- 1Department of Orthopedics, Ordos Central Hospital, Ordos, China
- 2Critical Care Medicine, Ordos Central Hospital, Ordos, China
Background: Adjacent segmental degeneration after lumbar fusion is one of the common long-term complications after lumbar fusion. With the continuous development of adjacent segmental degeneration, patients who fail conservative treatment often need reoperation to relieve symptoms. In recent years, the technique of bilateral microdecompression through unilateral approach under microchannel has been widely used in the treatment of lumbar degenerative diseases. However, the efficacy of this procedure for adjacent-segment degeneration after lumbar fusion has not been established. Here, we report a case of bilateral microscopic decompression via a unilateral approach through a microchannel in a patient with adjacent segmental degeneration after lumbar fusion.
Case report: A 70-year-old male patient was admitted to hospital because of lumbago accompanied by left lower extremity pain, numbness and weakness for 2 years, which aggravated for 2 months. Ten years ago, he underwent PLIF for lumbar spinal stenosis, and recovered well after the operation. According to imaging data and physical examination, the diagnosis was adjacent segmental degeneration after lumbar fusion. Bilateral microdecompression was performed through a unilateral approach under a microchannel. Good clinical outcomes was observed through 1-year postoperative follow-up.
Conclusions: This report reports the successful treatment of a patient with ASD 10 years after lumbar fusion. Bilateral microdecompression via a unilateral approach under a microchannel is a safe and effective method for the treatment of ASD after lumbar fusion with good surgical outcomes.
Introduction
Degenerative lumbar disease can be treated with lumbar fusion, but it may lead to spinal lesions in previously fused levels (1, 2). Adjacent segment degeneration (ASD) is a long-term complication that can occur after lumbar fusion, which refers to the degeneration of the intervertebral disc, instability, and slippage in the adjacent segment of the fusion segment (3). Current retrospective studies have shown that lumbar fusion surgery may lead to problems with adjacent motion segments, specifically post-fusion ASD (4). Battie et al. (5) found that fusion surgery does not directly cause this phenomenon, ASD can be considered a natural part of the aging process. However, changes in stress may play a role in this process. An in vitro mechanical study found that lumbar fusion can cause abnormal pressure in the intervertebral disc and excessive motion of adjacent spinal segments, which may contribute to ASD (6). As ASD continues to evolve, patients who do not respond to conservative treatment may require reoperation to alleviate symptoms. Numerous studies have indicated that adjacent segment degeneration occurs in 5%–75% of cases after lumbar fusion, with 20% requiring additional surgical intervention (7, 8). As ASD continues to develop, patients who do not respond to conservative treatment often require reoperation to alleviate symptoms. One common approach to addressing ASD after lumbar fusion is through posterior lumbar interbody fusion (PLIF). However, revising ASD with traditional PLIF carries certain risks. This operation involves extensive soft tissue stripping to expose the original internal fixation, resulting in significant bleeding, high postoperative pain levels at the incision site, a long recovery time, and high costs. In recent years, surgeons have been exploring less invasive procedures in order to enhance clinical outcomes. One such procedure, proposed by Young et al. (9) was the use of microscope-assisted unilateral laminectomy for the treatment of lumbar spinal stenosis. This procedure involves peeling off the muscles on one side of the paravertebral side and performing microdecompression delicately under a microscope. In recent years, minimally invasive spinal surgeries such as unilateral approach and bilateral microdecompression under percutaneous microchannel have become the forefront of spinal treatment. The intermuscular approach is used instead of the traditional subperiosteal muscle stripping, which reduces tissue damage and speeds up recovery. However, the effectiveness of bilateral microdecompression via a unilateral approach through percutaneous microchannels in treating ASD after lumbar fusion has not been established. This case report presents a successful treatment of ASD 10 years after lumbar fusion using bilateral microdecompression through a unilateral approach via percutaneous microchannel.
