
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 13 May 2024
Sec. Reconstructive and Plastic Surgery
Volume 11 - 2024 | https://doi.org/10.3389/fsurg.2024.1364340
This article is part of the Research Topic Precise Diagnosis of Acute and Chronic Wound Repair View all 4 articles
 Da Qian1,†
Da Qian1,† Lijie Jin2,†
Lijie Jin2,† Guoxin Huang3,†
Guoxin Huang3,† Ping Dai1,†
Ping Dai1,† Dong Li1
Dong Li1 Hui Lu1
Hui Lu1 Ming Xu1
Ming Xu1 Ke Wang1
Ke Wang1 Xian Zhong1
Xian Zhong1 Xiaochen Xu1*
Xiaochen Xu1* Jianchao Zhang1*
Jianchao Zhang1* Bin Yu1*
Bin Yu1*
Introduction: This study aims to investigate the clinical efficacy of V-Y advanced flap pedicled with freestyle perforator flap for repairing small range defects in the anterior knee region.
Methods: 8 patients with skin and soft tissue defect/necrosis in the anterior knee area admitted to the Changshu No.1 People's Hospital from January 2021 to January 2022 were selected, with a defect range of 4 cm × 3 cm–9 cm × 6 cm, designed a V-Y advanced flap pedicled with freestyle perforator flap to repair the wound in the anterior knee area. Adjust the size and position of the flap according to the number and position of perforating branches found during the surgery, with a cutting area of 6 cm × 5 cm–14 cm × 10 cm and the supply area was directly pulled and sutured.
Results: 4 patients were repaired by flaps pedicled with 2 perforating branches, 2 patients were repaired by flaps pedicled with 1 perforating branch and 2 patients were repaired by flaps pedicled with 3 perforating branches. 4 patients were repaired by flaps pedicled with 2 perforating branches, 2 patients were repaired by flaps pedicled with 1 perforating branch and 2 patients were repaired by flaps pedicled with 3 perforating branches. All flaps survived and following up for 6-15 months, the blood supply, appearance, and color of the flap were satisfactory, and the functions of knee joint flexion and extension were well preserved.
Discussion: The V-Y advancement flap pedicled with freestyle perforator flap has the advantages of reliable blood supply, simple surgical operation, texture and thickness similar to the skin of the anterior knee area, and direct suture of the donor area. It is a perforator flap with good repair effect for small scale defects in the anterior knee area.
Anterior knee injuries commonly occur in the clinical setting and often result from trauma or burns (1, 2). Due to the sparse soft tissue in the Anterior knee region, skin necrosis is a frequent issue (3). This area plays a crucial role in joint mobility; thus, maintaining aesthetic appearance and knee joint mobility presents a significant challenge to plastic surgeons (4). Direct suturing or grafting is typically not the preferred approach to treat these injuries; instead, flap repair is often used. This type of injury is usually repaired with a skin flap, including perforator, fascial, muscle, and musculocutaneous flaps (5). However, this method frequently leaves secondary wounds that require grafting (6, 7).
In the field of plastic and reconstructive surgery, a variety of techniques are commonly employed to manage soft tissue injuries and defects. Among these, the use of flap repair, including perforator flaps, has been well-documented (8). Despite their efficacy, these methods can leave secondary wounds that necessitate further grafting. Consequently, there is a constant need for surgical techniques that minimize such secondary complications while ensuring effective wound repair and patient recovery (8). Various experts have conducted extensive discussions and research on flap repairing in this area (1, 7, 9). However, each type of flap has its advantages and disadvantages. Local flaps offer limited soft tissue coverage, making it difficult to achieve optimal repair for larger Anterior knee area defects (10). Free flaps can provide superior tissue coverage but cause significant donor site morbidity and are often bulky, which is unfavorable for subsequent knee joint function recovery (10).
Our aim is to identify a surgical method that can be promoted in primary care hospitals to treat small Anterior knee area defects. In this study, we utilized freestyle-pattern V-Y advancement flaps to repair small Anterior knee area defects. Moreover, we discuss the preparation techniques, therapeutic effects, and complications of freestyle-pattern V-Y advancement flaps in this article.
