
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 21 February 2024
Sec. Neurosurgery
Volume 11 - 2024 | https://doi.org/10.3389/fsurg.2024.1361040
This article is part of the Research Topic Training and Education in Neurosurgery: Strategies and Challenges for the Next Ten Years, volume II View all 11 articles
 Despoina Chatzopoulou1,†
Despoina Chatzopoulou1,† Arif Hanafi Bin Jalal2,†
Arif Hanafi Bin Jalal2,† Danail Stoyanov3
Danail Stoyanov3 Hani J. Marcus3,4,‡
Hani J. Marcus3,4,‡ Anand S. Pandit4,5*‡
Anand S. Pandit4,5*‡
Introduction: Informed consent is a fundamental component in the work-up for surgical procedures. Statistical risk information pertaining to a procedure is by nature probabilistic and challenging to communicate, especially to those with poor numerical literacy. Visual aids and audio/video tools have previously been shown to improve patients' understanding of statistical information. In this study, we aimed to explore the impact of different methods of risk communication in healthy participants randomized to either undergo the consent process with visual aids or the standard consent process for lumbar puncture.
Material and methods: Healthy individuals above 18 years old were eligible. The exclusion criteria were prior experience of the procedure or relevant medical knowledge, lack of capacity to consent, underlying cognitive impairment and hospitalised individuals. After randomisation, both groups received identical medical information about the procedure of a lumbar puncture in a hypothetical clinical scenario via different means of consent. The control group underwent the standard consent process in current clinical practice (Consent Form 1 without any illustrative examples), whereas the intervention group received additional anatomy diagrams, the Paling Palette and the Paling perspective scale. Anonymised questionnaires were received to evaluate their perception of the procedure and its associated risks.
Results: Fifty-two individuals were eligible without statistically significant differences in age, sex, professional status and the familiarity of the procedure. Visual aids were noted to improve the confidence of participants to describe the risks by themselves (p = 0.009) and participants in the intervention group felt significantly less overwhelmed with medical information (p = 0.028). The enhanced consent process was found to be significantly more acceptable by participants (p = 0.03). There was a trend towards greater appropriateness (p = 0.06) and it appeared to have “good” usability (median SUS = 76.4), although this also did not reach statistical significance (p = 0.06)
Conclusion: Visual aids could be an appropriate alternative method for medical consent without being inferior regarding the understanding of the procedure, its risks and its benefits. Future studies could possibly compare or incorporate multiple interventions to determine the most effective tools in a larger scale of population including patients as well as healthy individuals.
Informed consent is a fundamental component in the work-up for surgical procedures. Statistical risk information pertaining to a procedure is by nature probabilistic and challenging to communicate, especially to those with poor numerical literacy (1). In the context of health literacy, numeracy refers to a person's ability to understand and interpret clinical and public health data (1). This is considered to be low in the general population with most adults having difficulty in converting small frequencies such as “1 in 1,000” to 0.1% (2).
In addition to individual patient factors, risk perception is affected by different formats of presentation resulting in “framing bias” (3, 4). This phenomenon refers to variable decision outcomes depending on the different modes of presentation of identical data among individuals. Healthcare professionals may communicate statistical risk information using descriptive terms such as “uncommon” or “rare” or as percentages and proportions. Risks are often verbally explained prior to obtaining consent without the acknowledgement of patients' numerical skills and without the use of other aids. In neurosurgery, patient recall of risks without their associated probabilities is noted to be poor with less than 50% of risks being retained (5, 6). This percentage further decreases over time following the original consent process and post-operatively (6). Ensuring patients have an adequate understanding of statistical risk is vital to prevent potential litigation with “lack of informed consent” being a factor in up to 40% of neurosurgical medicolegal cases (7).
