- 1Department of Orthopedic Surgery, Rutgers New Jersey Medical School, Newark, NJ, United States
- 2Department of Plastic and Reconstructive Surgery, Linkou Medical Center and Chang Gung Medical College and Chang Gung University, Chang Gung Memorial Hospital, Taoyuan, Taiwan
- 3Department of Clinical Sciences, Umeå University, Umeå, Sweden
- 4Department of Surgical and Perioperative Sciences, Faculty of Medicine, Umeå University, Umeå, Sweden
Background: We analyzed trends in age at surgery and surgical approach over time and geography.
Methods: We performed a systematic review according to PRISMA-IPD guidelines to include individual patient data. Collected data included age at surgery, location of surgery, and surgical approach. The surgical approach was independently categorized as the exploration of the brachial plexus (EBP) or nerve transfer without root exploration (NTwoRE). EBP was defined as exploring the brachial plexus in the supraclavicular fossa and applying a choice of coaptation procedures. NTwoRE included those sourcing donor nerves from, or entirely occurring outside of the plexus without exploring the root of the brachial plexus.
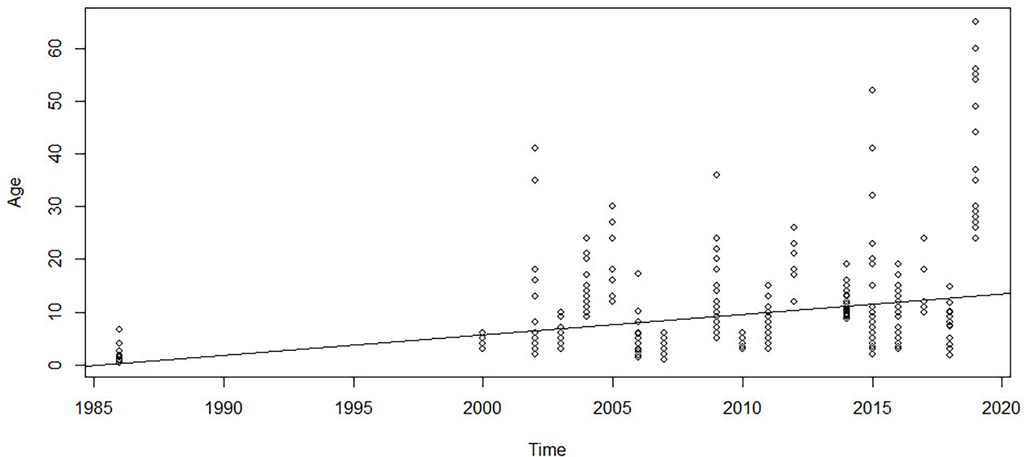
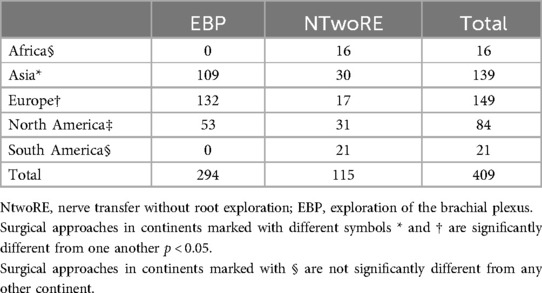
Results: Regression analysis of age at surgery 1985–2020 showed that age at BPBI surgery is rising (p < 0.05). Surgery was performed at a younger age in patients from Europe (7.06 ± 7.77 months) and Asia (7.58 ± 5.33 months) than those from North America (10.44 ± 5.01 months) and South America (14.71 ± 4.53 months) (p < 0.05). NTwoRE was more common in North America (37%) and least common in Europe (12%). Age at EBP was 7.2 ± 5.77 months, and age at NTwoRE was 15.85 ± 13.18 months (p < 0.05). The incidence of NTwoRE is increasing time.
Conclusions: Age at NBPP surgery is increasing over time. Regional differences exist in age at NBPP surgery. Approaches to NBPP surgery that avoid exploration of BP roots are becoming more popular. Age at EBP is lower than age at NTwoRE.
Introduction
Many factors potentially affect the outcome of neonatal brachial plexus palsy (NBPP), including the timing of diagnosis, severity of the palsy, surgeons’ experiences, timing of the approach, and different surgical approaches. However, the existing literature is often difficult to interpret because of different outcome measures and variability in the severity of plexus injuries. Because NBPP is a rare condition, much of the literature on surgical treatment is of a low level of evidence, with few randomized clinical trials (1). Surgeon preference affects decision-making in the timing and approach to surgery, as do several difficult-to-quantify factors: previous training, exposure to different techniques, volume of practice, and specialty of the surgeon. While some authors favor extensive proximal exploration of the nerve roots of the plexus, others with similar experience prefer nerve transfers without exploring the roots or orthopedic procedures that avoid nerve manipulation entirely (2).
Age at surgery has been investigated for its role in NBPP patient outcomes, with numerous authors providing recommendations on the topic. Gilbert and Tassin recommended surgery before 3 months (3), Chuang et al. before 6 months (4), and Clarke and Curtis before 9 months (5). More recently, a multicenter study from Bauer found no difference in surgical outcomes between groups aged 4.2 months and 10.7 months, while a systematic review from Srinivasan et al. suggested that intervention before 6 months was associated with improved Mallet scores (6, 7).
Initially, the technique of NBPP microsurgery was the exploration of supraclavicular fossa and arduous dissection around the scarred brachial plexus, with selective neurolysis and nerve grafting. Gradually, through the innovation of pioneering surgeons such as Oberlin (8) and Mackinnon (9), close target nerve transfers were developed and became adopted in the treatment of NBPP as well as traumatic adult brachial plexus injuries (10). In recent years, there were reports of NBPP patients with partial palsies, treated entirely with nerve transfers close to the target, without exploring the brachial plexus. The decision-making in the choice of treatment of NBPP is primarily influenced by the severity of the palsy, with total palsy necessitating brachial plexus exploration, preferably performed early, based on the biology of nerve injury in an immature nervous system (11). However, the rationale behind choosing not to explore the plexus in the group of patients with partial palsies has not been studied. Similarly, there are no studies investigating whether the introduction of nerve transfers in NBPP has proceeded uniformly across the world.