The study included two male and six female patients, with ages ranging from 21 to 65 years (average 46 years). The time from injury to hospital admission ranged from 2 h to 7 days. Two cases of car accident injuries, four cases of crushing injuries, and two cases of avulsion injury. The wound area ranged from 4 cm × 3 cm to 9 cm × 6 cm. There were no undermining injuries around the wound, and three cases had patellar or tendon exposure. Imaging showed no significant fractures or osteomyelitis.
The knee joint region has an abundant blood supply to the soft tissues of the skin, primarily from the muscular branches of the femoral artery, the genicular artery, and the superior and inferior medial and lateral genicular arteries. These arteries form an extensive anastomotic network, which serves as the vascular foundation for the survival of various pedicled flaps in the knee joint area (11).
The genicular artery usually originates from the femoral artery or occasionally from the popliteal artery and frequently gives off hidden and articular branches. The genicular artery has constant perforators that are closely connected to the surrounding vascular network. Each artery's contribution to skin nutrition has been quantified, providing the anatomical basis for the design and use of perforator flaps in the knee area.
In this study, flap repair surgery was performed 3 h–7 days after admission. The “V”-shaped flap was designed in a relatively relaxed area around the pre-knee wound, with the edge of the wound as the base. The length of the base was slightly longer than the width of the wound by about 1 cm, and the length of the flap was usually 2–3 times the width of the wound.
The procedure was performed under general anesthesia, with the patient in a supine position and the affected limb extended. A pneumatic tourniquet was applied at the root of the thigh. Thorough debridement of the wound was performed. The skin, subcutaneous tissue, and deep fascia on one side of the flap were first cut along the preoperative design line, and the flap was lifted from the deep fascia to the opposite side, carefully looking for perforators and protecting them properly.
The position and size of the flap were adjusted appropriately according to the number (as many as possible to ensure blood supply to the flap), position, and thickness of the perforators found, and large perforators located in the center of the flap were retained to ensure blood supply to the flap and increase the advancement distance of the flap.
The other side of the flap and the edge of the wound was cut in sequence, taking care to protect the nerve branches entering the flap. In this group of patients, the flap area was 6 cm × 5 cm–14 cm × 10 cm. The flap was freed under the deep fascia until only the perforators and cutaneous nerves supplying the flap were connected to the flap.
The tourniquet was released to observe the blood supply of the flap and to achieve complete hemostasis simultaneously. The “V”-shaped flap was advanced to cover the wound, and the wound edge was sutured in layers. The donor area was directly sutured, and the wound appeared “Y”-shaped after suturing. A drain was placed under the flap and connected to a negative pressure ball, routinely drained for 3–5 days, and removed as appropriate.
Postoperatively, the knee joint was routinely fixed with plaster until the suture was removed. Symptomatic treatments, including antibiotics for infection control, circulation improvement measures, anticoagulants, and muscle relaxants, were routinely administered. Observations were made on the time of capillary filling, color, and surface temperature of the skin flap to evaluate arterial perfusion and venous return of the flap. The sutures were removed after 2–3 weeks postoperatively.
The patient, a 37-year-old male, was admitted to the hospital 4 h after suffering from pain and bleeding due to an avulsion injury to his left knee caused by a fall. The skin defect area in the anterior region of the left knee was approximately 4 cm × 6 cm. The marginal abrasions were severe, and the wound was significantly contaminated. The ligament was exposed at the base, and no significant fracture signs were observed on the radiographs. Emergency debridement and VSD treatment were performed. The flap repair surgery was performed one week later.
In the preoperative design, a V-Y advancement flap with freestyle perforator as the pedicle was planned. After cutting the flap along the design line (the area was 12 cm × 7 cm), two perforators were found connected to the flap. The flap was advanced to repair the anterior knee wound, and the donor area was directly closed by suturing. Postoperative management included routine antibiotic administration, muscle relaxation, and anticoagulant treatment. After 72 h postoperatively, the flap survived. The sutures were removed two weeks postoperatively, and both the donor and recipient areas healed well.