The impact of several decision aids on patients' overall understanding of surgical or interventional procedures has been studied (8–11). However few studies compare multiple formats concurrently (9, 12) while focusing on patient understanding of statistical risk. Visual aids and audio/video tools have been shown to improve patients' understanding of statistical information (8, 9, 13, 14). Our study demonstrates the use of visual statistical risk communication adjuncts in a simulated procedural consent of a lumbar puncture and presents implementation outcome measures. We analyse participants’ understanding of the procedure, but also more specifically, their understanding of procedural complications, associated numerical probability and attitudes related to surgical consent.
Inclusion criteria were healthy individuals above 18 years old not requiring a lumbar puncture and without any underlying cognitive impairment. Exclusion criteria were individuals with prior experience receiving, performing or observing the procedure, individuals lacking capacity to consent and hospitalised individuals. The educational background of the participants varied from secondary level of education to postdoctoral level of studies within and outside the medical field.
The video recording was made with the use of Vyond (Vyond, San Mateo, Ca), a cloud-based video animation tool. The same voice recording was used in both groups, ensuring the content of the medical information is identical in both groups. While both groups received identical medical information and content regarding hypothetical clinical scenarios in which an intervention was consented for, the means of consent differed (Figure 1). The control group had the same risks verbally explained without any aids as is typical for pre-operative surgical consent. The intervention group received the statistical information in the form of visual aids—anatomy diagrams and Paling scales (Figures 2, 3) (15). At the end of the videos, the participants of both groups were presented with a written consent form as it is used in clinical practice summarising the name, the risks and the benefits of the procedure. It was requested that participants sign the consent form as they would do in clinical practice.
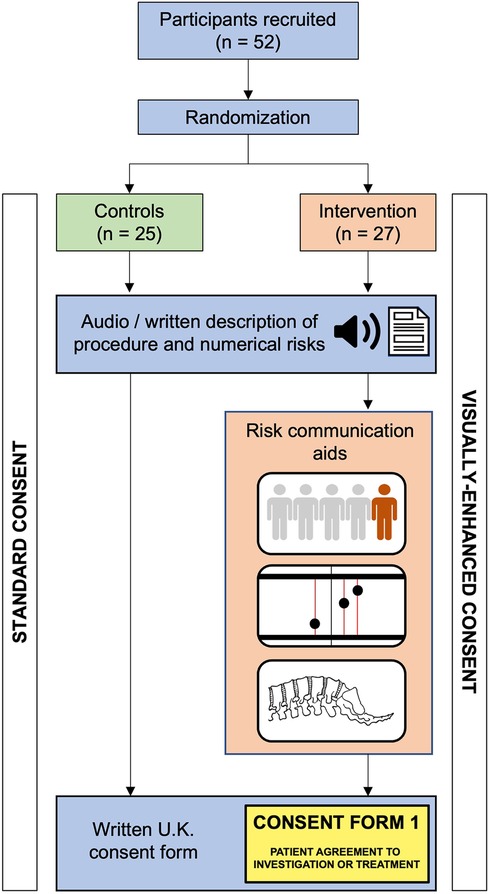
Figure 1. Flow diagram of participants allocated to the intervention (visually-enhanced consent) or control group.