The objective of this study is to systematically review individualized patient data (IPD) over the past 40 years of NBPP surgery globally to identify trends in surgical approach and age at surgery over time and by continent. The results offer insight into the impact of influential publications and techniques over time and help practitioners understand influences guiding their international colleagues' thinking.
Methods
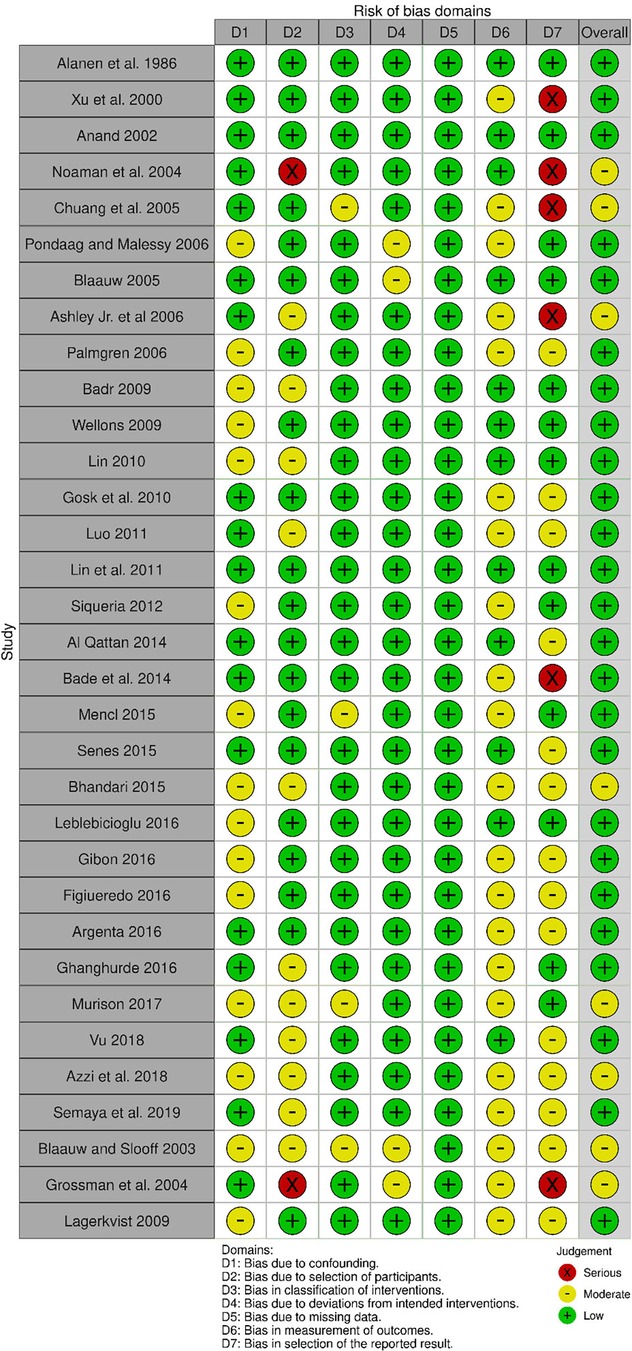
We searched PubMed, Cochrane, Web of Science, and the Cumulative Index to Nursing and Allied Health Literature databases in accordance with PRISMA-IPD guidelines. Boolean searches were performed using the terms “brachial plexus,” “injury,” “palsy,” “nerve plexus,” “upper plexus,” “pediatric,” “surgery,” and others. Search filters were non-full-text, non-human studies, review papers, commentaries, editorials, and non-English papers. Studies were included if they involved surgical treatment of NBPP, included >2 patients, included patient-level data, and included a description of surgery. Studies were excluded if they were irrelevant to NBPP; were case studies or reviews; were not microsurgical; were adult-only; were imaging studies or did not include patient-level data. We contacted authors of otherwise eligible papers missing IPD to request access to the full dataset. Disagreements regarding eligibility were resolved by senior authors AC and AM. The included studies were assessed for risk of bias using the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS)-1 tool (12). Four authors (ML, JS, KJ, and YS) graded the risk of bias. AM and AC resolved conflicts. Designations were made relative to the risk of bias for collected data, not the paper.
Data collected included age at surgery, location of surgery, and surgical approach. The location of surgery was based on continent definitions from the CIA World Factbook (13). The year associated with patient data was taken from the publication date of the article. The surgical approach was independently categorized by both senior authors (AM and AC) as the exploration of the brachial plexus (EBP) or nerve transfer without root exploration (NTwoRE). EBP was defined as exploring the brachial plexus in the supraclavicular fossa and applying a choice of coaptation procedures such as nerve grafting, neurolysis, or nerve transfers with targets in supraclavicular or infraclavicular fossa such as roots, divisions, and trunks from variety of donors, such as spinal accessory nerve, hypoglossal nerve, and contralateral C7 transfer or pectoral nerves. NTwoRE included those sourcing donor nerves from or entirely occurring outside of the plexus without exploring the root of the brachial plexus, such as intercostal nerve transfer, spinal accessory to suprascapular nerve transfer, Oberlin or MacKinnon procedure, and radial to axillary nerve transfer.
Statistical analysis of age at surgery vs. time was performed using simple linear regression. Age at surgery vs. continent was analyzed using ANOVA and then pairwise comparisons using t-tests with adjusted p-values, using the methods introduced by Bonferroni, Holm (14), Hochberg (15), Hommel (16), Benjamini and Hochberg (17), and Benjamini and Yekutieli (18). Statistical analysis of the proportion of NTwoRE surgeries over time was performed using logistic regression with a single numerical covariate. The proportion of NTwoRE surgeries in each continent was analyzed using logistic regression with categorical covariates. Statistical significance was defined as p < 0.05. Statistical analysis was performed using RStudio version 1.3.1093.