Case presentation
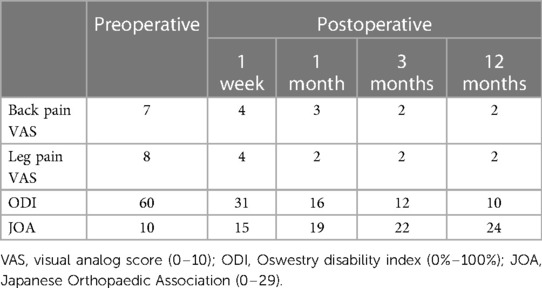
A 70-year-old male patient was admitted to hospital because of lumbago accompanied by left lower extremity pain, numbness and weakness for 2 years, which aggravated for 2 months. Ten years ago, he underwent PLIF for lumbar spinal stenosis, and recovered well after the operation. Physical examination revealed tenderness and percussion pain in the L3–4 spine area, and limited lumbar extension. Decreased skin sensation in the medial calf and medial malleolus of the left lower extremity. The muscle strength of the left lower extremity was grade III, the muscle strength of the right lower limb was grade IV, and the muscle tone was normal. The straight leg raising test of the left lower extremity was positive (30 degrees), and the straight leg raising test of the right lower extremity was negative. Physiological reflexes of the lower limbs were elicited normally, but pathological reflexes were not elicited. Based on the Japanese Orthopaedic Association (JOA) scoring system, the neurological function score of the patient was 10 points. Back pain Visual Analogue Scale (VAS) score is 7 points, leg pain VAS score is 8 points. Preoperative lumbar spine Oswestry Disability Index (ODI) score was 60%.
Magnetic resonance imaging (MRI) revealed disc herniation at the L3/4 level, along with hypertrophy of the ligamentum flavum, inward hyperplasia of the articular process, and spinal canal stenosis (Figure 1). A diagnosis of ASD after lumbar fusion was made. The treatment plan for ASD after lumbar fusion involved bilateral microdecompression through a unilateral percutaneous microchannel approach.
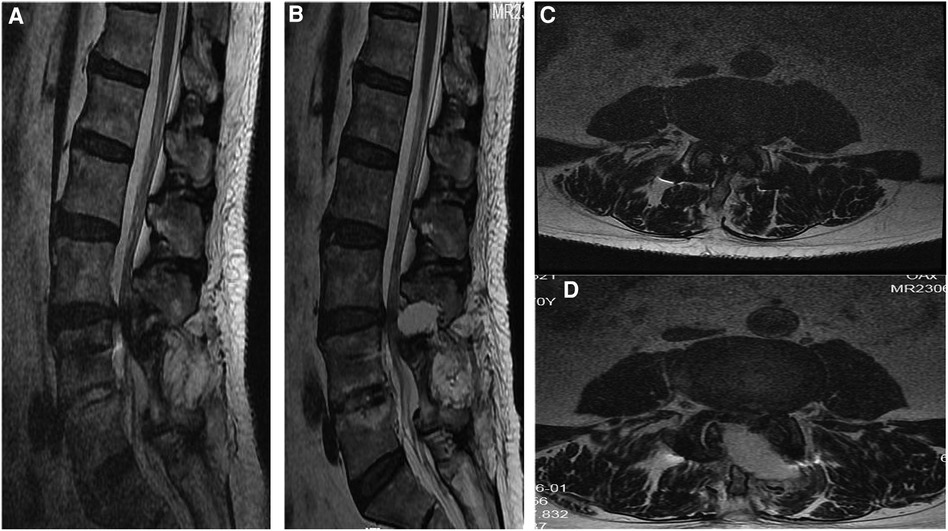
Figure 1. Preoperative and postoperative thoracic MRI. (A) Sagittal T2-weighted imaging showed spinal canal stenosis at the L3/4. (B) Three months after the operation, the sagittal view of the lumbar spine MRI showed satisfactory decompression at L3/4. (C) Axial t2-weighted imaging showing hypertrophy of the ligamentum flavum at the L3/4 level, causing spinal stenosis. (D) Three months after the operation, the lumbar spine MRI axial view showed satisfactory decompression at L3/4.