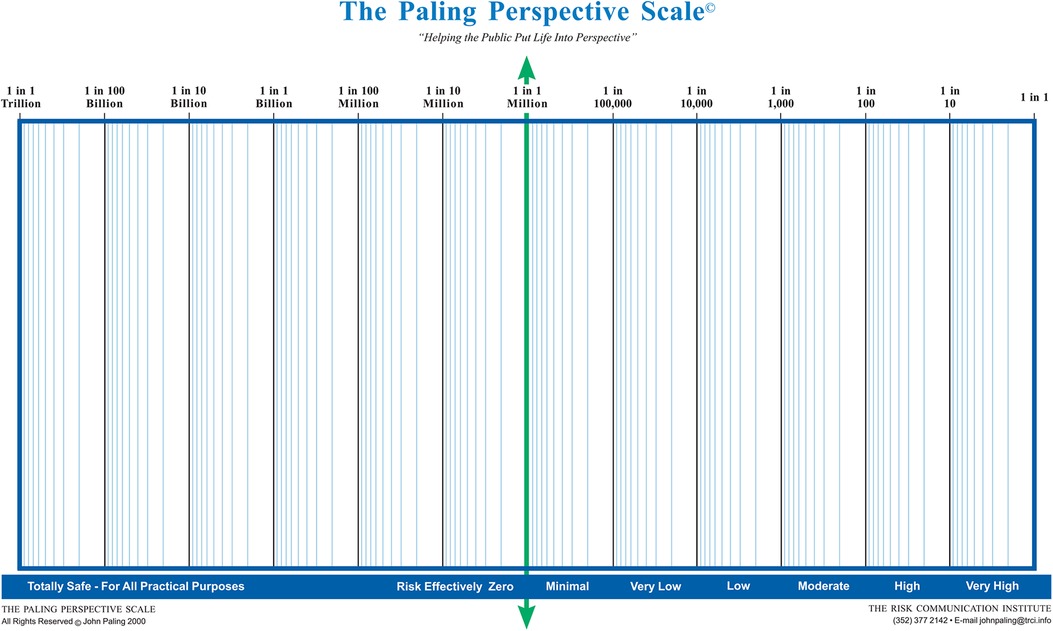
Figure 2. The paling perspective scale. Reproduced with permission from The Risk Communication Institute.
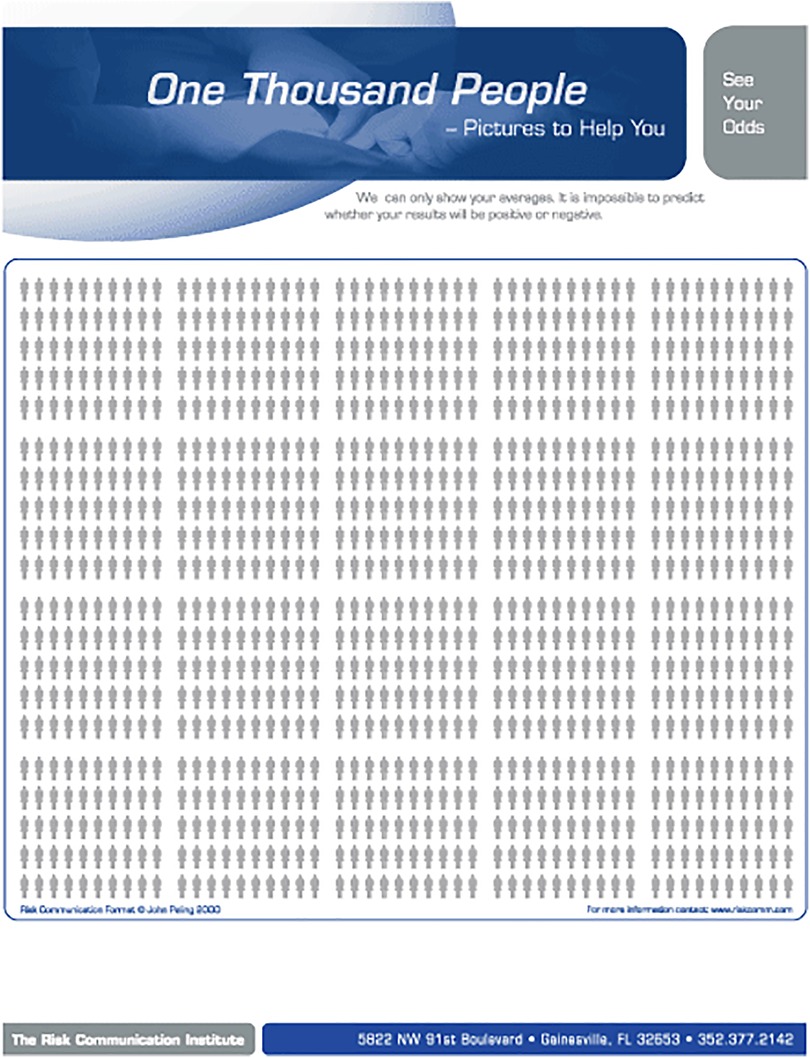
Figure 3. One thousand people figure. Reproduced with permission from The Risk Communication Institute.