Results
Starting with 3,009 titles, duplicates were removed until 2,936 titles remained. The screening was performed for the relevance of titles, after which 516 remained. Abstracts of these titles were screened, after which 160 remained. Two authors, ML and JS, then reviewed the full-text manuscripts of these 160 abstracts, and 93 were deemed suitable. Additionally, 57 relevant references were sourced from these 160 full-text manuscripts, cross-checked, and screened. Seventeen additional full-text manuscripts were added this way, for a total of 110 total texts in our database (Figure 1). Of these, 34 contained relevant IPD from a total of 409 patients (Table 1). We found an overall low to moderate risk of bias in all included studies (Figure 2). The bias that existed was largely a result of the selection of outcome measures.
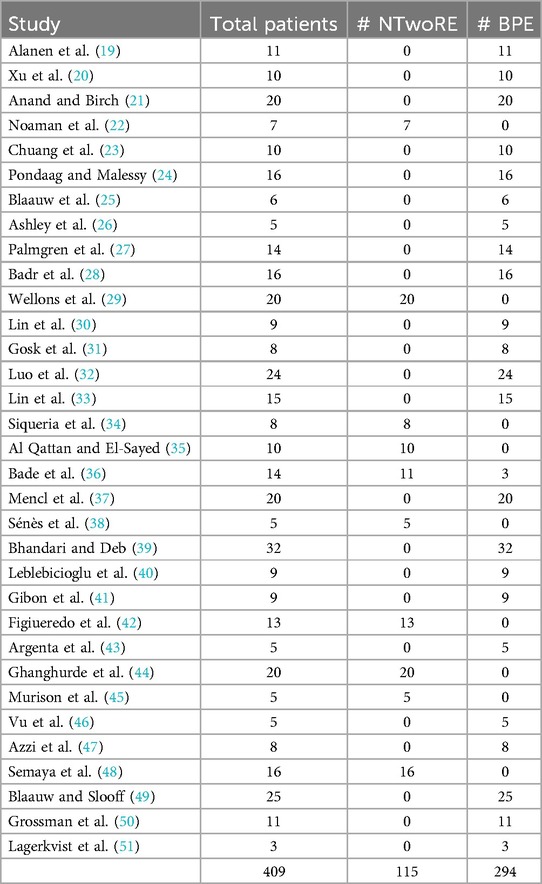
Table 1. All included studies in this research study are seen above with the author and publication year.
The mean patient age at surgery was 9.6 ± 9.2 months. The number of patients and ages at surgery in each continent are shown in Table 2. The surgical approach was NTwoRE in 115 cases and EBP in 294 cases. The number of patients and surgical approach in each continent are shown in Table 2. The average age of an EBP exploration was 7.2 ± 5.77 months, which was significantly different from the average age of an NTwoRE exploration of 15.85 ± 13.18 months (p < 0.05).
Simple linear regression was used to test if the years from 1984 to 2020 significantly predicted the age at surgery of patients undergoing brachial plexus surgery. The fitted regression model was as follows: age at surgery = −772.14 + 0.389 × (year of surgery). The overall regression was statistically significant [R2 = 0.075, F (1, 407), p < 0.05, Figure 3]. It was found that the year of surgery significantly predicted age at surgery (β = 0.382, p < 0.01), suggesting that there is a trend of increasing age at surgery over the years. The relationship between year and proportion of cases that were NTwoRE was analyzed using logistic regression. The odds of NTwoRE occurring increased with each year starting in 1985 (p < 0.05, Figure 4).
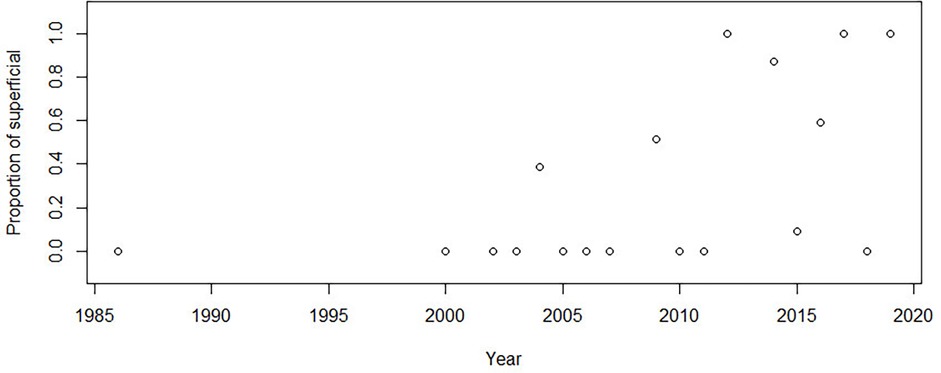
Figure 4. Y-axis proportion of surgeries that were nerve transfers without root exploration (ntwoRE) vs. x-axis year.
Comparisons between ages at surgery in different continents were tested by ANOVA with ad hoc pairwise t-tests using pooled standard deviation. The average age at surgery was youngest in Europe (7.06 ± 7.77 months) and Asia (7.6 ± 5.33 months) and significantly older in North America (10.44 ± 5.01 months) and South America (14.71 ± 4.53 months). Age at surgery in Africa (40.56 ± 13.94) was still higher than that in North and South America. The pairwise comparison proved that those differences were significant (p < 0.05, Figure 5, Table 3). Surgical approaches across continents were compared using logistic regression. The odds of an NTwoRE approach occurring in North America (37%) were higher than occurring in Europe (12%) (p < 0.05, Figure 6, Table 3).
