic musculature is performed with a monopolar scalpel.
○ The reconstruction is conducted using a microvascular free flap. Our workhorse flap is the anterolateral thigh flap (ALTF), which gives the advantage of harvesting a chimeric flap with the vastus lateralis muscle. This is particularly important in these patients in order to supply enough bulk of the tongue base, to achieve a proper swallowing during the pharyngeal phase (Figure 3). The suspension of the larynx, a fundamental step in swallowing recovery, is ensured by the contralateral digastric and stylohyoid muscles, which support the hyoid bone. On the ipsilateral side, the inset of the flap is performed as follows: the vastus lateralis muscle is fixed between the hyoid bone and the mandibular symphysis to achieve both flap support and suspension of the central part of the hyoid bone to the mandible. The fascia lata harvested with the flap is instead fixed between the lateral portion of the hyoid body and the mandible body, ensuring laryngeal suspension. In case the contralateral digastric muscle is also sectioned, hyoid suspension via the flap's fascia lata is made contralaterally as well.
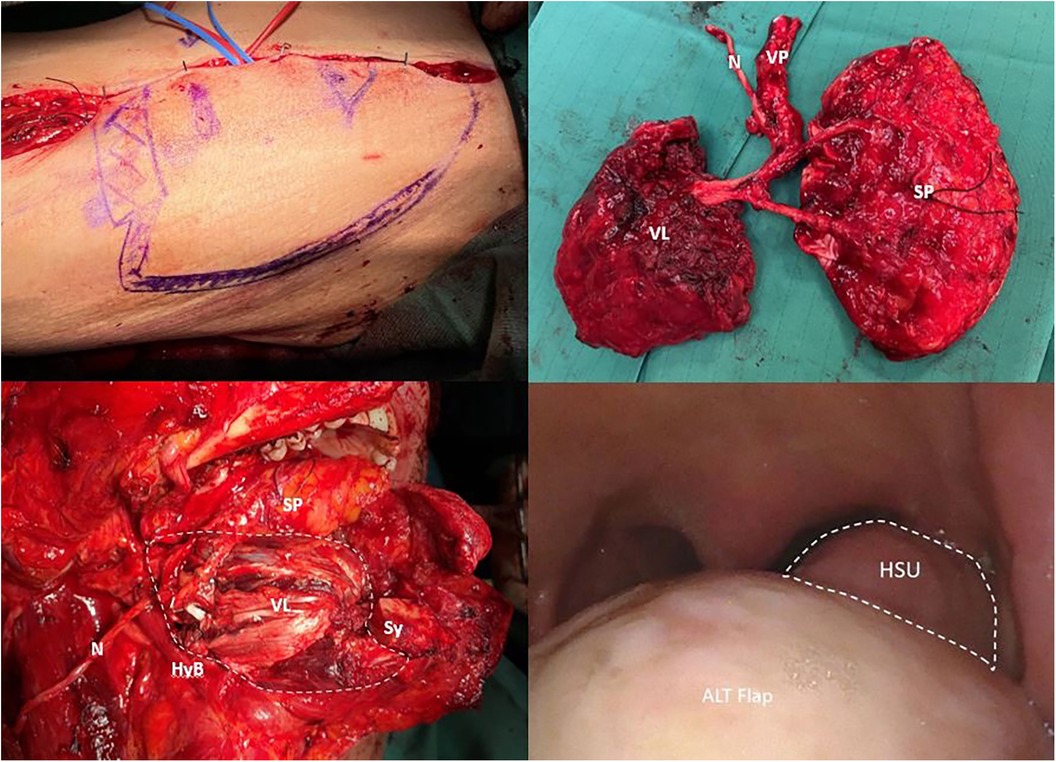
Figure 3 Insetting of the ALTF. The white dotted line indicates the preserved HSU. N, nerve; VP, vascular pedicle; VL, vastus lateralis muscle; SP, skin paddle; HyB, hyoid bone; Sy, mental symphysis.
All patients eligible for an EG Type B underwent swallowing assessment before surgery and received daily postoperative swallowing training with a speech and language therapist (SLT). At discharge, the patients continued swallowing training in an outpatient clinic. The goal of the swallowing rehabilitation is to obtain a functional swallowing act, which allows patients to reach oral feeding safety and the absence of aspiration pneumonia. The patients learn with an SLT how to manage oral and pharyngeal residue.