Please find the relevant video links below:
• Group A (Control Group): https://youtu.be/-QuOp-BTEKM”\h
• Group B (Visual Aid Group): https://youtu.be/wFe4KXEq8hw”\h
Participant knowledge and feedback with the respective consent process were assessed using a 41-item questionnaire developed in Qualtrics (Qualtrics, Provo, UT), the different sections and their respective questions are detailed in Table 1. The first section consisted of demographic information including age, gender and familiarity with the procedure. The second section required participants to rate their agreement to a series of seven statements specifically written for the study using a 5-point Likert scale. The intervention group received an additional three statements relating to the helpfulness of the three visual aids used in the video (Anatomy diagram, ten-man diagram and relative risk diagram). The ten-man diagram and the relative risk diagram are based on the Paling diagram and Paling Palette respectively with the permission of the Risk Communication Institute (Figures 2, 3) (15). A free-text prompt asking for additional feedback to improve the consent process was also included. This was followed by seven multiple choice questions assessing participants' knowledge on the procedure. The final section consisted of 19 questions to assess the implementation of the process in clinical practice using four validated scales (16, 17).
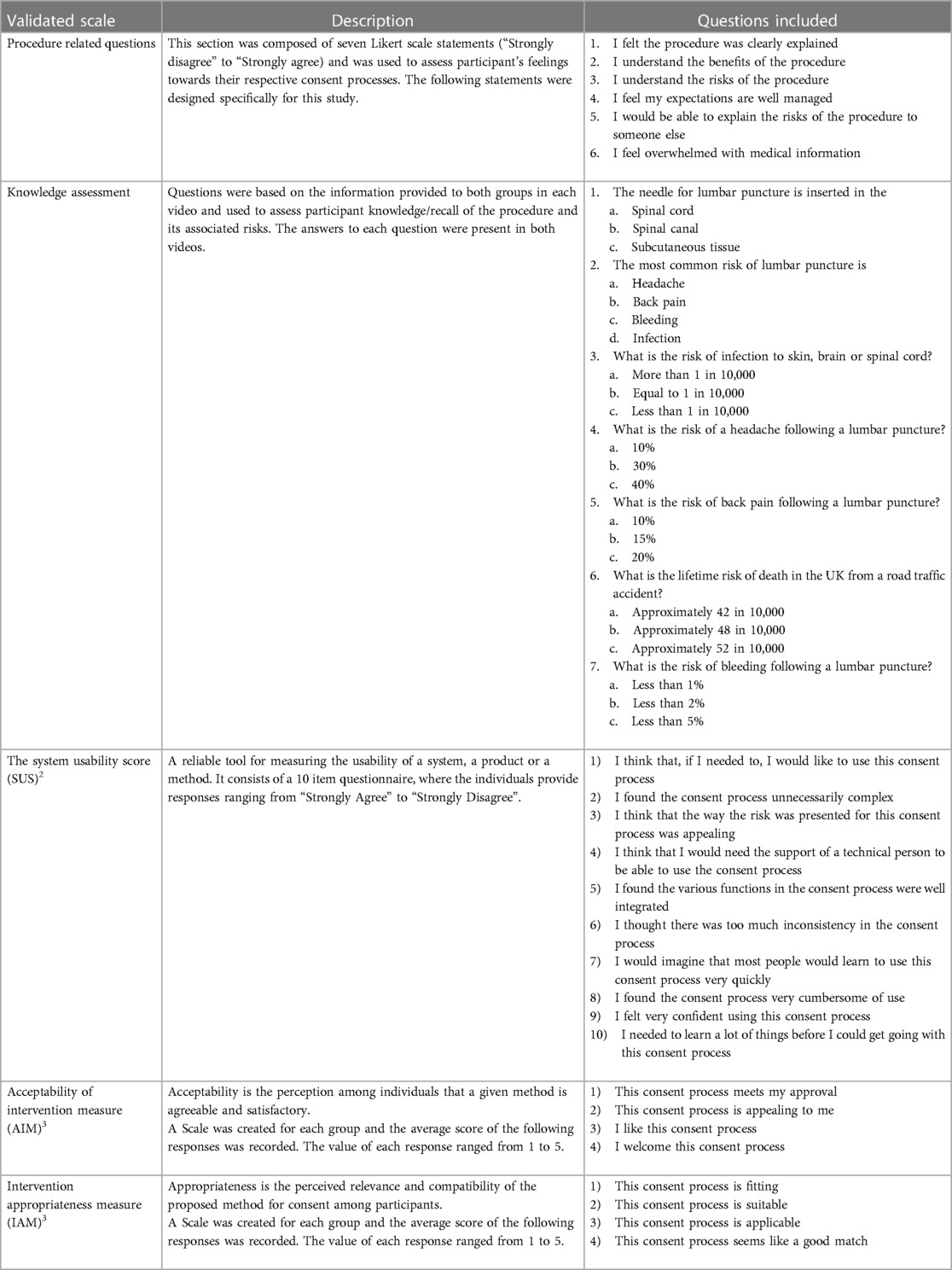
Table 1. Questions included in the questionnaire relating to knowledge of the procedure, participant sentiment, usability, acceptability and appropriateness.
The study was advertised online via social media and mailing lists within our institutional academic community therefore we are not able to report the number of individuals approached for the study. Furthermore, given the anonymised nature of the study it is not known what proportion of individuals directly approached by study staff completed the survey. Upon clicking the link to the questionnaire, participants were randomised in a 1:1 ratio using Qualtrics' built in randomization software to receive either the control group with the standard informed consent process or the intervention group which featured various visual aids. Researchers were blinded to the assignment of individual participants to the respective groups. Participant recruitment took place over a two-month period from 27th March 2022 to 26th May 2022. Data collection was concluded when the target sample size was reached. Participants completed anonymised questionnaires relating to how they recalled and perceived statistical risks, on their understanding of the procedure and how usable, acceptable, and appropriate their consent method was, using validated scales (17).