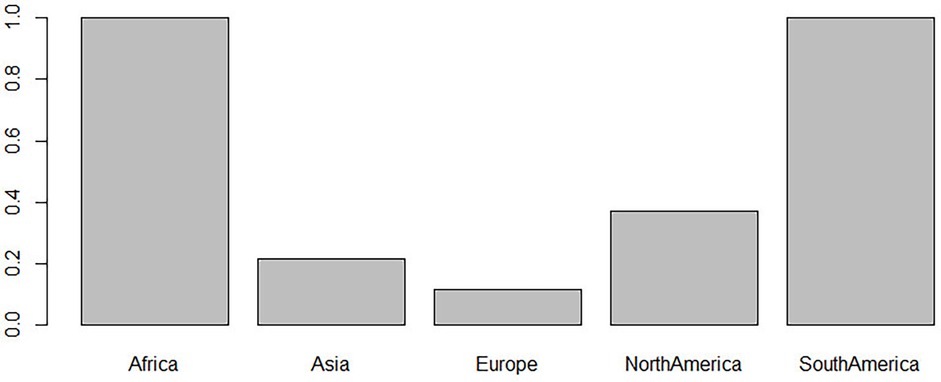
Figure 6. Y-axis proportion of nerve transfers without root exploration (ntwoRE) surgery vs. x-axis continent.
Discussion
In 1900, Thorburn described the first successful surgical repair of brachial plexus injury; however, surgical treatment failed to gain popularity (52, 53). It was not until 1967 that Millesi would pioneer the use of microsurgery in the treatment of brachial plexus injury with nerve grafting (54). In the 1980s, others such as Gilbert (55, 56) and Kawabata (57) applied microsurgical techniques to NBPP repair, with impressive results. Since then, the field has continued to evolve. This investigation was undertaken to describe how and where this evolution occurred. We documented a significant increase in age at surgery over time, changes in preferred surgical targets over time, and marked geographical differences in the management of BPBI.
Age at surgery has long been a focus among BPBI surgeons. Some favor an early (<3 months) intervention, citing potential advantages related to the biology of nerve regeneration, others seek to delay surgery, while others forego primary nerve surgery entirely (3–7, 58–62). Still, others suggest that a 3-month cutoff helps secure parental consent for potentially curative nerve surgery before limited non-operative recovery causes hesitance, introducing ethical dilemmas in the light of equivocal and low-quality evidence (1, 2, 44, 63, 64). In this systematic review, we found that, in data published over the past several decades, age at surgery has increased and the technique is more often NTwoRE. We also found that almost half of all patients from studies containing individual patient data (IPD) were treated with nerve transfers performed close to the target without exploring the supraclavicular fossa and that the proportion of patients treated this way is steadily increasing. Based on published data, the trends are moving from nerve grafts through (63) combined methods to abandoning exploration at the root level. Further, our data show variation in NBPP surgical approaches across the globe. Surgeons in North America tend to intervene at older ages and use NTwoRE nerve transfers more than surgeons in Europe and Asia.
The driving forces behind these geographical and temporal trends are not immediately apparent. In some of the included studies, authors included their rationale for abandoning supraclavicular exploration. It is important to note that in all cases, the patients had partial palsies, where potentially viable nerve stumps available for grafting could have been present and utilized if patients presented early enough. The reasons for choosing the nerve transfer approach were late presentation and recovery of shoulder function with concomitant absence of biceps function, initially non-consenting parents changing their minds, unsuccessful primary nerve surgery, and parents' choice between supraclavicular exploration or multiple nerve transfers. Others chose not to provide a reason, revealing a fundamental challenge with all NBPP studies, the large amount of surgeon's discretion. One example is the choice of outcome measures. Numerous grading systems are used: MRC force ratings, Raimondi scale, mallet, active movement scale (AMS), Gilbert shoulder score, assisting hand assessment, and more. Recently, the iPLUTO survey attempted to gather consensus on which measure is best (43). Certain outcome measures were identified for inclusion in future NBPP investigations: AROM-d, mallet, and passive ROM. The variability of plexus injury subtypes, follow-up times, and ages at surgery also raises questions as to the comparability of patient groups between studies.
Another factor that may contribute to the trends we documented is the lack of clear radiological parameters to guide diagnosis and approach to NBPP. No systematic reviews examining MRI's utility in diagnosing NBPP yet exist. Previous studies have found that the diagnostic accuracy is modest but varies depending on the location and severity of the injury and thus should remain a supplemental, not diagnostic, or treatment-guiding tool (66–68). Previous systematic reviews for adult plexus injuries concluded that MRI offers modest diagnostic accuracy and may help identify graftable stumps, but surgical exploration should remain the preferred method of diagnosis (69, 70). Given the acceptance of MRI in this treatment-guiding capacity, it is likely that factors surrounding the accuracy, availability, and interpretation of MRI have a significant impact on surgical timing and approach to NBPP. Access to MRI equipment and experienced musculoskeletal radiologists varies throughout the world, and with time (71, 72), which may contribute to the global and temporal trends that we documented. The availability of both factors, along with unambiguous MRI findings suggesting avulsion may convince surgeons to operate sooner.
Geographic trends may stem from the geographically fixed nature of NBPP training programs, whereby proponents of a certain approach train the next generation of surgeons. Another possible cause is geographic variation in the specialty responsible for NBPP surgery—pediatric surgery, plastic and reconstructive surgery, neurosurgery, or orthopedic surgery (43). For example, in the USA and Thailand, NBPP is treated largely by pediatric orthopedic surgeons; however, in France, this is not the case. Centralization of NBPP treatment may also play a role. Countries where NBPP is treated at specialized centers, such as Sweden and the UK, may have different preferences than those where treatment of NBPP is not centralized. Preferences in outcome measures were found to vary geographically by the iPLUTO survey, and this may also drive global preference in surgical approach and age at surgery (43). Differences in health systems between countries could also drive these differences. Later presentation may be more common in developing countries or those with high numbers of uninsured patients, such as the USA, or those with a low density of brachial plexus surgeons. There may be an urgency to make a decision skewed towards NtwoRE in places where follow-up is less likely.