Surgical treatment
After successful general anesthesia, the patient was placed in a prone position with the abdomen suspended, and a neurophysiological monitoring system was established. Accurately locate the narrowed spinal canal under the C-arm, and make a longitudinal skin incision 2.5 cm to the left of the posterior midline at the position corresponding to the spinal canal stenosis, with a length of about 1.8 cm. The subcutaneous and fascia were incised sequentially, and the paravertebral expansion cannula was used to bluntly separate the muscle layer step by step through a Gram needle, and a surgical microchannel (diameter of 1.6 cm) was inserted under the guidance of the expansion cannula (Figure 2). The expansion sleeve was placed along the periphery and connected to the fixation rod through a serpentine chain. It was then fixed beside the bed. The C-arm was used to confirm that the channel was at the level of the spinal canal stenosis. Install a microscope, use a drill to remove the root of the lumbar 3 spinous process and the lower edge of the L3 lamina, and open the lamina according to the preoperative imaging data. The ligamentum flavum is then removed with a rongeur. The left lumbar 4 nerve root was released, the nerve root canal was enlarged, and it was observed that the nerve was obviously released. Adjust the direction of the working channel, grind the right part of the inferior articular process of L3, resect the thickened ligamentum flavum between L3 and L4 on the right side, loosen the nerve root of L4 on the right side, expand the nerve root canal, and observe that the nerve is obviously released2 (Figure 3). During the surgery, the amount of blood lost was approximately 30 ml. Following the procedure, there was a slight improvement in muscle strength in the lower extremities.
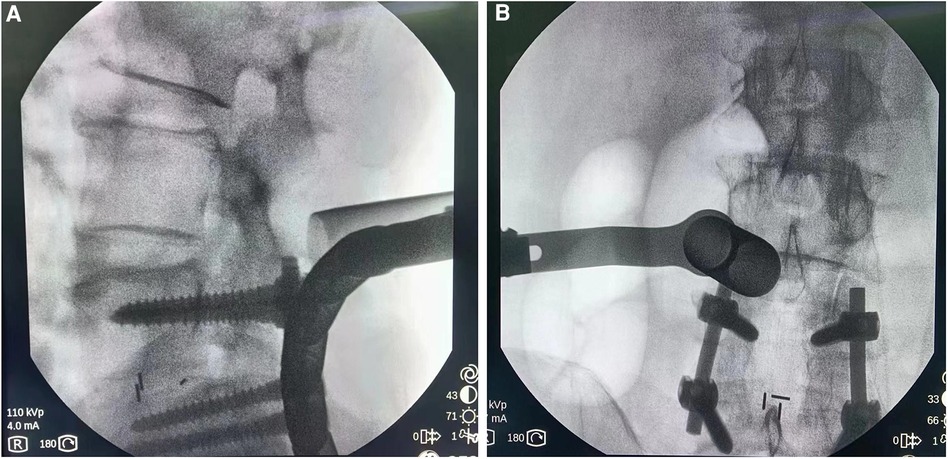
Figure 2. Intraoperative fluoroscopy (A) lateral view shows channel localization at L3/4 level. (B) The orthographic map shows channel localization at the L3/4 level.