A sample size calculation found a minimum of 25 participants in each group was required for a significant difference of 0.4 points between groups based on a 5-point Likert scale (Cohen's d = 0.8, alpha = 0.05, power = 0.80, GPower v = 3.1). All statistical analysis was performed in RStudio (RStudio Team, Boston, MA). Normality of the data was assessed using the Kolmogorov–Smirnov test, and by visually inspecting the distribution. If data was non-parametric, the Mann–Whitney U-test was used to assess the differences between the control and intervention groups, with a p-value < 0.05 being considered as significant.
This study's protocol was reviewed and approved by an institutional ethics committee (UCL Research Ethics Committee Project ID: 21837/001). Prior to being able to complete the questionnaire, participants were asked to confirm they meet the inclusion criteria of the study and voluntarily consent to completing the study through Qualtrics. Participants were directed to a participant information sheet within the study. Names and contact information of participants was not collected. Our study was retrospectively registered on ClinicalTrial.gov on 8th February 2023 (NCT05717465).
52 participants were included in the study. The demographics of the eligible population are presented after the randomisation, with reference to the age, sex, professional status, understanding of, and prior familiarity with the procedure between groups (Table 2). There was no statistical difference in numerical risk recall, and those in the intervention (visually enhanced consent) group were not inferior in their subjective understanding of the procedural benefits (p = 0.29) (Table 3). However, the intervention group seemed to have a better understanding of the risks (p = 0.05), they thought they could better explain the risks to others (p = 0.01), and they seemed to feel less overwhelmed with information (p = 0.03). Furthermore, the enhanced consent process was found by participants to be significantly more acceptable (p = 0.03). It showed a trend towards greater appropriateness (p = 0.06) and it appeared to have “good” usability (median SUS = 76.4), although this also did not reach statistical significance (p = 0.06).