At the one-month follow-up, the flap showed good color and texture, with a pleasing appearance, but slightly weak sensation; the flexion and extension functions of the knee joint were good (see Figure 1). An eight-month follow-up is shown in Figure 2.
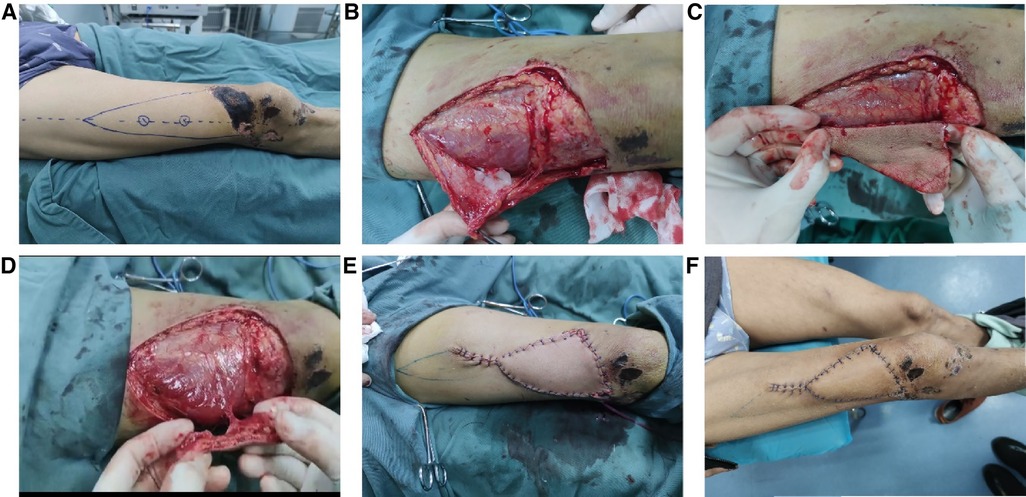
Figure 1. A typical case of repairing a small area of defect/necrosis in the anterior knee region using a V-Y flap with arbitrary perforator pedicle. The flap design (A), the surgical procedure of flap harvesting (B,C,D), the flap covering the defect area (E), and the condition of the flap 14 days postoperatively (F).

Figure 2. Follow-up images of a representative case at 8 months postoperative. Side view (A), 45° oblique view (B), frontal view (C), knee joint flexed at 90° (D), knee joint flexed at 180° (E).
In this group, four patients had flaps based on two perforators, two patients had flaps based on one perforator, and two patients had flaps based on three perforators. All flaps in this group survived at 72 h postoperatively, and both the donor and recipient site wounds healed at two weeks postoperatively. During the 1–12-month follow-up period, with an average follow-up of 8 months, the flaps showed no signs of congestion, had improved appearance, and slightly diminished sensation. The knee joint demonstrated good flexion and extension function. The patients’ conditions are outlined in Table 1.
The knee joint, being the largest, most complex, and highest weight-bearing joint in the human body, is prone to soft tissue defects around it due to factors such as trauma and infection (12). These injuries often involve exposed bones, joints, or ligaments, presenting significant challenges to clinicians. Several methods have been devised to repair soft tissue defects in the knee joint, each with their strengths and limitations (13–16). As the standards for wound repair escalate, the flap is required to not only repair the wound and minimize destruction to the donor area but also to retain functionality and meet high aesthetic demands (1).
Through literature review and understanding of the blood supply anatomy around the knee joint, we designed a V-Y advancement flap with arbitrary perforators as the pedicle to repair a small wound in the anterior knee area. This design leverages the advantages of traditional V-Y advancement flaps, offering small postoperative scar and direct closure of the donor area. The perforators, often unnamed, are arbitrary, and preoperative detection with a Doppler blood flow detector is not required (17). This flap does not cause damage to the main blood vessels and muscles, resulting in minimal destruction to the donor area. If necessary, moderately freeing the perforators towards the deep layer can increase the advancement distance of the flap, with the furthest advancement in our cases being 6 cm.