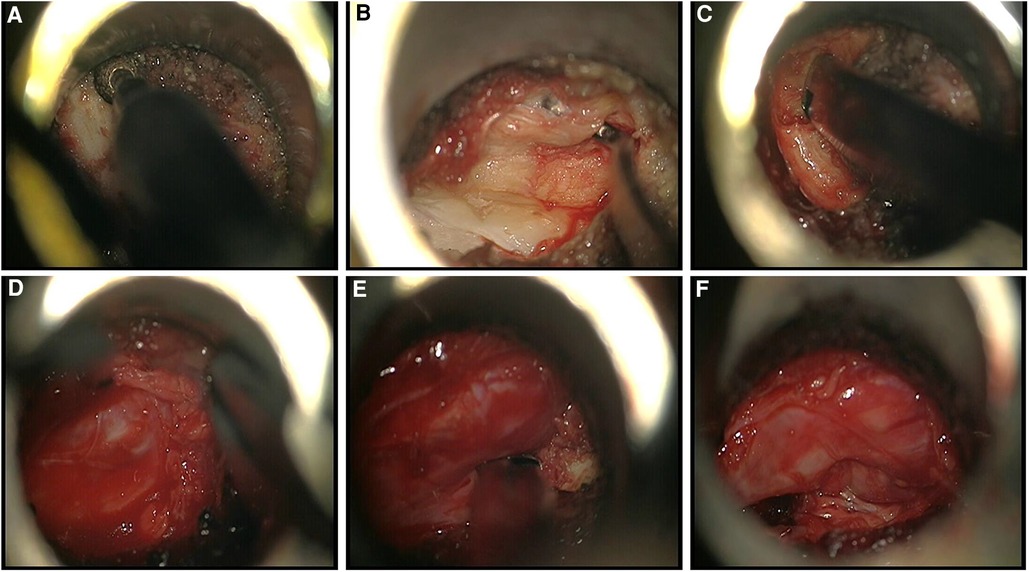
Figure 3. Intraoperative findings. (A) Removal of the lamina and spinous process bases using a powered system. (B) Exposed hypertrophic ligamentum flavum. (C) Removal of hypertrophic ligamentum flavum using Kerrison rongeurs. (D) Bipolar radiofrequency was used for hemostasis. (E) Removal of hypertrophic bone tissue using Kerrison rongeurs. (F) Nerve root after decompression.
Results
The patient experienced immediate relief from lower extremity and back pain after the operation. At last follow-up, the patient's VAS score for back pain and leg pain was 2. Within 2 weeks, the muscle strength of the left lower limb improved to grade IV, and the muscle strength of the right lower limb improved to grade IV+. Prior to the operation, the patient had a JOA score of 10 points. After 1 year of follow-up, the JOA score increased to 23 points, resulting in a 73% improvement rate in JOA score after treatment. The patient had an ODI score of 60% prior to the operation. After a year of follow-up, the ODI score showed significant improvement, reaching 10% (Table 1). Postoperative CT and MRI showed satisfactory decompression at the L3–4 level, the articular process was well preserved, and the stability of the lumbar spine was not damaged (Figures 1, 4).
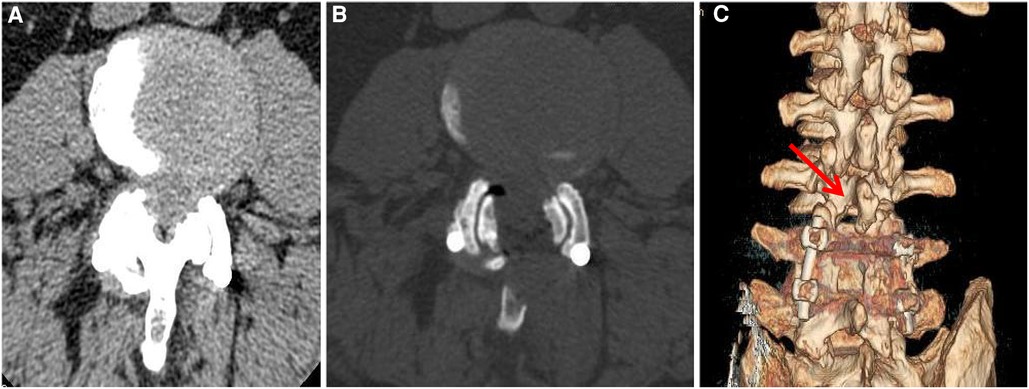
Figure 4. Preoperative and postoperative computed tomography (CT). (A) Preoperative CT showed hypertrophy of the ligamentum flavum at the L3/4 level, hypertrophy of the facet joints, and spinal canal stenosis. (B) Three months after the operation, CT of the lumbar spine showed satisfactory decompression at the L3/4 level, and the facet joints were well preserved. (C) At 3 months after the operation, three-dimensional reconstruction CT of the lumbar spine showed that the facet joints at the L3/4 level were well preserved.