Our study suggests that that visual risk communication adjuncts may offer some advantages when compared to traditionally obtained surgical consent, particularly with reference to subjective understanding and attitudes toward procedural risks. Statistically significant improvements were noted in the trial group regarding the ability to explain risks to others and greater acceptability and good usability of the consent adjunct, whilst also feeling less overloaded with medical information.
We acknowledge limitations in our approach, including the choice of individuals and the intervention. Recruiting healthy adults allowed us to test our hypothesis in a controlled simulated setting without bioethical concerns, but this does not fully replicate the atmosphere and anxieties associated with consent in hospital, nor having the procedure performed in the context of experiencing a disease process. The interventional choice of a lumbar puncture although simple remains a procedure that requires written informed consent and carries non-trivial complications (18). Further work should assess procedures of greater complexity, and the impact of framing bias, namely, whether consent outcomes depend on the mode and the conditions of presentation (3, 19). Another limitation of the study is the overall high rate of literacy in both groups according to the table of demographics. In this case, the numerical literacy of the participants could be considered higher than expected in the general surgical population and therefore not easily generalisable.
This controlled trial evaluates the utility of risk communication adjuncts for surgical consent and contributes to this expanding field of bioethics. The surgical decision-making process is not only related to risk perception, but also to risk acceptance in accordance with an individual's threshold for specific postoperative complications and the frequency in which they occur (20). To make consent fully informed, patient decision-making should be in line with, or adapted to, their probabilistic understanding of the intervention. Considering the findings of our study, we believe that visual risk communication tools could enable a more informed consent process. The systematic application of validated and widely accepted psychometric tools to evaluate patients' perception of a procedure and its associated risks in the field of medical consent is required to collect further supporting evidence. This proof-of-concept study provides a suggested methodology that could be useful in future larger-scale patient populations studies to translate our conclusions into clinical practice.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by University College London Research Ethics Committee. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
DC: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft. AJ: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft. DS: Conceptualization, Methodology, Supervision, Writing – review & editing. HM: Conceptualization, Methodology, Supervision, Writing – review & editing. AP: Conceptualization, Methodology, Supervision, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article.
HJM is supported by grants from the Wellcome (203145Z/16/Z) EPSRC (NS/A000050/1) Centre for Interventional and Surgical Sciences, National Institute for Health Research (NIHR) Biomedical Research Centre at University College London.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rothman RL, Montori VM, Cherrington A, Pignone MP. Perspective: the role of numeracy in health care. J Health Commun. (2008) 13(6):583–95. doi: 10.1080/10810730802281791
2. Gigerenzer G, Gaissmaier W, Kurz-Milcke E, Schwartz LM, Woloshin S. Helping doctors and patients make sense of health statistics. Psychol Sci Public Interest. (2007) 8(2):53–96. doi: 10.1111/j.1539-6053.2008.00033.x
3. Perneger TV, Agoritsas T. Doctors and patients’ susceptibility to framing bias: a randomized trial. J Gen Intern Med. (2011) 26(12):1411–7. doi: 10.1007/s11606-011-1810-x
4. Timmermans D, Molewijk B, Stiggelbout A, Kievit J. Different formats for communicating surgical risks to patients and the effect on choice of treatment. Patient Educ Couns. (2004) 54(3):255–63. doi: 10.1016/S0738-3991(03)00238-6