This flap is relatively simple to operate for surgeons, not requiring microsurgical techniques to anastomose vessels or nerves, making it suitable for clinical application in grassroots hospitals in China. The flap donor area can be directly sutured, avoiding the disadvantages of graft repair such as pigmentation, contraction, and scarring in the graft area. By using an advancement method to repair the wound, the flap avoids torsion and compression at the pedicle, ensuring the blood supply to the flap to the greatest extent.
The limitation of this flap is that it is only suitable for repairing smaller anterior knee wounds (advancement distance less or equal to 6 cm) and is not applicable for defects with deep cavity-like wounds. We consider wounds with an advancement distance greater than 6 cm or smaller than 2 cm unsuitable for this method. For wounds with an advancement distance smaller than 2 cm, the wound edge can be moderately freed and directly sutured, and postoperative influence on the knee joint activity is not significant. For wounds with an advancement distance larger than 6 cm, advancement may not fully cover the wound. Another limitation is the number and individual differences of perforators. Due to intraoperative manipulation and variation, the flap design may need to be adjusted according to the position of the perforators, which introduces some uncertainty.
During the treatment process, we must pay attention to ensure that there is no lurking avulsion injury around the wound preoperatively. One side of the flap is first incised, and the flap is lifted under the deep fascia to find the perforators and adjust the flap according to the quantity and thickness of the perforators. The quantity and size of the perforators vary from person to person, and special consideration is needed during the operation. During the operation, try to preserve as many perforators as possible to increase the blood supply to the flap, but too many perforators can affect the advancement distance of the flap. If you free the perforators towards the deep layer to increase the advancement distance, it will increase local damage and the operation time. According to our center's recommendation, a maximum of 3 perforators should be preserved. If a thicker perforator is observed intraoperatively, considering the advancement distance of the flap, other perforators can be ligated, and only 1 or 2 perforators are preserved. The subcutaneous tissue at the edge of the flap is sutured and fixed to the deep fascia to prevent separation that may affect the flap's blood supply. Finally, the flap is sutured in layers to reduce skin tension and minimize postoperative scarring.
In conclusion, our findings suggest that the V-Y advancement flap with arbitrary perforators as the pedicle exhibits substantial reliability in blood supply, simplicity in surgical operation, and mimicry of the texture and thickness of the anterior knee skin. In addition, the donor area can be directly sutured, which further enhances its applicability. This flap offers an effective approach to repairing smaller defects in the anterior knee area. Given its benefits and practicality, it merits wider adoption and promotion in clinical practice, particularly within grassroots hospitals. The technique represents an important addition to our armamentarium in reconstructive surgery, contributing to improved patient outcomes, and further research and clinical application are warranted.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by the Ethical Committee of the Changshu Hospital Affiliated with Soochow University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
DQ: Writing – original draft. LJ: Writing – original draft. GH: Writing – original draft. PD: Writing – original draft. DL: Writing – original draft. HL: Writing – original draft. MX: Writing – original draft. KW: Writing – original draft. XZ: Writing – original draft. XX: Writing – review & editing. JZ: Writing – review & editing. BY: Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