Discussion
This study reports on the clinical effects of 10-year ASD after lumbar fusion with bilateral microdecompression via a unilateral approach under a microchannel. The method used in this study can effectively decompress neural structures without significantly destabilizing the spine. The results showed significant improvement in VAS scores for back pain and leg pain, with a JOA improvement rate of 73% at the last follow-up. Postoperative imaging results indicated that there was no obvious spinal instability at the decompression segment and the decompression effect was satisfactory. Lumbar fusion is a well-established treatment option for degenerative lumbar disease (10, 11). When adjacent segment disease (ASD) develops following lumbar fusion, many surgeons opt for decompression by extending internal fixation (12, 13). However, we propose a more minimally invasive approach that involves bilateral microdecompression through a unilateral approach under a microchannel. This approach has yielded good surgical outcomes for patients with ASD after lumbar fusion. Our results are comparable or even better than those reported in other studies that have used extended decompression with internal fixation after lumbar fusion.
When considering treatment options for the lumbar spine, the cost of hospitalization is an important factor for patients. Bilateral microdecompression via a unilateral approach under a microchannel is a less expensive option compared to extended internal fixation and fusion because it does not require implant costs (14). Lumbar fusion surgery has been found to have a higher incidence of perioperative morbidity, as well as longer hospital stays and recovery times. These factors should be taken into consideration when evaluating the potential benefits and risks of this type of surgery (15). The microchannel is placed using the intermuscular approach to avoid scar tissue from previous surgery and minimize damage to muscle tissue. This technique can potentially decrease post-surgical pain, wound complications, and the risk of infection. To the best of our knowledge, this is the first report of bilateral microdecompression using a percutaneous microchannel unilateral approach for ASD 10 years after lumbar fusion. In this case, we analyzed clinicoradiologic data and made an accurate diagnosis before surgery. A surgical strategy was then developed to determine the extent of decompression segments and intraoperative decompression. The combination of percutaneous microchannel, microscope, burr and unilateral approach and bilateral decompression technology can fully decompress during operation and ensure the success of minimally invasive surgery.
In this study, we found that bilateral microdecompression via a unilateral approach under a microchannel is a safe and effective method for the treatment of ASD after lumbar fusion with good surgical outcomes. In the future, studies with longer follow-up and larger samples are needed to determine long-term prognosis. Furthermore, we have not yet conducted a comparative study of microdecompression and standard decompression. This is another limitation of this study and a new direction for future research.
Conclusion
This report reports the successful treatment of a patient with ASD 10 years after lumbar fusion. Bilateral microdecompression via a unilateral approach under a microchannel is a safe and effective method for the treatment of ASD after lumbar fusion with good surgical outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
TZ: Writing – original draft. GG: Writing – original draft. FG: Writing – original draft. NG: Writing – review & editing. YW: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fenton-White HA. Trailblazing: the historical development of the posterior lumbar interbody fusion (PLIF). Spine J. (2021) 21(9):1528–41. doi: 10.1016/j.spinee.2021.03.016
2. Rathbone J, Rackham M, Nielsen D, Lee SM, Hing W, Riar S, et al. A systematic review of anterior lumbar interbody fusion (ALIF) versus posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF), posterolateral lumbar fusion (PLF). Eur Spine J. (2023) 32(6):1911–26. doi: 10.1007/s00586-023-07567-x