The parameters measured in this research were functional oral intake ability and the patient's QoL. Swallowing function was assessed four times: pre-surgery, after 2 weeks of rehabilitation, 6 months post-surgery, and during long-term follow-up (at least 1 year post-surgery), using the Italian version of the Functional Oral Intake Scale (FOIS) (8). To assess the impact of oral dysphagia on quality of life, an Italian version of the M.D. Anderson Dysphagia Inventory (MDADI) by Chen et al. was used (9). The MDADI was self-administered at least 1 year post-surgery in a quiet room and in the presence of the SLT in case the patient required clarifications.
Six patients (five males and one female, with a median age of 49.2 years) were included in the study. Two patients were active smokers, whereas none had a history of alcohol abuse. All patients were affected by advanced tongue squamous cell carcinoma pT3 or pT4a. Data about patients, surgery, and follow-up are summarized in Table 1. The types of consistencies of foods and liquids are categorized according to the International Dysphagia Diet Standardisation Initiative (IDDSI) Framework of 2016 (10).
Regarding the swallowing results, five out of the six patients reached a full oral diet within 1-year follow-up, with a score of 6 on the FOIS. One patient with severe neurocognitive disorder continued to be fed through a percutaneous gastrostomy, since sufficient oral intake was not reached. Information regarding swallowing function and the patient's QoL is summarized in Tables 2, 3.
The primary goal of tumor ablation in OTSCC is to remove the entire tumor along with a “margin” of normal tissue. Inadequate clearance of tumor cells results in increased risks of local and regional recurrences, as well as decreased long-term survival rates (11, 12).
The extrinsic muscles of the tongue can be divided into a peripheral group including palatoglossus, styloglossus, and hyoglossus muscles, which are located laterally, and the genioglossus muscle, located in a deeper plane, which gives rise to fibers running to the periphery, the dorsal surface, and the apex of the tongue (13). Local tumor spread first involves the intrinsic musculature following the direction of muscle fibers, the genioglossus muscle in case of an anterior tumor, or the hyoglossus and styloglossus muscles in case of a posterior tumor. In the case of macroscopic infiltration of the extrinsic musculature of the tongue, CTS is indicated, with the aim of removing the entire oncological compartment with the pathways of tumor spread. These include the tumor, within the entire hemi-tongue and related floor of the mouth and the neck lymph nodes in continuity with the so-called tumor-node tract (TNT) (5, 12).
The lingual septum represents a barrier to contralateral spread, but it is not uncommon in advanced stages (cT3-cT4a) for it to be overcome. In those cases, the extension of the resection to the contralateral tongue may affect the postoperative tongue functionality and thus the patient's quality of life. The defect resulting from EG Type B requires reconstruction that includes free flaps to adequately restore bulk and prevent ankyloglossia (13). Radical surgical treatment often affects all oral functions, such as speech and swallowing physiology (13, 14). In the oral preparatory phase, there can be alterations related to tongue motility for bolus preparation and formation and, in the oral phase, alterations related to bolus transportation and bolus control. In the pharyngeal phase, alteration of swallow initiation, posterior tongue propulsion, hyolaryngeal excursion, bolus propulsion, post-swallow pharyngeal residue, and risk of penetration and aspiration can be observed (15, 16). Advanced tumor (T) stage, extraoral surgical approach, the incremental volume of glossectomy defect, and adjuvant radiotherapy correlate significantly with poor swallowing outcomes (17, 18).
Grammatica et al. investigated the long-term functional outcomes in patients treated by CTS and reconstructed by free flaps and demonstrated that CTS does not significantly affect speech and swallowing (5). However, the study included only patients who underwent ipsilateral CTS.
The important role of the BOT in the propulsion of food makes its removal of particular concern, even if tongue base resections are becoming increasingly common in the modern era of transoral robotic surgical approaches (2, 3).
In this scenario, the pivotal concept of HSU in the maintenance of an acceptable residual swallowing function should be highlighted. The HSU can be compared to the cricoarytenoid unit in partial OPHL laryngectomies, where preservation of one arytenoid with the underlying portion of the cricoid plate and the recurrent nerve allows normal motility of the arytenoid (functioning cricoarytenoid unit) (19, 20). A concept similar to HSU has been described in the works of Gawryszuk et al. in the field of radiotherapy (21, 22). They introduced a concept rooted in anatomy and physiology known as functional swallowing units (FSU), aiming to enhance comprehension of radiation-induced dysphagia.
Preserving HSU is one of the main goals of the EG Type B also in the case of bilateral involvement of the genioglossus muscles. This unit must only be sacrificed if there is a direct invasion of the hyoglossus muscle bilaterally, so in this case, the approach should be converted to total glossectomy.