We also found that age at surgery in NTwoRE surgeries was significantly older than the age for proximal plexus explorations. Daly et al. and Tarek et al. found that microsurgical repair via proximal plexus exploration is a viable option in late-presenting NBPP, with a combination of approaches in patients with varying degrees of severity of the palsy (73, 74). However, our findings indicate that surgeons still prefer NTwoRE when managing late-presenting patients (38). Evidence supports the notion that NTwoRE such as the Oberlin I procedure is useful in the late presentation of traumatic brachial plexus injury (75). Whether this finding translates to NBPP is yet unclear, but surgeons may be applying it thusly—our findings show that surgeons are performing more close target procedures, on older patients as time goes on (Figures 3, 4). One possible explanation is the relatively higher frequency of nerve transfer procedures in general when compared to plexus dissections. Surgeons may be more familiar with these procedures and thus more comfortable offering them to older NBPP patients. Another reason for associations between increasing age and type of surgery could be that surgeons wait longer with patients where nerve transfers would be performed to better assess the quality of donor nerves, making the decision about surgery easier. Better obstetric care leads to decreasing numbers of patients presenting with complete palsies, potentially leaving the surgeons used to perform technically easier NtwoRE procedures unprepared to tackle such cases, where difficult exploration of the brachial plexus is necessary.
The emergence and success of acellular processed nerve allografts in treating NBPP (76) may exert an opposing influence by obviating the need for donor nerve harvest or changing favored surgical approaches. These products' impacts should be followed closely in the future.
Limitations
This review included published studies only. It does not explore the full spectrum of surgeons' preferences and should be followed by a worldwide survey. Additionally, reliance on published information limited our classification of surgical approach to descriptions provided in the methods section of each paper. There were also numerous articles for which IPD was unavailable, even after attempts to contact the authors. The exclusion of these articles may have biased our results. Interpreting our results is complicated by the variability of NBPP severity that we included. We included any operative brachial plexus lesion; thus our results do not capture lesion-specific trends. Many surgeons tailor their surgical approach to the specific location of a lesion, and if there are geographic or time trends in these approaches, we are unable to detect them. The usage of publication date as the year of record also complicates our analysis. Many investigations into NBPP occur over the course of years and are published years after data collection is finished. Thus, the use of publication dates may present trends in a delayed fashion. Interpretation of data from Africa and South America is limited by the small number of included studies and patients from these areas. Finally, we analyzed trends in procedures targeted at NBPP, but not the specific deficit resulting from NBPP, largely due to the limited number of eligible papers for any given deficit. Thus, trends in procedures targeted at restoring deficits in, for example, elbow flexion vs. those targeted at restoring hand function are grouped together. More granular, deficit-based trends are not apparent from our data.
Conclusions
Age at the time of surgery for NBPP is increasing over time. Technically easier surgical approaches to NBPP surgery avoiding exploration of roots of brachial plexus are becoming more popular. Regional differences exist in the age at surgery for NBPP. North and South America tend toward later intervention while Asia and Europe favor earlier intervention. NTwoRE was most common in North America. EBP is more common in younger patients while NTwoRE is more common in older ones.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
ML: Writing – original draft, Writing – review & editing. AA: Writing – original draft, Writing – review & editing. JS: Writing – original draft. NS: Writing – original draft. JM: Writing – original draft. SG: Writing – original draft. GA: Writing – original draft. KP: Writing – original draft. KJ: Writing – original draft. YS: Writing – original draft. ZZ: Writing – original draft. JC-Y: Writing – review & editing. TC: Writing – review & editing. AC: Writing – original draft, Writing – review & editing. AM: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pondaag W, Malessy MJA. Evidence that nerve surgery improves functional outcome for obstetric brachial plexus injury. J Hand Surg Eur Vol. (2021) 46(3):229–36. doi: 10.1177/1753193420934676
2. Oberlin C. Rethinking surgical strategy in the management of obstetrical palsy. J Hand Surg Eur Vol. (2021) 46(7):705–7. doi: 10.1177/17531934211032032
3. Gilbert A, Tassin JL. Obstetrical palsy: a clinical pathologic and surgical review. J Hand Surg. (1987) 3(1):529–53. doi: 10.1016/0266-7681(91)90100-3
4. Chuang DC-C, Ma H-S. Current concepts in the management of obstetrical brachial plexus injuries: the Taipei experience. Semin Plast Surg. (2004) 18(04):309–17. doi: 10.1055/s-2004-837257
5. Clarke HM, Curtis CG. Brachial Plexus Injuries—Examination and Prognosis. Maryland Heights, MO: Dunitz M (2001).
6. Srinivasan N, Mahajan J, Gupta S, Shah YM, Shafei J, Levidy MF, et al. Surgical timing in neonatal brachial plexus palsy: a PRISMA-IPD systematic review. Microsurgery. (2022) 42(4):381–90. doi: 10.1002/micr.30871
7. Bauer AS, Kalish LA, Adamczyk MJ, Bae DS, Cornwall R, James MA, et al. Microsurgery for brachial plexus injury before versus after 6 months of age: results of the multicenter treatment and outcomes of brachial plexus injury (TOBI) study. JBJS. (2020) 102(3):194–204. doi: 10.2106/JBJS.18.01312
8. Oberlin C, Beal D, Leechavengvongs S, Salon A, Dauge MC, Sarcy JJ. Nerve transfer to biceps muscle using a part of ulnar nerve for C5‒C6 avulsion of the brachial plexus: anatomical study and report of four cases. J Hand Surg Am. (1994) 19(2):232–7. doi: 10.1016/0363-5023(94)90011-6
9. Tung TH, Novak CB, Mackinnon SE. Nerve transfers to the biceps and brachialis branches to improve elbow flexion strength after brachial plexus injuries. J Neurosurg. (2003) 98(2):313–8. doi: 10.3171/jns.2003.98.2.0313
10. Chang KWC, Wilson TJ, Popadich M, Brown SH, Chung KC, Yang LJS. Oberlin transfer compared with nerve grafting for improving early supination in neonatal brachial plexus palsy. J Neurosurg Pediatr. (2018) 21(2):178–84. doi: 10.3171/2017.8.PEDS17160
11. Bourke G, McGrath AM, Wiberg M, Novikov LN. Effects of early nerve repair on experimental brachial plexus injury in neonatal rats. J Hand Surg Eur Vol. (2018) 43(3):275–81. doi: 10.1177/1753193417732696
12. Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. Br Med J. (2016) 355:i4919. doi: 10.1136/bmj.i4919
13. United States Central Intelligence Agency. The World Factbook. Washington, DC: Central Intelligence Agency (1995). p. CD-ROMs.
15. Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. (1988) 75(4):800–2. doi: 10.1093/biomet/75.4.800
16. Hommel G. A stagewise rejective multiple test procedure based on a modified Bonferroni test. Biometrika. (1988) 75(2):383–6. doi: 10.1093/biomet/75.2.383
17. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. (1995) 57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x
18. Benjamini Y, Yekutieli D. The control of the false discovery rate in multiple testing under dependency. Ann Stat. (2001) 29. doi: 10.1214/aos/1013699998
19. Alanen M, Halonen JP, Katevuo K, Vilkki P. Early surgical exploration and epineural repair in birth brachial palsy. Z Kinderchir. (1986) 41(6):335–7. doi: 10.1055/s-2008-1043371
20. Xu J, Cheng X, Gu Y. Different methods and results in the treatment of obstetrical brachial plexus palsy. J Reconstr Microsurg. (2000) 16(6):417–22. doi: 10.1055/s-2006-947147
21. Anand P, Birch R. Restoration of sensory function and lack of long-term chronic pain syndromes after brachial plexus injury in human neonates. Brain. (2002) 125(Pt 1):113–22. doi: 10.1093/brain/awf017
22. Noaman HH, Shiha AE, Bahm J. Oberlin’s ulnar nerve transfer to the biceps motor nerve in obstetric brachial plexus palsy: indications, and good and bad results. Microsurgery. (2004) 24(3):182–7. doi: 10.1002/micr.20037
23. Chuang DC, Yeh MC, Wei FC. Intercostal nerve transfer of the musculocutaneous nerve in avulsed brachial plexus injuries: evaluation of 66 patients. J Hand Surg Am. (1992) 17(5):822–8. doi: 10.1016/0363-5023(92)90451-t
24. Pondaag W, Malessy MJ. Recovery of hand function following nerve grafting and transfer in obstetric brachial plexus lesions. J Neurosurg. (2006) 105(1 Suppl):33–40. doi: 10.3171/ped.2006.105.1.33
25. Blaauw G, Sauter Y, Lacroix CL, Slooff AC. Hypoglossal nerve transfer in obstetric brachial plexus palsy. J Plast Reconstr Aesthet Surg. (2006) 59(5):474–8. doi: 10.1016/j.bjps.2005.07.013
26. Ashley WW Jr, Weatherly T, Park TS. Collagen nerve guides for surgical repair of brachial plexus birth injury. J Neurosurg. (2006) 105(6 Suppl):452–6. doi: 10.3171/ped.2006.105.6.452
27. Palmgren T, Peltonen J, Linder T, Rautakorpi S, Nietosvaara Y. Sensory evaluation of the hands in children with brachial plexus birth injury. Dev Med Child Neurol. (2007) 49(8):582–6. doi: 10.1111/j.1469-8749.2007.00582.x
28. Badr Y, O'Leary S, Kline DG. Management of one hundred seventy-one operative and nonoperative obstetrical birth palsies at the Louisiana State University Health Sciences Center. Neurosurgery. (2009) 65(4 Suppl):A67–73. doi: 10.1227/01.NEU.0000345942.14391.1C
29. Wellons JC, Tubbs RS, Pugh JA, Bradley NJ, Law CR, Grabb PA. Medial pectoral nerve to musculocutaneous nerve neurotization for the treatment of persistent birth-related brachial plexus palsy: an 11-year institutional experience. J Neurosurg Pediatr. (2009) 3(5):348–53. doi: 10.3171/2008.11.PEDS08166
30. Lin H, Hou C, Chen D. Modified C7 neurotization for the treatment of obstetrical brachial plexus palsy. Muscle Nerve. (2010) 42(5):764–8. doi: 10.1002/mus.21752
31. Gosk J, Rutowski R, Urban M, Wiącek R, Mazurek P, Wnukiewicz W. Neurolysis of the conducting neuroma-in-continuity in perinatal brachial plexus palsy—evaluation of the results of surgical treatment. Folia Neuropathol. (2011) 49(3):197–203.22101953
32. Luo PB, Chen L, Zhou CH, Hu SN, Gu YD. Results of intercostal nerve transfer to the musculocutaneous nerve in brachial plexus birth palsy. J Pediatr Orthop. (2011) 31(8):884–8. doi: 10.1097/BPO.0b013e318230a783
33. Lin H, Hou C, Chen D. Contralateral C7 transfer for the treatment of upper obstetrical brachial plexus palsy. Pediatr Surg Int. (2011) 27(9):997–1001. doi: 10.1007/s00383-011-2894-4
34. Siqueira MG, Socolovsky M, Heise CO, Martins RS, Di Masi G. Efficacy and safety of Oberlin’s procedure in the treatment of brachial plexus birth palsy. Neurosurgery. (2012) 71(6):1156–61. doi: 10.1227/NEU.0b013e318271ee4a
35. Al-Qattan MM, El-Sayed AA. The use of the phrenic nerve communicating branch to the fifth cervical root for nerve transfer to the suprascapular nerve in infants with obstetric brachial plexus palsy. Biomed Res Int. (2014) 2014:153182. doi: 10.1155/2014/153182
36. Bade SA, Lin JC, Curtis CG, Clarke HM. Extending the indications for primary nerve surgery in obstetrical brachial plexus palsy. Biomed Res Int. (2014) 2014:627067. doi: 10.1155/2014/627067
37. Mencl L, Waldauf P, Haninec P. Results of nerve reconstructions in treatment of obstetrical brachial plexus injuries. Acta Neurochir (Wien). (2015) 157(4):673–80. doi: 10.1007/s00701-015-2347-2
38. Sénès F, Catena N, Sénès J. Nerve transfer in delayed obstetrical palsy repair. J Brachial Plex Peripher Nerve Inj. (2015) 10(1):e2–14. doi: 10.1055/s-0035-1549367