5. Krupp W, Spanehl O, Laubach W, Seifert V. Informed consent in neurosurgery: patients’ recall of preoperative discussion. Acta Neurochir (Wien. (2000) 142(3):233–8.; discussion 8-9. doi: 10.1007/s007010050030
6. Saigal R, Clark AJ, Scheer JK, Smith JS, Bess S, Mummaneni PV, et al. Adult spinal deformity patients recall fewer than 50% of the risks discussed in the informed consent process preoperatively and the recall rate worsens significantly in the postoperative period. Spine (Phila Pa 1976). (2015) 40(14):1079–85. doi: 10.1097/BRS.0000000000000964
7. Shlobin NA, Sheldon M, Lam S. Informed consent in neurosurgery: a systematic review. Neurosurg Focus. (2020) 49(5):E6. doi: 10.3171/2020.8.FOCUS20611
8. Xia T, Zhu YB, Zeng YB, Chen C, Wang SL, Zhao SB, et al. Video education can improve awareness of risks for patients undergoing endoscopic retrograde cholangiopancreatography: a randomized trial. J Dig Dis. (2019) 20(12):656–62. doi: 10.1111/1751-2980.12824
9. Shukla AN, Daly MK, Legutko P. Informed consent for cataract surgery: patient understanding of verbal, written, and videotaped information. J Cataract Refract Surg. (2012) 38(1):80–4. doi: 10.1016/j.jcrs.2011.07.030
10. Aremu SK, Alabi BS, Segun-Busari S. The role of informed consent in risks recall in otorhinolaryngology surgeries: verbal (nonintervention) vs written (intervention) summaries of risks. Am J Otolaryngol. (2011) 32(6):485–9. doi: 10.1016/j.amjoto.2010.09.012
11. Gyomber D, Lawrentschuk N, Wong P, Parker F, Bolton DM. Improving informed consent for patients undergoing radical prostatectomy using multimedia techniques: a prospective randomized crossover study. BJU Int. (2010) 106(8):1152–6. doi: 10.1111/j.1464-410X.2010.09309.x
12. Gett RM, Cooray AR, Gold D, Danta M. Evaluating informed consent for colonoscopy. Surg Laparosc Endosc Percutan Tech. (2014) 24(4):345–52. doi: 10.1097/SLE.0000000000000053
13. Raymond BL, Wanderer JP, Hawkins AT, Geiger TM, Ehrenfeld JM, Stokes JW, et al. Use of the American college of surgeons national surgical quality improvement program surgical risk calculator during preoperative risk discussion: the patient perspective. Anesth Analg. (2019) 128(4):643–50. doi: 10.1213/ANE.0000000000003718
14. Habib SB, Sonoda L, See TC, Ell PJ, Groves AM. How do patients perceive the benefits and risks of peripheral angioplasty? Implications for informed consent. J Vasc Interv Radiol. (2008) 19(2 Pt 1):177–81. doi: 10.1016/j.jvir.2007.10.016
15. Paling J. Strategies to help patients understand risks. Br Med J. (2003) 327(7417):745–8. doi: 10.1136/bmj.327.7417.745
16. Weiner BJ, Lewis CC, Stanick C, Powell BJ, Dorsey CN, Clary AS, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci. (2017) 12(1):108. doi: 10.1186/s13012-017-0635-3
17. Brooke J. SUS—a quick and dirty usability scale. Usability evaluation in industry. 1st edn. Taylor & Francis (1996). p. 189–94.
18. Sarela AI, Thomson M. Balancing law, ethics and reality in informed consent for surgery. Ann R Coll Surg Engl. (2014) 96(5):329–30. doi: 10.1308/003588414X13946184901803
19. Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of medical research council guidance. Br Med J. (2021) 374:n2061. doi: 10.1136/bmj.n2061
Keywords: informed consent, patient communication aids, health literacy, visual aids, health numeracy
Citation: Chatzopoulou D, Jalal AHB, Stoyanov D, Marcus HJ and Pandit AS (2024) Improving risk communication: a proof-of-concept randomised control trial assessing the impact of visual aids for neurosurgical consent. Front. Surg. 11:1361040. doi: 10.3389/fsurg.2024.1361040
Received: 24 December 2023; Accepted: 5 February 2024;
Published: 21 February 2024.
Edited by:
Cesare Zoia, San Matteo Hospital Foundation (IRCCS), ItalyReviewed by:
Baddr Shakhsheer, The University of Chicago, United States© 2024 Chatzopoulou, Jalal, Stoyanov, Marcus and Pandit. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anand S. Pandit YS5wYW5kaXRAdWNsLmFjLnVr
†These authors share first authorship
‡These authors share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.