The importance of preserving the HSU in advanced tongue tumors is supported by our encouraging results in terms of swallowing and QoL. Though the number of patients is limited, it is noteworthy that all patients but one resumed a regular oral food intake of liquid and solid of different consistencies, and did not develop aspiration pneumonia. All patients, except one, can swallow liquids and foods of different consistencies using the swallowing technics learned during rehabilitation. The long-term results regarding the impact of dysphagia on their QoL demonstrated that all patients present good day-to-day functioning and QoL.
In our series, only one patient with severe comorbidities was not reconstructed with a free microvascular flap but in a sub-optimal way with a major pectoralis flap. Furthermore, he was affected by a severe cognitive disorder that prevented swallowing rehabilitation. This was the only patient in our case series that was not able to resume a full oral diet and a percutaneous endoscopic gastrostomy was performed and maintained. This experience confirms that patients who are candidates for surgery should be carefully selected, including only those who are suitable for a highly demolitive procedure, microvascular reconstruction, and an intensive swallow rehabilitation program. Therefore, patients should be appropriately counseled on the risks of this strong demolitive surgery with emphasis placed on intensive swallow rehabilitation in the posttreatment setting (2, 13).
Regarding the oncological outcomes, as shown in Table 1, all patients thus far are disease-free except for one who passed away due to other reasons. These results demonstrate that preserving the HSU, which we have observed to be both functional and essential for swallowing, does not compromise oncological safety.
Further studies are needed to confirm the preliminary functional results shown in the present study.
In our experience, the minimal functional unit that allows an acceptable swallowing result is the so-called functional unit of the BOT, which includes the hyoglossus and styloglossus muscles innervated by the hypoglossal nerve (HSU).
The importance of preserving this functional unit is corroborated by the highly encouraging results we observed in terms of both swallowing and QoL.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the Provincial Ethics Committee of Bolzano. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
LG: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. AC: Formal Analysis, Investigation, Writing – review & editing. VD: Conceptualization, Supervision, Writing – original draft. EF: Writing – review & editing. MA: Writing – review & editing. AN: Writing – review & editing. CA: Writing – review & editing. RA: Writing – review & editing. ADV: Writing – review & editing, Data curation. AG: Writing – review & editing, Supervision, Validation. LC: Conceptualization, Writing – review & editing.
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Calabrese L, Bizzoca ME, Grigolato R, Maffini FA, Tagliabue M, Negro R, et al. From bench to bedside in tongue muscle cancer invasion and back again: gross anatomy, microanatomy, surgical treatments and basic research. Life. (2020) 10(9):197. doi: 10.3390/life10090197
2. Chen DW, Wang T, Shey-Sen Ni J, Sandulache VC, Graboyes EM, Worley M, et al. Prognostic factors associated with achieving total oral diet after glossectomy with microvascular free tissue transfer reconstruction. Oral Oncol. (2019) 92:59–66. doi: 10.1016/j.oraloncology.2019.03.005
3. Manrique OJ, Leland HA, Langevin CJ, Wong A, Carey JN, Ciudad P, et al. Optimizing outcomes following total and subtotal tongue reconstruction: a systematic review of the contemporary literature. J Reconstr Microsurg. (2017) 33(2):103–11. doi: 10.1055/s-0036-1593772
4. Gazzini L, Fazio E, Dallari V, Accorona R, Abousiam M, Nebiaj A, et al. Impact of the COVID-19 pandemic on head and neck cancer diagnosis: data from a single referral center, South Tyrol, Northern Italy. Eur Arch Otorhinolaryngol. (2022) 279(6):3159–66. doi: 10.1007/s00405-021-07164-y
5. Calabrese L, Giugliano G, Bruschini R, Ansarin M, Navach V, Grosso E, et al. Compartmental surgery in tongue tumours: description of a new surgical technique. Acta Otorhinolaryngol Ital. (2009) 29(5):259–64. PMID: 20162027; PMCID: PMC2821124.20162027