This study was supported by the Science and Technology Program of Changshu Health Commission (csws202005).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ramkumar R,RB,S, Venkatramani H. Soft tissue coverage for defects around the knee joint. Indian J Plast Surg. (2019) 52(1):125–33. doi: 10.1055/s-0039-1688536
2. Kerfant N, Ta P, Trimaille A, Henry AS, Dubrana F, Le Nen D, et al. Soft tissue coverage options around the knee. Ann Chir Plast Esthet. (2020) 65(5-6):517–23. doi: 10.1016/j.anplas.2020.07.003
3. Johns WL, Layon D, Golladay GJ, Kates SL, Scott M, Patel NK. Preoperative risk factor screening protocols in total joint arthroplasty: a systematic review. J Arthroplasty. (2020) 35(11):3353–63. doi: 10.1016/j.arth.2020.05.074
4. Rad AN, Christy MR, Rodriguez ED, Brazio P, Rosson GD. The anterior tibialis artery perforator (ATAP) flap for traumatic knee and patella defects: clinical cases and anatomic study. Ann Plast Surg. (2010) 64(2):210–6. doi: 10.1097/SAP.0b013e3181a13dd6
5. Hallock GG. Direct and indirect perforator flaps: the history and the controversy. Plast Reconstr Surg. (2003) 111(2):855–65. quiz 866. doi: 10.1097/01.PRS.0000040462.38363.C7
6. Qian D, Zheng J, Wang K, Lu H, Yu B, Xu M, et al. Clinical application of posterior tibial artery or peroneal artery perforator flap in curing plate exposure after ankle fracture fixation. Int Wound J. (2023) 21(2):e14423. doi: 10.1111/iwj.14423
7. Zhang J, Lu L, Jiang H. Research progress of soft tissue defect repair around the knee. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. (2012) 26(9):1138–41.23057366
8. Hallock GG. The complete nomenclature for combined perforator flaps. Plast Reconstr Surg. (2011) 127(4):1720–9. doi: 10.1097/PRS.0b013e31820a662b
9. Osei DA, Rebehn KA, Boyer MI. Soft-tissue defects after total knee arthroplasty: management and reconstruction. J Am Acad Orthop Surg. (2016) 24(11):769–79. doi: 10.5435/JAAOS-D-15-00241
10. Kozusko SD, Liu X, Riccio CA, Chang J, Boyd LC, Kokkalis Z, et al. Selecting a free flap for soft tissue coverage in lower extremity reconstruction. Injury. (2019) 50(Suppl 5):S32–9. doi: 10.1016/j.injury.2019.10.045
11. Hirtler L, Lubbers A, Rath C. Vascular coverage of the anterior knee region—an anatomical study. J Anat. (2019) 235(2):289–98. doi: 10.1111/joa.13004
12. Flandry F, Hommel G. Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev. (2011) 19(2):82–92. doi: 10.1097/JSA.0b013e318210c0aa
13. Qian YL. One-stage repair of a soft tissue defect around the knee joint with a posterior calf fascio-cutaneous island flap. Zhonghua Zheng Xing Shao Shang Wai Ke Za Zhi. (1988) 4(2):95–7.3151473
14. Yang R, Liu Y, Zhu S, Zang M, Chen B, Li S. Clinical application of superior lateral genicular artery perforator propeller flap in repair of soft-tissue defects around knee joint. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. (2021) 35(12):1603–8. doi: 10.7507/1002-1892.202106024
15. Luca-Pozner V, Delgove A, Kerfant N, Karra A, Herlin C, Chaput B. Medial sural artery perforator flap for leg and knee coverage: extended skin paddle with 2 perforators. Ann Plast Surg. (2020) 85(6):650–5. doi: 10.1097/SAP.0000000000002356
16. Shen Y, Ma C, Hu X, Wang C, Zhang C. Tissue flap repair strategy for severe defects of skin and soft tissue around the knee joints. Zhonghua Shao Shang Za Zhi. (2015) 31(5):331–6.26714400
Keywords: V-Y advanced flap, anterior region of knee, soft tissue injury, freestyle perforator flap, wound healing
Citation: Qian D, Jin L, Huang G, Dai P, Li D, Lu H, Xu M, Wang K, Zhong X, Xu X, Zhang J and Yu B (2024) The clinical application of V-Y advanced flap pedicled with freestyle perforator flap for repairing small range defects in the anterior knee region. Front. Surg. 11:1364340. doi: 10.3389/fsurg.2024.1364340
Received: 2 January 2024; Accepted: 2 May 2024;
Published: 13 May 2024.
Edited by:
Xue Qu, East China University of Science and Technology, ChinaReviewed by:
Jose M. Lasso, Hospital General Universitario Gregorio Marañón, Spain© 2024 Qian, Jin, Huang, Dai, Li, Lu, Xu, Wang, Zhong, Xu, Zhang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaochen Xu, NTI3MTE0MzYwQHFxLmNvbQ==
Jianchao Zhang, emhhbmdqaWFuY2hhbzEwOEAxNjMuY29t
Bin Yu, eXViaW41MTIyQDE2My5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.