3. Lee CK. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine (Phila Pa 1976). (1988) 13(3):375–7. doi: 10.1097/00007632-198803000-00029
4. Kumar MN, Jacquot F, Hall H. Long-term follow-up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J. (2001) 10(4):309–13. doi: 10.1007/s005860000207
5. Battié MC, Videman T, Parent E. Lumbar disc degeneration: epidemiology and genetic influences. Spine (Phila Pa 1976). (2004) 29(23):2679–90. doi: 10.1097/01.brs.0000146457.83240.eb
6. Lee CS, Hwang CJ, Lee SW, Ahn YJ, Kim YT, Lee DH, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. (2009) 18(11):1637–43. doi: 10.1007/s00586-009-1060-3
7. Imagama S, Kawakami N, Matsubara Y, Tsuji T, Ohara T, Katayama Y, et al. Radiographic adjacent segment degeneration at 5 years after L4/5 posterior lumbar interbody fusion with pedicle screw instrumentation: evaluation by computed tomography and annual screening with magnetic resonance imaging. Clin Spine Surg. (2016) 29(9):E442–51. doi: 10.1097/BSD.0b013e31828aec78
8. Lee JC, Kim Y, Soh JW, Shin BJ. Risk factors of adjacent segment disease requiring surgery after lumbar spinal fusion: comparison of posterior lumbar interbody fusion and posterolateral fusion. Spine (Phila Pa 1976). (2014) 39(5):E339–45. doi: 10.1097/BRS.0000000000000164
9. Young S, Veerapen R, O’Laoire SA. Relief of lumbar canal stenosis using multilevel subarticular fenestrations as an alternative to wide laminectomy: preliminary report. Neurosurgery. (1988) 23(5):628–33. doi: 10.1227/00006123-198811000-00014
10. Lawrence BD, Wang J, Arnold PM, Hermsmeyer J, Norvell DC, Brodke DS. Predicting the risk of adjacent segment pathology after lumbar fusion: a systematic review. Spine (Phila Pa 1976). (2012) 37(22 Suppl):S123–32. doi: 10.1097/BRS.0b013e31826d60d8
11. Kasliwal MK, Shaffrey CI, Lenke LG, Dettori JR, Ely CG, Smith JS. Frequency, risk factors, and treatment of distal adjacent segment pathology after long thoracolumbar fusion: a systematic review. Spine (Phila Pa 1976). (2012) 37(22 Suppl):S165–79. doi: 10.1097/BRS.0b013e31826d62c9
12. Adogwa O, Carr RK, Kudyba K, Karikari I, Bagley CA, Gokaslan ZL, et al. Revision lumbar surgery in elderly patients with symptomatic pseudarthrosis, adjacent-segment disease, or same-level recurrent stenosis. Part 1. Two-year outcomes and clinical efficacy: clinical article. J Neurosurg Spine. (2013) 18(2)):139–46. doi: 10.3171/2012.11.SPINE12224
13. Miwa T, Sakaura H, Yamashita T, Suzuki S, Ohwada T. Surgical outcomes of additional posterior lumbar interbody fusion for adjacent segment disease after single-level posterior lumbar interbody fusion. Eur Spine J. (2013) 22(12):2864–8. doi: 10.1007/s00586-013-2863-9
14. Lubelski D, Mihalovich KE, Skelly AC, Fehlings MG, Harrop JS, Mummaneni PV, et al. Is minimal access spine surgery more cost-effective than conventional spine surgery? Spine (Phila Pa 1976). (2014) 39(22 Suppl 1):S65–74. doi: 10.1097/BRS.0000000000000571
15. Parker SL, Mendenhall SK, Shau DN, Zuckerman SL, Godil SS, Cheng JS, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg. (2014) 82(1-2):230–8. doi: 10.1016/j.wneu.2013.01.041
Keywords: percutaneous microchannel, adjacent segmental degeneration, microchannel, micro decompression, lumbar
Citation: Zhang T, Gao G, Gao F, Guo N and Wang Y (2024) Percutaneous microchannel unilateral approach bilateral micro decompression for adjacent segmental degeneration after lumbar fusion at 10 years: a case report and review of literature. Front. Surg. 11:1284967. doi: 10.3389/fsurg.2024.1284967
Received: 29 August 2023; Accepted: 8 January 2024;
Published: 24 January 2024.
Edited by:
Laura Scaramuzzo, Ospedale Galeazzi S.p.A, ItalyReviewed by:
Osvaldo Mazza, Bambino Gesù Children’s Hospital (IRCCS), ItalyMaria Ludovica Pallotta, IRCCS Ospedale Galeazzi Sant’Ambrogio, Italy
© 2024 Zhang, Gao, Gao, Guo and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nana Guo Z3VvbmFuYWljdTJAMTYzLmNvbQ== Yongjiang Wang d3lqOTQ4MjYxNTEwQDE2My5jb20=
†These authors have contributed equally to this work
Abbreviations ASD, adjacent segment degeneration; PLIF, posterior lumbar interbody fusion; JOA, Japanese Orthopaedic Association; VAS, visual analogue scale; ODI, Oswestry disability index.
 Tingxin Zhang1,†
Tingxin Zhang1,† Yongjiang Wang
Yongjiang Wang