6. Grammatica A, Piazza C, Ferrari M, Verzeletti V, Paderno A, Mattavelli D, et al. Step-by-step cadaver dissection and surgical technique for compartmental tongue and floor of mouth resection. Front Oncol. (2021) 11:613945. doi: 10.3389/fonc.2021.613945
7. Gazzini L, Fazio E, Dallari V, Spirito L, Abousiam M, Nocini R, et al. Beyond the boundaries of compartmental hemiglossectomy: a proposal for an anatomically based classification of surgical approaches to advanced oral tongue squamous cell carcinoma. Eur Arch Otorhinolaryngol. (2023) 280(6):3015–22. doi: 10.1007/s00405-023-07915-z
8. Battel I, Calvo I, Walshe M. Cross-cultural validation of the Italian version of the functional oral intake scale. Folia Phoniatr Logop. (2018) 70(3-4):117–23. doi: 10.1159/000490792
9. Chen AY, Frankowski R, Bishop-Leone J, Hebert T, Leyk S, Lewin J, et al. The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the M. D. Anderson dysphagia inventory. Arch Otolaryngol Head Neck Surg. (2001) 127(7):870–6. PMID: 11448365
10. Cichero JA, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. (2017) 32(2):293–314. doi: 10.1007/s00455-016-9758-y
11. Touré G, Vlavonou S, Andrianantoandro I, Ndiaye MM. TNM classification: are cancers with extrinsic tongue muscle involvement systematically T4a? J Oral Maxillofac Surg. (2021) 79(1):259–65. doi: 10.1016/j.joms.2020.07.222
12. Tagliabue M, Gandini S, Maffini F, Navach V, Bruschini R, Giugliano G, et al. The role of the T-N tract in advanced stage tongue cancer. Head Neck. (2019) 41(8):2756–67. doi: 10.1002/hed.25761
13. Vincent A, Kohlert S, Lee TS, Inman J, Ducic Y. Free-flap reconstruction of the tongue. Semin Plast Surg. (2019) 33(1):38–45. doi: 10.1055/s-0039-1677789
14. Elfring T, Boliek CA, Winget M, Paulsen C, Seikaly H, Rieger JM. The relationship between lingual and hypoglossal nerve function and quality of life in head and neck cancer. J Oral Rehabil. (2014) 41(2):133–40. doi: 10.1111/joor.12116
15. Baijens LWJ, Walshe M, Aaltonen LM, Arens C, Cordier R, Cras P, et al. European white paper: oropharyngeal dysphagia in head and neck cancer. Eur Arch Otorhinolaryngol. (2021) 278(2):577–616. doi: 10.1007/s00405-020-06507-5
16. Bartolome G, Schröter-Morasch H. Schluckstörungen Diagnostik und Rehabilitation. 4th ed. München: Urban & Fischer (2010).
17. Zhang S, Wu S, Liu L, Zhu D, Zhu Q, Li W. Assessment of quality of life of free anterolateral thigh flap for reconstruction of tissue defects of total or near-total glossectomy. J Oncol. (2020) 2020:2920418. doi: 10.1155/2020/2920418
18. Bhattacharya S, Thankappan K, Sukumaran SV, Mayadevi M, Balasubramanian D, Iyer S. Volume and location of the defect as predictors of speech outcome after glossectomy: correlation with a classification. Int J Oral Maxillofac Surg. (2021) 50(12):1533–9. doi: 10.1016/j.ijom.2021.02.026
19. Rizzotto G, Succo G, Lucioni M, Pazzaia T. Subtotal laryngectomy with tracheohyoidopexy: a possible alternative to total laryngectomy. Laryngoscope. (2006) 116(10):1907–17. doi: 10.1097/01.mlg.0000236085.85790.d5
20. Molteni G, Bertolin A, Gazzini L, Sacchetto A, Marchioni D. Modular approach to open partial horizontal laryngectomy: step-by-step anatomic dissection. Otolaryngol Head Neck Surg. (2022) 166(3):601–2. doi: 10.1177/01945998211026528
21. Gawryszuk A, Bijl HP, Holwerda M, Halmos GB, Wedman J, Witjes MJH, et al. Functional swallowing units (FSUs) as organs-at-risk for radiotherapy. PART 1: physiology and anatomy. Radiother Oncol. (2019) 130:62–7. doi: 10.1016/j.radonc.2018.10.028
Keywords: compartmental surgery, oral tongue cancer, tongue surgery, anatomic-based surgery, reconstructive surgery
Citation: Gazzini L, Caselli A, Dallari V, Fazio E, Abousiam M, Nebiaj A, Albi C, Accorona R, De Virgilio A, Greco A and Calabrese L (2024) Subtotal glossectomy with conservation of the hyo-styloglossus unit (HSU): a new pivotal concept for preserving tongue function in extended glossectomy. Front. Surg. 11:1395936. doi: 10.3389/fsurg.2024.1395936
Received: 4 March 2024; Accepted: 20 May 2024;
Published: 4 July 2024.
Edited by:
Piero Nicolai, University of Padua, ItalyReviewed by:
Pietro De Luca, Fatebenefratelli Hospital, Italy© 2024 Gazzini, Caselli, Dallari, Fazio, Abousiam, Nebiaj, Albi, Accorona, De Virgilio, Greco and Calabrese. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Virginia Dallari, dmlyZ2luaWEuZGFsbGFyaUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.