39. Bhandari PS, Deb P. Dorsal approach in transfer of the distal spinal accessory nerve into the suprascapular nerve: histomorphometric analysis and clinical results in 14 cases of upper brachial plexus injuries. J Hand Surg Am. (2011) 36(7):1182–90. doi: 10.1016/j.jhsa.2011.02.025
40. Leblebicioglu G, Ayhan C, Firat T, Uzumcugil A, Yorubulut M, Doral MN. Recovery of upper extremity function following endoscopically assisted contralateral C7 transfer for obstetrical brachial plexus injury. J Hand Surg Eur Vol. (2016) 41(8):863–74. doi: 10.1177/1753193416638999
41. Gibon E, Romana C, Vialle R, Fitoussi F. Isolated C5‒C6 avulsion in obstetric brachial plexus palsy treated by ipsilateral C7 neurotization to the upper trunk: outcomes at a mean follow-up of 9 years. J Hand Surg Eur Vol. (2016) 41(2):185–90. doi: 10.1177/1753193415593493
42. Figueiredo Rde M, Grechi G, Gepp Rde A. Oberlin’s procedure in children with obstetric brachial plexus palsy. Childs Nerv Syst. (2016) 32(6):1085–91. doi: 10.1007/s00381-015-3007-9
43. Argenta AE, Brooker J, MacIssac Z, Natali M, Greene S, Stanger M, et al. Obstetrical brachial plexus palsy: can excision of upper trunk neuroma and nerve grafting improve function in babies with adequate elbow flexion at nine months of age? J Plast Reconstr Aesthet Surg. (2016) 69(5):629–33. doi: 10.1016/j.bjps.2015.12.020
44. Ghanghurde BA, Mehta R, Ladkat KM, Raut BB, Thatte MR. Distal transfers as a primary treatment in obstetric brachial plexus palsy: a series of 20 cases. J Hand Surg Eur Vol. (2016) 41(8):875–81. doi: 10.1177/1753193416663887
45. Murison J, Jehanno P, Fitoussi F. Nerve transfer to biceps to restore elbow flexion and supination in children with obstetrical brachial plexus palsy. J Child Orthop. (2017) 11(6):455–9. doi: 10.1302/1863-2548.11.170125
46. Vu AT, Sparkman DM, van Belle CJ, Yakuboff KP, Schwentker AR. Retropharyngeal contralateral C7 nerve transfer to the lower trunk for brachial plexus birth injury: technique and results. J Hand Surg Am. (2018) 43(5):417–24. doi: 10.1016/j.jhsa.2017.12.001
47. Azzi AJ, AlNaeem H, Aubin-Lemay C, Kvann JC, Alam P, Retrouvey H, et al. Restoration of shoulder motion using single- versus dual-nerve repair in obstetrical brachial plexus injury. J Neurosurg Pediatr. (2018) 21(5):511–5. doi: 10.3171/2017.11.PEDS17493
48. Semaya AE, El-Nakeeb R, Hasan M, Shams A. Intercostal nerve transfer in management of biceps and triceps cocontraction in spontaneously recovered obstetric brachial plexus palsy. Ann Plast Surg. (2019) 83(4):447–51. doi: 10.1097/SAP.0000000000002075
49. Blaauw G, Slooff AC. Transfer of pectoral nerves to the musculocutaneous nerve in obstetric upper brachial plexus palsy. Neurosurgery. (2003) 53(2):338–42. doi: 10.1227/01.neu.0000073420.66113.66
50. Grossman JA, DiTaranto P, Yaylali I, Alfonso I, Ramos LE, Price AE. Shoulder function following late neurolysis and bypass grafting for upper brachial plexus birth injuries. J Hand Surg Br. (2004) 29(4):356–8. doi: 10.1016/j.jhsb.2004.03.008
51. Lagerkvist AL, Johansson U, Johansson A, Bager B, Uvebrant P. Obstetric brachial plexus palsy: a prospective, population-based study of incidence, recovery, and residual impairment at 18 months of age. Dev Med Child Neurol. (2010) 52(6):529–34. doi: 10.1111/j.1469-8749.2009.03479.x
52. Thorburn W. A clinical lecture on secondary suture of the brachial plexus. Br Med J. (1900) 1(2053):1073–5. doi: 10.1136/bmj.1.2053.1073
53. Pirela-Cruz M, Mujadzic M, Kanlic E. Brachial plexus treatment. Bosn J Basic Med Sci. (2005) 5(3):7–15. doi: 10.17305/bjbms.2005.3264
54. Millesi H. Nerve transplantation for reconstruction of peripheral nerves injured by the use of the microsurgical technic. Minerva Chir. (1967) 22(17):950–1.6055379
55. Gilbert A, Tassin JL. Surgical repair of the brachial plexus in obstetric paralysis. Chirurgie. (1984) 110(1):70–5.6734350
56. Gilbert A, Khouri N, Carlioz H. Birth palsy of the brachial plexus–surgical exploration and attempted repair in twenty-one cases (author’s transl). Rev Chir Orthop Reparatrice Appar Mot. (1980) 66(1):33–42.6447338
57. Kawabata H, Masada K, Tsuyuguchi Y, Kawai H, Ono K, Tada R. Early microsurgical reconstruction in birth palsy. Clin Orthop Relat Res. (1987) 215:233–42. doi: 10.1097/00003086-198702000-00034
58. Chuang DC, Mardini S, Ma HS. Surgical strategy for infant obstetrical brachial plexus palsy: experiences at Chang Gung Memorial Hospital. Plast Reconstr Surg. (2005) 116(1):132–42; discussion 43–4. doi: 10.1097/01.PRS.0000169936.19073.B4
59. Philandrianos C, Baiada A, Salazard B, Benaim J, Casanova D, Magalon G, et al. Management of upper obstetrical brachial plexus palsy. Long-term results of non-operative treatment in 22 children. Ann Chir Plast Esthet. (2013) 58(4):327–35. doi: 10.1016/j.anplas.2011.05.002
60. DiTaranto P, Campagna L, Price AE, Grossman JA. Outcome following nonoperative treatment of brachial plexus birth injuries. J Child Neurol. (2004) 19(2):87–90. doi: 10.1177/08830738040190020101
61. Azzi AJ, Aubin-Lemay C, Kvann JC, Retrouvey H, Aldekhayel S, Zadeh T. Prompt referral in the nonoperative treatment of obstetrical brachial plexus injuries. Plast Reconstr Surg Glob Open. (2017) 5(12):e1587. doi: 10.1097/GOX.0000000000001587
62. Gilbert A, Pivato G, Kheiralla T. Long-term results of primary repair of brachial plexus lesions in children. Microsurgery. (2006) 26(4):334–42. doi: 10.1002/micr.20248
63. Sung CW, Huang JJ, Mao SH, Heredero S, Chen WF, Nguyen J, et al. International microsurgery club webinar series-bridging the knowledge gap during the COVID-19 pandemic. J Reconstr Microsurg. (2022) 38(4):296–305. doi: 10.1055/s-0041-1732427
64. Shafei J, Levidy MF, Srinivasan N, Mahajan J, Gupta S, Abdelmalek G, et al. Trends of age and geographical location in microsurgical treatment of obstetric brachial plexus palsy. Bull Hosp Jt Dis (2013). 2022;80(2):195–9.35643484
65. Pondaag W, Malessy MJA. Outcome assessment for brachial plexus birth injury. Results from the iPluto world-wide consensus survey. J Orthop Res. (2018) 36(9):2533–41.29566312
66. Gad DM, Hussein MT, Omar NNM, Kotb MM, Abdel-Tawab M, Yousef HAZ. Role of MRI in the diagnosis of adult traumatic and obstetric brachial plexus injury compared to intraoperative findings. Egypt J Radiol Nucl Med. (2020) 51(1):195. doi: 10.1186/s43055-020-00310-2
67. Grahn P, Pöyhiä T, Sommarhem A, Nietosvaara Y. Clinical significance of cervical MRI in brachial plexus birth injury. Acta Orthop. (2019) 90(2):111–8. doi: 10.1080/17453674.2018.1562621
68. Hung ND, Duc NM, Xoan NT, Doan NV, Huyen TTT, Dung LT. Diagnostic function of 3-tesla magnetic resonance imaging for the assessment of brachial plexus injury. Ann Neurosci. (2020) 27(3-4):124–30. doi: 10.1177/0972753120963299
69. Wade RG, Takwoingi Y, Wormald JCR, Ridgway JP, Tanner S, Rankine JJ, et al. MRI for detecting root avulsions in traumatic adult brachial plexus injuries: a systematic review and meta-analysis of diagnostic accuracy. Radiology. (2019) 293(1):125–33. doi: 10.1148/radiol.2019190218
70. Yeow YJ, Yeow KM, Su IH, Wu YM, Chen CM, Tseng JH, et al. Predicting healthy C5 spinal nerve stumps eligible for grafting with MRI, Tinel test, and rhomboid electromyography: a retrospective study of 295 consecutive brachial plexus surgeries. Radiology. (2021) 300(1):141–51. doi: 10.1148/radiol.2021202817
71. Organization WH. Medical Equipment Data by Country Global Health Observatory Data Repository 2016. Available online at: https://apps.who.int/gho/data/node.main.510 (Accessed March 29, 2022).
72. Nakajima Y, Yamada K, Imamura K, Kobayashi K. Radiologist supply and workload: international comparison. Radiat Med. (2008) 26(8):455–65. doi: 10.1007/s11604-008-0259-2
73. Daly MC, Bauer AS, Lynch H, Bae DS, Waters PM, Treatment and Outcomes of Brachial Plexus Birth Injury (TOBI) Study Group, et al. Outcomes of late microsurgical nerve reconstruction for brachial Plexus birth injury. J Hand Surg Am. (2020) 45(6):555.e1–9. doi: 10.1016/j.jhsa.2019.10.036
74. El-Gammal TA, El-Sayed A, Kotb MM, Saleh WR, Ragheb YF, Refai OA, et al. Long-term results of microsurgical brachial plexus reconstruction in late-presenting cases of brachial Plexus birth injury. J Hand Surg Am. (2023) 48(2):126–33. doi: 10.1016/j.jhsa.2022.11.003
75. Sedain G, Sharma MS, Sharma BS, Mahapatra AK. Outcome after delayed Oberlin transfer in brachial plexus injury. Neurosurgery. (2011) 69(4):822–7; discussion 7–8. doi: 10.1227/NEU.0b013e31822848eb
Keywords: brachial plexus, neonatal brachial palsy, trends, nerve transfer, nerve exploration
Citation: Levidy MF, Azer A, Shafei J, Srinivasan N, Mahajan J, Gupta S, Abdelmalek G, Pant K, Jain K, Shah Y, Zheng Z, Chuieng-Yi Lu J, Chang TN-J, Chu A and McGrath A (2025) Global trends in surgical approach to neonatal brachial plexus palsy: a systematic review. Front. Surg. 11:1359719. doi: 10.3389/fsurg.2024.1359719
Received: 21 December 2023; Accepted: 20 June 2024;
Published: 6 January 2025.
Edited by:
Filippo Maria Senes, Casa di Cura Villa Serena GVM, ItalyReviewed by:
Nunzio Catena, Giannina Gaslini Institute (IRCCS), ItalyErica Michela Cavalli, IRCCS San Gerardo dei Tintori Foundation, Italy
Copyright: © 2025 Levidy, Azer, Shafei, Srinivasan, Mahajan, Gupta, Abdelmalek, Pant, Jain, Shah, Zheng, Chuieng-Yi Lu, Chang, Chu and McGrath. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alice Chu, Y2h1YWxAbmptcy5ydXRnZXJzLmVkdQ==; Aleksandra McGrath, YWxla3NhbmRyYS5tY2dyYXRoQHVtdS5zZQ==
 Michael F. Levidy1
Michael F. Levidy1 Amanda Azer
Amanda Azer George Abdelmalek
George Abdelmalek Kunj Jain
Kunj Jain Tommy Nai-Jen Chang
Tommy Nai-Jen Chang Alice Chu
Alice Chu Aleksandra McGrath
Aleksandra McGrath